Académique Documents
Professionnel Documents
Culture Documents
Pedia Practice Test With Answers
Transféré par
nycjg15Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pedia Practice Test With Answers
Transféré par
nycjg15Droits d'auteur :
Formats disponibles
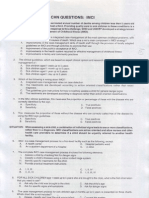
1. To examine an infant's thyroid gland, the nurse should place the infant in which position? a. Prone b. Sitting c.
Standing d. Supine Answer: D Rationale: To examine an infant's thyroid gland, the nurse should hyperextend the infant's neck slightly while the child is held supine on the caregiver's lap. Neck hyperextension promotes thyroid palpation by elongating the surface area of the infant's characteristically short neck. A prone position wouldn't allow an adequate area for palpation. A sitting position is appropriate when assessing the thyroid gland of an older child or an adult. An infant can't stand, so option C is inappropriate.
2. The nurse is caring for a newborn boy who has hypospadias. His parents are planning to have the baby circumcised before discharge. When teaching the parents about their child's condition, the nurse should tell them: a. the baby can still be circumcised as planned. b. the foreskin will be needed at the time of surgical correction. c. circumcision is necessary because the foreskin obstructs the urethral meatus. d. circumcision will correct the hypospadias. Answer: B Rationale: Circumcision is the surgical removal of the foreskin of the penis. In hypospadias, the urethral meatus is on the underside of the penis. A newborn with hypospadias shouldn't be circumcised because the surgeon may use the foreskin for surgical repair. The foreskin doesn't block the urethral meatus, which may be located near the glans, along the underside of the penis, or at the base. Circumcision doesn't 1
correct hypospadias because the location of the urethral meatus isn't changed during circumcision.
3. A bottle-fed infant, age 3 months, is brought to the pediatrician's office for a well-child visit. During the previous visit, the nurse taught the mother about infant nutritional needs. Which statement by the mother during the current visit indicates effective teaching? a. "I started the baby on cereals and fruits because he wasn't sleeping through the night." b. "I started putting cereal in the bottle with formula because the baby kept spitting it out." c. "I'm giving the baby iron-fortified formula and a fluoride supplement because our water isn't fluoridated." d. "I'm giving the baby skim milk because he was getting so chubby." Answer: C Rationale: Iron-fortified formula supplies all the nutrients an infant needs during the first 6 months; however, fluoride supplementation is necessary if the local water supply isn't fluoridated. Before age 6 months, solid foods, such as cereals, aren't recommended because the GI tract tolerates them poorly. Also, a strong extrusion reflex causes the infant to push food out of the mouth. Mixing solid foods in a bottle with liquids deprives the infant of experiencing new tastes and textures and may interfere with development of proper chewing. Skim milk doesn't provide sufficient fat for an infant's growth.
4. An infant is hospitalized for treatment of inorganic failure to thrive. Which nursing action is most appropriate for this child? a. Encouraging the infant to hold a bottle b. Keeping the infant on bed rest to conserve energy c. Rotating caregivers to provide more stimulation d. Maintaining a consistent, structured environment 2
Answer: D Rationale: The nurse caring for an infant with inorganic failure to thrive should strive to maintain a consistent, structured environment. Encouraging the infant to hold a bottle would reinforce an uncaring feeding environment. The infant should receive social stimulation rather than be confined to bed rest. The number of caregivers should be minimized to promote consistency of care. 5. Which of the following is an early sign of heart failure in an infant with a congenital heart defect? a. Tachypnea b. Tachycardia c. Poor weight gain d. Pulmonary edema Answer: A Rationale: The earliest sign of heart failure in infants is tachycardia (sleeping heart rate greater than 160 beats/minute) as a direct result of sympathetic stimulation. Tachypnea (respiratory rate greater than 60 breaths/minute in infants) occurs in response to decreased lung compliance. Poor weight gain is a result of the increased energy demands to the heart and breathing efforts. Pulmonary edema occurs as the left ventricle fails and blood volume and pressure increase in the left atrium, pulmonary veins, and lungs. 6. A mother brings her 8-month-old son to the pediatrician's office. When the nurse approaches to measure the child's vital signs, he clings to his mother tightly and starts to cry. The mother says, "He used to smile at everyone. I don't know why he's acting this way." Which response by the nurse would help the mother understand her child's behavior? a. "Your baby's behavior indicates stranger anxiety, which is common at his age." 3
b. "Children who behave that way are developing shy personalities." c. "Children at his age begin to fear pain." d. "Your baby's having a temper tantrum, which is common at his age." Answer: A Rationale: Stranger anxiety, common in infants ages 6 to 8 months, may cause the child to cry, cling to the caregiver, and turn away from strangers. Typically, it occurs when the child starts to differentiate familiar and unfamiliar people. The child's behavior doesn't necessarily indicate shyness. According to Piaget, fear of pain characterizes the operational stage of development in school-age children, not infants. Temper tantrums are typical in toddlers who are trying to assert their independence; during a temper tantrum, children may kick, scream, hold their breath, or throw themselves onto the floor. 7. The nurse is assessing an 8-month-old during a wellness checkup. Which of the following is a normal developmental task for an infant this age? a. Sitting without support b. Saying two words c. Feeding himself with a spoon d. Playing patty-cake Answer: A Rationale: According to the Denver Developmental Screening Test, most infants should be able to sit unsupported by age 7 months. A 15month-old child should be able to say two words. By 17 months, the toddler should be able to feed himself with a spoon. A 10-month-old should be able to play patty-cake.
8. Twenty-four hours after birth, a neonate hasn't passed meconium. The nurse suspects which condition?
a. Hirschsprung's disease b. Celiac disease c. Intussusception d. Abdominal wall defect Answer: A Rationale: Failure to pass meconium is an important diagnostic indicator for Hirschsprung's disease. The other options aren't associated with failure to pass meconium.
9. The mother of a hospitalized infant appears anxious and displays anger with the staff. Which response is most appropriate? a. "Some of the staff members don't want to talk to you because you might yell at them." b. "Why do you seem so angry today? It makes it hard for us to help you." c. "Is this your normal behavior or are you acting out because your child is hospitalized?" d. "You seem upset. Having your child hospitalized must be difficult." Answer: D Rationale: Acknowledging the mother's feelings and recognizing that it's difficult to cope with a hospitalized child allows the mother to express her feelings. Telling the mother that other staff members don't want to talk to her isn't therapeutic. Asking her to explain her behavior places the mother on the defensive and isn't therapeutic. 10. An infant, age 10 months, is brought to the well-baby clinic for a follow-up visit. The mother tells the nurse that she has been having trouble feeding her infant solid foods. To help correct this problem, the nurse should: a. point out that tongue thrusting is the infant's way of rejecting food. 5
b. instruct the mother to place the food at the back and toward the side of the infant's mouth. c. advise the mother to puree foods if the child resists them in solid form. d. suggest that the mother force-feed the child if necessary. Answer: B Rationale: Placing the food at the back and toward the side of the infant's mouth encourages swallowing. Tongue thrusting is a physiologic response to food placed incorrectly in the mouth. Offering pureed foods wouldn't encourage swallowing, which is a learned behavior. Forcefeeding may be frustrating for both the mother and child and may cause the child to gag and choke when attempting to reject the undesired food; also, it may lead to a higher-than-normal caloric intake, resulting in obesity.
11. When performing a physical examination on an infant, the nurse notes abnormally low-set ears. This finding is associated with: a. otogenous tetanus. b. tracheoesophageal fistula. c. congenital heart defects. d. renal anomalies. Answer: D Rationale: Normally, the top of the ear aligns with an imaginary line drawn across the inner and outer canthus of the eye. Ears set below this line are associated with renal anomalies or mental retardation. Low-set ears don't accompany otogenous tetanus, tracheoesophageal fistula, or congenital heart defects. 12. A mother is concerned that she might be spoiling her 2-month-old daughter by picking her up each time she cries. Which suggestion should the nurse offer?
a. "If the baby's diaper is dry when she's crying, leave her alone and she'll fall asleep." b. "Continue to pick her up when she cries because young infants need cuddling and holding to meet their needs." c. "Leave your baby alone for 10 minutes. If she hasn't stopped crying by then, pick her up." d. "Crying at this age indicates hunger. Try feeding her when she cries." Answer: B Rationale: The nurse should advise the mother to continue to pick the infant up when she cries because a young infant needs to be cuddled and held when crying. Because the infant's cognitive development isn't advanced enough for her to associate crying with getting attention, it would be difficult to spoil her at this age. Even if her diaper is dry, a gentle touch may be necessary until she falls asleep. Crying for 10 minutes wears an infant out; ignoring crying can make the infant mistrust caregivers and the environment. Infants cry for many reasons, not just when hungry. 13. The nurse is teaching parents about the nutritional needs of their full-term infant, age 2 months, who's breast-feeding. Which response shows that the parents understand their infant's dietary needs? a. "We won't start any new foods now." b. "We'll start the baby on skim milk." c. "We'll introduce cereal into the diet now." d. "We should add new fruits to the diet one at a time." Answer: A Rationale: Because breast milk provides all the nutrients a full-term infant needs for the first 6 months, the parents shouldn't introduce new foods into the infant's diet at this point. They shouldn't provide skim milk because it doesn't have sufficient fat for infant growth. The parents also shouldn't provide solid foods, such as cereal and fruit, before age 6 months because an infant's GI tract doesn't tolerate them well. 7
14. During a well-baby visit, a 2-month-old infant receives diphtheria pertussis tetanus (DPT) vaccine, trivalent oral poliovirus vaccine, and Haemophilus influenzae b (Hib) vaccine. The parents state that the child's older brother has never received the Hib vaccine and ask why the baby must have it. How should the nurse respond? a. "This vaccine prevents infection by various strains of the influenza virus." b. "This vaccine protects against bacterial infections, such as meningitis and bacterial pneumonia." c. "This vaccine prevents infection by the hepatitis B virus." d. "This vaccine prevents chickenpox." Answer: B Rationale: The Hib vaccine provides protection against serious
childhood infections caused by H. influenzae type B virus, such as meningitis and bacterial pneumonia. The influenza virus vaccine provides immunity to various strains of the influenza virus. The Heptavax available. vaccine prevents infection by the hepatitis B virus. Chickenpox is caused by the varicella virus; a chickenpox vaccine is now
15. The nurse is developing a plan to teach a mother how to reduce her baby's risk of developing otitis media. Which of the following directions should the nurse include in the teaching plan? a. Administer antibiotics whenever the baby has a cold. b. Place the baby in an upright position when giving a bottle. c. Avoid getting the ears wet while bathing or swimming. d. Clean the external ear canal daily. Answer: B Rationale: Feeding a baby in an upright position reduces the pooling of formula in the nasopharynx. Formula provides a good medium for the 8
growth of bacteria, which can travel easily through the short, horizontal eustachian tubes. The other interventions don't reduce the risk of a baby developing otitis media.
16. After gathering all necessary equipment and setting up the supplies, which of the following would be the first step in performing endotracheal (ET) or tracheal suctioning in an infant? a. Provide extra oxygen by using a ventilator or through manual bagging. b. Insert a suction catheter to the appropriate measured length. c. Insert a few drops of sterile saline solution. d. Put on clean gloves. Answer: A Rationale: Providing extra oxygen prior to suctioning helps prevent hypoxemia. Insertion of a suction catheter is performed after preoxygenation. Instilling a few drops of sterile saline solution is no longer part of routine suctioning. ET and tracheal suctioning require sterile technique and sterile gloves, not just clean gloves.
17. After the birth of her first neonate, a mother asks the nurse about the reddened areas ("stork bites") at the nape of the neonate's neck. How should the nurse respond? a. "They're normal and will disappear as the baby's skin thickens." b. "They're a common congenital abnormality." c. "They commonly result from a traumatic delivery." d. "They're caused by a blockage in the apocrine glands." Answer: A Rationale: Capillary hemangioma ("stork bites") may appear on the neonate's upper eyelids, the bridge of the nose, or the nape of the neck. They result from vascular congestion and disappear as the skin thickens. 9
They aren't associated with congenital abnormalities, traumatic delivery, or blocked apocrine glands.
18.
For
an
8-month-old
infant,
which
toy
promotes
cognitive
development? a. Finger paint b. Jack-in-the-box c. A small rubber ball d. A play gym strung across the crib Answer: B Rationale: According to Piaget's theory of cognitive development, an 8month-old child will look for an object once it disappears from sight to develop the cognitive skill of object permanence. Finger paint and small balls are potentially dangerous because infants frequently put their fingers or objects in their mouths. Anything strung across a crib, such as a play gym, is a safety hazard especially to a child who may use it to pull up to a standing position. 19. After an infant undergoes surgical repair of a cleft lip, the physician orders elbow restraints. For this infant, the postoperative plan of care should include which nursing action? a. Removing the restraints every 2 hours b. Removing the restraints while the infant is asleep c. Keeping the restraints on both arms only while the child is awake d. Using the restraints until the infant recovers fully from anesthesia Answer: A Rationale: The nurse should remove one elbow restraint at a time every 2 hours for about 5 minutes, to allow exercise of the arms and to inspect for skin irritation. To prevent the infant from touching and disrupting the suture line, the nurse should use the restraints when the infant is asleep
10
and awake. The nurse should maintain the elbow restraints from the time the infant recovers from anesthesia until the suture line is healed.
20. An infant undergoes surgery to remove a myelomeningocele. To detect increased intracranial pressure (ICP) as early as possible, the nurse should stay alert for which postoperative finding? a. Decreased urine output b. Increased heart rate c. Bulging fontanels d. Sunken eyeballs Answer: C Rationale: Because an infant's fontanels remain open, the skull may expand in response to increased ICP. Therefore, bulging fontanels are a cardinal sign of increased ICP in an infant. Decreased urine output and sunken eyeballs indicate dehydration, not increased ICP. With increased ICP, the heart rate decreases. 21. A mother asks the nurse why her 12-month-old baby gets otitis media more frequently than her 10-year-old son. What should the nurse tell her? a. The baby's eustachian tubes are shorter and lie more horizontally. b. The baby is too young to blow his nose when he has a cold. c. The baby spends more time lying down than his older brother; therefore, more dirt gets in the baby's ear. d. The baby puts dirty toys in his mouth. Answer: A Rationale: Infants and young children are more prone to otitis media because their eustachian tubes are shorter and lie more horizontally. Pathogens from the nasopharynx can more readily enter the eustachian tube of the middle ear. The inability to clear nasal passages by blowing the nose, lying down on the floor, and putting dirty toys in the mouth don't increase the tendency toward otitis media. 11
22. Before a routine checkup in the pediatrician's office, an 8-month-old infant sits contentedly on the mother's lap, chewing on a toy. When preparing to examine this infant, what should the nurse plan to do first? a. Measure the head circumference. b. Auscultate the heart and lungs. c. Elicit the pupillary reaction. d. Weigh the child. Answer: B Rationale: Heart and lung auscultation rarely distresses an infant, so it should be done early in the assessment. Placing a tape measure on the infant's head, shining a light in the eyes, or undressing the infant before weighing may cause distress, making the rest of the examination more difficult. 23. At a previous visit, the parents of an infant with cystic fibrosis received instruction in the administration of pancrelipase (Pancrease). At a follow-up visit, which finding in the infant suggests that the parents are not administering the pancreatic enzymes as instructed? a. Fatty stools b. Bloody urine c. Bloody stools d. Glucose in urine Answer: A Rationale: Pancreatic enzymes normally aid in food digestion in the intestine. In a child with cystic fibrosis, however, these natural enzymes cannot reach the intestine because mucus blocks the pancreatic duct. Without these enzymes, undigested fats and proteins produce fatty stools. Treatment with pancreatic enzymes should result in stools of normal consistency; noncompliance with the treatment produces fatty stools. Noncompliance doesn't cause bloody urine, bloody stools, or glucose in urine. 12
24. The nurse is caring for an infant with congenital clubfoot. After the final cast has been removed, which member of the health care team will most likely help the infant with leg and ankle exercises and provide his parents with a home exercise regimen? a. Occupational therapist b. Physical therapist c. Recreational therapist d. Speech therapist Answer: B Rationale: After the final cast has been removed, foot and ankle exercises may be necessary to improve range of motion. A physical therapist should work with the child. A physical therapist is trained to help clients restore function and mobility, which will prevent further disability. An occupational therapist, who helps the chronically ill or disabled to perform activities of daily living and adapt to limitations, isn't necessary at this time. A recreational therapist, who uses games and group activities to redirect maladaptive energy into appropriate behavior, also isn't required. A speech therapist isn't necessary; clubfoot isn't accompanied by speech problems.
25. A 2-month-old is brought to the clinic by his mother. His abdomen is distended, and he has been vomiting forcefully and with increasing frequency over the past 2 weeks. On examination, the nurse notes signs of dehydration and a palpable mass to the right of the umbilicus. Peristaltic waves are visible, moving from left to right. The nurse should suspect which of the following conditions? a. Colic b. Failure to thrive c. Intussusception d. Pyloric stenosis Answer: D 13
Rationale: These are classic symptoms of pyloric stenosis caused by hypertrophy of the circular pylorus muscle. Surgery is the standard treatment for this disorder. Abdominal masses and abnormal peristalsis aren't necessarily related to colic or failure to thrive. Intussusception is usually characterized by acute onset and severe abdominal pain.
26. A 3-month-old infant just had a cleft lip and palette repair. To prevent trauma to the operative site, the nurse should do which of the following? a. Give the baby a pacifier to help soothe him. b. Lie the baby in the prone position. c. Place the infant's arms in soft elbow restraints. d. Avoid touching the suture line, even to clean. Answer: C Rationale: Soft restraints from the upper arm to the wrist prevent the infant from touching his lip but allow him to hold a favorite item such as a blanket. Because they could damage the operative site, such objects as pacifiers, suction catheters, and small spoons shouldn't be placed in a baby's mouth after cleft palette repair. A baby in a prone position may rub his face on the sheets and traumatize the operative site. The suture line should be cleaned gently to prevent infection, which could interfere with healing and damage the cosmetic appearance of the repair. Dried blood collecting on the suture line can widen the scar.
27. A mother, who is visibly upset, carries her 2-month-old infant into the crowded emergency department. The child appears limp and lifeless. The mother screams to the nurse for help. The nurse should: a. take the infant from the mother and offer to help. b. take the infant and mother back to a treatment room. c. call the resuscitation team and the supervisor. d. call security and the hospital administration. 14
Answer: B Rationale: Taking the infant and mother into a treatment room for assessment provides privacy and a controlled environment. The mother should be allowed to remain with her child if she wishes. If she doesn't want to be present, the nurse should find a private area for her. The nurse must assess the child before calling the resuscitation team. Security isn't warranted in this situation.
28. A 10-month-old child with phenylketonuria (PKU) is being weaned from breast-feeding. When teaching the parents about the proper diet for their child, the nurse should stress the importance of restricting: a. vegetables. b. meats. c. grains. d. sugar. Answer: B Rationale: PKU is an inherited disorder characterized by the inability to metabolize phenylalanine, an essential amino acid. Phenylalanine accumulation in the blood results in central nervous system damage and progressive mental retardation. However, early detection of PKU and dietary restriction of phenylalanine can prevent disease progression. Intake of high-protein foods, such as meats and dairy products, must be restricted because they contain large amounts of phenylalanine. The child may consume measured amounts of vegetables, grains, and sugar, which are low in phenylalanine.
29. A baby boy has just had surgery to repair his cleft lip. Which nursing intervention is the most important during the immediate postoperative period?
15
a. Clean the suture line carefully with a sterile solution after every feeding. b. Lay the infant on his abdomen to help drain fluids from his mouth. c. Allow the infant to cry to promote lung reexpansion. d. Give the baby a pacifier to suck for comfort. Answer: A Rationale: To avoid an infection that could adversely affect the cosmetic outcome of the repair, the suture line must be cleaned very gently with a sterile solution after each feeding. Laying an infant on his abdomen after a cleft lip repair will put pressure on the suture line, causing damage. The infant can be positioned on his side to drain saliva without affecting the suture line. Crying puts tension on the suture line and should be avoided by anticipating the baby's needs, such as holding and cuddling him. Hard objects, such as pacifiers, should be kept away from the suture line because they can cause damage.
30. While preparing to discharge a 9-month-old infant who's recovering from gastroenteritis and dehydration, the nurse teaches the parents about their infant's dietary and fluid requirements. The nurse should include which other topic in the teaching session? a. Nursery schools b. Toilet training c. Safety guidelines d. Preparation for surgery Answer: C Rationale: The nurse always should reinforce safety guidelines when teaching parents how to care for their child. By giving anticipatory guidance, the nurse can help prevent many accidental injuries. For parents of a 9-month-old infant, it's too early to discuss nursery schools or toilet training. Because surgery isn't used to treat gastroenteritis, this topic is inappropriate.
16
31. When discharging a 5-month-old infant from the hospital, the nurse checks to see whether the parent's car restraint system for the infant is appropriate. Which of the following restraint systems would be safest? a. A front-facing convertible car seat in the middle of the backseat b. A rear-facing infant safety seat in the front passenger seat c. A rear-facing infant safety seat in the middle of the backseat d. A front-facing convertible car seat in the backseat next to the window Answer: C Rationale: Infants from birth to 20 lb (9.1 kg) and under age 1 must be in a rear-facing infant or convertible seat in the backseat, preferably in the middle. Infants and small children should never be placed in the front seat because of the risk of injuries from a breaking front windshield and an expanding airbag. The position next to the window isn't preferred.
32. A mother and grandmother bring a 3-month-old infant to the wellbaby clinic for a routine checkup. As the nurse weighs the infant, the grandmother asks, "Shouldn't the baby start eating solid food? My kids started on cereal when they were 2 weeks old." Which response by the nurse would be appropriate? a. "The baby is gaining weight and doing well. There is no need for solid food yet." b. "Things have changed a lot since your children were born." c. "We've found that babies can't digest solid food properly until they're 3 or 4 months old." d. "We've learned that introducing solid food early leads to eating disorders later in life." Answer: C
17
Rationale: Infants younger than 3 or 4 months lack the enzymes needed to digest complex carbohydrates. Option A doesn't address the grandmother's question directly. Option B is a clich that may block further communication with the grandmother. Option D is incorrect because no evidence suggests that introducing solid food early causes eating disorders. 33. A mother calls the clinic to report that her 9-month-old infant has diarrhea. Upon further questioning, the nurse determines that the child has mild diarrhea and no signs of dehydration. Which advice is most appropriate to give this mother? a. Call back if your baby has 10 stools in 1 day. b. Feed your baby clear liquids only. c. Continue your baby's normal feedings. d. Notify your baby's day care of his illness. Answer: C Rationale: If an infant has mild diarrhea, his mother should be advised to continue his normal diet and to call back if the diarrhea doesn't stop or if he shows signs of dehydration. Notifying the day care about the infant's illness is important but doesn't take priority.
34. While assessing a 2-month-old infant's airway, the nurse finds that he isn't breathing. After two unsuccessful attempts to establish an airway, the nurse should: a. attempt rescue breaths. b. attempt to reposition the airway a third time. c. administer five back blows. d. attempt to ventilate with a handheld resuscitation bag. Answer: C Rationale: The infant's airway is blocked despite attempts to establish it. The next step is to clear the airway with back blows and chest thrusts. Breaths can't be administered until the airway is patent. After two 18
attempts to position the airway, the nurse can assume the airway is blocked. The nurse can't ventilate the infant with a handheld resuscitation bag until the airway is patent.
35. An infant, age 8 months, has a tentative diagnosis of congenital heart disease. During physical assessment, the nurse measures a heart rate of 170 beats/minute and a respiratory rate of 70 breaths/minute. How should the nurse position the infant? a. Lying on the back b. Lying on the abdomen c. Sitting in an infant seat d. Sitting in high Fowler's position Answer: C Rationale: Because the infant's assessment findings suggest that respiratory distress is developing, the nurse should position the infant with the head elevated at a 45-degree angle to promote maximum chest expansion; an infant seat maintains this position. Placing an infant flat on the back or abdomen or in high Fowler's position could increase respiratory distress by preventing maximal chest expansion. 36. For the last 6 days, a 7-month-old infant has been receiving amoxicillin trihydrate (Amoxil) to treat an ear infection. Now the parents report redness in the diaper area and small, red patches on the infant's inner thighs and buttocks. After diagnosing Candida albicans, the physician prescribes topical nystatin (Mycostatin) to be applied to the perineum four times daily. Medication teaching should include which instruction? a. "Discontinue amoxicillin until the diaper area is no longer red." b. "Avoid using superabsorbent disposable diapers." c. "Inspect your infant's mouth for white patches." d. "Switch your infant to a soy-based formula." Answer: C 19
Rationale: The nurse should instruct the parents to inspect the infant's mouth for white patches. Signs of thrush, these patches are common in children with C. albicans infections and should be reported to the physician. The parents shouldn't discontinue amoxicillin; to treat an ear infection effectively, this drug must be administered for at least 10 days. The parents should use, not avoid, superabsorbent diapers because they help keep the diaper area dry especially if this area is red and irritated. Changing the infant's formula isn't necessary because the diaper irritation probably results from amoxicillin therapy. 37. When developing a postoperative plan of care for an infant scheduled for cleft lip repair, the nurse should assign highest priority to which intervention? a. Comforting the child as quickly as possible b. Maintaining the child in a prone position c. Restraining the child's arms at all times, using elbow restraints d. Avoiding disturbing any crusts that form on the suture line Answer: A Rationale: After surgery to repair a cleft lip, the primary goal of nursing care is to maintain integrity of the operative site. Crying causes tension on the suture line, so comforting the child as quickly as possible is the highest nursing priority. Parents may help by cuddling and comforting the child. The prone position is contraindicated after surgery because rubbing on the sheet may disturb the suture line. Elbow restraints may cause agitation; if used to prevent the child from disturbing the suture line, they must be removed, one at a time, every 2 to 4 hours so that the child can exercise and the nurse can assess for skin irritation. Crusts forming on the suture line contribute to scarring and must be cleaned carefully. 38. During a visit to the well-baby clinic, a mother who's breast-feeding her 2-month-old infant expresses concern over the infant's bowel movements. Which statement by the mother would lead the nurse to believe that the infant's bowel movements are normal?
20
a. "The baby's stools are yellow and semiformed." b. "The baby's stools are dark green and sticky." c. "The baby's stools are green and watery." d. "The baby's stools are bright yellow and soft." Answer: D Rationale: Breast-feeding infants typically have soft, bright yellow or light green stools with no offensive odor. Formula-fed infants typically have pale yellow, semiformed stools with a strong odor. A neonate's first stools typically are dark green to black, sticky, and odorless (representing meconium, usually present for the first 3 days). By the 4th day, yellowish green transitional stools appear. Green, watery stools indicate diarrhea.
39. A 4-month-old infant is taken to the pediatrician by his parents because they're concerned about his frequent respiratory infections, poor feeding habits, frequent vomiting, and colic. The physician notes that the baby has failed to gain expected weight and recommends that the baby have a sweat test performed to detect possible cystic fibrosis. To prepare the parents for the test, the nurse should explain that: a. the baby will need to fast before the test. b. a sample of blood will be necessary. c. a low-sodium diet is necessary for 24 hours before the test. d. a low-intensity, painless electrical current is applied to the skin. Answer: D Rationale: Because cystic fibrosis clients have elevated levels of sodium and chloride in their sweat, a sweat test is performed to confirm this disorder. After pilocarpine (a cholinergic medication that induces sweating) is applied to a gauze pad and placed on the arm, a lowintensity, painless electrical current is applied for several minutes. The arm is then washed off, and a filter paper is placed over the site with forceps to collect the sweat. Elevated levels of sodium and chloride are diagnostic of cystic fibrosis. No fasting is necessary before this test and 21
no blood sample is required. A low-sodium diet isn't required before the test. 40. A 10-month-old child with recurrent otitis media (middle ear inflammation) is brought to the clinic for evaluation. To help determine the cause of the child's condition, the nurse should ask the parents: a. "Does water ever get into the baby's ears during shampooing?" b. "Do you give the baby a bottle to take to bed?" c. "Have you noticed a lot of wax in the baby's ears?" d. "Can the baby combine two words when speaking?" Answer: B Rationale: In a young child, the eustachian tube is relatively short, wide, and horizontal, promoting drainage of secretions from the nasopharynx into the middle ear. If the child takes a bottle to bed and drinks while lying down, fluids may pool in the pharyngeal cavity, increasing the risk of otitis media. Cerumen in the external ear canal doesn't promote the development of otitis media. However, during shampooing, water may become trapped in the external ear canal by large amounts of cerumen, possibly causing otitis externa (external ear inflammation). Persistent fluid in the middle ear may impair language development and hearing; however, a 10-month-old child isn't expected to combine two words when speaking.
41. A client who has tested positive for the human immunodeficiency virus (HIV) delivers a girl. When she asks whether her baby has acquired immunodeficiency syndrome (AIDS), how should the nurse respond? a. "Don't worry. It's too soon to tell." b. "Chances are she'll be okay because you don't have AIDS yet." c. "She may have acquired HIV in utero, but we won't know for sure until she's older." d. "All babies born to HIV-positive women are infected with HIV, but your baby won't have symptoms for years."
22
Answer: C Rationale: Diagnosing AIDS in neonates is difficult because all neonates of women with HIV receive maternal antibodies and therefore initially test positive for HIV antibodies. However, not all such neonates actually are infected. The newborn of an HIV-positive mother has a 25% to 30% chance of developing HIV. 42. The mother of a 12-month-old child expresses concern about the effects of her child's frequent thumb-sucking. After the nurse provides instruction on this topic, which response by the mother indicates that teaching has been effective? a. "Thumb-sucking should be discouraged at age 12 months." b. "I'll give my baby a pacifier instead." c. "Sucking is important to the baby." d. "I'll wrap the baby's thumb in a bandage." Answer: C Rationale: Sucking is the infant's chief pleasure. However, thumbsucking may cause malocclusion if it persists after age 4. Many fetuses begin sucking on their fingers in utero and, as infants, refuse a pacifier as a substitute. A young child is likely to chew on a bandage, possibly leading to airway obstruction.
43. An infant goes into cardiac arrest. When delivering chest compressions as part of cardiopulmonary resuscitation (CPR), where should the rescuer place the fingers? a. One fingerbreadth below the nipple line, directly over the sternum b. Directly over the xiphoid process c. Over the lower third of the sternum d. Directly over the left nipple Answer: A
23
Rationale: When delivering chest compressions to an infant, the rescuer should place the fingers one fingerbreadth below the nipple line, directly over the sternum. Compared to the heart of an older child or adult, the infant's heart is higher and more horizontal relative to anatomical landmarks. Placing the fingers over the xiphoid process could cause injury; placing them over the lower third of the sternum or directly over the nipple could make chest compressions ineffective.
44. The nurse is approached by the mother of a child with hypospadias. She says to the nurse, "Why did this have to happen to my baby? Why couldn't he be perfect? How could this have happened?" What should the nurse say in response? a. "This is only a minor problem. Many other babies are born with worse defects." b. "Don't worry. After surgical repair you'll hardly remember there was anything wrong with your baby." c. "I'll ask the physician to explain to you how this defect occurs." d. "You seem upset. Tell me about it." Answer: D Rationale: By verbalizing observations of the client's behavior, the nurse acknowledges the client's feelings. By listening, the nurse can help the client understand her feelings and begin to deal with them. Telling the client that there are babies with worse defects doesn't acknowledge and may even belittle her feelings. Providing a stock answer, such as "Don't worry," shows a lack of interest in the client's feelings. Offering to ask the physician also doesn't address the client's feelings.
45. A 10-month-old infant with tetralogy of Fallot (TOF) experiences a cyanotic episode, or "blue spell." To improve oxygenation during such an episode, the nurse should place the infant in which position? a. Knee-to-chest 24
b. Fowler's c. Trendelenburg's d. Prone Answer: A Rationale: TOF ventricular involves four defects: pulmonary defect stenosis, (VSD), right and
hypertrophy,
ventricular-septal
dextroposition of the aorta with overriding of the VSD. Pulmonary stenosis decreases pulmonary blood flow and right-to-left shunting via the VSD, causing desaturated blood to circulate. The knee-to-chest position reduces venous return from the legs and increases systemic vascular resistance, maximizing pulmonary blood flow and improving oxygenation status. During a cyanotic episode, the child with TOF typically assumes this position instinctively. Fowler's, Trendelenburg's, and the prone positions don't improve oxygenation.
46.
An
infant
arrives arrest.
at
the
emergency at
department fail,
in
full he's
cardiopulmonary
Efforts
resuscitation
and
pronounced dead. The cause of death is sudden infant death syndrome (SIDS). Which of the following is true regarding the etiology of SIDS? a. It occurs in suspected child abuse cases. b. It occurs primarily in infants with congenital lung problems. c. It occurs primarily in black infants. d. It occurs more commonly in infants who sleep in the prone position. Answer: D Rationale: SIDS occurs in seemingly healthy infants. However, more infants who sleep in the prone position are affected. Because of the pooling of blood that occurs in the child with SIDS, child abuse is sometimes suspected. No correlation to race or lung disease exists.
25
47. Parents bring their infant to the clinic, seeking treatment for vomiting and diarrhea that has lasted for 2 days. On assessment, the nurse detects dry mucous membranes and lethargy. What other finding suggests a fluid volume deficit? a. A sunken fontanel b. Decreased pulse rate c. Increased blood pressure d. Low urine specific gravity Answer: A Rationale: In an infant, signs of fluid volume deficit (dehydration) include sunken fontanels, increased pulse rate, and decreased blood pressure. They occur when the body can no longer maintain sufficient intravascular fluid volume. When this happens, the kidneys conserve water to minimize fluid loss, which results in concentrated urine with a high specific gravity.
48. A baby undergoes surgery to correct an esophageal atresia and tracheoesophageal fistula. Which nursing diagnosis has the highest priority during the first 24 hours postoperatively? a. Ineffective airway clearance b. Imbalanced nutrition: Less than body requirements c. Interrupted breast-feeding d. Hypothermia Answer: A Rationale: Ineffective airway clearance is the priority nursing diagnosis in the immediate postoperative period. The infant's airway must be carefully assessed and frequent suctioning may be necessary to remove mucus while taking care not to pass the catheter as far as the suture line. Assess breath sounds, respiratory rate, skin color, and ease of breathing. Because of the risk of edema and airway obstruction, keep a laryngoscope and endotracheal intubation equipment readily available. 26
Imbalanced nutrition, Interrupted breast-feeding, and Hypothermia are also important during the postoperative period but only after a patent airway is ensured.
49. A neonate born 18 hours ago with myelomeningocele over the lumbosacral region is scheduled for corrective surgery. Preoperatively, what is the most important nursing goal? Preventing infection Ensuring adequate hydration Providing adequate nutrition Preventing contracture deformity Answer: A Rationale: Preventing infection is the nurse's primary preoperative goal for a neonate with myelomeningocele. Although the other options are relevant for this neonate, they're secondary to preventing infection. 50. A hospitalized infant, age 10 months, begins to choke while eating and quickly becomes unconscious. A foreign object isn't visible in the infant's airway, but respirations are absent and the pulse is 50 beats/minute and thready. The nurse attempts rescue breathing, but the ventilations are unsuccessful. What should the nurse do next? Deliver four back blows. Deliver four chest thrusts. Perform chest compressions. Deliver four abdominal thrusts. Answer: A Rationale: If rescue breathing is unsuccessful in a child under age 1, the nurse should deliver four back blows, followed by four chest thrusts, to try to expel the object from the obstructed airway. The nurse shouldn't perform chest compressions because the infant has a pulse and because chest compressions are ineffective without a patent airway for
27
ventilation. The nurse shouldn't use abdominal thrusts for a child under age 1 because they can injure the abdominal organs.
51. The nurse observes a 2-year-old child playing with another child of the same age in the playroom on the pediatric unit. What type of play should the nurse expect the children to engage in? Associative play Parallel play Cooperative play Therapeutic play Answer: B Rationale: Two-year-olds engage in parallel play, in which they play side by side but rarely interact. Associative play is characteristic of preschoolers, in which they are all engaged in a similar activity but there is little organization. School-age children engage in cooperative play, which is organized and goal-directed. Therapeutic play is a technique that can be used to help understand a child's feelings; it consists of energy release, dramatic play, and creative play.
52. A parent calls the pediatric clinic to express concern over her child's eating habits. She says the child eats very little and consumes only a single type of food for weeks on end. The nurse knows that this behavior is characteristic of: toddlers. preschool-age children. school-age children adolescents. Answer: A Rationale: Erratic eating is typical of toddlers. The physiologic need for food decreases at about age 18 months as growth declines from the 28
rapid rate of infancy. The toddler also develops strong food and taste preferences, sometimes eating just one type of food for days or weeks and then switching to another. The child shouldn't be forced to eat. Typically, the child switches to another food spontaneously after a while, correcting any nutritional imbalances. Parents may encourage the child to eat other foods by offering items from the various food groups at each meal.
53. A mother tells the nurse that she wants to begin toilet training her 22-month-old child. The most important factor regarding toilet-training that the nurse should stress to her is: developmental readiness of the child. consistency in approach. the mother's positive attitude. developmental level of the child's peers. Answer: B Rationale: If the child isn't developmentally ready, both child and parent will become frustrated. Consistency is important when toilet training is started. The mother's positive attitude is important when the child is determined to be ready. Developmental levels of children are individualized and comparison to peers isn't useful.
54. The nurse should expect a 3-year-old child to be able to perform which action? Ride a tricycle Tie the shoelaces Roller-skate Jump rope Answer: A
29
Rationale: At age 3, gross motor development and refinement in eyehand coordination enable a child to ride a tricycle. The fine motor skills required to tie shoelaces and the gross motor skills required for rollerskating and jumping rope develop around age 5.
55. A child, age 2, is brought to the emergency department after ingesting an unknown number of aspirin tablets about 30 minutes earlier. On entering the examination room, the child is crying and clinging to the mother. Which data should the nurse obtain first? Heart rate, respiratory rate, and blood pressure Recent exposure to communicable diseases Number of immunizations received Height and weight Answer: A Rationale: The most important data to obtain on a child's arrival in the emergency department are vital sign measurements. The nurse should gather the other data later.
56. The nurse is teaching a parent how to administer antibiotics at home to a toddler with acute otitis media. Which statement by the parent indicates that teaching has been successful? "I'll give the antibiotics for the full 10-day course of treatment." "I'll give the antibiotics until my child's ear pain is gone." "Whenever my child is cranky or pulls on an ear, I'll give a dose of antibiotics." "If the ear pain is gone, there's no need to see the physician for another examination of the ears." Answer: A Rationale: Antibiotics must be given for the full course of therapy, even if the child feels well; otherwise, the infection won't be eradicated. 30
Antibiotics should be taken at prescribed intervals to maintain blood levels and not as needed for pain. A reexamination at the end of the course of antibiotics is necessary to confirm that the infection is resolved.
57. What is the best advice for a nurse to give to the parents of a 2year-old child who frequently throws temper tantrums? a. Move the toddler to a different setting. b. Allow the toddler more choices. c. Ignore the behavior when it happens d. Give into the toddler's demands. Answer: C Rationale: Ignore tantrum behavior because attention to the behavior can reinforce the undesirable behavior. Changing settings can increase the tantrum behavior. Allowing the toddler more choices may increase tantrum behavior if the toddler is unable to follow through with choices. The toddler should be offered only allowable and reasonable choices. It's ill-advised to give into the toddler's demands because doing so only promotes tantrum behavior.
58. A toddler with a ventricular septal defect (VSD) is receiving digoxin (Lanoxin) to treat heart failure. The nurse should monitor the child for early signs of digoxin toxicity, which include: a. bradycardia. b. tachycardia. c. hypertension. d. hyperactivity. Answer: A Rationale: Digoxin enhances cardiac efficiency by increasing the force of contraction and decreasing the heart rate. An early sign of digoxin 31
toxicity is bradycardia (an abnormally slow heart rate). To help detect digoxin toxicity, the nurse always should measure the apical heart rate before administering each digoxin dose. Other signs and symptoms of digoxin toxicity include arrhythmias, vomiting, hypotension, fatigue, drowsiness, and visual halos around objects. The other options aren't associated with digoxin toxicity.
59. The nurse is planning a health teaching session for a group of parents with toddlers. When describing a toddler's typical eating pattern, the nurse should mention that many children of this age exhibit: a. consistent table manners. b. an increased appetite. c. strong food preferences. d. a preference for eating alone. Answer: C Rationale: A toddler typically exhibits strong food preferences, eating one type of food for several days and excluding others. A toddler can't be expected to use consistent table manners. Generally, the appetite decreases during the toddler stage because of a slowed growth rate. A toddler typically enjoys socializing during meals and often imitates others.
60. A toddler is diagnosed with iron deficiency anemia. When teaching the parents about using supplemental iron elixir, the nurse should provide which instruction? a. "Give the iron preparation with milk." b. "Give the elixir with water or juice." c. "Monitor the child for episodes of diarrhea." d. "Give the iron preparation before meals." Answer: B
32
Rationale: Because iron preparations may stain the teeth, the nurse should instruct the parents to give the elixir with water or juice. The iron preparation shouldn't be given with milk because milk impedes iron absorption. This preparation may darken the stools and cause constipation; parental instruction regarding increased fluid intake and fiber intake can relieve constipation. To prevent GI upset, the nurse should instruct the parents to mix the iron preparation with water or fruit juice and have the child take it with meals. (Giving it with fruit juice may be preferable because vitamin C enhances iron solubility and absorption.)
61. The nurse is about to give an I.M. injection to a 2-year-old child. Which site should be avoided? a. Vastus lateralis muscle b. Ventrogluteal muscle c. Dorsogluteal muscle d. Deltoid muscle Answer: C Rationale: The dorsogluteal muscle isn't sufficiently developed to be a safe injection site for infants and small children. The vastus lateralis, ventrogluteal, and deltoid muscles are considered safe sites for infants and small children.
62. When developing a plan of care for a toddler with a seizure disorder, which of the following would be inappropriate? a. Padded side rails b. Oxygen mask and bag system at bedside c. Arm restraints while asleep d. Cardiorespiratory monitoring Answer: C
33
Rationale: Restraints should never be used on a child with a seizure disorder because they could harm him if a seizure occurs. Padded side rails will prevent the child from injuring himself during a seizure. The bag and mask system should be present in case the child needs oxygen during a seizure. Cardiopulmonary monitoring should be readily available for checking vital signs during a seizure.
63. When assessing a toddler, age 18 months, the nurse should interpret which of the following as a sign of a neurologic dysfunction? a. Positive gag reflex b. Positive tonic neck reflex c. Positive Babinski's reflex d. Positive corneal reflex Answer: C Rationale: Babinski's reflex should disappear by age 12 months; its presence after this age indicates neurologic dysfunction. The gag reflex, tonic neck reflex, and corneal reflex are normal findings for a toddler.
64. A toddler requires emergency intervention for an obstructed airway. Which nursing intervention is appropriate? a. Hyperextending the child's neck to open the airway and delivering four rescue breaths b. Placing the child on the side and using a blind finger sweep to remove the foreign object c. Delivering four back blows followed by four chest thrusts d. Performing the tongue-jaw lift and removing the foreign object only if it's visible Answer: D Rationale: When checking for a foreign object in the airway of a child under age 8, the rescuer should perform the tongue-jaw lift and remove 34
the object only if it's visible. Neck hyperextension may occlude the airway; the head tilt/chin lift method is the correct way to open the airway. A blind finger sweep is contraindicated in a child under age 8 because it may push the object into the airway. After checking for a foreign object, the rescuer should open the airway and attempt to deliver two rescue breaths. Abdominal thrusts (the Heimlich maneuver) are indicated only for children over age 1. In a child under age 1, such thrusts may injure the abdominal organs; back blows and chest thrusts should be used instead.
65. The parents of a 2-year-old child with chronic otitis media are concerned that the disorder has affected their child's hearing. Which behavior suggests that the child has a hearing impairment? a. Stuttering b. Using gestures to express desires c. Babbling continuously d. Playing alongside rather than interacting with peers Answer: B Rationale: Using gestures instead of verbal communication to express desires especially in a child older than 15 months may indicate a hearing or communication impairment. Stuttering is normal in children ages 2 to 4, especially boys. Continuous babbling is a normal phase of speech development in young children; its absence, not presence, would be cause for concern. Parallel play playing alongside peers without interacting is typical of toddlers. However, in an older child, difficulty interacting with peers or avoiding social situations may indicate a hearing deficit. 66. A boy, age 2, is diagnosed with hemophilia, an X-linked recessive disorder. His parents and newborn sister are healthy. The nurse explains how the gene for hemophilia is transmitted. Which statement by the father indicates an understanding of X-linked recessive disorders? a. "Our newborn daughter may be a carrier of the trait." 35
b. "If we have more sons, all of them will have hemophilia." c. "All of our offspring will carry the trait for hemophilia." d. "Our daughter will develop hemophilia when she gets older." Answer: A Rationale: X-linked recessive genes behave like other recessive genes. A normal dominant gene hides the effects of an abnormal recessive gene. However, the gene is expressed primarily in male offspring because it's located on the X chromosome. Male offspring of a carrier mother and an unaffected father have a 50% chance of expressing the trait. These parents may produce normal offspring who neither express nor carry the trait for hemophilia. Female offspring typically don't express the trait, although they may carry it.
67. The nurse is caring for a toddler in respiratory arrest. The nurse will assist with endotracheal intubation and use an uncuffed tube because the: a. vocal cords provide a natural seal. b. trachea is shorter. c. larynx is anterior and cephalad. d. cricoid cartilage is the narrowest part of the larynx. Answer: D Rationale: The cricoid cartilage in the toddler is the narrowest part of larynx and provides a natural seal. This keeps the endotracheal tube in place without requiring a cuff. The vocal cords are narrower in an adult. The trachea is shorter and the larynx is anterior and cephalad, but these aren't reasons to choose an uncuffed tube.
68. The nurse is teaching a group of parents about otitis media. When discussing why children are predisposed to this disorder, the nurse should mention the significance of which anatomical feature?
36
a. Eustachian tubes b. Nasopharynx c. Tympanic membrane d. External ear canal Answer: A Rationale: In a child, the eustachian tubes are short and lie in a horizontal plane, promoting entry of nasopharyngeal secretions into the tubes and thus setting the stage for otitis media. The nasopharynx, tympanic membrane, and external ear canal have no unusual features that would predispose a child to otitis media.
69. A 2-year-old child with a low blood level of the immunosuppressive drug cyclosporine comes to a liver transplant clinic for her appointment. The mother says the child hasn't been vomiting and hasn't had diarrhea, but she admits that her daughter doesn't like taking the liquid medication. Based on knowledge of the drug, which of the following would the nurse instruct the mother to do? a. Let your daughter take her medication only when she wants it; it's okay for her to miss some doses. b. Offer the medication diluted with regular milk, chocolate milk, or orange juice to make it more palatable. c. Insert a nasogastric (NG) tube and administer the medication using the tube as ordered by the physician. d. Give the ordered dose a little bit at a time over 2 hours to ensure administration of the medication. Answer: B Rationale: Liquid cyclosporine has a very unpleasant taste. Diluting it will lessen the strong taste and help the child take the medication as ordered. It isn't acceptable to miss a dose because the drug's effectiveness is based on therapeutic blood levels, and skipping a dose could lower the level. Cyclosporine shouldn't be given by NG tube because it adheres to the plastic tube and, thus, all of the drug may not 37
be administered. Taking the medication over a period of time could negatively affect the blood level. 70. After administering ipecac syrup to a toddler, the nurse monitors the client for adverse drug reactions. Which adverse drug reaction can occur with high doses of ipecac? a. Orthostatic hypotension b. Cardiac arrhythmias c. Central nervous system (CNS) depression d. Tinnitus Answer: B Rationale: Ipecac contains a specific cardiotoxin that, in high doses, may cause cardiac arrhythmias or fatal myocarditis, especially in elderly clients. Ipecac syrup rarely produces adverse reactions when used in the recommended dosages. Orthostatic hypotension and CNS depression may occur with apomorphine, another emetic agent, rather than with ipecac syrup. Tinnitus doesn't occur with any emetic agent. 71. A toddler is hospitalized for treatment of injuries that the staff believes were caused by child abuse. A staff member states that the parents "shouldn't be allowed to visit because they caused the child's injuries." When responding to this staff member, the nurse should base the comments on which understanding? a. The parents shouldn't be allowed to visit the child. b. The parents shouldn't visit until the child is ready for discharge. c. The parents should visit on a schedule established by the health care team and should be supervised during visits. d. The parents should be encouraged to visit frequently and should be welcomed by the staff. Answer: D Rationale: Abusive parents should be encouraged to visit their child and should be welcomed by the staff. Many abusive parents love their 38
children but lack effective parenting skills. The child's hospitalization offers an opportunity for the staff to demonstrate appropriate parenting behaviors to the parents.
72. An emergency department nurse suspects neglect in a 3-year-old boy admitted for failure to thrive. Signs of neglect in the child would include: a. slapping, kicking, and punching others. b. poor hygiene and weight loss. c. loud crying and screaming. d. pulling hair and hitting. Answer: B Rationale: Neglect can involve failure to provide food, bed, shelter, health care, or hygiene. Slapping, kicking, pulling hair, hitting, and punching are examples of forms of physical abuse. Loud crying and screaming aren't abnormal findings in a 3-year-old boy. 73. Which assessment finding is an early sign of heart failure in a toddler? a. Increased respiratory rate b. Increased urine output c. Decreased weight d. Decreased heart rate Answer: A Rationale: Increased respiratory and heart rates are the earliest signs of heart failure. Decreased urine output and increased weight are later signs.
39
74. When caring for a 2-year-old child, the nurse should offer choices, when appropriate, about some aspects of care. According to Erikson, doing this helps the child achieve : a. trust. b. autonomy. c. industry. d. initiative. Answer: B Rationale: According to Erikson's theory of development, a 2-year-old child is at the stage of autonomy versus shame and doubt. An infant is at the stage of trust versus mistrust; a school-age child, industry versus inferiority; and a preschooler, initiative versus guilt. 75. After the nurse explains dietary restrictions to the parents of a child with celiac disease, which statement by the parents indicates effective teaching? a. "We'll follow these instructions until our child's symptoms disappear." b. "Our child must maintain these dietary restrictions until adulthood." c. "Our child must maintain these dietary restrictions for life." d. "We'll follow these instructions until our child has completely grown and developed." Answer: C Rationale: A client with celiac disease must maintain dietary restrictions for life to avoid recurrence of clinical manifestations of the disease. The other options are incorrect because signs and symptoms will reappear if the client eats prohibited foods.
76. A child's parents state that they childproofed their home for their 2year-old. During a home visit, the nurse discovers some situations that 40
show the parents don't fully understand the developmental abilities of their toddler. Which of the following situations displays misunderstanding by the parent? a. Syrup of ipecac in the upstairs bathroom medicine cabinet b. Toy chest in front of a second-story, locked window c. Pot handles turned toward the back of the stove d. Pot handles turned toward the back of the stove Answer: B Rationale: Toddlers are able to climb on low furniture and open windows that may not always be locked, especially in the summer. In such situations, the child could fall out of the window. Keeping syrup of ipecac in the house, turning pot handles toward the back of the stove, and setting the hot water heater at a nonscalding temperature are all safeguards against toddler injury.
77.
2-year-old child with
a tracheostomy
suddenly
becomes
diaphoretic and has an increased heart rate, an increased work of breath, and a decreased oxygen saturation level. Which of the following should be the nurse's first action? a. Suction the tracheostomy. b. Turn the child to a side-lying position. c. Administer pain medication. d. Perform chest physiotherapy Answer: A Rationale: Diaphoresis, increased heart rate, increased respiratory effort, and decreased oxygen saturation are signs that mucus is partially occluding the airway. The child needs suctioning immediately to prevent full occlusion. Turning the child to a side-lying position won't remove mucus from the airway. The child may require pain medication after his airway has been cleared if his condition warrants it. Chest physiotherapy
41
will help drain excess mucus from the lungs but not from a tracheostomy.
78. The mother of a hospitalized 3-year-old girl expresses concern because her daughter is wetting the bed. What should the nurse tell her? a. "It's common for a child to exhibit regressive behavior when anxious or stressed." b. "Your child is probably angry about being hospitalized. This is her way of acting out." c. "Don't worry. It's common for a 3-year-old child to not be fully toilet-trained." d. "The nurses probably haven't been answering the call button soon enough. They will try to respond more quickly." Answer: A Rationale: Young children commonly demonstrate regressive behavior when anxious, under stress, or in a strange environment. While the child could be deliberately wetting the bed out of anger, her behavior most likely isn't under voluntary control. It's appropriate to expect a 3-yearold child to be toilet-trained, but it isn't appropriate to expect the child to be able to utilize a call button to summon the nurse.
79. A 2-year-old child is brought to the emergency department with suspected croup. The child appears frightened and cries as the nurse approaches him. The nurse needs to assess the child's breath sounds. The best way to approach the 2-year-old child is to: a. expose the child's chest quickly and auscultate breath sounds as quickly and efficiently as possible. b. ask the mother to wait briefly outside until the assessment is over. c. tell the child the nurse is going to listen to his chest with the stethoscope.
42
d. allow the child to handle the stethoscope before listening to his lungs. Answer: D Rationale: Toddlers are naturally curious about their environment and letting them handle minor equipment is distracting and helps them gain trust with the nurse. The nurse should only expose one area at a time during assessment and should approach the child slowly and unhurriedly. The caregiver should be encouraged to hold and console her child. Also comfort the child with objects with which he's familiar. The child should be given limited choices to allow autonomy such as, "Do you want me to listen first to the front of your chest or your back?"
80. A 2-year-old child is brought to the emergency department with suspected croup. Which of the following assessment findings reflects increasing respiratory distress? a. Intercostal retractions b. Bradycardia c. Decreased level of consciousness d. Flushed skin Answer: A Rationale: Clinical and cyanosis. 81. What should the nurse do to ensure a safe hospital environment for a toddler? a. Place the child in a youth bed. b. Move stacking toys out of reach c. Pad the crib rails. d. Move the equipment out of reach. manifestations of respiratory distress include
tachypnea, tachycardia, restlessness, dyspnea, intercostal retractions,
43
Answer: D Rationale: Toddlers are curious and may try to play with items such as equipment that is within their reach. Doing so is dangerous. Toddlers in a strange hospital environment still need the security of a crib. Padded crib rails are necessary if seizure activity is present. Stacking toys are appropriate for this age-group and don't present a safety hazard.
82. The nurse is caring for a toddler with Down syndrome. To help the toddler cope with painful procedures, the nurse can: a. prepare the child by positive self-talk. b. establish a time limit to get ready for the procedure. c. hold and rock him and give him a security object. d. count and sing with the child. Answer: C Rationale: The child with Down syndrome may have difficulty coping with painful procedures and may regress during his illness. Holding, rocking, and giving the child a security object may be comforting to the child. An older child or a child without Down syndrome may benefit from positive self-talk, time limits, and diversionary tactics, such as counting and singing; however, the success of these tactics depends on the child.
83. To treat a child's atopic dermatitis, a physician prescribes a topical application of hydrocortisone cream twice daily. After medication instruction by the nurse, which statement by the parent indicates effective teaching? a. "I will spread a thick coat of hydrocortisone cream on the affected area and will wash this area once a week." b. "I will gently scrape the skin before applying the cream to promote absorption." c. "I will avoid using soap and water on the affected area and will apply an emollient cream on this area frequently." 44
d. "I will apply a moisturizing cream sparingly and will wash the affected area frequently." Answer: C Rationale: The parent should avoid washing the affected area with soap and water because this removes moisture from the horny layer of the skin. Applied in a thin layer, emollient cream holds moisture in the skin, provides a barrier to environmental irritants, and helps prevent infection. Topical steroid creams, such as hydrocortisone, should be applied sparingly as a light film; the affected area should be cleaned gently with water before the cream is applied. Scraping or abrading the skin may increase the risk of infection and alter drug absorption. Excessive application of steroidal creams may result in systemic absorption and Cushing's syndrome. Frequent washing dries the skin, making it more susceptible to cracking and further breakdown. 84. The nurse is assessing a 3-year-old child who has ingested toilet bowl cleaner. What finding should the nurse expect? a. Reddish-colored skin b. Edematous lips c. Hypertension d. Lower abdominal pain Answer: B Rationale: The child who has ingested a caustic poison, such as lye (found in toilet bowl cleaners), may develop edema, ulcers of the lips and mouth, pain in the mouth and throat, excessive salivation, dysphagia, and burns of the mouth, lips, esophagus and stomach. Bleeding from burns in the GI tract can lead to pallor, hypotension, tachypnea, and tachycardia. Reddish-colored skin, hypertension, and lower abdominal pain don't commonly occur in caustic poisoning.
85. A toddler is having a tonic-clonic seizure. What should the nurse do first?
45
a. Restrain the child. b. Place a tongue blade in the child's mouth. c. Remove objects from the child's surroundings d. Check the child's breathing. Answer: C Rationale: During a seizure, the nurse's first priority is to protect the child from injury. To prevent injury caused by uncontrolled movements, the nurse must remove objects from the child's surroundings and pad objects that can't be removed. Restraining the child or placing an object in the child's mouth during a seizure may cause injury. Once the seizure stops, the nurse should check for breathing and, if indicated, initiate rescue breathing. 86. The nurse should begin screening for lead poisoning when a child reaches which age? a. 6 months b. 12 months c. 18 months d. 24 months Answer: C Rationale: The nurse should start screening a child for lead poisoning at age 18 months and perform repeat screenings at ages 24, 30, and 36 months. High-risk infants, such as premature infants and formula-fed infants not receiving iron supplementation, should be screened for iron deficiency anemia at age 6 months. Regular dental visits should begin at age 24 months.
87. A 14-month-old child with acquired immunodeficiency syndrome (AIDS) is admitted to the facility with an infection. When developing a plan of care, the nurse must keep in mind that AIDS in children commonly is associated with: a. Kaposi's sarcoma. 46
b. congenital heart anomalies. c. developmental delays. d. Wiskott-Aldrich syndrome. Answer: C Rationale: Children with AIDS commonly exhibit developmental delays or regression. To plan developmentally appropriate care and establish realistic goals, the nurse must obtain information about the child's developmental status. Unlike adults with AIDS, children with this disease rarely develop Kaposi's sarcoma. AIDS isn't associated with congenital heart anomalies. Clinical manifestations of Wiskott-Aldrich syndrome, an X-linked recessive disorder characterized by immunodeficiency, resemble those of AIDS; however, the two syndromes aren't related.
88. The nurse is caring for a young child with tetralogy of Fallot. The child is upset and crying. The nurse observes that he's dyspneic and cyanotic. Which position would help relieve the child's dyspnea and cyanosis? a. Sitting in bed with the head of the bed at a 45-degree angle b. Squatting position c. Lying flat in bed d. Lying on his right side Answer: B Rationale: Placing the child in a squatting position sequesters a large amount of blood to the legs, reducing venous return. The other positions don't reduce venous return; therefore, they won't relieve the child's dyspnea and cyanosis. A child with tetralogy of Fallot may also assume a knee-chest position to reduce venous return to the heart.
89. The nurse teaches a mother how to provide adequate nutrition for her toddler, who has cerebral palsy. Which of the following observations indicates that teaching has been effective?
47
a. The nurse teaches a mother how to provide adequate nutrition for her toddler, who has cerebral palsy. Which of the following observations indicates that teaching has been effective? b. The toddler finishes the meal within a specified period of time. c. The child lies down to rest after eating. d. The child eats finger foods by himself. Answer: D Rationale: The child with cerebral palsy should be encouraged to be as independent as possible. Finger foods allow the toddler to feed himself. Because spasticity affects coordinated chewing and swallowing as well as the ability to bring food to the mouth, it's difficult for the child with cerebral palsy to eat neatly. Independence in eating should take precedence over neatness. The child with cerebral palsy may require more time to bring food to the mouth; thus, chewing and swallowing shouldn't be rushed to finish a meal by a specified time. The child with cerebral palsy may vomit after eating due to a hyperactive gag reflex. Therefore, the child should remain in an upright position after eating to prevent aspiration and choking.
90. When a toddler with croup is admitted to the facility, the physician orders treatment with a mist tent. As the parent attempts to put the toddler in the crib, the toddler cries and clings to the parent. What is the nurse's best approach for gaining the child's cooperation with the treatment? a. Turn off the mist so the noise doesn't frighten the toddler. b. Let the toddler sit on the parent's lap next to the mist tent. c. Encourage the parent to stand next to the crib and stay with the child. d. Put the side rail down so the toddler can get into and out of the crib unaided. Answer: C
48
Rationale: By encouraging the parent to stand next to the crib and stay with the child, the nurse promotes compliance with treatment while minimizing the toddler's separation anxiety. Because the mist helps thin secretions and make them easier to clear, turning off the mist or letting the toddler sit next to the mist tent defeats the treatment's purpose. To prevent falls, the nurse should keep the side rails up and shouldn't permit the toddler to climb into and out of the crib.
91. A child, age 3, is brought to the emergency department in respiratory distress caused by acute epiglottitis. Which clinical manifestations should the nurse expect to assess? a. Severe sore throat, drooling, and leaning forward to breathe b. Low-grade fever, stridor, and a barking cough c. Pulmonary congestion, a productive cough, and a fever d. Sore throat, a fever, and general malaise Answer: A Rationale: A child with acute epiglottitis appears acutely ill and clinical manifestations may include drooling (because of difficulty swallowing), severe sore throat, hoarseness, leaning forward with the neck hyperextended, a high fever, and severe inspiratory stridor. A low-grade fever, stridor, and barking cough that worsens at night are suggestive of croup. Pulmonary congestion, productive cough, and fever along with nasal flaring, retractions, chest pain, dyspnea, decreased breath sounds, and crackles are indicative of pneumococcal pneumonia. A sore throat, fever, and general malaise point to viral pharyngitis.
92. A toddler is hospitalized for evaluation and management of congenital heart disease (CHD). During discharge preparation, the nurse should discuss which topic with the parents? a. The need to withhold childhood immunizations b. The importance of restricting the child's fat intake c. How to perform postural drainage 49
d. When to administer prophylactic antibiotics Answer: D Rationale: In CHD, areas of turbulent blood flow provide an optimal environment for bacterial growth. Therefore, a child with CHD is at increased risk for bacterial endocarditis, an infection of the heart valves and lining, and requires prophylactic antibiotics before dental work and invasive procedures. These children should receive all childhood immunizations. They don't require postural drainage or dietary fat restriction.
93. A toddler is in the hospital. Which of the following would be the most appropriate response to the parents, who are concerned about the seriousness of the child's illness? a. "Please try not to worry. Your child will be fine." b. "If you look around, you'll see other children who are much sicker." c. "What seems to concern you about your child being hospitalized?" d. "It must be difficult for you when your child is ill and hospitalized." Answer: D Rationale: Expressing concern about the parents' feelings is the most appropriate response. False reassurance, such as telling parents not to worry, isn't helpful. Encouraging parents to look at how ill other children are also isn't helpful because the focus of the parents is on their own child. Asking what the concern is reinforces the parents' concern without addressing it.
94. The physician prescribes digoxin (Lanoxin) elixir for a toddler with heart failure. Immediately before administering this drug, the nurse must check the toddler's: a. serum sodium level. 50
b. urine output. c. weight. d. apical pulse. Answer: D Rationale: Because digoxin may reduce the heart rate and heart failure may cause a pulse deficit, the nurse should measure the toddler's apical pulse before administering the drug to prevent further slowing of the heart rate. The serum sodium level doesn't affect digoxin's action. For a child with heart failure, the nurse should check urine output and measure weight regularly, but not necessarily just before digoxin administration.
95. Which I.M. injection site might the nurse use for a 2-year-old child? a. Ventrogluteal muscle b. Pectoral muscle c. Femoral muscle d. Deltoid muscle Answer: A Rationale: When administering an I.M. injection to a 2-year-old child, the nurse might select the ventrogluteal muscle if the muscle is well developed. However, the preferred site is the vastus lateralis. The pectoral, femoral, and deltoid muscles aren't appropriate injection sites for a child.
96. The nurse in a clinic walks into a client's room and finds the mother of a 15-month-old in tears. The mother states that her child doesn't love her because the child says "no" to everything. Which of the following would be an appropriate response? a. "Have you punished your child for saying 'no' to you?" b. "This is normal at this age; it's best to ignore the behavior." 51
c. "Explain to your child that saying 'no' all of the time is inappropriate behavior." d. "Saying 'no' is part of toddler development and is normal at this age." Answer: D Rationale: Saying "no" is normal at this age. It doesn't mean that the child doesn't love the mother. The child is attempting to exert independence. Punishing the child isn't appropriate because this is a normal stage of development. Ignoring the behavior is also inappropriate because the child needs to learn about limits. Children at this age may not understand all that they say because they repeat what they hear. Explaining to the child that his behavior is inappropriate isn't an age-appropriate response for this child.
97. When teaching the parents of a toddler with congenital heart disease, the nurse should explain all medical treatments and emphasize which instruction? a. "Reduce your child's caloric intake to decrease cardiac demand." b. "Relax discipline and limit-setting to prevent crying." c. "Make sure your child avoids contact with small children to reduce overstimulation." d. "Try to maintain your child's usual lifestyle to promote normal development." Answer: D Rationale: Parents of a child with a congenital heart defect should treat the child normally and allow self-limited activity. Reducing the child's caloric intake wouldn't necessarily reduce cardiac demand. Altering disciplinary patterns and deliberately preventing crying or interactions with other children could foster maladaptive behaviors. Contact with peers promotes normal growth and development.
52
98. The nurse is helping a pregnant client devise a plan to help her 2year-old adjust to the birth of her second child. Which suggestion is least appropriate? a. Provide the toddler with a doll so he can imitate the parents when they care for the newborn. b. Enroll the toddler in a sibling class offered at the local hospital. c. Discuss with the toddler what routines will be the same and what will be different after the baby arrives. d. Discuss with the toddler what routines will be the same and what will be different after the baby arrives. Answer: D Rationale: Telling a toddler that he will have a new playmate when the baby arrives sets up unrealistic expectations. Instead, the parents should stress activities that will take place, such as feeding, changing, and crying. Giving the toddler a doll is a good strategy because having the doll allows the toddler to take part in the new routines. For example, the toddler can pretend to meet the needs of the doll just like the mother tends to the baby. Participation in a sibling preparation class may also decrease sibling rivalry behaviors. Discussing changes in family routines will help the toddler know what to expect.
99. A 2-year-old is admitted to the pediatric unit with fever, seizures, and vomiting. He's awake and alert. As the nurse is putting a gown on the child, the nurse notices petechiae across the child's chest, abdomen, and back. The nurse should: a. question the mother about the child's allergies. b. initiate standard precautions. c. evaluate the child's neurologic status. d. examine the child's throat and ears. Answer: C
53
Rationale: These are signs of meningitis and the priority is to evaluate neurologic status. Petechiae aren't allergic reactions. Standard precautions should be used when there is risk of contacting body fluids (contact precautions should be instituted for the client diagnosed with meningitis). Throat and ear examinations wouldn't be helpful in confirming a diagnosis of meningitis.
100. A nurse on the pediatric floor is caring for a toddler. The nurse should keep in mind that toddlers: a. A nurse on the pediatric floor is caring for a toddler. The nurse should keep in mind that toddlers: b. have reliable verbal responses to pain. c. have a good concept of danger d. have little fear. Answer: A Rationale: A toddler's increasing autonomy is commonly expressed by negativism. They're unreliable in expressing pain they respond just as strongly to painless procedures as they do to painful ones. They have little concept of danger and have common fears.
101. An 18-month-old male child is admitted to the pediatric unit with a diagnosis of celiac disease. What finding would the nurse expect in this child? a. A concave abdomen b. Bulges in the groin area c. A protuberant abdomen d. A palpable abdominal mass Answer: C Rationale: A child with celiac disease has a protuberant abdomen due to the presence of fat, bulky stools, undigested food, and flatus. A concave 54
abdomen, bulges in the groin area, and a palpable abdominal mass aren't associated with celiac disease.
102. A parent brings a toddler, age 19 months, to the clinic for a regular checkup. When palpating the toddler's fontanels, what should the nurse expect to find? a. Closed anterior fontanel and open posterior fontanel b. Open anterior fontanel and closed posterior fontanel c. Closed anterior and posterior fontanels d. Open anterior and posterior fontanels Answer: C Rationale: By age 18 months, the anterior and posterior fontanels should be closed. The diamond-shaped anterior fontanel normally closes between ages 9 and 18 months. The triangular posterior fontanel normally closes between ages 2 and 3 months.
103. Which statement by the mother of a toddler with nephrotic syndrome indicates that the nurse's discharge teaching was effective? a. "I know that I'll need to keep my child as quiet as possible." b. "I just went out and bought all I'll need for the special diet." c. "I've been checking the urine for protein so I'll be able to do it at home." d. "I'm sure that my child will be back to normal soon." Answer: C Rationale: Protein in urine is an indication of the progression of nephrotic syndrome, so parents are taught to test the child's urine. The child doesn't need to be kept quiet and usually isn't on a specific diet. How the child feels will dictate the child's activity level. Most children return to normal soon but may relapse.
55
104. A toddler is hospitalized with multiple injuries. Although the parent states that the child fell down the stairs, the child's history and physical findings suggest abuse as the cause of the injuries. What should the nurse do first? a. Refer the parent to a support group such as Parents Anonymous. b. Report the incident to the proper authorities. c. Prepare the child for foster care placement. d. Restrict the parent from the child's room. Answer: B Rationale: The nurse is required by law to report all incidents of suspected child abuse. Once the appropriate authorities have been notified, the child can be placed under protective custody. Later, the nurse may need to prepare the child for foster care placement and refer the parent to a support group. After reporting suspected abuse, the nurse should allow the parent to visit and help care for the child; during these visits, the nurse should exhibit and reinforce positive parenting behaviors.
105. The nurse is caring for a 2-year-old child with tetralogy of Fallot. Which assessment findings should the nurse expect? a. Aortic stenosis, atrial septal defect, overriding aorta, and left ventricular hypertrophy b. Pulmonic stenosis, intraventricular septal defect, overriding aorta, and right ventricular hypertrophy c. Pulmonic stenosis, patent ductus arteriosus, overriding aorta, and right ventricular hypertrophy d. Transposition of the great vessels, intraventricular septal defect, right ventricular hypertrophy, and patent ductus arteriosus Answer: B
56
Rationale: Tetralogy of Fallot consists of four congenital anomalies: pulmonic stenosis, intraventricular septal defect, overriding aorta, and right ventricular hypertrophy. The other combinations of defects aren't characteristic of tetralogy of Fallot.
106. A toddler is brought to the emergency department with sudden onset of abdominal pain, vomiting, and stools that look like red currant jelly. To confirm intussusception, the suspected cause of these findings, the nurse expects the physician to order: a. a barium enema. b. suprapubic aspiration. c. nasogastric (NG) tube insertion. d. indwelling urinary catheter insertion. Answer: A Rationale: A barium enema commonly is used to confirm and correct intussusception. Performing a suprapubic aspiration or inserting an NG tube or an indwelling urinary catheter wouldn't help diagnose or treat this disorder.
107. The nurse is caring for a toddler who has just been immunized. When teaching the child's parents about potential adverse effects, the nurse should instruct the parents to immediately report: a. pain at the injection site. b. generalized urticaria. c. mild temperature elevation. d. local swelling at the injection site. Answer: B Rationale: Generalized urticaria can herald the onset of a lifethreatening episode and medical assistance should be sought immediately. A child may experience some pain, redness at the sight, 57
localized swelling, or mild temperature elevation. These reactions can be treated symptomatically and aren't life-threatening.
108. A mother calls the poison control center after her 2-year-old son ingests half of a bottle of aspirin. The poison control center instructs her to give the child 15 ml of ipecac syrup followed by 200 ml of water. How soon after receiving ipecac should the child begin to vomit? a. Immediately b. Within 30 minutes c. Within 60 minutes d. Within 90 minutes Answer: B Rationale: After administration of ipecac syrup, a delay of
approximately 10 minutes usually occurs before onset of vomiting. About 50% of the clients receiving ipecac will begin vomiting in less than 20 minutes; about 90% will vomit within 30 minutes.
109. A 15-month-old child is being discharged after treatment for severe otitis media and bacterial meningitis. Which statement by the parents indicates effective discharge teaching? a. "We should have gone to the physician sooner. Next time, we will." b. "We'll take our child to the physician's office every week until everything is okay." c. "We'll go to the physician if our child pulls on the ears or won't lie down." d. "We're just so glad this is all behind us." Answer: C Rationale: The parents indicate full understanding of discharge teaching by repeating the specific, common signs of otitis media in toddlers, such 58
as pulling on the ears and refusing to lie down, and by verbalizing the need for immediate follow-up care if these signs arise. Option A implies a sense of guilt. Option B addresses only weekly follow-up care. Option D is unrealistic because the child's condition may recur.
110. A toddler is admitted to the facility for treatment of a severe respiratory infection. The child's recent history includes fatty stools and failure to gain weight steadily. The physician diagnoses cystic fibrosis. By the time of the child's discharge, the child's parents must be able to perform which task independently? a. Allergy-proofing the home b. Maintaining the child in an oxygen tent c. Maintaining the child on a fat-free diet d. Performing postural drainage Answer: D Rationale: The client with cystic fibrosis is at risk for frequent respiratory infections secondary to increased viscosity of mucus gland secretions. To help prevent respiratory infections, caregivers must perform postural drainage several times daily to loosen and drain secretions. Because exocrine gland dysfunction, not an allergic response, causes bronchial obstruction in cystic fibrosis, allergy-proofing the home isn't necessary. Oxygen therapy may be indicated, but only during acute disease episodes. Also, such therapy must be supervised closely; home oxygen therapy is inappropriate because chronic hypoxemia poses the risk of oxygen toxicity. If steatorrhea can't be controlled, the child should reduce, but not eliminate, dietary fat intake.
111. The nurse is providing dietary teaching for the parents of a child with celiac disease. This child should avoid: a. vegetables. b. fruits. c. prepared puddings. 59
d. rice. Answer: C Rationale: A child with celiac disease mustn't consume foods containing gluten and therefore should avoid prepared puddings, commercially prepared ice cream, malted milk, and all food and beverages containing wheat, rye, oats, or barley. The other options don't contain gluten and are permitted on a gluten-free diet.
112. A child with suspected rheumatic fever is admitted to the pediatric unit. When obtaining the child's history, the nurse considers which information to be most important? a. A fever that started 3 days ago b. Lack of interest in food c. A recent episode of pharyngitis d. Vomiting for 2 days Answer: C Rationale: A recent episode of pharyngitis is the most important factor in establishing the diagnosis of rheumatic fever. Although the child may have a history of fever or vomiting or lack interest in food, these findings aren't specific to rheumatic fever
113. When assessing a child for impetigo, the nurse expects which assessment findings? a. Small, brown, benign lesions b. Honey-colored, crusted lesions c. Linear, threadlike burrows d. Circular lesions that clear centrally Answer: B
60
Rationale: In impetigo, honey-colored, crusted lesions develop once the pustules rupture. Small, brown, benign lesions are common in children with warts. Linear, threadlike burrows are typical in a child with scabies. Circular lesions that clear centrally characterize tinea corporis.
114. The physician diagnoses leukemia in a child, age 4, who complains of being tired and sleeps most of the day. Which nursing diagnosis reflects the nurse's understanding of the physiologic effects of leukemia? a. Ineffective airway clearance related to fatigue b. Activity intolerance related to anemia c. Imbalanced nutrition: More than body requirements related to lack of activity d. Ineffective tissue perfusion related to central nervous system infiltration by leukemic cells Answer: B Rationale: A child with leukemia may experience anemia from bone marrow depression, such as from chemotherapy or replacement of normal bone marrow elements by immature white blood cells. Anemia results in fatigue, lack of energy, and activity intolerance. The information given in the question doesn't support the other diagnoses.
115. When planning care for a child with epiglottitis, the nurse should assign highest priority to: a. providing psychological support. b. ensuring respiratory patency. c. instituting infection control. d. administering prescribed drug therapy. Answer: B Rationale: Because respiratory obstruction is a life-threatening
complication of epiglottitis, ensuring respiratory patency takes highest 61
priority. The other options are important but don't take precedence over ensuring respiratory patency.
116.
A preschooler
goes
into cardiac
arrest.
When performing
cardiopulmonary resuscitation (CPR) on a child, how should the nurse deliver chest compressions? a. With two hands b. With two fingertips c. With the palm of one hand d. With the heel of one hand Answer: D Rationale: When performing CPR on a child between ages 1 and 8, the nurse should use the heel of one hand to compress the chest 1" to 1" (2.5 to 3.75 cm). The use of two hands (one placed on top of the other) is appropriate for adult CPR but can injure a child. The use of two fingertips is appropriate for infant CPR but can't compress the chest sufficiently on an older child. The palm is never used for chest compressions in CPR. 117. The mother of a child with sickle cell anemia confides in the nurse that she feels guilty about letting the child run and play with the neighborhood children and that if she had been a better mother, the child wouldn't have suffered a sickle cell crisis. Which response would be most appropriate? a. "She's just fine now, don't worry." b. "Tell me more about how you feel." c. "But you know that children with sickle cell anemia often have crises." d. "You shouldn't be so protective of her." Answer: B
62
Rationale: Many parents feel guilty when their child is sick. Encouraging parents to talk more about their feelings provides support and helps to develop a therapeutic relationship. Giving a stereotyped answer, such as "Don't worry," shows a lack of interest in what the parent is feeling. Commenting on the course of the disease doesn't address the parent's feelings. Being judgmental or offering an opinion can also block therapeutic communication by inhibiting the parent from discussing her feelings and developing solutions.
118. The nurse suspects that a child, age 4, is being neglected physically. To best assess the child's nutritional status, the nurse should ask the parents which question? a. "Has your child always been so thin?" b. "Is your child a picky eater?" c. "What did your child eat for breakfast?" d. "Do you think your child eats enough?" Answer: C Rationale: The nurse should obtain objective information about the child's nutritional intake such as by asking about what the child ate for a specific meal. The other options ask for subjective replies that would be open to interpretation.
119. When telling a 4-year-old child about an upcoming procedure, the nurse's most important consideration is to: a. use simple terms. b. speak loudly and clearly. c. offer a toy to keep the child happy. d. include every detail. Answer: A
63
Rationale: When explaining a procedure to a 4-year-old child, the nurse must use simple terms that the child can understand. Speaking loudly may provoke anxiety. Distracting the child with a toy is more appropriate during the procedure than before it. Because preschoolers have a limited attention span, the nurse should provide only the necessary basic facts to prevent anxiety.
120. Parents report that their daughter, age 4, resists going to bed at night. After instruction by the nurse, which statement by the parents indicates effective teaching? a. "We'll let her fall asleep in our room, then move her to her own room." b. "We'll lock her in her room if she gets up more than once." c. "We'll play running games with her before bedtime to tire her out, and then she'll fall asleep easily." d. "We'll read her a story and let her play quietly in her bed until she falls asleep." Answer: D Rationale: Spending time with the parents and playing quietly are positive bedtime routines that provide security and prepare a child for sleep. The child should sleep in her own bed. Locking the door is frightening and may cause insecurity. Active play before bedtime stimulates the child and increases the time needed to settle down for sleep.
121. A child, age 4, with a recent history of nausea, vomiting, and diarrhea is admitted to the pediatric unit with a diagnosis of gastroenteritis. During the physical examination, the nurse detects tenting. This finding supports a nursing diagnosis of: a. Deificient fluid volume related to dehydration. b. Risk for injury related to capillary fragility.
64
c. Ineffective peripheral tissue perfusion related to peripheral cyanosis. d. Activity intolerance related to hypoxia. Answer: A Rationale: Tenting, which indicates decreased skin turgor, is normal in geriatric clients and results from decreased elastin content. However, in other adults and in children, tenting more commonly results from dehydration. Therefore, this finding supports a nursing diagnosis of Deficient fluid volume related to dehydration. The other options are inappropriate because capillary fragility, altered tissue perfusion, and hypoxia rarely are associated with gastroenteritis.
122. The nurse is preparing a child, age 4, for cardiac catheterization. Which explanation of the procedure is mostappropriate? a. "Don't worry. It won't hurt." b. "The test usually takes an hour." c. "You must sleep the whole time that the test is being done." d. "The special medicine will feel warm when it's put in the tubing." Answer: D Rationale: To prepare a 4-year-old child without increasing anxiety, the nurse should provide concrete information in small amounts about nonthreatening aspects of the procedure. Saying that it won't hurt may prevent the child from trusting the nurse in the future. Explaining the time needed for the procedure wouldn't provide sufficient information. Stating that the child will need to sleep could provoke anxiety; also, it's untrue.
123. A boy, age 4, begins to use curse words. Concerned about this behavior, his parents ask the nurse how to curtail it. Which advice should the nurse offer?
65
a. "Just ignore it. He'll grow out of it." b. "Tell him it isn't acceptable and he'll be disciplined if he continues to do it." c. "Tell him that good little boys don't use curse words." d. "Tell him that his behavior makes you angry." Answer: B Rationale: By explaining their objections and expectations, the parents teach the child why the behavior is unacceptable and help him understand that he must stop it. Options A and D wouldn't teach the child that his behavior is inappropriate. Option C would reinforce the impression that the child is "bad," diminishing his self-image while doing little to change the objectionable behavior.
124. A mother complains to the nurse that her 4-year-old son often "lies." What is the nurse's best response? a. "Let the child know that he'll be punished for lying." b. "Ask him why he isn't telling the truth." c. "It's probably due to his vivid imagination and creativity." d. "Acknowledge him by saying, 'That's a pretend story.'" Answer: D Rationale: It's important to acknowledge the child's imagination, while also letting him know in a nice way that what he has said isn't real. Punishment isn't appropriate for a 4-year-old child using his imagination, and accusing him of lying is a negative reinforcement. The child isn't truly lying in the adult sense. Imagination and creativity need to be acknowledged.
125. For a child with hemophilia, what is the most important nursing goal? a. Enhancing tissue perfusion 66
b. Preventing bleeding episodes c. Promoting tissue oxygenation d. Controlling pain Answer: B Rationale: A child with hemophilia is prone to bleeding episodes stemming from coagulatory problems. Therefore, the primary nursing goal is to prevent bleeding episodes and possible hemorrhage. A secondary effect of preventing bleeding episodes is maintenance of tissue perfusion and oxygenation. Hemophilia rarely causes pain.
126. A preschool-age child refuses to take prescribed medication. Which nursing strategy would be most appropriate? a. Mixing the medication in milk so the child isn't aware that it's there b. Explaining the medication's effects in detail to ensure cooperation c. Making the child feel ashamed for not cooperating d. Showing trust in the child's ability to cooperate even with an unpleasant procedure Answer: D Rationale: To gain a preschooler's cooperation, the nurse should show trust and express faith in the child's ability to cooperate even with an unpleasant procedure. Hiding the medication in milk may foster mistrust. The nurse should provide simple, not detailed, explanations and should use terms the child can understand. Shaming the child is inappropriate and may lead to feelings of guilt.
127. When meeting with a family who'll learn that their 3-year-old is seriously ill, which action demonstrates the nurse's role as collaborator of care?
67
a. Provide the parents with information about financial assistance programs. b. Inform the family of the diagnosis and recently discovered findings c. Coordinate the multidisciplinary services and provide information about them. d. Refer and consult with other specialties to help in treating the diagnosis. Answer: C Rationale: The nurse can coordinate care when multiple services are involved, explaining the function of service (social service, case management, counseling services, and so forth). For instance, providing parents with information about financial assistance programs is the responsibility of social services. Informing the family of the diagnosis and recently discovered findings is a physician's responsibility as is referring and consulting with other specialties.
128. For a child who's admitted to the emergency department with an acute asthmatic attack, nursing assessment is most likely to reveal: a. apneic periods. b. expiratory wheezing. c. inspiratory stridor. d. absent breath sounds. Answer: B Rationale: Expiratory wheezing is common during an acute asthmatic attack and results from narrowing of the airway caused by edema. Acute asthma rarely causes apneic periods. Inspiratory stridor more commonly accompanies croup. Acute asthma is more likely to cause adventitious breath sounds than absent breath sounds.
129. A mother brings her preschool child to the emergency department because he hasn't vomited after receiving two doses of ipecac for
68
ingesting an unknown quantity of acetaminophen. Which treatment will the physician probably prescribe next? a. Administration of another dose of ipecac syrup b. Insertion of a nasogastric tube and administration of an antacid] c. I.V. infusion of normal saline solution d. Gastric lavage and administration of activated charcoal Answer: D Rationale: If two doses of ipecac syrup don't produce emesis, the nurse should prepare to take other measures as prescribed, such as gastric lavage or activated charcoal administration. A third dose of ipecac syrup isn't likely to be effective. An antacid isn't an effective treatment for poisoning. Infusing normal saline solution I.V. may be helpful in treating dehydration caused by vomiting but in itself isn't effective in eliminating the poisonous substance.
130. When assessing a family suspected of abusing its 4-year-old child, which of the following is the most important criteria that would suggest abuse? a. Attempts by the child to defend or verify what the parent states b. Incompatibility between the history (mechanism) and the injury c. Responsibility taken by the child for the act d. A complaint other than the one associated with the signs of abuse Answer: B Rationale: The most important criteria on which to base a decision for reporting suspected abuse is an incompatibility between the history and the injury. A maltreated child will rarely betray his parents by saying he has been abused and will, instead, attempt to defend the parent's action and verify the story. The child may even take responsibility for the act in attempt to vindicate them. A complaint other than the one associated with the signs of abuse (for example, a complaint of being cold when second-degree burns are visible) is a warning sign of abuse. 69
131. Which of the following techniques is most effective in preventing nosocomial infection transmission when caring for a preschooler? a. Client isolation b. Standard precautions c. Hand washing d. Needleless syringe system Answer: C Rationale: Hand washing is the single most important measure for preventing infection transmission. Isolating the child and using infection control precautions are required for certain diseases, such as varicella, diphtheria, mumps, pertussis, measles, and meningitis. Standard precautions, which include hand washing, are guidelines for treating all clients as potentially infectious. A needleless syringe system will prevent transmission through needle sticks but not from body fluid contact.
132. A child is admitted to the pediatric unit with a fracture of the hip. The physician orders Russell traction. This type of traction is: a. skin traction applied to a lower extremity, with the extremity suspended above the bed. b. skeletal traction applied to a lower extremity. c. skin traction applied to an extended lower extremity. d. skin traction applied bilaterally to the lower extremities. Answer: A Rationale: Russell traction is skin traction applied to a lower extremity, with the extremity suspended above the bed and a sling placed under the knee. Skeletal traction applied to a lower extremity is called 90-90 traction. Skin traction applied to an extended lower extremity is called Buck's extension traction. Skin traction applied bilaterally to the lower extremities is called Bryant's traction. 70
133. A preschool-age child underwent a tonsillectomy 4 hours ago. Which assessment finding would make the nurse suspect postoperative hemorrhage? a. Vomiting of dark brown emesis b. Refusal to drink clear fluids c. Decreased heart rate d. Frequent swallowing Answer: D Rationale: Frequent swallowing an attempt to clear the throat of trickling blood suggests postoperative hemorrhage. Emesis may be brown or blood-tinged after a tonsillectomy; only bright red emesis signals hemorrhage. The child may refuse fluids because of painful swallowing, not bleeding. Hemorrhage is associated with an increased, not decreased, heart rate.
134. A child, age 3, who tests positive for the human immunodeficiency virus (HIV) is placed in foster care. The foster parents ask the nurse how to prevent HIV transmission to other family members. How should the nurse respond? a. "Make sure the child uses disposable plates and utensils." b. "Use isopropyl alcohol to clean surfaces contaminated with the child's blood or body fluids." c. "Don't let the child share toys with other children." d. "Wear gloves when you're likely to come into contact with the child's blood or body fluids." Answer: D Rationale: HIV is transmitted by blood and body fluids. Therefore, family members should wear gloves when anticipating contact with the child's blood or body fluids. To disinfect HIV-contaminated surfaces, the nurse 71
should instruct the foster parents to use a solution of 1 part bleach to 10 parts water. Standard household methods for cleaning dishes and utensils are adequate, so the child needn't use disposable plates and utensils. The child may share toys; any toys that become soiled with the child's blood or body fluids should be disinfected with the bleach solution.
135. The nurse is developing a teaching plan for a child with acute poststreptococcal glomerulonephritis. What is the most important point to address in this plan? a. Infection control b. Nutritional planning c. Prevention of streptococcal pharyngitis d. Blood pressure monitoring Answer: D Rationale: Because poststreptococcal glomerulonephritis may cause severe, life-threatening hypertension, the nurse must teach the parents how to monitor the child's blood pressure. Infection control, nutritional planning, and prevention of streptococcal pharyngitis are important but are secondary to blood pressure monitoring.
136. When assessing a preschooler who has sustained a head trauma, the nurse notes that the child appears to be obtunded. Which of the following denotes the child's level of consciousness? a. No motor or verbal response to noxious (painful) stimuli b. Remains in a deep sleep; responsive only to vigorous and repeated stimulation c. Can be aroused with stimulation d. Limited spontaneous movement; sluggish speech Answer: C
72
Rationale: The child is obtunded if he can be aroused with stimulation. If the child shows no motor or verbal response to noxious stimuli, he's comatose. If the child remains in a deep sleep and is responsive only to vigorous and repeated stimulation, he's stuporous. If the child has limited spontaneous movement and sluggish speech, he's lethargic.
137. A child, age 3, is hospitalized for treatment of Kawasaki disease. During the acute phase of this disease, the nurse must assess the child frequently for: a. heart failure. b. kidney failure. c. desquamation of the hands and feet. d. hepatitis. Answer: A Rationale: Kawasaki disease, which affects young children, is
characterized by acute systemic vasculitis. Myocarditis, a major complication of this disease, commonly causes left-sided heart failure. Therefore, the nurse must monitor the client's weight, fluid intake and output, and vital signs closely for evidence of heart failure. Kidney failure and hepatitis aren't associated with Kawasaki disease. Desquamation of the hands and feet typically occurs after the acute disease phase ends and doesn't pose a danger.
138. The parents of a child with cystic fibrosis, an autosomal recessive disorder, are considering having a second child. Each parent is heterozygous for the cystic fibrosis trait. What is the chance that their second child will manifest the disorder? a. 0% b. 25% c. 50% d. 100% Answer: B 73
Rationale: To manifest, or express, an autosomal recessive disorder, a child must inherit the trait from both parents. A heterozygous person carries one normal gene and one affected gene and doesn't express the disorder. A child of two heterozygous parents has a one-in-four (25%) chance of manifesting an autosomal recessive disorder. Outcomes of previous pregnancies don't influence the probability of subsequent offspring expressing the genetic disorder.
139. When assessing a child with bronchiolitis, which finding does the nurse expect? a. Clubbed fingers b. Barrel chest c. Barking cough and stridor d. Productive cough Answer: D Rationale: Bronchiolitis causes a productive cough. Clubbed fingers and a barrel chest are more likely in a client with chronic respiratory problems. A barking cough is associated with acute laryngotracheobronchitis.
140. A preschool child presents with a history of vomiting and diarrhea for 2 days. Which assessment finding indicates that the child is in the late stages of shock? a. Tachycardia b. Bradycardia c. Irritability d. Urine output 1 to 2 ml/kg/hour Answer: B
74
Rationale: Bradycardia is a sign of late shock in a pediatric client. Cardiovascular dysfunction and impairment of cellular function lead to lowered perfusion pressures, increased precapillary arteriolar resistance, and venous capacitance. Decreased cardiac output occurs in late shock if the circulating volume isn't replaced. Sympathetic nervous innervation has limited compensation mechanisms if the volume isn't replaced. Tachycardia and irritability occur during the early phase of shock as compensatory mechanisms are implemented to increase cardiac output. Normal urine output for a pediatric client is 1 to 2 ml/kg/hour; volumes less than this would indicate a decrease in renal perfusion and activation of the renin-angiotensin-aldosterone system to decrease water and sodium excretion.
141. A child is suspected of having amblyopia ("lazy eye"). To help diagnose this disorder, the child will undergo which test? a. Snellen's test b. Near vision test c. Cover-uncover test d. Peripheral vision test Answer: C Rationale: The cover-uncover test assesses the fusion reflex, which makes binocular vision possible. During this test, the "lazy eye" exhibits wandering. Snellen's test assesses visual acuity, the near vision test evaluates near vision, and the peripheral vision test evaluates peripheral vision
142. A child, age 4, who has been hospitalized with asthma is to receive oral theophylline at home. Before discharge, the nurse teaches the parents about signs and symptoms of theophylline toxicity and the need to report these promptly. Which statement by the parents indicates effective teaching? a. "We will report irritability and restlessness." b. "We will report a slow pulse and lethargy." 75
c. "We will report a rash and swelling of the hands and feet." d. "We will report coughing and wheezing." Answer: A Rationale: Theophylline causes bronchodilation by promoting
adrenergic activation. Signs and symptoms of theophylline toxicity reflect adrenergic stimulation and include irritability, restlessness, tachycardia, and insomnia. Theophylline also may cause such adverse GI effects as nausea, vomiting, diarrhea, and epigastric pain. Rash and swelling of the hands and feet aren't associated with theophylline toxicity. Coughing and wheezing are signs of asthma, not theophylline toxicity.
143. A child, age 5, is hospitalized for treatment of Kawasaki disease. Which nursing action would best identify potential complications of this disease? a. Auscultating breath sounds b. Instituting cardiac monitoring c. Monitoring blood pressure d. Assessing the skin daily Answer: B Rationale: Kawasaki disease sometimes causes cardiac complications, including arrhythmias. Instituting cardiac monitoring is crucial in detecting such complications. Auscultating breath sounds, monitoring blood pressure, and assessing the skin daily are important but to a lesser degree.
144. The nurse has just administered a drug to a child. Which organ is most responsible for drug excretion in children? a. Heart b. Lungs 76
c. Kidneys d. Liver Answer: C Rationale: The kidneys are most responsible for drug excretion in children. Less commonly, some drugs may be excreted via the lungs or liver. Drugs are never excreted by the heart in children or adults.
145. A 4-year-old girl has a urinary tract infection (UTI). When teaching the parents how to help her avoid recurrent UTIs, the nurse should emphasize which preventive measure? a. Wiping her perineum from back to front after she uses the toilet b. Wiping her perineum from back to front after she uses the toilet c. Giving her a warm bath for 15 minutes daily d. Making sure she avoids bubble baths Answer: D Rationale: The child should avoid bubble baths because oils in the bubble bath preparation may irritate the urethra, contributing to UTIs. Girls and women should wipe the perineum from front to back, not back to front, to avoid contaminating the urinary tract with fecal bacteria. Although antibiotics UTIs. are used to treat UTIs, they aren't given prophylactically. No evidence suggests that warm baths help prevent
146. The nurse is evaluating a child with acute poststreptococcal glomerulonephritis (APSGN) for signs of improvement. Which finding typically is the earliest sign of improvement? a. Increased urine output b. Increased appetite c. Increased energy level d. Decreased diarrhea
77
Answer: A Rationale: Increased urine output, a sign of improving kidney function, typically is the first sign that a child with APSGN is improving. Increased appetite, an increased energy level, and decreased diarrhea aren't specific to APSGN.
147. The parents of a school-age child with asthma express concern about letting the child participate in sports. What should the nurse tell the parents about the relationship between exercise and asthma? Asthma attacks are triggered by allergens, not exercise. The child should avoid exercise because it may trigger asthma attacks. Continuous activities such as jogging are less likely to trigger asthma than intermittent activities such as baseball. Taking prophylactic drugs before the activity can prevent asthma attacks and enable the child to engage in most sports. Answer: D Rationale: Although exercise may trigger asthma attacks, taking prophylactic asthma drugs before beginning the activity can prevent attacks, enabling the child to engage in most sports. Asthma attacks may be triggered by various factors, including allergens, exercise, medications, upper respiratory infections, and psychological stress. Provided the asthma is under control, most children can participate in sports and other physical activities; in fact, they benefit from exercise. Activity restrictions hamper peer interaction, which is essential to the development of the school-age child. A child with asthma may tolerate intermittent activities better than continuous ones.
148. When planning care for a 7-year-old boy with Down syndrome, the nurse should:
78
plan interventions at the developmental level of a 7-year-old because that is the child's age. plan interventions at the developmental level of a 5-year-old because the child will have developmental delays. assess the child's current developmental level and plan care accordingly. direct all teaching to the parents because the child can't understand. Answer: C Rationale: Nursing care should be planned at the developmental age of a child with Down syndrome, not the chronological age. Because children with Down syndrome can vary from mildly to severely mentally challenged, each child should be individually assessed. A child with Down syndrome is capable of learning, especially one with mild limitations. Gear teaching toward the appropriate developmental age.
149. When attempting to facilitate spiritual support for a school-age child with a life-threatening disease and her family, which of the following would be least effective? Becoming familiar with the family's spiritual beliefs and practices Seeking assistance or referrals to the facility chaplain or other resources Being open to the family's and the child's expressions of spiritual concerns Promoting the nurse's personal values and beliefs if she considers the family's to be inappropriate Answer: D Rationale: The nurse needs to recognize that her personal values and beliefs may not be effective for others and that she shouldn't judge others' beliefs. Becoming familiar with the family's spiritual beliefs and practices, seeking assistance or referrals to the facility chaplain or other resources, and being open to the family's and the child's expressions of
79
spiritual concerns are all ways to help children and their families use their spiritual beliefs to cope with a life-threatening illness.
150. The nurse is interviewing the mother of a 7-year-old child. Which of the following symptoms reported by the mother would most lead the nurse to suspect that the child has type 1 diabetes? Recent bed-wetting Poor appetite Weight gain Boundless energy Answer: A Rationale: Polyuria is a hallmark sign of type 1 diabetes mellitus. Parents often notice this symptom as bed-wetting in a child previously toilet-trained. Polyphagia is also a hallmark sign of type 1 diabetes mellitus. A parent is likely to report that a child eats excessively but seems to be losing weight. The child with type 1 diabetes mellitus may also complain of fatigue.
151. What is the most common assessment finding in a child with ulcerative colitis? Intense abdominal cramps Profuse diarrhea Anal fissures Abdominal distention Answer: B Rationale: Ulcerative colitis causes profuse diarrhea. Intense abdominal cramps, anal fissures, and abdominal distention are more common in Crohn's disease.
80
152. A chronically ill school-age child is most vulnerable to which stressor? Mutilation anxiety Anticipatory grief Anxiety over school absences Fear of hospital procedures Answer: C Rationale: The school-age child is becoming industrious and attempts to master school-related activities. Therefore, school absences are likely to cause extreme anxiety for a school-age child who's chronically ill. Mutilation anxiety is more common in adolescents. Anticipatory grief is rare in a school-age child. Fear of hospital procedures is most pronounced in preschool-age children. 153. The nurse is caring for a school-age child with cerebral palsy. The child has difficulty eating using regular utensils and requires a lot of assistance. Which of the following referrals is most appropriate? a. Registered dietitian b. Physical therapist c. Occupational therapist d. Nursing assistant Answer: C Rationale: An occupational therapist helps physically disabled clients adapt to physical limitations and is most qualified to help a child with cerebral palsy eat and perform other activities of daily living. A registered dietitian manages and plans for the nutritional needs of children with cerebral palsy but isn't trained in modifying or fitting utensils with assistive devices. A physical therapist is trained to help a child with cerebral palsy gain function and prevent further disability but not to assist the child in performing activities of daily living. A nursing assistant can help a child eat; however, the nursing assistant isn't trained in modifying utensils.
81
154. The nurse in a well-child clinic is assessing children for scoliosis. Which of the following children is most at risk for scoliosis? a. 8-year-old boy b. Teenage boy c. 6-year-old girl d. 10-year-old girl Answer: D Rationale: The 10-year-old girl is most likely to have scoliosis. Scoliosis is five times more common in girls than boys, and its peak age of incidence is between ages 8 and 15. The 8-year-old boy or a teenage boy may develop scoliosis but it's more common in females. A 6-yearold girl is typically too young to be diagnosed with scoliosis.
155. One day after an appendectomy, a 9-year-old rates his pain at 4 out of 5 on the pain scale but is playing video games and laughing with his friend. Which of the following would the nurse document on the child's chart? a. The child is in no apparent distress, and no pain medication is needed at this time. b. The child rates pain at 4 out of 5. Pain medication administered as prescribed. c. The child doesn't understand the pain scale. Performed teaching to help child match his pain rating to how he appears to be feeling. d. The child rates his pain at 4 out of 5; however, he appears to be in no distress. Reassess when he's visibly showing signs of pain. Answer: B Rationale: Pain is what the child says it is, and the nurse must document what the child reports. If a child's behavior appears to differ from the child's rating of pain, believe the pain rating. A child who uses 82
passive coping behaviors (such as distraction and cooperative) may rate pain as more intense than children who use active coping behaviors (such as crying and kicking). Nurses frequently make judgments about pain based on behavior, which can result in children being inadequately medicated for pain.
156. The mother of a school-age child reports that her child is having some problems in school. Which of the following would be the priority action? a. Obtain more information from the mother and the child. b. Refer the child to the school psychologist for testing. c. Talk to the child's health care provider to understand the child better. d. Talk to the child's teacher to gain a perspective on the situation. Answer: A Rationale: In this situation, the nurse needs more information before proceeding and should question the mother and child about the problems. Referring the child to the school psychologist and talking to the child's health care provider and teacher are all important components of a treatment plan, but obtaining more information comes first.
157. The parents of a school-age child request anticipatory guidance. When developing a plan of care to address this matter, the nurse should keep in mind that this child's cognitive development is characterized by: a. magical thinking. b. transductive reasoning. c. abstract thought. d. conservation skills. Answer: D
83
Rationale: According to Piaget, a school-age child acquires cognitive operations to understand concepts related to objects, including conservation skills, classification skills, and combinational skills. Magical thinking and transductive reasoning are characteristic of the preschooler's preoperational thought. Abstract thought is characteristic of the adolescent's period of formal operations.
158. After a car accident, a child, age 10, is treated in the emergency department for a fractured clavicle and evaluated for a possible head injury. Alert and oriented, she keeps asking what will happen to her. Which nursing diagnosis is most appropriate? a. Anxiety related to separation from parents and an unfamiliar environment b. Hypothermia related to head injury c. Interrupted family processes related to maturational crisis d. Risk for infection related to sepsis Answer: A Rationale: The nature of the accident, the child's pain, and the unfamiliar facility environment support a nursing diagnosis of Anxiety. A diagnosis of Hypothermia related to head injury isn't appropriate because the child is alert and oriented, indicating that a head injury, if present, isn't severe and is unlikely to cause hypothermia. Unlike the homecoming of a new baby or riding a bicycle for the first time, a car accident isn't a maturational crisis. Risk for infection related to sepsis isn't a plausible nursing diagnosis at this time.
159. The parents of a child, age 6, who will begin school in the fall ask the nurse for anticipatory guidance. The nurse should explain that a child of this age: a. still depends on the parents. b. rebels against scheduled activities. c. is highly sensitive to criticism. d. loves to tattle. 84
Answer: C Rationale: In a 6-year-old child, a precarious sense of self causes overreaction to criticism and a sense of inferiority. By age 6, most children no longer depend on the parents for daily tasks and love the routine of a schedule. Tattling is more common at age 4 or 5; by age 6, the child wants to make friends and be a friend.
160. A child is admitted with a tentative diagnosis of clinical depression. Which assessment finding is most significant in confirming this diagnosis? a. Irritability b. Sadness c. Weight gain d. Fatigue Answer: B Rationale: Clinical depression is diagnosed if the child exhibits a depressed mood (sadness) or loss of interest. Irritability isn't diagnostic for depression. Although a depressed child may gain weight and report fatigue, these findings aren't essential to the diagnosis.
161. A 10-year-old girl visits the clinic for a check-up before entering school. The child's mother questions the nurse about what to expect of her daughter's growth and development at this stage. Which response is most appropriate? a. "Her physical development will be rapid at this stage and rapid development will continue from now on." b. "She'll become more independent and won't require parental supervision." c. "Don't anticipate any changes at this stage in her growth and development." 85
d. "Friends will be very important to her, and she'll develop an interest in the opposite sex." Answer: D Rationale: Friends become very important at this age. Children usually begin having an interest in the opposite sex around this age, although they aren't always willing to admit it. Her physical development towards maturity continues, but it isn't as rapid at this stage as in previous years. Although independence increases at this stage, children continue to need parental supervision. Growth and development slow down but gradual changes continue to occur.
162. When administering morphine, the drug of choice for pediatric pain relief, to a school-age child, which symptom should cause the nurse to be concerned? a. Constipation b. Nausea and vomiting c. Pruritus d. Anemia Answer: D Rationale: Anemia isn't a typical adverse effect of morphine and should be investigated if it's discovered during treatment. Constipation, nausea and vomiting, and pruritus are all treatable adverse effects of morphine and don't necessitate cessation of the medication.
163. According to Erikson's psychosocial theory of development, an 8year-old would be in which of the following stages? a. Trust versus mistrust b. Initiative versus guilt c. Industry versus inferiority d. Identity versus role confusion 86
Answer: C Rationale: In middle childhood, the 6- to 12-year-old child is mastering the task of industry versus inferiority. The trust versus mistrust task is in infancy (birth to 1 year). In early childhood, the 1- to 3-year-old child is in the stage of initiative versus guilt. Identity versus role confusion occurs during adolescence. 164. The parents of a 9-year-old child in the terminal phase of a fatal illness ask the nurse for guidance in discussing death with their child. Which response is appropriate? a. "Children of that age view death as temporary and reversible, which makes it hard to explain." b. "Children of that age typically fantasize about what dying will be like, which is much better than knowing the truth." c. "At this developmental stage, children are afraid of death, so it's best not to discuss it with them." d. "At this developmental stage, most children have an adult concept of death and should be encouraged to discuss it." Answer: D Rationale: By age 9 or 10, most children have an adult concept of death. Caregivers should discuss death with them in terms consistent with their developmental stage. School-age children respond well to concrete explanations about death and dying. Preschoolers, not schoolage children, typically view death as temporary and reversible. Schoolage children may fantasize about the unknown aspects of death; these fantasies may increase their anxiety. Although a child may fear death, accurate information about death can ease anxiety.
165. The physician prescribes corticosteroids for a child with nephrotic syndrome. What is the primary purpose of administering corticosteroids to this child? a. To increase blood pressure 87
b. To reduce inflammation c. To decrease proteinuria d. To prevent infection Answer: C Rationale: The primary purpose of administering corticosteroids to a child with nephrotic syndrome is to decrease proteinuria. Corticosteroids have no effect on blood pressure. Although they help reduce inflammation, this isn't the reason for their use in clients with nephrotic syndrome. Corticosteroids may predispose a client to infection. 166. After a series of tests, a 6-year-old client weighing 50 lb (22.7 kg) is diagnosed with complex partial seizures. The physician prescribes phenytoin (Dilantin), 125 mg by mouth twice a day. After the nurse administers phenytoin, where is the drug metabolized? a. Pancreas b. Kidneys c. Stomach d. Liver Answer: D Rationale: Phenytoin is metabolized in the liver. The pancreas isn't involved in the pharmacokinetic activity of phenytoin. The stomach absorbs orally administered phenytoin, which is excreted by the kidneys in the urine.
167. A nurse practicing in a nurse-managed clinic suspects that an 8year-old client's chronic sinusitis and upper respiratory infections may be due to allergies. She orders an immunoglobulin assay. Which of the following would the nurse expect to find elevated? a. Immunoglobulin E b. Immunoglobulin D c. Immunoglobulin G 88
d. Immunoglobulin M Answer: A Rationale: Immunoglobulin (Ig) E is predominantly found in saliva and tears as well as intestinal and bronchial secretions. Increased levels of IgE may be found in allergic disorders. IgD's physiological function is unknown and constitutes only 1% of the total number of circulating immunoglobulins. IgG is elevated in the presence of viral and bacterial infections. IgM is the first antibody activated after an antigen enters the body, and is especially effective against gram negative organisms.
168. Which assessment would alert the nurse that a hospitalized 7-yearold child is at high risk for a severe asthma exacerbation? a. Oxygen saturation of 95% b. Mild work of breath c. Intercostal or substernal retractions d. A history of steroid-dependent asthma Answer: D Rationale: A history of steroid-dependent asthma, a contributing factor to make this a high-risk client, requires the nurse to treat the situation as a severe exacerbation regardless of the severity of the current episode. Decreased oxygen saturation, cyanosis, and retractions are all assessments of an asthma exacerbation and should be treated with oxygen, nebulized respiratory treatments, and steroids. However, if a significant history of high-risk factors is absent, the episode can be moderately treated and followed up with the pediatrician.
169. A child is sent to the school nurse because, according to his teacher, he's constantly scratching his head. When the nurse assesses his hair and scalp, she finds evidence of lice. What did she see? a. Flaking of the scalp with pink, irritated skin exposed 89
b. Small white spots that adhere to the hair shaft, close to the scalp c. Scaly, circumscribed patches on the scalp, with mild alopecia in these areas d. Multiple tiny pustules on the scalp with no abnormal findings on the hair shafts Answer: B Rationale: The small white spots that adhere to the hair shafts are the eggs, or nits, of lice. These are easy to see and can't be brushed off like dandruff. Flaking of the scalp may indicate dandruff or a dry scalp. Scaly pustules, due to the scratching, may accompany a lice infestation, but nits would also be found on the hair shafts.
170. When administering total parenteral nutrition (TPN) through a peripheral I.V. to a school-age child, what is the lowest amount of glucose that is considered safe and not caustic to small veins that will also provide adequate TPN? a. 5% glucose b. 10% glucose c. 15% glucose d. 17% glucose Answer: B Rationale: The amount of glucose that is considered safe for peripheral veins while still providing adequate parenteral nutrition is 10%. A glucose amount of 5% isn't sufficient nutritional replacement, although it's safe for peripheral veins. Any amount above 10% glucose, such as 15% and 17%, must be administered via central venous access.
171. A child is admitted to the pediatric unit with a serum sodium level of 118 mEq/L. Which nursing action takes highest priority at this time? a. Replacing fluids slowly as ordered b. Instituting seizure precautions 90
c. Administering diuretic therapy as prescribed d. Administering sodium bicarbonate as prescribed Answer: B Rationale: A serum sodium level of 118 mEq/L indicates severe hyponatremia, which places the client at risk for seizures. Therefore, instituting seizure precautions takes highest priority. Fluid and sodium replacement should be done rapidly. Diuretic therapy isn't indicated because it may cause additional sodium loss. In a child with hyperkalemia, administering sodium bicarbonate would be appropriate because it promotes movement of potassium into the intracellular spaces.
172. A child who was hospitalized for sickle cell crisis is being discharged. Which client outcome demonstrates effective teaching regarding prevention of future crises? a. The client verbalizes the need to stay away from persons with known infections. b. The client verbalizes appropriate dietary restrictions. c. The client verbalizes the need to restrict fluid intake. d. The client participates in an aerobic exercise program. Answer: A Rationale: Preventing infections through proper hand washing and staying away from persons with known infections is an important measure in preventing sickle cell crises. Dietary restrictions aren't significant in preventing these crises. The client should maintain adequate hydration, not restrict fluid intake, and should avoid strenuous activity such as aerobics.
173. When caring for a child, age 12, who's diagnosed with osteomyelitis of the left femur, the nurse should take which action first?
91
a. Administering I.V. antibiotics as prescribed b. Drawing blood for cultures as ordered c. Monitoring hepatic and renal studies d. Preparing the child for immediate surgery Answer: B Rationale: Osteomyelitis, an infectious bone disease, typically results from Staphylococcus aureus or Haemophilus influenzae. Before antibiotic therapy begins, blood cultures must be obtained to identify the causative organism and determine its sensitivity to antimicrobial agents. Treatment may include high doses of antibiotics. Hepatic and renal studies are obtained during the course of antibiotic therapy to monitor for adverse effects. Later, surgery may be necessary to drain abscesses.
174. A 7-year-old child is admitted with epiglottitis. Which is the most likely finding on a lateral neck X-ray in a child with epiglottitis? a. Supraglottic narrowing b. Steeple sign c. Thickened mass d. Subglottic narrowing Answer: C Rationale: X-ray assessment of the lateral neck helps diagnose common respiratory emergencies in children. The lateral neck X-ray of a child with epiglottitis shows a thickened mass. The steeple sign is found in the client with viral croup syndrome. Subglottic narrowing with membranous tracheal exudate is found in bacterial tracheitis. Supraglottic narrowing isn't a diagnostic indicator. 175. A school-age child is admitted to the facility with a diagnosis of acute lymphoblastic leukemia. The nurse formulates a nursing diagnosis of Risk for infection. What is the most effective way for the nurse to reduce the child's risk of infection? 92
Implementing reverse isolation Maintaining universal precautions Requiring staff and visitors to wear masks Practicing thorough hand washing Answer: D Rationale: Both ALL and its treatment cause immunosuppression. Thorough hand washing is the single most effective way to prevent infection in an immunosuppressed client. Reverse isolation doesn't significantly reduce the incidence of infection in immunosuppressed clients; furthermore, isolation may cause psychological stress. Universal precautions are intended mainly to protect caregivers from contact with infectious matter, not to reduce the client's risk of infection. Staff and others needn't wear masks when visiting because most infections are transmitted by direct contact. Instead of relying on masks and other barrier methods, the nurse should keep persons with known infections out of the client's room.
176. A child, age 6, is anxious and upset before a scheduled bone marrow aspiration. During client preparation, the nurse should keep in mind that a. describing what the child will hear, see, smell, and feel will help the child cope with the procedure. b. the child's anxiety will decrease with each successive procedure. c. no small detail about the procedure should go unexplained. d. explaining bone marrow function will help the child understand the reason for the procedure. Answer: A Rationale: Children cope with situations better when they can anticipate sensations rather than just trying to comprehend technical explanations. Commonly, a child's anxiety increases rather than decreases with each successive procedure. A school-age child can't assimilate every detail. A 93
6-year-old can't understand an explanation of bone marrow function; also, such an explanation would be irrelevant. 177. When examining school-age and adolescent children, the nurse routinely screens for scoliosis. Which statement accurately summarizes how to perform this screening? Have the child stand firmly on both feet and bend forward at the hips, with the trunk exposed. Listen for a clicking sound as the child abducts the hips. Have the child run the heel of one foot down the shin of the other leg while standing. Have the child shrug the shoulders as the nurse applies mild pressure to the shoulders. Answer: A Rationale: To screen for scoliosis, a lateral curvature of the spine, the nurse has the child stand firmly on both feet with the trunk exposed and examines the child from behind, checking for asymmetry of the shoulders, scapulae, or hips. The nurse then asks the child to bend forward at the hips and inspects for a rib hump, a sign of scoliosis. The nurse would listen for a clicking sound while the child abducts the hips when screening for congenital hip dysplasia. The heel-to-shin test evaluates cerebellar function. Having the child shrug the shoulders against mild resistance helps evaluate the integrity of cranial nerve XI.
178. The nurse is giving instructions to parents of a school-age child diagnosed with sickle cell disease. The instructions should include which of the following? a. Apply cold to affected areas to reduce the child's discomfort. b. Restrict the child's fluids during crisis situations. c. Avoid areas of low oxygen concentration such as high altitudes. d. Encourage the child to exercise to reduce the likelihood of crisis. Answer: C 94
Rationale: The child should avoid areas of low oxygen, such as high altitudes, because they may precipitate sickle cell crisis. Applying warm compresses will reduce discomfort to the affected area; cold compresses, however, may add to discomfort by impairing circulation. The child should be encouraged to drink fluids to rehydrate cells. Strenuous exercise may induce sickle cell crisis. 179. Several children in a kindergarten class have been treated for pinworm. To prevent the spread of pinworm, the school nurse meets with the parents and explains that they should: tell the children not to bite their fingernails. not let children share hairbrushes. tell the children to cover their mouths and noses when they cough or sneeze. have their children immunized. Answer: A Rationale: Pinworms come out of the intestine through the anus at night to lay eggs, causing perianal itching. The child wakes up and may begin scratching. Eggs under the fingernails are carried to the mouth if the child chews on his nails, and the life-cycle of the pinworm continues. In addition to teaching children not to bite their fingernails, parents should keep the nails short and encourage hand washing before food preparation and eating. Sharing hairbrushes contributes to the spread of head lice, not pinworms. Although covering the mouth and nose are hygienic practices to reduce the spread of infections from respiratory droplets, doing so doesn't affect the spread of pinworms. There are no immunizations to protect against pinworms.
180. The nurse is planning care for a 10-year-old child in the acute phase of rheumatic fever. Which activity would be most appropriate for the nurse to schedule in the care plan? Playing ping-pong 95
Reading books Climbing on play equipment in the playroom Unrestricted ambulation Answer: B Rationale: During the acute phase of rheumatic fever, the child should be placed on bed rest to reduce the workload of the heart and prevent heart failure. An appropriate activity for this child would be reading books. The other activities are too strenuous during the acute phase.
181. A child with asthma is receiving theophylline. The nurse knows that theophylline is administered primarily to: a. decrease coughing induced by postnasal drip. b. dilate the bronchioles. c. reduce airway inflammation. d. eradicate the infection. Answer: B Rationale: Methylxanthines, such as theophylline, are highly potent bronchodilators used to relieve asthma symptoms. Antihistamines typically are used to relieve a cough induced by postnasal drip; corticosteroids, to reduce airway inflammation; and antibiotics, to treat infection.
182. A 10-year-old boy falls, injures his left shoulder, and is taken to the emergency department. While the client waits to be seen by the physician, what intervention should the nurse perform first? Apply a warm compresses to the injured shoulder. Ask him to demonstrate full range of motion of his left arm. Keep him in a comfortable position and apply ice to the injured shoulder. Give him a nonnarcotic analgesic for pain. 96
Answer: C Rationale: Ice would be applied first to reduce swelling and pain. The client should also be helped into a comfortable position. Warm compresses may increase swelling and cause bleeding into the injured tissue. Demonstrating full range of motion of the left arm may cause further damage the injured area. In the emergency department, the nurse must have a physician's order to administer an analgesic.
183. A child is receiving total parenteral nutrition (TPN). During TPN therapy, the most important nursing action is: a. assessing vital signs every 30 minutes. b. monitoring the blood glucose level closely. c. elevating the head of the bed 60 degrees d. providing a daily bath. Answer: B Rationale: Most TPN solutions contain a high glucose content, placing the client at risk for hyperglycemia. Therefore, the most important nursing action is to monitor the child's blood glucose level closely. A child receiving TPN isn't likely to require vital sign assessment every 30 minutes or elevation of the head of the bed. A daily bath isn't a priority.
184. A child, age 8, is immobilized with a hip spica cast. To minimize the child's feelings of isolation, the nurse should: a. let the child visit the playroom daily. b. sit with the child for an hour in the room. c. place a telephone in the child's room. d. arrange a visit by a cooperative child from the same unit. Answer: A
97
Rationale: School-age children need peer interaction and thrive on peer approval and acceptance. Allowing the child to visit the playroom daily provides a nonthreatening atmosphere for peer interaction and helps the child feel less isolated. Sitting with the child for an hour wouldn't foster the necessary peer interaction. Placing a telephone in the child's room would allow the child to communicate with family and friends but could reinforce feelings of isolation. Having another child visit would be appropriate only if the child is of the same age-group.
185. A 7-year-old boy is hospitalized with cystic fibrosis. To help him manage secretions and avoid respiratory distress, the nurse should: a. perform chest physiotherapy every 4 hours. b. give pancreatic enzymes as ordered. c. place the child in an oxygen tent and have oxygen administered continuously. d. serve a high-calorie diet. Answer: A Rationale: Chest physiotherapy aids in loosening secretions in the entire respiratory tract. Pancreatic enzymes aid in the absorption of necessary nutrients not in managing secretions. Oxygen therapy doesn't aid in loosening secretions and can cause carbon dioxide retention and respiratory distress in children with cystic fibrosis. A high-calorie diet is appropriate but doesn't facilitate respiratory effort.
186. The physician prescribes corticosteroids for a child with systemic lupus erythematosus (SLE). The nurse knows that the purpose of corticosteroid therapy for this child is to: a. combat inflammation. b. prevent infection. c. prevent platelet aggregation d. promote diuresis.
98
Answer: A Rationale: Corticosteroids are used to combat inflammation in a child with SLE. To prevent infection, the physician would prescribe antibiotics. Aspirin is used to prevent platelet aggregation. Diuretics aren't indicated in SLE.
187. An 8-year-old child enters a health care facility. During assessment, the nurse discovers that the child is experiencing the anxiety of separation from his parents. The nurse makes the nursing diagnosis of Fear related to separation from familiar environment and family. Which nursing intervention is most likely to help the child cope with fear and separation? a. Ask the parents not to visit the child until he is adjusted to the new environment. b. Ask the physician to explain to the child why he needs to stay in the health care facility. c. Explain to the child that he must act like an "adult" while he's in the facility. d. Explain to the child that he must act like an "adult" while he's in the facility. Answer: D Rationale: Allowing the parents to stay and participate in the child's care can provide support to both the parents and the child. The other interventions won't address the client's diagnosis and may exacerbate the problem. 188. child, age 9, is admitted to the emergency department with pain in the right lower abdominal quadrant, suggesting appendicitis. To further assess for pain associated with appendicitis, the nurse should examine which region? a. Left lower abdominal quadrant b. Right upper abdominal quadrant 99
c. Left upper abdominal quadrant d. Umbilical area Answer: D Rationale: In a child, pain that is diffuse or centered around the umbilicus may be associated with appendicitis. (However, the pain may localize later.) Pain in the left lower abdominal quadrant is associated with descending and sigmoid colon problems; in the right upper quadrant, with gallbladder disease; and in the left upper quadrant, with pancreatitis.
189. A 6-year-old child with a history of varicella and aspirin intake is brought to the emergency department. The nurse suspects Reye's syndrome. syndrome? a. Fever, decreased level of consciousness (LOC), and impaired liver function b. Joint inflammation, red macular rash with a clear center, and lowgrade fever c. Peripheral edema, fever for 5 or more days, and "strawberry tongue" d. Red, raised "bull's eye" rash, malaise, and joint pain Answer: A Rationale: Reye's syndrome occurs in children with a history of a viral infection, varicella, or influenza. It's often associated with the administration of aspirin. The child presents with fever and decreased LOC, which can lead to coma and death. As the disease progresses, the child also develops impaired liver function. A child with joint pain, a red macular rash with a clear center, and a low-grade fever probably has rheumatic fever. A child presenting with peripheral edema, fever for more than 5 days, and a "strawberry tongue" probably has Kawasaki disease. A child with a red, raised "bull's eye" rash, malaise, and joint pain should be tested for Lyme disease. 100 Which assessment findings are consistent with this
190. After a head injury, a child experiences enuresis, polydipsia, and weight loss. Based on these findings, the nurse should monitor closely for signs and symptoms of: a. hypercalcemia. b. hyperglycemia. c. hyponatremia. d. hypokalemia. Answer: D Rationale: Enuresis, polydipsia, and weight loss suggest diabetes insipidus, a disorder that may result from a head injury that damages the neurohypophyseal structures. Diabetes insipidus places the child at risk for fluid volume depletion and hypokalemia. It doesn't cause hypercalcemia, hyperglycemia, or hyponatremia.
191. A school-age child experiences symptoms of excessive polyphagia, polyuria, and weight loss. The physician diagnoses Type I diabetes mellitus and admits the child to the facility for insulin regulation. The physician prescribes an insulin regimen of insulin (Humulin R) and isophane insulin (Humulin N) administered subcutaneously. How soon after administration can the nurse expect the regular insulin to begin to act? a. to 1 hour b. 1 to 2 hours c. 4 to 8 hours d. 8 to 10 hours Answer: A Rationale: Regular insulin, a rapid-acting insulin, begins to act in to 1 hour, reaches peak concentration levels in 2 to 10 hours, and has a duration of action of 5 to 15 hours. 101
192. An 8-year-old child is suspected of having meningitis. Signs of meningitis include which of the following? a. Cullen's sign b. Koplick's spots c. Kernig's sign d. Chvostek's sign Answer: C Rationale: In Kernig's sign, the client is in the supine position with knees flexed; a leg is flexed then at the hip so that the thigh is brought to a position perpendicular to the trunk. An attempt is then made to extend the knee. If meningeal irritation is present, the knee can't be extended and attempts to extend the knee result in pain. Other common symptoms include stiff neck, headache, and fever. Cullen's sign is the bluish discoloration of the periumbilical skin due to intraperitoneal hemorrhage. Koplik's spots are reddened areas with grayish blue centers that are found on the buccal mucosa of a client with measles. Chvostek's sign is elicited by tapping the client's face lightly over the facial nerve, just below the temple. A calcium deficit is suggested if the facial muscles twitch.
193. The nurse is teaching parents how to reduce the spread of impetigo. The nurse should encourage parents to: a. teach children to cover mouths and noses when they sneeze. b. have their children immunized against impetigo. c. teach children the importance of proper hand washing. d. isolate the child with impetigo from other members of the family. Answer: C Rationale: The spread of childhood infections, including impetigo, can be reduced when children are taught proper hand-washing technique. 102
Because impetigo is spread through direct contact, covering the mouth and nose when sneezing won't prevent its spread. Currently, there is no vaccine to prevent a child from contracting impetigo. Isolating the child with impetigo is unnecessary.
194. A child is receiving chemotherapy for treatment of acute lymphoblastic leukemia. During discharge preparation, which topic is most important for the nurse to discuss with the child and parents? a. How to help the child adjust to an altered body image b. How to increase the child's interactions with peers c. The need to decrease the child's activity level d. Ways to prevent infection Answer: D Rationale: Because overwhelming infection is the most common cause of death in clients with leukemia, preventing infection is the most important teaching topic. Although promoting adjustment to an altered body image and increasing peer interactions are important, they don't address life-threatening concerns and therefore take lower priority. The nurse should advise the parents to let the child's desire and tolerance for activity determine the child's activity level.
195. The nurse formulates a nursing diagnosis of Risk for infection for a child with Down syndrome. Which condition typically seen in children with this syndrome supports this nursing diagnosis? a. Muscular hypotonicity b. Muscle spasticity c. Increased mucus viscosity d. Hypothyroidism Answer: A
103
Rationale: Several conditions make the child with Down syndrome highly vulnerable to respiratory infections. For example, the hypotonicity of chest muscles leads to diminished respiratory expansion and pooling of secretions, while an underdeveloped nasal bone impairs mucus drainage. Down syndrome isn't associated with muscle spasticity or increased mucus viscosity. Although hypothyroidism is common in children with Down syndrome, it doesn't increase the risk of infection.
196. Which of the following would be an effective relaxation strategy for a school-age child to use during a painful procedure? a. Having the child keep his eyes shut at all times b. Having the child hold his breath and not yell c. Having the child take a deep breath and blow it out until told to stop d. Being honest with the child and telling him the procedure will hurt a lot Answer: C Rationale: Having the child take a deep breath, then blow it out is a form of distraction and will help the child cope better with the procedure. A child may prefer to keep his eyes open during a procedure so he can see what is going on and can anticipate what is going to happen. Letting a child yell during a procedure is a form of distraction. Holding the breath isn't beneficial and could have adverse effects (such as feeling dizzy or faint). The nurse should prepare a child for a procedure by using nonpain descriptors and not suggesting pain. For example, the nurse might say, "Sometimes this feels like pushing or sticking, and sometimes it doesn't bother children at all."
197. When teaching the parent of a school-age child about signs and symptoms of fever that require immediate notification of the physician, which of the following descriptions should the nurse include? a. Burning or pain with urination 104
b. Complaints of a stiff neck c. Fever disappearing for longer than 24 hours, then returning d. History of febrile seizures Answer: B Rationale: A child with a fever and a stiff neck should be evaluated immediately for meningitis. All other symptoms should be addressed by the physician but can wait until office hours.
198. Which of the following should the nurse do first when admitting an 11-year-old in sickle cell crisis? a. Administer oral pain medication while obtaining the child's history. b. Begin I.V. fluids after obtaining the child's history. c. Instruct the parents about what to expect during this hospitalization. d. Start oxygen therapy as soon as the child's vital signs are taken. Answer: B Rationale: Fluids are one of the most important components of therapy for sickle cell crisis. Fluids help increase blood volume and prevent sickling and thrombosis. A child experiencing a sickle cell crisis often has severe pain requiring the use of I.V. analgesics such as morphine, which would be administered after fluid therapy has been started. Instructing the parents about what to expect during hospitalization is important but it isn't the first action the nurse should take. Oxygen therapy is used only if the child is hypoxic.
199. The parents of a child with cystic fibrosis ask the nurse why their child must receive supplemental pancreatic enzymes. Which response by the nurse would be most appropriate? a. "Pancreatic enzymes promote absorption of nutrients and fat." b. "Pancreatic enzymes promote adequate rest." 105
c. "Pancreatic enzymes prevent intestinal mucus accumulation." d. "Pancreatic enzymes help prevent meconium ileus." Answer: A Rationale: Pancreatic enzymes are given to a child with cystic fibrosis to aid fat and protein digestion. They don't promote rest or prevent mucus accumulation or meconium ileus.
200. A child, age 6, is about to be discharged after treatment for acute rheumatic fever. Which statement by the parents indicates effective discharge teaching? a. "We will keep our child in bed for at least a week." b. "We will give our child penicillin twice a day for 5 years." c. "We will measure our child's blood pressure every day." d. "We will keep giving our child corticosteroids." Answer: B Rationale: A child recovering from acute rheumatic fever must receive prophylactic penicillin for at least 5 years. Bed rest isn't indicated once the acute disease phase ends. Rheumatic fever doesn't call for blood pressure monitoring or corticosteroid therapy.
201. During chemotherapy, a boy, age 10, loses his appetite. When teaching the parents about his food intake, the nurse should include which instruction? a. "Offer dry toast and crackers." b. "Withhold all food and fluids." c. "Ignore your child's lack of food intake." d. "Let your child eat any food he wants." Answer: D
106
Rationale: The nurse should instruct the parents to let the child eat any food he wants because any form of intake is better than none. Dry crackers would be appropriate for a child experiencing nausea. Withholding all foods and fluids or ignoring lack of food intake would be inappropriate. 202. A school-age child has a fever, joint inflammation, and a nonpruritic rash. Knowing that these are signs of rheumatic fever, the nurse should ask the parents: a. "Has your child recently been exposed to other children with rheumatic fever?" b. Has your child had strep throat recently?" c. "Has your child had strep throat recently?" d. "Is your child's Haemophilus influenzae vaccine up to date?" Answer: B Rationale: Group A streptococcal infection typically precedes rheumatic fever. An inflammatory disease, rheumatic fever affects the heart, joints, and central nervous system. It isn't infectious and can't be transmitted from one person to another. Congenital heart defects don't play a role in the development of rheumatic fever. H. influenzae vaccine doesn't prevent streptococcal infection or rheumatic fever.
203. The school nurse is examining a student at an elementary school. Which of the following findings would lead the nurse to suspect impetigo? a. Small, red lesions on the trunk and in the skin folds b. A discrete pink-red maculopapular rash that starts on the head and progresses down the body c. Red spots with a blue base found on the buccal membranes d. Vesicular lesions that ooze, forming crusts on the face and extremities
107
Answer: D Rationale: Impetigo starts as papulovesicular lesions surrounded by redness. The lesions become purulent and begin to ooze, forming crusts. Impetigo occurs most often on the face and extremities. Small red lesions on the trunk and in the skin folds are characteristic of scarlet fever. A discrete pink-red maculopapular rash that starts on the face and progresses down to the trunk and extremities is characteristic of rubella (German measles). Red spots with a blue base found on the buccal membranes, known as Koplik's spots, are characteristic of measles (rubeola).
204. The nurse is caring for an 8-year-old with acute asthma exacerbation. Which of the following would be of greatest concern to the nurse? a. The child's respiratory rate is now 24 breaths/minute. b. Recent blood gas analysis indicates an oxygen saturation of 95% c. Before a respiratory therapy treatment, wheezing isn't heard on auscultation. d. The child's mother reports that the child sometimes forgets to take the inhalers. Answer: C Rationale: Typically, before a respiratory therapy treatment, wheezing has increased and the client has increased respiratory distress. No wheezing on auscultation is an indication that the child isn't moving air in and out and is in respiratory distress. A respiratory rate of 24 breaths/minute in an 8-year-old is normal. An oxygen saturation of 95% is somewhat of a concern, possibly indicating that the client needs oxygen or needs to clear the airways. The fact that the mother makes the 8-year-old responsible for taking medications is of concern and needs to be investigated but this isn't as important at this time as the lack of wheezing.
108
205. A child, age 6, is brought to the health clinic for a routine checkup. To assess the child's vision, the nurse should ask: a. "Do you have any problems seeing different colors?" b. "Do you have trouble seeing at night?" c. "Do you have problems with glare?" d. "How are you doing in school?" Answer: D Rationale: A child's poor progress in school may indicate a visual disturbance. The other options are more appropriate questions to ask when assessing vision in a geriatric client.
206. A child, age 8, complains of leg pain shortly after being admitted with a fractured tibia sustained in a fall. The most effective way for the nurse to assess the severity of the pain is to: a. ask the child what makes the leg feel better. b. ask the child what the pain feels like. c. ask the child what makes the leg feel worse. d. ask the child to rate the pain on a scale of 1 to 10. Answer: D Rationale: Although all four options describe methods that would help the nurse assess the child's pain, having the child rate the pain on a scale of 1 to 10 is the most effective way to assess pain severity because it quantifies the pain objectively.
207. A child, age 10, is hospitalized for treatment of acute osteomyelitis. After assessing swelling and tenderness of the left tibia, the nurse initiates antibiotic therapy as prescribed. The child's left leg is immobilized in a splint. What is an appropriate expected outcome for this child? a. "The client will change position with minimal discomfort." 109
b. "The client will bear weight on the affected limb." c. "The client will ambulate with crutches." d. "The client will participate in age-appropriate activities." Answer: A Rationale: To prevent pressure sores, the child must turn and change positions periodically. However, during the acute phase of osteomyelitis, moving the affected leg may cause extreme pain and discomfort. Therefore, the nurse must support and handle the leg gently during turning and repositioning. Weight bearing is contraindicated because it may cause pathologic fractures. Ambulating with crutches is an inappropriate outcome because the child is restricted to bed rest and the affected leg is immobilized to limit the spread of infection. Participation in age-appropriate activities isn't a realistic outcome because an acutely ill child isn't likely to be interested in activities; this outcome would be suitable after the acute disease phase ends.
208. After a child has a cardiopulmonary arrest, which of the following drugs would the nurse expect to administer during the initial phase of treatment? a. dopamine b. epinephrine c. sodium bicarbonate d. atropine Answer: A Rationale: After successful resuscitation, dopamine would be given as an infusion to increase cardiac output and maintain blood pressure. Epinephrine, sodium bicarbonate, and atropine are first-round drugs in a cardiopulmonary arrest.
110
209. The physician orders an antibiotic for a child, age 6, who has an upper respiratory infection. To avoid tooth discoloration, the nurse expects the physician to avoid prescribing which drug? a. penicillin b. erythromycin c. tetracycline d. amoxicillin Answer: C Rationale: Tetracycline should be avoided in children under age 8 because it may cause enamel hypoplasia and permanent yellowish gray to brownish tooth discoloration. Penicillin, erythromycin, and amoxicillin don't discolor the teeth.
210. When performing a physical assessment on a girl, age 10, the nurse keeps in mind that the first sign of sexual maturity in girls is: a. breast bud development. b. pubic hair. c. axillary hair. d. menarche. Answer: A Rationale: Breast bud development elevation of the nipple and areola to form a breast bud is the first sign of sexual maturity in girls. Sexual maturation continues with the appearance of pubic hair, axillary hair, and menarche, consecutively.
211. The nurse is taking a history from the parents of a 11-year-old girl admitted with Reye's syndrome. Which illness would the nurse expect the parents to report their child having the previous week? a. Chickenpox 111
b. Bacterial meningitis c. Strep throat d. Lyme disease Answer: A Rationale: Reye's syndrome commonly occurs about 1 week after a child has had a viral infection, such as chickenpox (varicella) or influenza. Children with flulike symptoms or chickenpox who receive aspirin are at increased risk for Reye's syndrome. Bacterial meningitis and strep throat are caused by bacteria and don't lead to Reye's syndrome. Lyme disease is caused by a spirochete and isn't implicated in Reye's syndrome.
212. Parents of a 6-year-old tell a physician that the child has been having periods of unawareness with short periods of staring. Based on his history, the child is probably having which type of seizure? a. Complex partial b. Myoclonic c. Typical absence d. Tonic Answer: C Rationale: A typical absence seizure has an onset between ages 4 and 8. It's exhibited by an abrupt loss of consciousness, amnesia, or unawareness characterized by staring and a 3-cycle/second spike and waveform on an EEG. The attack lasts from 10 to 30 seconds and may occur as frequently as 50 to 100 times a day. No postictal or confused state follows the attack. A complex partial seizure most commonly occurs in older children and adults, causing a brief impairment of consciousness. A myoclonic seizure occurs in older children and is exhibited by lightning jerks without loss of consciousness. An abrupt increase in muscle tone, loss of consciousness, and marked autonomic signs and symptoms characterize the tonic seizure.
112
213. In the family of a 7-year-old child with a chronic illness, which of the following family members feel jealous, resentment, embarrassment, shame, fear of becoming ill, and guilt at causing the illness? a. Siblings b. Parents c. Child with the illness d. Grandparents Answer: A Rationale: When a brother or sister is ill, siblings frequently experience jealousy and resentment of the increased attention given to the ill child, embarrassment and shame, fear of becoming ill, and guilt at causing the illness. Parents may experience grieving, denial, overprotectiveness, rejection, and overcompensation. The ill child may regress to a previous developmental stage and feel anxiety, depression, and anger. Both the child's and the siblings' reactions are influenced by the parents' response. Grandparents may experience ambivalence, disappointment, and grief.
214.
Craniocerebral
injury
in
child
differs
substantially
from
craniocerebral trauma in an adult. Which of the following identifies a negative difference between children and adults that could produce a life-threatening complication for a child? a. Cerebral tissues in children are softer, thinner, and more flexible. b. A child's skull can expand more than an adult's can. c. Greater portions of a child's blood volume flows to the head. d. Hematomas in children can include subdural, epidural, and intracerebral. Answer: C Rationale: If hemorrhage is associated with a head injury and it goes undetected, a child may experience hypovolemic shock because a large portion of a child's blood volume goes to the head. In children, cerebral tissues are softer, thinner, and more flexible conditions that permit 113
diffusion of the impact. Because a child's skull can expand more than an adult's can, a greater amount of posttraumatic edema can occur without evidence of neurologic deficits. Subdural, epidural, and intracerebral hematomas are the different types of head injury that can occur in children and adults.
215. According to Erikson's theory of development, chronic illness can interfere with which stage of development in an 11-year-old? a. Intimacy versus isolation b. Trust versus mistrust c. Industry versus inferiority d. Identity versus role confusion Answer: C Rationale: According to Erikson, an 11-year-old is working through the stage of industry versus inferiority. Chronic illness may interfere with this stage of development in an 11-year-old child. Intimacy is the developmental task of a young adult. Trust is the developmental task to be achieved during infancy. Identity is the developmental task of adolescence.
216. Where should the nurse instill an ophthalmic medication in a 6year-old child? a. The sclera b. The lower conjunctival sac c. The upper conjunctival sac d. The outer canthus Answer: B Rationale: Ophthalmic sac, or outer canthus. 114 medication is best instilled in the lower
conjunctival sac. Eyedrops are instilled in the sclera, upper conjunctival
217. When teaching school-age children important injury prevention strategies, the nurse must use creativity to gain cooperation because children tend not to comply with which of the following? a. Wearing safety apparel (helmets, knee pads, elbow pads) b. Learning to swim c. Saying "no" when offered illegal or dangerous drugs d. Learning "stranger danger" Answer: A Rationale: School-age children are subject to peer pressure, and they would rather not participate in a sport if they must wear safety apparel that provokes taunts from peers. Therefore, the nurse should discuss stylishness, comfort, and social acceptance because these are major determinants of compliance. School-age children like to swim and may work hard to perfect that skill. This age-group will usually listen to reasons for not taking illegal drugs and will adhere to group rules for not tolerating drug use. Regarding stranger danger, this age-group simply needs to be reminded of potential dangers.
218. In the parents of a chronically ill child, which behavior may indicate feelings of guilt about the child's illness? a. Anger b. Sadness c. Shock d. Overindulgence Answer: D Rationale: Parents who feel guilty about a child's illness may
overindulge the child. Anger, sadness, and shock are common in parents of chronically ill children but don't necessarily indicate feelings of guilt.
115
219. A 10-year-old diagnosed with acute glomerulonephritis is admitted to the pediatric unit. The nurse should ensure that which of the following is a part of the child's care? a. Taking vital signs every 4 hours and obtaining daily weight b. Obtaining a blood sample for electrolyte analysis every morning c. Checking every urine specimen for protein and specific gravity d. Ensuring that the child has accurate intake and output and eats a high-protein diet Answer: A Rationale: Because major complications such as hypertensive encephalopathy, acute renal failure, and cardiac decompensation can occur, monitoring vital signs (including blood pressure) is an important measure for a child with acute glomerulonephritis. Obtaining daily weight and monitoring intake and output also provide evidence of the child's fluid balance status. Sodium and water restrictions may be ordered depending on the severity of the edema and the extent of impaired renal function. Typically, protein intake remains normal for the child's age and is only increased if the child is losing large amounts of protein in the urine. Checking urine specimens for protein and specific gravity and daily monitoring of serum electrolyte levels may be done, but their frequency is determined by the child's status. These are less important nursing measures in this situation.
220. The nurse is developing a plan of care for a 10-year-old child who has recently been diagnosed with diabetes mellitus. Which of the following would be inappropriate to include in a teaching plan focusing on proper hygiene? a. Encourage regular dental care. b. Teach blood glucose monitoring. c. Teach care of cuts and scratches. d. Teach proper foot care. Answer: B 116
Rationale: Teaching blood glucose monitoring and the use of equipment is necessary in diabetic teaching within the plan of care that focuses on demonstrating testing blood glucose levels. Encouraging regular dental care is important for the child's general health. Teaching proper care of cuts and scratches will minimize the risk of infection. Teaching proper foot care is necessary and becomes a priority when the child becomes an adult.
221. A school-age child is being discharged with a diagnosis of rheumatic fever. Which of the following should be included in the teaching plan for the family? a. The child should stay on penicillin and return for a follow-up appointment. b. At home, be sure to keep the child on bed rest. c. All children with rheumatic fever need monthly blood tests. d. The child should stay out of school until the source of the infection is determined. Answer: A Rationale: A child with rheumatic fever, which is caused by group A beta-hemolytic streptococci, should stay on penicillin either oral daily or a monthly injection to prevent a recurrence. A follow-up appointment is needed to determine how the child is responding to treatment. Neither bed rest nor monthly blood tests will be prescribed for all children. Rheumatic fever is caused by group A beta-hemolytic streptococci, so the source of the infection is already known.
222. A 10-year-old child is in the hospital for the first time. The nurse has provided support and teaching to help the family and child adjust and to reduce their anxiety related to the child's hospitalization. Which of the following would the nurse view as unexpected? a. The parents relate readily with the staff and calmly with the child. 117
b. The child accepts and responds positively to comforting measures. c. The child discusses procedures and activities without evidence of anxiety. d. The parents choose to leave to let the child build a relationship with the staff. Answer: D Rationale: The parents of an adolescent might leave to help the teen maintain a fragile identity, but a 10-year-old would prefer to have his parents with him. Expected outcomes for a child and parents new to the hospital would include the parents' relating readily to the staff and calmly with the child, the child's accepting and responding positively to comforting measures, and the child's discussing procedures and activities without evidence of anxiety.
223. The nurse is caring for a 10-year-old child with cystic fibrosis. The child's parents tell the nurse that they're having difficulty coping with their child's disease. Which actionwouldn't be appropriate for the nurse to take? a. Helping the child and family obtain necessary equipment, supplies, and medication b. Pointing out to the parents ways in which they might have done things differently c. Providing referrals to local community agencies and the Cystic Fibrosis Foundation d. Encouraging the parents to allow their child to follow as normal a childhood as possible Answer: B Rationale: The nurse should avoid being critical when talking with parents about how they have handled their child's disease or condition. The nurse can help this family by assisting them with finding appropriate financial, psychological, and social support. Providing referrals to the local community agencies and the Cystic Fibrosis Foundation is also an 118
appropriate intervention. The child should be treated as much like a normal child as possible.
224. A disabled school-age child whose parents are overprotective might display which of the following sets of characteristics? a. Dependency, fearfulness, and lack of outside interests b. Extreme independence, defiance, and a high level of risk taking c. Shyness and loneliness d. Pride and confidence in one's ability to cope Answer: A Rationale: Disabled children whose parents are overprotective tend to have marked dependency, fearfulness, inactivity, and lack of outside interests. Children who are raised by oversolicitous and guilt-ridden parents are often overly independent, defiant, and high-risk takers. Children who are reared by parents who emphasize the child's deficits and tend to isolate the child may appear shy and lonely. Children who are reared by parents who establish reasonable limits have pride and confidence in their ability to cope successfully.
225. The nurse is caring for a 10-year-old child with rheumatic fever. While obtaining the child's health history from the mother, the nurse should ask if the child recently had which illness? a. Strep throat b. Influenza c. Chickenpox d. Mononucleosis Answer: A Rationale: Rheumatic fever often follows an infection with group A betahemolytic streptococcus, as in strep throat, impetigo, scarlet fever, or pharyngitis. Influenza, chickenpox, and mononucleosis are caused by viruses and don't lead to rheumatic fever. 119
226. The mother of several young children calls the nurse when her school-age child comes down with chickenpox. The nurse provides instruction on communicability and home management of this disease. Which response by the mother indicates effective teaching? a. "I should keep my child at home until the fever is gone." b. "I should have my child soak in oatmeal baths twice daily." c. "I should give my child aspirin every 4 hours until the fever is gone." d. "I should start checking my other children for lesions in about 4 weeks." Answer: B Rationale: Chickenpox is characterized by pruritic lesions; colloidal oatmeal baths may soothe the skin and relieve itching. A fever is common during the first 24 hours. However, the communicable period extends beyond the febrile stage and a normal temperature shouldn't be used as the basis for letting the child leave home. Chickenpox is communicable from 1 day before the lesions erupt until they dry approximately 1 week. The child should stay home during this time to prevent disease transmission. Aspirin isn't recommended because it's associated with Reye's syndrome; acetaminophen is a suitable substitute. The incubation period for chickenpox is 2 to 3 weeks; the mother should begin to check the other children for lesions 2 weeks after exposure to the infected child.
227. A 13-year-old may have appendicitis. Which of the following symptoms would help determine the child's condition? a. The severity, location, and movement of pain b. The degree of fever c. A history of vomiting and diarrhea, if present d. A history of irritability and lethargy
120
Answer: A Rationale: The pattern of pain is a reliable indicator of acute appendicitis. It begins with a severe colicky abdominal pain that gets progressively worse. The pain starts in the midabdominal (periumbilical) region and moves to the right lower quadrant after 6 to 12 hours. The degree of fever, a history of vomiting and diarrhea, and a history of irritability and lethargy are all clinical manifestations of acute appendicitis; however, these conditions can also be present in a number of other childhood illnesses.
228. The parents of an adolescent girl have recently learned that their daughter has a terminal illness. At first, as they try to cope, they display avoidance behaviors. Then they demonstrate behaviors that indicate possible acceptance of the diagnosis. Which of the following behaviors would indicate acceptance? a. Failure to recognize the seriousness of the child's condition despite physical evidence b. Intellectualization about the illness in areas unrelated to the child's condition c. Expression of feelings, such as sorrow and anger, about the child's condition d. Avoidance of staff, family members, or the child Answer: C Rationale: The ability to express feelings and relate them to the diagnosis is the first step in accepting the situation. Failing to recognize the seriousness of the child's condition despite physical evidence, intellectualizing about the illness in areas unrelated to child's condition, and avoiding staff, family members, or the child are all avoidance behaviors that represent a parent's inability to cope with the situation.
229. The nurse is interviewing a 16-year-old female at a clinic. It's her first visit and she says that she has been exposed to herpes by her 121
boyfriend. Initially, with primary genital or Type 2 herpes simplex, the nurse would expect the client to have: a. dysuria and urine retention. b. perineal ulcers and erosions. c. bilateral inguinal lymphadenopathy. d. burning or tingling on vulva, perineum, or vagina. Answer: D Rationale: Burning and tingling genital discomfort is the most common initial finding. This symptom will advance to vesicular lesions rupturing into ulcerations, which then dry into a crusty erosion. The client may also experience fever, headache, malaise, myalgia, regional lymphadenopathy, and dysuria.
230. A child, age 14, is diagnosed with scoliosis and scheduled for brace application. The mother asks the nurse how long her child will have to wear the brace. What is the nurse's best response? a. "About 6 to 8 weeks." b. "About 6 months." c. "About 2 to 4 years." d. "About 4 to 7 years." Answer: D Rationale: Most children with scoliosis must wear a brace until the spine matures typically between ages 18 and 21. Therefore, this 14-yearold child will need to wear the brace for 4 to 7 years.
231. To establish a good interview relationship with an adolescent, which of the following strategies is most appropriate? a. Asking personal questions unrelated to the situation b. Writing down everything the teen says 122
c. Asking open-ended questions d. Discussing the nurse's own thoughts and feelings about the situation Answer: C Rationale: Open-ended questions allow the teen to share information and feelings. Asking personal questions not related to the situation jeopardizes the trust that must be established because the adolescent may feel as though he's being probed with unnecessary questions. Writing everything down during the interview can be a distraction and won't allow the nurse to observe how the adolescent behaves. Discussing the nurse's thoughts and feelings may bias the assessment and is inappropriate when interviewing any client. 232. During chemotherapy for lymphoma, a child, age 15, is at risk for stomatitis. Which statement by the child supports a nursing diagnosis of Deficient knowledge related to mouth care? a. "I use a soft toothbrush to clean my teeth." b. "I remove white patches on my tongue and cheeks with my toothbrush." c. "I rinse my mouth every 2 to 4 hours with a solution of baking soda and water." d. "I don't use bottled mouthwashes." Answer: B Rationale: White patches on the tongue and oral mucosa indicate infection; the client should report, not remove, them. The child should use a soft toothbrush to prevent injury to the fragile oral mucosa. To prevent stomatitis, the child should rinse the mouth every 2 to 4 hours with a nonirritating solution, such as baking soda and water or normal saline solution, and should avoid commercial mouthwashes containing alcohol, which may dry the oral mucosa.
123
234. The nurse is performing a psychosocial assessment on an adolescent, age 14. Which emotional response is typical during early adolescence? a. Frequent anger b. Cooperativeness c. Moodiness d. Combativeness Answer: C Rationale: During early adolescence, a child may become moody. Frequent anger and combativeness are more typical of middle adolescence. Cooperativeness typically occurs during late adolescence.
235. The nurse is assigned to an adolescent. Which nursing diagnosis is most appropriate for a hospitalized adolescent? a. Anxiety related to separation from parents b. Fear related to the unknown c. Fear related to altered body image d. Ineffective individual coping related to activity restrictions Answer: C Rationale: Fear related to altered body image is the most appropriate nursing diagnosis for a hospitalized adolescent because of the adolescent's developmental level and concern for physical appearance. An adolescent may fear disfigurement resulting from procedures and treatments. Separation is rarely a major stressor for the adolescent, eliminating a diagnosis of Anxiety related to separation from parents. Adolescents may have Fear related to the unknown but typically ask questions if they want information. A diagnosis of Ineffective individual coping related to activity restrictions may be appropriate for a toddler who has difficulty tolerating activity restrictions but is an unlikely nursing diagnosis for an adolescent.
124
236. After assessing an adolescent with sickle cell anemia, the nurse formulates a nursing diagnosis of Impaired skin integrity. Which assessment finding best supports this nursing diagnosis? a. Swelling of the hands and feet b. Petechiae c. Leg ulcers d. Hemangiomas Answer: C Rationale: In sickle cell anemia, sickling of red blood cells leads to increased blood viscosity and impaired circulation. Diminished peripheral circulation makes the adolescent or adult with sickle cell anemia susceptible to chronic leg ulcers. In children under age 2 who have sickle cell anemia, swelling of the hands and feet (hand-foot syndrome) commonly occurs during a vaso-occlusive crisis as a result of infarction of short tubular bones. Petechiae aren't associated specifically with sickle cell anemia. Hemangiomas, benign tumors of dilated blood vessels, aren't linked to sickle cell anemia.
237. An adolescent, age 16, is brought to the clinic for evaluation for a suspected eating disorder. To best assess the effects of role and relationship patterns on the child's nutritional intake, the nurse should ask: a. "What activities do you engage in during the day?" b. "Do you have any allergies to foods?" c. "Do you like yourself physically?" d. "What kinds of foods do you like to eat?" Answer: C Rationale: Role and relationship patterns focus on body image and the client's relationship with others, which commonly interrelate with food intake. Questions about activities and food preferences elicit information 125
about health promotion and health protection behaviors. Questions about food allergies elicit information about health and illness patterns.
238. A child is admitted for treatment of bulimia nervosa. When developing the plan of care, the nurse anticipates including interventions that address which metabolic disorder? a. Hypoglycemia b. Metabolic alkalosis c. Metabolic acidosis d. Hyperkalemia Answer: B Rationale: In a client with bulimia nervosa, metabolic alkalosis may occur secondary to hydrogen loss caused by frequent, self-induced vomiting. Typically, the blood glucose level is within normal limits, making hypoglycemia unlikely. In bulimia nervosa, hypokalemia is more common than hyperkalemia and typically results from potassium loss related to frequent vomiting.
239. The nurse is caring for a teenage client involved in a motor vehicle accident. The client has a chest tube in place. If the chest tube is accidentally removed, the nurse should immediately: a. reintroduce the tube and attach it to water seal drainage. b. call the physician and obtain a chest tray. c. cover the opening with petroleum gauze. d. clean the wound with povidone-iodine and apply a gauze dressing. Answer: C Rationale: If a chest tube is accidentally removed, the nurse should cover the insertion site with sterile petroleum gauze. The nurse should then observe the client for respiratory distress, as tension pneumothorax may develop. If so, the nurse should remove the gauze to allow air to escape. The nurse shouldn't reintroduce the tube. Rather, 126
the nurse should have another staff member call a physician so another tube can be introduced by the physician under sterile conditions.
240. Which of the following parameters would not be an appropriate indicator of pain relief in an adolescent? a. Intermittent sleeping b. Change in behavior c. Statement of decreased pain d. Change in vital signs Answer: A Rationale: Sleeping isn't a reliable indicator of pain relief because the teen may use sleep as a coping mechanism. Positive changes in behavior and vital signs and a statement of less pain are indicators of an effective response to pain medication.
241. According to Erikson, the psychosocial task of adolescence is the development of a sense of identity. The nurse can best promote the development of a hospitalized adolescent by: a. emphasizing the need to follow the facility regimen. b. allowing parents and siblings to visit frequently. c. arranging for tutoring in school work. d. encouraging peer visitation. Answer: D Rationale: Peer visitation gives the adolescent an opportunity to continue along the path toward independence and identity. Knowledge of the facility regimen prepares the adolescent for upcoming procedures but doesn't affect development. To achieve a sense of identity, the adolescent must gain independence from the family; in contrast, parent and sibling visits tend to encourage dependence on the family. Tutoring
127
may help maintain a positive self-image relative to schoolwork but doesn't affect development.
242. A girl, age 15, is brought to the pediatrician's office by her mother, who's concerned about her daughter's dramatic weight loss over the past 2 months. The nurse suspects that the child has anorexia nervosa. Besides weight loss, nursing assessment of this client is likely to reveal: a. insomnia. b. dysphagia. c. diarrhea. d. amenorrhea. Answer: D Rationale: Amenorrhea is common in girls and women with anorexia nervosa; researchers don't know whether it results from starvation or an underlying metabolic disturbance. Insomnia isn't associated with anorexia nervosa. Clients with anorexia nervosa are capable of eating and rarely have dysphagia (difficulty swallowing). Anorexia nervosa is more likely to cause constipation than diarrhea because limited oral intake decreases GI motility.
243. When caring for an adolescent who's at risk for injury related to intracranial pathology, which of the following actions would maintain stable intracranial pressure (ICP)? a. Turn the client's head from side to side frequently. b. Keep the head in midline position while raising the head of the bed 15 to 30 degrees. c. Hyperextend the client's head with a blanket roll. d. Suction frequently to maintain a clear airway. Answer: B
128
Rationale: Elevating the head of the bed while keeping the client's head in midline position will facilitate venous drainage and avoid jugular compression. Turning the head, hyperextending the neck, and suctioning will increase ICP. 244. A 14-year-old client reports right lower quadrant pain, nausea, vomiting, and a low-grade fever for the past 12 hours. A physical examination reveals rebound tenderness and a positive psoas sign. Based on these findings, what would the nurse suspect? a. Appendicitis b. Pancreatitis c. Cholecystitis d. Constipation Answer: A Rationale: Right lower quadrant pain, rebound tenderness, nausea, vomiting, a positive psoas sign, and a low-grade fever are findings consistent with acute appendicitis. The other disorders may mimic appendicitis; however, the pain of pancreatitis is usually localized in the left upper quadrant. Cholecystitis is associated with right upper quadrant pain. Constipation wouldn't cause a fever.
245. A teenager is brought to the facility by friends after accidentally ingesting gasoline while siphoning it from a car. Based on the nurse's knowledge of petroleum distillates, which system should be the priority assessment? a. GI system b. Respiratory system c. Neurologic system d. Cardiovascular system Answer: B
129
Rationale: The primary concern with petroleum distillate ingestion is its effect on the respiratory system. Aspiration or absorption of petroleum distillates can cause severe chemical pneumonitis and impaired gas exchange. The GI, neurologic, and cardiovascular systems may also be affected if the petroleum contains additives such as pesticides.
246. The nurse is caring for an adolescent client who underwent surgery for a perforated appendix. When caring for this client, the nurse should keep in mind that the main life-stage task for an adolescent is to: a. resolve conflict with parents. b. develop an identity and independence. c. develop trust. d. plan for the future. Answer: B Rationale: The adolescent strives for a sense of independence and identity. During this time, conflicts are heightened, not resolved. Trust begins to develop during infancy and matures along with development. Adolescents rarely finalize plans for the future; this normally happens later in adulthood.
247. A child, age 14, is hospitalized for nutritional management and drug therapy after experiencing an acute episode of ulcerative colitis. Which nursing intervention would be appropriate? a. Administering digestive enzymes before meals as prescribed b. Providing small, frequent meals c. Administering antibiotics with meals as prescribed d. Providing high-fiber snacks Answer: B Rationale: Clients with ulcerative colitis, an inflammatory bowel disorder (IBD), tolerate small, frequent meals better than a few large meals daily. 130
Eating large amounts of food may exacerbate the abdominal distention, cramps, and nausea typically caused by IBD. Frequent meals also provide the additional calories needed to restore nutritional balance. This client doesn't lack digestive enzymes and therefore doesn't need enzyme supplementation. Antibiotics are contraindicated because they may interfere with the actions of other prescribed drugs and because ulcerative colitis isn't caused by bacteria. High-fiber foods may irritate the bowel further. 248. During a health teaching session, a student, age 14, asks the school nurse the reason for using underarm deodorant. The nurse should base the response on which physiologic change occurring during adolescence? a. An increase in adipose tissue distribution, which boosts sweat production b. The apocrine sweat glands reaching secretory capacity c. The eccrine sweat glands becoming fully functional d. The sebaceous glands becoming highly active Answer: B Rationale: The apocrine sweat glands grow in conjunction with hair follicles in the underarm areas; during adolescence, they reach their secretory capacity. Although adipose tissue increases during adolescence, this isn't associated with sweat production. The eccrine sweat glands, distributed over the entire body, aren't associated with pubertal physiologic changes. The sebaceous glands contribute to acne, not sweat production. 249. A child, age 13, is being evaluated for possible Crohn's disease. The nurse expects to prepare the child for which diagnostic study? a. Genetic testing b. Cystoscopy c. Myelography d. Sigmoidoscopy
131
Answer: D Rationale: Crohn's disease is an inflammatory bowel disorder
characterized by inflammation, ulceration, and edema of the bowel wall (typically involving the terminal ileum). Sigmoidoscopy and biopsy are the primary procedures used to establish the diagnosis; a barium enema also may be indicated. Although genetics may play a role in Crohn's disease, genetic testing isn't part of the diagnostic workup. Cystoscopy visualizes the bladder and urinary tract and isn't indicated for this client. Myelography is a radiographic procedure used to evaluate the spinal cord.
250. The nurse is caring for a 16-year-old female client who isn't sexually active. The client asks if she needs a Papanicolaou (Pap) test. The nurse should reply: a. yes, she should have a Pap test after the onset of menstruation. b. no because she isn't sexually active. c. yes because she's 16 years old. d. no because she isn't 21 years old. Answer: B Rationale: A 16-year-old who isn't sexually active doesn't need a Pap test. When a client is sexually active or reaches age 18, a Pap test should be performed.
132
Vous aimerez peut-être aussi
- Situation: Intrapartal Nursing Care 1. in The Delivery Room, Mrs.Document183 pagesSituation: Intrapartal Nursing Care 1. in The Delivery Room, Mrs.ederliza75% (4)
- Community Health Nursing and Care of The Mother and ChildDocument22 pagesCommunity Health Nursing and Care of The Mother and ChildMitz MagtotoPas encore d'évaluation
- Finals Part 1 (G&D)Document7 pagesFinals Part 1 (G&D)RandyPas encore d'évaluation
- MCN Exam Gestational ConditionsDocument9 pagesMCN Exam Gestational ConditionsEdith Cabrera Cabigas - SabalboroPas encore d'évaluation
- Nclex Questions - Pediatric NursingDocument8 pagesNclex Questions - Pediatric NursingAngelique Ramos PascuaPas encore d'évaluation
- Maternal and Child HealthDocument72 pagesMaternal and Child Healthannamargie07100% (3)
- MCN Test BankDocument10 pagesMCN Test BankMho Pimentel Vanguardia100% (1)
- Funda ExamDocument18 pagesFunda Examronnax100% (2)
- Gynecology Test QuestionsDocument6 pagesGynecology Test Questionsdhodejun lizhaldePas encore d'évaluation
- Funda Prof - Ad LMR AnswersDocument35 pagesFunda Prof - Ad LMR AnswersFreeNursingNotesPas encore d'évaluation
- Ob 1Document13 pagesOb 1iandame100% (1)
- NURSING PRACTICE 3 Edited AnswerkeyDocument9 pagesNURSING PRACTICE 3 Edited Answerkeykim_liñanPas encore d'évaluation
- OB Power Point Presentation 002Document57 pagesOB Power Point Presentation 002RitamariaPas encore d'évaluation
- Quiz 2 Obstetrics Nursing: Untitled SectionDocument11 pagesQuiz 2 Obstetrics Nursing: Untitled SectionBeverly DatuPas encore d'évaluation
- Maternal ReviewerDocument15 pagesMaternal ReviewerIvy DG100% (2)
- Manage Childhood Cough, Colds and DiarrheaDocument87 pagesManage Childhood Cough, Colds and Diarrheabibs_caigas3744100% (1)
- MCN Post Test IDocument15 pagesMCN Post Test Iquidditch07Pas encore d'évaluation
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument23 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralPas encore d'évaluation
- SEO-Optimized Title for Postpartum Nursing QuestionsDocument6 pagesSEO-Optimized Title for Postpartum Nursing QuestionsCharles Malcolm Dalugdug100% (1)
- 100 Item Obstetrics-Maternal and Child Health Nursing ExaminationDocument50 pages100 Item Obstetrics-Maternal and Child Health Nursing ExaminationMaria Ibarrola100% (1)
- NP1 Family Nursing 3Document2 pagesNP1 Family Nursing 3Jonas Marvin AnaquePas encore d'évaluation
- NP2Document12 pagesNP2mhamaenphapa27100% (1)
- Sec. 3C - 1 - OB Questions (Answer Key) - BrendaDocument20 pagesSec. 3C - 1 - OB Questions (Answer Key) - Brendacididok84Pas encore d'évaluation
- Maternal and Child Healthe Nursing MCQ 6Document18 pagesMaternal and Child Healthe Nursing MCQ 6shanika100% (1)
- Silvestri001100Document55 pagesSilvestri001100lilchibabyPas encore d'évaluation
- Maternal and Child NCLEX Questions Part2Document4 pagesMaternal and Child NCLEX Questions Part2Shengxy Ferrer100% (1)
- Pfinal Pedia With AnswerDocument5 pagesPfinal Pedia With AnswerplmokjniPas encore d'évaluation
- Pediatrics Ratio PresentationDocument112 pagesPediatrics Ratio PresentationRobert John SaronaPas encore d'évaluation
- Pediatric NursingDocument3 pagesPediatric Nursingjegel23100% (1)
- PNLE NCLEX Practice Exam For Maternal and Child Health Nursing 2Document5 pagesPNLE NCLEX Practice Exam For Maternal and Child Health Nursing 2bobtaguba100% (1)
- Compre - Maternal Answer KeyDocument8 pagesCompre - Maternal Answer KeyrabsibalaPas encore d'évaluation
- CHN Questions ImciDocument5 pagesCHN Questions Imciredskie08100% (6)
- Post-Partum Review Questions - Handout 2 With Answers /rationalesDocument9 pagesPost-Partum Review Questions - Handout 2 With Answers /rationalesnkuligowski100% (2)
- Local Nursing Licensure ExamDocument14 pagesLocal Nursing Licensure Examnikko042790Pas encore d'évaluation
- IMCIDocument148 pagesIMCILloyd Rafael EstabilloPas encore d'évaluation
- PNLE III For Care of Clients With Physiologic and Psychosocial Alterations (Part 1) 100 ItemaDocument30 pagesPNLE III For Care of Clients With Physiologic and Psychosocial Alterations (Part 1) 100 ItemaIk-ik Miral100% (1)
- Community Health NursingDocument43 pagesCommunity Health NursingNina Oaip100% (2)
- Nursing Exam Questions 2023 Part 1Document4 pagesNursing Exam Questions 2023 Part 1Lejo Sunny100% (1)
- CHILD HEALTH NCLEX QUESTIONSDocument42 pagesCHILD HEALTH NCLEX QUESTIONSEllen AngelPas encore d'évaluation
- Pedia Nursing - QuestionsDocument10 pagesPedia Nursing - Questionssinayawan001Pas encore d'évaluation
- Practice Test Maternity-Nsg 100 ItemsDocument21 pagesPractice Test Maternity-Nsg 100 ItemsPaul Christian P. Santos, RN100% (21)
- Maternal Child Nursing Exam ReviewDocument14 pagesMaternal Child Nursing Exam Reviewjames_manuel11187084100% (1)
- Obstetric Sample Questions With RationaleDocument31 pagesObstetric Sample Questions With RationaleTomzki Cornelio50% (2)
- MS ExamDocument7 pagesMS Examjosephine100% (2)
- Positioning QuestionsDocument5 pagesPositioning QuestionsShara SampangPas encore d'évaluation
- EINCDocument2 pagesEINCNess G. Mamasabulod100% (2)
- Maternity Nursing ObDocument11 pagesMaternity Nursing ObMayls Sevilla Calizo74% (19)
- Compt - Appraisal Prelim 2 Glenda CasundoDocument19 pagesCompt - Appraisal Prelim 2 Glenda CasundoJoanne Bernadette AguilarPas encore d'évaluation
- Philippine Nursing Licensure ExaminationDocument32 pagesPhilippine Nursing Licensure ExaminationVera100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- Nur - 100 Session 3 - SemillaDocument8 pagesNur - 100 Session 3 - SemillaVon R SemillaPas encore d'évaluation
- Iwas Paputok LectureDocument31 pagesIwas Paputok LectureShan Dave TupasPas encore d'évaluation
- Pediatric Nursing - QuizDocument13 pagesPediatric Nursing - QuizChy ChyPas encore d'évaluation
- Understanding Child DevelopmentDocument73 pagesUnderstanding Child DevelopmentPrince Jhessie L. AbellaPas encore d'évaluation
- That ApplyDocument14 pagesThat ApplyEmmanuel Glenn L. JulioPas encore d'évaluation
- PedsDocument17 pagesPedsAaron Michael100% (1)
- Chapter 10: Developmental Management of Infants Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument3 pagesChapter 10: Developmental Management of Infants Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuPas encore d'évaluation
- MedsDocument6 pagesMedsnycjg15Pas encore d'évaluation
- Ortho NCLEX QuestionsDocument39 pagesOrtho NCLEX QuestionsJED92% (13)
- HAAD ReviewerDocument35 pagesHAAD ReviewerSydRey92% (24)
- ObstetricsDocument25 pagesObstetricsnycjg15Pas encore d'évaluation
- Review MuskuloDocument183 pagesReview Muskulonycjg15Pas encore d'évaluation
- Understanding the Biology of Cancer CellsDocument11 pagesUnderstanding the Biology of Cancer Cellsnycjg15Pas encore d'évaluation
- Vascular Disease A Handbook For NursesDocument271 pagesVascular Disease A Handbook For NursesMonika JosephPas encore d'évaluation
- HAAD ReviewerDocument35 pagesHAAD ReviewerSydRey92% (24)
- MedsDocument6 pagesMedsnycjg15Pas encore d'évaluation
- Childhood DisordersDocument63 pagesChildhood Disordersnycjg15Pas encore d'évaluation
- HAAD ReviewerDocument35 pagesHAAD ReviewerSydRey92% (24)
- The Nature of CHN Practice Requires That Current Knowledge Derived From TheDocument17 pagesThe Nature of CHN Practice Requires That Current Knowledge Derived From TheAlexis TrinidadPas encore d'évaluation
- OncoDocument6 pagesOnconycjg15Pas encore d'évaluation
- Ortho NCLEX QuestionsDocument39 pagesOrtho NCLEX QuestionsJED92% (13)
- The Nature of CHN Practice Requires That Current Knowledge Derived From TheDocument17 pagesThe Nature of CHN Practice Requires That Current Knowledge Derived From TheAlexis TrinidadPas encore d'évaluation
- Communicable Dse ReviewerDocument13 pagesCommunicable Dse ReviewerRichard Ines Valino100% (29)
- Psychiatric TherapiesDocument78 pagesPsychiatric Therapiesnycjg15Pas encore d'évaluation
- Our Lady of Fatima University - QC: Guest Ledger ReportDocument1 pageOur Lady of Fatima University - QC: Guest Ledger Reportnycjg15Pas encore d'évaluation
- Ortho NCLEX QuestionsDocument39 pagesOrtho NCLEX QuestionsJED92% (13)
- Oncology ReviewerDocument2 pagesOncology Reviewernycjg15Pas encore d'évaluation
- PEDIADocument56 pagesPEDIAstuffednurse100% (3)
- Kwini 20Document1 pageKwini 20nycjg15Pas encore d'évaluation
- Subarachnoid Hemorrhage Case StudyDocument11 pagesSubarachnoid Hemorrhage Case Studynycjg15Pas encore d'évaluation
- BresDocument1 pageBresnycjg15Pas encore d'évaluation
- PN303 Brief Psychotic DisorderDocument8 pagesPN303 Brief Psychotic DisorderFryam BellsPas encore d'évaluation
- Patient HistoryDocument2 pagesPatient Historynycjg15Pas encore d'évaluation
- Nursing InformaticsDocument50 pagesNursing Informaticsnycjg15Pas encore d'évaluation
- Essential Interventions Commodities and Guidelines Guidelines For Reproductive Maternal Newborn and Child HealthDocument28 pagesEssential Interventions Commodities and Guidelines Guidelines For Reproductive Maternal Newborn and Child HealthNewborn2013Pas encore d'évaluation
- Essential Interventions Commodities and Guidelines Guidelines For Reproductive Maternal Newborn and Child HealthDocument28 pagesEssential Interventions Commodities and Guidelines Guidelines For Reproductive Maternal Newborn and Child HealthNewborn2013Pas encore d'évaluation