Académique Documents
Professionnel Documents
Culture Documents
Basic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.
Transféré par
Marc Imhotep Cray, M.D.Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Basic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.
Transféré par
Marc Imhotep Cray, M.D.Droits d'auteur :
Formats disponibles
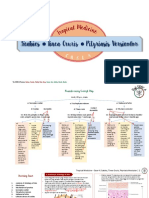
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
IVMS| Basic Medical Science
of the Kidney
The Scientific Basis of Clinical Disease
Compiled by Marc Imhotep Cray, M.D.(12-13-v1)
For Imhotep Virtual Medical School USMLE Step 1 and Step 2 review preparation programs.
Visit our website: http://www.imhotepvirtualmedsch.com/
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Contents
Articles
Kidney
Renal function
13
Renal corpuscle
22
Nephron
24
Glomerulus
29
Bowman's capsule
33
Renal physiology
36
Renal glucose reabsorption
41
Renal sodium reabsorption
42
Renal chloride reabsorption
44
Renal protein reabsorption
45
Renal tubular acidosis
46
Proximal renal tubular acidosis
49
Distal renal tubular acidosis
51
Renal urea handling
53
Ammonia
54
Urine
74
Clearance (medicine)
81
Blood pressure
85
Erythropoietin
100
Calcium metabolism
109
Fluid balance
113
Vasopressin
117
Aldosterone
128
Countercurrent multiplication
134
Osmoregulation
135
Loop of Henle
139
Water-electrolyte imbalance
142
Hyponatremia
143
Hypernatremia
149
Acidbase homeostasis
151
Acidosis
154
Alkalosis
157
Glomerulonephritis
159
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Interstitial nephritis
164
Diabetic nephropathy
166
Acute kidney injury
171
Acute tubular necrosis
176
Chronic kidney disease
178
Dialysis
185
Kidney transplantation
190
References
Article Sources and Contributors
199
Image Sources, Licenses and Contributors
204
Article Licenses
License
207
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Kidney
Kidney
Human kidneys viewed from behind with spine removed
Latin
Ren (Greek: nephros)
System
Urinary system and endocrine system
Artery
Renal artery
Vein
Renal vein
Nerve
Renal plexus
MeSH
Kidney
[1]
Dorlands/Elsevier Kidney [2]
The kidneys are organs that serve several essential regulatory roles in vertebrate animals. They are essential in the
urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acidbase
balance, and regulation of blood pressure (via maintaining salt and water balance). They serve the body as a natural
filter of the blood, and remove wastes, which are diverted to the urinary bladder. In producing urine, the kidneys
excrete wastes such as urea and ammonium, and they are also responsible for the reabsorption of water, glucose, and
amino acids. The kidneys also produce hormones including calcitriol, erythropoietin, and the enzyme renin.
Located at the rear of the abdominal cavity in the retroperitoneum, the kidneys receive blood from the paired renal
arteries, and drain into the paired renal veins. Each kidney excretes urine into a ureter, itself a paired structure that
empties into the urinary bladder.
Renal physiology is the study of kidney function, while nephrology is the medical specialty concerned with kidney
diseases. Diseases of the kidney are diverse, but individuals with kidney disease frequently display characteristic
clinical features. Common clinical conditions involving the kidney include the nephritic and nephrotic syndromes,
renal cysts, acute kidney injury, chronic kidney disease, urinary tract infection, nephrolithiasis, and urinary tract
obstruction. Various cancers of the kidney exist; the most common adult renal cancer is renal cell carcinoma.
Cancers, cysts, and some other renal conditions can be managed with removal of the kidney, or nephrectomy. When
renal function, measured by glomerular filtration rate, is persistently poor, dialysis and kidney transplantation may
be treatment options. Although they are not normally harmful, kidney stones can be painful and repeated, chronic
formation of stones can scar the kidneys. The removal of kidney stones involves ultrasound treatment to break up the
stones into smaller pieces, which are then passed through the urinary tract. One common symptom of kidney stones
is a sharp to disabling pain in the medial/lateral segments of the lower back or groin.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Anatomy
Location
In humans the kidneys are located in
the abdominal cavity, more specifically
in the paravertebral gutter and lie in a
retroperitoneal position at a slightly
oblique angle. There are two kidneys.
One is on each side of the spine. The
asymmetry within the abdominal
cavity caused by the liver typically
results in the right kidney being
slightly lower than the left, and left
kidney being located slightly more
medial than the right. The left kidney
is approximately at the vertebral level
T12 to L3,[3] and the right slightly
lower. The right kidney sits just below
the diaphragm and posterior to the
liver, the left below the diaphragm and
posterior to the spleen. Resting on top
of each kidney is an adrenal gland. The
upper (cranial) parts of the kidneys are
partially protected by the eleventh and
twelfth ribs, and each whole kidney
and adrenal gland are surrounded by
two layers of fat (the perirenal and
pararenal fat) and the renal fascia.
Each adult kidney weighs between 125
and 170grams in males and between
115 and 155grams in females. The left
kidney is usually slightly larger than
the right kidney.
Surface projections of the organs of the trunk, showing kidneys
at the level of T12 to L2.
A CT scan in which the kidneys are shown
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Structure
The kidney has a bean-shaped structure; each kidney
has a convex and concave surface. The concave
surface, the renal hilum, is the point at which the renal
artery enters the organ, and the renal vein and ureter
leave. The kidney is surrounded by tough fibrous
tissue, the renal capsule, which is itself surrounded by
perinephric fat, renal fascia (of Gerota) and paranephric
fat. The anterior (front) border of these tissues is the
peritoneum, while the posterior (rear) border is the
transversalis fascia.
The superior border of the right kidney is adjacent to
the liver; and the spleen, for the left kidney. Therefore,
both move down on inhalation.
The kidney is approximately 1114cm in length, 6cm
wide and 4cm thick.
1.Renal pyramid 2.Interlobular artery 3.Renal artery 4.Renal
vein 5.Renal hilum 6.Renal pelvis 7.Ureter 8.Minor calyx
9.Renal capsule 10.Inferior renal capsule 11.Superior renal
capsule 12.Interlobular vein 13.Nephron 14.Minor calyx
15.Major calyx 16.Renal papilla 17.Renal column
The substance, or parenchyma, of the kidney is divided
into two major structures: superficial is the renal cortex
and deep is the renal medulla. Grossly, these structures
take the shape of 8 to 18 cone-shaped renal lobes, each
containing renal cortex surrounding a portion of
medulla called a renal pyramid (of Malpighi). Between the renal pyramids are projections of cortex called renal
columns (of Bertin). Nephrons, the urine-producing functional structures of the kidney, span the cortex and medulla.
The initial filtering portion of a nephron is the renal corpuscle, located in the cortex, which is followed by a renal
tubule that passes from the cortex deep into the medullary pyramids. Part of the renal cortex, a medullary ray is a
collection of renal tubules that drain into a single collecting duct.
The tip, or papilla, of each pyramid empties urine into a minor calyx; minor calyces empty into major calyces, and
major calyces empty into the renal pelvis, which becomes the ureter. At the hilum, the ureter and renal vein exit the
kidney while the renal artery enters. Surrounding these structures is hilar fat and lymphatic tissue with lymph nodes.
The hilar fat is contiguous with a fat-filled cavity called the renal sinus. The renal sinus collectively contains the
renal pelvis and calyces and separates these structures from the renal medullary tissue.[4]
Blood supply
The kidneys receive blood from the renal arteries, left and right, which
branch directly from the abdominal aorta. Despite their relatively small
size, the kidneys receive approximately 20% of the cardiac output.
Each renal artery branches into segmental arteries, dividing further into
interlobar arteries, which penetrate the renal capsule and extend
through the renal columns between the renal pyramids. The interlobar
arteries then supply blood to the arcuate arteries that run through the
boundary of the cortex and the medulla. Each arcuate artery supplies
several interlobular arteries that feed into the afferent arterioles that
supply the glomeruli.
3D-rendered computed tomography, showing
renal arteries and veins.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
The interstitium is the functional space in the kidney beneath the individual filters (glomeruli), which are rich in
blood vessels. The interstitum absorbs fluid recovered from urine. Various conditions can lead to scarring and
congestion of this area, which can cause kidney dysfunction and failure.
After filtration occurs the blood moves through a small network of venules that converge into interlobular veins. As
with the arteriole distribution the veins follow the same pattern, the interlobular provide blood to the arcuate veins
then back to the interlobar veins, which come to form the renal vein exiting the kidney for transfusion for blood.
Histology
Renal histology studies the structure of the kidney as viewed under a
microscope. Various distinct cell types occur in the kidney, including:
Kidney glomerulus parietal cell
Kidney glomerulus podocyte
Kidney proximal tubule brush border cell
Loop of Henle thin segment cell
Thick ascending limb cell
Kidney distal tubule cell
Kidney collecting duct cell
Interstitial kidney cells
Renal arteries and their branches
Microscopic photograph of the renal medulla
The renal artery enters into the kidney at the level of first lumbar
vertebra just below the superior mesenteric artery. As it enters the
kidney it divides into branches: first the segmental artery, which
divides into 2 or 3 lobar arteries, then further divides into interlobar
arteries, which further divide into the arcuate artery, which leads into
the interlobular artery, which form afferent arterioles. The afferent
arterioles form the glomerulus (network of capillaries closed in
Bowman's capsule). From here, efferent arterioles leaves the
glomerulus and divide into peritubular capillaries, which drain into the
Microscopic photograph of the renal cortex
interlobular veins and then into arcuate vein and then into interlobar
vein, which runs into lobar vein, which opens into the segmental vein and which drains into the renal vein, and then
from it blood moves into the inferior vena cava.
Innervation
The kidney and nervous system communicate via the renal plexus, whose fibers course along the renal arteries to
reach each kidney. Input from the sympathetic nervous system triggers vasoconstriction in the kidney, thereby
reducing renal blood flow. The kidney also receives input from the parasympathetic nervous system, by way of the
renal branches of the vagus nerve (cranial nerve X); the function of this is yet unclear. Sensory input from the kidney
travels to the T10-11 levels of the spinal cord and is sensed in the corresponding dermatome. Thus, pain in the flank
region may be referred from corresponding kidney.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Functions
The kidney participates in whole-body homeostasis, regulating acid-base balance, electrolyte concentrations,
extracellular fluid volume, and regulation of blood pressure. The kidney accomplishes these homeostatic functions
both independently and in concert with other organs, particularly those of the endocrine system. Various endocrine
hormones coordinate these endocrine functions; these include renin, angiotensin II, aldosterone, antidiuretic
hormone, and atrial natriuretic peptide, among others.
Many of the kidney's functions are accomplished by relatively simple mechanisms of filtration, reabsorption, and
secretion, which take place in the nephron. Filtration, which takes place at the renal corpuscle, is the process by
which cells and large proteins are filtered from the blood to make an ultrafiltrate that eventually becomes urine. The
kidney generates 180 liters of filtrate a day, while reabsorbing a large percentage, allowing for the generation of only
approximately 2 liters of urine. Reabsorption is the transport of molecules from this ultrafiltrate and into the blood.
Secretion is the reverse process, in which molecules are transported in the opposite direction, from the blood into the
urine.
Excretion of wastes
The kidneys excrete a variety of waste products produced by metabolism. These include the nitrogenous wastes
called "urea", from protein catabolism, as well as uric acid, from nucleic acid metabolism. Formation of urine is also
the function of the kidney. The concentration of nitrogenous wastes, in the urine of mammals and some birds, is
dependent on an elaborate countercurrent multiplication system. This requires several independent nephron
characteristics to operate: a tight hair pin configuration of the tubules, water and ion permeability in the descending
limb of the loop, water impermeability in the ascending loop and active ion transport out of most of the ascending
loop. In addition, countercurrent exchange by the vessels carrying the blood supply to the nephron is essential for
enabling this function.
Reabsorption of vital nutrients
Glucose at normal plasma levels is completely reabsorbed in the proximal tubule. The mechanism for this is the
Na+/glucose cotransporter. A plasma level of 350mg/dL will fully saturate the transporters and glucose will be lost
in the urine. A plasma glucose level of approximately 160 is sufficient to allow glucosuria, which is an important
clinical clue to diabetes mellitus.
Amino acids are reabsorbed by sodium dependent transporters in the proximal tubule. Hartnup's disease is a
deficiency of the tryptophan amino acid transporter, which results in pellagra.[5]
Location of
Reabsorption
Reabsorbed nutrient
Notes
Early proximal tubule
Glucose (100%), amino acids (100%), bicarbonate (90%),
Na+ (65%), Cl, phosphate and H2O (65%)
PTH will inhibit phosphate excretion
AT II stimulates Na+, H2O and HCO3 reabsorption.
Thin descending loop
of Henle
H2O
Reabsorbs via medullary hypertonicity and makes
urine hypertonic.
Thick ascending loop
of Henle
Na+ (1020%), K+, Cl; indirectly induces para cellular
reabsorption of Mg2+, Ca2+
This region is impermeable to H2O and the urine
becomes less concentrated as it ascends.
Early distal convoluted Na+, Cl
tubule
PTH causes Ca2+ reabsorption.
Collecting tubules
Na+ is reabsorbed in exchange for K+, and H+, which is
regulated by aldosterone.
ADH acts on the V2 receptor and inserts aquaporins on
the luminal side
Na+(35%), H2O
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Pregnancy reduces the reabsorption of glucose and amino acids.
Acid-base homeostasis
Two organ systems, the kidneys and lungs, maintain acid-base homeostasis, which is the maintenance of pH around
a relatively stable value. The lungs contribute to acid-base homeostasis by regulating carbon dioxide (CO2)
concentration. The kidneys have two very important roles in maintaining the acid-base balance: to reabsorb
bicarbonate from urine, and to excrete hydrogen ions into urine
Osmolality regulation
Any significant rise in plasma osmolality is detected by the hypothalamus, which communicates directly with the
posterior pituitary gland. An increase in osmolality causes the gland to secrete antidiuretic hormone (ADH), resulting
in water reabsorption by the kidney and an increase in urine concentration. The two factors work together to return
the plasma osmolality to its normal levels.
ADH binds to principal cells in the collecting duct that translocate aquaporins to the membrane, allowing water to
leave the normally impermeable membrane and be reabsorbed into the body by the vasa recta, thus increasing the
plasma volume of the body.
There are two systems that create a hyperosmotic medulla and thus increase the body plasma volume: Urea recycling
and the 'single effect.'
Urea is usually excreted as a waste product from the kidneys. However, when plasma blood volume is low and ADH
is released the aquaporins that are opened are also permeable to urea. This allows urea to leave the collecting duct
into the medulla creating a hyperosmotic solution that 'attracts' water. Urea can then re-enter the nephron and be
excreted or recycled again depending on whether ADH is still present or not.
The 'Single effect' describes the fact that the ascending thick limb of the loop of Henle is not permeable to water but
is permeable to NaCl. This allows for a countercurrent exchange system whereby the medulla becomes increasingly
concentrated, but at the same time setting up an osmotic gradient for water to follow should the aquaporins of the
collecting duct be opened by ADH.
Blood pressure regulation
Although the kidney cannot directly sense blood, long-term regulation of blood pressure predominantly depends
upon the kidney. This primarily occurs through maintenance of the extracellular fluid compartment, the size of
which depends on the plasma sodium concentration. Renin is the first in a series of important chemical messengers
that make up the renin-angiotensin system. Changes in renin ultimately alter the output of this system, principally the
hormones angiotensin II and aldosterone. Each hormone acts via multiple mechanisms, but both increase the kidney's
absorption of sodium chloride, thereby expanding the extracellular fluid compartment and raising blood pressure.
When renin levels are elevated, the concentrations of angiotensin II and aldosterone increase, leading to increased
sodium chloride reabsorption, expansion of the extracellular fluid compartment, and an increase in blood pressure.
Conversely, when renin levels are low, angiotensin II and aldosterone levels decrease, contracting the extracellular
fluid compartment, and decreasing blood pressure.
Hormone secretion
The kidneys secrete a variety of hormones, including erythropoietin, and the enzyme renin. Erythropoietin is
released in response to hypoxia (low levels of oxygen at tissue level) in the renal circulation. It stimulates
erythropoiesis (production of red blood cells) in the bone marrow. Calcitriol, the activated form of vitamin D,
promotes intestinal absorption of calcium and the renal reabsorption of phosphate. Part of the
renin-angiotensin-aldosterone system, renin is an enzyme involved in the regulation of aldosterone levels.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Development
The mammalian kidney develops from intermediate mesoderm. Kidney development, also called nephrogenesis,
proceeds through a series of three successive phases, each marked by the development of a more advanced pair of
kidneys: the pronephros, mesonephros, and metanephros.
Evolutionary adaptation
Kidneys of various animals show evidence of evolutionary adaptation and have long been studied in ecophysiology
and comparative physiology. Kidney morphology, often indexed as the relative medullary thickness, is associated
with habitat aridity among species of mammals.
Related terms
Medical terms related to the kidneys commonly use terms such as renal and the prefix nephro-. The adjective renal,
meaning related to the kidney, is from the Latin rns, meaning kidneys; the prefix nephro- is from the Ancient
Greek word for kidney, nephros (). For example, surgical removal of the kidney is a nephrectomy, while a
reduction in kidney function is called renal dysfunction.
Diseases and disorders
Congenital
Congenital hydronephrosis
Congenital obstruction of urinary tract
Duplex kidneys, or double kidneys, occur in approximately 1% of the population. This occurrence normally
causes no complications, but can occasionally cause urine infections.
Duplicated ureter occurs in approximately one in 100 live births
Horseshoe kidney occurs in approximately one in 400 live births
Nutcracker Syndrome
Polycystic kidney disease
Autosomal dominant polycystic kidney disease afflicts patients later in life. Approximately one in 1000 people
will develop this condition
Autosomal recessive polycystic kidney disease is far less common, but more severe, than the dominant
condition. It is apparent in utero or at birth.
Renal agenesis. Failure of one kidney to form occurs in approximately one in 750 live births. Failure of both
kidneys to form is invariably fatal.
Renal dysplasia
Unilateral small kidney
Multicystic dysplastic kidney occurs in approximately one in every 2400 live births
Ureteropelvic Junction Obstruction or UPJO; although most cases appear congenital, some appear to be an
acquired condition
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Acquired
Diabetic nephropathy
Glomerulonephritis
Hydronephrosis is the enlargement of one or both of the kidneys
caused by obstruction of the flow of urine.
Interstitial nephritis
Kidney stones (nephrolithiasis) are a relatively common and
particularly painful disorder.
Kidney tumors
Wilms tumor
Renal cell carcinoma
Lupus nephritis
Minimal change disease
In nephrotic syndrome, the glomerulus has been damaged so that a
large amount of protein in the blood enters the urine. Other frequent
features of the nephrotic syndrome include swelling, low serum
albumin, and high cholesterol.
Pyelonephritis is infection of the kidneys and is frequently caused
by complication of a urinary tract infection.
Drawing of an enlarged kidney by John Hunter.
Renal failure
Acute renal failure
Stage 5 Chronic Kidney Disease
Kidney Failure
Generally, humans can live normally with just one kidney, as one has more functioning renal tissue than is needed to
survive. Only when the amount of functioning kidney tissue is greatly diminished does one develop chronic kidney
disease. Renal replacement therapy, in the form of dialysis or kidney transplantation, is indicated when the
glomerular filtration rate has fallen very low or if the renal dysfunction leads to severe symptoms.
Diagnosis
Clinical
Many renal diseases are diagnosed on the basis of classical clinical findings. A physician (usually a nephrologist)
begins by taking a detailed clinical history and performs a physical examination. In addition to medical history and
presenting symptoms, a physician will ask about medication history, family history recent infections, toxic/chemical
exposures and other historical factors that may indicate an etiology for the patient's renal disease. Often, some
diseases are suggested by clinical history and time course alone. For example, in a formerly healthy child with a
recent upper respiratory tract infection and facial/lower limb swelling, findings of proteinuria on urinalysis, a
diagnosis of minimal change disease is highly suggested. Similarly, a patient with a history of diabetes who presents
with decreased urine output is most likely to be suffering from diabetic nephropathy. Often, such cases do not
require extensive workup (such as with renal biopsy). A presumptive diagnosis can be made on the basis of history,
physical exam and supportive laboratory studies.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
Laboratory
Laboratory studies are an important adjunct to clinical evaluation for assessment of renal function. An initial workup
of a patient may include a complete blood count (CBC); serum electrolytes including sodium, potassium, chloride,
bicarbonate, calcium, and phosphorus; blood urea, nitrogen and creatinine; blood glucose and glycocylated
hemoglobin. Glomerular filtration rate (GFR) can be calculated.[6]
Urine studies may include urine electrolytes, creatinine, protein, fractional excretion of sodium (FENA) and other
studies to assist in evaluation of the etiology of a patient's renal disease.
Urinalysis is used to evaluate urine for its pH, protein, glucose, specific gravity and the presence of
blood/hemoglobin. Microscopic analysis can be helpful in the identification of casts, red blood cells, white blood
cells and crystals.
Imaging studies
Imaging studies are important in the evaluation of structural renal disease caused by urinary tract obstruction, renal
stones, renal cyst, mass lesions, renal vascular disease, and vesicoureteral reflux.
Imaging techniques used most frequently include renal ultrasound and helical CT scan. Patients with suspected
vesicoureteral reflux may undergo voiding cystourethrogram (VCUG).
Renal biopsy
The role of the renal biopsy is to diagnose renal disease in which the etiology is not clear based upon noninvasive
means (clinical history, past medical history, medication history, physical exam, laboratory studies, imaging studies).
A detailed description of renal biopsy interpretation is beyond the scope of this article. In general, a renal pathologist
will perform a detailed morphological evaluation and integrate the morphologic findings with the clinical history and
laboratory data, ultimately arriving at a pathological diagnosis. A renal pathologist is a physician who has undergone
general training in anatomic pathology and additional specially training in the interpretation of renal biopsy
specimens.
Ideally, multiple core sections are obtained and evaluated for adequacy (presence of glomeruli) intraoperatively. A
pathologist/pathology assistant divides the specimen(s) for submission for light microscopy, immunofluorescence
microscopy and electron microscopy.
The pathologist will examine the specimen using light microscopy with multiple staining techniques (hematoxylin
and eosin/H&E, PAS, trichrome, silver stain) on multiple level sections. Multiple immunofluorescence stains are
performed to evaluate for antibody, protein and complement deposition. Finally, ultra-structural examination is
performed with electron microscopy and may reveal the presence of electron-dense deposits or other characteristic
abnormalities that may suggest an etiology for the patient's renal disease.
Calculations
Calculations of kidney performance are an important part of physiology and can be estimated using the calculations
below.
Filtration Fraction
The filtration fraction is the amount of plasma that is actually filtered through the kidney. This can be defined using
the equation:
FF=GFR/RPF
FF is the filtration fraction
GFR is the glomerular filtration rate
RPF is the renal plasma flow
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
10
Normal human FF is 20%.
Renal Clearance
Renal clearance is the volume of plasma from which the substance is completely cleared from the blood per unit
time.
Cx=(Ux)V/Px
Cx is the clearance of X (normally in units of mL/min.
Ux is the urine concentration of X.
Px is the plasma concentration of X.
V is the urine flow rate.
More information regarding renal function can be found on the Renal function Wikipedia page.
In other animals
In the majority of vertebrates, the mesonephros persists into the adult,
albeit usually fused with the more advanced metanephros; only in
amniotes is the mesonephros restricted to the embryo. The kidneys of
fish and amphibians are typically narrow, elongated organs, occupying
a significant portion of the trunk. The collecting ducts from each
cluster of nephrons usually drain into an archinephric duct, which is
homologous with the vas deferens of amniotes. However, the situation
is not always so simple; in cartilaginous fish and some amphibians,
there is also a shorter duct, similar to the amniote ureter, which drains
A pig's kidney opened.
the posterior (metanephric) parts of the kidney, and joins with the
archinephric duct at the bladder or cloaca. Indeed, in many
cartilaginous fish, the anterior portion of the kidney may degenerate or cease to function altogether in the adult.
In the most primitive vertebrates, the hagfish and lampreys, the kidney is unusually simple: it consists of a row of
nephrons, each emptying directly into the archinephric duct. Invertebrates may possess excretory organs that are
sometimes referred to as "kidneys", but, even in Amphioxus, these are never homologous with the kidneys of
vertebrates, and are more accurately referred to by other names, such as nephridia.
The kidneys of reptiles consist of a number of lobules arranged in a broadly linear pattern. Each lobule contains a
single branch of the ureter in its centre, into which the collecting ducts empty. Reptiles have relatively few nephrons
compared with other amniotes of a similar size, possibly because of their lower metabolic rate.
Birds have relatively large, elongated kidneys, each of which is divided into three or more distinct lobes. The lobes
consists of several small, irregularly arranged, lobules, each centred on a branch of the ureter. Birds have small
glomeruli, but about twice as many nephrons as similarly sized mammals.
The human kidney is fairly typical of that of mammals. Distinctive features of the mammalian kidney, in comparison
with that of other vertebrates, include the presence of the renal pelvis and renal pyramids, and of a clearly
distinguishable cortex and medulla. The latter feature is due to the presence of elongated loops of Henle; these are
much shorter in birds, and not truly present in other vertebrates (although the nephron often has a short intermediate
segment between the convoluted tubules). It is only in mammals that the kidney takes on its classical "kidney" shape,
although there are some exceptions, such as the multilobed reniculate kidneys of cetaceans.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
11
History
The Latin term renes is related to the English word "reins", a synonym for the kidneys in Shakespearean English
(e.g. Merry Wives of Windsor 3.5), which was also the time the King James Version was translated. Kidneys were
once popularly regarded as the seat of the conscience and reflection,[7][8] and a number of verses in the Bible (e.g.
Ps. 7:9, Rev. 2:23) state that God searches out and inspects the kidneys, or "reins", of humans. Similarly, the Talmud
(Berakhoth 61.a) states that one of the two kidneys counsels what is good, and the other evil.
Kidneys as food
The kidneys can be cooked and eaten (along with other offal).
Kidneys are usually grilled or sauted, but in more complex dishes
they are stewed with a sauce that will improve their flavor. In many
preparations, kidneys are combined with pieces of meat or liver, as in
mixed grill or meurav Yerushalmi. Dishes include the British steak and
kidney pie, the Swedish hkarpanna (pork and kidney stew), the
French rognons de veau sauce moutarde (veal kidneys in mustard
sauce) and the Spanish riones al Jerez (kidneys stewed in sherry
sauce) .[9]
Hkarpanna, Swedish pork and kidney stew
Additional Images
Kidney Posterior View
Anterior relation of Left Kidney
Kidney Cross Section
Dissection images
Right Kidney
Kidney
Right Kidney
Right kidney
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney
12
Left kidney
Kidneys
Left kidney
References
[1] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?mode=& term=Kidney
[2] http:/ / www. mercksource. com/ pp/ us/ cns/ cns_hl_dorlands_split. jsp?pg=/ ppdocs/ us/ common/ dorlands/ dorland/ five/ 000056330. htm
[3] Blens ytanatomy (Superficial anatomy of the trunk). Anca Dragomir, Mats Hjortberg and Godfried M. Romans. Section for human anatomy
at the Department of medical biology, Uppsala university, Sweden.
[4] Clapp, WL. "Renal Anatomy". In: Zhou XJ, Laszik Z, Nadasdy T, D'Agati VD, Silva FG, eds. Silva's Diagnostic Renal Pathology. New
York: Cambridge University Press; 2009.
[5] Le, Tao. First Aid for the USMLE Step 1 2013. New York: McGraw-Hill Medical, 2013. Print.
[6] Post TW, Rose BD, auths and Curhan GC, Sheridan AM, eds. Diagnostic Approach to the Patient With Acute Kidney Injury (Acute Renal
Failure) or Chronic Kidney Disease. UpToDate.com, Dec. 2012. http:/ / www. uptodate. com. ezproxy2. library. arizona. edu/ contents/
diagnostic-approach-to-the-patient-with-acute-kidney-injury-acute-renal-failure-or-chronic-kidney-disease?source=preview& anchor=H12&
selectedTitle=1~150#H12
[7] The Patient as Person: Explorations in Medical Ethics p. 60 by Paul Ramsey, Margaret Farley, Albert Jonsen, William F. May (2002)
[8] History of Nephrology 2 p. 235 by International Association for the History of Nephrology Congress, Garabed Eknoyan, Spyros G. Marketos,
Natale G. De Santo, 1997; Reprint of American Journal of Nephrology; v. 14, no. 46, 1994.
[9] Rognons dans les recettes (http:/ / cuisine. notrefamille. com/ recettes-cuisine/ rognons-recette. html)
External links
The NephCure Foundation offers educational materials on the kidney diseases/conditions Nephrotic Syndrome
and FSGS (http://www.nephcure.org)
The Kidney Foundation of Canada (http://www.kidney.ca)
electron microscopic images of the kidney (Dr. Jastrow's EM-Atlas) (http://www.uni-mainz.de/FB/Medizin/
Anatomie/workshop/EM/EMNiereE.html)
European Renal Genome project kidney function tutorial (http://www.euregene.org/euregene/pages/
kidney_tut_e.html)
Kidney Foundation of Canada kidney disease information (http://www.kidneyquebec.ca/ang/kidney_disease/
index.htm)
Renal Fellow Network: Structure & Function of Other Animals' Kidneys (http://renalfellow.blogspot.com/
2009/06/structure-function-of-other-animals.html)
Kidney Stones (http://symptomsofakidneystone.com)
Kidney Diseases (http://www.kidney-stone.us)
Kidney Information (http://www.redurine.com/urinary_tract/kidney_facts.html)
Animated Presentatin on Kidney Function (http://www.davita.com/kidney_animation/)
CAT Scans of various kidney diseases and conditions (http://www.ctcases.net/ct-cases-database/4 Abdomen
And Pelvis/6 Kidneys/) - CT Cases
Kidney Stones; Information and Treatments (http://www.mountsinai.org/patient-care/service-areas/
urological-conditions-and-surgery/areas-of-care/kidney-disease-program)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
Renal function
Renal function, in nephrology, is an
indication of the state of the kidney and its
role in renal physiology. Glomerular
filtration rate (GFR) describes the flow
rate of filtered fluid through the kidney.
Creatinine clearance rate (CCr or CrCl) is
the volume of blood plasma that is cleared
of creatinine per unit time and is a useful
measure for approximating the GFR.
Creatinine clearance exceeds GFR due to
creatinine secretion, which can be blocked
by cimetidine. In alternative fashion,
overestimation by older serum creatinine
methods resulted in an underestimation of
creatinine clearance, which provided a less
biased estimate of GFR. Both GFR and CCr
may
be
accurately
calculated
by
comparative measurements of substances in
the blood and urine, or estimated by
formulas using just a blood test result
(eGFR and eCCr).
Diagram showing the basic physiologic mechanisms of the kidney
The results of these tests are important in
assessing the excretory function of the
kidneys. For example, grading of chronic renal insufficiency and dosage of drugs that are excreted primarily via
urine are based on GFR (or creatinine clearance).
It is commonly believed to be the amount of liquid filtered out of the blood that gets processed by the kidneys. In
physiological terms, these quantities (volumetric blood flow and mass removal) are related only loosely.
Indirect markers
Most doctors use the plasma concentrations of the waste substances of creatinine and urea (U), as well as electrolytes
(E), to determine renal function. These measures are adequate to determine whether a patient is suffering from
kidney disease.
However, blood urea nitrogen (BUN) and creatinine will not be raised above the normal range until 60% of total
kidney function is lost. Hence, the more accurate Glomerular filtration rate or its approximation of the creatinine
clearance is measured whenever renal disease is suspected or careful dosing of nephrotoxic drugs is required.
Another prognostic marker for kidney disease is an elevated level of protein in the urine. The most sensitive marker
of proteinuria is elevated urine albumin. Persistent presence of more than 30mg albumin per gram creatinine in the
urine is diagnostic of chronic kidney disease (microalbuminuria is a level of 30299mg/L urine or 30-299 mg/24
hrs; a concentration of albumin in the urine that is not detected by usual urine dipstick methods).
13
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
Glomerular filtration rate
Glomerular filtration rate (GFR) is the volume of fluid filtered from the renal (kidney) glomerular capillaries into
the Bowman's capsule per unit time.[1] Central to the physiologic maintenance of GFR is the differential basal tone
of the afferent and efferent arterioles (see diagram).
Glomerular filtration rate (GFR) is equal to the Clearance Rate when any solute is freely filtered and is neither
reabsorbed nor secreted by the kidneys. The rate therefore measured is the quantity of the substance in the urine that
originated from a calculable volume of blood. Relating this principle to the below equation - for the substance used,
the product of urine concentration and urine flow equals the mass of substance excreted during the time that urine
has been collected. This mass equals the mass filtered at the glomerulus as nothing is added or removed in the
nephron. Dividing this mass by the plasma concentration gives the volume of plasma which the mass must have
originally come from, and thus the volume of plasma fluid that has entered Bowman's capsule within the
aforementioned period of time. The GFR is typically recorded in units of volume per time, e.g., milliliters per minute
mL/min. Compare to filtration fraction.
There are several different techniques used to calculate or estimate the glomerular filtration rate (GFR or eGFR). The
above formula only applies for GFR calculation when it is equal to the Clearance Rate.
Measurement using inulin
The GFR can be determined by injecting inulin or the inulin-analog sinistrin into the plasma. Since both, inulin and
sinsitrin, are neither reabsorbed nor secreted by the kidney after glomerular filtration, their rate of excretion is
directly proportional to the rate of filtration of water and solutes across the glomerular filter. Compared to the
MDRD formula, the inulin clearance slightly overestimates the glomerular function. In early stage renal disease, the
inulin clearance may remain normal due to hyperfiltration in the remaining nephrons.[2] Incomplete urine collection
is an important source of error in inulin clearance measurement.
Pressure definition
More precisely, GFR is the fluid flow rate between the glomerular capillaries and the Bowman's capsule:
Where:
is the GFR.
is called the filtration constant and is defined as the product of the hydraulic conductivity and the surface
area of the glomerular capillaries.
is the hydrostatic pressure within the glomerular capillaries.
is the hydrostatic pressure within the Bowman's capsule.
is the colloid osmotic pressure within the glomerular capillaries.
and
is the colloid osmotic pressure within the Bowman's capsule.
14
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
15
Kf
Because this constant is a measurement of hydraulic conductivity multiplied by the capillary surface area, it is almost
impossible to measure physically. However, it can be determined experimentally. Methods of determining the GFR
are listed in the above and below sections and it is clear from our equation that
can be found by dividing the
experimental GFR by the net filtration pressure:
PG
The hydrostatic pressure within the glomerular capillaries is determined by the pressure difference between the fluid
entering immediately from the afferent arteriole and leaving through the efferent arteriole. The pressure difference is
approximated by the product of the total resistance of the respective arteriole and the flux of blood through it:
Where:
is the afferent arteriole pressure.
is the efferent arteriole pressure.
is the afferent arteriole resistance.
is the efferent arteriole resistance.
is the afferent arteriole flux.
And,
is the efferent arteriole flux.
PB
The pressure in the Bowman's capsule and proximal tubule can be determined by the difference between the pressure
in the Bowman's capsule and the descending tubule:
Where:
is the pressure in the descending tubule.
And,
is the resistance of the descending tubule.
G
Blood plasma has a good many proteins in it and they exert an inward directed force called the colloid osmotic
pressure on the water in hypotonic solutions across a membrane, i.e., in the Bowman's capsule. Because plasma
proteins are virtually incapable of escaping the glomerular capillaries, this oncotic pressure is defined, simply, by the
ideal gas law:
Where:
R is the universal gas constant
T is the temperature.
And, c is concentration in mol/L of plasma proteins (remember the solutes can freely diffuse through the
glomerular capsule).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
B
This value is almost always taken to be equal to zero because, in a healthy nephron, there should be no proteins in
the Bowman's Capsule.
Creatinine-based approximations of GFR
In clinical practice, however, creatinine clearance or estimates of creatinine clearance based on the serum creatinine
level are used to measure GFR. Creatinine is produced naturally by the body (creatinine is a breakdown product of
creatine phosphate, which is found in muscle). It is freely filtered by the glomerulus, but also actively secreted by the
peritubular capillaries in very small amounts such that creatinine clearance overestimates actual GFR by 10-20%.
This margin of error is acceptable, considering the ease with which creatinine clearance is measured. Unlike precise
GFR measurements involving constant infusions of inulin, creatinine is already at a steady-state concentration in the
blood, and so measuring creatinine clearance is much less cumbersome. However, creatinine estimates of GFR have
their limitations. All of the estimating equations depend on a prediction of the 24-hour creatinine excretion rate,
which is a function of muscle mass. One of the equations, the Cockcroft and Gault equation (see below) does not
correct for race, and it is known that black men and women have a higher amount of muscle mass than
Caucasians[citation needed]; hence, they will have higher serum creatinine levels at any level of clearance.
A common mistake made when just looking at serum creatinine is the failure to account for muscle mass. Hence, an
older woman with a serum creatinine of 1.4 mg/dL may actually have a moderately severe degree of renal
insufficiency, whereas a young muscular male, in particular if black, can have a normal level of renal function at this
serum creatinine level. Creatinine-based equations should be used with caution in cachectic patients and patients
with cirrhosis. They often have very low muscle mass and a much lower creatinine excretion rate than predicted by
the equations below, such that a cirrhotic patient with a serum creatinine of 0.9 mg/dL may have a moderately severe
degree of renal insufficiency.
Creatinine Clearance CCr
One method of determining GFR from creatinine is to collect urine (usually for 24 hours) to determine the amount of
creatinine that was removed from the blood over a given time interval. If one removes, say, 1440mg in 24 hours,
this is equivalent to removing 1mg/min. If the blood concentration is 0.01mg/mL (1mg/dL), then one can say that
100 mL/min of blood is being "cleared" of creatinine, since, to get 1mg of creatinine, 100 mL of blood containing
0.01mg/mL would need to have been cleared.
Creatinine clearance (CCr) is calculated from the creatinine concentration in the collected urine sample (UCr), urine
flow rate (V), and the plasma concentration (PCr). Since the product of urine concentration and urine flow rate yields
creatinine excretion rate, which is the rate of removal from the blood, creatinine clearance is calculated as removal
rate per min (UCrV) divided by the plasma creatinine concentration. This is commonly represented mathematically
as
Example: A person has a plasma creatinine concentration of 0.01mg/ml and in 1 hour produces 60ml of urine with a
creatinine concentration of 1.25mg/mL.
The common procedure involves undertaking a 24-hour urine collection, from empty-bladder one morning to the
contents of the bladder the following morning, with a comparative blood test then taken. The urinary flow rate is still
calculated per minute, hence:
16
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
To allow comparison of results between people of different sizes, the CCr is often corrected for the body surface area
(BSA) and expressed compared to the average sized man as mL/min/1.73 m2. While most adults have a BSA that
approaches 1.7 (1.6-1.9), extremely obese or slim patients should have their CCr corrected for their actual BSA.
BSA can be calculated on the basis of weight and height.
Twenty-four hour urine collection to assess creatinine clearance is no longer widely performed, due to difficulty in
assuring complete specimen collection. To assess the adequacy of a complete collection, one always calculates the
amount of creatinine excreted over a 24-hour period. This amount varies with muscle mass, and is higher in young
people vs. old, in blacks vs. whites, and in men vs. women. An unexpectedly low or high 24-hour creatinine
excretion rate voids the test. Nevertheless, in cases where estimates of creatinine clearance from serum creatinine are
unreliable, creatinine clearance remains a useful test. These cases include "estimation of GFR in individuals with
variation in dietary intake (vegetarian diet, creatine supplements) or muscle mass (amputation, malnutrition, muscle
wasting), since these factors are not specifically taken into account in prediction equations."
Estimated values
A number of formulae have been devised to estimate GFR or Ccr values on the basis of serum creatinine levels.
Estimated creatinine clearance rate (eCCr) using Cockcroft-Gault formula
A commonly used surrogate marker for estimate of creatinine clearance is the Cockcroft-Gault (CG) formula, which
in turn estimates GFR in ml/min:[3] It is named after the scientists who first published the formula, and it employs
serum creatinine measurements and a patient's weight to predict the creatinine clearance. The formula, as originally
published, is:
This formula expects weight to be measured in kilograms and creatinine to be measured in mg/dL, as is
standard in the USA. The resulting value is multiplied by a constant of 0.85 if the patient is female. This
formula is useful because the calculations are simple and can often be performed without the aid of a
calculator.
When serum creatinine is measured in mol/L:
Where Constant is 1.23 for men and 1.04 for women.
One interesting feature of the Cockcroft and Gault equation is that it shows how dependent the estimation of CCr is
based on age. The age term is (140 - age). This means that a 20-year-old person (140-20 = 120) will have twice the
creatinine clearance as an 80-year-old (140-80 = 60) for the same level of serum creatinine (120 is twice as great as
60). The C-G equation assumes that a woman will have a 15% lower creatinine clearance than a man at the same
level of serum creatinine.
17
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
Estimated GFR (eGFR) using Modification of Diet in Renal Disease (MDRD) formula
The most recently advocated formula for calculating the GFR is the one that was developed by the Modification of
Diet in Renal Disease Study Group. Most laboratories in Australia, and The United Kingdom now calculate and
report the MDRD estimated GFR along with creatinine measurements and this forms the basis of chronic kidney
disease. The adoption of the automatic reporting of MDRD-eGFR has been widely criticised.
The most commonly used formula is the "4-variable MDRD," which estimates GFR using four variables: serum
creatinine, age, ethnicity, and gender. The original MDRD used six variables with the additional variables being the
blood urea nitrogen and albumin levels. The equations have been validated in patients with chronic kidney disease;
however both versions underestimate the GFR in healthy patients with GFRs over 60 mL/min. The equations have
not been validated in acute renal failure.
For creatinine in mol/L:
For creatinine in mg/dl:
Creatinine levels in mol/L can be converted to mg/dL by dividing them by 88.4. The 32788 number above is
equal to 18688.41.154.
A more elaborate version of the MDRD equation also includes serum albumin and blood urea nitrogen (BUN) levels:
Where the creatinine and blood urea nitrogen concentrations are both in mg/dL. The albumin concentration is
in g/dL.
These MDRD equations are to be used only if the laboratory has NOT calibrated its serum creatinine measurements
to isotope dilution mass spectrometry (IDMS). When IDMS-calibrated serum creatinine is used (which is about 6%
lower), the above equations should be multiplied by 175/186 or by 0.94086.
Since these formulae do not adjust for body mass, they (relative to the Cockcroft-Gault formula) underestimate
eGFR for heavy people and overestimate it for underweight people. (see Cockcroft-Gault formula above).
Estimated GFR (eGFR) using the CKD-EPI formula
The CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) formula was published in May 2009. It was
developed in an effort to create a formula more accurate than the MDRD formula, especially when actual GFR is
greater than 60 mL/min per 1.73 m2.
Researchers pooled data from multiple studies to develop and validate this new equation. They used 10 studies that
included 8254 participants, randomly using 2/3 of the data sets for development and the other 1/3 for internal
validation. Sixteen additional studies, which included 3896 participants, were used for external validation.
The CKD-EPI equation performed better than the MDRD (Modification of Diet in Renal Disease Study) equation,
especially at higher GFR, with less bias and greater accuracy. When looking at NHANES (National Health and
Nutrition Examination Survey) data, the median estimated GFR was 94.5 mL/min per 1.73 m2 vs. 85.0 mL/min per
1.73 m2, and the prevalence of chronic kidney disease was 11.5% versus 13.1%.
The CKD-EPI equation, expressed as a single equation, is:
where SCr is serum creatinine (mg/dL), k is 0.7 for females and 0.9 for males, a is -0.329 for females and -0.411 for
males, min indicates the minimum of SCr/k or 1, and max indicates the maximum of SCr/k or 1.
A clearer version may be as follows: For creatinine (IDMS calibrated) in mg/dL:
Black Female
18
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
19
If serum creatinine (Scr) <= 0.7
If serum creatinine (Scr) > 0.7
Black male
If serum creatinine (Scr) <= 0.9
If serum creatinine (Scr) > 0.9
White or other race female
If serum creatinine (Scr) <= 0.7
If serum creatinine (Scr) > 0.7
White or other race male
If serum creatinine (Scr) <= 0.9
If serum creatinine (Scr) > 0.9
This formula was developed by Levey et al.
The formula CKD-EPI may provide improved cardiovascular risk prediction over the MDRD Study formula in a
middle-age population.
Estimated GFR (eGFR) using the Mayo Quadratic formula
Another estimation tool to calculate GFR is the Mayo Quadratic formula. This formula was developed by Rule et al.
in an attempt to better estimate GFR in patients with preserved kidney function. It is well recognized that the MDRD
formula tends to underestimate GFR in patients with preserved kidney function.
The equation is:
If Serum Creatinine < 0.8mg/dL, use 0.8mg/dL for Serum Creatinine
Estimated GFR for children using Schwartz formula
In children, the Schwartz formula is used. This employs the serum creatinine (mg/dL), the child's height(cm) and a
constant to estimate the glomerular filtration rate:
Where k is a constant that depends on muscle mass, which itself varies with a child's age:
In first year of life, for pre-term babies K=0.33 and for full-term infants K=0.45
For infants and children of age 1 to 12 years, K=0.55.
The method of selection of the K-constant value has been questioned as being dependent upon the gold-standard of
renal function used (i.e., creatinine clearance, inulin clearance, etc.) and also may be dependent upon the urinary
flow rate at the time of measurement.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
In 2009, the formula was updated to use standardized serum creatinine (recommend k=0.413) and additional
formulas that allow improved precision were derived if serum cystatin measured in addition to serum creatinine.
Importance of calibration of the serum creatinine level and the IDMS standardization
effort
One problem with any creatinine-based equation for GFR is that the methods used to assay creatinine in the blood
differ widely in their susceptibility to non-specific chromogens, which cause the creatinine value to be
overestimated. In particular, the MDRD equation was derived using serum creatinine measurements that had this
problem. The NKDEP program in the United States has attempted to solve this problem by trying to get all
laboratories to calibrate their measures of creatinine to a "gold standard", which in this case is isotope dilution mass
spectrometry (IDMS). In late 2009 not all labs in the U.S. had changed over to the new system. There are two forms
of the MDRD equation that are available, depending on whether or not creatinine was measured by an
IDMS-calibrated assay. The CKD-EPI equation is designed to be used with IDMS-calibrated serum creatinine values
only.
Cystatin C
Problems with creatinine (varying muscle mass, recent meat ingestion, etc.) have led to evaluation of alternative
agents for estimation of GFR. One of these is cystatin C, a ubiquitous protein secreted by most cells in the body (it is
an inhibitor of cysteine protease).
Cystatin C is freely filtered at the glomerulus. After filtration, Cystatin C is reabsorbed and catabolized by the
tubular epithelial cells, with only small amounts excreted in the urine. Cystatin C levels are therefore measured not
in the urine, but in the bloodstream.
Equations have been developed linking estimated GFR to serum cystatin C levels. Most recently, some proposed
equations have combined (sex, age and race) adjusted cystatin C and creatinine. The most accurate is (sex, age and
race) adjusted cystatin C, followed by (sex, age and race) adjusted creatinine and then cystatine C alone in slightly
different with adjusted creatinine.
Normal ranges
The normal range of GFR, adjusted for body surface area, is 100-130 ml/min/1.73m2 in men and women. In children,
GFR measured by inulin clearance is 110 ml/min/1.73m2 until 2 years of age in both sexes, and then it progressively
decreases. After age 40, GFR decreases progressively with age, by about 0.4 - 1.2 mL/min per year.[citation needed]
Chronic kidney disease stages
Risk factors for kidney disease include diabetes, high blood pressure, family history, older age, ethnic group and
smoking. For most patients, a GFR over 60 mL/min/1.73m2 is adequate. But significant decline of the GFR from a
previous test result can be an early indicator of kidney disease requiring medical intervention. The sooner kidney
dysfunction is diagnosed and treated the greater odds of preserving remaining nephrons, and preventing the need for
dialysis.
20
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal function
21
CKD stage GFR level (mL/min/1.73 m2)
Stage 1
90
Stage 2
60 89
Stage 3
30 59
Stage 4
15 29
Stage 5
< 15
The severity of chronic kidney disease (CKD) is described by six stages; the most severe three are defined by the
MDRD-eGFR value, and first three also depend on whether there is other evidence of kidney disease (e.g.,
proteinuria):
0) Normal kidney function GFR above 90mL/min/1.73m2 and no proteinuria
1) CKD1 GFR above 90mL/min/1.73m2 with evidence of kidney damage
2) CKD2 (mild) GFR of 60 to 89 mL/min/1.73m2 with evidence of kidney damage
3) CKD3 (moderate) GFR of 30 to 59 mL/min/1.73m2
4) CKD4 (severe) GFR of 15 to 29 mL/min/1.73m2
5) CKD5 kidney failure - GFR less than 15 mL/min/1.73m2 Some people add CKD5D for those stage 5
patients requiring dialysis; many patients in CKD5 are not yet on dialysis.
Note: others add a "T" to patients who have had a transplant regardless of stage.
Not all clinicians agree with the above classification, suggesting that it may mislabel patients with mildly reduced
kidney function, especially the elderly, as having a disease. A conference was held in 2009 regarding these
controversies by Kidney Disease: Improving Global Outcomes (KDIGO) on CKD: Definition, Classification and
Prognosis, gathering data on CKD prognosis to refine the definition and staging of CKD.
References
[1] - "Glomerular Filtration Rate"
[2] GFR (Cockcroft & MDRD) calculator at medical-calculator.nl (http:/ / www. medical-calculator. nl/ calculator/ GFR/ ) - Cockcroft and
MDRD calculator and details about inulin clearance
[3] GFR Calculator at cato.at - Cockcroft-Gault (http:/ / www. cato. at/ webservice/ servlet/ location?goto=SERVICE_CALC& lang=EN&
URL="calc/ cato_GFR_CG. htm") - GFR calculation (Cockcroft-Gault formula)
31. Creatinine clearance calculator (Cockcroft-Gault Equation)- by MDCalc (http:/ / www. mdcalc. com/
creatinine-clearance-cockcroft-gault-equation/)
External links
Online GFR calculators
Online GFR Calculator (http://nkdep.nih.gov/lab-evaluation/gfr-calculators.shtml)
Schwartz formula (http://www-users.med.cornell.edu/~spon/picu/calc/crclschw.htm) for estimating
pediatric renal function
Reference links
National Kidney Disease Education Program website. (http://www.nkdep.nih.gov/professionals/index.htm)
Includes professional references and GFR calculators
eGFR at Lab Tests Online (http://labtestsonline.org/understanding/analytes/gfr/tab/test)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal corpuscle
22
Renal corpuscle
Renal corpuscle of Malpighi
The structure on the left in blue and pink is the renal corpuscle. The structure on the right is the renal tubule. The blue structure (A) is
the Bowman's capsule (2 and 3). The pink structure is the glomerulus with its capillaries. At the left, blood flows from the afferent
areteriole (9), through the capillaries (10), and out the efferent arteriole (11). The mesangium is the pink structure inside the
glomerulus between the capillaries (5a) and extending outside the glomerulus (5b).
The renal corpuscle in the cortex (outer layer) of the kidney. At the top, the renal corpuscle containing the glomerulus. The filtered
blood exits into the renal tubule, at right. At left, blood flows from the afferent arteriole (red), enters into the renal corpuscle and feeds
the glomerulus; blood flows out of the efferent arteriole (blue).
Latin
corpusculum renis
Gray's
subject #253 1221
[1]
In the kidney, a renal corpuscle is the initial blood-filtering component of a nephron. It consists of two structures: a
glomerulus and a Bowman's capsule.
The glomerulus is a small tuft of capillaries containing two cell types. Endothelial cells, which have large fenestrae,
are not covered by diaphragms. Mesangial cells are modified smooth muscle cells that lie between the capillaries.
They regulate blood flow by their contractile activity and secrete extracellular matrix, prostaglandins, and cytokines.
Mesangial cells also have phagocytic activity, removing proteins and other molecules trapped in the glomerular
basement membrane or filtration barrier.
The Bowman's capsule has an outer parietal layer composed of simple squamous epithelium. The visceral layer,
composed of modified simple squamous epithelium, is lined by podocytes. Podocytes have foot processes, pedicels,
that wrap around glomerular capillaries. These pedicels interdigitate with pedicels of adjacent podocytes forming
filtration slits.
The renal corpuscle filtration barrier is composed of: the fenestrated endothelium of glomerular capillaries, the fused
basal lamina of endothelial cells and podocytes, and the filtration slits of the podocytes. This barrier permits passage
of water, ions, and small molecules from the bloodstream into Bowman's space (the space between the visceral and
parietal layers). Large and/or negatively charged proteins are prevented from passing into Bowman's space, thus
retaining these proteins in the circulation. The basal lamina is composed of 3 layers: lamina rara externa, lamina
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal corpuscle
23
densa, and lamina rara interna. The lamina rara externa is adjacent to the podocyte processes. The lamina densa is the
central layer consisting of type IV collagen and laminin. This layer acts as a selective macromolecular filter,
preventing the passage of large protein molecules into Bowman's space. The lamina rara interna is adjacent to
endothelial cells. This layer contains heparan sulfate, a negatively charged glycosaminoglycan that contributes to the
electrostatic barrier of the glomerular filter.
There are two poles in the renal corpuscle, a vascular pole, and a urinary pole. The vascular pole is where the
afferent and efferent arterioles communicate with the glomerulus. The urinary pole is where the corpuscle opens into
the lumen of the proximal convoluted tubule.
Fluid from blood in the glomerulus is collected in the Bowman's capsule to form "glomerular filtrate", which is then
further processed along the nephron to form urine. The three types of filtration carried out in the Bowman's capsule
are: 1) Basement Filtration 2) Visceral Filtration 3) Endothermic Filtration
Eponym
A renal corpuscle is also known as a Malpighian corpuscle, named after Marcello Malpighi (16281694), an Italian
physician and biologist. This name is not used widely anymore, probably to avoid confusion with a Malpighian
corpuscle in the spleen.
Additional images
Glomerulus is red; Bowman's capsule is pink.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal corpuscle
24
External links
Renal+corpuscle [2] at eMedicine Dictionary
BU Histology Learning System: 16003loa [3]
References
[1] http:/ / education. yahoo. com/ reference/ gray/ subjects/ subject?id=253#p1221
[2] http:/ / www. emedicinehealth. com/ script/ main/ srchcont_dict. asp?src=Renal+ corpuscle
[3] http:/ / www. bu. edu/ histology/ p/ 16003loa. htm
Nephron
Nephron
Nephron of the kidney. The labelled parts are 1. Glomerulus, 2. Efferent arteriole, 3. Bowman's capsule, 4. Proximal convoluted
tubule, 5. Cortical collecting duct, 6. Distal convoluted tubule, 7. Loop of Henle, 8. Duct of Bellini, 9. Peritubular capillaries, 10.
Arcuate vein, 11. Arcuate artery, 12. Afferent arteriole, 13. Juxtaglomerular apparatus.
Latin
Nephroneum
Gray's
subject #253 1221
System
Urinary system
Precursor
Metanephric blastema (intermediate mesoderm)
MeSH
Nephrons
[1]
[1]
Nephron (from Greek - nephros, meaning "kidney") is the basic structural and functional unit of the kidney.
Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the
blood, reabsorbing what is needed and excreting the rest as urine. A nephron eliminates wastes from the body,
regulates blood volume and blood pressure, controls levels of electrolytes and metabolites, and regulates blood pH.
Its functions are vital to life and are regulated by the endocrine system by hormones such as antidiuretic hormone,
aldosterone, and parathyroid hormone. In humans, a normal kidney contains 800,000 to 1.5 million nephrons.
Types of nephrons
Two general classes of nephrons are cortical nephrons and juxtamedullary nephrons, both of which are classified
according to the length of their associated Loop of Henle and location of their renal corpuscle. All nephrons have
their renal corpuscles in the cortex. Cortical nephrons have their Loop of Henle in the renal medulla near its junction
with the renal cortex, while the Loop of Henle of juxtamedullary nephrons is located deep in the renal medulla; they
are called juxtamedullary because their renal corpuscle is located near the medulla (but still in the cortex). The
nomenclature for cortical nephrons varies, with some sources distinguishing between superficial cortical nephrons
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Nephron
and midcortical nephrons, depending on where their corpuscle is located within the cortex.
The majority of nephrons are cortical. Cortical nephrons have a shorter loop of Henle compared to juxtamedullary
nephrons. The longer loop of Henle in juxtamedullary nephrons create a hyperosmolar gradient that allows for the
creation of concentrated urine.
Anatomy
Each nephron is composed of an initial filtering component (the "renal
corpuscle") and a tubule specialized for reabsorption and secretion (the
"renal tubule"). The renal corpuscle filters out solutes from the blood,
delivering water and small solutes to the renal tubule for
modification.[citation needed]
Renal corpuscle
Composed of a glomerulus and the Bowman's capsule, the renal
corpuscle (or Malphigian corpuscle) is the beginning of the nephron. It
is the nephron's initial filtering component.[citation needed]
The glomerulus is a capillary tuft that receives its blood supply from an
afferent arteriole of the renal circulation. The glomerular blood
pressure provides the driving force for water and solutes to be filtered
out of the blood and into the space made by Bowman's capsule. The
remainder of the blood (only approximately 1/5 of all plasma passing
through the kidney is filtered through the glomerular wall into the
Bowman's capsule) passes into the efferent arteriole.The diameter of
Kidney nephron drawing with labels of the
efferent arteriole is comparatively less than that of afferent arteriole,
following: the Bowman's capsule, proximal
increasing the hydrostatic pressure in the glomerulus. It then moves
convoluted tubule, loop of Henle, descending
into the vasa recta, which are only found in juxtamedullary nephrons
limb of loop of Henle, ascending limb of loop of
Henle, distal convoluted tubule, and collecting
and not cortical nephrons. The vasa recta are collecting capillaries
duct.
intertwined with the convoluted tubules through the interstitial space,
in which the reabsorbed substances will also enter. This then combines
with efferent venules from other nephrons into the renal vein, and rejoins the main bloodstream.[citation needed]
The Bowman's capsule, also called the glomerular capsule, surrounds the glomerulus. It is composed of a visceral
inner layer formed by specialized cells called podocytes, and a parietal outer layer composed of simple squamous
epithelium. Fluids from blood in the glomerulus are filtered through the visceral layer of podocytes, and the resulting
glomerular filtrate is further processed along the nephron to form urine.[citation needed]
25
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Nephron
26
Renal tubule
Renal tubule
Latin
tubulus renalis
Gray's subject #253 1223 [2]
The renal tubule is the portion of the nephron containing the tubular fluid filtered through the
glomerulus.[3]Wikipedia:Link rot After passing through the renal tubule, the filtrate continues to the collecting duct
system, which is not part of the nephron.[citation needed]
The components of the renal tubule are:
Proximal convoluted tubule (lies in cortex and lined by simple cuboidal epithelium with brushed borders which
help to increase the area of absorption greatly.)
Loop of Henle (hair-pin like i.e. U-shaped and lies in medulla)
Descending limb of loop of Henle
Ascending limb of loop of Henle
The ascending limb of loop of Henle is divided into 2 segments: Lower end of ascending limb is very thin
and is lined by simple squamous epithelium. The distal portion of ascending limb is thick and is lined by
simple cuboidal epithelium.
Thin ascending limb of loop of Henle
Thick ascending limb of loop of Henle (enters cortex and becomes DCT-distal convoluted tubule.)
Distal convoluted tubule
Functions
The nephron carries out nearly all of the kidney's functions. Most of these functions concern the reabsorption and
secretion of various solutes such as ions (e.g., sodium), carbohydrates (e.g., glucose), and amino acids (e.g.,
glutamate). Properties of the cells that line the nephron change dramatically along its length; consequently, each
segment of the nephron has highly specialized functions.[citation needed]
The proximal tubule as a part of the nephron can be divided into an initial convoluted portion and a following
straight (descending) portion. Fluid in the filtrate entering the proximal convoluted tubule is reabsorbed into the
peritubular capillaries, including approximately two-thirds of the filtered salt and water and all filtered organic
solutes (primarily glucose and amino acids).[citation needed]
The loop of Henle, also called the nephron loop or the loop of Hundley, is a U-shaped tube that extends from the
proximal tubule. It consists of a descending limb and ascending limb. It begins in the cortex, receiving filtrate from
the proximal convoluted tubule, extends into the medulla as the descending limb, and then returns to the cortex as the
ascending limb to empty into the distal convoluted tubule. The primary role of the loop of Henle is to concentrate the
salt in the interstitium, the tissue surrounding the loop.[citation needed]
Considerable differences aid in distinguishing the descending and ascending limbs of the loop of Henle. The
descending limb is permeable to water and noticeably less impermeable to salt, and thus only indirectly contributes
to the concentration of the interstitium. As the filtrate descends deeper into the hypertonic interstitium of the renal
medulla, water flows freely out of the descending limb by osmosis until the tonicity of the filtrate and interstitium
equilibrate. Longer descending limbs allow more time for water to flow out of the filtrate, so longer limbs make the
filtrate more hypertonic than shorter limbs.[citation needed]
Unlike the descending limb, the Thin ascending limb of loop of Henle is impermeable to water, a critical feature of
the countercurrent exchange mechanism employed by the loop. The ascending limb actively pumps sodium out of
the filtrate, generating the hypertonic interstitium that drives countercurrent exchange. In passing through the
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Nephron
ascending limb, the filtrate grows hypotonic since it has lost much of its sodium content. This hypotonic filtrate is
passed to the distal convoluted tubule in the renal cortex.[citation needed]
The distal convoluted tubule has a different structure and function to that of the proximal convoluted tubule. Cells
lining the tubule have numerous mitochondria to produce enough energy (ATP) for active transport to take place.
Much of the ion transport taking place in the distal convoluted tubule is regulated by the endocrine system. In the
presence of parathyroid hormone, the distal convoluted tubule reabsorbs more calcium and secretes more phosphate.
When aldosterone is present, more sodium is reabsorbed and more potassium secreted. Atrial natriuretic peptide
causes the distal convoluted tubule to secrete more sodium. In addition, the tubule also secretes hydrogen and
ammonium to regulate pH.[citation needed]
Collecting duct system
Each distal convoluted tubule delivers its filtrate to a system of collecting ducts, the first segment of which is the
connecting tubule. The collecting duct system begins in the renal cortex and extends deep into the medulla. As the
urine travels down the collecting duct system, it passes by the medullary interstitium which has a high sodium
concentration as a result of the loop of Henle's countercurrent multiplier system.[citation needed]
Though the collecting duct is normally impermeable to water, it becomes permeable in the presence of antidiuretic
hormone (ADH). ADH affects the function of aquaporins, resulting in the reabsorption of water molecules as it
passes through the collecting duct. Aquaporins are membrane proteins that selectively conduct water molecules
while preventing the passage of ions and other solutes. As much as three-quarters of the water from urine can be
reabsorbed as it leaves the collecting duct by osmosis. Thus the levels of ADH determine whether urine will be
concentrated or diluted. An increase in ADH is an indication of dehydration, while water sufficiency results in low
ADH allowing for diluted urine.[citation needed]
Lower portions of the collecting organ are also permeable to urea, allowing some of it to enter the medulla of the
kidney, thus maintaining its high concentration (which is very important for the nephron).[citation needed]
Urine leaves the medullary collecting ducts through the renal papillae, emptying into the renal calyces, the renal
pelvis, and finally into the urinary bladder via the ureter.[citation needed]
Because it has a different origin during the development of the urinary and reproductive organs than the rest of the
nephron, the collecting duct is sometimes not considered a part of the nephron. Instead of originating from the
metanephrogenic blastema, the collecting duct originates from the ureteric bud.[citation needed]
Juxtaglomerular apparatus
The juxtaglomerular apparatus is a specialized region of the nephron responsible for production and secretion of the
enzyme renin, involved in the renin-angiotensin system. This apparatus occurs near the site of contact between the
thick ascending limb and the afferent arteriole. It contains three components: the macula densa, juxtaglomerular
cells, and extraglomerular mesangial cells.[citation needed]
Clinical relevance
Because of its importance in body fluid regulation, the nephron is a common target of drugs that treat high blood
pressure and edema. These drugs, called diuretics, inhibit the ability of the nephron to retain electrolytes (and
consequently water), thereby increasing the amount of urine produced.
27
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Nephron
28
Additional images
Distribution of
blood vessels in
cortex of kidney.
(Although the
figure labels the
efferent vessel as a
vein, it is actually
an arteriole.)
Glomerulus is red;
Bowman's capsule
is white.
This images shows the cells
that make up a nephron in
the kidneys. The following
parts are seen: Lumen of a
distal convoluted tubule
(DCT), Macula densa,
juxtaglomerular cells, lacis
cells, mesangial cells,
podocytesvisceral layer of
Bowmans capsule, parietal
layer of Bowmans capsule,
lumen of a glomerular
capillary, and the urinary
space.
This image shows the types of
cells present in the glomerulus
part of a kidney nephron.
Podocytes, Endothelial cells, and
Glomerular mesangial cell are
present.
Kidney tissue
Glomerulus
References
[1] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?mode=& term=Nephrons
[2] http:/ / education. yahoo. com/ reference/ gray/ subjects/ subject?id=253#p1223
[3] Ecology & Evolutionary Biology - University of Colorado at Boulder. "The Kidney Tubule I: Urine Production." URL: (http:/ / www.
colorado. edu/ eeb/ web_resources/ cartoons/ nephrex1. html). Accessed on: March 6, 2007.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulus
29
Glomerulus
Glomerulus
The glomerulus is the network (tuft) of capillaries in red. Blood flows in via the afferent arteriole and out via the efferent arteriole
(arrows). The round, double-walled structure in white is Bowman's capsule. The liquid component of blood (plasma)is filtered by
passing through the glomerular membrane, which consists of the capillary wall and the epithelial layer of Bowman's capsule. The
filtered blood leaves through the tubule at the top.
Distribution of bloodvessels in cortex of kidney.
Latin
glomerulus renis
Gray's
subject #253 1221
Precursor
Metanephric blastema
MeSH
Kidney+Glomerulus
[1]
[1]
In the kidney, a tubular structure called the nephron filters blood to form urine. At the beginning of the nephron, the
glomerulus /lmrls/ is a network (tuft) of capillaries that performs the first step of filtering blood.
The glomerulus is surrounded by Bowman's capsule. The blood plasma is filtered through the capillaries of the
glomerulus into the Bowman's capsule. The Bowman's capsule empties the filtrate into a tubule that is also part of
the nephron.
A glomerulus receives its blood supply from an afferent arteriole of the renal circulation. Unlike most other capillary
beds, the glomerulus drains into an efferent arteriole rather than a venule. The resistance of these arterioles results in
high pressure within the glomerulus, aiding the process of ultrafiltration, where fluids and soluble materials in the
blood are forced out of the capillaries and into Bowman's capsule.
A glomerulus and its surrounding Bowman's capsule constitute a renal corpuscle, the basic filtration unit of the
kidney. The rate at which blood is filtered through all of the glomeruli, and thus the measure of the overall renal
function, is the glomerular filtration rate (GFR).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulus
30
Afferent circulation
The afferent arteriole that supplies the capillaries of a glomerulus branches off an interlobular artery in the renal
cortex. Glomerular capillary pressure, and thus glomerular filtration rate, can be influenced by constriction or
relaxation of the afferent arteriole, resulting in decreases or increases in pressure. As an example, one study
involving rats found that having narrowed afferent arterioles contributed to the development of increased blood
pressure. Sympathetic nervous system action as well as hormones can also impact glomerular filtration rate by
modulating afferent arteriole diameter.
Layers
If a substance has passed through the glomerular capillary endothelial cells, glomerular basement membrane, and
podocytes, then it enters the lumen of the tubule and is known as glomerular filtrate. Otherwise, it exits the
glomerulus through the efferent arteriole and continues circulation as discussed below and as shown on the picture.
Endothelial cells
The endothelial cells of the glomerulus
contain numerous pores (fenestrae)
that, unlike those of other fenestrated
capillaries, are not spanned by
diaphragms.
The
cells
have
fenestrations that are 70 to 100 nm in
diameter. Since these pores are
relatively large, they allow for the free
filtration of fluid, plasma solutes and
protein. However they are not large
enough that red blood cells can be
filtered.
Glomerular basement
membrane
Scheme of filtration barrier (blood-urine) in the kidney. A. The endothelial cells of the
glomerulus; 1. pore (fenestra).
B. Glomerular basement membrane: 1. lamina rara interna 2. lamina densa 3. lamina rara
externa
C. Podocytes: 1. enzymatic and structural protein 2. filtration slit 3. diaphragma
The glomerular endothelium sits on a very thick (250350 nm) glomerular basement membrane.
Podocytes
Podocytes line the other side of the glomerular basement membrane and form part of the lining of Bowman's space.
Podocytes form a tight interdigitating network of foot processes (pedicels) that control the filtration of proteins from
the capillary lumen into Bowman's space.
The space between adjacent podocyte foot processes is spanned by a slit diaphragm formed by several proteins
including podocin and nephrin. In addition, foot processes have a negatively charged coat (glycocalyx) that limits the
filtration of negatively charged molecules, such as serum albumin.
The podocytes are sometimes considered the "visceral layer of Bowman's capsule", rather than part of the
glomerulus.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulus
31
Intraglomerular mesangial cell
Intraglomerular mesangial cells are found in the interstitium between endothelial cells of the glomerulus. They are
not part of the filtration barrier but are specialized pericytes that participate indirectly in filtration by contracting and
reducing the glomerular surface area, and therefore filtration rate, in response mainly to stretch.
Selectivity
The structures of the layers determine their permeability-selectivity permselectivity. The factors that influence
permselectivity are the negative charge of the basement membrane and the podocytic epithelium, and the effective
pore size of the glomerular wall (8nm). As a result, large and/or negatively charged molecules will pass through far
less frequently than small and/or positively charged ones. For instance, small ions such as sodium and potassium
pass freely, while larger proteins, such as hemoglobin and albumin have practically no permeability at all.
Efferent circulation
Blood is carried out of the glomerulus by an efferent arteriole instead of a venule, as is observed in most other
capillary systems. This provides tighter control over the blood flow through the glomerulus, since arterioles dilate
and constrict more readily than venules, owing to arterioles' larger smooth muscle layer (tunica media).
Efferent arterioles of juxtamedullary nephrons (i.e., the 15% of nephrons closest to the medulla) send straight
capillary branches that deliver isotonic blood to the renal medulla. Along with the loop of Henle, these vasa recta
play a crucial role in the establishment of the nephron's countercurrent exchange system.
The efferent arteriole, into which the glomerulus delivers blood, empties into an interlobular vein.
Juxtaglomerular cells
The walls of the afferent arteriole contain specialized smooth muscle cells that synthesize renin. These
juxtaglomerular cells play a major role in the renin-angiotensin system, which helps regulate blood volume and
pressure.
History
In 1666, Malpighi first described the glomeruli and demonstrated their continuity with the renal vasculature
(281,282). About 175 years later, Bowman elucidated in detail the capillary architecture of the glomerulus and the
continuity between its surrounding capsule and the proximal tubule .[2] .
Additional images
1 Glomerulus, 2
proximal tubule, 3 distal
tubule
Glomerulus.
Section of cortex of human
kidney.
Mouse glomerulus in the
Scanning Electron Microscope
("SEM"), magnification 1,000x
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulus
Mouse glomerulus in the
SEM, magnification 5,000x
32
Mouse glomerulus in the SEM
with one capillary broken,
magnification 10,000x
View on the inside of broken
capillary with fenestrae
visible, magnification
100,000x
Renal corpuscle
References
[1] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?mode=& term=Kidney+ Glomerulus
[2] "lippicotts histology for pathologesits; satcey e. mills
External links
Image and article at FGCU (http://coe.fgcu.edu/faculty/greenep/kidney/Glomerulus.html)
Histology at KUMC epithel-epith02 (http://www.kumc.edu/instruction/medicine/anatomy/histoweb/epithel/
epith02.htm) "Kidney (Glomerulus)"
Organology at UC Davis Urinary/mammal/cortex1/cortex1 (http://trc.ucdavis.edu/mjguinan/apc100/modules/
Urinary/mammal/cortex1/cortex1.html) - "Mammal, kidney cortex (LM, Medium)"
BU Histology Learning System: 16010loa (http://www.bu.edu/histology/p/16010loa.htm)
UNC Nephropathology (http://www.uncnephropathology.org)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Bowman's capsule
33
Bowman's capsule
Bowman's capsule
Glomerulus. (Bowman's capsule not labeled, but visible at top.)
Latin
capsula glomeruli
Gray's
subject #253 1222
Precursor
Metanephric blastema
MeSH
Bowman+Capsule
[1]
[2]
The Bowman's capsule (or capsula glomeruli, glomerular capsule) is a cup-like sac at the beginning of the tubular
component of a nephron in the mammalian kidney that performs the first step in the filtration of blood to form urine.
A glomerulus is enclosed in the sac. Fluids from blood in the glomerulus are collected in the Bowman's capsule (i.e.,
glomerular filtrate) and further processed along the nephron to form urine. This process is known as
ultrafiltration.[citation needed] The Bowman's capsule is named after Sir William Bowman, who identified it in 1842.
Anatomy
Outside the capsule, there are two "poles":
The vascular pole is the side with the afferent arteriole and efferent arteriole.
the urinary pole is the side with the proximal convoluted tubule.
Inside the capsule, the layers are as follows, from outside to inside:[citation needed]
Parietal layer -- A single layer of simple squamous epithelium. Does not function in filtration.
Bowman's space (or "urinary space", or "capsular space") -- Between the visceral and parietal layers, into which
the filtrate enters after passing through the filtration slits.
Visceral layer -- Lies just above the thickened glomerular basement membrane and is made of podocytes.
Beneath the visceral layer lie the glomerular capillaries.[citation needed]
Filtration barrier -- The filtration barrier is composed of the fenestrated endothelium of the glomerular
capillaries, the fused basal lamina of the endothelial cells and podocytes, and the filtration slits of the podocytes.
The barrier permits the passage of water, ions, and small molecules from the bloodstream into the Bowman's
space. The barrier prevents the passage of large and/or negatively charged proteins (such as albumin). The basal
lamina of the filtration barrier is composed of three layers. The first layer is the lamina rara externa, adjacent to
the podocyte processes. The second layer is the lamina rara interna, adjacent to the endothelial cells. The final
layer is the lamina densa which is a darker central zone of the basal lamina. It consists of the meshwork of type
IV collagen and laminin which act as a selective macromolecular filter.[citation needed]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Bowman's capsule
34
A - Renal corpuscle
B - Proximal tubule
C - Distal convoluted tubule
D - Juxtaglomerular apparatus
1. Basement membrane (Basal lamina)
2. Bowman's capsule - parietal layer
3. Bowman's capsule - visceral layer
3a. Pedicels (podocytes)
3b. Podocyte or sometimes called Bowman's
cells
4. Bowman's space (urinary space)
5a. Mesangium - Intraglomerular cell
5b. Mesangium - Extraglomerular cell
6. Granular cells (Juxtaglomerular cells)
7. Macula densa
8. Myocytes (smooth muscle)
9. Afferent arteriole
10. Glomerulus Capillaries
11. Efferent arteriole
Physiology
The process of filtration of the blood in the Bowman's capsule is ultrafiltration (or glomerular filtration), and the
normal rate of filtration is 125 ml/min, equivalent to 80 times the daily blood volume.[citation needed]
Any proteins under roughly 30 kilodaltons can pass freely through the membrane, although there is some extra
hindrance for negatively charged molecules due to the negative charge of the basement membrane and the
podocytes.[citation needed]
Any small molecules such as water, glucose, salt (NaCl), amino acids, and urea pass freely into Bowman's space, but
cells, platelets and large proteins do not.[citation needed]
As a result, the filtrate leaving the Bowman's capsule is very similar to blood plasma in composition as it passes into
the proximal convoluted tubule.[citation needed]
Clinical significance
Measuring the glomerular filtration rate (GFR) is a diagnostic test of kidney function.[citation needed]
A decreased GFR may be a sign of renal failure.[citation needed]
A number of diseases can result in various problems within the glomerulus. Examples include acute proliferative
(endocapillary)
glomerulonephritis,
mesangioproliferative
glomerulonephritis,
mesangiocapillary
(membranoproliferative)
glomerulonephritis,
acute
crescentic
glomerulonephritis,
focal
segmental
[citation needed]
glomerulonephritis, and diabetic glomerulosclerosis.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Bowman's capsule
35
Eponym
Bowman's capsule is named after Sir William Bowman (1816-1892), a British surgeon and anatomist.[citation needed]
Together with the glomerulus it is known as a renal corpuscle, or a Malpighian corpuscle, named after Marcello
Malpighi (1628-1694), an Italian physician and biologist. This name is not used widely anymore, probably to avoid
confusion with Malpighian bodies of the spleen.[citation needed]
Additional images
Distribution of blood vessels in cortex of
kidney.
Glomerulus.
References
[1] http:/ / education. yahoo. com/ reference/ gray/ subjects/ subject?id=253#p1222
[2] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?mode=& term=Bowman+ Capsule
External links
BU Histology Learning System: 16006loa (http://www.bu.edu/histology/p/16006loa.htm)
Diagram at ircc.edu (http://faculty.ircc.edu/faculty/tfischer/images/Bowman's capsule.jpg)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
Renal physiology
Renal physiology (Latin rns, "kidney") is
the study of the physiology of the kidney.
This encompasses all functions of the
kidney, including reabsorption of glucose,
amino acids, and other small molecules;
regulation of sodium, potassium, and other
electrolytes; regulation of fluid balance and
blood pressure; maintenance of acid-base
balance; the production of various hormones
including erythropoietin, and the activation
of vitamin D
Much of renal physiology is studied at the
This illustration demonstrates the normal kidney physiology. It also includes
level of the nephron, the smallest functional
illustrations showing where some types of diuretics act, and what they do.
unit of the kidney. Each nephron begins
with a filtration component that filters blood entering the kidney. This filtrate then flows along the length of the
nephron, which is a tubular structure lined by a single layer of specialized cells and surrounded by capillaries. The
major functions of these lining cells are the reabsorption of water and small molecules from the filtrate into the
blood, and the secretion of wastes from the blood into the urine.
Proper function of the kidney requires that it receives and adequately filters blood. This is performed at the
microscopic level by many hundreds of thousands of filtration units called renal corpuscles, each of which is
composed of a glomerulus and a Bowman's capsule. A global assessment of renal function is often ascertained by
estimating the rate of filtration, called the glomerular filtration rate (GFR).
Functions of the kidney
The functions of the kidney can be divided into three groups: secretion of hormones, gluconeogenesis and
extracellular homeostasis of pH and blood components. The nephron is the functional unit of the kidney.
Secretion of hormones
Secretion of erythropoietin, which regulates red blood cell production in the bone marrow.
Secretion of renin, which is a key part of the renin-angiotensin-aldosterone system.
Secretion of the active form of vitamin D (calcitriol) and prostaglandins.
36
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
37
Gluconeogenesis
The kidney in humans is capable of producing glucose from lactate, glycerol and glutamine. The kidney is
responsible for about half of the total gluconeogenesis in fasting humans. The regulation of glucose production in the
kidney is achieved by action of insulin, catecholamines and other hormones. Renal gluconeogenesis takes place in
the renal cortex. The renal medulla is incapable of producing glucose due to absence of necessary enzymes.
Extracellular homeostasis
The kidney is responsible for maintaining a balance of the following substances:
Substance
Description
Proximal tubule
Loop of Henle
Distal tubule
Collecting duct
Glucose
If glucose is not reabsorbed
by the kidney, it appears in
the urine, in a condition
known as glycosuria. This
is associated with diabetes
[1]
mellitus.
reabsorption (almost
100%) via
sodium-glucose transport
[2]
proteins (apical) and
GLUT (basolateral).
Oligopeptides,
proteins, and
amino acids
All are reabsorbed nearly
[3]
completely.
reabsorption
Urea
Regulation of osmolality.
[4][5]
Varies with ADH
reabsorption (50%) via
passive transport
secretion
reabsorption in medullary
collecting ducts
Sodium
Uses Na-H antiport,
Na-glucose symport,
sodium ion channels
[6]
(minor)
reabsorption (65%,
isosmotic)
reabsorption
(25%, thick
ascending,
Na-K-2Cl
symporter)
reabsorption (5%,
sodium-chloride
symporter)
reabsorption (5%,
principal cells), stimulated
by aldosterone via ENaC
Chloride
Usually follows sodium.
Active (transcellular) and
passive (paracellular)
reabsorption
reabsorption (thin reabsorption
ascending, thick (sodium-chloride
ascending,
symporter)
Na-K-2Cl
symporter)
Water
Uses aquaporin water
channels. See also diuretic.
absorbed osmotically
along with solutes
reabsorption
(descending)
reabsorption (regulated by
ADH, via arginine
vasopressin receptor 2)
Bicarbonate
Helps maintain acid-base
[7]
balance.
reabsorption (8090%)
[8]
reabsorption
(thick ascending)
[9]
reabsorption (intercalated
cells, via band 3 and
pendrin)
Protons
Uses vacuolar H+ATPase
secretion (intercalated
cells)
Potassium
Varies upon dietary needs.
reabsorption (65%)
reabsorption
(20%, thick
ascending,
Na-K-2Cl
symporter)
secretion (common, via
Na+/K+-ATPase,
increased by aldosterone),
or reabsorption (rare,
hydrogen potassium
ATPase)
Calcium
Uses calcium ATPase,
sodium-calcium exchanger
reabsorption
reabsorption
(thick ascending)
via passive
transport
reabsorption in
response to PTH and
reabsorption with
Thiazide Diuretics.
[10]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
38
Magnesium
Calcium and magnesium
reabsorption
compete, and an excess of
one can lead to excretion of
the other.
reabsorption
(thick ascending)
reabsorption
Phosphate
Excreted as titratable acid.
Carboxylate
reabsorption (85%) via
sodium/phosphate
cotransporter. Inhibited
by parathyroid hormone.
[11]
reabsorption (100%
via carboxylate
transporters.
The body is very sensitive to its pH. Outside the range of pH that is compatible with life, proteins are denatured and
digested, enzymes lose their ability to function, and the body is unable to sustain itself. The kidneys maintain
acid-base homeostasis by regulating the pH of the blood plasma. Gains and losses of acid and base must be balanced.
Acids are divided into "volatile acids"[12] and "nonvolatile acids".[13] See also titratable acid.
The major homeostatic control point for maintaining this stable balance is renal excretion. The kidney is directed to
excrete or retain sodium via the action of aldosterone, antidiuretic hormone (ADH, or vasopressin), atrial natriuretic
peptide (ANP), and other hormones. Abnormal ranges of the fractional excretion of sodium can imply acute tubular
necrosis or glomerular dysfunction.
Mechanisms
The kidney's ability to perform many of its
functions depends on the three fundamental
functions of filtration, reabsorption, and
secretion, whose sum is renal excretion.
That is:
Urinary excretion rate = Filtration rate
Reabsorption rate + Secretion
rate[14]
Filtration
The blood is filtered by nephrons, the
functional units of the kidney. Each nephron
begins in a renal corpuscle, which is
composed of a glomerulus enclosed in a
Bowman's capsule. Cells, proteins, and
other large molecules are filtered out of the
glomerulus by a process of ultrafiltration,
leaving an ultrafiltrate that resembles
plasma (except that the ultrafiltrate has
negligible plasma proteins) to enter
Bowman's space. Filtration is driven by
Starling forces.
Diagram showing the basic physiologic mechanisms of the kidney
The ultrafiltrate is passed through, in turn, the proximal convoluted tubule, the loop of Henle, the distal convoluted
tubule, and a series of collecting ducts to form urine.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
Reabsorption
Tubular reabsorption is the process by which solutes and water are removed from the tubular fluid and transported
into the blood. It is called reabsorption (and not absorption) because these substances have already been absorbed
once (particularly in the intestines).
Reabsorption is a two-step process beginning with the active or passive extraction of substances from the tubule fluid
into the renal interstitium (the connective tissue that surrounds the nephrons), and then the transport of these
substances from the interstitium into the bloodstream. These transport processes are driven by Starling forces,
diffusion, and active transport.
Indirect reabsorption
In some cases, reabsorption is indirect. For example, bicarbonate (HCO3-) does not have a transporter, so its
reabsorption involves a series of reactions in the tubule lumen and tubular epithelium. It begins with the active
secretion of a hydrogen ion (H+) into the tubule fluid via a Na/H exchanger:
In the lumen
The H+ combines with HCO3- to form carbonic acid (H2CO3)
Luminal carbonic anhydrase enzymatically converts H2CO3 into H2O and CO2
CO2 freely diffuses into the cell
In the epithelial cell
Cytoplasmic carbonic anhydrase converts the CO2 and H2O (which is abundant in the cell) into H2CO3
H2CO3 readily dissociates into H+ and HCO3 HCO3- is facilitated out of the cell's basolateral membrane
Hormones
Some key regulatory hormones for reabsorption include:
aldosterone, which stimulates active sodium reabsorption (and water as a result)
antidiuretic hormone, which stimulates passive water reabsorption
Both hormones exert their effects principally on the collecting ducts.
Secretion
Tubular secretion is the transfer of materials from peritubular capillaries to renal tubular lumen. Tubular secretion is
caused mainly by active transport.
Usually only a few substances are secreted. These substances are present in great excess, or are natural poisons.
Many drugs are eliminated by tubular secretion. Further reading: Table of medication secreted in kidney
Measurement of renal function
A simple means of estimating renal function is to measure pH, blood urea nitrogen, creatinine, and basic electrolytes
(including sodium, potassium, chloride, and bicarbonate). As the kidney is the most important organ in controlling
these values, any derangement in these values could suggest renal impairment.
There are several more formal tests and ratios involved in estimating renal function:
39
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
Measurement
40
Calculation
Details
renal plasma
flow
Volume of blood plasma delivered to the kidney per unit time.
PAH clearance is a renal analysis method used to provide an
estimate. Approximately 625 ml/min.
[15]
renal blood flow
Volume of blood delivered to the kidney per unit time. In humans,
the kidneys together receive roughly 20% of cardiac output,
amounting to 1 L/min in a 70-kg adult male.
(HCT is hematocrit)
glomerular
filtration rate
(estimation using creatinine
clearance)
filtration fraction
anion gap
Measures portion of renal plasma that is filtered.
[16]
AG = [Na+] ([Cl] + [HCO3])
Clearance (other
than water)
Volume of fluid filtered from the renal glomerular capillaries into
the Bowman's capsule per unit time. Estimated using inulin.
Usually a creatinine clearance test is performed but other markers,
such as the plant polysaccharide inulin or radiolabelled EDTA,
may be used as well.
Cations minus anions. Excludes K+ (usually), Ca2+, H2PO4. Aids
in the differential diagnosis of metabolic acidosis
Rate of removal
where U = concentration, V =urine volume /
time, U*V = urinary excretion, and P = plasma
[17]
concentration
free water
clearance
Net acid
excretion
or
[18]
The volume of blood plasma that is cleared of solute-free water
per unit time.
Net amount of acid excreted in the urine per unit time
References
[1] Sect. 7, Ch. 6: Characteristics of Proximal Glucose Reabsorption (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg.
edu/ edu/ eshuphysio/ program/ section7/ 7ch06/ 7ch06p11. htm). lib.mcg.edu
[2] Sect. 7, Ch. 5: Cotransport (Symport) (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg. edu/ edu/ eshuphysio/
program/ section7/ 7ch05/ 7ch05p13. htm). lib.mcg.edu
[3] Sect. 7, Ch. 6: Proximal Reabsorption of Amino Acids: Site of Reabsorption (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www.
lib. mcg. edu/ edu/ eshuphysio/ program/ section7/ 7ch06/ 7ch06p17. htm). lib.mcg.edu
[4] Sect. 7, Ch. 6: Proximal Reabsorption of Urea (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg. edu/ edu/
eshuphysio/ program/ section7/ 7ch06/ 7ch06p10. htm). lib.mcg.edu
[5] V. Excretion of Organic Molecules (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www2. kumc. edu/ ki/ physiology/ course/ five/
5_1. htm). lib.mcg.edu
[6] VI. Mechanisms of Salt & Water Reabsorption (http:/ / www2. kumc. edu/ ki/ physiology/ course/ six/ 6_1. htm)
[7] Sect. 7, Ch. 6: Proximal Reabsorption of Bicarbonate (http:/ / web. archive. org/ web/ 20070219065040/ http:/ / lib. mcg. edu/ edu/
eshuphysio/ program/ section7/ 7ch06/ 7ch06p08. htm). lib.mcg.edu
[8] Sect. 7, Ch. 12: Proximal Tubular Reabsorption of Bicarbonate (http:/ / web. archive. org/ web/ 20070715121612/ http:/ / www. lib. mcg. edu/
edu/ eshuphysio/ program/ section7/ 7ch12/ 7ch12p21. htm). lib.mcg.edu
[9] Sect. 7, Ch. 12: Bicarbonate Reabsorption, Thick Limb of Henles Loop (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib.
mcg. edu/ edu/ eshuphysio/ program/ section7/ 7ch12/ 7ch12p22. htm). lib.mcg.edu
[10] en.wikipedia.org/wiki/Distal_convoluted_tubule
[11] Page 799
[12] Sect. 7, Ch. 12: Physiological Definition of Acids: Volatile Acid (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg.
edu/ edu/ eshuphysio/ program/ section7/ 7ch12/ 7ch12p12. htm). lib.mcg.edu
[13] Sect. 7, Ch. 12: Nonvolatile Acids (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg. edu/ edu/ eshuphysio/ program/
section7/ 7ch12/ 7ch12p13. htm). lib.mcg.edu
[14] p 314, Guyton and Hall, Medical Physiology, 11th edition
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal physiology
41
[15] Sect. 7, Ch. 4: Measurement of Renal Plasma Flow; Renal Clearance of PAH (http:/ / web. archive. org/ web/ 20070715122822/ http:/ /
www. lib. mcg. edu/ edu/ eshuphysio/ program/ section7/ 7ch04/ 7ch04p28. htm). lib.mcg.edu
[16] Sect. 7, Ch. 4: Filtration Fraction (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg. edu/ edu/ eshuphysio/ program/
section7/ 7ch04/ 7ch04p17. htm). lib.mcg.edu
[17] IV. Measurement of Renal Function (http:/ / web. archive. org/ web/ 20090124041511/ http:/ / www2. kumc. edu/ ki/ physiology/ course/
four/ 4_2. htm). kumc.edu
[18] Sect. 7, Ch. 8: Free water clearance (CH2O) (http:/ / web. archive. org/ web/ 20070715122822/ http:/ / www. lib. mcg. edu/ edu/ eshuphysio/
program/ section7/ 7ch08/ 7ch08p21. htm). lib.mcg.edu
Renal glucose reabsorption
Renal glucose reabsorption is the part of renal physiology that deals with the retrieval of filtered glucose,
preventing it from disappearing from the body through the urine.
If glucose is not reabsorbed by the kidney, it appears in the urine, in a condition known as glucosuria. This is
associated with diabetes mellitus.[1]
Selective Reabsorption of glucose is achieved by a combination of processes.
Firstly, the glucose in the proximal tubule is co-transported with sodium ions into the proximal convoluted tubule
walls. Some (typically smaller) amino acids are also transported in this way. Once in the tubule wall, the glucose and
amino acids diffuse directly into the blood capillaries along a concentration gradient. This blood is flowing, so the
gradient is maintained. Lastly, sodium/potassium ion active transport pumps remove sodium from the tubule wall
and the sodium is put back into the blood. This maintains a sodium concentration gradient in the proximal tubule
lining, so the first step continues to happen.
Overview table
Characteristics of Glucose reabsorption
Characteristic
proximal tubule
S1
reabsorption (%)
S2
[2]
98
loop of Henle Distal convoluted tubule Collecting duct system
S3
Beyond the Distal convoluted tubule: 2%
reabsorption (mmoles/day)
Concentration
apical transport proteins
SGLT2
SGLT1
basolateral transport proteins
GLUT2
GLUT1
Other reabsorption features
References
[1] Sect. 7, Ch. 6: Characteristics of Proximal Glucose Reabsorption (http:/ / www. lib. mcg. edu/ edu/ eshuphysio/ program/ section7/ 7ch06/
7ch06p11. htm)
[2] Page 793
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal sodium reabsorption
Renal sodium reabsorption
Renal reabsorption of sodium (Na+) is a part of renal physiology. It uses Na-H antiport, Na-glucose symport,
sodium ion channels (minor).[1] It is stimulated by angiotensin II and aldosterone, and inhibited by atrial natriuretic
peptide.
It is very efficient, since more than 25,000 mmoles/day of sodium is filtered into the nephron, but only ~100
mmoles/day, or less than 0.4% remains in the final urine.
Proximal tubule
Most of the reabsorption (65%) occurs in the proximal tubule. In the latter part it is favoured by an electrochemical
driving force, but initially it needs the cotransporter SGLT and the Na-H antiporter. Water is reabsorbed to the same
degree, resulting in the concentration in the end of the proximal tubule being the same as in the beginning. In other
words, the reabsorption in the proximal tubule is isosmotic.
Loop of Henle
Sodium is reabsorbed in the thick ascending limb of loop of Henle, by Na-K-2Cl symporter and Na-H antiporter. It
goes against its chemical driving force, but the high electrical driving force renders the overall electrochemical
driving force positive anyway, availing some sodium to diffuse passively either the transcellular or paracellular way.
Distal tubule
In the distal convoluted tubule sodium is transported against an electrochemical gradient by sodium-chloride
symporters.
Collecting duct
The principal cells are the sodium-transporting cells in the collecting duct system.
Regulation
Although only a fragment of total reabsorption happens here, it is the main part of intervention. This is e.g. done by
endogenous production of aldosterone, increasing reabsorption. Since the normal excretion rate of sodium is
~100mmoles/day, then a regulation of the absorption of still more than 1000 mmoles/day entering the collecting duct
system has a substantial influence of the total sodium excreted.
Overview table
42
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal sodium reabsorption
43
Characteristics of Na+ reabsorption
Characteristic
proximal tubule
S1
S2 S3
reabsorption
(%)
67%
reabsorption
(mmoles/day)
~17,000
Concentration
(mM)
142
electrical
driving force
(mV)
chemical
driving force
(mV)
loop of Henle
descending thin
limb
ascending
limb
Distal
convoluted
tubule
thick
ascending
limb
Collecting duct system
connecting initial
cortical
medullary
tubule
collecting collecting collecting
tubule
ducts
ducts
25%
5%
3%
~6,400
~1,300
~700
142
100
70
40
-3
+3
+15
-5 to +5
-40
-9
-19
-34
+3
+6
-24 to -14
-74
[]
[2]
electrochemical -3
driving force
(mV)
apical transport
proteins
SGLT,
Na-H
[3]
antiporter
basolateral
transport
proteins
Na+/K+-ATPase
Other
reabsorption
features
isosmotic
(passively) Na-K-2Cl sodium-chloride
symporter symporter
(Na-H
antiporter
and
passively)
ENaC
by principal cells, stimulated by aldosterone
References
[1] VI. Mechanisms of Salt & Water Reabsorption (http:/ / www2. kumc. edu/ ki/ physiology/ course/ six/ 6_1. htm)
[2] Page 777
[3] Page 778
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal chloride reabsorption
44
Renal chloride reabsorption
Renal reabsorption of chloride (Cl) is a part of renal physiology, in order not to lose too much chloride in the
urine.
Overview table
Characteristics of Cl reabsorption
Characteristic
proximal tubule
S1
S2 S3
loop of Henle
Distal
convoluted
tubule
descending thin
thick ascending
limb
ascending limb
limb
Collecting duct system
connecting initial
cortical
tubule
collecting collecting ducts
tubule
reabsorption
(%)
reabsorption
(mmoles/day)
Concentration
(mM)
115
electrical
driving force
(mV)
[1]
135
+3
+15
5 to +5
40
chemical
driving force
(mV)
electrochemical (positive)
[2]
driving force
(mV)
apical transport (passively)
proteins
Cl-formate
exchanger
Cl-oxalate
exchanger
Cl/HCO3
exchanger
Cl-OH
exchanger
Na-K-2Cl
cotransporter
Na-Cl
cotransporter
chloride
channels
chloride
channels
chloride
channels
Cl-K
[]
cotransporter
chloride channels
intercalated
cells: ClHCO3
exchanger
basolateral
transport
proteins
Other
reabsorption
features
principal
cells:
paracellularily
medullary
collecting
ducts
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal chloride reabsorption
45
References
[1] Page 777
[2] Page 779
Renal protein reabsorption
Renal protein reabsorption is the part of renal physiology that deals with the retrieval of filtered proteins,
preventing them from disappearing from the body through the urine.
Almost all reabsorption takes place in the proximal tubule. Only ~1% is left in the final urine.
The proteins cross the apical membrane by endocytosis. They are subsequently degraded in lysosomes. The
remaining free amino acids are transported across the basolateral membrane by amino acid transporters.
Overview table
Characteristics of oligopeptide reabsorption
Characteristic
proximal tubule
S1
reabsorption (%)
S2
loop of Henle Distal convoluted tubule Collecting duct system
S3
[]
99
reabsorption (mmoles/day)
Concentration
apical transport
basolateral transport proteins
Other reabsorption features
References
endocytosis
amino acid transporter
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal tubular acidosis
46
Renal tubular acidosis
Renal tubular acidosis
Classification and external resources
Significant bilateral nephrocalcinosis (calcification of the kidneys) on a frontal X-ray (radiopacities (white) in the right upper and left upper
quadrant of the image), as seen in distal renal tubular acidosis.
[1]
ICD-10
N25.8
ICD-9
588.89
OMIM
179800
DiseasesDB
11687
eMedicine
med/1071
MeSH
D000141
[2]
[3]
[4]
11673
[5]
11705
[6]
[7]
[8]
Renal tubular acidosis (RTA) is a medical condition that involves an accumulation of acid in the body due to a
failure of the kidneys to appropriately acidify the urine. When blood is filtered by the kidney, the filtrate passes
through the tubules of the nephron, allowing for exchange of salts, acid equivalents, and other solutes before it drains
into the bladder as urine. The metabolic acidosis that results from RTA may be caused either by failure to recover
sufficient (alkaline) bicarbonate ions from the filtrate in the early portion of the nephron (proximal tubule) or by
insufficient secretion of (acid) hydrogen ions into the latter portions of the nephron (distal tubule). Although a
metabolic acidosis also occurs in those with renal insufficiency, the term RTA is reserved for individuals with poor
urinary acidification in otherwise well-functioning kidneys. Several different types of RTA exist, which all have
different syndromes and different causes.
The word acidosis refers to the tendency for RTA to lower the blood's pH. When the blood pH is below normal
(7.35), this is called acidemia. The metabolic acidosis caused by RTA is a normal anion gap acidosis.
An overview of types 1, 2, and 4 is presented below (type 3 is usually excluded from modern classifications):
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal tubular acidosis
Type
47
Type 1
Type 2
Type 4
Location
Distal tubules
Proximal tubules
Adrenal
Acidosis?
Yes (severe)
Yes
Mild when present
Potassium
Hypokalemia
Hypokalemia
Hyperkalemia
Failed HCO3 reabsorption from the
urine by the proximal tubular cells
Deficiency of aldosterone, or a resistance to its effects,
(hypoaldosteronism or pseudohypoaldosteronism)
Pathophysiology Failure of H+ secretion by
the intercalated cells
Type 1-Distal RTA
Distal RTA (dRTA) is the classical form of RTA, being the first
described. Distal RTA is characterized by a failure of acid secretion by
the alpha intercalated cells of the cortical collecting duct of the distal
nephron. This failure of acid secretion may be due to a number of
causes, and it leads to an inability to acidify the urine to a pH of less
than 5.3. Because renal excretion is the primary means of eliminating
acid from the body, there is consequently a tendency towards acidemia.
There is an inability to excrete H+
while K+
cannot be reabsorbed, leading to acidemia (as H+
builds up in the body) and hypokalemia (as K+
cannot be reabsorbed). This leads to the clinical features of dRTA; In
other words, the intercalated cells' apical H+/K+ antiporter is
non-functional, resulting in potassium-wasting and proton retention.
Since calcium stones demonstrate a proclivity for deposition at higher
pHs (alkaline), the substance of the kidney develops stones bilaterally;
this does not occur in the other RTA types.
Normal anion gap metabolic acidosis/acidemia
Hypokalemia
Urinary stone formation (related to alkaline urine, hypercalciuria,
and low urinary citrate).
Radiograph of a child with rickets, a complication
of both distal and proximal RTA.
Nephrocalcinosis (deposition of calcium in the substance of the kidney)
Bone demineralisation (causing rickets in children and osteomalacia in adults)
Type 2-Proximal RTA
Proximal RTA (pRTA) is caused by a failure of the proximal tubular cells to reabsorb filtered bicarbonate from the
urine, leading to urinary bicarbonate wasting and subsequent acidemia. The distal intercalated cells function
normally, so the acidemia is less severe than dRTA and the urine can acidify to a pH of less than 5.3. pRTA also has
several causes, and may occasionally be present as a solitary defect, but is usually associated with a more
generalized dysfunction of the proximal tubular cells called Fanconi's syndrome, in which there is also phosphaturia,
glycosuria, aminoaciduria, uricosuria, and tubular proteinuria. The principal feature of Fanconi's syndrome is bone
demineralization (osteomalacia or rickets) due to phosphate wasting.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal tubular acidosis
48
Type 3 RTA-Combined proximal and distal RTA
In some patients, RTA shares features of both dRTA and pRTA. This rare pattern was observed in the 1960s and
1970s as a transient phenomenon in infants and children with dRTA (possibly in relation with some exogenous
factor such as high salt intake) and is no longer observed. This form of RTA has also been referred to as juvenile
RTA.
Combined dRTA and pRTA is also observed as the result of inherited carbonic anhydrase II deficiency. Mutations in
the gene encoding this enzyme give rise to an autosomal recessive syndrome of osteopetrosis, renal tubular acidosis,
cerebral calcification, and mental retardation. It is very rare and cases from all over the world have been reported, of
which about 70% are from the Magreb region of North Africa, possibly due to the high prevalence of consanguinity
there. The kidney problems are treated as described above. There is no treatment for the osteopetrosis or cerebral
calcification.
Type 3 is rarely discussed. Most comparisons of RTA are limited to a comparison of types 1, 2, and 4.
Type 4 RTA
Type 4 RTA is not actually a tubular disorder at all nor does it have a
clinical syndrome similar to the other types of RTA described above. It
was included in the classification of renal tubular acidoses as it is
associated with a mild (normal anion gap) metabolic acidosis due to a
physiological reduction in proximal tubular ammonium excretion
(impaired ammoniagenesis), which is secondary to hypoaldosteronism,
and results in a decrease in urine buffering capacity. Its cardinal feature
is hyperkalemia, and measured urinary acidification is normal, hence it
is often called hyperkalemic RTA or tubular hyperkalemia.
Causes include:
Type 4 RTA is due either to a deficiency of
Aldosterone, or to a resistance to its effects.
Aldosterone deficiency (hypoaldosteronism): Primary vs.
hyporeninemic
Aldosterone resistance
1. Drugs: NSAIDs, ACE inhibitors and ARBs, Eplerenone, Spironolactone, Trimethoprim, Pentamidine
2. Pseudohypoaldosteronism
History
Renal tubular acidosis was first described in 1935 by Lightwood and 1936 by Butler et al. in children. Baines et al.
first described it in adults in 1945.
It has been postulated the Dickens character, Tiny Tim in A Christmas Carol, was suffering from renal tubular
acidosis. [9]
References
[1]
[2]
[3]
[4]
[5]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N25. 8
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=588. 89
http:/ / omim. org/ entry/ 179800
http:/ / www. diseasesdatabase. com/ ddb11687. htm
http:/ / www. diseasesdatabase. com/ ddb11673. htm
[6] http:/ / www. diseasesdatabase. com/ ddb11705. htm
[7] http:/ / www. emedicine. com/ med/ topic1071. htm
[8] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D000141
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal tubular acidosis
49
[9] http:/ / www. ncbi. nlm. nih. gov/ pubmed/ 1340779
Proximal renal tubular acidosis
Proximal renal
tubular acidosis
Classification and external resources
[1]
OMIM
179830
DiseasesDB
11687
MedlinePlus
000497
MeSH
D000141
[4]
[2]
[8]
Proximal renal tubular acidosis (pRTA) or Type 2 Renal tubular acidosis (RTA) is a type of RTA caused by a
failure of the proximal tubular cells to reabsorb filtered bicarbonate from the urine, leading to urinary bicarbonate
wasting and subsequent acidemia. The distal intercalated cells function normally, so the acidemia is less severe than
dRTA and the urine can acidify to a pH of less than 5.3. pRTA also has several causes, and may occasionally be
present as a solitary defect, but is usually associated with a more generalised dysfunction of the proximal tubular
cells called Fanconi's syndrome where there is also phosphaturia, glycosuria, aminoaciduria, uricosuria and tubular
proteinuria. The principal feature of Fanconi's syndrome is bone demineralization (osteomalacia or rickets) due to
phosphate wasting.
Causes
Familial disorders
Cystinosis
Galactosemia
Glycogen storage disease (type I)
Hereditary fructose intolerance
Lowe syndrome
Tyrosinemia
Wilson's disease
Acquired disorders
Amyloidosis
Multiple myeloma
Paroxysmal nocturnal hemoglobinuria
Toxins, such as HAART, ifosfamide, lead, and cadmium
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Proximal renal tubular acidosis
Treatment
Again this depends on oral bicarbonate supplementation. However, this will increase urinary bicarbonate wasting
and may well promote a bicarbonate diuresis. The amount of bicarbonate given may have to be very large, to stay
ahead of the urinary losses. Correction with oral bicarbonate may exacerbate urinary potassium losses and precipitate
hypokalemia. As with dRTA, reversal of the chronic acidosis should reverse bone demineralization.
Thiazide diuretics can also be used as treatment by making use of contraction alkalosis caused by them.
References
[1] http:/ / omim. org/ entry/ 179830
[2] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000497. htm
50
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Distal renal tubular acidosis
51
Distal renal tubular acidosis
Distal renal tubular
acidosis
Classification and external resources
[3]
OMIM
179800
MedlinePlus
000493
MeSH
D000141
[1]
[8]
Distal renal tubular acidosis (dRTA) or Type 1 Renal tubular
acidosis (RTA) is the classical form of RTA, being the first described.
Distal RTA is characterized by a failure of acid secretion by the alpha
intercalated cells of the cortical collecting duct of the distal nephron.
This failure of acid secretion may be due to a number of causes, and it
leads to an inability to acidify the urine to a pH of less than 5.3.
Symptoms
Because renal excretion is the primary means of eliminating acid from
the body, there is consequently a tendency towards acidemia. This
leads to the clinical features of dRTA;.
Normal anion gap metabolic acidosis/acidemia
Hypokalemia
Urinary stone formation (related to alkaline urine, hypercalciuria,
and low urinary citrate).
Nephrocalcinosis (deposition of calcium in the substance of the
kidney)
Bone demineralisation (causing rickets in children and osteomalacia
in adults)
Radiograph of a rickets sufferer, a complication
of both distal and proximal RTA.
The symptoms and sequelae of dRTA are variable and range from being completely asymptomatic, to loin pain and
hematuria from kidney stones, to failure to thrive and severe rickets in childhood forms as well as possible renal
failure and even death.
dRTA commonly leads to sodium loss and volume contraction, which causes a compensatory increase in blood
levels of aldosterone. Aldosterone causes increased resorption of sodium and loss of potassium in the collecting duct
of the kidney, so these increased aldosterone levels cause the hypokalemia which is a common symptom of dRTA.
Diagnosis
The acidosis is variable, and one may have dRTA with alpha intercalated cell failure without necessarily being
acidemic; this is termed incomplete dRTA. The diagnosis of dRTA can be made by the observation of a urinary pH of
greater than 5.3 in the face of a systemic acidemia (usually taken to be a serum bicarbonate of 20 mmol/l or less). In
the case of an incomplete dRTA, failure to acidify the urine following an oral acid loading challenge is often used as
a test. The test usually performed is the short ammonium chloride test, in which ammonium chloride capsules are
used as the acid load. More recently, an alternative test using furosemide and fludrocortisone has been described.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Distal renal tubular acidosis
52
Interestingly, dRTA has been proposed as a possible diagnosis for the unknown malady plaguing Tiny Tim in
Charles Dickens' A Christmas Carol.
Causes
Autoimmune disease. Classically Sjgren's syndrome, but it is also
associated with systemic lupus erythematosus, rheumatoid arthritis
and even hypergammaglobulinemia. Hypokalaemia is often severe
in these cases.
Hereditary causes include mutations of Band 3 the basolateral
bicarbonate transporter of the intercalated cell, which may be
transmitted in an autosomal dominant fashion in western European
cases, or in an autosomal recessive fashion in South East Asian
cases. The South East Asian cases are associated with more severe
hypokalemia. Other hereditary causes include mutations of subunits
of the apical proton pump vH+-ATPase, which are transmitted in an
autosomal recessive fashion, and may be associated with
sensorineural deafness.
Diagram depicting an alpha intercalated cell with
the apical proton pump and basolateral band 3
(kAE1)
Liver cirrhosis.
Nephrocalcinosis. While it is a consequence of dRTA, it can also be a cause; related to calcium-induced damage
of the cortical collecting duct.
Renal transplantation.
Sickle cell anemia.
Toxins, including ifosfamide (more commonly causing pRTA than dRTA), toluene, lithium carbonate and
amphotericin B.
Chronic urinary tract obstruction.
Possible side effect of IV-administered bisphosphonates, such as zoledronate (~10%)
Treatment
This is relatively straightforward. It involves correction of the acidemia with oral sodium bicarbonate, sodium citrate
or potassium citrate. This will correct the acidemia and reverse bone demineralisation. Hypokalemia and urinary
stone formation and nephrocalcinosis can be treated with potassium citrate tablets which not only replace potassium
but also inhibit calcium excretion and thus do not exacerbate stone disease as sodium bicarbonate or citrate may do.
References
[1] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000493. htm
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Renal urea handling
53
Renal urea handling
Renal urea handling is the part of renal physiology that deals with the reabsorption and secretion of urea.
Movement of large amounts of urea across cell membranes is made possible by urea transporter proteins.
Urea allows the kidneys to create hyperosmotic urine (urine that has more ions in it - is "more concentrated" - than
that same person's blood plasma). Preventing the loss of water in this manner is important if the person's body must
save water in order to maintain a suitable blood pressure or (more likely) in order to maintain a suitable
concentration of sodium ions in the blood plasma.
About 40% of the urea filtered is normally found in the final urine, since there is more reabsorption than secretion
along the nephron.
It is regulated by antidiuretic hormone, which controls the amount reabsorbed in the collecting duct system and
secreted into the loop of Henle.
Overview table
Characteristic
proximal
tubule
S1
S2
S3
loop of Henle
descending
limb
thin ascending thick
limb
ascending
limb
Distal
convoluted
tubule
Collecting duct system
connecting initial
cortical
medullary
tubule
collecting collecting collecting
tubule
ducts
ducts
reabsorption (% 50[]
compared to
filtered amount)
70
secretion (%
compared to
filtered amount)
60
reabsorption
(mmoles/day)
Concentration
electrical
driving force
(mV)
[1]
-3
+3
+15
-5 to +5
-40
chemical
driving force
(mV)
electrochemical
driving force
(mV)
apical transport
proteins
solvent drag
unknown
transporter
Urea
transporter
2?
unknown
transporter
urea
transporter
1
basolateral
transport
proteins
unknown
transporter
Urea
transporter
2?
unknown
transporter
urea
transporter
4
Other
reabsorption
features
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Ammonia
68
Ammonia
Redox properties of liquid ammonia
E (V, ammonia) E (V, water)
Li+ + e Li
2.24
3.04
K+ + e K
1.98
2.93
Na+ + e Na
1.85
2.71
Zn2+ + 2e Zn
0.53
0.76
NH4+ + e H2 + NH3
0.00
Cu2+ + 2e Cu
+0.43
+0.34
Ag+ + e Ag
+0.83
+0.80
The range of thermodynamic stability of liquid ammonia solutions is very narrow, as the potential for oxidation to
dinitrogen, E (N2 + 6NH4+ + 6e 8NH3), is only +0.04V. In practice, both oxidation to dinitrogen and reduction
to dihydrogen are slow. This is particularly true of reducing solutions: the solutions of the alkali metals mentioned
above are stable for several days, slowly decomposing to the metal amide and dihydrogen. Most studies involving
liquid ammonia solutions are done in reducing conditions; although oxidation of liquid ammonia is usually slow,
there is still a risk of explosion, particularly if transition metal ions are present as possible catalysts.
Ammonia's role in biological systems and human disease
Ammonia is an important source of nitrogen for living
systems. Although atmospheric nitrogen abounds (more
than 75%), few living creatures are capable of using
this nitrogen. Nitrogen is required for the synthesis of
amino acids, which are the building blocks of protein.
Some plants rely on ammonia and other nitrogenous
wastes incorporated into the soil by decaying matter.
Others, such as nitrogen-fixing legumes, benefit from
symbiotic relationships with rhizobia that create
ammonia from atmospheric nitrogen.
Biosynthesis
In certain organisms, ammonia is produced from
atmospheric nitrogen by enzymes called nitrogenases.
Main symptoms of hyperammonemia (ammonia reaching toxic
The overall process is called nitrogen fixation.
concentrations).
Although it is unlikely that biomimetic methods that
are competitive with the Haber process will be
developed, intense effort has been directed toward understanding the mechanism of biological nitrogen fixation. The
scientific interest in this problem is motivated by the unusual structure of the active site of the enzyme, which
consists of an Fe MoS ensemble.
7
Ammonia is also a metabolic product of amino acid deamination catalyzed by enzymes such as glutamate
dehydrogenase 1. Ammonia excretion is common in aquatic animals. In humans, it is quickly converted to urea,
which is much less toxic, particularly less basic. This urea is a major component of the dry weight of urine. Most
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Ammonia
reptiles, birds, insects, and snails excrete uric acid solely as nitrogenous waste.
In physiology
Ammonia also plays a role in both normal and abnormal animal physiology. It is biosynthesised through normal
amino acid metabolism and is toxic in high concentrations. The liver converts ammonia to urea through a series of
reactions known as the urea cycle. Liver dysfunction, such as that seen in cirrhosis, may lead to elevated amounts of
ammonia in the blood (hyperammonemia). Likewise, defects in the enzymes responsible for the urea cycle, such as
ornithine transcarbamylase, lead to hyperammonemia. Hyperammonemia contributes to the confusion and coma of
hepatic encephalopathy, as well as the neurologic disease common in people with urea cycle defects and organic
acidurias.
Ammonia is important for normal animal acid/base balance. After formation of ammonium from glutamine,
-ketoglutarate may be degraded to produce two molecules of bicarbonate, which are then available as buffers for
dietary acids. Ammonium is excreted in the urine, resulting in net acid loss. Ammonia may itself diffuse across the
renal tubules, combine with a hydrogen ion, and thus allow for further acid excretion.
Excretion
Ammonium ions are a toxic waste product of the metabolism in animals. In fish and aquatic invertebrates, it is
excreted directly into the water. In mammals, sharks, and amphibians, it is converted in the urea cycle to urea,
because it is less toxic and can be stored more efficiently. In birds, reptiles, and terrestrial snails, metabolic
ammonium is converted into uric acid, which is solid, and can therefore be excreted with minimal water loss.
Reference ranges for blood tests, comparing blood content of ammonia (shown in yellow near middle) with other
constituents
69
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Ammonia
References
"Aqua Ammonia" (http://www.airgasspecialtyproducts.com/Libraries/
Aqua_Ammonia_Technical_Data_Manual/Physical_Properties.sflb.ashx). airgasspecialtyproducts.com.
Archived (http://web.archive.org/web/20101119084300/http://airgasspecialtyproducts.com/Libraries/
Aqua_Ammonia_Technical_Data_Manual/Physical_Properties.sflb.ashx) from the original on 19 November
2010. Retrieved 28 November 2010.
Attribution
This articleincorporates text from a publication now in the public domain:Chisholm, Hugh, ed. (1911).
"Ammonia" (http://www.1911encyclopedia.com/Ammonia). Encyclopdia Britannica (11th ed.). Cambridge
University Press
Further reading
Bretherick, L., ed. (1986). Hazards in the Chemical Laboratory (4th ed.). London: Royal Society of Chemistry.
ISBN0-85186-489-9. OCLC 16985764 (http://www.worldcat.org/oclc/16985764).
Greenwood, Norman N.; Earnshaw, Alan (1997). Chemistry of the Elements (2nd ed.). ButterworthHeinemann.
ISBN0080379419.
Housecroft, C. E.; Sharpe, A. G. (2000). Inorganic Chemistry (1st ed.). New York: Prentice Hall.
ISBN978-0582310803.
Weast, R. C., ed. (1972). Handbook of Chemistry and Physics (53rd ed.). Cleveland, OH: Chemical Rubber Co.
External links
International Chemical Safety Card 0414 (http://www.inchem.org/documents/icsc/icsc/eics0414.htm)
(anhydrous ammonia), ilo.org.
International Chemical Safety Card 0215 (http://www.inchem.org/documents/icsc/icsc/eics0215.htm)
(aqueous solutions), ilo.org.
CID 222 (http://pubchem.ncbi.nlm.nih.gov/summary/summary.cgi?cid=222) from PubChem
"Ammoniac et solutions aqueuses" (http://www.inrs.fr/fichetox/ft16.html). Institut National de Recherche et
de Scurit. (French)
Emergency Response to Ammonia Fertilizer Releases (Spills) (http://www.ammoniaspills.org/) for the
Minnesota Department of Agriculture.ammoniaspills.org
National Institute for Occupational Safety and Health Ammonia Page (http://www.cdc.gov/niosh/topics/
ammonia), cdc.gov
NIOSH Pocket Guide to Chemical Hazards - Ammonia (http://www.cdc.gov/niosh/npg/npgd0028.html),
cdc.gov
73
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
74
Urine
Urine (from Latin Urina, ae, f.) is a typically sterile liquid by-product of the body secreted by the kidneys through a
process called urination and excreted through the urethra. Cellular metabolism generates numerous by-products,
many rich in nitrogen, that require elimination from the bloodstream. These by-products are eventually expelled
from the body during urination, the primary method for excreting water-soluble chemicals from the body. These
chemicals can be detected and analyzed by urinalysis. Certain disease conditions can result in
pathogen-contaminated urine.[1]
Physiology
Most animals have excretory systems for elimination of soluble toxic
wastes. In humans, soluble wastes are excreted primarily by the urinary
system and, to a lesser extent in terms of urea removed, by
perspiration. The urinary system consists of the kidneys, ureters,
urinary bladder, and urethra. The system produces urine by a process
of filtration, reabsorption, and tubular secretion. The kidneys extract
the soluble wastes from the bloodstream, as well as excess water,
sugars, and a variety of other compounds. The resulting urine contains
high concentrations of urea and other substances, including toxins.
Urine flows from the kidney through the ureter, bladder, and finally the
urethra before passing from the body.
Composition
Exhaustive detailed description of the composition of human urine can
be found in NASA Contractor Report No. NASA CR-1802, D. F.
Putnam, July 1971.[2] That report provided detailed chemical analyses
for inorganic and organic constituents, methods of analysis, chemical
and physical properties and its behavior during concentrative processes
such as evaporation, distillation and other physiochemical operations.
Urine is an aqueous solution of greater than 95% water, with the
remaining constituents, in order of decreasing concentration urea 9.3
g/L, chloride 1.87 g/L, sodium 1.17 g/L, potassium 0.750 g/L,
creatinine 0.670 g/L and other dissolved ions, inorganic and organic
compounds.
Sample of human urine
Urine is sterile until it reaches the urethra, where epithelial cells lining
the urethra are colonized by facultatively anaerobic Gram negative
rods and cocci. Subsequent to elimination from the body, urine can
acquire strong odors due to bacterial action,[citation needed] and in
particular the release of ammonia from the breakdown of urea.
Some diseases alter the quantity and consistency of urine, such as
diabetes introducing sugar. Consuming beets can result in beeturia
(pink/red urine containing betanin) for some 1014% of the population.
Urea structure
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
75
Hazards
Healthy urine is not toxic.[3] However, it contains compounds
eliminated by the body as undesirable, and can be irritating to skin and
eyes. After suitable processing it is possible to extract potable water
from urine.
Characteristics
Chemical analysis
Urine is principally water. It also contains an assortment of inorganic
salts and organic compounds, including proteins, hormones, and a wide
range of metabolites, varying by what is introduced into the body.
Image of two facing pages of the illuminated
manuscript of "Isagoge", fols. 42b and 43a. On
the top of the left hand page is an illuminated
letter "D" - initial of "De urinarum differencia
negocium" (The matter of the differences of
urines). Inside the letter is a picture of a master
on bench pointing at a raised flask while lecturing
on the "Book on urines" of Theophilus. The right
hand page is only shown in part. On its very
bottom is an illuminated letter "U" - initial of
"Urina ergo est colamentum sanguinis" (Urine is
the filtrate of the blood). Inside the letter is a
picture of a master holding up a flask while
explaining the diagnostic significance of urine to
a student or a patient. HMD Collection, MS E 78.
Color
Urine varies in appearance, depending principally upon a body's level
of hydration, as well as other factors. Normal urine is a transparent
solution ranging from colorless to amber but is usually a pale yellow.
In the urine of a healthy individual the color comes primarily from the
presence of urobilin. Urobilin in turn is a final waste product resulting
from the breakdown of heme from hemoglobin during the destruction
of aging blood cells.
Colorless urine indicates over-hydration, generally preferable to
dehydration (though it can remove essential salts from the body).
Colorless urine in drug tests can suggest an attempt to avoid detection
of illicit drugs in the bloodstream through over-hydration.
Dark yellow urine is often indicative of dehydration.
Yellowing/light orange may be caused by removal of excess B
vitamins from the bloodstream.
Green urine during long term infusion of the
sedative propofol
Certain medications such as rifampin and phenazopyridine can cause orange urine.
Bloody urine is termed hematuria, a symptom of a wide variety of medical conditions.
Dark orange to brown urine can be a symptom of jaundice, rhabdomyolysis, or Gilbert's syndrome.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
Black or dark-colored urine is referred to as melanuria and may be caused by a melanoma.
Pinkish urine can result from the consumption of beets.
Greenish urine can result from the consumption of asparagus.
Reddish or brown urine may be caused by porphyria (not to be confused with the harmless, temporary pink or
reddish tint caused by beeturia).
Blue urine can be caused by the ingestion of methylene blue (e.g., in medications).
Blue urine stains can be caused by blue diaper syndrome.
Odor
The odor of normal human urine can reflect what has been consumed or specific diseases. For example, an
individual with diabetes mellitus may present a sweetened urine odor. This can be due to kidney diseases as well,
such as kidney stones.
Eating asparagus can cause a strong odor reminiscent of the vegetable caused by the body's breakdown of
asparagusic acid. Likewise consumption of saffron, alcohol, coffee, tuna fish, and onion can result in telltale
scents.[citation needed] Particularly spicy foods can have a similar effect, as their compounds pass through the kidneys
without being fully broken down before exiting the body.[4]
Turbidity
Turbid (cloudy) urine may be a symptom of a bacterial infection, but can also be caused by crystallization of salts
such as calcium phosphate.[citation needed]
pH
The pH of urine can vary between 4.6 and 8, with neutral (7) being norm. In persons with hyperuricosuria, acidic
urine can contribute to the formation of stones of uric acid in the kidneys, ureters, or bladder. Urine pH can be
monitored by a physician or at home.
A diet high in citrus, vegetables, or dairy can increase urine pH (more basic).[5] Some drugs also can increase urine
pH, including acetazolamide, potassium citrate, and sodium bicarbonate.[citation needed]
A diet high in meat can decrease urine pH (more acidic).[citation needed] Cranberries, popularly thought to decrease the
pH of urine, have actually been shown not to acidify urine. Drugs that can decrease urine pH include ammonium
chloride, chlorothiazide diuretics, and methenamine mandelate.[6][7]
Volume
Average urine production in adult humans is about 1 2 L per day, depending on state of hydration, activity level,
environmental factors, weight, and the individual's health. Producing too much or too little urine needs medical
attention. Polyuria is a condition of excessive production of urine (> 2.5 L/day), oliguria when < 400 mL are
produced, and anuria one of < 100 mL per day.
Density or specific gravity
Normal urine density or specific gravity values vary between 1.0031.035 (gcm3), and any deviations may be
associated with urinary disorders.
76
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
Urine in medicine
Examination
Many physicians in ancient history have resorted
to the inspection and examination of the urine of
their patients. Hermogenes wrote about the color
and other attributes of urine as indicators of certain
diseases. Abdul Malik Ibn Habib of Andalusia
d.862 AD, mentions numerous reports of urine
examination throughout the Umayyad empire.[8]
Diabetes mellitus got its name because the urine is
plentiful and sweet. A urinalysis is a medical
examination of the urine and part of routine
examinations. A culture of the urine is performed
A Doctor Examining Urine. Trophime Bigot.
when a urinary tract infection is suspected. A
microscopic examination of the urine may be
helpful to identify organic or inorganic substrates and help in the diagnosis.
The color and volume of urine can be reliable indicators of hydration level. Clear and copious urine is generally a
sign of adequate hydration. Dark urine is a sign of dehydration. The exception occurs when diuretics or excessive
amounts of alcohol[citation needed] or caffeine[citation needed] are consumed, in which case urine can be clear and
copious and the person still be dehydrated.
Source of Medications
Urine contains proteins and other substances that are useful for medical therapy and are ingredients in many
prescription drugs (e.g., Ureacin, Urecholine, Urowave).[citation needed] Urine from postmenopausal women is rich in
gonadotropins that can yield follicle stimulating hormone and luteinizing hormone for fertility therapy.[9] One such
commercial product is Pergonal.[10] Urine from pregnant women contains enough human chorionic gonadotropins
for commercial extraction and purification to produce hCG medication. Pregnant mare urine is the source of
estrogens, namely Premarin. Urine also contains antibodies, which can be used in diagnostic antibody tests for a
range of pathogens, including HIV-1.[11]
Other uses
Agriculture
Urine contains large quantities of nitrogen (mostly as urea), as well as significant quantities of dissolved phosphates
and potassium, the main macronutrients required by plants, with urine having plant macronutrient percentages (i.e.
NPK) of approximately 11-1-2 by one study or 15-1-2 by another report, illustrating that exact composition varies
with diet. Undiluted, it can chemically burn the roots of some plants, but it can be used safely as a source of
complementary nitrogen in carbon-rich compost.
When diluted with water (at a 1:5 ratio for container-grown annual crops with fresh growing medium each season, or
a 1:8 ratio for more general use), it can be applied directly to soil as a fertilizer. The fertilization effect of urine has
been found to be comparable to that of commercial fertilizers with an equivalent NPK rating. Urine contains most
(94% according to Wolgast) of the NPK nutrients excreted by the human body. Conversely, concentrations of heavy
metals such as lead, mercury, and cadmium, commonly found in solid human waste, are much lower in urine (though
not low enough to qualify for use in organic agriculture under current EU rules). The more general limitations to
77
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
using urine as fertilizer then depend mainly on the potential for buildup of excess nitrogen (due to the high ratio of
that macronutrient), and inorganic salts such as sodium chloride, which are also part of the wastes excreted by the
renal system. The degree to which these factors impact the effectiveness depends on the term of use, salinity
tolerance of the plant, soil composition, addition of other fertilizing compounds, and quantity of rainfall or other
irrigation.
Urine typically contains 70% of the nitrogen and more than half the phosphorus and potassium found in urban waste
water flows, while making up less than 1% of the overall volume. Thus far, source separation, or urine diversion and
on-site treatment has been implemented in South Africa, China, and Sweden among other countries with the Bill and
Melinda Gates Foundation provided some of the funding implementations.[12] China reportedly had 685,000
operating source separation toilets spread out among 17 provinces in 2003.[13]
"Urine management" is a relatively new way to view closing the cycle of agricultural nutrient flows and reducing
sewage treatment costs and ecological consequences such as eutrophication resulting from the influx of nutrient rich
effluent into aquatic or marine ecosystems. Proponents of urine as a natural source of agricultural fertilizer claim the
risks to be negligible or acceptable. Their views seem to be backed by research showing there are more
environmental problems when it is treated and disposed of compared with when it is used as a resource.[14]
It is unclear whether source separation, urine diversion, and on-site urine treatment can be made cost effective; nor
whether required behavioral changes would be regarded as socially acceptable, as the largely successful trials
performed in Sweden may not readily generalize to other industrialized societies. In developing countries the use of
whole raw sewage (night soil) has been common throughout history, yet the application of pure urine to crops is rare.
Increasingly there are calls for urine's use as a fertilizer, such as a Scientific American article "Human urine is an
effective fertilizer".[15]
Cleaning
In pre-industrial times urine, being rich in ammonia, was used in the form of lant as a cleaning fluid.[16] Urine
was also used for whitening teeth in Ancient Rome.
Gunpowder
Urine was used before the development of a chemical industry in the manufacture of gunpowder. Urine, a nitrogen
source, was used to moisten straw or other organic material, which was kept moist and allowed to rot for several
months to over a year. The resulting salts were washed from the heap with water, which was evaporated to allow
collection of crude saltpeter crystals, that were usually refined before being used in making gunpowder.
Survival uses
The US Army Field Manual,[17] advises against drinking urine for survival. These guides explain that drinking urine
tends to worsen, rather than relieve dehydration due to the salts in it, and that urine should not be consumed in a
survival situation, even when there is no other fluid available. In hot weather survival situations where other sources
of water are not available, soaking cloth (a shirt for example) in urine and putting it on the head can help cool the
body.
During World War I the Germans experimented with numerous poisonous gases for use during war. After the first
German chlorine gas attacks, Allied troops were supplied with masks of cotton pads that had been soaked in urine. It
was believed that the ammonia in the pad neutralized the chlorine. These pads were held over the face until the
soldiers could escape from the poisonous fumes, although it is now known that chlorine gas reacts with urine to
produce toxic fumes (see chlorine and use of poison gas in World War I).[citation needed] The Vickers machine gun,
used by the British Army during World War 1, required water for cooling when fired so soldiers would resort to
urine if water was unavailable.
78
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
Urban myth states that urine works well against jellyfish stings, and this scenario was demonstrated on a Season 4
episode of the NBC-TV show Friends, "The One With the Jellyfish", an early episode of the CBS-TV show Survivor
and the documentary film The Real Cancun. At best, it is ineffective and in some cases this treatment may make the
injury worse.[18][19][20]
Tanning
Tanners soaked animal skins in urine to remove hair fibersa necessary step in the preparation of leather.[citation
needed]
Textiles
Urine has often been used as a mordant to help prepare textiles, especially wool, for dyeing. In Scotland, the process
of "walking" (stretching) tweed cloth is preceded by soaking in urine.[21]
Metals
Because of its high nitrogen content, urine can be used to harden metal. In 1983, in an effort to cope with the high
pressures reached in a turbocharged racing engine, the BMW formula 1 engineering team strengthened their cars'
engine blocks by urinating on them.[22]
History and language
Prior to the acquisition of soap from the Germanic peoples during the first century AD, Ancient Romans used
fermented human urine (in the form of lant) to cleanse grease stains from clothing. The emperor Nero instituted a tax
(Latin: vectigal urinae) on the urine industry, continued by his successor, Vespasian. It is Vespasian to whom the
Latin saying Pecunia non olet (money doesn't smell) is attributed said to have been the emperor's reply to a
complaint from his son about the unpleasant nature of the tax. Vespasian's name is still attached to public urinals in
France (vespasiennes), Italy (vespasiani), and Romania (vespasiene).
Alchemists spent much time trying to extract gold from urine, which led to discoveries such as white phosphorus by
German alchemist Hennig Brand when distilling fermented urine in 1669. In 1773 the French chemist Hilaire
Rouelle discovered the organic compound urea by boiling urine dry.
The onomatopoetic term "piss" was the usual word for urination prior to the 14th century. "Urinate" was at first used
mostly in medical contexts. "Piss" continues to be used, but is considered vulgar; it is also used in such
colloquialisms as "to piss off" and "piss poor". Euphemisms and expressions used between parents and children such
as "wee", "pee", and many others, arose.
References
Notes
[1] Does a reservoir need emptying if someone urinates in it? (http:/ / www. bbc. co. uk/ news/ magazine-13874089). BBC Magazine. 22 June
2011. Retrieved on 2011-06-22.
[2] David F. Putnam Composition and Concentrative Properties of Human Urine (http:/ / ntrs. nasa. gov/ archive/ nasa/ casi. ntrs. nasa. gov/
19710023044_1971023044. pdf). NASA Contractor Report. July 1971
[3] Urine therapy (http:/ / www. vanderbilt. edu/ AnS/ psychology/ health_psychology/ Urine_Therapy. htm). Vanderbilt.edu (1992-10-16).
Retrieved on 2011-04-27.
[4] Foods that Affect the Odor of Urine (http:/ / web. archive. org/ web/ 20110713222322/ http:/ / www. livestrong. com/ article/
248141-foods-that-affect-the-odor-of-urine/ ). livestrong.com. December 27, 2010.
[5] Urine pH is an indicator of dietary acid-base load, fruit and vegetables and meat intakes: results from the European Prospective Investigation
into Cancer and Nutrition (EPIC)-Norfolk population study Br J Nutr. 2008 Jun;99(6):1335-43. Epub 2007 Nov 28 (http:/ / www. ncbi. nlm.
nih. gov/ pubmed/ 18042305)
79
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
[6] Urine pH: MedlinePlus Medical Encyclopedia (http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 003583. htm). Nlm.nih.gov
(2011-03-28). Retrieved on 2011-04-27.
[7] Discovery Health "Urine PH Medical Dictionary" (http:/ / healthguide. howstuffworks. com/ urine-ph-dictionary. htm).
Healthguide.howstuffworks.com (2007-05-16). Retrieved on 2011-04-27.
[8] Ibn Habib, Abdul Malik d.862CE/283AH "Kitaab Tib Al'Arab" (The Book of Arabian Medicine), Published by Dar Ibn Hazm, Beirut,
Lebanon 2007(Arabic)
[9] Carrell, D.T., & Peterson, C. M. eds. (2010). Chapter 31, Artificial insemination: intrauterine insemination. 31.3.1.2 Gonadotrophins,
Reproductive endocrinology and infertility.(Excerpt, p. 489), New York, New York: Springer. DOI 10.1007/978-1-4419-1436-1 (http:/ /
books. google. ca/ books?id=lcBEheiufVcC& pg=PA489& lpg=PA489& dq=urine-derived+ gonadotropins& source=bl& ots=bcwNoc6zP3&
sig=5rt-D-RU9ipfKL3dvGbUHz9VWY0& hl=en& sa=X& ei=6odTUYWFB-eY2AXT7IHoCA& sqi=2& ved=0CFkQ6AEwBg#v=onepage&
q=urine-derived gonadotropins& f=false). Retrieved on 2013-03-26.
[10] [Adelson, Andrea. Wall Street; A Fertility Drug Grows Scarce. http:/ / www. nytimes. com/ 1995/ 02/ 26/ business/
wall-street-a-fertility-drug-grows-scarce. html New York Times 1995-02-26 Retrieved 2013-03-27.].
[11] Urine Antibody Tests: New Insights into the Dynamics of HIV-1 Infection Urnovitz et al. 45 (9): 1602 Clinical Chemistry (http:/ / www.
clinchem. org/ cgi/ content/ abstract/ 45/ 9/ 1602). Clinchem.org. Retrieved on 2011-04-27.
[12] South African city looks to turn urine into fertilizer, UN Office for the Coordination of Humanitarian Affairs, November 2010 (http:/ / www.
sanitationfinance. org/ blog/ urine-fertilizer-south-africa). Sanitationfinance.org (2010-11-13). Retrieved on 2011-12-07.
[13] water- and sanitation-related activities of GTZ focus on ecosan projects (http:/ / www. iwc-berlin. de/ medienpool/
iwc_m77_61000000012/ iwc_20071011140736_1_840856. pdf). (PDF) Retrieved on 2011-12-07.
[14] UDD-Toilets and urine management (http:/ / ecosanservices. org/ pdf/ UDD-ToiletsTraining material. pdf). (PDF). ecosanservices.org.
Retrieved on 2011-12-07.
[15] Mara Grunbaum Shown to be an effective agricultural fertilizer (http:/ / www. scientificamerican. com/ article.
cfm?id=human-urine-is-an-effective-fertilizer), Scientific American, July 2010. Retrieved on 2011-12-07.
[16] Sueton, Vespasian 23 English (http:/ / penelope. uchicago. edu/ Thayer/ E/ Roman/ Texts/ Suetonius/ 12Caesars/ Vespasian*. html#23),
Latin (http:/ / penelope. uchicago. edu/ Thayer/ L/ Roman/ Texts/ Suetonius/ 12Caesars/ Vespasian*. html#23). Cf. Dio Cassius, Roman
History, Book 65, chapter 14,5 English (http:/ / penelope. uchicago. edu/ Thayer/ E/ Roman/ Texts/ Cassius_Dio/ 65*. html#14),
Greek/French (66, 14) (http:/ / remacle. org/ bloodwolf/ historiens/ Dion/ livre66. htm)
[17] Water Procurement (http:/ / www. equipped. com/ 21-76/ ch6. pdf), US Army Field Manual
[18] Old Wives' Tale? Urine as Jellyfish Sting Remedy (http:/ / abcnews. go. com/ Health/ story?id=2283933& page=1). ABC News
(2006-08-08). Retrieved on 2011-04-27.
[19] Fact or Fiction?: Urinating on a Jellyfish Sting is an Effective Treatment (http:/ / www. sciam. com/ article. cfm?chanID=sa004&
articleID=EEC8FE59-E7F2-99DF-3F08DA1A6F42454F& ref=rss). Scientific American. 4 January 2007. Retrieved on 2011-04-27.
[20] Jellyfish Sting Treatment How to Treat a Jellyfish Sting (http:/ / firstaid. about. com/ od/ bitesstings/ ht/ 06_jellyfish. htm).
Firstaid.about.com. 22 August 2010. Retrieved on 2011-04-27.
[21] Mentioned by an interviewee in Lomax the Songhunter, a 2004 documentary film.
[22] Turbocharged Engines in Formula One. (http:/ / www. autoevolution. com/ news/ turbocharged-engines-in-formula-one-18108. html)
Autoevolution. 16 March 2010. Retrieved on 2013-10-31.
Further reading
Definition of oliguria and anuria (http://medres.med.ucla.edu/curriculum/lectures/acute_oliguria.htm)
Hermogenes on urine (http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowPDF&
ProduktNr=223979&Ausgabe=225203&ArtikelNr=13449)
"Urine." Oxford English Dictionary. October 29, 2008 OED.com (http://dictionary.oed.com/entrance.dtl)
Geoffrey Chaucer, Department of English. Dept. home page. October 3, 2006. Harvard University October 27,
2008 Harvard.edu (http://www.courses.fas.harvard.edu/~chaucer/)
Kelly, John F. " The Urine Cure and Other Curious Medical Treatments (http://www.wfmu.org/LCD/19/
urine.html)" Hippocrates Magazine. (May/June 1988)
80
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Urine
81
External links
Urinanalysis (http://www-medlib.med.utah.edu/WebPath/TUTORIAL/URINE/URINE.html) at the
University of Utah Eccles Health Sciences Library
Urine Chemistry (http://www.drugs.com/enc/urine-chemistry.html) at drugs.com
Urinary Health Education (http://www.redurine.com/urine.html) at redurine.com
Clearance (medicine)
In medicine, the clearance is a pharmacokinetic measurement of the renal excretion ability. Although clearance may
also involve other organs than the kidney, it is almost synonymous with renal clearance or renal plasma clearance.
Each substance has a specific clearance that depends on its filtration characteristics. Clearance is a function of
glomerular filtration, secretion from the peritubular capillaries to the nephron, and reabsorption from the nephron
back to the peritubular capillaries. Clearance is constant in first-order kinetics because a constant fraction of the drug
is eliminated per unit time, but it is variable in zero-order kinetics, because a constant amount of drug is eliminated
per unit time.[1]
Definition
When referring to the function of the
kidney, clearance is considered to be the
amount of liquid filtered out of the blood
that gets processed by the kidneys or the
amount of blood cleaned per time because it
has the units of a volumetric flow rate [
volume / time ]. However, it does not refer
to a real value; "the kidney does not
completely remove a substance from the
total renal plasma flow."[2] From a mass
transfer perspective and physiologically,
volumetric blood flow (to the dialysis
machine and/or kidney) is only one of
several factors that determine blood
concentration and removal of a substance
from the body. Other factors include the
mass transfer coefficient, dialysate flow and
dialysate
recirculation
flow
for
hemodialysis, and the glomerular filtration
rate and the tubular reabsorption rate, for the
kidney. A physiologic interpretation of
clearance (at steady-state) is that clearance
is a ratio of the mass generation and blood
(or plasma) concentration.
Diagram showing the basic physiologic mechanisms of the kidney
Its definition follows from the differential equation that describes exponential decay and is used to model kidney
function and hemodialysis machine function:
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Clearance (medicine)
82
Where:
is the mass generation rate of the substance - assumed to be a constant, i.e. not a function of time (equal to
zero for foreign substances/drugs) [mmol/min] or [mol/s]
t is dialysis time or time since injection of the substance/drug [min] or [s]
V is the volume of distribution or total body water [L] or [m]
K is the clearance [mL/min] or [m/s]
C is the concentration [mmol/L] or [mol/m] (in the USA often [mg/mL])
From the above definitions it follows that
is the first derivative of concentration with respect to time, i.e. the
change in concentration with time.
It is derived from a mass balance.
Clearance of a substance is sometimes expressed as the inverse of the time constant that describes its removal rate
from the body divided by its volume of distribution (or total body water).
In steady-state, it is defined as the mass generation rate of a substance (which equals the mass removal rate) divided
by its concentration in the blood.
Effect of plasma protein binding
For substances that exhibit substantial plasma protein binding, clearance is generally defined as the total
concentration (free + protein-bound) and not the free concentration.[3]
Most plasma substances have primarily their free concentrations regulated, which thus remains the same, so
extensive protein binding increases total plasma concentration (free + protein-bound). This gives a decreased
clearance than what would have been the case with no protein binding. However, the mass removal rate is the same,
because it depends only on concentration of free substance, and is independent on plasma protein binding, even with
the fact that plasma proteins increase in concentration in the distal renal glomerulus as plasma is filtered into
Bowman's capsule, because the relative increases in concentrations of substance-protein and non-occupied protein
are equal and therefore give no net binding or dissociation of substances from plasma proteins, thus giving a constant
plasma concentration of free substance throughout the glomerulus, which also would have been the case without any
plasma protein binding.
In other sites than the kidneys, however, where clearance is made by membrane transport proteins rather than
filtration, extensive plasma protein binding may increase clearance by keeping concentration of free substance fairly
constant throughout the capillary bed, inhibiting a decrease in clearance caused by decreased concentration of free
substance through the capillary.
Derivation of equation
Equation 1 is derived from a mass balance:
where:
is a period of time
the change in mass of the toxin in the body during
is the toxin intake rate
is the toxin removal rate
is the toxin generation rate
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Clearance (medicine)
83
In words, the above equation states:
The change in the mass of a toxin within the body (
) during some time
is equal to the toxin intake
plus the toxin generation minus the toxin removal.
Since
and
Equation A1 can be rewritten as:
If one lumps the in and gen. terms together, i.e.
and divides by
the result is a difference
equation:
If one applies the limit
one obtains a differential equation:
Using the Product Rule this can be rewritten as:
If one assumes that the volume change is not significant, i.e.
, the result is Equation 1:
Solution to the differential equation
The general solution of the above differential equation (1) is:
[4]
Where:
Co is the concentration at the beginning of dialysis or the initial concentration of the substance/drug (after it has
distributed) [mmol/L] or [mol/m]
e is the base of the natural logarithm
Steady-state solution
The solution to the above differential equation (9) at time infinity (steady state) is:
The above equation (10a) can be rewritten as:
The above equation (10b) makes clear the relationship between mass removal and clearance. It states that (with a
constant mass generation) the concentration and clearance vary inversely with one another. If applied to creatinine
(i.e. creatinine clearance), it follows from the equation that if the serum creatinine doubles the clearance halves and
that if the serum creatinine quadruples the clearance is quartered.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Clearance (medicine)
Measurement of renal clearance
Renal clearance can be measured with a timed collection of urine and an analysis of its composition with the aid of
the following equation (which follows directly from the derivation of (10b)):
Where:
K is the clearance [mL/min]
CU is the urine concentration [mmol/L] (in the USA often [mg/mL])
Q is the urine flow (volume/time) [mL/min] (often [mL/24 hours])
CB is the plasma concentration [mmol/L] (in the USA often [mg/mL])
When the substance "C" is creatinine, an endogenous chemical that is excreted only by filtration, the calculated
clearance is equivalent to the glomerular filtration rate. Inulin clearance is also used to estimate glomerular filtration
rate.
Note - the above equation (11) is valid only for the steady-state condition. If the substance being cleared is not at a
constant plasma concentration (i.e. not at steady-state) K must be obtained from the (full) solution of the differential
equation (9).
References
[1] Kaplan Step1 Pharmacology 2010, page 14
[2] Available at: (http:/ / www. sin-italy. org/ jnonline/ Vol17n1/ 166. html). Accessed on: Sept 2, 2007.
[3] Basic clinical pharmacokinetics, Page 32: Plasma protein binding (http:/ / books. google. dk/ books?id=JIajn4ebtq0C& pg=PA32&
lpg=PA32& dq=Plasma+ Protein+ Binding) By Michael E. Winter Edition: 4, illustrated Published by Lippincott Williams & Wilkins, 2003
ISBN 0-7817-4147-5, ISBN 978-0-7817-4147-7 511 pages
[4] Full Text (http:/ / ndt. oxfordjournals. org/ cgi/ reprint/ 13/ suppl_6/ 10)
84
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
85
Blood pressure
Blood pressure
Diagnostics
A sphygmomanometer, a device used for measuring arterial pressure.
MeSH
D001795
[1]
Blood pressure (BP), sometimes referred to as arterial blood pressure, is the pressure exerted by circulating blood
upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification,
"blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, blood
pressure varies between a maximum (systolic) and a minimum (diastolic) pressure. The blood pressure in the
circulation is principally due to the pumping action of the heart. Differences in mean blood pressure are responsible
for blood flow from one location to another in the circulation. The rate of mean blood flow depends on the resistance
to flow presented by the blood vessels. Mean blood pressure decreases as the circulating blood moves away from the
heart through arteries and capillaries due to viscous losses of energy. Mean blood pressure drops over the whole
circulation, although most of the fall occurs along the small arteries and arterioles. Gravity affects blood pressure via
hydrostatic forces (e.g., during standing), and valves in veins, breathing, and pumping from contraction of skeletal
muscles also influence blood pressure in veins.
Blood pressure without further specification usually refers to the systemic arterial pressure measured at a person's
upper arm and is a measure of the pressure in the brachial artery, the major artery in the upper arm. A persons blood
pressure is usually expressed in terms of the systolic pressure over diastolic pressure and is measured in millimetres
of mercury (mmHg), for example 120/80.
Blood pressure varies in healthy people and animals, but its variation is under control by the nervous and endocrine
systems. Blood pressure that is pathologically low is called hypotension, and that which is pathologically high is
hypertension. Both have many causes and can range from mild to severe.
Systemic arterial blood pressure
Classification
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
86
Classification of blood pressure for adults
Category
systolic, mmHg diastolic, mmHg
Hypotension
< 90
< 60
Desired
90119
6079
Prehypertension
120139
8089
Stage 1 Hypertension
140159
9099
Stage 2 Hypertension
160179
100109
Hypertensive Emergency
180
110
The table on the right shows the classification of blood pressure adopted by the American Heart Association for
adults who are 18 years and older. It assumes the values are a result of averaging blood pressure readings measured
at two or more visits to the doctor.
In the UK, blood pressures are usually categorised into three groups; low (90/60 or lower), high (140/90 or higher),
and normal (values above 90/60 and below 130/80).[2][3]
Normal range of blood pressure
While average values for arterial pressure could be computed for a given population, there is often a large variation
from person to person; arterial pressure also varies in individuals from moment to moment. Additionally, the average
of any given population may have a questionable correlation with its general health; thus the relevance of such
average values is equally questionable. However, in a study of 100 human subjects with no known history of
hypertension, an average blood pressure of 120/80mmHg was found, which are currently classified as desirable or
"normal" values. Normal values fluctuate through the 24-hour cycle, with highest readings in the afternoons and
lowest readings at night.[4]
Various factors, such as age and sex, influence a person's average blood pressure and variations in it. In children, the
normal ranges are lower than for adults and depend on height.[5] As adults age, systolic pressure tends to rise and
diastolic tends to fall.[6] In the elderly, blood pressure tends to be above the normal adult range,[7] largely because of
reduced flexibility of the arteries. Also, an individual's blood pressure varies with exercise, emotional reactions,
sleep, digestion, time of day and circadian rhythm.
Differences between left and right arm blood pressure measurements tend to be random and average to nearly zero if
enough measurements are taken. However, in a small percentage of cases there is a consistent difference greater than
10mmHg which may need further investigation, e.g. for obstructive arterial disease.
The risk of cardiovascular disease increases progressively above 115/75mmHg. In the past, hypertension was only
diagnosed if secondary signs of high arterial pressure were present, along with a prolonged high systolic pressure
reading over several visits. Regarding hypotension, in practice blood pressure is considered too low only if
noticeable symptoms are present.
Clinical trials demonstrate that people who maintain arterial pressures at the low end of these pressure ranges have
much better long term cardiovascular health. The principal medical debate concerns the aggressiveness and relative
value of methods used to lower pressures into this range for those who do not maintain such pressure on their own.
Elevations, more commonly seen in older people, though often considered normal, are associated with increased
morbidity and mortality.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
87
Reference ranges for blood pressure in children[8]
Stage
Infants
Approximate age Systolic Diastolic
1 to 12 months
Toddlers and preschoolers 1 to 5 years
75100 5070
80110 5080
School age
6 to 12 years
85120 5080
Adolescents
13 to 18 years
95140 6090
Physiology
There are many physical factors that influence arterial pressure. Each
of these may in turn be influenced by physiological factors, such as:
diet, exercise, disease, drugs or alcohol, stress, and obesity.
Some physical factors are:
Volume of fluid or blood volume, the amount of blood that is
present in the body. The more blood present in the body, the higher
the rate of blood return to the heart and the resulting cardiac output.
There is some relationship between dietary salt intake and increased
blood volume, potentially resulting in higher arterial pressure,
though this varies with the individual and is highly dependent on
autonomic nervous system response and the renin-angiotensin
system.
Illustration demonstrating how vessel narrowing,
or vasoconstriction, increases blood pressure.
Resistance. In the circulatory system, this is the resistance of the blood vessels. The higher the resistance, the
higher the arterial pressure upstream from the resistance to blood flow. Resistance is related to vessel radius (the
larger the radius, the lower the resistance), vessel length (the longer the vessel, the higher the resistance), blood
viscosity, as well as the smoothness of the blood vessel walls. Smoothness is reduced by the build up of fatty
deposits on the arterial walls. Substances called vasoconstrictors can reduce the size of blood vessels, thereby
increasing blood pressure. Vasodilators (such as nitroglycerin) increase the size of blood vessels, thereby
decreasing arterial pressure. Resistance, and its relation to volumetric flow rate (Q) and pressure difference
between the two ends of a vessel are described by Poiseuille's Law.
Viscosity, or thickness of the fluid. If the blood gets thicker, the result is an increase in arterial pressure. Certain
medical conditions can change the viscosity of the blood. For instance, anemia (low red blood cell concentration),
reduces viscosity, whereas increased red blood cell concentration increases viscosity. It had been thought that
aspirin and related "blood thinner" drugs decreased the viscosity of blood, but instead studies found that they act
by reducing the tendency of the blood to clot.
In practice, each individual's autonomic nervous system responds to and regulates all these interacting factors so that,
although the above issues are important, the actual arterial pressure response of a given individual varies widely
because of both split-second and slow-moving responses of the nervous system and end organs. These responses are
very effective in changing the variables and resulting blood pressure from moment to moment.
Moreover, blood pressure is the result of cardiac output increased by peripheral resistance: blood pressure = cardiac
output X peripheral resistance. As a result, an abnormal change in blood pressure is often an indication of a problem
affecting the heart's output, the blood vessels' resistance, or both. Thus, knowing the patient's blood pressure is
critical to assess any pathology related to output and resistance.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
88
Mean arterial pressure
The mean arterial pressure (MAP) is the average over a cardiac cycle and is determined by the cardiac output (CO),
systemic vascular resistance (SVR), and central venous pressure (CVP),[9]
MAP can be approximately determined from measurements of the systolic pressure
and the diastolic pressure
Pulse pressure
The up and down fluctuation of the arterial pressure results from the
pulsatile nature of the cardiac output, i.e. the heartbeat. The pulse
pressure is determined by the interaction of the stroke volume of the
heart, compliance (ability to expand) of the aorta, and the resistance to
flow in the arterial tree. By expanding under pressure, the aorta absorbs
some of the force of the blood surge from the heart during a heartbeat.
In this way, the pulse pressure is reduced from what it would be if the
aorta wasn't compliant.[10] The loss of arterial compliance that occurs
with aging explains the elevated pulse pressures found in elderly
patients.
Curve of the arterial pressure during one cardiac
cycle
The pulse pressure can be simply calculated from the difference of the
measured systolic and diastolic pressures,
Armleg gradient
The armleg (blood pressure) gradient is the difference between the blood pressure measured in the arms and that
measured in the legs. It is normally less than 10 mmHg, but may be increased in e.g. coarctation of the aorta.
Vascular resistance
The larger arteries, including all large enough to see without magnification, are conduits with low vascular resistance
(assuming no advanced atherosclerotic changes) with high flow rates that generate only small drops in pressure. The
smaller arteries and arterioles have higher resistance, and confer the main blood pressure drop across major arteries
to capillaries in the circulatory system.
Vascular pressure wave
Modern physiology developed the concept of the vascular pressure wave (VPW). This wave is created by the heart
during the systole and originates in the ascending aorta. Much faster than the stream of blood itself, it is then
transported through the vessel walls to the peripheral arteries. There the pressure wave can be palpated as the
peripheral pulse. As the wave is reflected at the peripheral veins, it runs back in a centripetal fashion. When the
reflected wave meets the next outbound pressure wave, the pressure inside the vessel rises higher than the pressure in
the aorta. This concept explains why the arterial pressure inside the peripheral arteries of the legs and arms is higher
than the arterial pressure in the aorta, and in turn for the higher pressures seen at the ankle compared to the arm with
normal ankle brachial pressure index values.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
Regulation
The endogenous regulation of arterial pressure is not completely understood, but the following mechanisms of
regulating arterial pressure have been well-characterized:
Baroreceptor reflex: Baroreceptors in the high pressure receptor zones detect changes in arterial pressure. These
baroreceptors send signals ultimately to the medulla of the brain stem, specifically to the Rostral ventrolateral
medulla (RVLM). The medulla, by way of the autonomic nervous system, adjusts the mean arterial pressure by
altering both the force and speed of the heart's contractions, as well as the total peripheral resistance. The most
important arterial baroreceptors are located in the left and right carotid sinuses and in the aortic arch.[11]
Renin-angiotensin system (RAS): This system is generally known for its long-term adjustment of arterial
pressure. This system allows the kidney to compensate for loss in blood volume or drops in arterial pressure by
activating an endogenous vasoconstrictor known as angiotensin II.
Aldosterone release: This steroid hormone is released from the adrenal cortex in response to angiotensin II or high
serum potassium levels. Aldosterone stimulates sodium retention and potassium excretion by the kidneys. Since
sodium is the main ion that determines the amount of fluid in the blood vessels by osmosis, aldosterone will
increase fluid retention, and indirectly, arterial pressure.
Baroreceptors in low pressure receptor zones (mainly in the venae cavae and the pulmonary veins, and in the
atria) result in feedback by regulating the secretion of antidiuretic hormone (ADH/Vasopressin), renin and
aldosterone. The resultant increase in blood volume results an increased cardiac output by the FrankStarling law
of the heart, in turn increasing arterial blood pressure.
These different mechanisms are not necessarily independent of each other, as indicated by the link between the RAS
and aldosterone release. Currently, the RAS is targeted pharmacologically by ACE inhibitors and angiotensin II
receptor antagonists. The aldosterone system is directly targeted by spironolactone, an aldosterone antagonist. The
fluid retention may be targeted by diuretics; the antihypertensive effect of diuretics is due to its effect on blood
volume. Generally, the baroreceptor reflex is not targeted in hypertension because if blocked, individuals may suffer
from orthostatic hypotension and fainting.
Measurement
Arterial pressure is most commonly measured via a
sphygmomanometer, which historically used the height of a column of
mercury to reflect the circulating pressure. Blood pressure values are
generally reported in millimetres of mercury (mmHg), though aneroid
and electronic devices do not contain mercury.
For each heartbeat, blood pressure varies between systolic and diastolic
pressures. Systolic pressure is peak pressure in the arteries, which
occurs near the end of the cardiac cycle when the ventricles are
contracting. Diastolic pressure is minimum pressure in the arteries,
A medical student checking blood pressure using
which occurs near the beginning of the cardiac cycle when the
a sphygmomanometer and stethoscope.
ventricles are filled with blood. An example of normal measured
values for a resting, healthy adult human is 120mmHg systolic and 80mmHg diastolic (written as 120/80 mmHg,
and spoken as "one-twenty over eighty").
Systolic and diastolic arterial blood pressures are not static but undergo natural variations from one heartbeat to
another
and
throughout
the
day
89
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
90
(in a circadian rhythm). They also change in response to stress,
nutritional factors, drugs, disease, exercise, and momentarily from
standing up. Sometimes the variations are large. Hypertension refers to
arterial pressure being abnormally high, as opposed to hypotension,
when it is abnormally low. Along with body temperature, respiratory
rate, and pulse rate, blood pressure is one of the four main vital signs
routinely monitored by medical professionals and healthcare providers.
Right position for taking blood pressure
Measuring pressure invasively, by penetrating the arterial wall to take the measurement, is much less common and
usually restricted to a hospital setting.
Noninvasive
The noninvasive auscultatory and oscillometric measurements are simpler and quicker than invasive measurements,
require less expertise, have virtually no complications, are less unpleasant and less painful for the patient. However,
noninvasive methods may yield somewhat lower accuracy and small systematic differences in numerical results.
Noninvasive measurement methods are more commonly used for routine examinations and monitoring.
Palpation
A minimum systolic value can be roughly estimated by palpation, most often used in emergency situations, but
should be used with caution. It has been estimated that, using 50% percentiles, carotid, femoral and radial pulses are
present in patients with a systolic blood pressure > 70 mmHg, carotid and femoral pulses alone in patients with
systolic blood pressure of > 50 mmHg, and only a carotid pulse in patients with a systolic blood pressure of > 40
mmHg.
A more accurate value of systolic blood pressure can be obtained with a sphygmomanometer and palpating the radial
pulse.[12] The diastolic blood pressure cannot be estimated by this method.[13] The American Heart Association
recommends that palpation be used to get an estimate before using the auscultatory method.
Auscultatory
The auscultatory method (from the Latin word for "listening") uses a
stethoscope and a sphygmomanometer. This comprises an inflatable
(Riva-Rocci) cuff placed around the upper arm at roughly the same
vertical height as the heart, attached to a mercury or aneroid
manometer. The mercury manometer, considered the gold standard,
measures the height of a column of mercury, giving an absolute result
without need for calibration and, consequently, not subject to the errors
and drift of calibration which affect other methods. The use of mercury
manometers is often required in clinical trials and for the clinical
measurement of hypertension in high-risk patients, such as pregnant
women.
Auscultatory method aneroid
sphygmomanometer with stethoscope
A cuff of appropriate size is fitted smoothly and snugly, then inflated manually by repeatedly squeezing a rubber
bulb until the artery is completely occluded. Listening with the stethoscope to the brachial artery at the elbow, the
examiner
slowly
releases
the
pressure
in
the
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
cuff. When blood just starts to flow in the artery, the turbulent flow
creates a "whooshing" or pounding (first Korotkoff sound). The
pressure at which this sound is first heard is the systolic blood pressure.
The cuff pressure is further released until no sound can be heard (fifth
Korotkoff sound), at the diastolic arterial pressure.
The auscultatory method is the predominant method of clinical
measurement.[14]
Oscillometric
The oscillometric method was first demonstrated in 1876 and involves
the observation of oscillations in the sphygmomanometer cuff
pressure[15] which are caused by the oscillations of blood flow, i.e., the
Mercury manometer
pulse. The electronic version of this method is sometimes used in
long-term measurements and general practice. It uses a
sphygmomanometer cuff, like the auscultatory method, but with an electronic pressure sensor (transducer) to observe
cuff pressure oscillations, electronics to automatically interpret them, and automatic inflation and deflation of the
cuff. The pressure sensor should be calibrated periodically to maintain accuracy.
Oscillometric measurement requires less skill than the auscultatory technique and may be suitable for use by
untrained staff and for automated patient home monitoring.
The cuff is inflated to a pressure initially in excess of the systolic arterial pressure and then reduced to below
diastolic pressure over a period of about 30seconds. When blood flow is nil (cuff pressure exceeding systolic
pressure) or unimpeded (cuff pressure below diastolic pressure), cuff pressure will be essentially constant. It is
essential that the cuff size is correct: undersized cuffs may yield too high a pressure; oversized cuffs yield too low a
pressure. When blood flow is present, but restricted, the cuff pressure, which is monitored by the pressure sensor,
will vary periodically in synchrony with the cyclic expansion and contraction of the brachial artery, i.e., it will
oscillate. The values of systolic and diastolic pressure are computed, not actually measured from the raw data, using
an algorithm; the computed results are displayed.
Oscillometric monitors may produce inaccurate readings in patients with heart and circulation problems, which
include arterial sclerosis, arrhythmia, preeclampsia, pulsus alternans, and pulsus paradoxus [citation needed].
In practice the different methods do not give identical results; an algorithm and experimentally obtained coefficients
are used to adjust the oscillometric results to give readings which match the auscultatory results as well as possible.
Some equipment uses computer-aided analysis of the instantaneous arterial pressure waveform to determine the
systolic, mean, and diastolic points. Since many oscillometric devices have not been validated, caution must be given
as most are not suitable in clinical and acute care settings.
The term NIBP, for non-invasive blood pressure, is often used to describe oscillometric monitoring equipment.
Continuous noninvasive techniques (CNAP)
Continuous Noninvasive Arterial Pressure (CNAP) is the method of measuring arterial blood pressure in real-time
without any interruptions and without cannulating the human body. CNAP combines the advantages of the following
two clinical gold standards: it measures blood pressure continuously in real-time like the invasive arterial catheter
system and it is noninvasive like the standard upper arm sphygmomanometer. Latest developments in this field show
promising results in terms of accuracy, ease of use and clinical acceptance.
91
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
Non-occlusive techniques: the Pulse Wave Velocity (PWV) principle
Since the 1990s a novel family of techniques based on the so-called pulse wave velocity (PWV) principle have been
developed. These techniques rely on the fact that the velocity at which an arterial pressure pulse travels along the
arterial tree depends, among others, on the underlying blood pressure. Accordingly, after a calibration maneuver,
these techniques provide indirect estimates of blood pressure by translating PWV values into blood pressure values.
The main advantage of these techniques is that it is possible to measure PWV values of a subject continuously
(beat-by-beat), without medical supervision, and without the need of inflating brachial cuffs. PWV-based techniques
are still in the research domain and are not adapted to clinical settings.
White-coat hypertension
For some patients, blood pressure measurements taken in a doctor's office may not correctly characterize their typical
blood pressure. In up to 25% of patients, the office measurement is higher than their typical blood pressure. This
type of error is called white-coat hypertension (WCH) and can result from anxiety related to an examination by a
health care professional. The misdiagnosis of hypertension for these patients can result in needless and possibly
harmful medication. WCH can be reduced (but not eliminated) with automated blood pressure measurements over 15
to 20 minutes in a quiet part of the office or clinic.[16]
Debate continues regarding the significance of this effect.[citation needed] Some reactive patients will react to many
other stimuli throughout their daily lives and require treatment. In some cases a lower blood pressure reading occurs
at the doctor's office.[17]
Home monitoring
Ambulatory blood pressure devices that take readings every half hour throughout the day and night have been used
for identifying and mitigating measurement problems like white-coat hypertension. Except for sleep, home
monitoring could be used for these purposes instead of ambulatory blood pressure monitoring. Home monitoring
may be used to improve hypertension management and to monitor the effects of lifestyle changes and medication
related to blood pressure. Compared to ambulatory blood pressure measurements, home monitoring has been found
to be an effective and lower cost alternative, but ambulatory monitoring is more accurate than both clinic and home
monitoring in diagnosing hypertension. Ambulatory monitoring is recommended for most patients before the start of
antihypertensive drugs.[18]
Aside from the white-coat effect, blood pressure readings outside of a clinical setting are usually slightly lower in the
majority of people. The studies that looked into the risks from hypertension and the benefits of lowering blood
pressure in affected patients were based on readings in a clinical environment.
When measuring blood pressure, an accurate reading requires that one not drink coffee, smoke cigarettes, or engage
in strenuous exercise for 30minutes before taking the reading. A full bladder may have a small effect on blood
pressure readings; if the urge to urinate arises, one should do so before the reading. For 5minutes before the reading,
one should sit upright in a chair with one's feet flat on the floor and with limbs uncrossed. The blood pressure cuff
should always be against bare skin, as readings taken over a shirt sleeve are less accurate. During the reading, the
arm that is used should be relaxed and kept at heart level, for example by resting it on a table.
Since blood pressure varies throughout the day, measurements intended to monitor changes over longer time frames
should be taken at the same time of day to ensure that the readings are comparable. Suitable times are:
immediately after awakening (before washing/dressing and taking breakfast/drink), while the body is still resting,
immediately after finishing work.
Automatic self-contained blood pressure monitors are available at reasonable prices, some of which are capable of
Korotkoff's measurement in addition to oscillometric methods, enabling irregular heartbeat patients to accurately
measure their blood pressure at home.
92
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
Invasive
Arterial blood pressure (BP) is most accurately measured invasively through an arterial line. Invasive arterial
pressure measurement with intravascular cannulae involves direct measurement of arterial pressure by placing a
cannula needle in an artery (usually radial, femoral, dorsalis pedis or brachial).
The cannula must be connected to a sterile, fluid-filled system, which is connected to an electronic pressure
transducer. The advantage of this system is that pressure is constantly monitored beat-by-beat, and a waveform (a
graph of pressure against time) can be displayed. This invasive technique is regularly employed in human and
veterinary intensive care medicine, anesthesiology, and for research purposes.
Cannulation for invasive vascular pressure monitoring is infrequently associated with complications such as
thrombosis, infection, and bleeding. Patients with invasive arterial monitoring require very close supervision, as
there is a danger of severe bleeding if the line becomes disconnected. It is generally reserved for patients where rapid
variations in arterial pressure are anticipated.
Invasive vascular pressure monitors are pressure monitoring systems designed to acquire pressure information for
display and processing. There are a variety of invasive vascular pressure monitors for trauma, critical care, and
operating room applications. These include single pressure, dual pressure, and multi-parameter (i.e. pressure /
temperature). The monitors can be used for measurement and follow-up of arterial, central venous, pulmonary
arterial, left atrial, right atrial, femoral arterial, umbilical venous, umbilical arterial, and intracranial pressures.
Fetal blood pressure
In pregnancy, it is the fetal heart and not the mother's heart that builds up the fetal blood pressure to drive its blood
through the fetal circulation.
The blood pressure in the fetal aorta is approximately 30 mmHg at 20 weeks of gestation, and increases to
approximately 45 mmHg at 40 weeks of gestation.
The average blood pressure for full-term infants:
Systolic 6595mm Hg
Diastolic 3060mm Hg[19]
Blood pressure is the measurement of force that is applied to the walls of the blood vessels as the heart pumps blood
throughout the body. The human circulatory system is 400,000 miles (600,000km) long, and the magnitude of blood
pressure is not uniform in all the blood vessels in the human body. The blood pressure is determined by the diameter,
flexibility and the amount of blood being pumped through the blood vessel. Blood pressure is also affected by other
factors including exercise, stress level, diet and sleep.
The average normal blood pressure in the brachial artery, which is the next direct artery from the aorta after the
subclavian artery, is 120/80mmHg. Blood pressure readings are measured in millimeters of mercury (mmHg) using
sphygmomanometer. Two pressures are measured and recorded namely as systolic and diastolic pressures. Systolic
pressure reading is the first reading, which represents the maximum exerted pressure on the vessels when the heart
contracts, while the diastolic pressure, the second reading, represents the minimum pressure in the vessels when the
heart relaxes. Other major arteries have similar levels of blood pressure recordings indicating very low disparities
among major arteries. The innominate artery, the average reading is 110/70mmHg, the right subclavian artery
averages 120/80 and the abdominal aorta is 110/70mmHg. The relatively uniform pressure in the arteries indicate
that these blood vessels act as a pressure reservoir for fluids that are transported within them.
Pressure drops gradually as blood flows from the major arteries, through the arterioles, the capillaries until blood is
pushed up back into the heart via the venules, the veins through the vena cava with the help of the muscles. At any
given pressure drop, the flow rate is determined by the resistance to the blood flow. In the arteries, with the absence
of diseases, there is very little or no resistance to blood. The vessel diameter is the most principal determinant to
control resistance. Compared to other smaller vessels in the body, the artery has a much bigger diameter (4mm),
93
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
therefore the resistance is low.
In addition, flow rate (Q) is also the product of the cross-sectional area of the vessel and the average velocity
(Q=AV). Flow rate is directly proportional to the pressure drop in a tube or in this case a vessel. PQ. The
relationship is further described by Poisseulles equation P=8lQ/r4. As evident in the Poisseulles equation,
although flow rate is proportional to the pressure drop, there are other factors of blood vessels that contribute
towards the difference in pressure drop in bifurcations of blood vessels. These include viscosity, length of the vessel,
and radius of the vessel.
Factors that determine the flows resistance as described by Poiseuilles relationship:
P: pressure drop/gradient
: viscosity
l: length of tube. In the case of vessels with infinitely long lengths, l is replaced with diameter of the vessel.
Q: flow rate of the blood in the vessel
r: radius of the vessel
Assuming steady, laminar flow in the vessel, the blood vessels behavior is similar to that of a pipe. For instance if p1
and p2 are pressures are at the ends of the tube, the pressure drop/gradient is:
In the arterioles blood pressure is lower than in the major arteries. This is due to bifurcations, which cause a drop in
pressure. The more bifurcations, the higher the total cross-sectional area, therefore the pressure across the surface
drops. This is why the arterioles have the highest pressure-drop. The pressure drop of the arterioles is the product of
flow rate and resistance: P=Q xresistance. The high resistance observed in the arterioles, which factor largely in the
P is a result of a smaller radius of about 30m. The smaller the radius of a tube, the larger the resistance to fluid
flow.
Immediately following the arterioles are the capillaries. Following the logic obvserved in the arterioles, we expect
the blood pressure to be lower in the capillaries compared to the arterioles. Since pressure is a function of force per
unit area, (P=F/A), the larger the surface area, the lesser the pressure when an external force acts on it. Though the
radii of the capillaries are very small, the network of capillaries have the largest surface area in the vascular network.
They are known to have the largest surface area (485mm) in the human vascular network. The larger the total
cross-sectional area, the lower the mean velocity as well as the pressure.
Reynolds number also affects the blood flow in capillaries. Due to its smaller radius and lowest velocity compared
to other vessels, the Reynolds number at the capillaries is very low, resulting in laminar instead of turbulent flow.
The Reynolds number (denoted NR or Re) is a relationship that helps determine the behavior of a fluid in a tube, in
this case blood in the vessel. The equation for this dimensionless relationship is written as:
: density of the blood
v: mean velocity of the blood
L: characteristic dimension of the vessel, in this case diameter
: viscosity of blood
The Reynolds number is directly proportional to the velocity and diameter of the tube. Note that NR is directly
proportional to the mean velocity as well as the diameter. A Reynolds number of less than 2300 is laminar fluid
flow, which is characterized by constant flow motion, whereas a value of over 4000, is represented as turbulent flow.
Turbulent flow is characterized as chaotic and irregular flow.
94
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
Disorders
Disregulation disorders of blood pressure control include: high blood pressure, low blood pressure, and blood
pressure that shows excessive or maladaptive fluctuation.
High
Arterial hypertension can be an indicator of
other problems and may have long-term
adverse effects. Sometimes it can be an
acute problem, for example hypertensive
emergency.
Levels of arterial pressure put mechanical
stress on the arterial walls. Higher pressures
increase heart workload and progression of
unhealthy tissue growth (atheroma) that
develops within the walls of arteries. The
higher the pressure, the more stress that is
present and the more atheroma tend to
progress and the heart muscle tends to
thicken, enlarge and become weaker over
time.
Persistent hypertension is one of the risk
factors for strokes, heart attacks, heart
Overview of main complications of persistent high blood pressure.
failure and arterial aneurysms, and is the
leading cause of chronic renal failure. Even moderate elevation of arterial pressure leads to shortened life
expectancy. At severely high pressures, mean arterial pressures 50% or more above average, a person can expect to
live no more than a few years unless appropriately treated.[20]
In the past, most attention was paid to diastolic pressure; but nowadays it is recognised that both high systolic
pressure and high pulse pressure (the numerical difference between systolic and diastolic pressures) are also risk
factors. In some cases, it appears that a decrease in excessive diastolic pressure can actually increase risk, due
probably to the increased difference between systolic and diastolic pressures (see the article on pulse pressure). If
systolic blood pressure is elevated (>140) with a normal diastolic blood pressure (<90), it is called "isolated systolic
hypertension" and may present a health concern.
For those with heart valve regurgitation, a change in its severity may be associated with a change in diastolic
pressure. In a study of people with heart valve regurgitation that compared measurements 2 weeks apart for each
person, there was an increased severity of aortic and mitral regurgitation when diastolic blood pressure increased,
whereas when diastolic blood pressure decreased, there was a decreased severity.
95
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
Low
Blood pressure that is too low is known as hypotension. Hypotension is a medical concern if it causes signs or
symptoms, such as dizziness, fainting, or in extreme cases, shock.
When arterial pressure and blood flow decrease beyond a certain point, the perfusion of the brain becomes critically
decreased (i.e., the blood supply is not sufficient), causing lightheadedness, dizziness, weakness or fainting.
Sometimes the arterial pressure drops significantly when a patient stands up from sitting. This is known as
orthostatic hypotension (postural hypotension); gravity reduces the rate of blood return from the body veins below
the heart back to the heart, thus reducing stroke volume and cardiac output.
When people are healthy, the veins below their heart quickly constrict and the heart rate increases to minimize and
compensate for the gravity effect. This is carried out involuntarily by the autonomic nervous system. The system
usually requires a few seconds to fully adjust and if the compensations are too slow or inadequate, the individual will
suffer reduced blood flow to the brain, dizziness and potential blackout. Increases in G-loading, such as routinely
experienced by aerobatic or combat pilots 'pulling Gs', greatly increases this effect. Repositioning the body
perpendicular to gravity largely eliminates the problem.
Other causes of low arterial pressure include:
Sepsis
Hemorrhage blood loss
Toxins including toxic doses of blood pressure medicine
Hormonal abnormalities, such as Addison's disease
Eating disorders, particularly anorexia nervosa and bulimia
Shock is a complex condition which leads to critically decreased perfusion. The usual mechanisms are loss of blood
volume, pooling of blood within the veins reducing adequate return to the heart and/or low effective heart pumping.
Low arterial pressure, especially low pulse pressure, is a sign of shock and contributes to and reflects decreased
perfusion.
If there is a significant difference in the pressure from one arm to the other, that may indicate a narrowing (for
example, due to aortic coarctation, aortic dissection, thrombosis or embolism) of an artery .
Fluctuating blood pressure
Normal fluctuation in blood pressure is adaptive and necessary. Fluctuations in pressure that are significantly greater
than the norm are associated with greater white matter hyperintensity, a finding consistent with reduced local
cerebral blood flow[21] and a heightened risk of cerebrovascular disease.[22] Within both high- and low-blood
pressure groups, a greater degree of fluctuation was found to correlate with an increase in cerebrovascular disease
compared to those with less variability, suggesting the consideration of the clinical management of blood pressure
fluctuations, even among normotensive older adults. Older individuals and those who had received blood pressure
medications were more likely to exhibit larger fluctuations in pressure.
At other sites
96
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
97
Site
Normal
pressure
range
[23]
(in mmHg)
Central venous pressure
38
Right ventricular pressure systolic
1530
diastolic 38
Pulmonary artery pressure systolic
1530
diastolic 412
Pulmonary vein/
215
Pulmonary capillary wedge pressure
Left ventricular pressure
systolic
100140
diastolic 3-12
Blood pressure generally refers to the arterial pressure in the systemic circulation. However, measurement of
pressures in the venous system and the pulmonary vessels plays an important role in intensive care medicine but
requires an invasive central venous catheter.
Systemic venous pressure
Venous pressure is the vascular pressure in a vein or in the atria of the heart. It is much less than arterial pressure,
with common values of 5mmHg in the right atrium and 8mmHg in the left atrium.
Variants of venous pressure include:
Central venous pressure, which is a good approximation of right atrial pressure, which is a major determinant of
right ventricular end diastolic volume. (However, there can be exceptions in some cases.)
The jugular venous pressure (JVP) is the indirectly observed pressure over the venous system. It can be useful in
the differentiation of different forms of heart and lung disease.
The portal venous pressure is the blood pressure in the portal vein. It is normally 510mm Hg
Pulmonary pressure
Normally, the pressure in the pulmonary artery is about 15 mmHg at rest.[24]
Increased blood pressure in the capillaries of the lung cause pulmonary hypertension, with interstitial edema if the
pressure increases to above 20 mmHg, and to frank pulmonary edema at pressures above 25 mmHg.[25]
Relation to wall tension
Regardless of site, blood pressure is related to the wall tension of the vessel according to the YoungLaplace
equation (assuming that the thickness of the vessel wall is very small as compared to the diameter of the lumen):
where
P is the blood pressure
t is the wall thickness
r is the inside radius of the cylinder.
is the cylinder stress or "hoop stress".
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
98
For the thin-walled assumption to be valid the vessel must have a wall thickness of no more than about one-tenth
(often cited as one twentieth) of its radius.
The cylinder stress, in turn, is the average force exerted
circumferentially (perpendicular both to the axis and to the radius of
the object) in the cylinder wall, and can be described as:
where:
F is the force exerted circumferentially on an area of the cylinder
wall that has the following two lengths as sides:
t is the radial thickness of the cylinder
l is the axial length of the cylinder
Components of cylinder stress.
References
[1] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?field=uid& term=D001795
[2] NHS choices: What is blood pressure? (http:/ / www. nhs. uk/ chq/ pages/ what-is-blood-pressure. aspx?categoryid=201&
subcategoryid=201) Retrieved 2012-03-27
[3] NHS choices: High blood pressure (hypertension) (http:/ / www. nhs. uk/ conditions/ Blood-pressure-(high)/ Pages/ Introduction. aspx)
Retrieved 2012-03-27
[4] Table: Comparison of ambulatory blood pressures and urinary norepinephrine and epinephrine excretion measured at work, home, and during
sleep between EuropeanAmerican (n = 110) and AfricanAmerican (n = 51) women (http:/ / www. ncbi. nlm. nih. gov/ pmc/ articles/
PMC2655229/ table/ T2/ )
[5] (Note that the median blood pressure is given by the 50th percentile and hypertension is defined by the 95th percentile for a given age, height,
and gender.)
[6] See Isolated Systolic Hypertension.
[7] "...more than half of all Americans aged 65 or older have hypertension."
[8] PEDIATRIC AGE SPECIFIC (http:/ / hr. uclahealth. org/ workfiles/ AgeSpecificSLM-Peds. pdf), page 6. Revised 6/10. By Theresa
Kirkpatrick and Kateri Tobias. UCLA Health System
[9] Archived version 2009-10-03 (http:/ / www. webcitation. org/ 5kGLMdqnn)
[10] Archived version 2009-10-03 (http:/ / www. webcitation. org/ 5kGLuC47S)
[11] Archived version 2009-10-03 (http:/ / www. cvphysiology. com/ Blood Pressure/ BP012. htm)
[12] Interpretation Blood Pressure Vitals (http:/ / bcs. medinfo. ufl. edu/ sample/ page06. html), University of Florida
[13] G8 Secondary Survey (http:/ / www. gov. mb. ca/ health/ ems/ guidelines/ G8. pdf), "Manitoba"
[14] See Blood Pressure Measurement Methods.
[15] See The Oscillometric Technique.
[16] See White Coat Hypertension or Isolated Office Hypertension.
[17] See Masked Hypertension or Isolated Ambulatory Hypertension.
[18] Kate Lovibond, Sue Jowett, Pelham Barton, Mark Caulfield et al. " Cost-effectiveness of options for the diagnosis of high blood pressure in
primary care: a modelling study (http:/ / www. thelancet. com/ journals/ lancet/ article/ PIIS0140-6736(11)61184-7/ fulltext)", The Lancet, 24
August 2011. Retrieved 24 August 2011.
[19] Sharon, S. M. & Emily, S. M.(2006). Foundations of Maternal-Newborn Nursing. (4th ed p.476). Philadelphia:Elsevier.
[20] Textbook of Medical Physiology, 7th Ed., Guyton & Hall, Elsevier-Saunders, ISBN 0-7216-0240-1, page 220.
[21] Thomas, A.J., Perry, R., Barber, R., Kalaria, R.N., OBrien, J.T. (2002)
" Pathologies and pathological mechanisms for white matter hyperintensities in depression (http:/ / www3.
interscience.wiley.com/journal/120778635/abstract)," '
'Ann N Y Acad Sci., 977:333339.
[22] Brickman AM, Reitz C, Luchsinger JA, Manly JJ, Schupf N, Muraskin J, DeCarli C, Brown TR, Mayeux R.
Long-term blood pressure fluctuation and cerebrovascular disease in an elderly cohort.
Arch Neurol. 2010 May 67(5):5649
PMID 20457955
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Blood pressure
PMCID PMC2917204 Free Full Text: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2917204/?tool=pubmed
NIHMSID NIHMS216309
http://archneur.ama-assn.org/cgi/content/short/67/5/564
[23] Table 30-1 in:
[24] What Is Pulmonary Hypertension? (http:/ / www. nhlbi. nih. gov/ health/ dci/ Diseases/ pah/ pah_what. html) From Diseases and Conditions
Index (DCI). National Heart, Lung, and Blood Institute. Last updated September 2008. Retrieved on 6 April 2009.
[25] Chapter 41, page 210 in: Cardiology secrets (http:/ / books. google. com/ books?id=IYFAsxAUA_MC& printsec=frontcover#PPR3,M1) By
Olivia Vynn Adair Edition: 2, illustrated Published by Elsevier Health Sciences, 2001 ISBN 1-56053-420-6, ISBN 978-1-56053-420-4
Further reading
Pickering, TG; Hall, JE; Appel, LJ et al. (2005). "Recommendations for blood pressure measurement in humans
and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the
Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood
Pressure Research" (http://hyper.ahajournals.org/cgi/content/full/45/1/142). Hypertension 45 (5): 14261.
doi: 10.1161/01.HYP.0000150859.47929.8e (http://dx.doi.org/10.1161/01.HYP.0000150859.47929.8e).
PMID 15611362 (http://www.ncbi.nlm.nih.gov/pubmed/15611362). Retrieved 2009-10-01.
External links
Blood Pressure Association (UK)ension/ Pulmonary Hypertension (http://www.bpassoc.org.uk), Cleveland
Clinic Center for Continuing Education
About High Blood Pressure (http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/
AboutHighBloodPressure/About-High-Blood-Pressure_UCM_002050_Article.jsp), American Heart Association
Control of Blood Pressure (http://pie.med.utoronto.ca/CA/CA_content/CA_cardiacPhys_intro.html),
Toronto General Hospital
Blood Pressure Chart (http://www.vaughns-1-pagers.com/medicine/blood-pressure.htm), Vaughn's
Summaries
99
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
100
Erythropoietin
Erythropoietin
Available structures
PDB Ortholog search: PDBe [1], RCSB [2]
List of PDB id codes
1BUY
[3]
, 1CN4
[4]
, 1EER
[5]
Identifiers
[6]
Symbols
EPO
External IDs
OMIM: 133170
; EP; MVCD2
[7]
MGI: 95407
[8]
HomoloGene: 624
[9]
ChEMBL: 5837
[10]
GeneCards: EPO Gene
[11]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
101
Gene Ontology
Molecular function erythropoietin receptor binding [12]
[13]
hormone activity
[14]
protein binding
[15]
protein kinase activator activity
[16]
eukaryotic cell surface binding
Cellular component extracellular region [17]
[18]
extracellular space
Biological process
[19]
apoptotic process
[20]
signal transduction
[21]
embryo implantation
[22]
aging
[23]
blood circulation
[24]
positive regulation of cell proliferation
[25]
response to salt stress
[26]
negative regulation of sodium ion transport
[27]
peptidyl-serine phosphorylation
[28]
negative regulation of ion transmembrane transporter activity
[29]
response to lipopolysaccharide
[30]
negative regulation of myeloid cell apoptotic process
[31]
response to vitamin A
[32]
cellular response to stress
[33]
response to testosterone stimulus
[34]
positive regulation of tyrosine phosphorylation of Stat5 protein
[35]
hemoglobin biosynthetic process
[36]
negative regulation of apoptotic process
[37]
erythrocyte maturation
[38]
response to estrogen stimulus
[39]
positive regulation of neuron differentiation
[40]
positive regulation of DNA replication
[41]
positive regulation of transcription, DNA-dependent
[42]
positive regulation of Ras protein signal transduction
[43]
response to axon injury
[44]
response to electrical stimulus
[45]
response to hyperoxia
regulation of transcription from RNA polymerase II promoter in response to hypoxia
[46]
[47]
response to interleukin-1
[48]
cellular response to hypoxia
[49]
cellular hyperosmotic response
Sources: Amigo
[50]
/ QuickGO
[51]
RNA expression pattern
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
102
More reference expression data
[52]
Orthologs
Species
Human
Mouse
Entrez
2056
Ensembl
ENSG00000130427
UniProt
P01588
RefSeq (mRNA)
NM_000799
RefSeq (protein)
NP_000790
[53]
13856
[55]
[57]
[54]
ENSMUSG00000029711
P07321
[59]
[61]
[58]
NM_007942
NP_031968
[60]
[62]
Location (UCSC) Chr 7:
[63]
100.32 100.32 Mb
Chr 5:
[64]
137.48 137.53 Mb
PubMed search
[66]
[65]
[56]
Erythropoietin, also known as erythropoetin or erthropoyetin (/rrp.tn/, /rrptn/, and /rir-/) or
EPO, is a glycoprotein hormone that controls erythropoiesis, or red blood cell production. It is a cytokine (protein
signaling molecule) for erythrocyte (red blood cell) precursors in the bone marrow. Human EPO has a molecular
weight of 34 kDa.
Also called hematopoietin or hemopoietin, it is produced by interstitial fibroblasts in the kidney in close association
with peritubular capillary and tubular epithelial tubule. It is also produced in perisinusoidal cells in the liver. While
liver production predominates in the fetal and perinatal period, renal production is predominant during adulthood. In
addition to erythropoiesis, erythropoietin also has other known biological functions. For example, it plays an
important role in the brain's response to neuronal injury. EPO is also involved in the wound healing process.
When exogenous EPO is used as a performance-enhancing drug, it is classified as an erythropoiesis-stimulating
agent (ESA). Exogenous EPO can often be detected in blood, due to slight differences from the endogenous protein,
for example, in features of posttranslational modification.
Function
Primary role in red blood cell production
Erythropoietin is an essential hormone for red cell production. Without it, definitive erythropoiesis does not take
place. Under hypoxic conditions, the kidney will produce and secrete erythropoietin to increase the production of red
blood cells by targeting CFU-E, proerythroblast and basophilic erythroblast subsets in the differentiation.
Erythropoietin has its primary effect on red blood cell progenitors and precursors (which are found in the bone
marrow in humans) by promoting their survival through protecting these cells from apoptosis.
Erythropoietin is the primary erythropoietic factor that cooperates with various other growth factors (e.g., IL-3, IL-6,
glucocorticoids, and SCF) involved in the development of erythroid lineage from multipotent progenitors. The
burst-forming unit-erythroid (BFU-E) cells start erythropoietin receptor expression and are sensitive to
erythropoietin. Subsequent stage, the colony-forming unit-erythroid (CFU-E), expresses maximal erythropoietin
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
receptor density and is completely dependent on erythropoietin for further differentiation. Precursors of red cells, the
proerythroblasts and basophilic erythroblasts also express erythropoietin receptor and are therefore affected by it.
Additional nonhematopoietic roles
Erythropoietin has a range of actions including vasoconstriction-dependent hypertension, stimulating angiogenesis,
and inducing proliferation of smooth muscle fibers. It can increase iron absorption by suppressing the hormone
hepcidin.
EPO also affects neuronal protection during hypoxic conditions (stroke, etc.). Trials on human subjects are not yet
reported; if proven to be a viable treatment of heart attack and stroke patients, it could improve the outcome and
quality of life. The reasoning behind such a proposal is that EPO levels of 100 times the baseline have been detected
in brain tissue as a natural response to (primarily) hypoxic damage.
Multiple studies have suggested that EPO improves memory. This effect is independent of its effect on hematocrit.
Rather, it is associated with an increase in hippocampal response and effects on synaptic connectivity, neuronal
plasticity, and memory-related neural networks. EPO may also be an effective treatment for depression.
Mechanism of action
Erythropoietin has been shown to exert its effects by binding to the erythropoietin receptor (EpoR).
EPO is highly glycosylated (40% of total molecular weight), with half-life in blood around five hours. EPO's
half-life may vary between endogenous and various recombinant versions. Additional glycosylation or other
alterations of EPO via recombinant technology have led to the increase of EPO's stability in blood (thus requiring
less frequent injections). EPO binds to the erythropoietin receptor on the red cell progenitor surface and activates a
JAK2 signaling cascade. Erythropoietin receptor expression is found in a number of tissues, such as bone marrow
and peripheral/central nervous tissue. In the bloodstream, red cells themselves do not express erythropoietin receptor,
so cannot respond to EPO. However, indirect dependence of red cell longevity in the blood on plasma erythropoietin
levels has been reported, a process termed neocytolysis.
Synthesis and regulation
Erythropoietin levels in blood are quite low in the absence of anemia, at around 10 mU/ml. However, in hypoxic
stress, EPO production may increase 1000-fold, reaching 10,000 mU/ml of blood. EPO is produced mainly by
peritubular capillary lining cells of the renal cortex, which are highly specialized, epithelial-like cells. It is
synthesized by renal peritubular cells in adults, with a small amount being produced in the liver. Regulation is
believed to rely on a feedback mechanism measuring blood oxygenation. Constitutively synthesized transcription
factors for EPO, known as hypoxia-inducible factors, are hydroxylated and proteosomally digested in the presence of
oxygen.
Medical uses
Erythropoietins available for use as therapeutic agents are produced by recombinant DNA technology in cell culture,
and include Epogen/Procrit (epoetin alfa) and Aranesp (darbepoetin alfa); they are used in treating anemia resulting
from chronic kidney disease, inflammatory bowel disease (Crohn's disease and ulcer colitis) and myelodysplasia
from the treatment of cancer (chemotherapy and radiation), but include boxed warnings of increased risk of death,
myocardial infarction, stroke, venous thromboembolism, tumor recurrence, and other severe off-target effects.
103
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
104
Available forms
Recombinant EPO has a variety of glycosylation patterns giving rise to alfa, beta, delta, and omega forms:
epoetin alfa:
epoetin beta:
NeoRecormon, made by HoffmannLa Roche
Recormon
Methoxy polyethylene glycol-epoetin beta (Mircera) by Roche
epoetin delta:
Darbepoetin (Aranesp)
Epocept (Lupin pharma)
Nanokine (Nanogen Pharmaceutical biotechnology, Vietnam
Epofit (Intas pharma)
Epogen, made by Amgen
Epogin
Eprex, made by Janssen-Cilag
Binocrit, made by Sandoz
Procrit
Dynepo trademark name for an erythropoiesis stimulating
protein, by Shire plc
epoetin zeta (biosimilar forms for epoetin alpha):
Silapo (Stada)
Retacrit (Hospira)
Miscellaneous:
Epocept, made by Lupin Pharmaceuticals
EPOTrust, made by Panacea Biotec Ltd
Erypro Safe, made by Biocon Ltd.
Repoitin, made by Serum Institute of India Limited
Vintor, made by Emcure Pharmaceuticals
Epofit, made by Intas pharma
Erykine, made by Intas Biopharmaceutica
Wepox, made by Wockhardt Biotech
Espogen, made by LG life sciences.
ReliPoietin, made by Reliance Life Sciences
Shanpoietin, made by Shantha Biotechnics Ltd
Zyrop, made by Cadila Healthcare Ltd.
EPIAO (rHuEPO), made by Shenyang Sunshine Pharmaceutical
Co.. LTD. China
epoetin omega:
Epomax
Darbepoetin alfa is a form created by five substitutions (Asn-57, Thr-59, Val-114, Asn-115 and Thr-117) that create
two new N-glycosylation sites.
More recently, a novel erythropoiesis-stimulating protein (NESP) has been produced. This glycoprotein
demonstrates anti-anemic capabilities and has a longer terminal half-life than erythropoietin. NESP offers chronic
renal-failure patients a lower dose of hormones to maintain normal hemoglobin levels.
Blood doping
Erythropoiesis-stimulating agents (ESAs) have a history of use as blood doping agents in endurance sports, such as
horseracing, boxing, cycling, rowing, distance running, race walking, snowshoeing, cross country skiing, biathlon,
and triathlon. The overall oxygen delivery system (blood oxygen levels, as well as heart stroke volume,
vascularization, and lung function) is one of the major limiting factors to muscles' ability to perform endurance
exercise. Therefore, the primary reason athletes may use ESAs is to improve oxygen delivery to muscles, which
directly improves their endurance capacity. With the advent of recombinant erythropoietin in the 1990s, the practice
of autologous and homologous blood transfusion has been partially replaced by injecting erythropoietin such that the
body naturally produces its own red cells. ESAs increase hematocrit (% of blood volume that is red cell mass) and
total red cell mass in the body, providing a good advantage in sports where such practice is banned. In addition to
ethical considerations in sports, providing an increased red cell mass beyond the natural levels reduces blood flow
due to increased viscosity, and increases the likelihood of thrombosis and stroke. Due to dangers associated with
using ESAs, their use should be limited to the clinic where anemic patients are boosted back to normal hemoglobin
levels (as opposed to going above the normal levels for performance advantage, leading to an increased risk of
death).
Though EPO was believed to be widely used in the 1990s in certain sports, there was no way at the time to directly
test for it, until in 2000, when a test developed by scientists at the French national antidoping laboratory (LNDD) and
endorsed by the World Anti-Doping Agency (WADA) was introduced to detect pharmaceutical EPO by
distinguishing it from the nearly identical natural hormone normally present in an athlete's urine.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
In 2002, at the Winter Olympic Games in Salt Lake City, Dr. Don Catlin, the founder and then-director of the UCLA
Olympic Analytical Lab, reported finding darbepoetin alfa, a form of erythropoietin, in a test sample for the first
time in sports. At the 2012 Summer Olympics in London, Alex Schwazer, the gold medalist in the 50-kilometer race
walk in the 2008 Summer Olympics in Beijing, tested positive for EPO and was disqualified.[67]
Since 2002, EPO tests performed by US sports authorities have consisted of only a urine or "direct" test. From
20002006, EPO tests at the Olympics were conducted on both blood and urine. However, several compounds have
been identified that can be taken orally to stimulate endogenous EPO production. Most of the compounds stabilize
the hypoxia-inducible transcription factors which activate the EPO gene. The compounds include oxo-glutarate
competitors, but also simple ions such as cobalt(II) chloride. [68]
Cycling
Synthetic EPO is believed to have come into use in cycling about 1990. In theory, EPO use can increase VO2max by
a significant amount, making it useful for endurance sports like cycling. Italian antidoping advocate Sandro Donati
has claimed that the history of doping in cycling can be traced to the Italian Dr Francesco Conconi at the University
of Ferrara. Conconi had worked on the idea of giving athletes tranfusions of their own blood in the 1980s. Donati felt
this work "opened the road to EPO . . . because blood doping was a trial to understand the role of EPO".
Dr Michele Ferrari, a former student and mentee of Conconi, had a controversial interview mentioning the drug in
1994, just after his Gewiss-Ballan team had a remarkable performance in the La Flche Wallonne race. Ferrari told
l'Equipe journalist Jean-Michel Rouet that EPO had no "fundamental" effect on performance and that if his riders
used it, it wouldn't "scandalize" himself. After the journalist pointed out several riders were suspected of dying from
EPO, Ferrari said EPO was not dangerous, and only abuse of it was dangerous, saying, "It's also dangerous to drink
10 liters of orange juice." The 'orange juice' comment has been widely misquoted.[69] Ferrari was fired shortly after,
but continued to work in the industry. That same year, Sandro Donati, working for the Italian National Olympic
Committee, presented a report accusing Conconi of being linked to the use of EPO in the sport.
In 1997, the Union Cycliste Internationale (UCI) instituted a new rule that riders testing above 50% haematocrit
were not allowed to race. Robert Millar, former racer, later wrote for Cycling News that the 50% limit was "an open
invitation to dope to that level", pointing out that normally haematocrit levels would start "around 40-42%" and drop
during the course of a "grand tour", but after EPO, they were staying at 50% for "weeks at a time". By 1998, EPO
use had become widespread, and the Festina affair tarnished the 1998 Tour de France. One manager offered a
270,000-franc-per-month raise to Christophe Bassons if he would use EPO, but Bassons refused.
In the 1998 Tour de France Stuart O'Grady won one stage, held the Tour de France yellow jersey for three days, and
came second in the points classification with the assistance of EPO. In 2010, Floyd Landis admitted to using
performance-enhancing drugs, including EPO, throughout his career as a professional cyclist. In 2012, the USADA
released a report on its investigation into the US Postal Service cycling team and blood doping. The report contained
affidavits from numerous riders on the team, including Frankie Andreu, Tyler Hamilton, George Hincapie, Floyd
Landis, Levi Leipheimer, and others, outlining that they, and Lance Armstrong, used a cocktail of
performance-enhancing substances for the Tour de France, most notably EPO, during the 1999 tour. Armstrong was
later stripped of his seven tour wins by USADA, and the UCI concurred with the decision. Tour organisers have
removed Armstrong's name and results from the race's history. Witnesses testified that code words used for EPO
included "Edgar", "Poe", "Edgar Allen Poe", and "Zumo" (Spanish for 'juice').
105
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
History
In 1905, Paul Carnot, a professor of medicine in Paris, and his assistant, Clotilde Deflandre, proposed the idea that
hormones regulate the production of red blood cells. After conducting experiments on rabbits subject to bloodletting,
Carnot and Deflandre attributed an increase in red blood cells in rabbit subjects to a hemotropic factor called
hemopoietin. Eva Bonsdorff and Eeva Jalavisto continued to study red cell production and later called the
hemopoietic substance 'erythropoietin'. Further studies investigating the existence of EPO by K.R. Reissman
(unknown location) and Allan J. Erslev (Thomas Jefferson Medical College) demonstrated that a certain substance,
circulated in the blood, is able to stimulate red blood cell production and increase hematocrit. This substance was
finally purified and confirmed as erythropoietin, opening doors to therapeutic uses for EPO in diseases such as
anemia.
Haematologist John Adamson and nephrologist Joseph W. Eschbach looked at various forms of renal failure and the
role of the natural hormone EPO in the formation of red blood cells. Studying sheep and other animals in the 1970s,
the two scientists helped establish that EPO stimulates the production of red cells in bone marrow and could lead to a
treatment for anemia in humans. In 1968, Goldwasser and Kung began work to purify human EPO, and managed to
purify milligram quantities of over 95% pure material by 1977. Pure EPO allowed the amino acid sequence to be
partially identified and the gene to be isolated. Later, an NIH-funded researcher at Columbia University discovered a
way to synthesize EPO. Columbia University patented the technique, and licensed it to Amgen. Controversy has
ensued over the fairness of the rewards that Amgen reaped from NIH-funded work, and Goldwasser was never
financially rewarded for his work.
In the 1980s, Adamson, Joseph W. Eschbach, Joan C. Egrie, Michael R. Downing and Jeffrey K. Browne conducted
a clinical trial at the Northwest Kidney Centers for a synthetic form of the hormone, Epogen, produced by Amgen.
The trial was successful, and the results were published in the New England Journal of Medicine in January 1987.
In 1985, Lin et al isolated the human erythropoietin gene from a genomic phage library and were able to characterize
it for research and production. Their research demonstrated the gene for erythropoietin encoded the production of
EPO in mammalian cells that is biologically active in vitro and in vivo. The industrial production of recombinant
human erythropoietin (RhEpo) for treating anemia patients would begin soon after.
In 1989, the US Food and Drug Administration approved the hormone Epogen, which remains in use today.
References
[1] http:/ / www. ebi. ac. uk/ pdbe/ searchResults. html?display=both&
term=P01588%20or%20P33707%20or%20P48617%20or%20P07321%20or%20Q0VED9%20or%20P29676%20or%20B1N8Y1
[2] http:/ / www. rcsb. org/ pdb/ search/ smartSubquery. do?smartSearchSubtype=UpAccessionIdQuery&
accessionIdList=P01588,P33707,P48617,P07321,Q0VED9,P29676,B1N8Y1
[3] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1BUY
[4] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1CN4
[5] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1EER
[6] http:/ / www. genenames. org/ data/ hgnc_data. php?hgnc_id=3415
[7] http:/ / omim. org/ entry/ 133170
[8] http:/ / www. informatics. jax. org/ searches/ accession_report. cgi?id=MGI:95407
[9] http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?cmd=Retrieve& db=homologene& dopt=HomoloGene& list_uids=624
[10] https:/ / www. ebi. ac. uk/ chembldb/ index. php/ target/ inspect/ CHEMBL5837
[11] http:/ / www. genecards. org/ cgi-bin/ carddisp. pl?id_type=entrezgene& id=2056
[12] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005128
[13] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005179
[14] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005515
[15] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0030295
[16] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043499
[17] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005576
[18] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005615
[19] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0006915
106
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
[20]
[21]
[22]
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007165
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007566
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007568
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0008015
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0008284
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0009651
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0010766
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0018105
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0032413
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0032496
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0033033
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0033189
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0033554
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0033574
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0042523
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0042541
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043066
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043249
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043627
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0045666
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0045740
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0045893
[42] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0046579
[43] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0048678
[44] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0051602
[45] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0055093
[46] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0061418
[47] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0070555
[48] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0071456
[49] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0071474
[50] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ gp-assoc. cgi?gp=UniProtKB:P01588
[51] http:/ / www. ebi. ac. uk/ QuickGO/ GProtein?ac=P01588
[52] http:/ / biogps. org/ gene/ 2056/
[53] http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?db=gene& cmd=retrieve& dopt=default& list_uids=2056& rn=1
[54] http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?db=gene& cmd=retrieve& dopt=default& list_uids=13856& rn=1
[55] http:/ / www. ensembl. org/ Homo_sapiens/ geneview?gene=ENSG00000130427;db=core
[56] http:/ / www. ensembl. org/ Mus_musculus/ geneview?gene=ENSMUSG00000029711;db=core
[57] http:/ / www. uniprot. org/ uniprot/ P01588
[58] http:/ / www. uniprot. org/ uniprot/ P07321
[59] http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NM_000799
[60] http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NM_007942
[61] http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NP_000790
[62] http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NP_031968
[63] http:/ / genome. ucsc. edu/ cgi-bin/ hgTracks?org=Human& db=hg19& position=chr7:100318423-100321323
[64] http:/ / genome. ucsc. edu/ cgi-bin/ hgTracks?org=Mouse& db=mm9& position=chr5:137482259-137533242
[65] http:/ / www. ncbi. nlm. nih. gov/ sites/ entrez?db=gene& cmd=Link& LinkName=gene_pubmed& from_uid=2056
[66] http:/ / www. ncbi. nlm. nih. gov/ sites/ entrez?db=gene& cmd=Link& LinkName=gene_pubmed& from_uid=13856
[67] "Ousted Olympic race walk champion says he bought EPO in Turkey, hid it in refrigerator at home" (http:/ / www. washingtonpost. com/
sports/ olympics/ 2008-olympic-race-walk-champ-i-bought-epo-in-turkey-hid-doping-from-kostner-im-destroyed/ 2012/ 08/ 29/
5c7b3c7a-e14d-11e1-89f7-76e23a982d06_story. html) Associated Press story in the Washington Post (August 8, 2012)
[68] W. Jelkmann: The disparate roles of cobalt in erythropoiesis, and doping relevance. Open Journal of Hematology, 2012, 3-6. http:/ /
rossscience. org/ ojhmt/ 2075-907X-3-6. php
[69] 10 liters of orange juice: see the article on Water intoxication, for example.
107
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Erythropoietin
Further reading
Takeuchi M, Kobata A (1992). "Structures and functional roles of the sugar chains of human erythropoietins".
Glycobiology 1 (4): 33746. doi: 10.1093/glycob/1.4.337 (http://dx.doi.org/10.1093/glycob/1.4.337).
PMID 1820196 (http://www.ncbi.nlm.nih.gov/pubmed/1820196).
Semba RD, Juul SE (2002). "Erythropoietin in human milk: physiology and role in infant health". Journal of
human lactation : official journal of International Lactation Consultant Association 18 (3): 25261. PMID
12192960 (http://www.ncbi.nlm.nih.gov/pubmed/12192960).
Ratcliffe PJ (2003). "From erythropoietin to oxygen: hypoxia-inducible factor hydroxylases and the hypoxia
signal pathway". Blood Purif. 20 (5): 44550. doi: 10.1159/000065201 (http://dx.doi.org/10.1159/
000065201). PMID 12207089 (http://www.ncbi.nlm.nih.gov/pubmed/12207089).
Westenfelder, Christof (2002). "Unexpected renal actions of erythropoietin". Exp. Nephrol. 10 (56): 2948. doi:
10.1159/000065304 (http://dx.doi.org/10.1159/000065304). PMID 12381912 (http://www.ncbi.nlm.nih.
gov/pubmed/12381912).
Becerra SP, Amaral J (2002). "Erythropoietin--an endogenous retinal survival factor". N. Engl. J. Med. 347 (24):
196870. doi: 10.1056/NEJMcibr022629 (http://dx.doi.org/10.1056/NEJMcibr022629). PMID 12477950
(http://www.ncbi.nlm.nih.gov/pubmed/12477950).
Genc S, Koroglu TF, Genc K (2004). "Erythropoietin and the nervous system". Brain Res. 1000 (12): 1931.
doi: 10.1016/j.brainres.2003.12.037 (http://dx.doi.org/10.1016/j.brainres.2003.12.037). PMID 15053948
(http://www.ncbi.nlm.nih.gov/pubmed/15053948).
Fandrey J (2004). "Oxygen-dependent and tissue-specific regulation of erythropoietin gene expression". Am. J.
Physiol. Regul. Integr. Comp. Physiol. 286 (6): R97788. doi: 10.1152/ajpregu.00577.2003 (http://dx.doi.org/
10.1152/ajpregu.00577.2003). PMID 15142852 (http://www.ncbi.nlm.nih.gov/pubmed/15142852).
Juul S (2004). "Recombinant erythropoietin as a neuroprotective treatment: in vitro and in vivo models". Clinics
in perinatology 31 (1): 12942. doi: 10.1016/j.clp.2004.03.004 (http://dx.doi.org/10.1016/j.clp.2004.03.
004). PMID 15183662 (http://www.ncbi.nlm.nih.gov/pubmed/15183662).
Buemi M, Caccamo C, Nostro L, et al. (2005). "Brain and cancer: the protective role of erythropoietin". Med Res
Rev 25 (2): 24559. doi: 10.1002/med.20012 (http://dx.doi.org/10.1002/med.20012). PMID 15389732
(http://www.ncbi.nlm.nih.gov/pubmed/15389732).
Sytkowski AJ (2007). "Does erythropoietin have a dark side? Epo signaling and cancer cells". Sci. STKE 2007
(395): e38. doi: 10.1126/stke.3952007pe38 (http://dx.doi.org/10.1126/stke.3952007pe38). PMID 17636183
(http://www.ncbi.nlm.nih.gov/pubmed/17636183).
Goldwasser, Eugene. A Bloody Long Journey: Erythropoietin and the Person Who Isolated It. Xlibris, 2011.
ISBN 978-1-4568-5737-0
External links
NYT - 1987 announcement of Epogen's clinical success (http://query.nytimes.com/gst/fullpage.
html?res=9B0DE2D81138F93BA35752C0A961948260&sec=&spon=&partner=permalink&
exprod=permalink)
108
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Calcium metabolism
109
Calcium metabolism
Calcium metabolism or calcium
homeostasis is the mechanism by
which the body maintains adequate
calcium levels. Derangements of this
mechanism lead to hypercalcemia or
hypocalcemia, both of which can have
important consequences for health.
Calcium
Calcium location and quantity
Calcium is the most abundant mineral in the human body. The average adult body contains in total approximately
1kg, 99% in the skeleton in the form of calcium phosphate salts. The extracellular fluid (ECF) contains
approximately 22.5mmol, of which about 9mmol is in the plasma. Approximately 500mmol of calcium is
exchanged between bone and the ECF over a period of twenty-four hours.
Biological functions
Structural function: Supporting material in bones. Present as calcium phosphate.
Signalling function: Intracellular calcium functions as a second messenger for the secretion of some hormones
and neurotransmitters. Also acts as an intracellular permeation regulator and mediator of muscle contraction.
Enzymatic function: Calcium acts as a coenzyme for clotting factors.
Calcium also causes the release of Acetylcholine from pre-synaptic terminals in the transmission of nerve impulses.
Calcium causes the contraction of muscles, removing the Triosephosphate isomerase (TPI) subunit from Myosin
head which has ATPase activity to cause contraction.
Normal ranges
The plasma level of calcium is closely regulated with a normal total calcium of 2.2-2.6mmol/L (9-10.5mg/dL) and
a normal ionized calcium of 1.1-1.4mmol/L (4.5-5.6mg/dL). The amount of total calcium varies with the level of
serum albumin, a protein to which calcium is bound. The biologic effect of calcium is determined by the amount of
ionized calcium, rather than the total calcium. Ionized calcium does not vary with the albumin level, and therefore it
is useful to measure the ionized calcium level when the serum albumin is not within normal ranges, or when a
calcium disorder is suspected despite a normal total calcium level.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Calcium metabolism
Corrected calcium level
One can derive a corrected calcium (also known as adjusted calcium) level, to allow for the change in total calcium
due to the change in albumin-bound calcium. This gives an estimate of what the total calcium level would be if the
albumin were a specified normal value. Exact formulae used to derive corrected calcium may depend on the
analytical methods used for calcium and albumin. However the traditional method of calculating it is shown below.
Corrected calcium (mg/dL) = measured total Ca (mg/dL) + 0.8 (4.0 - serum albumin [g/dL]), where 4.0
represents the average albumin level in g/dL.
in other words, each 1 g/dL decrease of albumin will decrease 0.8mg/dL in measured serum Ca and thus 0.8 must be
added to the measured Calcium to get a corrected Calcium value.
Or: Corrected calcium (mmol/L) = measured total Ca (mmol/L) + 0.02 (40 - serum albumin [g/L]), where 40
represents the average albumin level in g/L
in other words, each 1 g/L decrease of albumin, will decrease 0.02mmol/L in measured serum Ca and thus 0.02
must be added to the measured value to take this into account and get a corrected calcium.
When there is hypoalbuminemia (a lower than normal albumin), the corrected calcium level is higher than the total
calcium.
Effector organs
Absorption
About 25 mmol of calcium enters the body in a normal diet. Of this, about 40% (10mmol) is absorbed in small
intestine, and 5mmol leaves the body in feces, netting 5mmol of calcium a day.[1]
Calcium is absorbed across the intestinal brush border membrane, passing through ion channels such as TRPV6.
Calbindin is a vitamin D-dependent calcium-binding protein inside intestinal epithelial cells which functions together
with TRPV6 and calcium pumps (PMCA1) in the basal membrane to actively transport calcium into the body.
Active transport of calcium occurs primarily in the duodenum portion of the intestine when calcium intake is low;
and through passive paracellular transport occurs in the jejunum and ileum parts when calcium intake is high,
independent of Vitamin D level.[2]
Excretion
The kidney excretes 250mmol a day in pro-urine, and resorbs 245mmol, leading to a net loss in the urine of
5mmol/d. In addition to this, the kidney processes Vitamin D into calcitriol, the active form that is most effective in
assisting intestinal absorption. Both processes are stimulated by parathyroid hormone.
The role of bone
Although calcium flow to and from the bone is neutral, about 5mmol is turned over a day. Bone serves as an
important storage point for calcium, as it contains 99% of the total body calcium. Calcium release from bone is
regulated by parathyroid hormone. Calcitonin stimulates incorporation of calcium in bone, although this process is
largely independent of calcitonin.
Low calcium intake may also be a risk factor in the development of osteoporosis. In one meta-analysis, the authors
found that fifty out of the fifty-two studies that they reviewed showed that calcium intake promoted better bone
balance. With a better bone balance, the risk of osteoporosis is lowered.
110
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Calcium metabolism
111
Interaction with other chemicals
Potential positive interactions
Vitamin D is an important co-factor in the intestinal absorption of calcium, as it increases the number of calcium
binding proteins, involved in calcium absorption through the apical membrane of enterocytes in small intestine. It
also promotes re-absorption of calcium in the kidneys.[citation needed]
Magnesium also plays an important role in calcium absorption by bones. Release of calcium from the
sarcoplasmic reticulum is inhibited by magnesium. Thus hypomagnesemia results in an increased intracellular
calcium level. This inhibits the release of parathyroid hormone, which can result in hypoparathyroidism and
hypocalcemia. Furthermore, it makes skeletal and muscle receptors less sensitive to parathyroid hormone. [citation
needed]
Boron[citation needed]
Potential negative interactions
"Unesterified long-chain saturated fatty acids, i.e. palmitic acid, have a melting point above body temperature
and, with sufficient calcium in the intestinal lumen, form insoluble calcium soaps."
Sodium binding to calcium
Phytic acid binding to calcium
Oxalic acid binding to calcium
Cortisol binding to calcium
Low pH food and proteins (the latter promotes gastric acid)[citation needed]
Regulatory organs
Primarily calcium is regulated by the actions of
1,25-Dihydroxycholecalciferol, parathyroid hormone
(PTH) and calcitonin and direct exchange with the bone
matrix. Plasma calcium levels are regulated by
hormonal and non-hormonal mechanisms. After
ingestion of substantial amounts of calcium the short
term control that prevents calcium spiking in the serum
is absorption by the bone matrix. After about an hour,
PTH will be released and not peak for about 8 hours.[4]
The PTH is, over time, a very potent regulator of
plasma calcium, and controls the conversion of vitamin
D into its active form in the kidney. The parathyroid
glands are located behind the thyroid, and produce
parathyroid hormone in response to low calcium levels.
The parafollicular cells of the thyroid produce
calcitonin in response to high calcium levels, but its
significance is much smaller than that of PTH.
[3]
Calcium regulation in the human body.
Pathology
Hypocalcemia and hypercalcemia are both serious medical disorders.
Renal osteodystrophy is a consequence of chronic renal failure related to the calcium metabolism.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Calcium metabolism
Osteoporosis and osteomalacia have been linked to calcium metabolism disorders.
Research into cancer prevention
The role that calcium might have in reducing the rates of colorectal cancer has been the subject of many studies.
However, given its modest efficacy, there is no current medical recommendation to use calcium for cancer reduction.
Several epidemiological studies suggest that people with high calcium intake have a reduced risk of colorectal
cancer. These observations have been confirmed by experimental studies in volunteers and in rodents. One large
scale clinical trial shows that 1.2 g calcium each day reduces, modestly, intestinal polyps recurrence in volunteers.
Data from the four published trials are available.[5] Some forty carcinogenesis studies in rats or mice, reported in the
Chemoprev.Database, also support that calcium could prevent intestinal cancer.[6]
References
[1] Barrett KE, Barman SM, Boitano S, Brooks H, "Chapter 23. Hormonal Control of Calcium & Phosphate Metabolism & the Physiology of
Bone" (Chapter). Barrett KE, Barman SM, Boitano S, Brooks H: Ganong's Review of Medical Physiology, 23e: http:/ / www. accessmedicine.
com/ content. aspx?aID=5244785.
[2] http:/ / www. vivo. colostate. edu/ hbooks/ pathphys/ digestion/ smallgut/ absorb_minerals. html
[3] Page 1094 (The Parathyroid Glands and Vitamin D) in:
[4] Medical Physiology; Guyton, Saunders and Co. 1976pp.1062
[5] Potency-Man (http:/ / www. inra. fr/ reseau-nacre/ sci-memb/ corpet/ Data/ table. php?file=Potency-Man. txt)
[6] Calcium meta-analysis Colon Cancer chemoprevention systematic review (http:/ / www. inra. fr/ reseau-nacre/ sci-memb/ corpet/
MAcalcium. html)
External links
Calcium (http://labtestsonline.org/understanding/analytes/calcium/tab/test) at Lab Tests Online
Physiology at MCG 5/5ch6/5ch6line (http://web.archive.org/web/20080401093403/http://www.lib.mcg.
edu/edu/eshuphysio/program/section5/5ch6/5ch6line.htm)
112
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Fluid balance
Fluid balance
Fluid balance is the concept of human homeostasis that the amount of fluid lost from the body is equal to the
amount of fluid taken in. Euvolemia is the state of normal body fluid volume. Water is necessary for all life on Earth.
Humans can survive for 46 weeks without food, but for only a few days without water.
The amount of water varies with the individual, as it depends on the condition of the subject, the amount of physical
exercise, and on the environmental temperature and humidity. In the US, the reference daily intake (RDI) for water is
3.7 litres per day (l/day) for human males older than 18, and 2.7 l/day for human females older than 18[1] including
water contained in food, beverages, and drinking water. The common misconception that everyone should drink two
litres (68 ounces, or about eight 8-oz glasses) of water per day is not supported by scientific research. Various
reviews of all the scientific literature on the topic performed in 2002 and 2008 could not find any solid scientific
evidence that recommended drinking eight glasses of water per day.[2][3] For example, people in hotter climates will
require greater water intake than those in cooler climates. An individual's thirst provides a better guide for how much
water they require rather than a specific, fixed number. A more flexible guideline is that a normal person should
urinate 4 times per day, and the urine should be a light yellow color.
A constant supply is needed to replenish the fluids lost through normal physiological activities, such as respiration,
perspiration and urination. Food contributes 0.5 to 1 l/day, and the metabolism of protein, fat, and carbohydrates
produces another 0.25 to 0.4 l/day,[4] which means that 2 to 3 l/day of water for men and 1 to 2 l/day of water for
women should be taken in as fluid, i.e. drunk, in order to meet the Recommended Daily Intake (RDI). In terms of
mineral nutrients intake, it is unclear what the drinking water contribution is. However, inorganic minerals generally
enter surface water and ground water via storm water runoff or through the Earth's crust. Treatment processes also
lead to the presence of some minerals. Examples include calcium, zinc, manganese, phosphate, fluoride and sodium
compounds.[5] Water generated from the biochemical metabolism of nutrients provides a significant proportion of
the daily water requirements for some arthropods and desert animals, but provides only a small fraction of a human's
necessary intake. There are a variety of trace elements present in virtually all potable water, some of which play a
role in metabolism. For example sodium, potassium and chloride are common chemicals found in small quantities in
most waters, and these elements play a role (not necessarily major) in body metabolism. Other elements such as
fluoride, while beneficial in low concentrations, can cause dental problems and other issues when present at high
levels. Water is essential for the growth and maintenance of our bodies, as it is involved in a number of biological
processes.
Profuse sweating can increase the need for electrolyte (salt) replacement. Water intoxication (which results in
hyponatremia), the process of consuming too much water too quickly, can be fatal.
The human kidneys will normally adjust to varying levels of water intake. The kidneys will require time to adjust to
the new water intake level. This can cause someone who drinks a lot of water to become dehydrated more easily than
someone who routinely drinks less.
113
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Fluid balance
Routes of fluid loss and gain
Fluid can leave the body in many ways. Fluid can enter the body as preformed water, ingested food and drink and to
a lesser extent as metabolic water which is produced as a by-product of aerobic respiration (cellular respiration) and
dehydration synthesis.[6]
Input
A constant supply is needed to replenish the fluids lost through normal physiological activities, such as respiration,
sweating and urination. Water generated from the biochemical metabolism of nutrients provides a significant
proportion of the daily water requirements for some arthropods and desert animals, but provides only a small fraction
of a human's necessary intake.
In the normal resting state, input of water through ingested fluids is approximately 1200 ml/day, from ingested foods
1000 ml/day and from aerobic respiration 300 ml/day, totaling 2500 ml/day.[7]
Regulation of input
Input of water is regulated mainly through ingested fluids, which, in turn, depends on thirst. An insufficiency of
water results in an increased osmolarity in the extracellular fluid. This is sensed by osmoreceptors in the organum
vasculosum of the lamina terminalis, which trigger thirst. Thirst can to some degree be voluntarily resisted, as during
fluid restriction.
Output
The majority of fluid output occurs via the urine, approximately 1500 ml/day (approx 1.59 qt/day) in the normal
adult resting state.
Some fluid is lost through perspiration (part of the body's temperature control mechanism) and as water vapor in
expired air. These are termed "insensible fluid losses" as they cannot be easily measured. Some sources say
insensible losses account for 500 to 650 ml/day (0.5 to 0.6 qt.) of water in adults, while other sources put the
minimum value at 800 ml (0.8 qt.).[8] In children, one calculation used for insensible fluid loss is 400ml/m2 body
surface area.
In addition, an adult loses approximately 100ml/day of fluid through feces.
For females, an additional 50 ml/day is lost through vaginal secretions.
These outputs are in balance with the input of ~2500 ml/day.
Regulation of output
The body's homeostatic control mechanisms, which maintain a constant internal environment, ensure that a balance
between fluid gain and fluid loss is maintained. The hormones ADH (Anti-diuretic Hormone, also known as
vasopressin) and Aldosterone play a major role in this.
If the body is becoming fluid-deficient, there will be an increase in the secretion of these hormones, causing fluid
to be retained by the kidneys and urine output to be reduced.
Conversely, if fluid levels are excessive, secretion of these hormones is suppressed, resulting in less retention of
fluid by the kidneys and a subsequent increase in the volume of urine produced.
114
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Fluid balance
Antidiuretic hormone
If the body is becoming fluid-deficient, this will be sensed by osmoreceptors in the organum vasculosum of lamina
terminalis and subfornical organ. These areas project to the supraoptic nucleus and paraventricular nucleus, which
contain neurons that secrete the antidiuretic hormone, vasopressin, from their nerve endings in the posterior pituitary.
Thus, there will be an increase in the secretion of antidiuretic hormone, causing fluid to be retained by the kidneys
and urine output to be reduced.
Aldosterone
A fluid-insufficiency causes a decreased perfusion of the juxtaglomerular apparatus in the kidneys. This activates the
renin-angiotensin system. Among other actions, it causes renal tubules (i.e. the distal convoluted tubules and the
cortical collecting ducts) to reabsorb more sodium and water from the urine. Potassium is secreted into the tubule in
exchange for the sodium, which is reabsorbed. The activated renin-angiotensin system stimulates zona glomerulosa
of the adrenal cortex which in turn secretes hormone aldosterone. This hormone stimulates the reabsorption of
sodium ions from distal tubules and collecting ducts. Water in the tubular lumen cannot follow the sodium
reabsorption osmotically, as this part of the kidney is impermeable to water; release of AHD (vasopressin) is
required to increase expression of aquaporin channels in the cortical collecting duct, allowing reabsorption of water.
Effects of illness
When a person is ill, fluid may also be lost through vomiting, diarrhea, and hemorrhage. An individual is at an
increased risk of dehydration in these instances, as the kidneys will find it more difficult to match fluid loss by
reducing urine output (the kidneys must produce at least some urine in order to excrete metabolic waste.)
Fluid balance in an acute hospital setting
In an acute hospital setting, fluid balance is monitored carefully. This provides information on the patient's state of
hydration, renal function and cardiovascular function.
If fluid loss is greater than fluid gain (for example if the patient vomits and has diarrhoea), the patient is said to be
in negative fluid balance. In this case, fluid is often given intravenously to compensate for the loss.
On the other hand, a positive fluid balance (where fluid gain is greater than fluid loss) might suggest a problem
with either the renal or cardiovascular system.
If blood pressure is low (hypotension), the filtration rate in the kidneys will lessen, causing less fluid reabsorption
and thus less urine output.
An accurate measure of fluid balance is therefore an important diagnostic tool, and allows for prompt intervention to
correct the imbalance.
115
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Fluid balance
Trace elements
There are a variety of trace elements present in virtually all potable water, some of which play a role in metabolism;
for example sodium, potassium and chloride are common chemicals found in very small amounts in most waters, and
these elements play a major role in body metabolism. Water is essential for the growth and maintenance of our
bodies, as it is involved in a number of biological processes.
References
[1] US daily reference intake values (http:/ / iom. edu/ Reports/ 2004/ Dietary-Reference-Intakes-Water-Potassium-Sodium-Chloride-and-Sulfate.
aspx)
[2] Research debunks health value of guzzling water (http:/ / www. reuters. com/ article/ healthNews/ idUSN0236679720080402). Reuters, April
2008.
[3] H. Valtin, Drink at least eight glasses of water a day." Really? Is there scientific evidence for "8 8"? (http:/ / ajpregu. physiology. org/ cgi/
content/ full/ 283/ 5/ R993) Am J Physiol Regul Integr Comp Physiol 283: R993-R1004, 2002.
[4] Swedish DFA (http:/ / www. slv. se/ templates/ SLV_Page. aspx?id=13974& epslanguage=SV) (in Swedish)
[5] World Health Organization (http:/ / www. who. int/ en/ ) (WHO). Geneva, Switzerland. Joyce Morrissey Donohue, Charles O. Abernathy,
Peter Lassovszky, George Hallberg. "The contribution of drinking-water to total dietary intakes of selected trace mineral nutrients in the
United States." (http:/ / www. who. int/ entity/ water_sanitation_health/ dwq/ nutintakes. pdf) Draft, August 2004.
[6] Saladin, Kenneth S. Water, Electrolyte, and Acid-Base Balance (New York: McGraw-Hill Companies, Inc., 2010), 943-944.
[7] Page 829
[8] 3.2 Insensible Water Loss (http:/ / www. anaesthesiamcq. com/ FluidBook/ fl3_2. php)
116
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
117
Vasopressin
Arginine vasopressin
Space-filling model of arginine vasopressin
Available structures
PDB Ortholog search: PDBe [1], RCSB [2]
List of PDB id codes
1jk4
[3]
, 1jk6
[4]
, 1npo
[5]
, 2bn2
[6]
Identifiers
[7]
Symbols
AVP
External IDs
OMIM: 192340
; ADH; ARVP; AVP-NPII; AVRP; VP
[8]
MGI: 88121
[9]
HomoloGene: 417
[10]
GeneCards: AVP Gene
[11]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
118
Gene Ontology
Molecular function protein kinase activity [12]
[13]
signal transducer activity
[14]
receptor binding
[15]
neuropeptide hormone activity
[16]
neurohypophyseal hormone activity
[17]
V1A vasopressin receptor binding
[18]
V1B vasopressin receptor binding
[19]
cysteine-type endopeptidase inhibitor activity involved in apoptotic process
Cellular component extracellular region [17]
[18]
extracellular space
[20]
cytosol
[21]
secretory granule
[22]
dendrite
Biological process
[23]
maternal aggressive behavior
[24]
positive regulation of systemic arterial blood pressure
[25]
generation of precursor metabolites and energy
[26]
protein phosphorylation
[27]
water transport
[20]
signal transduction
[28]
elevation of cytosolic calcium ion concentration
[29]
cell-cell signaling
[30]
negative regulation of female receptivity
[31]
grooming behavior
[32]
locomotory behavior
[24]
positive regulation of cell proliferation
[33]
positive regulation of gene expression
[34]
positive regulation of glutamate secretion
[35]
positive regulation of cell growth
[36]
positive regulation of cAMP biosynthetic process
[37]
positive regulation of prostaglandin biosynthetic process
[38]
positive regulation of cellular pH reduction
[39]
positive regulation of peptidyl-serine phosphorylation
[40]
response to nicotine
[41]
social behavior
[42]
regulation of renal sodium excretion
[43]
vasoconstriction
[44]
hyperosmotic salinity response
[45]
maternal behavior
[36]
negative regulation of apoptotic process
[46]
penile erection
negative regulation of cysteine-type endopeptidase activity involved in apoptotic process
[47]
[48]
sodium-independent organic anion transport
[49]
response to ethanol
[50]
positive regulation of vasoconstriction
[51]
multicellular organismal water homeostasis
[52]
negative regulation of transmission of nerve impulse
[53]
transmembrane transport
[54]
ERK1 and ERK2 cascade
[55]
protein kinase C signaling cascade
[56]
negative regulation of release of cytochrome c from mitochondria
Sources: Amigo
[57]
/ QuickGO
[58]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
119
RNA expression pattern
More reference expression data
[59]
Orthologs
Species
Human
Mouse
Entrez
551
Ensembl
ENSG00000101200
UniProt
P01185
RefSeq (mRNA)
NM_000490
RefSeq (protein)
NP_000481
Location (UCSC)
Chr 20:
[70]
3.06 3.07 Mb
Chr 2:
[71]
130.58 130.58 Mb
PubMed search
[72]
[73]
[60]
11998
[64]
[62]
[61]
ENSMUSG00000037727
P35455
[66]
[68]
[63]
[65]
NM_009732
NP_033862
[67]
[69]
Arginine vasopressin (AVP), also known as vasopressin, argipressin or antidiuretic hormone (ADH), is a
neurohypophysial hormone found in most mammals. Its two primary functions are to retain water in the body and to
constrict blood vessels. Vasopressin regulates the body's retention of water by acting to increase water absorption in
the collecting ducts of the kidney nephron. Vasopressin is a peptide hormone that increases water permeability of the
kidney's collecting duct and distal convoluted tubule by inducing translocation of aquaporin-CD water channels in
the kidney nephron collecting duct plasma membrane. It also increases peripheral vascular resistance, which in turn
increases arterial blood pressure. It plays a key role in homeostasis, by the regulation of water, glucose, and salts in
the blood. It is derived from a preprohormone precursor that is synthesized in the hypothalamus and stored in
vesicles at the posterior pituitary. Most of it is stored in the posterior pituitary to be released into the bloodstream.
However, some AVP may also be released directly into the brain, and accumulating evidence suggests it plays an
important role in social behavior, sexual motivation and bonding, and maternal responses to stress. It has a very short
half-life between 16-24 minutes.
Physiology
Function
One of the most important roles of AVP is to regulate the body's retention of water; it is released when the body is
dehydrated and causes the kidneys to conserve water, thus concentrating the urine and reducing urine volume. At
high concentrations, it also raises blood pressure by inducing moderate vasoconstriction. In addition, it has a variety
of neurological effects on the brain, having been found, for example, to influence pair-bonding in voles. The
high-density distributions of vasopressin receptor AVPr1a in prairie vole ventral forebrain regions have been shown
to facilitate and coordinate reward circuits during partner preference formation, critical for pair bond formation.
A very similar substance, lysine vasopressin (LVP) or lypressin, has the same function in pigs and is often used in
human therapy.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
120
Kidney
Vasopressin has two main effects by which it contributes to increased urine osmolarity (increased concentration) and
decreased water excretion:
1. Increasing the water permeability of distal tubule and collecting duct cells in the kidney, thus allowing water
reabsorption and excretion of more concentrated urine, i.e., antidiuresis. This occurs through insertion of water
channels (Aquaporin-2) into the apical membrane of distal tubule and collecting duct epithelial cells. Aquaporins
allow water to move down their osmotic gradient and out of the nephron, increasing the amount of water
re-absorbed from the filtrate (forming urine) back into the bloodstream.
V2 receptors, which are G protein-coupled receptors on the basolateral plasma membrane of the epithelial cells,
couple to the heterotrimeric G-protein Gs, which activates adenylyl cyclases III and VI to convert ATP into
cAMP, plus 2 inorganic phosphates. The rise in cAMP then triggers the insertion of aquaporin-2 water channels
by exocytosis of intracellular vesicles, recycling endosomes. Vasopressin also increases the concentration of
calcium in the collecting duct cells, by episodic release from intracellular stores. Vasopressin, acting through
cAMP, also increases transcription of the aquaporin-2 gene, thus increasing the total number of aquaporin-2
molecules in collecting duct cells.
Cyclic-AMP activates protein kinase A (PKA) by binding to its regulatory subunits and allowing them to detach
from the catalytic subunits. Detachment exposes the catalytic site in the enzyme, allowing it to add phosphate
groups to proteins (including the aquaporin-2 protein), which alters their functions.
2. Increasing permeability of the inner medullary portion of the collecting duct to urea by regulating the cell surface
expression of urea transporters, which facilitates its reabsorption into the medullary interstitium as it travels down
the concentration gradient created by removing water from the connecting tubule, cortical collecting duct, and
outer medullary collecting duct.
Cardiovascular system
Vasopressin increases peripheral vascular resistance (vasoconstriction) and thus increases arterial blood pressure.
This effect appears small in healthy individuals; however it becomes an important compensatory mechanism for
restoring blood pressure in hypovolemic shock such as that which occurs during hemorrhage.
Central nervous system
Vasopressin released within the brain has many actions:
It has been implicated in memory formation, including delayed
reflexes, image, short- and long-term memory, though the
mechanism remains unknown; these findings are controversial.
However, the synthetic vasopressin analogue desmopressin has
come to interest as a likely nootropic.
[74]
Avp
is expressed in the periventricular
region of the hypothalamus in the adult mouse.
Allen Brain Atlases
Vasopressin is released into the brain in a circadian rhythm by
neurons of the supraoptic nucleus.
Vasopressin released from centrally projecting hypothalamic
neurons is involved in aggression, blood pressure regulation, and
temperature regulation.
It is likely that vasopressin acts in conjunction with corticotropin-releasing hormone to modulate the release of
corticosteroids from the adrenal gland in response to stress, particularly during pregnancy and lactation in
mammals.
Selective AVPr1a blockade in the ventral pallidum has been shown to prevent partner preference in prairie voles,
suggesting that these receptors in this ventral forebrain region are crucial for pair bonding.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
Recent evidence suggests that vasopressin may have analgesic effects. The analgesia effects of vasopressin were
found to be dependent on both stress and gender.
Evidence for this comes from experimental studies in several species, which indicate that the precise distribution of
vasopressin and vasopressin receptors in the brain is associated with species-typical patterns of social behavior. In
particular, there are consistent differences between monogamous species and promiscuous species in the distribution
of AVP receptors, and sometimes in the distribution of vasopressin-containing axons, even when closely related
species are compared. Moreover, studies involving either injecting AVP agonists into the brain or blocking the
actions of AVP support the hypothesis that vasopressin is involved in aggression toward other males. There is also
evidence that differences in the AVP receptor gene between individual members of a species might be predictive of
differences in social behavior. One study has suggested that genetic variation in male humans affects pair-bonding
behavior. The brain of males uses vasopressin as a reward for forming lasting bonds with a mate, and men with one
or two of the genetic alleles are more likely to experience marital discord. The partners of the men with two of the
alleles affecting vasopressin reception state disappointing levels of satisfaction, affection, and cohesion. Vasopressin
receptors distributed along the reward circuit pathway, to be specific in the ventral pallidum, are activated when
AVP is released during social interactions such as mating, in monogamous prairie voles. The activation of the reward
circuitry reinforces this behavior, leading to conditioned partner preference, and thereby initiates the formation of a
pair bond.
Control
Vasopressin is secreted from the posterior pituitary gland in response to reductions in plasma volume, in response to
increases in the plasma osmolality, and in response to cholecystokinin (CCK) secreted by the small intestine:
Secretion in response to reduced plasma volume is activated by pressure receptors in the veins, atria, and carotids.
Secretion in response to increases in plasma osmotic pressure is mediated by osmoreceptors in the hypothalamus.
Secretion in response to increases in plasma CCK is mediated by an unknown pathway.
The neurons that make AVP, in the hypothalamic supraoptic nuclei (SON) and paraventricular nuclei (PVN), are
themselves osmoreceptors, but they also receive synaptic input from other osmoreceptors located in regions adjacent
to the anterior wall of the third ventricle. These regions include the organum vasculosum of the lamina terminalis
and the subfornical organ.
Many factors influence the secretion of vasopressin:
Ethanol (alcohol) reduces the calcium-dependent secretion of AVP by blocking voltage-gated calcium channels in
neurohypophyseal nerve terminals.
Angiotensin II stimulates AVP secretion, in keeping with its general pressor and pro-volumic effects on the body.
Atrial natriuretic peptide inhibits AVP secretion, in part by inhibiting Angiotensin II-induced stimulation of AVP
secretion.
Secretion
The main stimulus for secretion of vasopressin is increased osmolality of plasma. Reduced volume of extracellular
fluid also has this effect, but is a less sensitive mechanism.
The AVP that is measured in peripheral blood is almost all derived from secretion from the posterior pituitary gland
(except in cases of AVP-secreting tumours). Vasopressin is produced by magnocellular neurosecretory neurons in
the Paraventricular nucleus of hypothalamus (PVN) and Supraoptic nucleus (SON). It then travels down the axon
through the infundibulum within neurosecretory granules that are found within Herring bodies, localized swellings of
the axons and nerve terminals. These carry the peptide directly to the posterior pituitary gland, where it is stored until
released into the blood. However there are two other sources of AVP with important local effects:
121
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
122
AVP is also synthesized by parvocellular neurosecretory neurons at the PVN, transported and released at the
median eminence, which then travels through the hypophyseal portal system to the anterior pituitary where it
stimulates corticotropic cells synergistically with CRH to produce ACTH (by itself it is a weak secretagogue).
Vasopressin is also released into the brain by several different populations of smaller neurons.
Receptors
Below is a table summarizing some of the actions of AVP at its four receptors, differently expressed in different
tissues and exerting different actions:
Type
Second messenger system
Locations
AVPR1A
Phosphatidylinositol/calcium Liver, kidney, peripheral
vasculature, brain
Vasoconstriction, gluconeogenesis, platelet aggregation, and release
of factor VIII and von Willebrand factor; social recognition,
circadian tau
AVPR1B
or AVPR3
Phosphatidylinositol/calcium Pituitary gland, brain
Adrenocorticotropic hormone secretion in response to stress; social
interpretation of olfactory cues
AVPR2
Adenylate cyclase/cAMP
Insertion of aquaporin-2 (AQP2) channels (water channels). This
allows water to be reabsorbed down an osmotic gradient, and so the
urine is more concentrated. Release of von Willebrand factor and
surface expression of P-selectin through exocytosis of
Weibel-Palade bodies from endothelial cells
VACM-1
Phosphatidylinositol/calcium Vascular endothelium and renal
collecting tubules
Basolateral membrane of the
cells lining the collecting ducts of
the kidneys (especially the
cortical and outer medullary
collecting ducts)
Actions
Increases cytosolic calcium and acts as an inverse agonist of cAMP
accumulation
Structure and relation to oxytocin
The vasopressins are peptides consisting of nine amino acids
(nonapeptides). (NB: the value in the table above of 164 amino acids is
that obtained before the hormone is activated by cleavage). The amino
acid
sequence
of
arginine
vasopressin
is
Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly, with the cysteine residues
forming a disulfide bond. Lysine vasopressin has a lysine in place of
the arginine.
The structure of oxytocin is very similar to that of the vasopressins: It
is also a nonapeptide with a disulfide bridge and its amino acid
sequence differs at only two positions (see table below). The two genes
are located on the same chromosome separated by a relatively small
distance of less than 15,000 bases in most species. The magnocellular
neurons that make vasopressin are adjacent to magnocellular neurons
that make oxytocin, and are similar in many respects. The similarity of
the two peptides can cause some cross-reactions: oxytocin has a slight
antidiuretic function, and high levels of AVP can cause uterine
contractions.
Below is a table showing the superfamily of vasopressin and oxytocin
neuropeptides:
Chemical structure of the argipressin (indicating
that this compound is of the vasopressin family
with an arginine at the 8th amino acid position.
Chemical structure of oxytocin
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
123
Vertebrate Vasopressin Family
Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2
Argipressin (AVP,
ADH)
Most mammals
Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly-NH2
Lypressin (LVP)
Pigs, hippos, warthogs, some marsupials
Cys-Phe-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2
Phenypressin
Some marsupials
Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2
Vasotocin
Non-mammals
Vertebrate Oxytocin Family
Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly-NH2
Oxytocin (OXT)
Most mammals, ratfish
Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Pro-Gly-NH2
Prol-Oxytocin
Some New World monkeys, northern tree shrews
Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Ile-Gly-NH2
Mesotocin
Most marsupials, all birds, reptiles, amphibians, lungfishes,
coelacanths
Cys-Tyr-Ile-Gln-Ser-Cys-Pro-Ile-Gly-NH2
Seritocin
Frogs
Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Ile-Gly-NH2
Isotocin
Bony fishes
Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Gln-Gly-NH2
Glumitocin
Skates
Cys-Tyr-Ile-Asn/Gln-Asn-Cys-Pro-Leu/Val-Gly-NH2 Various tocins
Sharks
Invertebrate VP/OT Superfamily
Cys-Leu-Ile-Thr-Asn-Cys-Pro-Arg-Gly-NH2
Diuretic Hormone
Locust
Cys-Phe-Val-Arg-Asn-Cys-Pro-Thr-Gly-NH2
Annetocin
Earthworm
Cys-Phe-Ile-Arg-Asn-Cys-Pro-Lys-Gly-NH2
Lys-Connopressin
Geography & imperial cone snail, pond snail, sea hare, leech
Cys-Ile-Ile-Arg-Asn-Cys-Pro-Arg-Gly-NH2
Arg-Connopressin
Striped cone snail
Cys-Tyr-Phe-Arg-Asn-Cys-Pro-Ile-Gly-NH2
Cephalotocin
Octopus
Cys-Phe-Trp-Thr-Ser-Cys-Pro-Ile-Gly-NH2
Octopressin
Octopus
Vasotocin is the evolutionary progenitor of all the vertebrate neurohypophysial hormones.
Role in disease
Lack of AVP
Decreased AVP release or decreased renal sensitivity to AVP leads to diabetes insipidus, a condition featuring
hypernatremia (increased blood sodium concentration), polyuria (excess urine production), and polydipsia (thirst).
Excess AVP
High levels of AVP secretion may lead to hyponatremia. In many cases, the AVP secretion is appropriate (due to
severe hypovolemia), and the state is labelled "hypovolemic hyponatremia". In certain disease states (heart failure,
nephrotic syndrome) the body fluid volume is increased but AVP production is not suppressed for various reasons;
this state is labelled "hypervolemic hyponatremia". A proportion of cases of hyponatremia feature neither hyper- nor
hypovolemia. In this group (labelled "euvolemic hyponatremia"), AVP secretion is either driven by a lack of cortisol
or thyroxine (hypoadrenalism and hypothyroidism, respectively) or a very low level of urinary solute excretion
(potomania, low-protein diet), or it is entirely inappropriate. This last category is classified as the syndrome of
inappropriate antidiuretic hormone (SIADH).
SIADH in turn can be caused by a number of problems. Some forms of cancer can cause SIADH, particularly small
cell lung carcinoma but also a number of other tumors. A variety of diseases affecting the brain or the lung
(infections, bleeding) can be the driver behind SIADH. A number of drugs has been associated with SIADH, such as
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
124
certain antidepressants (serotonin reuptake inhibitors and tricyclic antidepressants), the anticonvulsant
carbamazepine, oxytocin (used to induce and stimulate labor), and the chemotherapy drug vincristine. It has also
been associated with fluoroqionolones, moxifloxacin and ciprofloxacin. Finally, it can occur without a clear
explanation.
Hyponatremia can be treated pharmaceutically through the use of vasopressin receptor antagonists.
Pharmacology
Vasopressin analogues
Vasopressin agonists are used therapeutically in various conditions, and its long-acting synthetic analogue
desmopressin is used in conditions featuring low vasopressin secretion, as well as for control of bleeding (in some
forms of von Willebrand disease and in mild haemophilia A) and in extreme cases of bedwetting by children.
Terlipressin and related analogues are used as vasoconstrictors in certain conditions. Use of vasopressin analogues
for esophageal varices commenced in 1970.
Vasopressin infusion has also been used as a second line of management in septic shock patients not responding to
high dose of inotropes (e.g., dopamine or norepinephrine).
The role of vasopressin analogues in cardiac arrest
Injection of vasopressors for the treatment of cardiac arrest was first suggested in the literature in 1896 when
Austrian scientist Dr. R. Gottlieb described the vasopressor epinephrine as an "infusion of a solution of suprarenal
extract [that] would restore circulation when the blood pressure had been lowered to unrecordable levels by chloral
hydrate." Modern interest in vasopressors as a treatment for cardiac arrest stem mostly from canine studies
performed in the 1960s by anesthesiologists Dr. John W. Pearson and Dr. Joseph Stafford Redding in which they
demonstrated improved outcomes with the use of adjunct intracardiac epinephrine injection during resuscitation
attempts after induced cardiac arrest. Also contributing to the idea that vasopressors may be useful treatments in
cardiac arrest are studies performed in the early to mid 1990's that found significantly higher levels of endogenous
serum vasopressin in adults after successful resuscitation from out-of-hospital cardiac arrest compared to those who
did not live. Results of animal models have supported the use of either vasopressin or epinephrine in cardiac arrest
resuscitation attempts, showing improved coronary perfusion pressure and overall improvement in short-term
survival as well as neurological outcomes.
Vasopressin vs. epinephrine
Table 1. Meta-analysis of outcomes for patients treated with vasopressin versus epinephrine
RR (95% CI)
Failure of ROSC
0.81 (0.58-1.12)
Death before hospital admission
0.72 (0.38-1.39)
Death within 24 hours
0.74 (0.38-1.43)
Death before hospital discharge
0.96 (0.87-1.05)
Number of deaths and neurologically impaired survivors 1.00 (0.94-1.07)
Although both vasopressors, vasopressin and epinephrine differ in that vasopressin does not have direct effects on
cardiac contractility as epinephrine does. Thus, vasopressin is theorized to be of increased benefit over epinephrine
in cardiac arrest due to its properties of not increasing myocardial and cerebral oxygen demands. This idea has led to
the advent of several studies searching for the presence of a clinical difference in benefit of these two treatment
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
125
choices. Initial small studies demonstrated improved outcomes with vasopressin in comparison to epinephrine.
However, subsequent studies have not all been in agreement. Several randomized controlled trials have been unable
to reproduce positive results with vasopressin treatment in both return of spontaneous circulation (ROSC) and
survival to hospital discharge, including a systematic review and meta-analysis completed in 2005 that found no
evidence of a significant difference with vasopressin in five studied outcomes (see Table 1).
Vasopressin and epinephrine vs. epinephrine alone
Table 2. Significant outcomes for combined vasopressin and epinephrine treatment
RR (95% CI)
p value
ROSC
1.42 (1.14-1.77)
Survival to hospital admission
1.42 (1.02-2.04) 0.05
In subgroup: PEA
1.30 (0.90-2.06) 0.02
In subgroup: Collapse to ED arrival time of 1530 minutes 1.22 (1.01-1.49) 0.05
In subgroup: Collapse to ED arrival time of 3045 minutes 1.11 (1.00-1.24) 0.05
Survival to hospital discharge
3.69 (1.52-8.95)
There is no current evidence of significant survival benefit with improved neurological outcomes in patients given
combinations of both epinephrine and vasopressin during cardiac arrest. A systematic review from 2008 did,
however, find one study that showed a statistically significant improvement in ROSC and survival to hospital
discharge with this combination treatment; unfortunately, those patients that survived to hospital discharge had
overall poor outcomes and many suffered permanent, severe neurological damage. A more recently published
clinical trial out of Singapore has shown similar results, finding combination treatment to only improve the rate of
survival to hospital admission, especially in the subgroup analysis of patients with longer "collapse to emergency
department" arrival times of 15 to 45 minutes. Table 2 lists all statistically significant findings of a correlation
between combined treatment and positive outcomes found in these two studies.
2010 American Heart Association Guidelines
The 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care recommend the consideration of vasopressor treatment in the form of epinephrine in adults with
cardiac arrest (Class IIb, LOE A recommendation). Due to the absence of evidence that vasopressin administered
instead of or in addition to epinephrine has significant positive outcomes, the guidelines do not currently contain
vasopressin as a part of the cardiac arrest algorithms. It does, however, allow for one dose of vasopressin to replace
either the first or second dose of epinephrine in the treatment of cardiac arrest (Class IIb, LOE A recommendation).
Vasopressin receptor inhibition
A vasopressin receptor antagonist is an agent that interferes with action at the vasopressin receptors. They can be
used in the treatment of hyponatremia.
References
[1] http:/ / www. ebi. ac. uk/ pdbe/ searchResults. html?display=both&
term=P01185%20or%20P01180%20or%20Q3UUQ5%20or%20P35455%20or%20P24787%20or%20Q8AV79
[2] http:/ / www. rcsb. org/ pdb/ search/ smartSubquery. do?smartSearchSubtype=UpAccessionIdQuery&
accessionIdList=P01185,P01180,Q3UUQ5,P35455,P24787,Q8AV79
[3] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1jk4
[4] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1jk6
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
[5] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=1npo
[6] http:/ / www. rcsb. org/ pdb/ cgi/ explore. cgi?pdbId=2bn2
[7] http:/ / www. genenames. org/ data/ hgnc_data. php?hgnc_id=894
[8] http:/ / omim. org/ entry/ 192340
[9] http:/ / www. informatics. jax. org/ searches/ accession_report. cgi?id=MGI:88121
[10] http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?cmd=Retrieve& db=homologene& dopt=HomoloGene& list_uids=417
[11] http:/ / www. genecards. org/ cgi-bin/ carddisp. pl?id_type=entrezgene& id=551
[12] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0004672
[13] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0004871
[14] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005102
[15] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005184
[16] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005185
[17] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0031894
[18] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0031895
[19] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043027
[20] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0005829
[21] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0030141
[22] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0030425
[23] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0002125
[24] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0003084
[25] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0006091
[26] http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0006468
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
[43]
[44]
[45]
[46]
[47]
[48]
[49]
[50]
[51]
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0006833
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007204
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007267
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007621
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007625
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0007626
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0010628
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0014049
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0030307
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0030819
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0031394
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0032849
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0033138
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0035094
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0035176
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0035813
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0042310
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0042538
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0042711
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043084
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043154
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0043252
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0045471
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0045907
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0050891
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0051970
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0055085
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0070371
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0070528
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ go. cgi?view=details& search_constraint=terms& depth=0& query=GO:0090201
http:/ / amigo. geneontology. org/ cgi-bin/ amigo/ gp-assoc. cgi?gp=UniProtKB:P01185
http:/ / www. ebi. ac. uk/ QuickGO/ GProtein?ac=P01185
http:/ / biogps. org/ gene/ 551/
http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?db=gene& cmd=retrieve& dopt=default& list_uids=551& rn=1
[61] http:/ / www. ncbi. nlm. nih. gov/ entrez/ query. fcgi?db=gene& cmd=retrieve& dopt=default& list_uids=11998& rn=1
[62] http:/ / www. ensembl. org/ Homo_sapiens/ geneview?gene=ENSG00000101200;db=core
[63] http:/ / www. ensembl. org/ Mus_musculus/ geneview?gene=ENSMUSG00000037727;db=core
126
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Vasopressin
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
[72]
[73]
[74]
http:/ / www. uniprot. org/ uniprot/ P01185
http:/ / www. uniprot. org/ uniprot/ P35455
http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NM_000490
http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NM_009732
http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NP_000481
http:/ / www. ncbi. nlm. nih. gov/ entrez/ viewer. fcgi?val=NP_033862
http:/ / genome. ucsc. edu/ cgi-bin/ hgTracks?org=Human& db=hg19& position=chr20:3063202-3065370
http:/ / genome. ucsc. edu/ cgi-bin/ hgTracks?org=Mouse& position=chr2:130580620-130582554
http:/ / www. ncbi. nlm. nih. gov/ sites/ entrez?db=gene& cmd=Link& LinkName=gene_pubmed& from_uid=551
http:/ / www. ncbi. nlm. nih. gov/ sites/ entrez?db=gene& cmd=Link& LinkName=gene_pubmed& from_uid=11998
http:/ / mouse. brain-map. org/ experiment/ show/ 78153149
Further reading
Rector, Floyd C.; Brenner, Barry M. (2004). Brenner & Rector's the kidney (http://home.mdconsult.com/das/
search/openres/56203699-5?searchisbn=460046813) (7th ed.). Philadelphia: Saunders. ISBN0-7216-0164-2.
External links
Molecular neurobiology of social bonding: Implications for autism spectrum disorders (http://videocast.nih.
gov/Summary.asp?File=15521) a lecture by Prof. Larry Young, Jan. 4, 2010.
127
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
128
Aldosterone
Aldosterone
Identifiers
[1]
CAS number
52-39-1
PubChem
5839
ChemSpider
5633
UNII
4964P6T9RB
DrugBank
DB04630
KEGG
C01780
MeSH
Aldosterone
ChEBI
CHEBI:27584
ChEMBL
CHEMBL273453
ATC code
H02 AA01
Jmol-3D images
Image 1
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
Properties
Molecular formula
C H O
Molar mass
360.44 g mol1
21 28 5
(verify)
[12]
(what is: / ?)
Except where noted otherwise, data are given for materials in their standard state (at 25C, 100kPa)
Infobox references
Aldosterone is a steroid hormone (mineralocorticoid family) produced by the outer section (zona glomerulosa) of
the adrenal cortex in the adrenal gland.[13] It plays a central role in the regulation of blood pressure mainly by acting
on the distal tubules and collecting ducts of the nephron, increasing reabsorption of ions and water in the kidney, to
cause the conservation of sodium, secretion of potassium, increased water retention, and increased blood pressure.
When dysregulated, aldosterone is pathogenic and contributes to the development and progression of cardiovascular
and renal disease. Aldosterone has exactly the opposite function of the atrial natriuretic hormone secreted by the
heart.
Drugs that interfere with the secretion or action of aldosterone are in use as antihypertensives, like Lisinopril; which
lowers blood pressure by blocking the Angiotensin Converting Enzyme (ACE), leading to lower aldosterone
secretion; its net effect is to reduce sodium and water retention, but increase retention of potassium. Aldosterone is
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
part of the renin-angiotensin system. Another example is spironolactone, a potassium sparing diuretic, which
decreases blood pressure by releasing fluid from the body, while retaining potassium.
It was first isolated by Simpson and Tait in 1953.
Synthesis
The corticosteroids are synthesized from cholesterol within the adrenal cortex. Most steroidogenic reactions are
catalysed by enzymes of the cytochrome P450 family. They are located within the mitochondria and require
adrenodoxin as a cofactor (except 21-hydroxylase and 17-hydroxylase).
Aldosterone and corticosterone share the first part of their biosynthetic pathways. The last parts are mediated either
by the aldosterone synthase (for aldosterone) or by the 11-hydroxylase (for corticosterone). These enzymes are
nearly identical (they share 11-hydroxylation and 18-hydroxylation functions), but aldosterone synthase is also able
to perform a 18-oxidation. Moreover, aldosterone synthase is found within the zona glomerulosa at the outer edge of
the adrenal cortex; 11-hydroxylase is found in the zona fasciculata and reticularis.
Note: aldosterone synthase is absent in
other sections of the adrenal gland.
Stimulation
Aldosterone synthesis is stimulated by
several factors:
increase in the plasma concentration
of angiotensin III, a metabolite of
angiotensin II
increase in plasma angiotensin II,
ACTH, or potassium levels, which
are present in proportion to plasma
sodium deficiencies. (The increased
potassium level works to regulate
aldosterone synthesis by
depolarizing the cells in the zona
glomerulosa, which opens the
Steroidogenesis, showing aldosterone synthesis at upper-right corner
voltage-dependent calcium
channels.) The level of angiotensin
II is regulated by angiotensin I, which is in turn regulated by renin, an enzyme secreted in the kidneys. Potassium
levels are the most sensitive stimulator of aldosterone.
the ACTH stimulation test, which is sometimes used to stimulate the production of aldosterone along with cortisol
to determine whether primary or secondary adrenal insufficiency is present. However, ACTH has only a minor
role in regulating aldosterone production; with hypopituitarism there is no atrophy of the zona glomerulosa.
plasma acidosis
the stretch receptors located in the atria of the heart. If decreased blood pressure is detected, the adrenal gland is
stimulated by these stretch receptors to release aldosterone, which increases sodium reabsorption from the urine,
sweat, and the gut. This causes increased osmolarity in the extracellular fluid, which will eventually return blood
pressure toward normal.
adrenoglomerulotropin, a lipid factor, obtained from pineal extracts. It selectively stimulates secretion of
aldosterone.
129
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
The secretion of aldosterone has a diurnal rhythm.
Function
Aldosterone is the primary of several endogenous members of the class of mineralocorticoids in humans.
Deoxycorticosterone is another important member of this class. Aldosterone tends to promote Na+ and water
retention, and lower plasma K+ concentration by the following mechanisms:
1. Acting on the nuclear mineralocorticoid receptors (MR) within the principal cells of the distal tubule and the
collecting duct of the kidney nephron, it upregulates and activates the basolateral Na+/K+ pumps, which pumps
three sodium ions out of the cell and two potassium ions into the cell. This results in reabsorption of sodium (Na+)
ions and water (which follows sodium) into the blood, and secreting potassium (K+) ions into the urine (lumen of
collecting duct).
2. Aldosterone upregulates epithelial sodium channels (ENaCs), increasing apical membrane permeability for Na+.
3. Cl is reabsorbed in conjunction with sodium cations to maintain the system's electrochemical balance.
4. Aldosterone stimulates the secretion of K+ into the tubular lumen.
5. Aldosterone stimulates Na+ and water reabsorption from the gut, salivary and sweat glands in exchange for K+.
6. Aldosterone stimulates secretion of H+ in exchange for Na+ in the intercalated cells of the cortical collecting
tubules, regulating plasma bicarbonate (HCO3) levels and its acid/base balance.
Aldosterone is responsible for the reabsorption of about 2% of filtered sodium in the kidneys, which is nearly equal
to the entire sodium content in human blood under normal glomerular filtration rates.
Aldosterone, probably acting through mineralocorticoid receptors, may positively influence neurogenesis in the
dentate gyrus.
Location of receptors
Steroid receptors are intracellular. The aldosterone mineralcorticoid receptor complex binds on the DNA to specific
hormone response element, which leads to gene specific transcription.
Some of the transcribed genes are crucial for transepithelial sodium transport, including the three subunits of the
epithelial sodium channel (ENaC), the Na+/K+ pumps and their regulatory proteins serum and
glucocorticoid-induced kinase, and channel-inducing factor, respectively.
The mineralcorticoid receptor is stimulated by both aldosterone and cortisol, but a mechanism protects the body from
excess aldosterone receptor stimulation by glucocorticoids (such as cortisol), which happen to be present at much
higher concentrations than mineralcorticoids in the healthy individual. The mechanism consists of an enzyme called
11 -hydroxysteroid dehydrogenase (11 -HSD). This enzyme co-localizes with intracellular adrenal steroid
receptors and converts cortisol into cortisone, a relatively inactive metabolite with little affinity for the MR.
Liquorice, which contains glycyrrhetinic acid, can inhibit 11 -HSD and lead to a mineralcorticoid excess syndrome.
130
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
Control of aldosterone release from the adrenal cortex
Major regulators
The role of the renin-angiotensin system
Angiotensin is involved in regulating aldosterone and is the core
regulation. Angiotensin II acts synergistically with potassium, and
the potassium feedback is virtually inoperative when no
angiotensin II is present. A small portion of the regulation
resulting from angiotensin II must take place indirectly from
decreased blood flow through the liver due to constriction of
capillaries. When the blood flow decreases so does the destruction
of aldosterone by liver enzymes.
Although sustained production of aldosterone requires persistent
calcium entry through low-voltage activated Ca2+ channels,
isolated zona glomerulosa cells are considered nonexcitable, with
recorded membrane voltages that are too hyperpolarized to permit
Ca2+ channels entry. However, mouse zona glomerulosa cells
The renin-angiotensin system, showing role of
within adrenal slices spontaneously generate membrane potential
aldosterone between the adrenal glands and the
[14]
kidneys
oscillations of low periodicity; this innate electrical excitability of
zona glomerulosa cells provides a platform for the production of a
recurrent Ca2+ channels signal that can be controlled by angiotensin II and extracellular potassium, the 2 major
regulators of aldosterone production.
The plasma concentration of potassium
The amount of aldosterone secreted is a direct function of the serum potassium as probably determined by sensors in
the carotid artery.
ACTH
ACTH, a pituitary peptide, also has some stimulating effect on aldosterone, probably by stimulating the formation of
deoxycorticosterone, a precursor of aldosterone. Aldosterone is increased by blood loss,[15] pregnancy, and possibly
by other circumstances such as physical exertion, endotoxin shock, and burns.[16]
Miscellaneous regulators
The role of sympathetic nerves
The aldosterone production is also affected to one extent or another by nervous control, which integrates the inverse
of carotid artery pressure,[] pain, posture, and probably emotion (anxiety, fear, and hostility) (including surgical
stress). Anxiety increases aldosterone, which must have evolved because of the time delay involved in migration of
aldosterone into the cell nucleus.[17] Thus, there is an advantage to an animal's anticipating a future need from
interaction with a predator, since too high a serum content of potassium has very adverse effects on nervous
transmission.
131
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
The role of baroreceptors
Pressure-sensitive baroreceptors are found in the vessel walls of nearly all large arteries in the thorax and neck, but
are particularly plentiful in the sinuses of the carotid arteries and in the arch of the aorta. These specialized receptors
are sensitive to changes in mean arterial pressure. An increase in sensed pressure results in an increased rate of firing
by the baroreceptors and a negative feedback response, lowering systemic arterial pressure. Aldosterone release
causes sodium and water retention, which causes increased blood volume, and a subsequent increase in blood
pressure, which is sensed by the baroreceptors.[18] To maintain normal homeostasis these receptors also detect low
blood pressure or low blood volume, causing aldosterone to be released. This results in sodium retention in the
kidney, leading to water retention and increased blood volume.[19]
The plasma concentration of sodium
Aldosterone is a function of the inverse of the sodium intake as sensed via osmotic pressure. The slope of the
response of aldosterone to serum potassium is almost independent of sodium intake. Aldosterone is much increased
at low sodium intakes, but the rate of increase of plasma aldosterone as potassium rises in the serum is not much
lower at high sodium intakes than it is at low. Thus, the potassium is strongly regulated at all sodium intakes by
aldosterone when the supply of potassium is adequate, which it usually is in primitive diets.
Aldosterone feedback
Feedback by aldosterone concentration itself is of a nonmorphological character (that is, other than changes in the
cells' number or structure) and is poor, so the electrolyte feedbacks predominate, short term.
Associated clinical conditions
Hyperaldosteronism is abnormally increased levels of aldosterone, while hypoaldosteronism is abnormally decreased
levels of aldosterone.
A measurement of aldosterone in blood may be termed a plasma aldosterone concentration (PAC), which may be
compared to plasma renin activity (PRA) as an aldosterone-to-renin ratio.
Hyperaldosteronism
Primary aldosteronism, also known as primary hyperaldosteronism, is characterized by the overproduction of
aldosterone by the adrenal glands, when not a result of excessive renin secretion. It leads to arterial hypertension
(high blood pressure) associated with hypokalemia, usually a diagnostic clue. Secondary hyperaldosteronism, on the
other hand, is due to overactivity of the renin-angiotensin system.
Conn's syndrome is primary hyperaldosteronism caused by an aldosterone-producing adenoma.
Depending on cause and other factors, hyperaldosteronism can be treated by surgery and/or medically, such as by
aldosterone antagonists.
132
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Aldosterone
133
Hypoaldosteronism
An ACTH stimulation test for aldosterone can help in determining the cause of hypoaldosteronism, with a low
aldosterone response indicating a primary hypoaldosteronism of the adrenals, while a large response indicating a
secondary hypoaldosteronism.
Additional images
Corticosteroid biosynthetic pathway in rat
Corticosterone
References
[1] http:/ / www. commonchemistry. org/ ChemicalDetail. aspx?ref=52-39-1
[2] http:/ / pubchem. ncbi. nlm. nih. gov/ summary/ summary. cgi?cid=5839
[3] http:/ / www. chemspider. com/ Chemical-Structure. 5633. html
[4] http:/ / fdasis. nlm. nih. gov/ srs/ srsdirect. jsp?regno=4964P6T9RB
[5] http:/ / www. drugbank. ca/ drugs/ DB04630
[6] http:/ / www. kegg. jp/ entry/ C01780
[7] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2007/ MB_cgi?mode=& term=Aldosterone
[8] https:/ / www. ebi. ac. uk/ chebi/ searchId. do?chebiId=27584
[9] https:/ / www. ebi. ac. uk/ chembldb/ index. php/ compound/ inspect/ CHEMBL273453
[10] http:/ / www. whocc. no/ atc_ddd_index/ ?code=H02AA01
[11] http:/ / chemapps. stolaf. edu/ jmol/ jmol.
php?model=O%3DC%28CO%29%5BC%40%40H%5D4%5BC%40%40%5D3%28C%3DO%29C%5BC%40H%5D%28O%29%5BC%40%40H%5D2%5BC%40
[12] http:/ / en. wikipedia. org/ w/ index. php?title=Special:ComparePages& rev1=477316959& page2=Aldosterone
[13] Marieb Human Anatomy & Physiology 9th edition, chapter:16, page:629, question number:14
[14] Page 866-867 (Integration of Salt and Water Balance) and 1059 (The Adrenal Gland) in:
[15] Ruch TC Fulton JF 1960 Medical Physiology and Biophysics. W.B. Saunders and Co., Phijl & London. On p1099.
[16] on 529
[17] Sharp GUG Leaf A 1966 in; Recent Progress in Hormone Research.(Pincus G, ed.
[18] Copstead, E. C. & Banasik, J. L. (2010.) Pathophysiology. (4th ed.). St. Louis, Mo: Saunders Elsevier.
[19] Marieb, E. N. (2004) Human anatomy and physiology (6th ed) San Francisco: Pearson Benjamin Cummings.
External Links
Aldosterone at Lab Tests Online (http://labtestsonline.org/understanding/analytes/aldosterone/tab/test)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Countercurrent multiplication
Countercurrent multiplication
A countercurrent multiplier system is a mechanism that expends energy to create a concentration gradient.
It is found widely in nature and especially in mammalian organs. For example, it can refer to the process that is
underlying the process of urine concentration, that is, the production of hyperosmotic urine by the mammalian
kidney.[citation needed] The ability to concentrate urine is also present in birds, but involves another mechanism which
is not comparable.[citation needed]
Countercurrent multiplication is frequently mistaken for countercurrent exchange, a similar but different
mechanism where gradients are maintained, but not established.
Physiological principles
The term derives from the form and function of the loop of Henle, which consists of two parallel limbs of renal
tubules running in opposite directions, separated by the interstital space of the renal medulla.[citation needed]
The descending limb of the loop of Henle is permeable to water but impermeable to solutes, due to the presence
of aquaporin 1 in its tubular wall. Thus water moves across the tubular wall into the medullary space, making the
urine hypertonic.[citation needed]
The ascending limb is impermeable to water (because of a lack of aquaporin, a common transporter protein for
water channels in all cells except the walls of the ascending limb of the loop of Henle) but permeable to solutes,
but here Na+, Cl, and K+ are actively transported into the medullary space, making the filtrate hypotonic (with a
higher water potential). This constitutes the single effect of the countercurrent multiplication process.[citation
needed]
Active transport of these ions from the thick ascending limb creates an osmotic pressure drawing water from the
descending limb into the hyperosmolar medullary space, making the filtrate hypertonic (with a lower water
potential).[citation needed]
The countercurrent flow within the descending and ascending limb thus increases, or multiplies the osmotic
gradient between tubular fluid and interstitial space.[citation needed]
Details
Countercurrent multiplication was originally studied as a mechanism whereby urine is concentrated in the nephron.
Initially studied in the 1950s by Gottschalk and Mylle following Werner Kuhn's postulations, this mechanism gained
popularity only after a series of complicated micropuncture experiments.
The proposed mechanism consists of pump, equilibration, and shift steps. In the proximal tubule, the osmolarity is
isomolar to plasma (300 mOsm/L). In a hypothetical model where there was no equilibration or pump steps, the
tubular fluid and interstitial osmolarity would be 300 mOsm/L as well.{Respicius Rwehumbiza, 2010}
Pump: The Na+/K+/2Cl transporter in the ascending limb of the loop of Henle helps to create a gradient by shifting
Na+ into the medullary interstitium. The thick ascending limb of the loop of Henle is the only part of the nephron
lacking in aquaporina common transporter protein for water channels. This makes the thick ascending limb
impermeable to water. The action of the Na+/K+/2Cl transporter therefore creates a hypoosmolar solution in the
tubular fluid and a hyperosmolar fluid in the interstitium, since water cannot follow the solutes to produce osmotic
equilibrium.[citation needed]
Equilibration: Since the descending limb of the loop of henle consists of very leaky epithelium, the fluid inside the
descending limb becomes hyperosmolar.[citation needed]
Shift: The movement of fluid through the tubules causes the hyperosmotic fluid to move further down the loop.
Repeating many cycles causes fluid to be near isosmolar at the top of Henle's loop and very concentrated at the
134
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Countercurrent multiplication
bottom of the loop. Interestingly, animals with a need for very concentrated urine (such as desert animals) have very
long loops of Henle to create a very large osmotic gradient. Animals that have abundant water on the other hand
(such as beavers) have very short loops. The vasa recta have a similar loop shape so that the gradient does not
dissipate into the plasma.[citation needed]
The mechanism of counter current multiplication works together with the vasa recta's counter current exchange to
prevent the wash out of salts and maintain a high osmolarity at the inner medulla.[citation needed]
References
The Loop of Henle: Concentration (http://www.liv.ac.uk/~petesmif/teaching/1bds_mb/notes/kidney/loop.
htm) at University of Liverpool
Countercurrent Multiplier Animation (http://www.colorado.edu/intphys/Class/IPHY3430-200/
countercurrent_ct.html) at University of Colorado
Osmoregulation
Osmoregulation is the active regulation of the osmotic pressure of an organism's fluids to maintain the homeostasis
of the organism's water content; that is, it keeps the organism's fluids from becoming too diluted or too concentrated.
Osmotic pressure is a measure of the tendency of water to move into one solution from another by osmosis. The
higher the osmotic pressure of a solution, the more water tends to move into it. Pressure must be exerted on the
hypertonic side of a selectively permeable membrane to prevent diffusion of water by osmosis from the side
containing pure water.
Organisms in aquatic and terrestrial environments must maintain the right concentration of solutes and amount of
water in their body fluids; this involves excretion (getting rid of metabolic wastes and other substances such as
hormones that would be toxic if allowed to accumulate in the blood) through organs such as the skin and the kidneys.
Regulators and conformers
Two major types of osmoregulation are osmoconformers
and osmoregulators. Osmoconformers match their body
osmolarity to their environment actively or passively. Most
marine invertebrates are osmoconformers, although their
ionic composition may be different from that of seawater.
Osmoregulators tightly regulate their body osmolarity,
which always stays constant, and are more common in the
animal kingdom. Osmoregulators actively control salt
concentrations despite the salt concentrations in the
Movement of water and ions in saltwater fish
environment. An example is freshwater fish. The gills
actively uptake salt from the environment by the use of
mitochondria-rich cells. Water will diffuse into the fish, so it excretes a very hypotonic (dilute) urine to expel all the
excess water. A marine fish has an internal osmotic concentration lower than that of the surrounding seawater, so it
tends
to
lose
water
and
gain
salt.
It
actively
excretes
135
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Osmoregulation
salt out from the gills. Most fish are stenohaline, which
means they are restricted to either salt or fresh water and
cannot survive in water with a different salt concentration
than they are adapted to. However, some fish show a
tremendous ability to effectively osmoregulate across a
broad range of salinities; fish with this ability are known as
euryhaline species, e.g., salmon. Salmon has been observed
to inhabit two utterly disparate environments marine
and fresh water and it is inherent to adapt to both by
bringing in behavioral and physiological modifications.
136
Movement of water and ions in freshwater fish
Some marine fish, like sharks, have adopted a different, efficient mechanism to conserve water, i.e., osmoregulation.
They retain urea in their blood in relatively higher concentration. Urea is damaging to living tissue so, to cope with
this problem, some fish retain trimethylamine oxide. This provides a better solution to urea's toxicity. Sharks, having
slightly higher solute concentration (i.e., above 1000 mOsm which is sea solute concentration), do not drink water
like fresh water fish.
Osmoregulation in plants
While there are no specific osmoregulatory organs in higher plants, the stomata are important in regulating water
loss through evapotranspiration, and on the cellular level the vacuole is crucial in regulating the concentration of
solutes in the cytoplasm. Strong winds, low humidity and high temperatures all increase evapotranspiration from
leaves. Abscisic acid is an important hormone in helping plants to conserve water it causes stomata to close and
stimulates root growth so that more water can be absorbed.
Plants share with animals the problems of obtaining water but, unlike in animals, the loss of water in plants is crucial
to create a driving force to move nutrients from the soil to tissues. Certain plants have evolved methods of water
conservation.
Xerophytes are plants that can survive in dry habitats, such as deserts, and are able to withstand prolonged periods of
water shortage. Succulent plants such as the cacti store water in the vacuoles of large parenchyma tissues. Other
plants have leaf modifications to reduce water loss, such as needle-shaped leaves, sunken stomata, and thick, waxy
cuticles as in the pine. The sand-dune marram grass has rolled leaves with stomata on the inner surface.
Hydrophytes are plants in water habitats. They mostly grow in water or in wet or damp places. In these plants the
water absorption occur through the whole surface of the plant, e.g. the water lily.
Halophytes are plants living in marshy areas (close to sea). They have to absorb water from such a soil which has
higher salt concentration and therefore lower water potential(higher osmotic pressure). Halophytes cope with this
situation by activating salts in their roots. As a consequence,the cells of the roots develop lower water potential
which brings in water by osmosis. The excess salt can be stored in cells or excreted out from salt glands on leaves.
The salt thus secreted by some species help them to trap water vapours from the air, which is absorbed in liquid by
leaf cells. Therefore this is another way of obtaining additional water from air, e.g. glasswort and cord-grass.
Mesophytes [1] are plants living in lands of temperate zone, which grow in well watered soil. They can easily
compensate the water lost by transpiration through absorbing water from the soil. To prevent excessive transpiration
they have developed a water proof external covering called cuticle.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Osmoregulation
137
Osmoregulation in animals
Kidneys play a very large role in human osmoregulation by regulating the amount of water reabsorbed from
glomerular filtrate in kidney tubules, which is controlled by hormones such as antidiuretic hormone (ADH),
aldosterone, and angiotensin II. For example, a decrease in water potential of blood is detected by osmoreceptors in
hypothalamus, which stimulates ADH release from pituitary gland to increase the permeability of the wall of the
collecting ducts in the kidneys. Therefore a large proportion of water is reabsorbed from fluid to prevent a fair
proportion of water from being excreted.
A major way animals have evolved to osmoregulate is by controlling the amount of water lost through the excretory
system.
Osmoregulation in protists
Amoeba make use of contractile vacuoles to collect excretory waste,
such as ammonia, from the intracellular fluid by diffusion and active
transport. As osmotic action pushes water from the environment into
the cytoplasm, the vacuole moves to the surface and disposes the
contents into the environment.
Osmoregulation in bacteria
Prokaryotes respond via altered gene expression to changes in the
osmotic environment. The model organism E. coli's osmoregulation is
well described.
Vertebrate excretory systems
Protist Paramecium aurelia with contractile
vacuoles.
Waste products of the nitrogen metabolism
Ammonia is a toxic by-product of protein metabolism and is generally converted to less toxic substances after it is
produced then excreted; mammals convert ammonia to urea, whereas birds and reptiles form uric acid to be excreted
with other wastes via their cloacas.
Achieving osmoregulation in vertebrates
Four processes occur:
filtration fluid portion of blood (plasma) is filtered from a nephron (functional unit of vertebrate kidney)
structure known as the glomerulus into Bowman's capsule or glomerular capsule (in the kidney's cortex) and
flows down the proximal convoluted tubule to a "u-turn" called the Loop of Henle (loop of the nephron) in the
medulla portion of the kidney.
reabsorption most of the viscous glomerular filtrate is returned to blood vessels that surround the convoluted
tubules.
secretion the remaining fluid becomes urine, which travels down collecting ducts to the medullary region of
the kidney.
excretion the urine (in mammals) is stored in the urinary bladder and exits via the urethra; in other vertebrates,
the urine mixes with other wastes in the cloaca before leaving the body (frogs also have a urinary bladder).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Osmoregulation
References
E. Solomon, L. Berg, D. Martin, Biology 6th edition. Brooks/Cole Publishing. 2002
References
[1] http:/ / en. wikipedia. org/ wiki/ Mesophyte
138
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Loop of Henle
139
Loop of Henle
Loop of Henle
Scheme of renal tubule and its vascular supply. (Loop of Henle visible center-left.)
Latin
Ansa nephroni
Gray's
subject #253 1223
Precursor
Metanephric blastema
MeSH
loop+of+henle
[2]
[1]
In the kidney, the loop of Henle (or Henle's loop, nephron loop [2] or its Latin counterpart ansa nephroni) is the
portion of a nephron that leads from the proximal convoluted tubule to the distal convoluted tubule. Named after its
discoverer F. G. J. Henle, the loop of Henle's main function is to create a concentration gradient in the medulla of the
kidney.
By means of a countercurrent multiplier system, which utilizes electrolyte pumps, the loop of Henle creates an area
of high urea concentration deep in the medulla, near the collecting duct. Water present in the filtrate in the collecting
duct flows through aquaporin channels out of the collecting duct, moving passively down its concentration gradient.
This process reabsorbs water and creates a concentrated urine for excretion.
Anatomy
It can be divided into four parts:
Thin descending limb of loop of Henle
The thin descending limb has low permeability to ions and urea, while being highly permeable to water. The
loop has a sharp bend in the renal medulla going from descending to ascending thin limb.
Thin ascending limb of loop of Henle
The thin ascending limb is impermeable to water, but it is permeable to ions.
Thick ascending limb of loop of Henle
Sodium (Na+), potassium (K+) and chloride (Cl-) ions are reabsorbed from the urine by secondary active
transport by a Na-K-Cl cotransporter (NKCC2). The electrical and concentration gradient drives more
reabsorption of Na+, as well as other cations such as magnesium (Mg2+) and calcium (Ca2+).
Cortical thick ascending limb
The cortical thick ascending limb drains urine into the distal convoluted tubule.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Loop of Henle
140
Blood supply
The loop of Henle is supplied by blood in a series of straight capillaries
descending from the cortical efferent arterioles. These capillaries
(called the vasa recta; recta is from the Latin for "straight") also have a
countercurrent multiplier mechanism that prevents washout of solutes
from the medulla, thereby maintaining the medullary concentration. As
water is osmotically driven from the descending limb into the
interstitium, it readily enters the vasa recta. The low bloodflow through
the vasa recta allows time for osmotic equilibration, and can be altered
by changing the resistance of the vessels' efferent arterioles.[citation needed]
Counter current multiplier diagram
Also, the vasa recta still has the large proteins and ions which were not filtered through the glomerulus, which
provides an oncotic pressure for ions to enter the vasa recta from the interstitium.[citation needed]
The main function of the Loop of Henle is to set up a concentration gradient.[citation needed]
Physiology
The descending loop of Henle receives isotonic (300 mOsm/L) fluid from the proximal convoluted tubule (PCT).
The fluid is isotonic because as ions are reabsorbed by the gradient time system, water is also reabsorbed
maintaining the osmolarity of the fluid in the PCT. Substances reabsorbed in the PCT include urea, water, potassium,
sodium, chloride, glucose, amino acids, lactate, phosphate, and bicarbonate. Since water is also reabsorbed the
volume of fluid in the loop of Henle is less than the PCT, approximately one-third of the original volume.
The interstitium of the kidney increases in osmolarity outside as the loop of Henle descends from 600 mOsm/L in the
outer medulla of the kidney to 1200 mOsm/L in the inner medulla. The descending portion of the loop of Henle is
extremely permeable to water and is less permeable to ions, therefore water is easily reabsorbed here and solutes are
not readily reabsorbed. The 300 mOsm/L fluid from the loop loses water to the higher concentration outside the loop
and increases in tonicity until it reaches its maximum at the bottom of the loop. This area represents the highest
concentration in the nephron, but the collecting duct can reach this same tonicity with maximum ADH effect.
The ascending limb of the loop of Henle receives an even lower volume of fluid and has different characteristics
compared to the descending limb. In the ascending portion, the loop becomes impermeable to water and the cells of
the loop actively reabsorb solutes from the luminal fluid; therefore water is not reabsorbed and ions are readily
reabsorbed. As ions leave the lumen via the Na-K-2Cl symporter and the Na-H antiporter, the concentration becomes
more and more hypotonic until it reaches approximately 100-150 mOsm/L. The ascending limb is also called the
diluting segment of the nephron because of its ability to dilute the fluid in the loop from 1200 mOsm/L to 100
mOsm/L.
Flow of the fluid through the entire loop of Henle is considered slow. As flow increases, the ability of the loop to
maintain its osmolar gradient is reduced. The vasa recta (capillary loops) also have a slow flow as well. Increases in
vasa recta flow wash away metabolites and cause the medulla to lose osmolarity as well. Increases in flow will
disrupt the kidney's ability to form concentrated urine.
Overall the loop of Henle resorbs about 25% of filtered ions and 20% of the filtered water in a normal kidney. These
ions are mostly Na, Cl, K, Ca and HCO3. The powering force is the Na/K ATPase on the basolateral membrane
which maintains the ion concentrations inside the cells. On the luminal membrane Na enters the cells passively
utilizing the Na-K-2Cl symporter. Then the Na/K ATPase will pump 3 Na out into the peritubular fluid and 2 K into
the cell on the non-lumen side of the cell. This gives the lumen of the fluid in the loop a positive charge in
comparison and creates a Na concentration gradient, which both push more Na into the cell via the Na-H antiporter.
The hydrogen for the antiporter comes from the enyzme carbonic anhydrase, which takes water and carbon dioxide
and forms bicarbonate and hydrogen. The hydrogen is exchanged for the Na in the tubular fluid of the loop of Henle.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Loop of Henle
141
Additional images
Transverse section of pyramidal substance of kidney of pig, the
bloodvessels of which are injected.
Diagram of physiological functions of nephron, including the loop
of Henle.
References
[1] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?mode=& term=loop+ of+ henle
[2] http:/ / www. unifr. ch/ ifaa/ Public/ EntryPage/ ViewTH/ THh306. html
Further reading
Douglas C. Eaton, John Pooler (2004). Vander's Renal Physiology (6th edition ed.). McGraw-Hill Medical.
ISBN0-07-135728-9.
Lote, Christopher J. (2000). "The loop of Henle, distal tubing and collecting duct" (http://books.google.com/
books?id=-joihQfwXzwC&pg=PA70). Principles of Renal Physiology. Springer. p.70.
ISBN978-0-7923-6178-7.
External links
Loop of Henle physiology (http://www.acbrown.com/renal/OutLoop.htm)
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Water-electrolyte imbalance
142
Water-electrolyte imbalance
Water-electrolyte
imbalance
Classification and external resources
[1]
ICD-10
E86
ICD-9
276
MeSH
D014883
-E87
[2]
[3]
[4]
Electrolytes play a vital role in maintaining homeostasis within the body. They help to regulate myocardial and
neurological function, fluid balance, oxygen delivery, acid-base balance and much more. Electrolyte imbalances can
develop by the following mechanisms: excessive ingestion; diminished elimination of an electrolyte; diminished
ingestion or excessive elimination of an electrolyte. The most common cause of electrolyte disturbances is renal
failure.
The most serious electrolyte disturbances involve abnormalities in the levels of sodium, potassium, and/or calcium.
Other electrolyte imbalances are less common, and often occur in conjunction with major electrolyte changes.
Chronic laxative abuse or severe diarrhoea or vomiting (Gastroenteritis) can lead to electrolyte disturbances along
with dehydration. People suffering from bulimia or anorexia nervosa are at especially high risk for an electrolyte
imbalance.
General function
Electrolytes are important because they are what cells (especially nerve, heart, muscle) use to maintain voltages
across their cell membranes and to carry electrical impulses (nerve impulses, muscle contractions) across themselves
and to other cells. Kidneys work to keep the electrolyte concentrations in blood constant despite changes in your
body. For example, during heavy exercise, electrolytes are lost in sweat, particularly sodium and potassium. These
electrolytes must be replaced to keep the electrolyte concentrations of the body fluids constant.
References
[1]
[2]
[3]
[4]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E86
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E87
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=276
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D014883
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
143
Hyponatremia
Hyponatremia
Classification and external resources
Sodium
[1]
ICD-10
E87.1
ICD-9
276.1
DiseasesDB
6483
MedlinePlus
000394
eMedicine
emerg/275
MeSH
D007010
[2]
[3]
[4]
[5]
med/1130
[6]
ped/1124
[7]
[8]
Hyponatremia (American English) or hyponatraemia (British English) is an electrolyte disturbance in which the
sodium ion concentration in the plasma is lower than normal. Sodium is the dominant extracellular cation (positive
ion) and cannot freely cross from the interstitial space into the cell, because charged sodium ions attract up to 25
water molecules around them, creating a large polar structure that is too large to pass through the cell membrane. Its
homeostasis (stability of concentration) inside the cell is vital to the normal function of any cell. Normal serum
sodium levels are between approximately 135 and 145 mEq/L (135 - 145 mmol/L). Hyponatremia is generally
defined as a serum level of less than 135 mEq/L and is considered severe when the serum level is below 125 mEq/L.
Many conditions including congestive heart failure, liver failure, kidney failure and pneumonia can have an
associated hyponatremia. It can also be caused by overhydration from drinking too much water (polydipsia).
In the vast majority of cases, hyponatremia occurs as a result of a proportional excess of water relative to the plasma
sodium (salt level in the blood). Lack of sodium (salt) alone is very rarely the cause of hyponatremia, although it can
promote hyponatremia indirectly. In particular, sodium loss can lead to a state of volume depletion (loss of blood
volume in the body), with volume depletion serving as a signal for the release of ADH (anti-diuretic
hormone).[citation needed] As a result of ADH-stimulated water retention (too much water in the body), blood sodium
becomes diluted and hyponatremia results.
Exercise-associated hyponatremia (EAH), however, is common at marathons and other endurance events.
Researchers found, for instance, that 13% of the athletes who finished the 2002 Boston Marathon were in a clinically
hyponatremic condition, i.e. their salt levels in their blood had fallen below an acceptable level. Tim Noakes' 2012
book "Waterlogged" addresses this phenomenon clearly.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
Signs and symptoms
Symptoms of hyponatremia include nausea and vomiting, headache, confusion, lethargy, fatigue, loss of appetite,
restlessness and irritability, muscle weakness, spasms, or cramps, seizures, and decreased consciousness or coma.
The presence and severity of symptoms are associated with the level of plasma sodium (salt level in the blood), with
the lowest levels of plasma sodium associated with the more prominent and serious symptoms (the less the salt the
more severe the symptoms). However, emerging data suggest that mild hyponatremia (plasma sodium levels at 131
mEq/L or above) is associated with numerous complications or subtle, presently unrecognized symptoms (e.g.,
increased falls, altered posture and gait, reduced attention).
Neurological (brain) symptoms typically occur with very low levels of plasma sodium (usually <115 mEq/L). When
sodium levels in the blood become excessively low, excess water enters the brain cells and the cells swell. This is
called hyponatremic encephalopathy. This is very dangerous because the soft brain is confined by the rigid skull. As
the brain expands tentorial herniation can occur which is a squeezing of the brain across the internal structures of the
skull.
This can lead to headache, nausea, vomiting and confusion, seizures, brain stem compression and respiratory arrest
(stopping breathing), and non-cardiogenic pulmonary edema (fluid in the lungs). This can be fatal if not treated
promptly.
The severity of symptoms depends on how fast and how severe the drop in blood salt level. A gradual drop, even to
very low levels, may be tolerated well if it occurs over several days or weeks, because of neuronal adaptation. The
presence of underlying neurological disease, like a seizure disorder, or non-neurological metabolic abnormalities,
also affects the severity of neurologic symptoms.
Causes
Based on the above classification, some of the many specific causes of hyponatremia can be listed as follows:
Hypervolemic hyponatremia Both sodium & water content increase: Increase in sodium content leads to
hypervolemia and water content to hyponatremia. Total body water and sodium are regulated independently
cirrhosis of the liver
congestive heart failure
nephrotic syndrome in the kidneys
massive edema of any cause
Euvolemic hyponatremia total body water increases, but the body's sodium content stays the same
states of severe pain or nausea
in the setting of trauma or other damage to the brain
SIADH (and its many causes)
Hypothyroidism
Glucocorticoid (steroid) deficiency
Hypovolemic hyponatremia The hypovolemia (extracellular volume loss) is consequent on total body sodium loss
but, overall, total body water is decreased and is the aetiology of the hyponatremia
any cause of hypovolemia such as prolonged vomiting, decreased oral intake, severe diarrhea
diuretic use (due to the diuretic causing a volume depleted state and thence ADH release, and not a direct result of
diuretic-induced urine sodium loss)
Addison's disease in which the adrenal glands do not produce sufficient steroid hormones (combined
glucocorticoid and mineralocorticoid deficiency)
Miscellaneous causes of hyponatremia that are not included under the above classification scheme include:
144
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
factitious hyponatremia (due to massive increases in blood triglyceride levels, extreme elevation of
immunoglobulins as may occur in multiple myeloma, and extreme hyperglycemia)
hypothyroidism and adrenal insufficiency (both thyroid hormone and cortisol are required to excrete free water)
beer potomania and other malnourished states where poor dietary protein intake leads to inadequate urine solute
formation thereby impeding the kidney's ability to excrete free water
primary polydipsia (where the amount of urine solute required to excrete huge quantities of ingested water
exceeds the body's ability to produce it; this typically occurs when 12 or more litres of water are ingested per day)
Diagnosis
Examination includes taking vital signs when lying, sitting, and standing, and an assessment of how much blood is in
the body. This determination (i.e. hypervolemic, euvolemic, hypovolemic) helps guide treatment decisions. A full
assessment of other medical conditions (comorbidity) is also taken, because heart and brain conditions affect the
results and the treatment decisions.
Pathophysiology
The hyponatremia can be spurious (false) and/or artifactual hyponatremia in which case there is no hypotonicity.
Hypertonic hyponatremia, caused by resorption of water drawn by molecules such as glucose (hyperglycemia or
diabetes) or mannitol (hypertonic infusion). Isotonic hyponatremia, more commonly called "pseudohyponatremia,"
is caused by measurement error due to hypertriglyceridemia (most common) or paraproteinemia. It occurs when
using techniques that measure the amount of sodium in a specified volume of serum/plasma, or that dilute the sample
before analysis.
True hyponatremia is Hypotonic hyponatremia and is by far the most common type, and is often simply referred to
as "hyponatremia." Hypotonic hyponatremia is categorized in 3 ways based on the patient's blood volume status.
Each category represents a different underlying reason for the increase in ADH that led to the water retention and
thence hyponatremia:
Hypervolemic hyponatremia, wherein there is decreased effective circulating volume (less blood flowing in the
body) even though total body volume is increased (by the presence of edema or swelling, especially in the
ankles). The decreased effective circulating volume stimulates the release of anti-diurectic hormone(ADH), which
in turn leads to water retention. Hypervolemic hyponatremia is most commonly the result of congestive heart
failure, liver failure (cirrhosis), or kidney disease (nephrotic syndrome).
Euvolemic hyponatremia, wherein the increase in ADH is secondary to either physiologic but excessive ADH
release (as occurs with nausea or severe pain) or inappropriate and non-physiologic secretion of ADH, i.e.
syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH). Often categorized under euvolemic is
hyponatremia due to inadequate urine solute (not enough chemicals or electrolytes to produce urine) as occurs in
beer potomania or "tea and toast" hyponatremia, hyponatremia due to hypothyroidism or central adrenal
insufficiency, and those rare instances of hyponatremia that are truly secondary to excess water intake (i.e.,
extreme psychogenic polydipsia)
Hypovolemic hyponatremia, wherein ADH secretion is stimulated by or associated with volume depletion (not
enough water in the body).
The volemic classification fails to include spurious (fake) and/or artifactual hyponatremia, which is addressed in the
osmolar classification. This includes hyponatremia that occurs in the presence of massive hypertriglyceridemia,
severe hyperglycemia, and extreme elevation of immunoglobulin levels.
In chronic hyponatremia, sodium (salt) levels drop gradually over several days or weeks and symptoms and
complications are typically moderate. Chronic hyponatremia is often called asymptomatic hyponatremia in clinical
settings because it is thought to have no symptoms; however, emerging data suggests that "asymptomatic"
145
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
hyponatremia is not actually asymptomatic.
In acute hyponatremia sodium (salt) levels drop rapidly, resulting in potentially dangerous effects, such as rapid
brain swelling, which can result in coma and death.
Treatment
The treatment of hyponatremia depends on the underlying cause and whether the patient's blood volume status is
hypervolemic, euvolemic, or hypovolemic. In the setting of hypovolemia, intravenous administration of normal
saline (salt) is usual, careful care taken not to raise the serum sodium level (salt level in the blood) too quickly (see
below). Euvolemic hyponatremia is usually managed by fluid restriction and treatment to abolish any stimuli for
ADH secretion such as nausea. Likewise, drugs causing SIADH are discontinued if possible. Patients with
euvolemic hyponatremia that persists despite those measures may be candidates for a so-called vaptan drug as
discussed below. Hypervolemic hyponatremia is usually treated by addressing the underlying heart or liver failure. If
it is not be possible to do so, the treatment becomes the same as that for euvolemic hyponatremia (i.e. fluid
restriction and/or use of a vaptan drug).
Hyponatremia is corrected slowly in order to lessen the chance of the development of central pontine myelinolysis
(CPM), a severe neurological disease involving a breakdown of the myelin sheaths covering parts of nerve cells. In
fact, overly rapid correction of hyponatremia is the most common cause of that potentially devastating disorder.
During treatment of hyponatremia, the serum sodium (salt level in the blood) is not allowed to rise by more than
8mmol/l over 24 hours (i.e. 0.33mmol/l/h rate of rise). In practice, too rapid correction of hyponatremia and thence
CPM is most likely to occur during the treatment of hypovolemic hyponatremia. In particular, once the hypovolemic
state has been corrected, the signal for ADH release disappears. At that point, there will be an abrupt water diuresis
(an increase in urination since there is no longer any ADH acting to retain the water). A rapid and profound rise in
serum sodium (salt level in the blood) can then occur. Should the rate of rise of serum sodium exceed 0.33mmol/l/h
over several hours, vasopressin may be administered to prevent ongoing rapid water diuresis (excessive urination).
Pharmaceutically, vasopressin receptor antagonists can be used in the treatment of hyponatremia, especially in
patients with SIADH, congestive heart failure or liver cirrhosis. A vasopressin receptor antagonist is an agent that
interferes with the action at the vasopressin receptors. A new class of medication, the "vaptan" drugs has been
specifically developed to inhibit the action of vasopressin on its receptors (V1A, V1B, and V2). These receptors
have a variety of functions, with the V1A and V2 receptors are expressed peripherally and involved in the
modulation of blood pressure and kidney function respectively, while the V1A and V1B receptors are expressed in
the central nervous system. V1A is expressed in many regions of the brain, and has been linked to a variety of social
behaviors in humans and animals.
Vaptan drugs
The vaptan class of drugs contains a number of compounds with varying selectivity, several of which are either
already in clinical use or in clinical trials as of 2010.
Unselective (mixed V1A, V2)
Conivaptan
V1A selective
Relcovaptan
V1B selective
Nelivaptan
V2 selective
Lixivaptan
146
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
Mozavaptan
Satavaptan
Tolvaptan
The V2-receptor antagonists tolvaptan and conivaptan allow excretion of electrolyte free water and are effective in
increasing serum sodium in euvolemic and hypervolemic hyponatremia.
Complications
Chronic hyponatremia can lead to such complications as neurological impairments. These neurological impairments
most often affect gait (walking) and attention, and can lead to falls, osteoporosis, and decreased reaction time.
Complications for chronic hyponatremia are most dangerous for geriatric patients. Falls are the leading cause of
deaths related to injury among people 65 years or older. In a recent study the incidence of hyponatremia in elderly
patients with large-bone fractures was more than double that of non-fracture patients. Recent work by Verbalis et al.
suggests that hyponatremia induces osteoporosis and found the adjusted odds ratio for developing osteoporosis to be
2.87 times higher among adults with mild hyponatremia compared to those without.
Acute hyponatremia can lead to much more serious complications including brain disease, brain herniation,
cardiopulmonary arrest, cerebral edema (brain swelling), seizures, coma, and death.
Epidemiology
Hyponatremia is the most common electrolyte disorder. Electrolytes are sodium (salt), potassium, calcium,
magnesium, chloride, hydrogen phosphate, and hydrogen carbonate. The disorder is more frequent in females, the
elderly, and in patients who are hospitalized. The incidence of hyponatremia depends largely on the patient
population. A hospital incidence of 1520% is common, while only 35% of patients who are hospitalized have a
serum sodium level (salt blood level) of less than 130 mEq/L. Hyponatremia has been reported in up to 30% of
elderly patients in nursing homes and is also present in approximately 30% of depressed patients on selective
serotonin reuptake inhibitors.
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E87. 1
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=276. 1
http:/ / www. diseasesdatabase. com/ ddb6483. htm
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000394. htm
http:/ / www. emedicine. com/ emerg/ topic275. htm
http:/ / www. emedicine. com/ med/ topic1130. htm#
http:/ / www. emedicine. com/ ped/ topic1124. htm#
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D007010
147
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hyponatremia
External links
Sandy Craig, Erik D Schraga, Francisco Talavera, Howard A Bessen, John D Halamka (2010-04-13).
"Hyponatremia in Emergency Medicine" (http://emedicine.medscape.com/article/767624-overview).
Medscape.
James L. Lewis, III, MD (May 2009). "Hyponatremia" (http://www.merckmanuals.com/professional/sec12/
ch156/ch156d.html#CIHEIHHA). Merck Manual of Diagnosis and Therapy.
Kugler JP, Hustead T (June 2000). "Hyponatremia and hypernatremia in the elderly" (http://www.aafp.org/afp/
20000615/3623.html). Am Fam Physician 61 (12): 362330. PMID 10892634 (http://www.ncbi.nlm.nih.
gov/pubmed/10892634).
Elizabeth Quinn (2011-03-07). "What Is Hyponatremia: Hyponatremia or water intoxication Can Athletes
Drink Too Much Water?" (http://sportsmedicine.about.com/od/hydrationandfluid/a/Hyponatremia.htm).
About.com.
"Salt and the ultraendurance athlete" (http://www.rice.edu/~jenky/sports/salt.html). SportsMed Web. 1997.
Sean Rothwell (2010-06-07). "Kokoda Medicine" (http://lifeinthefastlane.com/2010/06/kokoda-medicine/).
Hyponatremia (http://www.mayoclinic.com/health/hyponatremia/DS00974/DSECTION=causes) Mayo
Clinic
Sodium (http://labtestsonline.org/understanding/analytes/sodium/tab/test) at Lab Tests Online
148
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hypernatremia
149
Hypernatremia
Hypernatremia
Classification and external resources
Sodium
[1]
ICD-10
E87.0
ICD-9
276.0
DiseasesDB
6266
eMedicine
emerg/263
[2]
[3]
[4]
Hypernatremia or hypernatraemia (see American and British English spelling differences) is an electrolyte
disturbance that is defined by an elevated sodium level in the blood. Hypernatremia is generally not caused by an
excess of sodium, but rather by a relative deficit of free water in the body. For this reason, hypernatremia is often
synonymous with the less precise term, dehydration.
Water is lost from the body in a variety of ways, including perspiration, imperceptible losses from breathing, and in
the feces and urine. If the amount of water ingested consistently falls below the amount of water lost, the plasma
sodium level will begin to rise, leading to hypernatremia. Rarely, hypernatremia can result from massive salt
ingestion,[5][6] such as may occur from drinking seawater or excessive amounts of a salty liquid like soy sauce.[7][8]
Ordinarily, even a small rise in the plasma sodium concentration above the normal range results in a strong sensation
of thirst, an increase in free water intake, and correction of the abnormality. Therefore, hypernatremia most often
occurs in people such as infants, those with impaired mental status, or the elderly, who may have an intact thirst
mechanism but are unable to ask for or obtain water.
Signs and symptoms
Clinical manifestations of hypernatremia can be subtle, consisting of lethargy, weakness, irritability, neuromuscular
excitability, and edema. With more severe elevations of the sodium level, seizures and coma may occur.
Severe symptoms are usually due to acute elevation of the plasma sodium concentration to above 157 mEq/L
(normal blood levels are generally about 135-145 mEq/L for adults and elderly) Values above 180 mEq/L are
associated with a high mortality rate, particularly in adults. However such high levels of sodium rarely occur without
severe coexisting medical conditions.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hypernatremia
150
Cause
Common causes of hypernatremia include:
Hypovolemic
Inadequate intake of free water associated with total body
sodium depletion. Typically in elderly or otherwise disabled
patients who are unable to take in water as their thirst dictates
and also are sodium depleted. This is the most common cause of
hypernatremia.
Excessive losses of water from the urinary tract, which may be
caused by glycosuria, or other osmotic diuretics - leads to a
combination of sodium and free water losses.
Water losses associated with extreme sweating.
Severe watery diarrhea
Euvolemic
Excessive excretion of water from the kidneys caused by
diabetes insipidus, which involves either inadequate production
of the hormone vasopressin, from the pituitary gland or impaired
responsiveness of the kidneys to vasopressin.
Management of hypernatremia
Hypervolemic
Intake of a hypertonic fluid (a fluid with a higher concentration of solutes than the remainder of the body) with
restricted free water intake. This is relatively uncommon, though it can occur after a vigorous resuscitation
where a patient receives a large volume of a concentrated sodium bicarbonate solution. Ingesting seawater also
causes hypernatremia because seawater is hypertonic and free water is not available. There are several
recorded cases of forced ingestion of concentrated salt solution in exorcism rituals leading to death.
Mineralcorticoid excess due to a disease state such as Conn's syndrome usually does not lead to hypernatremia
unless free water intake is restricted.
Treatment
The cornerstone of treatment is administration of free water to correct the relative water deficit. Water can be
replaced orally or intravenously. Water alone cannot be administered intravenously (because of osmolarity issue),
but rather can be given with addition to dextrose or saline infusion solutions. However, overly rapid correction of
hypernatremia is potentially very dangerous. The body (in particular the brain) adapts to the higher sodium
concentration. Rapidly lowering the sodium concentration with free water, once this adaptation has occurred, causes
water to flow into brain cells and causes them to swell. This can lead to cerebral edema, potentially resulting in
seizures, permanent brain damage, or death. Therefore, significant hypernatremia should be treated carefully by a
physician or other medical professional with experience in treatment of electrolyte imbalance, specific treatment like
ACE inhibitors in heart failure and corticosteroids in nephropathy also can be used.[9]
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Hypernatremia
151
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E87. 0
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=276. 0
http:/ / www. diseasesdatabase. com/ ddb6266. htm
http:/ / www. emedicine. com/ emerg/ topic263. htm
Ofran, Y., Lavi, D., Opher, D., Weiss, T. A. and Elinav, E. (2004), Fatal voluntary salt intake resulting in the highest ever documented
sodium plasma level in adults (255 mmol L1): a disorder linked to female gender and psychiatric disorders. Journal of Internal Medicine,
256: 525528. doi: 10.1111/j.1365-2796.2004.01411.x
http:/ / dx. doi. org/ 10. 1016/ S0379-0738(98)00179-0
http:/ / www. huffingtonpost. com/ 2013/ 06/ 07/ soy-sauce-overdose-coma-hypernatremia_n_3402726. html
Survival of Acute Hypernatremia Due to Massive Soy Sauce Ingestion (http:/ / www. jem-journal. com/ article/ S0736-4679(13)00202-3/
abstract), The Journal of Emergency Medicine
Hypernatremia NEJM (http:/ / www. nejm. org/ doi/ full/ 10. 1056/ NEJM200005183422006)
External links
Sodium (http://labtestsonline.org/understanding/analytes/sodium/tab/test) at Lab Tests Online
Acidbase homeostasis
Acids and bases
Acid dissociation constant
Acid-base extraction
Acidbase reaction
Acidbase titration
Dissociation constant
Acidity function
Buffer solutions
pH
Proton affinity
Amphoterism
Self-ionization of water
Acid strength
Acid types
Brnsted
Lewis
Mineral
Organic
Strong
Superacids
Weak
Base types
Brnsted
Lewis
Organic
Strong
Superbases
Non-nucleophilic
Weak
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acidbase homeostasis
Acidbase homeostasis is the part of human homeostasis concerning the proper balance between acids and bases,
also called body pH. The body is very sensitive to its pH level, so strong mechanisms exist to maintain it. Outside
the acceptable range of pH, proteins are denatured and digested, enzymes lose their ability to function, and death
may occur.
Mechanism
The body's acidbase balance is normally tightly regulated, keeping
the arterial blood pH between 7.38 and 7.42. Several buffering agents
that reversibly bind hydrogen ions and impede any change in pH exist.
Extracellular buffers include bicarbonate and ammonia, whereas
proteins and phosphate act as intracellular buffers. The bicarbonate
buffering system is especially key, as carbon dioxide (CO2) can be
shifted through carbonic acid (H
2CO
3) to hydrogen ions and bicarbonate (HCO
3) as shown below.
Acidbase imbalances that overcome the buffer system can be
compensated in the short term by changing the rate of ventilation. This alters the concentration of carbon dioxide in
the blood, shifting the above reaction according to Le Chatelier's principle, which in turn alters the pH. For instance,
if the blood pH drops too low (acidemia), the body will compensate by increasing breathing thereby expelling CO2,
and shifting the above reaction to the left such that fewer hydrogen ions are free; thus the pH will rise back to
normal. For alkalemia, the opposite occurs.
The kidneys are slower to compensate, but renal physiology has several powerful mechanisms to control pH by the
excretion of excess acid or base. In response to acidosis, tubular cells reabsorb more bicarbonate from the tubular
fluid, collecting duct cells secrete more hydrogen and generate more bicarbonate, and ammoniagenesis leads to
increased formation of the NH
3 buffer. In responses to alkalosis, the kidney may excrete more bicarbonate by decreasing hydrogen ion secretion
from the tubular epithelial cells, and lowering rates of glutamine metabolism and ammonium excretion.
Imbalance
Acidbase imbalance occurs when a significant insult causes the blood pH to shift out of the normal range (7.35 to
7.45). In the fetus, the normal range differs based on which umbilical vessel is sampled (umbilical vein pH is
normally 7.25 to 7.45; umbilical artery pH is normally 7.18 to 7.38). An excess of acid in the blood is called
acidemia and an excess of base is called alkalemia. The process that causes the imbalance is classified based on the
etiology of the disturbance (respiratory or metabolic) and the direction of change in pH (acidosis or alkalosis). There
are four basic processes: metabolic acidosis, respiratory acidosis, metabolic alkalosis, and respiratory alkalosis. One
or a combination may occur at any given time.
152
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acidbase homeostasis
References
External links
Stewart's original text at acidbase.org (http://www.acidbase.org)
On-line text at AnaesthesiaMCQ.com (http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php)
Overview at kumc.edu (http://www2.kumc.edu/ki/physiology/course/nine/9_1.htm)
Tutorial at acid-base.com (http://www.acid-base.com/physiology.php)
Online acidbase physiology text (http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php)
Diagnoses at lakesidepress.com (http://www.lakesidepress.com/pulmonary/ABG/MixedAB.htm)
Interpretation at nda.ox.ac.uk (http://www.nda.ox.ac.uk/wfsa/html/u16/u1602_01.htm)
153
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acidosis
154
Acidosis
Acidosis
Classification and external resources
[1]
ICD-10
E87.2
ICD-9
276.2
DiseasesDB
87
MedlinePlus
001181
[2]
[3]
[4]
Acidosis is an increased acidity in the blood and other body tissue (i.e. an increased hydrogen ion concentration). If
not further qualified, it usually refers to acidity of the blood plasma.
Acidosis is said to occur when arterial pH falls below 7.35 (except in the fetus - see below), while its counterpart
(alkalosis) occurs at a pH over 7.45. Arterial blood gas analysis and other tests are required to separate the main
causes.
The term acidemia describes the state of low blood pH, while acidosis is used to describe the processes leading to
these states. Nevertheless, the terms are sometimes used interchangeably. The distinction may be relevant where a
patient has factors causing both acidosis and alkalosis, wherein the relative severity of both determines whether the
result is a high or a low pH.
The rate of cellular metabolic activity affects and, at the same time, is affected by the pH of the body fluids. In
mammals, the normal pH of arterial blood lies between 7.35 and 7.50 depending on the species (e.g. healthy
human-arterial blood pH varies between 7.35 and 7.45). Blood pH values compatible with life in mammals are
limited to a pH range between 6.8 and 7.8. Changes in the pH of arterial blood (and therefore the extracellular fluid)
outside this range result in irreversible cell damage.[5]
Metabolic acidosis
Metabolic acidosis may result from increased
production of metabolic acids or disturbances in the
ability to excrete acid via the kidneys. Renal acidosis is
associated with an accumulation of urea and creatinine
as well as metabolic acid residues of protein
catabolism.
An increase in the production of other acids may also
produce metabolic acidosis. For example, lactic
acidosis may occur from:
1. severe (PaO2 <36mm Hg) hypoxemia causing a fall
in the rate of oxygen diffusion from arterial blood to
tissues
2. hypoperfusion (e.g., hypovolemic shock) causing an
inadequate blood delivery of oxygen to tissues.
[6][7]
General symptoms of acidosis.
These usually accompany
symptoms of another primary defect (respiratory or metabolic).
A rise in lactate out of proportion to the level of pyruvate, e.g. in mixed venous blood, is termed "excess lactate", and
may also be an indicator of fermentation due to anaerobic metabolism occurring in muscle cells, as seen during
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acidosis
strenuous exercise. Once oxygenation is restored, the acidosis clears quickly. Another example of increased
production of acids occurs in starvation and diabetic acidosis. It is due to the accumulation of ketoacids (ketosis) and
reflects a severe shift from glycolysis to lipolysis for energy needs.
Acid consumption from poisoning such as hypercapnia, elevated levels of iron in the blood, and chronically
decreased production of bicarbonate may also produce metabolic acidosis.
Metabolic acidosis is compensated for in the lungs, as increased exhalation of carbon dioxide promptly shifts the
buffering equation to reduce metabolic acid. This is a result of stimulation to chemoreceptors, which increases
alveolar ventilation, leading to respiratory compensation, otherwise known as Kussmaul breathing (a specific type of
hyperventilation). Should this situation persist, the patient is at risk for exhaustion leading to respiratory failure.
Mutations to the V-ATPase 'a4' or 'B1' isoforms result in distal renal tubular acidosis, a condition that leads to
metabolic acidosis, in some cases with sensorineural deafness.
Arterial blood gases will indicate low pH, low blood HCO3, and normal or low PaCO2. In addition to arterial blood
gas, an anion gap can also differentiate between possible causes.
The Henderson-Hasselbalch equation is useful for calculating blood pH, because blood is a buffer solution. The
amount of metabolic acid accumulating can also be quantitated by using buffer base deviation, a derivative estimate
of the metabolic as opposed to the respiratory component. In hypovolemic shock for example, approximately 50% of
the metabolic acid accumulation is lactic acid, which disappears as blood flow and oxygen debt are corrected.
Treatment of uncompensated metabolic acidosis is focused upon correcting the underlying problem. When metabolic
acidosis is severe and can no longer be compensated for adequately by the lungs, neutralizing the acidosis with
infusions of bicarbonate may be required.
Fetal metabolic acidemia
In the fetus, the normal range differs based on which umbilical vessel is sampled (umbilical vein pH is normally 7.25
to 7.45; umbilical artery pH is normally 7.18 to 7.38). Fetal metabolic acidemia is defined as an umbilical vessel pH
of less than 7.20 and a base excess of less than -8.
Respiratory acidosis
Respiratory acidosis results from a build-up of carbon dioxide in the blood (hypercapnia) due to hypoventilation. It is
most often caused by pulmonary problems, although head injuries, drugs (especially anaesthetics and sedatives), and
brain tumors can cause this acidemia. Pneumothorax, emphysema, chronic bronchitis, asthma, severe pneumonia,
and aspiration are among the most frequent causes. It can also occur as a compensatory response to chronic
metabolic alkalosis.
One key to distinguish between respiratory and metabolic acidosis is that in respiratory acidosis, the CO2 is increased
while the bicarbonate is either normal (uncompensated) or increased (compensated). Compensation occurs if
respiratory acidosis is present, and a chronic phase is entered with partial buffering of the acidosis through renal
bicarbonate retention.
However, in cases where chronic illnesses that compromise pulmonary function persist, such as late-stage
emphysema and certain types of muscular dystrophy, compensatory mechanisms will be unable to reverse this
acidotic condition. As metabolic bicarbonate production becomes exhausted, and extraneous bicarbonate infusion
can no longer reverse the extreme buildup of carbon dioxide associated with uncompensated respiratory acidosis,
mechanical ventilation will usually be applied.
155
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acidosis
Fetal respiratory acidemia
In the fetus, the normal range differs based on which umbilical vessel is sampled (umbilical vein pH is normally 7.25
to 7.45; umbilical artery pH is normally 7.20 to 7.38). In the fetus, the lungs are not used for ventilation. Instead, the
placenta performs ventilatory functions (gas exchange). Fetal respiratory acidemia is defined as an umbilical vessel
pH of less than 7.20 and an umbilical artery PCO2of 66 or higher or umbilical vein PCO2 of 50 or higher.
References
[1]
[2]
[3]
[4]
[5]
[6]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E87. 2
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=276. 2
http:/ / www. diseasesdatabase. com/ ddb87. htm
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 001181. htm
Needham, A. 2004. Comparative and Environmental Physiology. Acidosis and Alkalosis.
Answers.com Medical Encyclopedia: Metabolic Acidosis: Causes and symptoms (http:/ / www. answers. com/ topic/
metabolic-acidosis-causes-and-symptoms) By Altha Roberts Edgren. Retrieved on April 13, 2009
[7] Symptoms mentioned in both metabolic and respiratory acidosis from the following two references: - Wrongdiagnosis.com > Symptoms of
Metabolic Acidosis (http:/ / www. wrongdiagnosis. com/ m/ metabolic_acidosis/ symptoms. htm#symptom_list) Retrieved on April 13, 2009 Wrongdiagnosis.com > Symptoms of Respiratory acidosis (http:/ / www. wrongdiagnosis. com/ r/ respiratory_acidosis/ symptoms.
htm-symptom_list) Retrieved on April 13, 2009
Notes
Hobler KE, Carey LC. Effect of acute progressive hypoxemia on cardiac output and plasma excess lactate. Ann
Surg. 1973 Feb;177(2):199-202.
Hobler KE, Napodano RJ, Tolerance of swine to acute blood volume deficits.
J Trauma. 1974 Aug;14(8):716-8.
Clinical Physiology of Acid-Base and Electrolyte Disorders by Rose, Post (http://books.mcgraw-hill.com/
getbook.php?isbn=0071346821&template=medical)
Intensive Care Medicine by Irwin and Rippe (http://www.lww.com/product/?0-7817-3548-3)
The ICU Book by Marino (http://www.lww.com/product/?0-683-05565-8)
156
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Alkalosis
157
Alkalosis
Alkalosis
Classification and external resources
[1]
ICD-10
E87.3
ICD-9
276.3
DiseasesDB
32458
MedlinePlus
001183
MeSH
D000471
[2]
[3]
[4]
[5]
Alkalosis refers to a condition reducing hydrogen ion concentration of arterial blood plasma (alkalemia). Generally,
alkalosis is said to occur when pH of the blood exceeds 7.45. The opposite condition is acidosis (when pH falls
below 7.35).
Types
Alkalosis can refer to:
Respiratory alkalosis
Metabolic alkalosis
Causes
The main cause of respiratory alkalosis is hyperventilation, resulting in a loss of carbon dioxide. Compensatory
mechanisms for this would include increased dissociation of the carbonic acid buffering intermediate into hydrogen
ions, and the related excretion of bicarbonate,[citation needed] both of which lower blood pH.
Metabolic alkalosis can be caused by prolonged vomiting, resulting in a loss of hydrochloric acid with the stomach
content. Severe dehydration, and the consumption of alkali are other causes. It can also be caused by administration
of diuretics and endocrine disorders such as Cushing's syndrome. Compensatory mechanism for metabolic alkalosis
involve slowed breathing by the lungs to increase serum carbon dioxide, a condition leaning toward respiratory
acidosis. As respiratory acidosis often accompanies the compensation for metabolic alkalosis, and viceversa, a
delicate balance is created between these two conditions.
Complications
Metabolic alkalosis is usually accompanied with hypokalemia, causing, e.g., muscular weakness, myalgia, and
muscle cramps (from disturbed function of the skeletal muscles), and muscle spasms (from disturbed function of
smooth muscles).
It may also cause hypocalcemia. As the pH of blood increases, blood transport proteins, such as albumin, become
more ionised into anions. This causes the free calcium present in blood to bind more strongly with albumin. If
severe, it may cause tetany (alkalotic tetany).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Alkalosis
References
IUPAC, Compendium of Chemical Terminology, 2nd ed. (the "Gold Book") (1997). Online corrected version:
(2006) "alkalosis [6]".
References
[1]
[2]
[3]
[4]
[5]
[6]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ E87. 3
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=276. 3
http:/ / www. diseasesdatabase. com/ ddb32458. htm
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 001183. htm
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D000471
http:/ / goldbook. iupac. org/ A00221. html
158
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulonephritis
159
Glomerulonephritis
Glomerulonephritis
Classification and external resources
Photomicrograph of a kidney biopsy from a patient with crescentic glomerulonephritis showing prominent fibrocellular crescent formation and
moderate mesangial proliferation in a glomerulus. Hematoxylin and eosin stain.
ICD-10
N00, N01, N03, N18
ICD-9
580
DiseasesDB
5245
MedlinePlus
000484
MeSH
D005921
[1]
-582
[2]
[3]
[4]
[5]
Glomerulonephritis, also known as glomerular nephritis, is a term used to refer to several renal diseases (usually
affecting both kidneys). Many of the diseases are characterised by inflammation either of the glomeruli or small
blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.
As it is not strictly a single disease, its presentation depends on the specific disease entity: it may present with
isolated hematuria and/or proteinuria (blood or protein in the urine); or as a nephrotic syndrome, a nephritic
syndrome, acute renal failure, or chronic renal failure.
They are categorized into several different pathological patterns, which are broadly grouped into non-proliferative or
proliferative types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different
types. Primary causes are intrinsic to the kidney. Secondary causes are associated with certain infections (bacterial,
viral or parasitic pathogens), drugs, systemic disorders (SLE, vasculitis), or diabetes.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulonephritis
160
Signs and symptoms
Glomerulonephritis refers to an inflammation of the glomerulus, which
is the unit involved in filtration in the kidney. This inflammation
typically results in one or both of the nephrotic or nephritic syndromes.
:500
Nephrotic syndrome
The nephrotic syndrome is characterised by the finding of oedema in a
patient that has increase protein in the urine and decreased protein in
the blood, with increased fat in the blood. Inflammation that affects the
cells surrounding the glomerulus, podocytes, increases the permeability
to proteins, resulting in an increased in excreted proteins. When the
amount of proteins excreted in the urine exceeds the liver's ability to
compensate, less proteins are detected in the blood - in particular
albumin, which makes up the majority of circulating proteins. With
decreased proteins in the blood, there is a decrease in the osmotic
A glomerulus, a functional unit that represents the
pressure of the blood. This results in oedema, as the osmotic pressure
first step in the filtration of blood and generation
of urine.
in tissue remains the same. This is worsened by the secretion of the
hormone Aldosterone by the kidney, which is secreted in response to
the decrease in circulating blood and causes sodium and water retention. Hyperlipidemia is thought to be a result of
the increased activity of the liver. :549
Nephritic syndrome
The nephritic syndrome is characterised by blood in the urine and a
decrease in the amount of urine in the presence of hypertension. In this
syndrome, inflammatory damage to cells lining the glomerulus are
thought to result destruction of the epithelial barrier, leading to blood
being found in the urine. At the same time, reactive changes
Wikipedia:Avoid weasel words may result in a decrease in renal
perfusion, resulting in a decrease in the production of urine. The
renin-angiotensin system may be subsequently activated, because of
the decrease in perfusion of juxtaglomerular apparatus, which may
result in hypertension. :554
Podocytes, cells which line the glomerulus, are
negatively charged and have small gaps,
preventing the filtration of large molecules. When
damaged by inflammation, this can result in an
increased permeability to proteins
Nonproliferative
This is characterised by forms of glomerulonephritis in which the number of cells is not changed. These forms
usually result in the nephrotic syndrome. Causes include:
Minimal change disease
Minimal change disease is characterised as a cause of nephrotic syndrome without visible changes in the glomerulus
on microscopy. Minimal change disease typically presents with oedema, an increase in proteins passed from urine
and decrease in blood protein levels, and an increase in circulating lipids; the nephrotic syndrome, and is the most
common cause of the nephrotic syndrome in children. Although no changes may be visible by light microscopy,
changes on electron microscopy within the glomerules may show a thinning of the foot processes of the cells lining
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulonephritis
the glomerulus. It is typically managed with corticosteroids and does not progress to chronic kidney disease. :500 :550
Focal segmental glomerulosclerosis
Focal segmental glomerulosclerosis is characterised by a sclerosis of segments of some glomerules. It is likely to
present as a nephrotic syndrome. This form of glomerulonephritis may be associated with conditions such as HIV
and heroin abuse, or inherited as Alport syndrome. The cause of about 20-30\% of focal-segmental
glomerulosclerosis is unknown. On microscopy, affected glomerules may show an increase in hyalin, a pink and
homogenous material, fat cells, an increase in the mesangial matrix and collagen. Treatment may involve
corticosteroids, but up to half of people with focal segmental glomerulonephritis continue to have progressive
deterioration of kidney function, ending in renal failure. :550-551
Membranous glomerulonephritis
Membranous glomerulonephritis may cause either nephrotic or a nephritic picture. About two-thirds are associated
with auto-antibodies to phospholipase A2 receptor, but other associations include cancers of the lung and bowel,
infections such as hepatitis B and malaria, drugs including penicillamine, and connective tissue diseases such as
systemic lupus erythematosus. Individuals with cerebral shunts are at risk of developing shunt nephritis, which
frequently produces MGN.
Microscopically, MGN is characterized by a thickened glomerular basement membrane without a hypercellular
glomerulus. Immunofluorescence demonstrates diffuse granular uptake of IgG. The basement membrane may
completely surround the granular deposits, forming a "spike and dome" pattern. Tubules also display the symptoms
of a typical Type III hypersensitivity reaction, which causes the endothelial cells to proliferate, which can be seen
under a light microscope with a PAS stain.
Prognosis follows the rule of thirds: one-third remain with MGN indefinitely, one-third remit, and one-third progress
to end-stage renal failure. As the glomerulonephritis progresses, the tubules of the kidney become infected, leading
to atrophy and hyalinisation. The kidney appears to shrink. Treatment with corticosteroids is attempted if the disease
progresses.
In extremely rare cases, the disease has been known to run in families, usually passed down through the females.
This condition, similarly, is called Familial Membranous Glomerulonephritis. There have only been about nine
documented cases in the world.
Thin basement membrane disease
Thin basement membrane disease is an autosomal dominant inherited disease characterized by thin glomerular
basement membranes on electron microscopy. It is a benign condition that causes persistent microscopic hematuria.
This also may cause proteinuria which is usually mild and overall prognosis is excellent. [citation needed]
Proliferative
Proliferative glomerulonephritis is characterised by an increased number of cells in the glomeruls. These forms
usually present with a triad of blood in the urine, decreased urine production, and hypertension, the nephritic
syndrome. These forms usually progress to end-stage renal failure (ESRF) over weeks to years (depending on type).
161
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulonephritis
162
IgA nephropathy
IgA nephropathy, also known as Berger's disease, is the most common type of glomerulonephritis, and generally
causes a nephritic syndrome characterised by protein in the urine, and visible blood in the urine. IgA nephropathy is
classically described as a self-resolving form in young adults several days after a respiratory infection. It is
characterised by deposits of IgA in the space between glomerular capillaries. :501:554-555
Henoch-Schonlein purpura refers to a form of IgA nephropathy, typically affecting children, chararcterised by a rash
of small bruises affecting the buttocks and lower legs, with abdominal pain. :501
Post-infectious
Post-infectious glomerulonephritis can occur after essentially any infection, but classically occurs after infection
with the bacteria Streptococcus pyogenes. It typically occurs 1-4 weeks after a pharyngeal infection with this
bacterium, and is likely to present with malaise, a slight fever, nausea and a mild nephritic syndrome of moderately
increased blood pressure, gross haematuria, and smoky-brown urine. Circulating immune complexes that deposit in
the glomerules may lead to an inflammatory reaction. :554-555
Diagnosis may be made on clinical findings or through antistreptolysin O antibodies found in the blood. A biopsy is
seldom done, and the disease is likely to self-resolve in children in 1-4 weeks, with a poorer prognosis if adults are
affected. :501
Membranoproliferative
Membranoproliferative GN (MPGN), also known as mesangiocapillary glomerulonephritis,:502 is characterised by
an increase in the number of cells in the glomerulus, and alterations in the glomerular basement membrane. These
forms present with the nephrotic syndrome, hypocomplementemia, and have a poor prognosis. Two primary
subtypes exist: :552-553
Type 1 MPGN is caused by circulating immune complexes, typically secondary to systemic lupus erythematosis,
hepatitis B and C, or other chronic or recurring infections. Circulating immune complexes may activate the
complement system, leading to inflammation and an influx of inflammatory cells.:552-553
Type 2 MPGN, also known as Dense Deposit Disease, is characterised by an excessive activation of the
complement system. The C3 Nephritic Factor autoantibody stabilises C3-convertase, which may lead to an
excessive activation of complement. :553
Rapidly progressive glomerulonephritis
Rapidly progressive glomerulonephritis, also known as Crescentic GN
is characterised by a progressive, rapid deterioration in kidney
function. Patients with rapidly progressive glomerulonephritis may
present with a nephritic syndrome. In management, steroid therapy is
sometimes used, although the prognosis remains poor. Three main
subtypes are recognised::557-558
Type 1 is Goodpasture syndrome, an autoimmune disease also
affecting the lung. In Goodpasture syndrome, IgG antibodies
directed against the glomerular basement membrane trigger an
inflammatory reaction, causing a nephritic syndrome and the
coughing up of blood. :557 High dose immunosuppression is
required (intravenous methylprednisolone) and cyclophosphamide,
plus plasmapheresis. Immunohistochemistry staining of tissue
specimens shows linear IgG deposits.
Crescentic glomerulonephritis induced by
infective endocarditis on PAS staining and
immunofluorescence. PAS staining (left)
demonstrated circumferential and cellular
crescent formation with interstitial nephritis.
Immunofluorescence (right) demonstrated C3
positive staining in mesangial area.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Glomerulonephritis
Type 2 is characterised by immune-complex-mediated damage, and
may be associated with systemic lupus erythematosis, post-infective
glomerulonephritis, IgA nephropathy, and Henoch-Scholein
purpura. :558
Type 3 rapidly progressive glomerulonephritis, also called
pauciimmune type, is associated with causes of vascular
inflammation including Wegener granulomatosis and microscopic
polyangitis. No immune deposits can be seen on staining, however
blood tests may be positive for the ANCA antibody. :558-559
Photomicrograph of renal biopsy showing
Histopathology: The majority of glomeruli present "crescents".
crescent formation and tuft narrowing. Periodic
Formation of crescents is initiated by passage of fibrin into the
acid silver methenamine stain.
Bowman space as a result of increased permeability of glomerular
basement membrane. Fibrin stimulates the proliferation of endothelial
cells of Bowman capsule, and an influx of monocytes. Rapid growing and fibrosis of crescents compresses the
capillary loops and decreases the Bowman space, which leads to renal failure within weeks or months. [citation needed]
Investigations
Some forms of glomerulonephritis are diagnosed clinically, based on findings on history and examination. Other
tests may include:
Urine examination
Blood tests investigating the cause, including FBC, inflammatory markers and special tests including (ASLO,
ANCA, Anti-GBM, Complement levels, Antinuclear antibodies
Biopsy of the kidney
References
[1] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=580
[2] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=582
[3] http:/ / www. diseasesdatabase. com/ ddb5245. htm
[4] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000484. htm
[5] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D005921
163
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Interstitial nephritis
164
Interstitial nephritis
Interstitial nephritis
Classification and external resources
[1]
ICD-10
N10
ICD-9
580.89
DiseasesDB
6854
-N12
[2]
[3]
, 581.89
[4]
, 582.89
[5]
, 583.89
[6]
[7]
MedlinePlus 000464 [8]
eMedicine
med/1596
MeSH
D009395
[9]
[10]
Interstitial nephritis (or Tubulo-interstitial nephritis) is a form of nephritis affecting the interstitium of the
kidneys surrounding the tubules. This disease can be either acute, meaning it occurs suddenly, or chronic, meaning it
is ongoing and eventually ends in kidney failure.
Etiologies
Common causes include infection, or reaction to medication (such as an analgesic or antibiotics such as Methicillin
(Meticillin). Reaction to medications causes 71% to 92% of cases.
This disease is also caused by other diseases and toxins that do damage to the kidney. Both acute and chronic
tubulointerstitial nephritis can be caused by a bacterial infection in the kidneys, known as pyelonephritis. The most
common cause is by an allergic reaction to a drug. The drugs that are known to cause this sort of reaction are
antibiotics such as penicillin and cephalexin, and nonsteroidal anti-inflammatory drugs, such as aspirin, as well as
rifampin, sulfa drugs, quinolones, diuretics, allopurinol, and phenytoin. The time between exposure to the drug and
the development of acute tubulointerstitial nephritis can be anywhere from 5 days to 5 months (fenoprofen induced).
Diagnosis
At times there are no symptoms of this disease, but when they do occur they are widely varied and can occur rapidly
or gradually. When caused by an allergic reaction, the symptoms of acute tubulointerstitial nephritis are fever (27%
of patients), rash (15% of patients), and enlarged kidneys. Some people experience dysuria, and lower back pain. In
chronic tubulointerstitial nephritis the patient can experience symptoms such as nausea, vomiting, fatigue, and
weight loss. Other conditions that may develop include hyperkalemia, metabolic acidosis, and kidney failure.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Interstitial nephritis
Blood tests
About 23% of patients have eosinophilia.
Urinary findings
Urinary findings include:
Eosinophiluria: sensitivity is 67% and specificity is 83%. The sensitivity is higher in patients with interstitial
nephritis induced by methicillin or when the Hansel's stain is used.
Isosthenuria.
Hematuria
Sterile pyuria: white blood cells and no bacteria
Gallium scan
The sensitivity of an abnormal gallium scan has been reported to range from 60% to 100%.
Treatment
Remove the etiology such as an offending drug. Corticosteroids do not clearly help. Nutrition therapy consists of
adequate fluid intake, which can require several liters of extra fluid.
Prognosis
The kidneys are the only body system that are directly affected by tubulointerstitial nephritis. Kidney function is
usually reduced; the kidneys can be just slightly dysfunctional, or fail completely.
In chronic tubulointerstitial nephritis, the most serious long-term effect is kidney failure. When the proximal tubule
is injured, sodium, potassium, bicarbonate, uric acid, and phosphate reabsorption may be reduced or changed,
resulting in low bicarbonate, known as metabolic acidosis, low potassium, low uric acid known as hypouricemia, and
low phosphate known as hypophosphatemia. Damage to the distal tubule may cause loss of urine-concentrating
ability and polyuria.
In most cases of acute tubulointerstitial nephritis, the function of the kidneys will return after the harmful drug is not
taken anymore, or when the underlying disease is cured by treatment. If the illness is caused by an allergic reaction, a
corticosteroid may speed the recovery kidney function; however, this is often not the case.
Chronic tubulointerstitial nephritis has no cure. Some patients may require dialysis. Eventually, a kidney transplant
may be needed.
References
[1] http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N10
[2] http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N12
[3] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=580. 89
[4] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=581. 89
[5] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=582. 89
[6] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=583. 89
[7] http:/ / www. diseasesdatabase. com/ ddb6854. htm
[8] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000464. htm
[9] http:/ / www. emedicine. com/ med/ topic1596. htm
[10] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D009395
165
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Interstitial nephritis
166
External links
Merck Manual (http://www.merck.com/mmpe/sec17/ch236/ch236c.html)
Diabetic nephropathy
Diabetic nephropathy
Classification and external resources
Photomicrography of nodular glomerulosclerosis in Kimmelstein-Wilson syndrome. Source: CDC
ICD-10
E10.2, E11.2, E12.2, E13.2, E14.2
ICD-9
250.4
MedlinePlus
000494
MeSH
D003928
[1]
[2]
[3]
Diabetic nephropathy (nephropatia diabetica), also known as Kimmelstiel-Wilson syndrome, or nodular
diabetic glomerulosclerosis and intercapillary glomerulonephritis, is a progressive kidney disease caused by
angiopathy of capillaries in the kidney glomeruli. It is characterized by nephrotic syndrome and diffuse
glomerulosclerosis. It is due to longstanding diabetes mellitus, and is a prime indication for dialysis in many Western
countries.
Signs and symptoms
Kidney failure provoked by glomerulosclerosis leads to fluid filtration deficits and other disorders of kidney
function. There is an increase in blood pressure (hypertension) and fluid retention in the body plus a reduced plasma
oncotic pressure causes edema. Other complications may be arteriosclerosis of the renal artery and proteinuria.
Throughout its early course, diabetic nephropathy has no symptoms. They develop in late stages and may be a result
of excretion of high amounts of protein in the urine or due to renal failure:
edema: swelling, usually around the eyes in the mornings; later, general body swelling may result, such as
swelling of the legs
foamy appearance or excessive frothing of the urine (caused by the proteinuria)
unintentional weight gain (from fluid accumulation)
anorexia (poor appetite)
nausea and vomiting
malaise (general ill feeling)
fatigue
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Diabetic nephropathy
167
headache
frequent hiccups
The first laboratory abnormality is a positive microalbuminuria test. Most often, the diagnosis is suspected when a
routine urinalysis of a person with diabetes shows too much protein in the urine (proteinuria). The urinalysis may
also show glucose in the urine, especially if blood glucose is poorly controlled. Serum creatinine and BUN may
increase as kidney damage progresses.
A kidney biopsy confirms the diagnosis, although it is not always necessary if the case is straightforward, with a
documented progression of proteinuria over time and presence of diabetic retinopathy on examination of the retina of
the eyes.
Cause
The word diabetes means "passing through", referring to the polyuria (abnormal increase of urine production), a
symptom historically present in those affected by the disease. When the level of blood glucose rises beyond the
kidney's capacity to reabsorb glucose from the renal ultrafiltrate, glucose remains diluted in the fluid, raising its
osmotic pressure and causing more water to be carried out, thus, increasing the excreted urine volume. The increased
volume dilutes the sodium chloride in the urine, signalling the macula densa to release more renin, causing
vasoconstriction, a survival mechanism to retain water by passing less blood through the kidneys. Because the
kidney is nurtured exclusively by the blood it filtrates, the vasoconstriction also reduces the nutrients supplied to it,
causing infarct of its tissues and reduction of renal function.
Pathophysiology
The earliest detectable change in the course of diabetic nephropathy is
a thickening in the glomerulus. At this stage, the kidney may leak more
serum albumin (plasma protein) than normal in the urine
(albuminuria), and this can be detected by sensitive medical tests for
albumin. This stage is called "microalbuminuria". As diabetic
nephropathy progresses, increasing numbers of glomeruli are destroyed
by progressive nodular glomerulosclerosis. Consequently, urine
albumin increases to the point that it may be detected by ordinary
urinalysis techniques. At this stage, a kidney biopsy generally clearly
shows diabetic nephropathy.
Illustration depicting diabetic nephropathy
The Armanni-Ebstein change (or Armanni-Ebstein cells) consists of deposits of glycogen in the tubular epithelial
cells (pars straight of proximal convoluted tubule and loop of Henle). Because most diabetics are treated before this
stage, it is very rare to see it at the present time. It appears in decompensated diabetics with glycemia higher than
500mg/dL and in the presence of severe glycosuria; it is a reversible alteration without functional manifestations.
The interstitium shows nonspecific chronic changes.
Treatment
The goals of treatment are to slow the progression of kidney damage and control related complications. The main
treatment, once proteinuria is established, is ACE inhibitor drugs, which usually reduces proteinuria levels and slows
the progression of diabetic nephropathy. Several effects of the ACEIs that may contribute to renal protection have
been related to the association of rise in Kinins which is also responsible for some of the side effects associated with
ACEIs therapy such as dry cough. The renal protection effect is related to the antihypertensive effects in normal and
hypertensive patients, renal vasodilatation resulting in increased renal blood flow and dilatation of the efferent
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Diabetic nephropathy
arterioles.[4] Many studies have shown that related drugs, angiotensin receptor blockers (ARBs), have a similar
benefit. However, combination therapy, according to the ONTARGET study, is known to worsen major renal
outcomes, such as increasing serum creatinine and causing a greater decline in estimated glomerular filtration rate
(eGFR).
Blood-glucose levels should be closely monitored and controlled. This may slow the progression of the disorder,
especially in the very early ("microalbuminuria") stages. Medications to manage diabetes include oral hypoglycemic
agents and insulin injections. As kidney failure progresses, less insulin is excreted, so lesser doses may be needed to
control glucose levels.
Diet may be modified to help control blood-sugar levels. Modification of protein intake can affect hemodynamic and
nonhemodynamic injury.
High blood pressure should be aggressively treated with antihypertensive medications, in order to reduce the risks of
kidney, eye, and blood vessel damage in the body. It is also very important to control lipid levels, maintain a healthy
weight, and engage in regular physical activity.
Patients with diabetic nephropathy should avoid taking the following drugs:
Contrast agents containing iodine
Commonly used non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, or COX-2
inhibitors like celecoxib, because they may injure the weakened kidney.
Urinary tract and other infections are common and can be treated with appropriate antibiotics.
Dialysis may be necessary once end-stage renal disease develops. At this stage, a kidney transplantation must be
considered. Another option for type 1 diabetes patients is a combined kidney-pancreas transplant.
C-peptide, a by-product of insulin production, may provide new hope for patients suffering from diabetic
nephropathy.
Several compounds are in development for diabetic kidney disease. These include, but are not limited to,
bardoxolone methyl,[5] olmesartan medoxomil, sulodexide, and avosentan.[6]
Prognosis
Diabetic nephropathy continues to get gradually worse. Complications of chronic kidney failure are more likely to
occur earlier, and progress more rapidly, when it is caused by diabetes than other causes. Even after initiation of
dialysis or after transplantation, people with diabetes tend to do worse than those without diabetes.
Possible complications include:
hypoglycemia (due to decreased renal clearance of insulin)
rapidly progressing chronic kidney failure
end-stage kidney disease
hyperkalemia
severe hypertension
complications of hemodialysis
complications of kidney transplant
coexistence of other diabetes complications
peritonitis (if peritoneal dialysis used)
increased infections
168
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Diabetic nephropathy
169
Epidemiology
The syndrome can be seen in patients with diabetes (usually less than 15 years after onset) after about 5 years in type
1 diabetes. Clinical nephropathy secondary to glomerular disease usually manifests 1525 years after diagnosis of
diabetes and affects 25-35% of patients under the age of 30 years. It is the leading cause of premature death in young
diabetic patients (between 50 and 70 years old). The disease is progressive and may cause death two or three years
after the initial lesions, and is more frequent in men. Diabetic nephropathy is the most common cause of chronic
kidney failure and end-stage kidney disease in the United States. People with both type 1 and type 2 diabetes are at
risk. The risk is higher if blood-glucose levels are poorly controlled. Furthermore, once nephropathy develops, the
greatest rate of progression is seen in patients with poor control of their blood pressure. Also people with high
cholesterol level in their blood have much more risk than others.
History
The syndrome was discovered by British physician Clifford Wilson (19061997) andGerman-born American
physician Paul Kimmelstiel (19001970) and was published for the first time in 1936.
Additional images
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. H&E stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. Another
glomerulus. H&E stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. Another
glomerulus. H&E stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. PAS stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. PAM stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. PAM stain.
Histopathological image of
diabetic glomerulosclerosis with
nephrotic syndrome. PAS stain.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Diabetic nephropathy
References
[1]
[2]
[3]
[4]
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=250. 4
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000494. htm
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D003928
Diabetes Mellitus and Angiotensin Converting Enzyme Inhibitors (http:/ / www. ksu. edu. sa/ sites/ Colleges/ Medicine/ Lists/ Medical
Subjects/ Flat. aspx?RootFolder=http:/ / www. ksu. edu. sa/ sites/ Colleges/ Medicine/ Lists/ Medical Subjects/ Diabetes Mellitus and
Angiotensin Converting Enzyme Inhibitors& FolderCTID=0x01200200CEDE56CEF8D11C46824F2F6116DF88AA)
[5] http:/ / www. medscape. com/ viewarticle/ 590644
[6] http:/ / www. medicalnewstoday. com/ articles/ 139028. php
External links
Diabetic nephropathy (http://www.healthcentral.com/mhc/top/000494.cfm). HealthCentral.
Diabetic nephropathy (http://www.nlm.nih.gov/medlineplus/ency/article/000494.htm). MedlinePlus
Medical Encyclopedia. Text from this public domain article was partially used here.
Texas University Classification (http://www.podomedic.it/modules/news/article.php?storyid=108)
170
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute kidney injury
171
Acute kidney injury
Acute kidney injury
Classification and external resources
Pathologic kidney specimen showing marked pallor of the cortex, contrasting to the darker areas of surviving medullary tissue. The patient died
with acute kidney injury.
[1]
ICD-10
N17
ICD-9
584
DiseasesDB
11263
MedlinePlus
000501
eMedicine
med/1595
MeSH
D058186
[2]
[3]
[4]
[5]
[6]
Acute kidney injury (AKI), previously called acute renal failure (ARF), is a rapid loss of kidney function.
Its causes are numerous and include low blood volume from any cause, exposure to substances harmful to the
kidney, and obstruction of the urinary tract. AKI is diagnosed on the basis of characteristic laboratory findings, such
as elevated blood urea nitrogen and creatinine, or inability of the kidneys to produce sufficient amounts of urine.
AKI may lead to a number of complications, including metabolic acidosis, high potassium levels, uremia, changes in
body fluid balance, and effects to other organ systems. Management includes supportive care, such as renal
replacement therapy, as well as treatment of the underlying disorder.
Signs and symptoms
The symptoms of acute kidney injury result from the various disturbances of kidney function that are associated with
the disease. Accumulation of urea and other nitrogen-containing substances in the bloodstream lead to a number of
symptoms, such as fatigue, loss of appetite, headache, nausea and vomiting. Marked increases in the potassium level
can lead to irregularities in the heartbeat, which can be severe and life-threatening. Fluid balance is frequently
affected, though hypertension is rare.
Pain in the flanks may be encountered in some conditions (such as thrombosis of the renal blood vessels or
inflammation of the kidney); this is the result of stretching of the fibrous tissue capsule surrounding the kidney. If the
kidney injury is the result of dehydration, there may be thirst as well as evidence of fluid depletion on physical
examination. Physical examination may also provide other clues as to the underlying cause of the kidney problem,
such as a rash in interstitial nephritis and a palpable bladder.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute kidney injury
172
Inability to excrete sufficient fluid from the body can cause accumulation of fluid in the limbs (peripheral edema)
and the lungs (pulmonary edema), as well as cardiac tamponade as a result of fluid effusions.
Causes
AKI can be caused by disease, crush injury, contrast agents, some antibiotics, and more.
The causes of acute kidney injury are commonly categorized into prerenal, intrinsic, and postrenal.
Classic laboratory findings in AKI
Type
UOsm UNa FeNa
BUN/Cr
Prerenal
>500 <10 <1%
>20
Intrinsic
<350 >20 >2% <15[citation needed]
Postrenal <350 >40 >4%
>15
Prerenal
Prerenal causes of AKI ("pre-renal azotemia") are those that decrease effective blood flow to the kidney. These
include systemic causes, such as low blood volume, low blood pressure, heart failure, and local changes to the blood
vessels supplying the kidney. The latter include renal artery stenosis, or the narrowing of the renal artery which
supplies the kidney with blood, and renal vein thrombosis, which is the formation of a blood clot in the renal vein
that drains blood from the kidney.
Renal ischaemia ultimately results in functional disorder, depression of GFR, or both. These causes stem from the
inadequate cardiac output and hypovolemia or vascular diseases causing reduced perfusion of both kidneys. Both
kidneys need to be affected as one kidney is still more than adequate for normal kidney function.
Intrinsic
Sources of damage to the kidney itself are dubbed intrinsic. Intrinsic AKI can be due to damage to the glomeruli,
renal tubules, or interstitium. Common causes of each are glomerulonephritis, acute tubular necrosis (ATN), and
acute interstitial nephritis (AIN), respectively. A cause of intrinsic acute renal failure is tumor lysis syndrome.
Postrenal
Postrenal AKI is a consequence of urinary tract obstruction. This may be related to benign prostatic hyperplasia,
kidney stones, obstructed urinary catheter, bladder stone, bladder, ureteral or renal malignancy. It is useful to
perform a bladder scan or a post void residual to rule out urinary retention. In post void residual, a catheter is
inserted immediately after urinating to measure fluid still in the bladder. 50-100ml suggests neurogenic bladder. A
renal ultrasound will demonstrate hydronephrosis if present. A CT scan of the abdomen will also demonstrate
bladder distension or hydronephrosis, however, in case of acute renal failure, the use of IV contrast is
contraindicated. On the basic metabolic panel, the ratio of BUN to creatinine may indicate post renal failure.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute kidney injury
Diagnosis
Detection
The deterioration of renal function may be discovered by a measured decrease in urine output. Often, it is diagnosed
on the basis of blood tests for substances normally eliminated by the kidney: urea and creatinine. Both tests have
their disadvantages. For instance, it takes about 24 hours for the creatinine level to rise, even if both kidneys have
ceased to function. A number of alternative markers has been proposed (such as NGAL, KIM-1, IL18 and cystatin
C), but none are currently established enough to replace creatinine as a marker of renal function.
Further testing
Once the diagnosis of AKI is made, further testing is often required to determine the underlying cause. These may
include urine sediment analysis, renal ultrasound and/or kidney biopsy. Indications for renal biopsy in the setting of
AKI include:
1. Unexplained AKI
2. AKI in the presence of the nephritic syndrome
3. Systemic disease associated with AKI
Classification
Acute kidney injury is diagnosed on the basis of clinical history and laboratory data. A diagnosis is made when there
is rapid reduction in kidney function, as measured by serum creatinine, or based on a rapid reduction in urine output,
termed oliguria.
Definition
Introduced by the Acute Kidney Injury Network (AKIN), specific criteria exist for the diagnosis of AKI:
1. Rapid time course (less than 48 hours)
2. Reduction of kidney function
Rise in serum creatinine, defined by either:
Absolute increase in serum creatinine of 0.3mg/dl (26.4 mol/l)
Percentage increase in serum creatinine of 50%
Reduction in urine output, defined as <0.5ml/kg/h for more than 6 hours
Staging
The RIFLE criteria, proposed by the Acute Dialysis Quality Initiative (ADQI) group, aid in the staging of patients
with AKI:
Risk: GFR decrease >25%, serum creatinine increased 1.5 times or urine production of <0.5ml/kg/h for 6 hours
Injury: GFR decrease >50%, doubling of creatinine or urine production <0.5ml/kg/h for 12 hours
Failure: GFR decrease >75%, tripling of creatinine or creatinine >355mol/l (with a rise of >44) (>4mg/dl)
OR urine output below 0.3ml/kg/h for 24 hours
Loss: persistent AKI or complete loss of kidney function for more than 4 weeks
End-stage renal disease: need for renal replacement therapy (RRT) for more than 3 months
173
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute kidney injury
Treatment
The management of AKI hinges on identification and treatment of the underlying cause. In addition to treatment of
the underlying disorder, management of AKI routinely includes the avoidance of substances that are toxic to the
kidneys, called nephrotoxins. These include NSAIDs such as ibuprofen, iodinated contrasts such as those used for
CT scans, many antibiotics such as gentamicin, and a range of other substances.
Monitoring of renal function, by serial serum creatinine measurements and monitoring of urine output, is routinely
performed. In the hospital, insertion of a urinary catheter helps monitor urine output and relieves possible bladder
outlet obstruction, such as with an enlarged prostate.
Specific therapies
In prerenal AKI without fluid overload, administration of intravenous fluids is typically the first step to improve
renal function. Volume status may be monitored with the use of a central venous catheter to avoid over- or
under-replacement of fluid.
Should low blood pressure prove a persistent problem in the fluid-replete patient, inotropes such as norepinephrine
and dobutamine may be given to improve cardiac output and hence renal perfusion. While a useful pressor, there is
no evidence to suggest that dopamine is of any specific benefit, and may be harmful.
The myriad causes of intrinsic AKI require specific therapies. For example, intrinsic AKI due to Wegener's
granulomatosis may respond to steroid medication. Toxin-induced prerenal AKI often responds to discontinuation of
the offending agent, such as aminoglycoside, penicillin, NSAIDs, or paracetamol.
If the cause is obstruction of the urinary tract, relief of the obstruction (with a nephrostomy or urinary catheter) may
be necessary.
Diuretic agents
The use of diuretics such as furosemide, is widespread and sometimes convenient in ameliorating fluid overload, and
is not associated with higher mortality (risk of death).
Renal replacement therapy
Renal replacement therapy, such as with hemodialysis, may be instituted in some cases of AKI. A systematic review
of the literature in 2008 demonstrated no difference in outcomes between the use of intermittent hemodialysis and
continuous venovenous hemofiltration (CVVH). Among critically ill patients, intensive renal replacement therapy
with CVVH does not appear to improve outcomes compared to less intensive intermittent hemodialysis.
Complications
Metabolic acidosis, hyperkalemia, and pulmonary edema may require medical treatment with sodium bicarbonate,
antihyperkalemic measures, and diuretics.
Lack of improvement with fluid resuscitation, therapy-resistant hyperkalemia, metabolic acidosis, or fluid overload
may necessitate artificial support in the form of dialysis or hemofiltration.
Prognosis
Depending on the cause, a proportion of patients will never regain full renal function, thus entering end-stage renal
failure and requiring lifelong dialysis or a kidney transplant. Patients with AKI are more likely to die prematurely
after they were discharged from hospital even if their kidney function has recovered.
174
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute kidney injury
Epidemiology
New cases of AKI are unusual but not rare, affecting approximately 0.1% of the UK population per year (2000
ppm/year), 20x incidence of new ESRD. AKI requiring dialysis (10% of these) is rare (200 ppm/year), 2x incidence
of new ESRD.
Acute kidney injury is common among hospitalized patients. It affects some 3-7% of patients admitted to the
hospital and approximately 25-30% of patients in the intensive care unit.
Acute renal failure was one of the most expensive conditions seen in U.S. hospitals in 2011, with an aggregated cost
of nearly $4.7 billion for approximately 498,000 hospital stays.[7] This was a 346% increase in hospitalizations from
1997, when there were 98,000 acute renal failure stays.[8]
History
Before the advancement of modern medicine, acute kidney injury was referred to as uremic poisoning while uremia
was contamination of the blood with urine. Starting around 1847, uremia came to be used for reduced urine output, a
condition now called oliguria, which was thought to be caused by the urine's mixing with the blood instead of being
voided through the urethra.[citation needed]
Acute kidney injury due to acute tubular necrosis (ATN) was recognised in the 1940s in the United Kingdom, where
crush injury victims during the London Blitz developed patchy necrosis of renal tubules, leading to a sudden
decrease in renal function. During the Korean and Vietnam wars, the incidence of AKI decreased due to better acute
management and administration of intravenous fluids.
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N17
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=584
http:/ / www. diseasesdatabase. com/ ddb11263. htm
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000501. htm
http:/ / www. emedicine. com/ med/ topic1595. htm
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D058186
Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160.
Agency for Healthcare Research and Quality, Rockville, MD. August 2013. (http:/ / hcup-us. ahrq. gov/ reports/ statbriefs/ sb160. jsp)
[8] Pfuntner A., Wier L.M., Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011. HCUP Statistical Brief #162. September 2013. Agency
for Healthcare Research and Quality, Rockville, MD. (http:/ / www. hcup-us. ahrq. gov/ reports/ statbriefs/ sb162. jsp)
175
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute tubular necrosis
176
Acute tubular necrosis
Acute tubular necrosis
Classification and external resources
[1]
ICD-10
N17.0
ICD-9
584.5
DiseasesDB
11263
MedlinePlus
000512
eMedicine
med/39
MeSH
D007683
[2]
[3]
[3]
[4]
ped/28
[5]
[6]
Acute tubular necrosis (ATN) is a medical condition involving the death of tubular cells that form the tubule that
transports urine to the ureters while reabsorbing 99% of the water (and highly concentrating the salts and metabolic
byproducts). Tubular cells continually replace themselves and if the cause of ATN is removed then recovery is
likely. ATN presents with acute kidney injury (AKI) and is one of the most common causes of AKI. The presence of
"muddy brown casts" of epithelial cells found in the urine during urinalysis is pathognomonic for ATN.
Classification
It may be classified as either toxic or ischemic. Toxic ATN occurs when the tubular cells are exposed to a toxic
substance (nephrotoxic ATN). Ischemic ATN occurs when the tubular cells do not get enough oxygen, a condition
that they are highly sensitive and susceptible to, due to their very high metabolism.
Diagnosis
Acute tubular necrosis is classified as a "renal" (i.e. not pre-renal or post-renal) cause of acute kidney injury.
Diagnosis is made by a FENa (fractional excretion of sodium) > 3% and presence of muddy casts (a type of granular
cast) in urinalysis. On histopathology, there is usually tubulorrhexis, that is, localized necrosis of the epithelial lining
in renal tubules, with focal rupture or loss of basement membrane.[7] Proximal tubule cells can shed with variable
viability and not be purely "necrotic". 40_75%
Toxic ATN
Toxic ATN can be caused by free hemoglobin or myoglobin, by medication such as antibiotics such as
aminoglycoside and cytoxic drugs such as cisplatin, or by intoxication (ethylene glycol, "anti-freeze").
Histopathology: Toxic ATN is characterized by proximal tubular epithelium necrosis (no nuclei, intense eosinophilic
homogeneous cytoplasm, but preserved shape) due to a toxic substance (poisons, organic solvents, drugs, heavy
metals). Necrotic cells fall into the tubule lumen, obturating it, and determining acute renal failure. Basement
membrane is intact[citation needed], so the tubular epithelium regeneration is possible. Glomeruli are not affected.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Acute tubular necrosis
Ischemic ATN
Ischemic ATN can be caused when the kidneys are not sufficiently perfused for a long period of time (i.e. renal
artery stenosis) or during shock. Hypoperfusion can also be caused by embolism of the renal arteries. Ischemic ATN
specifically causes skip lesions through the tubules.
External links
Photo at: Atlas of Pathology [8]
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N17. 0
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=584. 5
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000512. htm
http:/ / www. emedicine. com/ med/ topic39. htm
http:/ / www. emedicine. com/ ped/ topic28. htm#
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D007683
TheFreeDictionary > tubulorrhexis (http:/ / medical-dictionary. thefreedictionary. com/ tubulorrhexis) Citing: The American Heritage
Medical Dictionary 2007
[8] http:/ / www. pathologyatlas. ro/ toxic-tubular-necrosis. php
177
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
178
Chronic kidney disease
Chronic kidney disease
Classification and external resources
Uremic frost on the forehead and scalp of a young man who presented with complaints of chronic anorexia and fatigue with blood urea nitrogen and
serum creatinine levels of approximately 100 and 50 mg/dL respectively.
[1]
ICD-10
N18
ICD-9
585.9
DiseasesDB
11288
MedlinePlus
000471
eMedicine
article/238798
MeSH
D007676
[2]
585.1-585.5
[3]
403
[4]
[5]
[6]
[7]
[8]
Chronic kidney disease (CKD), also known as chronic renal disease, is a progressive loss in renal function over a
period of months or years. The symptoms of worsening kidney function are non-specific, and might include feeling
generally unwell and experiencing a reduced appetite. Often, chronic kidney disease is diagnosed as a result of
screening of people known to be at risk of kidney problems, such as those with high blood pressure or diabetes and
those with a blood relative with chronic kidney disease. Chronic kidney disease may also be identified when it leads
to one of its recognized complications, such as cardiovascular disease, anemia or pericarditis. It is differentiated from
acute kidney disease in that the reduction in kidney function must be present for over 3 months.
Chronic kidney disease is identified by a blood test for creatinine. Higher levels of creatinine indicate a lower
glomerular filtration rate and as a result a decreased capability of the kidneys to excrete waste products. Creatinine
levels may be normal in the early stages of CKD, and the condition is discovered if urinalysis (testing of a urine
sample) shows that the kidney is allowing the loss of protein or red blood cells into the urine. To fully investigate the
underlying cause of kidney damage, various forms of medical imaging, blood tests and often renal biopsy (removing
a small sample of kidney tissue) are employed to find out if there is a reversible cause for the kidney malfunction.
Recent professional guidelines classify the severity of chronic kidney disease in five stages, with stage 1 being the
mildest and usually causing few symptoms and stage 5 being a severe illness with poor life expectancy if untreated.
Stage 5 CKD is often called end stage renal disease (ESRD), end stage renal failure (ESRF), or end-stage kidney
disease (ESKD) and is synonymous with the now outdated terms chronic kidney failure (CKF) or chronic renal
failure (CRF).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
There is no specific treatment unequivocally shown to slow the worsening of chronic kidney disease. If there is an
underlying cause to CKD, such as vasculitis, this may be treated directly to slow the damage. In more advanced
stages, treatments may be required for anemia and bone disease. Severe CKD requires renal replacement therapy,
which may involve a form of dialysis, but ideally constitutes a kidney transplant.
Signs and symptoms
CKD is initially without specific symptoms and is generally only detected as an increase in serum creatinine or
protein in the urine. As the kidney function decreases:
Blood pressure is increased due to fluid overload and production of vasoactive hormones created by the kidney
via the RAS (renin-angiotensin system), increasing one's risk of developing hypertension and/or suffering from
congestive heart failure
Urea accumulates, leading to azotemia and ultimately uremia (symptoms ranging from lethargy to pericarditis and
encephalopathy). Urea is excreted by sweating and crystallizes on skin ("uremic frost").
Potassium accumulates in the blood (known as hyperkalemia with a range of symptoms including malaise and
potentially fatal cardiac arrhythmias)
Erythropoietin synthesis is decreased
Fluid volume overload symptoms may range from mild edema to life-threatening pulmonary edema
Hyperphosphatemia due to reduced phosphate excretion
Hypocalcemia due to 1,25 dihydroxyvitamin D3 deficiency. The 1,25 dihydroxyvitamin D3 deficiency is due to
stimulation of fibroblast growth factor-23.
Later this progresses to secondary hyperparathyroidism, renal osteodystrophy and vascular calcification that
further impairs cardiac function.
Metabolic acidosis, due to accumulation of sulfates, phosphates, uric acid etc. This may cause altered enzyme
activity by excess acid acting on enzymes and also increased excitability of cardiac and neuronal membranes by
the promotion of hyperkalemia due to excess acid (acidemia)
Iron deficiency anemia, which increases in prevalence as kidney function decreases, and is especially prevalent in
those requiring haemodialysis. It is multifactoral in cause but includes increased inflammation, reduction in
Erythropoietin, hyperuricemia leading to bone marrow suppression.
People with chronic kidney disease suffer from accelerated atherosclerosis and are more likely to develop
cardiovascular disease than the general population. Patients afflicted with chronic kidney disease and cardiovascular
disease tend to have significantly worse prognoses than those suffering only from the latter.[citation needed]
Sexual dysfunction is very common in both men and women with chronic kidney disease. A majority of men have a
reduced sex drive, difficulty obtaining an erection and reaching orgasm, and the problems get worse with age. A
majority of women have trouble with sexual arousal, and painful periods and problems with performing and enjoying
sex are common.
179
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
Causes
The three most common causes of CKD are diabetes mellitus, hypertension, and glomerulonephritis.[9] Together,
these cause approximately 75% of all adult cases.
Historically, kidney disease has been classified according to the part of the renal anatomy that is involved.[citation
needed]
Vascular, includes large vessel disease such as bilateral renal artery stenosis and small vessel disease such as
ischemic nephropathy, hemolytic-uremic syndrome and vasculitis
Glomerular, comprising a diverse group and subclassified into
Primary Glomerular disease such as focal segmental glomerulosclerosis and IgA nephropathy (or nephritis)
Secondary Glomerular disease such as diabetic nephropathy and lupus nephritis
Tubulointerstitial including polycystic kidney disease, drug and toxin-induced chronic tubulointerstitial nephritis
and reflux nephropathy
Obstructive such as with bilateral kidney stones and diseases of the prostate
On rare cases, pin worms infecting the kidney can also cause nephropathy.
non traditional causes of CKD are denoted if the common causes of CKD are not present, e.g. in El Salvador [10],
Nicaragua, ... in rural communities with agriculture.
Diagnosis
In many CKD patients, previous renal disease or other underlying
diseases are already known. A small number present with CKD of
unknown cause. In these patients, a cause is occasionally identified
retrospectively.[citation needed]
It is important to differentiate CKD from acute renal failure (ARF)
because ARF can be reversible. Abdominal ultrasound, in which the
size of the kidneys is measured, is commonly performed. Kidneys with
12-lead ECG of a person with chronic renal
CKD are usually smaller (< 9cm) than normal kidneys, with notable
disease and a severe electrolyte imbalance:
hyperkalemia
(7.4 mmol/l) with hypocalcemia
exceptions such as in diabetic nephropathy and polycystic kidney
(1.6 mmol/l). The T-waves are peaked and the
disease. Another diagnostic clue that helps differentiate CKD from
QT interval is prolonged.
ARF is a gradual rise in serum creatinine (over several months or
years) as opposed to a sudden increase in the serum creatinine (several
days to weeks). If these levels are unavailable (because the patient has been well and has had no blood tests), it is
occasionally necessary to treat a patient briefly as having ARF until it has been established that the renal impairment
is irreversible.[citation needed]
Additional tests may include nuclear medicine MAG3 scan to confirm blood flows and establish the differential
function between the two kidneys. DMSA scans are also used in renal imaging; with both MAG3 and DMSA being
used chelated with the radioactive element Technetium-99.[citation needed]
In chronic renal failure treated with standard dialysis, numerous uremic toxins accumulate. These toxins show
various cytotoxic activities in the serum, have different molecular weights and some of them are bound to other
proteins, primarily to albumin. Such toxic protein bound substances are receiving the attention of scientists who are
interested in improving the standard chronic dialysis procedures used today.[citation needed]
180
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
181
Stages
CKD Stage GFR level (mL/min/1.73 m2)
Stage 1
90
Stage 2
60 89
Stage 3
30 59
Stage 4
15 29
Stage 5
< 15
All individuals with a glomerular filtration rate (GFR) <60 mL/min/1.73 m2 for 3 months are classified as having
chronic kidney disease, irrespective of the presence or absence of kidney damage. The rationale for including these
individuals is that reduction in kidney function to this level or lower represents loss of half or more of the adult level
of normal kidney function, which may be associated with a number of complications.
All individuals with kidney damage are classified as having chronic kidney disease, irrespective of the level of GFR.
The rationale for including individuals with GFR > 60 mL/min/1.73 m2 is that GFR may be sustained at normal or
increased levels despite substantial kidney damage and that patients with kidney damage are at increased risk of the
two major outcomes of chronic kidney disease: loss of kidney function and development of cardiovascular disease.
The loss of protein in the urine is regarded as an independent marker for worsening of renal function and
cardiovascular disease. Hence, British guidelines append the letter "P" to the stage of chronic kidney disease if there
is significant protein loss.
Stage 1
Slightly diminished function; kidney damage with normal or relatively high GFR (90 mL/min/1.73 m2). Kidney
damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine test
or imaging studies.
Stage 2
Mild reduction in GFR (6089 mL/min/1.73 m2) with kidney damage. Kidney damage is defined as pathological
abnormalities or markers of damage, including abnormalities in blood or urine test or imaging studies.
Stage 3
Moderate reduction in GFR (3059 mL/min/1.73 m2). British guidelines distinguish between stage 3A (GFR 4559)
and stage 3B (GFR 3044) for purposes of screening and referral.
Stage 4
Severe reduction in GFR (1529 mL/min/1.73 m2) Preparation for renal replacement therapy
Stage 5
Established kidney failure (GFR <15 mL/min/1.73 m2, permanent renal replacement therapy (RRT), or end stage
renal disease (ESRD)
NDD-CKD vs. ESRD
The term non-dialysis dependent CKD, also abbreviated as NDD-CKD, is a designation used to encompass the status
of those persons with an established CKD who do not yet require the life-supporting treatments for renal failure
known as renal replacement therapy (including maintenance dialysis or renal transplantation). The condition of
individuals with CKD, who require either of the 2 types of renal replacement therapy (dialysis or transplantation), is
referred to as the end-stage renal disease (ESRD). Hence, the start of the ESRD is practically the irreversible
conclusion of the NDD-CKD. Even though the non-dialysis dependent status refers to the status of persons with
earlier stages of CKD (stages 1 to 4), patients with advanced stage of CKD (Stage 5), who have not yet started renal
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
replacement therapy are also referred to as NDD-CKD.
Screening
Screening those who neither have symptoms or risk factors for chronic kidney disease is not recommended. Those
who should be screened include: those with hypertension or history of cardiovascular disease, those with diabetes or
marked obesity, those aged > 60 years, subjects with indigenous racial origin, those with a history of renal disease in
the past, as well as subjects who have relatives who had kidney disease requiring dialysis. Screening should include
calculation of estimated GFR/1.73 m2 from the serum creatinine level, and measurement of urine-to-albumin
creatinine ratio in a first-morning urine specimen as well as dipstick screen for hematuria. Guidelines for
nephrologist referral vary among different countries. Nephrology referral is useful when eGFR/1.73m2 is less than 30
or decreasing by more than 3 mL/min/year, when urine albumin-to-creatinine ratio is more than 30mg/g, when
blood pressure is difficult to control, or when hematuria or other findings suggest either a primarily glomerular
disorder or secondary disease amenable to specific treatment. Other benefits of early nephrology referral include
proper patient education regarding options for renal replacement therapy as well as pre-emptive transplantation, and
timely workup and placement of an arteriovenous fistula in those patients opting for future hemodialysis.
Treatment
The presence of chronic kidney disease confers a markedly increased risk of cardiovascular disease, and people with
CKD often have other risk factors for heart disease, such as hyperlipidemia. The most common cause of death in
people with CKD is therefore cardiovascular disease rather than renal failure. Aggressive treatment of
hyperlipidemia is warranted.
Apart from controlling other risk factors, the goal of therapy is to slow down or halt the progression of CKD to stage
5. Control of blood pressure and treatment of the original disease, whenever feasible, are the broad principles of
management. Generally, angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor antagonists
(ARBs) are used, as they have been found to slow the progression of CKD to stage 5. Although the use of ACE
inhibitors and ARBs represents the current standard of care for patients with CKD, patients progressively lose kidney
function while on these medications, as seen in the IDNT and RENAAL studies, which reported a decrease over time
in estimated glomerular filtration rate (an accurate measure of CKD progression, as detailed in the K/DOQI
guidelines) in patients treated by these conventional methods.
Currently, several compounds are in development for CKD. These include, but are not limited to, bardoxolone
methyl, olmesartan medoxomil, sulodexide, and avosentan.
Replacement of erythropoietin and calcitriol, two hormones processed by the kidney, is often necessary in people
with advanced disease. Guidelines[11] recommend treatment with parenteral iron prior to treatment with
erythropoietin. A target hemoglobin level of 9-12 g/dL is recommended. Phosphate binders are also used to control
the serum phosphate levels, which are usually elevated in advanced chronic kidney disease. Zerenex(TM), a very
promising new drug developed by Keryx Biopharma will have the ability to treat both elevated serum phosphate
levels and anemia in CKD patients likely reducing or eliminating the need for other drugs i.e. IV iron and ESA's.
When one reaches stage 5 CKD, renal replacement therapy is usually required, in the form of either dialysis or a
transplant.
The normalization of hemoglobin has not been found to be of any benefit to the CKD but does significantly improve
the patient's quality of life in reducing symptoms such as fatigue and can improve other co-morbidities that might be
present, such as chronic heart failure (CHF).[citation needed] Although the evidence for them is limited,
phosphodiesterase-5 inhibitors and zinc show potential for helping men with sexual dysfunction.
182
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
Prognosis
The prognosis of patients with chronic kidney disease is guarded as epidemiological data has shown that all cause
mortality (the overall death rate) increases as kidney function decreases. The leading cause of death in patients with
chronic kidney disease is cardiovascular disease, regardless of whether there is progression to stage 5.
While renal replacement therapies can maintain patients indefinitely and prolong life, the quality of life is severely
affected. Renal transplantation increases the survival of patients with stage 5 CKD significantly when compared to
other therapeutic options; however, it is associated with an increased short-term mortality due to complications of the
surgery. Transplantation aside, high intensity home hemodialysis appears to be associated with improved survival
and a greater quality of life, when compared to the conventional three times a week hemodialysis and peritoneal
dialysis.
Cancer risk
Patients with end-stage renal disease are at increased overall risk for cancer. This risk is particularly high in younger
patients and gradually diminishes with age. Medical specialty professional organizations recommend that physicians
not perform routine cancer screening in patients with limited life expectancies due to ESRD because evidence does
not show that such tests lead to improved patient outcomes.
Epidemiology
Chronic kidney disease globally resulted in 735,000 deaths in 2010 up from 400,000 deaths in 1990.
In Canada 1.9 to 2.3 million people have chronic kidney disease. In the US, the Centers for Disease Control and
Prevention found that CKD affected an estimated 16.8% of adults aged 20 years and older, during 1999 to 2004. UK
estimates suggest that 8.8% of the population of Great Britain and Northern Ireland have symptomatic CKD.[12]
Chronic kidney disease (CKD) is a major concern in African Americans, mostly due to increased prevalence of
hypertension. As an example, 37% of end-stage renal disease cases in African Americans can be attributed to high
blood pressure, compared with 19% among caucasians. Treatment efficacy also differs between racial groups.
Administration of anti-hypertensive drugs generally halts disease progression in white populations, but has little
effect in slowing renal disease among blacks, and additional treatment such as bicarbonate therapy is often required.
While lower socioeconomic status contributes to prevalence of CKD, there are still significant differences in CKD
prevalence between African Americans and whites when controlling for environmental factors. Studies have shown
that there is a true association between history of chronic renal failure in first or second-degree relatives, and risk of
disease. In addition, African Americans may have higher serum levels of human leukocyte antigens (HLA). High
HLA concentrations can contribute to increased systemic inflammation, which indirectly may lead to heightened
susceptibility for developing kidney disease. Lack of nocturnal reduction in blood pressure among groups of African
Americans is also offered as an explanation, which lends further credence to a genetic etiology of CKD racial
disparities.
A high and so-far unexplained incidence of chronic kidney disease, referred to as the Mesoamerican nephropathy,
has been noted among male workers in Central America, mainly in sugar cane fields in the low-lands of El Salvador
and Nicaragua. Heat stress from long hours of piece-rate work at high average temperatures[13][14][15] (in the range
of 96F) is suspected as are agricultural chemicals and other factors.
183
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Chronic kidney disease
Organizations
In the USA, the National Kidney Foundation is a national organization representing patients and professionals who
treat kidney diseases. The American Kidney Fund (AKF) is a national non-profit organization providing
treatment-related financial assistance to 1 out of every 5 dialysis patients each year. The Renal Support Network
(RSN) is a nonprofit, patient-focused, patient-run organization that provides non-medical services to those affected
by CKD. The American Association of Kidney Patients (AAKP) is a non-profit, patient-centric group focused on
improving the health and well-being of CKD and dialysis patients. The Renal Physicians Association (RPA) is an
association representing nephrology professionals.
In the United Kingdom, the UK National Kidney Federation represents patients, and the Renal Association
represents renal physicians and works closely with the National Service Framework for kidney disease.
Kidney Health Australia serves that country.
The International Society of Nephrology is an international body representing specialists in kidney diseases.
References
[1] http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ N18
[2] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=585. 9
[3] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=585. 1-585. 5
[4] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=403
[5] http:/ / www. diseasesdatabase. com/ ddb11288. htm
[6] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 000471. htm
[7] http:/ / emedicine. medscape. com/ article/ 238798-overview
[8] http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2013/ MB_cgi?field=uid& term=D007676
[9] http:/ / www. usrds. org/
[10] http:/ / www. youtube. com/ watch?v=wO2crSCFE08
[11] NICE: Anaemia management in people with chronic kidney disease (CG114)
[12] The Association of Public Health Observatories Chronic Kidney Disease Prevalence Estimates. 2007 [cited 1/3/2010]; Available from:
http:/ / www. apho. org. uk/ resource/ item. aspx?RID=63798.
[13] http:/ / ajkdblog. org/ 2013/ 07/ 29/ mesoamerican-nephropathy-a-new-entity/
[14] Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH. The Epidemic of Chronic Kidney Disease of Unknown Etiology in
Mesoamerica: A Call for Interdisciplinary Research and Action. Am J Public Health. 2013 Sep 12. [Epub ahead of print]
[15] Johnson RJ, Snchez-Lozada LG. Chronic kidney disease: Mesoamerican nephropathy-new clues to the cause. Nat Rev Nephrol. 2013
Oct;9(10):560-1. doi: 10.1038/nrneph.2013.174. [Epub ahead of print]
External links
National Kidney Foundation (http://www.kidney.org/)
Dialysis Complications of Chronic Renal Failure (http://emedicine.medscape.com/article/1918879-overview)
at eMedicine
The Kidney Foundation of Canada (http://www.kidney.ca)
184
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Dialysis
185
Dialysis
Dialysis
Intervention
Patient receiving dialysis
[1]
ICD-9-CM
39.95
MeSH
D006435
MedlinePlus
007434
[2]
[3]
In medicine dialysis (from Greek dialusis,"", meaning dissolution, dia, meaning through, and lysis,
meaning loosening or splitting) is a process for removing waste and excess water from the blood, and is used
primarily as an artificial replacement for lost kidney function in people with renal failure. Dialysis may be used for
those with an acute disturbance in kidney function (acute kidney injury, previously acute renal failure), or
progressive but chronically worsening kidney functiona state known as chronic kidney disease stage 5 (previously
chronic renal failure or end-stage renal disease). The latter form may develop over months or years, but in contrast to
acute kidney injury is not usually reversible, and dialysis is regarded as a "holding measure" until a renal transplant
can be performed, or sometimes as the only supportive measure in those for whom a transplant would be
inappropriate.[4]
The kidneys have important roles in maintaining health. When healthy, the kidneys maintain the body's internal
equilibrium of water and minerals (sodium, potassium, chloride, calcium, phosphorus, magnesium, sulfate). The
acidic metabolism end-products that the body cannot get rid of via respiration are also excreted through the kidneys.
The kidneys also function as a part of the endocrine system, producing erythropoietin and calcitriol. Erythropoietin is
involved in the production of red blood cells and calcitriol plays a role in bone formation.[5] Dialysis is an imperfect
treatment to replace kidney function because it does not correct the compromised endocrine functions of the kidney.
Dialysis treatments replace some of these functions through diffusion (waste removal) and ultrafiltration (fluid
removal).
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Dialysis
186
History
Dr. Willem Kolff, a Dutch physician, constructed the first working dialyzer in
1943 during the Nazi occupation of the Netherlands.[6] Due to the scarcity of
available resources, Kolff had to improvise and build the initial machine
using sausage casings, beverage cans, a washing machine, and various other
items that were available at the time. Over the following two
years,[1943-1945] Kolff used his machine to treat 16 patients suffering from
acute kidney failure, but the results were unsuccessful. Then, in 1945, a
67-year-old comatose woman regained consciousness following 11 hours of
hemodialysis with the dialyzer, and lived for another seven years before dying
of an unrelated condition. She was the first-ever patient successfully treated with dialysis.
Arm showing tubes
Principle
Dialysis works on the principles of the diffusion of solutes and
ultrafiltration of fluid across a semi-permeable membrane. Diffusion is
a property of substances in water; substances in water tend to move
from an area of high concentration to an area of low concentration.[7]
Blood flows by one side of a semi-permeable membrane, and a
dialysate, or special dialysis fluid, flows by the opposite side. A
semipermeable membrane is a thin layer of material that contains holes
of various sizes, or pores. Smaller solutes and fluid pass through the
membrane, but the membrane blocks the passage of larger substances
(for example, red blood cells, large proteins). This replicates the
filtering process that takes place in the kidneys, when the blood enters
the kidneys and the larger substances are separated from the smaller
ones in the glomerulus.
The two main types of dialysis, hemodialysis and peritoneal dialysis,
remove wastes and excess water from the blood in different ways.
Hemodialysis removes wastes and water by circulating blood outside
A hemodialysis machine
the body through an external filter, called a dialyzer, that contains a
semipermeable membrane. The blood flows in one direction and the
dialysate flows in the opposite. The counter-current flow of the blood and dialysate maximizes the concentration
gradient of solutes between the blood and dialysate, which helps to remove more urea and creatinine from the blood.
The concentrations of solutes (for example potassium, phosphorus, and urea) are undesirably high in the blood, but
low or absent in the dialysis solution, and constant replacement of the dialysate ensures that the concentration of
undesired solutes is kept low on this side of the membrane. The dialysis solution has levels of minerals like
potassium and calcium that are similar to their natural concentration in healthy blood. For another solute,
bicarbonate, dialysis solution level is set at a slightly higher level than in normal blood, to encourage diffusion of
bicarbonate into the blood, to act as a pH buffer to neutralize the metabolic acidosis that is often present in these
patients. The levels of the components of dialysate are typically prescribed by a nephrologist according to the needs
of the individual patient.
In peritoneal dialysis, wastes and water are removed from the blood inside the body using the peritoneal membrane
of the peritoneum as a natural semipermeable membrane. Wastes and excess water move from the blood, across the
peritoneal membrane, and into a special dialysis solution, called dialysate, in the abdominal cavity which has a
composition similar to the fluid portion of blood.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Dialysis
Types
There are three primary and two secondary types of dialysis: hemodialysis (primary), peritoneal dialysis (primary),
hemofiltration (primary), hemodiafiltration (secondary), and intestinal dialysis (secondary).
Hemodialysis
In hemodialysis, the patient's blood is
pumped
through
the
blood
compartment of a dialyzer, exposing it
to a partially permeable membrane.
The dialyzer is composed of thousands
of tiny synthetic hollow fibers. The
fiber wall acts as the semipermeable
membrane. Blood flows through the
fibers, dialysis solution flows around
the outside of the fibers, and water and
wastes move between these two
solutions.[8] The cleansed blood is then
returned via the circuit back to the
body. Ultrafiltration occurs by
increasing the hydrostatic pressure
across the dialyzer membrane. This
usually is done by applying a negative
pressure to the dialysate compartment
Hemodialysis schematic
of the dialyzer. This pressure gradient
causes water and dissolved solutes to move from blood to dialysate, and allows the removal of several litres of
excess fluid during a typical 4-hour treatment. In the US, hemodialysis treatments are typically given in a dialysis
center three times per week (due in the US to Medicare reimbursement rules); however, as of 2007 over 2,500 people
in the US are dialyzing at home more frequently for various treatment lengths. Studies have demonstrated the
clinical benefits of dialyzing 5 to 7 times a week, for 6 to 8 hours. This type of hemodialysis is usually called
"nocturnal daily hemodialysis", which a study has shown a significant improvement in both small and large
molecular weight clearance and decrease the requirement of taking phosphate binders.[9] These frequent long
treatments are often done at home while sleeping, but home dialysis is a flexible modality and schedules can be
changed day to day, week to week. In general, studies have shown that both increased treatment length and
frequency are clinically beneficial.[10]
Hemodialysis was one of the most common procedures performed in U.S. hospitals in 2011, occurring in 909,000
stays (a rate of 29 stays per 10,000 population).[11]
187
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Dialysis
Peritoneal dialysis
In peritoneal dialysis, a sterile solution containing glucose
(called dialysate) is run through a tube into the peritoneal
cavity, the abdominal body cavity around the intestine, where
the peritoneal membrane acts as a partially permeable
membrane. The peritoneal membrane or peritoneum is a layer
of tissue containing blood vessels that lines and surrounds the
peritoneal, or abdominal, cavity and the internal abdominal
organs (stomach, spleen, liver, and intestines).[12] Diffusion
and osmosis drive waste products and excess fluid through the
peritoneum into the dialysate until the dialysate approaches
equilibrium with the body's fluids. Then the dialysate is
drained, discarded, and replaced with fresh dialysate.[13]
This exchange is repeated 4-5 times per day; automatic
systems can run more frequent exchange cycles overnight.
Peritoneal dialysis is less efficient than hemodialysis, but
Schematic diagram of peritoneal dialysis
because it is carried out for a longer period of time the net
effect in terms of removal of waste products and of salt and
water are similar to hemodialysis. Peritoneal dialysis is carried out at home by the patient, often without help. This
frees patients from the routine of having to go to a dialysis clinic on a fixed schedule multiple times per week.
Peritoneal dialysis can be performed with little to no specialized equipment (other than bags of fresh dialysate).
Hemofiltration
Hemofiltration is a similar treatment to hemodialysis, but it makes use of a different principle. The blood is pumped
through a dialyzer or "hemofilter" as in dialysis, but no dialysate is used. A pressure gradient is applied; as a result,
water moves across the very permeable membrane rapidly, "dragging" along with it many dissolved substances,
including ones with large molecular weights, which are not cleared as well by hemodialysis. Salts and water lost
from the blood during this process are replaced with a "substitution fluid" that is infused into the extracorporeal
circuit during the treatment. Hemodiafiltration is the combining of hemodialysis and hemofiltration in one process.
Hemodiafiltration
Hemodiafiltration is a combination of hemodialysis and hemofiltration.
Intestinal dialysis
In intestinal dialysis, the diet is supplemented with soluble fibres such as acacia fibre, which is digested by bacteria
in the colon. This bacterial growth increases the amount of nitrogen that is eliminated in fecal waste. An alternative
approach utilizes the ingestion of 1 to 1.5 liters of non-absorbable solutions of polyethylene glycol or mannitol every
fourth hour.
188
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Dialysis
Starting indications
The decision to initiate dialysis or hemofiltration in patients with renal failure depends on several factors. These can
be divided into acute or chronic indications.
Indications for dialysis in the patient with acute kidney injury are summarized with the vowel acronym of
"AEIOU":
1. Acidemia from metabolic acidosis in situations in which correction with sodium bicarbonate is impractical or
may result in fluid overload
2. Electrolyte abnormality, such as severe hyperkalemia, especially when combined with AKI
3. Intoxication, that is, acute poisoning with a dialyzable substance. These substances can be represented by the
mnemonic SLIME: salicylic acid, lithium, isopropanol, Magnesium-containing laxatives, and ethylene glycol
4. Overload of fluid not expected to respond to treatment with diuretics
5. Uremia complications, such as pericarditis, encephalopathy, or gastrointestinal bleeding.
Chronic indications for dialysis:
1. Symptomatic renal failure
2. Low glomerular filtration rate (GFR) (RRT often recommended to commence at a GFR of less than 10-15
mls/min/1.73m2). In diabetics, dialysis is started earlier.
3. Difficulty in medically controlling fluid overload, serum potassium, and/or serum phosphorus when the GFR
is very low
References
[1]
[2]
[3]
[4]
[5]
[6]
http:/ / icd9cm. chrisendres. com/ index. php?srchtype=procs& srchtext=39. 95& Submit=Search& action=search
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?field=uid& term=D006435
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 007434. htm
Pendse S, Singh A, Zawada E. Initiation of Dialysis. In: Handbook of Dialysis. 4th ed. New York, NY; 2008:1421
Brundage D. Renal Disorders. St. Louis, MO: Mosby; 1992
Willem Kolff, Doctor Who Invented Kidney and Heart Machines, Dies at 97. http:/ / www. nytimes. com/ 2009/ 02/ 13/ health/ 13kolff.
html?pagewanted=all; New York Times, 2009
[7] Mosbys Dictionary of Medicine, Nursing, & Health Professions. 7th ed. St. Louis, MO; Mosby: 2006
[8] Ahmad S, Misra M, Hoenich N, Daugirdas J. Hemodialysis Apparatus. In: Handbook of Dialysis. 4th ed. New York, NY; 2008:59-78.
[9] Rocco MV.More frequent hemodialysis: back to the future? In: Advances in Chronic Kidney Disease. Volume 14, issue 3; 2007:e1-9.
[10] Daily therapy study results compared (http:/ / www. homedialysis. org/ learn/ types/ )
[11] Pfuntner A., Wier L.M., Stocks C. Most Frequent Procedures Performed in U.S. Hospitals, 2011. HCUP Statistical Brief #165. October
2013. Agency for Healthcare Research and Quality, Rockville, MD. (http:/ / www. hcup-us. ahrq. gov/ reports/ statbriefs/ sb165. jsp).
[12] Blake P, Daugirdas J. Physiology of Peritoneal Dialysis. In: Handbook of Dialysis. 4th ed. New York, NY; 2008:323-338
[13] Kallenbach J.Z. In: Review of hemodialysis for nurses and dialysis personnel. 7th ed. St. Louis, Missouri:Elsevier Mosby; 2005.
External links
Machine Cleans Blood While You Wait (http://books.google.com/books?id=ZyEDAAAAMBAJ&
pg=PA103#v=onepage&f=true)1950 article on early use of Dialysis machine at Bellevue Hospital New York
Cityi.e. example of how complex and large early dialysis machines were
Home Dialysis Museum (http://www.homedialysis.org/home-dialysis-basics/machines-and-supplies/
dialysis-museum)History and pictures of dialysis machines through time
Introduction to Dialysis Machines (http://www.maximintegrated.com/app-notes/index.mvp/id/
4698)Tutorial describing the main subfunctions of dialysis systems.
189
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
190
Kidney transplantation
Kidney transplantation
Intervention
[1]
ICD-10-PCS
OTY
ICD-9-CM
55.6
MeSH
D016030
OPS-301code:
5-555
MedlinePlus
003005
[2]
[3]
[4]
[5]
Kidney transplantation or renal transplantation is the organ transplant of a kidney into a patient with end-stage
renal disease. Kidney transplantation is typically classified as deceased-donor (formerly known as cadaveric) or
living-donor transplantation depending on the source of the donor organ. Living-donor renal transplants are further
characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on
whether a biological relationship exists between the donor and recipient. Exchanges and chains are a novel approach
to expand the living donor pool.
History
The first kidney transplantation in the United States was performed on June 17, 1950, on Ruth Tucker, a 44-year-old
woman with polycystic kidney disease, at Little Company of Mary Hospital in Evergreen Park, Illinois. Although the
donated kidney was rejected ten months later because no immunosuppressive therapy was available at the timethe
development of effective antirejection drugs was years awaythe intervening time gave Tucker's remaining kidney
time to recover and she lived another five years.
The first kidney transplants between living patients were undertaken in 1954 in Boston and Paris. The Boston
transplantation, performed on December 23, 1954, at Brigham Hospital was performed by Joseph Murray, J.
Hartwell Harrison, John P. Merrill and others. The procedure was done between identical twins Ronald and Richard
Herrick to eliminate any problems of an immune reaction. For this and later work, Dr. Murray received the Nobel
Prize for Medicine in 1990. The recipient, Richard Herrick, died eight years after the transplantation.
The first kidney transplantation in the United Kingdom did not occur until 1960, when Michael Woodruff performed
one between identical twins in Edinburgh. Until the routine use of medications to prevent and treat acute rejection,
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
introduced in 1964, deceased donor transplantation was not performed. The kidney was the easiest organ to
transplant: tissue typing was simple, the organ was relatively easy to remove and implant, live donors could be used
without difficulty, and in the event of failure, kidney dialysis was available from the 1940s. Tissue typing was
essential to the success: early attempts in the 1950s on sufferers from Bright's disease had been very unsuccessful.
The major barrier to organ transplantation between genetically non-identical patients lay in the recipient's immune
system, which would treat a transplanted kidney as a "non-self" and immediately or chronically, reject it. Thus,
having medications to suppress the immune system was essential. However, suppressing an individual's immune
system places that individual at greater risk of infection and cancer (particularly skin cancer and lymphoma), in
addition to the side effects of the medications.
The basis for most immunosuppressive regimens is prednisolone, a corticosteroid. Prednisolone suppresses the
immune system, but its long-term use at high doses causes a multitude of side effects, including glucose intolerance
and diabetes, weight gain, osteoporosis, muscle weakness, hypercholesterolemia, and cataract formation.
Prednisolone alone is usually inadequate to prevent rejection of a transplanted kidney. Thus other, non-steroid
immunosuppressive agents are needed, which also allow lower doses of prednisolone.
Indications
The indication for kidney transplantation is end-stage renal disease (ESRD), regardless of the primary cause. This is
defined as a glomerular filtration rate <15ml/min/1.73 sq.m. Common diseases leading to ESRD include malignant
hypertension, infections, diabetes mellitus, and focal segmental glomerulosclerosis; genetic causes include
polycystic kidney disease, a number of inborn errors of metabolism, and autoimmune conditions such as lupus.
Diabetes is the most common cause of kidney transplantation, accounting for approximately 25% of those in the US.
The majority of renal transplant recipients are on dialysis (peritoneal dialysis or hemofiltration) at the time of
transplantation. However, individuals with chronic renal failure who have a living donor available may undergo
pre-emptive transplantation before dialysis is needed.
Contraindications and requirements
Contraindications include both cardiac and pulmonary insufficiency, as well as hepatic disease. Concurrent tobacco
use and morbid obesity are also among the indicators putting a patient at a higher risk for surgical complications.
Kidney transplant requirements vary from program to program and country to country. Many programs place limits
on age (e.g. the person must be under a certain age to enter the waiting list) and require that one must be in good
health (aside from the kidney disease). Significant cardiovascular disease, incurable terminal infectious diseases and
cancer often are transplant exclusion criteria. In addition, candidates are typically screened to determine if they will
be compliant with their medications, which is essential for survival of the transplant. People with mental illness
and/or significant on-going substance abuse issues may be excluded.
HIV was at one point considered to be a complete contraindication to transplantation. There was fear that
immunosuppressing someone with a depleted immune system would result in the progression of the disease.
However, some research seem to suggest that immunosuppressive drugs and antiretrovirals may work synergistically
to help both HIV viral loads/CD4 cell counts and prevent active rejection.
191
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
Sources of kidneys
Since medication to prevent rejection is so effective, donors do not need to be similar to their recipient. Most donated
kidneys come from deceased donors; however, the utilization of living donors in the United States is on the rise. In
2006, 47% of donated kidneys were from living donors.[6] This varies by country: for example, only 3% of kidneys
transplanted during 2006 in Spain came from living donors.[7]
Living donors
Approximately one in three donations in the US, UK, and Israel is now from a live donor.[8][9] Potential donors are
carefully evaluated on medical and psychological grounds. This ensures that the donor is fit for surgery and has no
disease which brings undue risk or likelihood of a poor outcome for either the donor or recipient. The psychological
assessment is to ensure the donor gives informed consent and is not coerced. In countries where paying for organs is
illegal, the authorities may also seek to ensure that a donation has not resulted from a financial transaction.
The relationship the donor has to the recipient has evolved over the years. In the 1950s, the first successful living
donor transplants were between identical twins. In the 1960s-1970s, live donors were genetically related to the
recipient. However, during the 1980s-1990s, the donor pool was expanded further to emotionally related individuals
(spouses, friends). Now the elasticity of the donor relationship has been stretched to include acquaintances and even
strangers ("altruistic donors").
The acceptance of altruistic donors has enabled chains of transplants to form. Kidney chains [10] are initiated when
an altruistic donor donates a kidney to a patient who has a willing but incompatible donor. This incompatible donor
then "pays it forward" and passes on the generosity to another recipient who also had a willing but incompatible
donor. Michael Rees from the University of Toledo developed the concept of open-ended chains.[11] This was a
variation of a concept developed at Johns Hopkins University.[12] On July 30, 2008, an altruistic donor kidney was
shipped via commercial airline from Cornell to the University of California, Los Angeles, thus triggering a chain of
transplants.[13] The shipment of living donor kidneys, computer-matching software algorithms, and cooperation
between transplant centers has enabled long-elaborate chains to be formed.[14]
There is good evidence that kidney donation is not associated with long-term harm to the donor. Traditionally, the
donor procedure has been through a single incision of 47 inches (1018cm), but live donation is being increasingly
performed by laparoscopic surgery. This reduces pain and accelerates recovery for the donor. Operative time and
complications decreased significantly after a surgeon performed 150 cases. Live donor kidney grafts have higher
long-term success rates than those from deceased donors. Since the increase in the use of laparoscopic surgery, the
number of live donors has increased. Any advance which leads to a decrease in pain and scarring and swifter
recovery has the potential to boost donor numbers. In January 2009, the first all-robotic kidney transplant was
performed at Saint Barnabas Medical Center through a two-inch incision. In the following six months, the same team
performed eight more robotic-assisted transplants.[15]
In 2004 the FDA approved the Cedars-Sinai High Dose IVIG therapy which reduces the need for the living donor to
be the same blood type (ABO compatible) or even a tissue match. The therapy reduced the incidence of the
recipient's immune system rejecting the donated kidney in highly sensitized patients.
In 2009 at the Johns Hopkins Medical Center, a healthy kidney was removed through the donor's vagina. Vaginal
donations promise to speed recovery and reduce scarring. The first donor was chosen as she had previously had a
hysterectomy. The extraction was performed using natural orifice transluminal endoscopic surgery, where an
endoscope is inserted through an orifice, then through an internal incision, so that there is no external scar. The
recent advance of single port laparoscopy requiring only one entry point at the navel is another advance with
potential for more frequent use.
192
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
Organ trade
In the developing world some people sell their organs. Such people are often in grave poverty or are exploited by
salespersons. The people who travel to make use of these kidneys are often known as "transplant tourists." This
practice is opposed by a variety of human rights groups, including Organs Watch, a group established by medical
anthropologists, which was instrumental in exposing illegal international organ selling rings. These patients may
have increased complications owing to poor infection control and lower medical and surgical standards. One surgeon
has said that organ trade could be legalized in the UK to prevent such tourism, but this is not seen by the National
Kidney Research Fund as the answer to a deficit in donors.[16]
Deceased donors
Deceased donors can be divided in two groups:
Brain-dead (BD) donors
Donation after Cardiac Death (DCD) donors
Although brain-dead (or "beating heart") donors are considered dead, the donor's heart continues to pump and
maintain the circulation. This makes it possible for surgeons to start operating while the organs are still being
perfused. During the operation, the aorta will be cannulated, after which the donor's blood will be replaced by an
ice-cold storage solution, such as UW (Viaspan), HTK, or Perfadex. Depending on which organs are transplanted,
more than one solution may be used simultaneously. Due to the temperature of the solution, and since large amounts
of cold NaCl-solution are poured over the organs for a rapid cooling, the heart will stop pumping.
"Donation after Cardiac Death" donors are patients who do not meet the brain-dead criteria but, due to the unlikely
chance of recovery, have elected via a living will or through family to have support withdrawn. In this procedure,
treatment is discontinued (mechanical ventilation is shut off). After a time of death has been pronounced, the patient
is rushed to the operating room where the organs are recovered. Storage solution is flushed through the organs. Since
the blood is no longer being circulated, coagulation must be prevented with large amounts of anti-coagulation agents
such as heparin. Several ethical and procedural guidelines must be followed; most importantly, the organ recovery
team should not participate in the patient's care in any manner until after death has been declared.
Compatibility
In general, the donor and recipient should be ABO blood group and crossmatch (HLA antigen) compatible. If a
potential living donor is incompatible with their recipient, the donor could be exchange for a compatible kidney.
Kidney exchange, also known as "kidney paired donation" or "chains" had recently gained popularity over the past
few years.
In an effort to reduce the risk of rejection during incompatible transplantation, ABO-incompatible and
densensitization protocols utilizing intravenous immunoglobulin (IVIG) have been developed, with the aim to reduce
ABO and HLA antibodies that the recipient may have to the donor.
In the 1980s, experimental protocols were developed for ABO-incompatible transplants using increased
immunosuppression and plasmapheresis. Through the 1990s these techniques were improved and an important study
of long-term outcomes in Japan was published ([17]). Now, a number of programs around the world are routinely
performing ABO-incompatible transplants.
The level of sensitization to donor HLA antigens is determined by performing a panel reactive antibody test on the
potential recipient. In the United States, up to 17% of all deceased donor kidney transplants have no HLA mismatch.
However, HLA matching is a relatively minor predictor of transplant outcomes. In fact, living non-related donors are
now almost as common as living (genetically)-related donors.
193
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
Procedure
In most cases the barely functioning existing kidneys are not removed, as this has been shown to increase the rates of
surgical morbidities. Therefore, the kidney is usually placed in a location different from the original kidney, often in
the iliac fossa, so it is often necessary to use a different blood supply:
The renal artery of the kidney, previously branching from the abdominal aorta in the donor, is often connected to
the external iliac artery in the recipient.
The renal vein of the new kidney, previously draining to the inferior vena cava in the donor, is often connected to
the external iliac vein in the recipient.
There is disagreement in surgical textbooks regarding which side of the recipients pelvis to use in receiving the
transplant. Campbell's Urology (2002) recommends placing the donor kidney in the recipients contralateral side (i.e.
a left sided kidney would be transplanted in the recipient's right side) to ensure the renal pelvis and ureter are anterior
in the event that future surgeries are required. In an instance where there is doubt over whether there is enough space
in the recipients pelvis for the donor's kidney the textbook recommends using the right side because the right side
has a wider choice of arteries and veins for reconstruction. Smith's Urology (2004) states that either side of the
recipient's pelvis is acceptable, however the right vessels are more horizontal with respect to each other and
therefore easier to use in the anastomoses. It is unclear what is meant by the words more horizontal. Glen's
Urological Surgery (2004) recommends putting the kidney in the contralateral side in all circumstances. No reason is
explicitly put forth; however, one can assume the rationale is similar to that of Campbell'sto ensure that the renal
pelvis and ureter are most anterior in the event that future surgical correction becomes necessary.
Kidney-pancreas transplant
Occasionally, the kidney is transplanted together with the pancreas.
University of Minnesota surgeons Richard Lillehei and William Kelly
perform the first successful simultaneous pancreas-kidney transplant in
the world in 1966. This is done in patients with diabetes mellitus type
1, in whom the diabetes is due to destruction of the beta cells of the
pancreas and in whom the diabetes has caused renal failure (diabetic
nephropathy). This is almost always a deceased donor transplant. Only
a few living donor (partial) pancreas transplants have been done. For
individuals with diabetes and renal failure, the advantages of earlier
transplant from a living donor (if available) are far superior to the risks
of continued dialysis until a combined kidney and pancreas are
available from a deceased donor.[citation needed] A patient can either
receive a living kidney followed by a donor pancreas at a later date
(PAK, or pancreas-after-kidney) or a combined kidney-pancreas from a
donor (SKP, simultaneous kidney-pancreas).
Transplanting just the islet cells from the pancreas is still in the
Kidney-pancreas transplant
experimental stage, but shows promise. This involves taking a
deceased donor pancreas, breaking it down, and extracting the islet
cells that make insulin. The cells are then injected through a catheter into the recipient and they generally lodge in
the liver. The recipient still needs to take immunosuppressants to avoid rejection, but no surgery is required. Most
people need two or three such injections, and many are not completely insulin-free.
194
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
Post operation
The transplant surgery takes about three hours. The donor kidney will be placed in the lower abdomen and its blood
vessels connected to arteries and veins in the recipient's body. When this is complete, blood will be allowed to flow
through the kidney again. The final step is connecting the ureter from the donor kidney to the bladder. In most cases,
the kidney will soon start producing urine.
Depending on its quality, the new kidney usually begins functioning immediately. Living donor kidneys normally
require 35 days to reach normal functioning levels, while cadaveric donations stretch that interval to 715 days.
Hospital stay is typically for 47 days. If complications arise, additional medications (diuretics) may be administered
to help the kidney produce urine.
Immunosuppressant drugs are used to suppress the immune system from rejecting the donor kidney. These
medicines must be taken for the rest of the patient's life. The most common medication regimen today is a cocktail of
tacrolimus, mycophenolate, and prednisone. Some patients may instead take cyclosporine, sirolimus, or azathioprine.
Cyclosporine, considered a breakthrough immunosuppressive when first discovered in the 1980s, ironically causes
nephrotoxicity and can result in iatrogenic damage to the newly transplanted kidney. Blood levels must be monitored
closely and if the patient seems to have declining renal function, a biopsy may be necessary to determine whether
this is due to rejection or cyclosporine intoxication.
Postoperative diet
Kidney transplant recipients are discouraged from consuming grapefruit, pomegranate and green tea products. These
food products are known to interact with the transplant medications, specifically tacrolimus, cyclosporin and
sirolimus; the blood levels of these drugs may be increased, potentially leading to an overdose.
Acute rejection occurs in 1025% of people after transplant during the first 60 days.[citation needed] Rejection does not
necessarily mean loss of the organ, but it may necessitate additional treatment and medication adjustments.
Complications
Problems after a transplant may include:
Transplant rejection (hyperacute, acute or chronic)
Infections and sepsis due to the immunosuppressant drugs that are required to decrease risk of rejection
Post-transplant lymphoproliferative disorder (a form of lymphoma due to the immune suppressants)
Imbalances in electrolytes including calcium and phosphate which can lead to bone problems among other things
Other side effects of medications including gastrointestinal inflammation and ulceration of the stomach and
esophagus, hirsutism (excessive hair growth in a male-pattern distribution), hair loss, obesity, acne, diabetes
mellitus type 2, hypercholesterolemia, and osteoporosis.
A patient's age and health condition before transplantation affect the risk of complications. Different transplant
centers have different success at managing complications and therefore, complication rates are different from center
to center.
The average lifetime for a donated kidney is ten to fifteen years. When a transplant fails, a patient may opt for a
second transplant, and may have to return to dialysis for some intermediary time.
Infections due to the immunosuppressant drugs used in people with kidney transplants most commonly occurs in
mucocutaneous areas (41%), the urinary tract (17%) and the respiratory tract (14%).[18] The most common infective
agents are bacterial (46%), viral (41%), fungal (13%), and protozoan (1%). Of the viral illnesses, the most common
agents are human cytomegalovirus (31.5%), herpes simplex (23.4%), and herpes zoster (23.4%). Infection is the
cause of death in about one third of people with renal transplants, and pneumonias account for 50% of the patient
deaths from infection.
195
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
196
Prognosis
Kidney transplantation is a life-extending procedure. The typical patient will live 10 to 15 years longer with a kidney
transplant than if kept on dialysis.[19] The increase in longevity is greater for younger patients, but even 75-year-old
recipients (the oldest group for which there is data) gain an average four more years of life. People generally have
more energy, a less restricted diet, and fewer complications with a kidney transplant than if they stay on
conventional dialysis.
Some studies seem to suggest that the longer a patient is on dialysis before the transplant, the less time the kidney
will last. It is not clear why this occurs, but it underscores the need for rapid referral to a transplant program. Ideally,
a kidney transplant should be preemptive, i.e., take place before the patient begins dialysis.
At least four professional athletes have made a comeback to their sport after receiving a transplant: New Zealand
rugby union player Jonah Lomu, German-Croatian Soccer Player Ivan Klasni, and NBA basketballers Sean Elliott
and Alonzo Mourning.[citation needed]
Statistics
Statistics by country, year and donor type
Country Year Cadaveric donor Living donor Total transplants
Canada 2000
724
388
1,112
France 2003
1,991
136
2,127
Italy 2003
1,489
135
1,624
[20] 2010
208
1276
2,484
Spain 2003
1,991
60
2,051
United Kingdom 2003
1,297
439
1,736
[21] 2008
10,551
5,966
16,517
1,854
1,932
Japan
United States
[22][citation needed] 2008
Pakistan - SIUT
Bill Thompson is the longest-surviving American kidney recipient from an unrelated donor, having received his
kidney in 1966 at age 15; it has survived over 40 years.
Denice Lombard of Washington, D.C., received her father's kidney on August 30, 1967, at age 13 and is still alive
and healthy 45 years, 9 months later as of 5-5-13. Her father will turn 85 in October and is still healthy and active.
Robert Brice of Adelaide, South Australia received a cadaver kidney in September 1981 at the age of 42 and is
alive and healthy in 2013.
John Dan of Nairobi, Kenya, was the known longest-surviving kidney recipient in East Africa. He received a
kidney from his brother in 1984 and lived for 27 years.
Chakravarthy from Chennai, India, received kidney from his brother on 2 May 1983 at the age of 29, is still alive
and healthy 27 years later.
Annemarie Grosskopf of Johannesburg, South Africa, received a kidney from a deceased donor in 1981 at the age
of 21, and is alive and healthy 32 years later.
In addition to nationality, transplantation rates differ based on race, sex, and income. A study done with patients
beginning long-term dialysis showed that the sociodemographic barriers to renal transplantation present themselves
even before patients are on the transplant list. For example, different groups express definite interest and complete
pretransplant workup at different rates. Previous efforts to create fair transplantation policies had focused on patients
currently on the transplantation waiting list.
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
In the U.S. health system
Transplant recipients must take immunosuppressive anti-rejection drugs for as long as the transplanted kidney
functions. For the routine immunosuppressives Prograf, Cellcept, and prednisone, these drugs cost US$1,500 per
month. In 1999 the United States Congress passed a law that restricts Medicare from paying for more than three
years for these drugs, unless the patient is otherwise Medicare-eligible. Transplant programs may not transplant a
patient unless the patient has a reasonable plan to pay for medication after the Medicare expires; however, patients
are almost never turned down for financial reasons alone. Half of end-stage renal disease patients only have
Medicare coverage.
In March 2009 a bill was introduced in the U.S. Senate, 565 and in the House, H.R. 1458 that will extend Medicare
coverage of the drugs for as long as the patient has a functioning transplant. This means that patients who have lost
their jobs and insurance will not also lose their kidney and be forced back on dialysis. Dialysis is currently using up
$17 billion yearly of Medicare funds and total care of these patients amounts to over 10% of the entire Medicare
budget.
Bibliography
Brook, Nicholas R.; Nicholson, Michael L. (2003). "Kidney transplantation from non heart-beating donors".
Surgeon 1 (6): 311322. doi:10.1016/S1479-666X(03)80065-3 [23]. PMID15570790 [24].
Danovitch, Gabriel M.; Delmonico, Francis L. (2008). "The prohibition of kidney sales and organ markets should
remain" [25]. Current Opinion in Organ Transplantation 13 (4): 386394. doi:10.1097/MOT.0b013e3283097476
[26]
.
El-Agroudy, Amgad E.; El-Husseini, Amr A.; El-Sayed, Moharam; Ghoneim, Mohamed A. (2003). "Preventing
Bone Loss in Renal Transplant Recipients with Vitamin D" [27]. Journal of the American Society of Nephrology
14 (11): 29752979. doi:10.1097/01.ASN.0000093255.56474.B4 [28]. PMID14569109 [29].
El-Agroudy, Amgad E.; Sabry, Alaa A.; Wafa, Ehab W.; Neamatalla, Ahmed H.; Ismail, Amani M.; Mohsen,
Tarek; Khalil, Abd Allah; Shokeir, Ahmed A. et al. (2007). "Long-term follow-up of living kidney donors: a
longitudinal study" [30]. BJU International 100 (6): 13511355. doi:10.1111/j.1464-410X.2007.07054.x [31].
ISSN1464-4096 [32]. PMID17941927 [33].
Kerry Grens, "Living kidney donations favor some patient groups: study", 'Reuters', Apr 9, 2012. http://www.
reuters.com/article/2012/04/10/health-kidney-donations-idUSL3E8FA0A720120410
John L. Gore, et al., "The Socioeconomic Status of Donors and Recipients of Living Unrelated Renal Transplants
in the United States", 'The Journal of Urology', Volume 187, Issue 5, May 2012, Pages 17601765. http://www.
sciencedirect.com/science/article/pii/S0022534711060617
Notes
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
http:/ / www. icd10data. com/ ICD10PCS/ Codes/ 0/ T/ Y
http:/ / icd9cm. chrisendres. com/ index. php?srchtype=procs& srchtext=55. 6& Submit=Search& action=search
http:/ / www. nlm. nih. gov/ cgi/ mesh/ 2011/ MB_cgi?field=uid& term=D016030
http:/ / ops. icd-code. de/ ops/ code/ 5-555. html
http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 003005. htm
Organ Procurement and Transplantation Network, 2007
Organizacin Nacional de Transplantes (ONT), 2007
http:/ / www. highbeam. com/ doc/ 1P1-5994618. html Judy Siegel, "Live liver and lung donations approved. New regulations will give hope
to dozens." 'Jerusalem Post', 09-05-1995 "(subscription required)
[9] "National Data Reports". The Organ Procurement and Transplant Network (OPTN). dynamic. Retrieved 22 Oct 2013. (the link is to a query
interface; Choose Category = Transplant, Organ = Kidney, and select the 'Transplant by donor type' report link)
[10] http:/ / transplants. ucla. edu/ body. cfm?id=112
[11] Rees, M. A., Kopke, J. E., Pelletier, R. P., Segev, D. L., Rutter, M. E., Fabrega, A. J., et al. (2009). A nonsimultaneous, extended,
altruistic-donor chain" The New England journal of medicine 360(11), 10961101.
197
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Kidney transplantation
[12] Montgomery, R. A., Gentry, S. E., Marks, W. H., Warren, D. S., Hiller, J., Houp, J., et al. (2006). Domino paired kidney donation: a strategy
to make best use of live non-directed donation" Lancet 368(9533), 419421.
[13] Butt, F. K., Gritsch, H. A., Schulam, P., Danovitch, G. M., Wilkinson, A., Del Pizzo, J., et al. (2009). Asynchronous, Out-of-Sequence,
Transcontinental Chain Kidney Transplantation: A Novel Concept. American Journal of Transplantation, 9(9), 21802185.
[14] Sack, Kevin. "60 Lives, 30 Kidneys, All Linked." The New York Times. 19 Feb. 2012. http:/ / www. nytimes. com/ 2012/ 02/ 19/ health/
lives-forever-linked-through-kidney-transplant-chain-124. html?pagewanted=all& _r=0. 22 Oct 2013.
[15] New Robot Technology Eases Kidney Transplants (http:/ / wcbstv. com/ health/ da. vinci. robot. 2. 1055154. html), CBS News, June 22,
2009 - accessed July 8, 2009
[16] http:/ / news. bbc. co. uk/ 1/ hi/ health/ 3041363. stm Call to legalise live organ trade
[17] http:/ / www. centerspan. org/ pubs/ transplantation/ 1998/ 0127/ tr029800224o. pdf
[18] Renal Transplants > Renal Transplantation Complications (http:/ / emedicine. medscape. com/ article/ 778255-overview#aw2aab6b7) from
eMedicine. Author: Mert Erogul, MD; Chief Editor: Erik D Schraga, MD. Updated: Dec 5, 2008
[19] Wolfe RA, Ashby VB, Milford EL, et al. Comparison of Mortality in All Patients on Dialysis, Patients on Dialysis Awaiting
Transplantation, and Recipients of a First Cadaveric Transplant. NEJM 1999: 341, 1725-1730.
[20] "Kidney Transplantation Factbook 2011" (http:/ / www. asas. or. jp/ jst/ pdf/ factbook/ factbook2011. pdf)
[21] (the link is to a query interface; Choose Category = Transplant, Organ = Kidney, and select the 'Transplant by donor type' report link)
[22] Official Website of Sindh Institute of Urology & Transplant
[23] http:/ / dx. doi. org/ 10. 1016%2FS1479-666X%2803%2980065-3
[24] http:/ / www. ncbi. nlm. nih. gov/ pubmed/ 15570790
[25] http:/ / journals. lww. com/ co-transplantation/ Abstract/ 2008/ 08000/ The_prohibition_of_kidney_sales_and_organ_markets. 11. aspx
[26] http:/ / dx. doi. org/ 10. 1097%2FMOT. 0b013e3283097476
[27] http:/ / jasn. asnjournals. org/ cgi/ content/ full/ 14/ 11/ 2975
[28]
[29]
[30]
[31]
[32]
[33]
http:/ / dx. doi. org/ 10. 1097%2F01. ASN. 0000093255. 56474. B4
http:/ / www. ncbi. nlm. nih. gov/ pubmed/ 14569109
http:/ / www3. interscience. wiley. com/ cgi-bin/ fulltext/ 118508127/ PDFSTART
http:/ / dx. doi. org/ 10. 1111%2Fj. 1464-410X. 2007. 07054. x
http:/ / www. worldcat. org/ issn/ 1464-4096
http:/ / www. ncbi. nlm. nih. gov/ pubmed/ 17941927
External links
Kidney transplantation (http://www.dmoz.org/Health/Conditions_and_Diseases/Genitourinary_Disorders/
Kidney/End_Stage_Disease/Transplantation//) at the Open Directory Project
198
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Article Sources and Contributors
Article Sources and Contributors
Kidney Source: https://en.wikipedia.org/w/index.php?oldid=583954820 Contributors: 03141119, 1607m4dsk1llz, 16clumsyandshy, 62.253.64.xxx, A3RO, AGodofIrony, AS, Abrech,
Accurizer, Acd1208, Acroterion, Adashiel, AdjustShift, Agentmoose, Ageyban, Ahoerstemeier, Alansohn, Albert Tellier, Aldenrw, Aldis90, Alex.tan, AlexiusHoratius, Allens, Alperen,
Alphachimp, Americanluck, AnakngAraw, Anatomist90, Anaxial, Anclation, Andre Engels, Andrea.gf, Andreas Toth, Andy Dingley, Angela, Animum, Anmats, Anomalocaris, Antandrus,
Antennaman, Anthony, Anthonyhcole, Apparition11, Aravindk editing, Arcadian, ArcticFrog, ArielGold, Ascidian, Askari Mark, Athar shams, Austinpow, AxelBoldt, B'er Rabbit, B-rat,
Babajobu, Back ache, Badger Drink, Basharh, Bass fishing physicist, Beetstra, Bell cheese jk, BenBreen2003, Bensaccount, Bertinho, Bgwhite, Big iron, Big.tuna1515, BigDogRufus, BillpSea,
Blac8, Blah987654, Blast Ulna, Bloodshedder, Blueman1878, BobKawanaka, Bobblewik, Bobsmith040689, Bogey97, Boing! said Zebedee, Bomac, Bongwarrior, Bonhomie, Boofs, Brainmouse,
Broderick, Brother Jonathan, Bryan Aldea, Bryan Derksen, Bryan121, Bunchofgrapes, C.Fred, CE, CFCF, CIreland, Can't sleep, clown will eat me, CanDo, CanadianLinuxUser, Canuckle,
Capricorn42, CardinalDan, Carpentc, Caryw123, Catgut, Ceccomaster, Cedricclint, Ceoil, Chaldor, Chaojoker, Charltonasmith, Chaveso, Cheesemongerbumcheese, Chris Roy, Chrislk02, Ckatz,
Closedmouth, Clovis Sangrail, Cmdrjameson, Common Good, CommonsDelinker, Consequencefree, Conversion script, Corvus cornix, Cpsoper, Craig Pemberton, CrazyChemGuy,
CrazyTerabyte, Cremepuff222, DARTH SIDIOUS 2, DDima, DVD R W, DVdm, Dah Supa Panda, Dale013, DanMS, DanaCake, Dandonkey, DanielCD, Daonguyen95, Darth Pejka,
DavidTanCool, Davidjk, Davidruben, Dawnseeker2000, Dbouillo, Dduck, Delirium, Delldot, Deor, DerHexer, Derpidness123, Diberri, Discospinster, Diyako, Diyar se, DjMD, Doc.mari, Doddy
Wuid, Dooky, Doops, DoriSchatell, Dougofborg, Dpwkbw, DrBethersMD, Drsupermikey, Drunken Pirate, Dthomsen8, Duagloth, Dublinflorg231, ERcheck, Earthengine, Ebdonaldson,
Echothegecko, Ecopley, Edgar181, Edward, Eeekster, Eekerz, Ejdjr, El C, EliasAlucard, Ely1, Epbr123, Eperotao, Eras-mus, Eribro, Erudecorp, Euniceespiritu, Evaa, EvergreenFir, Ewen,
Ewulp, Excirial, Exciter1001, FJPB, Falcon8765, Fama Clamosa, Fantasticarlo, Faradayplank, Fastily, Favonian, FelisLeo, Felix-felix, Fieldday-sunday, Fluffernutter, Forschung, Fratter, Freecat,
FreplySpang, Furrykef, F, GB fan, Gabbe, Gaff, Gaia Octavia Agrippa, Gail, Galactor213, Gareth Griffith-Jones, Garik, Garion96, Gary King, Gaseous Snake, Gc9580, Gciriani, Geeoharee,
Gekritzl, Geneb1955, GermanX, Giftlite, Gilgamesh he, Gilliam, Gillyweed, Ginger555, Ginsengbomb, Glacious, Gludwiczak, Goalie1998, Gobonobo, Gogo Dodo, Googie man, Gouerouz,
GraemeL, Grafikm fr, Graham87, Greeney, GregorB, Grundle, Gtstricky, Gurch, Gurchzilla, Gwernol, HMSSolent, Hadal, Hagerman, Hancong, Hannabee, Hannes Hirzel, Haoie, Harej, Harris7,
Harry, Hauberg, Hawaiian717, Headwes, Hede2000, HendrixEesti, HenryLi, Hermant patel, Hersfold, HiDrNick, Hmsedit, Hoplophile, HowiAuckland, Huckfinne, HumbleGod, Husond, I dream
of horses, Icarus, Icarus3, IceCreamAntisocial, Iggy402, Indiajal, Inoculatedcities, InverseHypercube, Iridescent, Ivan Bajlo, J.delanoy, JForget, JPalonus, JWSchmidt, JaGa, JackPetersen,
Jahnavisatyan, Jakob Theorell, JakobSteenberg, James McNally, Jamoche, January, Jaranda, Jasonasosa, Jauhienij, Jazzbeer27, Jbeans, Jbelker, Jclemens, Jeff G., Jerryseinfeld, Jessdro, Jfdwolff,
Jguard18, Jhelton, Jhenderson777, Jidanni, Jim Douglas, JimVC3, JisterMister, Jlautier, Jmjanzen, John, Johndarrington, Johndheathcote, Johnleemk, Johnny235, Jojhutton, Joliefille,
Jonathan.s.kt, Jose Ramos, Jose77, Joseph Solis in Australia, Joshays, Jovianeye, Jpkb24, Jpogi, JuJube, Julia823, JulieADriver, Juliusceaser101, Jumbo Snails, JustinMullins,
Jvander@sbcglobal.net, Jwkpiano1, Jyril, KC Panchal, Ka Faraq Gatri, Kabeman1001, Kajasudhakarababu, Kappa, Karada, Karlhahn, Karolfranks, Kartano, Katalaveno, Keegscee, Keenan
Pepper, Keilana, Kelly Katula, Kevin Rector, Khazar, Kibi78704, KidneyQuest, King steal7, Kingpin13, Kirrages, Kku, Kleptosquirrel, Knutux, Kochipoik, KokomoNYC, Korg, Kozuch, Kpjas,
Kukini, Kungfuadam, Kuru, L Kensington, LPJamesBond007, Lamro, LearnAnatomy, Leevclarke, Legaldeath, Leonard^Bloom, Leslie Mateus, Lexor, Liam Skoda, Linkinparkdawg, Lisatwo,
Littlealien182, Lordofthe9, Lova Falk, Luckas Blade, Lugia2453, Luk, Luka Krstulovi, Luna Santin, Lycurgus, MC10, MER-C, MONGO, Maartentje, Madskile, Magister Mathematicae,
Makeemlighter, Manderso, Mani1, Mansavian, Maork, Marcatz18, Marcsin, Marek69, Marnanel, Maroux, Marshman, Martin S Taylor, Massimo Catarinella, Matt Deres, Mav, Max Naylor,
Maxxicum, McGeddon, McSly, Mentifisto, Merbabu, Michael H 34, MichaelMaggs, Michig, Mikael Hggstrm, Mike Rosoft, Mikefadock, Milanlan, Mintleaf, Miquonranger03, Mojo Hand,
Moonriddengirl, Mooquackwooftweetmeow, Mothpit, Motmit, MrDarcy, MrTroy, Mridhula, Mseliw, MuanN, Mulder416, Mushroom, Myanw, N5iln, NCurse, NHRHS2010, Nahum Reduta,
Nakon, Nathan B. Kitchen, NawlinWiki, Ndkartik, Nepenthes, Nephron, NerdyScienceDude, NewEnglandYankee, Nezzadar, Ngantengyuen, Ni1997, NickGorton, NickW557, Nightenbelle,
Nihiltres, Nikkislayer7, Niteowlneils, No madol, Noommos, Northumbrian, NotWith, Nthngb, Nubiatech, NuclearWarfare, Numbo3, Nv8200p, O.Koslowski, Oda Mari, Ohnoitsjamie,
OldakQuill, Onceonthisisland, Onlyemarie, Orangepoobumapple, Ossip Groth, Oxymoron83, Ozgod, PFHLai, Pan narrans, Pancreas eater303, Parfait3000, Pashute, Patrick, Patxi lurra, Pb30,
Pdcook, Pekinensis, Pepper, Peytons, Philpossett, Phrasont, Piano non troppo, Picpower13, Pilotguy, Pinethicket, Pinko1977, Planet88 co .uk, Polskigirl16, Prashanthns, PrincessofLlyr, Prodego,
Puffin, QFlyer, Quintote, Qxz, RAlbert NIDDK, RGshredfox, Radiant chains, RadioFan, Rajkiandris, Random Nonsense, RandomAct, Ranveig, Ratarsed, Ratemonth, RattusMaximus,
RealGrouchy, Regulov, RenamedUser01302013, Resoru, RexNL, RhiannonAmelie, Rhomboid, Riana, Richard001, Rje, Rjwilmsi, Rock mechanics, Rodhullandemu, Ronhjones, Ronnoc6655,
Ronz, Rossj81, Rossumcapek, Routerone, Roux, RoyBoy, Rror, RubberDuckyMan, Rumping, Ryan032, SC Young Republican, SJP, SPUI, Saavedro300, Salguy, Salvio giuliano, Sam42,
Sandgem Addict, Sannse, Satellizer, Sayeth, Sbblr0803, Sceptre, Schafferm, Schmancy47, SchreiberBike, Schzmo, Scorpian ad, Scottalter, Scotty mctotty, Scray, Secretlondon, Sephiroth BCR,
Serephine, Shadowbeast656, ShakingSpirit, Shanes, Shawn in Montreal, Shoeofdeath, Shoessss, SimonMayer, Sjakkalle, Sj, Smalljim, Smooth O, Snek01, Soakologist, Soap, Softlavender,
Sonjaaa, Soosed, Sophos II, Sougato, Sovereignscience, SpaceFlight89, Spaully, Spongefrog, Spoonaway, Squids and Chips, Squirepants101, StephenBuxton, Stephenb, Stitchmniac123,
Sugarcolt, Sulnan7358, Summer Song, Sun Creator, Sunlei431, Supapuerco, Sven Manguard, Swiley1983, Syth, Tam83, Tangent747, Tapir Terrific, Tarquin, Tassedethe, Tatterfly, Tdb 32,
Techman224, Terry Vaserum, The Evil Spartan, The JPS, The Magnificent Clean-keeper, The Thing That Should Not Be, TheAMmollusc, TheWeakWilled, Theresa knott, Thesnuffla, Think
outside the box, Thumperward, Thurinym, Tide rolls, Til Eulenspiegel, Timc, Tlsnyder, Tnabtaf, Tnxman307, Tomcowley, Tommy2010, Top.Squark, Toreau, Tpbradbury, TranscendTranslation,
Travelbird, Trevor MacInnis, Trevor Wennblom, Tristanb, Trumpy, Tsemii, Tubular, Tweetlebeetle367, Twix617, Tyrol5, Ubiq, Ucucha, Ugog Nizdast, Uhai, Unckc, Unschool, Unveiled,
Unyoyega, V.narsikar, Vadith, Vanished user 39948282, Vary, Versageek, Versus22, ViciousPotato, Vihsadas, Vishnava, Vivio Testarossa, Vrenator, WadeSimMiser, Walter2cobb, Wavelength,
Wayne Slam, Webclient101, Wham Bam Rock II, Whatiguana, Whkoh, Widr, Wikid77, WikipedianMarlith, Wikipelli, Will Beback, Willlead, Wimt, WinContro, Woohookitty, World,
Worldedixor, Woudloper, Wouterstomp, Wronghumor67, Wtmitchell, Xanchester, Xcentaur, Xufanc, Yanamad, YauTou, Ybbor, Yboord028, Yintan, Yojimbo9102, Yurei-eggtart, Zackkelly,
Zannah, Zefr, Zuzuu, ..24, , 1634 anonymous edits
Renal function Source: https://en.wikipedia.org/w/index.php?oldid=579276975 Contributors: Aadrbi, Aarktica, Adifferentgame, Agonizedsoxfan, Alex Pascual, Altenmann, Andrei S,
Anthonyhcole, Anypodetos, Aravindk editing, Arcadian, Arripay, Axl, Bdesruis, Beetstra, BillpSea, Bloomingdedalus, Bogwhistle, Caramesc, CarrieVS, Chat mauve, Chester Markel, Chris
Capoccia, Chris the speller, CliffC, DGJM, DRosenbach, Danielsc2, Dark-X, Davidruben, Dean.jenkins, Diberri, Docprobly, Download, Drphilharmonic, Eleassar, Eubulides, GLHamilton, GR
Scriptor, Gene Nygaard, GermanX, Grannos, Gsarwa, Hancong, HandsomeFella, Hulek, Jayjg, Jfdwolff, Jiu9, Joewc, Joncomelately, Joshua, Jtdaugir, Kainaw, Kopaka649, Kuhlor, Luke poa,
Madalev, Madhero88, Martin451, Materialscientist, MegaFusionY, Mikael Hggstrm, Mild Bill Hiccup, MrOllie, Muskdial, My Core Competency is Competency, Natural Cut, Nbauman,
Nephron, NikeTenis, Ninad 1999, NoJin, Ntsimp, OldakQuill, Pbleic, Petersam, Pgk, Ph.eyes, Pietrow, Polyethylen, Psc, Qwfp, R.hackney64, RDBrown, Redrafts, Rich Farmbrough, Richardsur,
Rjwilmsi, Robparty, Rrawwbb, Saehrimnir, Scott5834, Shaun, Skittleys, Soaringbear, Suffusion of Yellow, The Illusive Man, The Thing That Should Not Be, Vinnypatel, Wikipelli,
Xabian40409, Yobol, Yurivict, 145 anonymous edits
Renal corpuscle Source: https://en.wikipedia.org/w/index.php?oldid=574091229 Contributors: Alex.tan, Arcadian, Beeswaxcandle, Bensaccount, Bizz42, Bonadea, Centenarian,
ComputerHotline, Cptmurdok, Diberri, Eshan chakraborty, GermanX, Jfdwolff, Jmarchn, Joyous!, Karada, Karsten Adam, M.Komorniczak, Massimo Catarinella, Mysid, Nbauman, Nlu, PFHLai,
Scottalter, Shakiestone, Slaanesh17, Spaully, Taka, 22 anonymous edits
Nephron Source: https://en.wikipedia.org/w/index.php?oldid=581102137 Contributors: 28421u2232nfenfcenc, 3dscience, Abukar29386, AgentCDE, Alansohn, Alex.tan, Alphaarchae,
Angelito7, Anmats, Antandrus, Arcadian, Artaxiad, Atethnekos, AubreyEllenShomo, Auntof6, Axl, Baldhur, Bensaccount, Billyb, Blehfu, Bobianite, Bomac, Bomazi, Burton Radons, Butros,
ButterflyGirlKMC, CSWarren, CattleGirl, Chaldor, ChillyMD, ChrisGualtieri, CielProfond, Cohesion, Cuzimcoolandall, Danfrombontoc, Darkwind, Davegabe, Diberri, DocWatson42,
Dysprosia, Epbr123, Eras-mus, Fraggle81, Freakofnurture, G Clark, Garvin58, Gaurav1146, Geoking66, GermanX, Glenn, Godcast, Hayk, Hermant patel, Heron, Huhsunqu, Husond, Hyalos,
Icarusgeek, Ipvsix, Ismi bigboss, Ixfd64, J.delanoy, JakobSteenberg, Jane Fairfax, Jblongley, Jfdwolff, Jim1138, Jklin, Jrtayloriv, Jsherwood0, Kalaiarasy, Kingpin13, Kpa4941, Kupirijo, LOL,
Leptictidium, Luk, Mac Davis, Mar4ela, Mark Lundquist, Master of Puppets, Materialscientist, Mikael Hggstrm, Mintleaf, MrSomeone, Mysid, NawlinWiki, Nbauman, Nephron,
NewsAndEventsGuy, Nlu, Nuviapalomar, OlEnglish, Omnipaedista, PFHLai, Petesmif, Quadalpha, Ratel, Ratiocinate, Rhadamante, Romanm, Samir, Satori Son, Sayeth, Scorpian ad, Scottalter,
SingleIntegral, Slightsmile, Sonett72, Spaully, Spencer, Spesh531, Spiritia, Stitchmniac123, Sun Creator, Taka, Temporaluser, Thattoe, TheLimbicOne, Thedjatclubrock, Thue, Trevor
Wennblom, Tycho, Van helsing, Versus22, Virgil Vaduva, Weetoddid, Wikid77, WikipedianMarlith, Xwu, 274 anonymous edits
Glomerulus Source: https://en.wikipedia.org/w/index.php?oldid=569963839 Contributors: Alfio, Americanluck, Arakunem, Arcadian, Ccocallas, Chaldor, Chris the speller, DBigXray,
Davidruben, Deflective, Diberri, Dicklyon, Drphilharmonic, Eribro, Gene Nygaard, GermanX, IONTRANSP, Jag123, JamesBWatson, Jfdwolff, Jmarchn, Jonnyerwi, Jujhaar123, KC Panchal,
Karada, Knowledgeforever2, Kwamikagami, L Kensington, M1ss1ontomars2k4, Merbabu, Mikael Hggstrm, Miracle Pen, Moin 525, Mouya, Mysid, Nbauman, NifCurator1, Nlu, NotWith,
Ntsimp, PFHLai, Paulsky, Peter morrell, Phrasont, Pred7799, Prof. Squirrel, Rpseal, Satyajitus, Sayeth, Scottalter, SecretDisc, Shriram, Spaully, Steven J. Anderson, Sun Creator, Temporaluser,
Vojtech.dostal, Vokesk, Vwslee, 66 anonymous edits
Bowman's capsule Source: https://en.wikipedia.org/w/index.php?oldid=578354897 Contributors: 3dscience, A3RO, Acgator09, Agamemnon2, Alex.tan, Alice Mudgarden, Alphachimp,
Anasalfakeer, Arcadian, Auroranorth, Bearly541, Bensaccount, Betacommand, CFCF, Celuici, DancingHorses, Ddlamb, Dogah, Dolanclass, EryZ, Heron, Hpswimmer, Infrogmation, Jag123,
Jfdwolff, Jmarchn, Jonathan.s.kt, Jrtayloriv, Karada, Ken Gallager, M.Komorniczak, Mysid, Nbauman, NeilN, Nlu, PFHLai, Pax:Vobiscum, Philip Trueman, Prof. Squirrel, Rickjpelleg, Sbisolo,
Scottalter, Shenme, Spaully, Sportsguy17, Taka, Talon Artaine, Tartan, Telekenesis, Triwbe, VenomousConcept, Xullius, YaacovCR, 79 anonymous edits
Renal physiology Source: https://en.wikipedia.org/w/index.php?oldid=583335202 Contributors: AK2AK2, AdjustShift, Afacerop, AhMedRMaaty, Alex.tan, Allen3, Arcadian, Arthurvander,
Bensaccount, Bloodshedder, Blueyoshi321, Christian75, DaDannyBoy, DaiM, Diberri, Dieseldrinker, Eleventh Guard, Eribro, Gaff, GermanX, Gilliam, Glane23, GrahamColm, Haisook,
Hreid11, Huckfinne, Iridescent, Ismi bigboss, Jfdwolff, Jonkerz, Kevin Rector, Lomnes, Luckydhaliwal, Madhero88, Materialscientist, Meddstudd, Megaman en m, Mikael Hggstrm,
OldakQuill, Opelio, Ottawa4ever, Rich257, Rjwilmsi, Ruslik0, Sayeth, Seth Ilys, Sinujutsu, Soliloquial, Tapir Terrific, The Rambling Man, The Thing That Should Not Be, Trevyn, Wmahan, 99
199
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Article Sources and Contributors
anonymous edits
Renal glucose reabsorption Source: https://en.wikipedia.org/w/index.php?oldid=526552519 Contributors: KhoousesWiki, Lilac Soul, Mikael Hggstrm, Mogism, Scottalter, 2 anonymous
edits
Renal sodium reabsorption Source: https://en.wikipedia.org/w/index.php?oldid=526548517 Contributors: Adrian J. Hunter, Armando Navarro, Mikael Hggstrm, Scottalter, 6 anonymous
edits
Renal chloride reabsorption Source: https://en.wikipedia.org/w/index.php?oldid=577441031 Contributors: Adrian J. Hunter, Anomalocaris, Mikael Hggstrm, Scottalter, 2 anonymous edits
Renal protein reabsorption Source: https://en.wikipedia.org/w/index.php?oldid=266810464 Contributors: Mikael Hggstrm, Scottalter
Renal tubular acidosis Source: https://en.wikipedia.org/w/index.php?oldid=584085393 Contributors: Alanhay, Anonymos869, Anupam, Arcadian, Area51, BD2412, Baronnet, Bobjgalindo,
Cheekyal, Clam0p, Colonies Chris, Dammalapati.doc, Danielil, Diberri, Diptanshu.D, Dr.queso, Eleassar, Exprobratio, Felix-felix, Fvasconcellos, GermanX, Haddendaddendoedenda, Headbomb,
IronChefSakai, Jmh649, LittleWink, Mat8989, Materialscientist, Mike Dillon, Mike2vil, Mild Bill Hiccup, Nephron, Nick Number, Nimorn, Nrsmoll, Prof. Squirrel, RDBrown, Rhcastilhos, Rich
Farmbrough, Rjwilmsi, RobinHood70, Rswarbrick, Serephine, Smodtactical, Spaschos, Stiffwoolf, Supernova0, Tremello, 76 anonymous edits
Proximal renal tubular acidosis Source: https://en.wikipedia.org/w/index.php?oldid=546189078 Contributors: AManWithNoPlan, Angelito7, Arcadian, Diptanshu.D, GuySh, Magioladitis,
Rewster, SchreiberBike
Distal renal tubular acidosis Source: https://en.wikipedia.org/w/index.php?oldid=572110477 Contributors: Angelito7, Arcadian, BD2412, Bobjgalindo, Diptanshu.D, GuySh, Kirbymaur,
Magioladitis, Mcstrother, 7 anonymous edits
Renal urea handling Source: https://en.wikipedia.org/w/index.php?oldid=533423493 Contributors: Drphilharmonic, Horiavulpe, IONTRANSP, Mikael Hggstrm, Narayansg, Scottalter, 2
anonymous edits
Ammonia Source: https://en.wikipedia.org/w/index.php?oldid=584197275 Contributors: 12 Noon, 198.106.161.xxx, 28421u2232nfenfcenc, 2help, 478jjjz, 9258fahsflkh917fas, A876, ABCD,
Access Denied, Adam Bishop, Ageturnipseed, Ahoerstemeier, Alan Liefting, Alansohn, Ale jrb, Alex.muller, Altar, Ameliorate!, Aminaq, An-nh3, Andre Engels, AndrewBuck, Anindra72, Ann
Stouter, Annabel, Anomalocaris, Antandrus, Apm963, Arakunem, Arjayay, Arkwatem, Arya.kk, AssegaiAli, Ataleh, Aussie Alchemist, AxelBoldt, Az29, Azo bob, BD2412, Baa, Bakasuprman,
Bayerischermann, Bazonka, Bbi5291, Bearfoot, Beetstra, Benbest, Bencbartlett, Bendzh, Benjah-bmm27, Bergsten, BerserkerBen, Bigtophat, Billwhittaker, Biscuittin, Bjohns86, Blackhawk
charlie2003, Blubba112, BluefieldWV, Blueswimmer1, Bobblewik, Bobo192, Bomac, Bongwarrior, Booyabazooka, BoredTerry, Bped1985, Br77rino, Brequinda, Brian1975, Brockert,
Brutus1996, Bryan Derksen, Bunceboy, Can't sleep, clown will eat me, CanisRufus, Cantons-de-l'Est, CardinalDan, Casforty, Catsmeat, Ccrrccrr, Centered1, Cfailde, ChadyWady, Charlieaingel,
Chem540f09grp6, ChemNerd, Chemya, Chmod007, Chodorkovskiy, Chris the speller, ChrisGualtieri, Christopher Parham, Christopher Thomas, Chuunen Baka, Cimex, Cimon Avaro, Civil
Engineer III, Coffee, ColetteHoch, Congruence, Connormah, Conversion script, Cool3, Cpl Syx, CrookedAsterisk, Cyde, Cyrius, DVdm, Danarmak, Dante Alighieri, Darkfight, Darkneonflame,
Darth Panda, Dave19880, Dave3457, David Souther, David.Mestel, Dawnseeker2000, DeLtA, Dekisugi, Deli nk, Delirium, Delldot, Delta G, Denelson83, Dennis Estenson II, DerHexer,
Derek.cashman, Deryck Chan, Dirac1933, Discospinster, Diza, Dkronst, Dmn, DoSiDo, DocWatson42, Don4of4, Donarreiskoffer, Dougmcdonell, Dr. Universe, DrBob, DragonflySixtyseven,
Drahkrub, Dreindl, Drphilharmonic, Dspradau, Duckyphysics, E Wing, Ebe123, EdChem, EdDavies, Edgar181, Edgey, Edgjerp, Editor182, Edsanville, EdwinHJ, Eequor, Eguygabe, Eleuther,
Eliz81, Eloc Jcg, Emayv, Engineman, Eog1916, Epbr123, Espen180, Evercat, Everyking, Ewen, Eyesnore, Farmercarlos, FayssalF, Fenix 9696969, Fenrith, Ferred, Ferroequus, Filemon,
Flyingsquirell19, Foobar, Foobaz, Freestyle-69, FreplySpang, Frymaster, Fys, GA-Chemist, GaMEChld, Gabethenerd, Gadolinist, Gaedheal, Gail, Gaius Cornelius, Gene Nygaard, Gene Ward
Smith, Geni, Gentgeen, George100, Ghirlandajo, Giftlite, Gigemag76, Gign-9, Gilliam, Glaisher, Glenn, Glimmer721, Glst2, Gnarlodious, GoatGuy, Green meklar, Greg Vezina, Guardian of the
Rings, Gurch, Gurubrahma, Gwernol, Gzuckier, Gtz, H Padleckas, HBGary, Hadal, HammerHeadHuman, Hanjifi, HarlandQPitt, Harryboyles, Harthacnut, Hdt83, Hebrides, Hellbus, Hemmer,
Herbee, Heron, Hersfold, HexaChord, Hhhippo, Hi ruwen, Hillrhpc, Honeywell Analytics, Hu, Hut 8.5, Huw Powell, IONTRANSP, IRKAIN, Icairns, Icseaturtles, Ideyal, Iepeulas, Ike9898,
Inetpup, Infrogmation, Intangir, InvictaHOG, Iridescent, Ironman5247, Isilanes, Itub, J.delanoy, J8079s, JHunterJ, JNW, JZNIOSH, Jabowery, Jackollie, Jag450, Jagged 85, JamesGrimshaw,
Jane Bennet, Jarble, Jauhienij, Jcm, Jcwf, Jeff Seeman, Jeffrey O. Gustafson, Jerrypaulmorgan, Jewb1, Jfdwolff, Jimfbleak, Jimmy xu wrk, Jimmyreno, Jkelly, JoanneB, John, John Riemann
Soong, JohnChrysostom, JohnSRoberts99, Johnkarp, JonathanSeale, Jonathanfu, Jonesey95, Jose77, Joseph Solis in Australia, Josh Parris, Joshuas88, Jrockley, Jsjsjs1111, Julesd, Juliancolton,
Jun-Dai, Jynto, Kbk, Keegan, Keenan Pepper, Kelisi, Keyesc, Khazar, Kilo-Lima, King of Hearts, Kjhf, Kjkolb, Kksf5164, Kku, KnowledgeOfSelf, Koavf, Kostisl, Kozuch, Kungming2,
Kupirijo, Kuru, Kwantus, Kweckzilber, L Kensington, Laladonkeykong, Lamarck001, Lamro, LanthanumK, Lawl95, LeaveSleaves, LegacyOfValor, Leonard G., Lexi Marie, Leyo, Lifung, Light
current, Lightmouse, Ligulem, Ling.Nut, Liridon, Lotje, Louisajb, Lowell Larsson, LoyalSoldier, Lstrong2k, Luna Santin, Lysdexia, M1ss1ontomars2k4, M1tk4, MADe,
MATTISMYBESTFRIEND, MER-C, MONGO, MacGyverMagic, Magioladitis, Magister Mathematicae, Magnus Manske, Majoche09090, Malbi, Mangwanani, Mani1, Marauder40, Marc
Venot, Margana, Mark Foskey, Marnanel, Martarius, Materialscientist, Matticus78, Maurreen, Mav, Max Jetzer, Maxim, Max, Mayur, Mbeychok, Mboverload, Mbsbuyer, Medicus587,
Meghas2, Mejor Los Indios, Melsaran, Mentifisto, Metal.lunchbox, MightyWarrior, Mikael Hggstrm, Mikespedia, Mild Bill Hiccup, Mitchellisaacs, Mkweise, Mogism, Moshe Constantine
Hassan Al-Silverburg, Mothmolevna, Mr pand, MrBell, Munita Prasad, Mvsk mohan, Myanw, Mysterious Whisper, N0YKG, NHJG, NHRHS2010, Naidevinci, Narayansg, Narchy, Navdar,
NawlinWiki, Naxletus, Neutrality, Neverquick, Nibuod, Nirmos, Nishkid64, Noctibus, Nohat, Nono64, Northumbrian, NotWith, NuclearWarfare, OllieFury, Onco p53, Onthegogo, Opelio,
Owen214, Owllord97, P. B. Mann, PAK Man, PBS, Palefire, Parent5446, Pashute, PauloCalipari, Pax:Vobiscum, Peak, Pedro, Pegasus1138, Perlzzz, Persian Poet Gal, Petercascio, Phil Boswell,
Philip Trueman, Physchim62, Pinethicket, Pion, Pit, Piwam, PlanetStar, Plasmic Physics, Plasticup, Pmetzger, Porterjoh, Preaky, Psy guy, Pwhitwor, Pyrotec, Qemist, Quadell, Quantumobserver,
Qxz, R'n'B, RB972, RJHall, RJaguar3, Raeky, RainbowOfLight, Ram-Man, Randy Johnston, Rawrrr11, Reaper Eternal, Recognizance, Reedy, RetiredUser2, Rexy88, Reywas92, Rezecib,
Rfc1394, Riana, Rich 988, Richard Arthur Norton (1958- ), Ricka0, Rickjpelleg, Rifleman 82, Riventree, Rjwilmsi, Rmhermen, Rnb.chatterjee, Roberta F., Ronzon775, RoyBoy, Royalbroil,
Russoc4, Rwflammang, Ryan Postlethwaite, RyanJones, Ryanboesch, Rycecube57, Ryulong, SD5, SDC, SJP, Samw, Sanketsingh, Saranghae honey, Sats.mohanty, Sbmehta, Sbrools, Scaryman,
Scot.parker, Scott Roy Atwood, Seanwal111111, SebastianHelm, Securiger, Seresin, SergeyKurdakov, SeventyThree, Sfan00 IMG, Sgr927, Shaddack, Shadowjams, Shanel, Shimmin, Shinpah1,
Shirik, Shoefly, Siafu, Sidhu 2201, SidneySM, Sillybilly, Silverchemist, Smalleditor, Smartse, Smokefoot, Snow Blizzard, Sobolewski, Sonett72, Spaceninja123, Spangineer, Spinningspark,
Squid661, Srleffler, Srtory, Staticd, Steamturn, SteinbDJ, Stephenb, Stephenchou0722, Steven Zhang, Stone, Stwalkerster, Subversive.sound, SuddenFrost, Sunny910910, Sunnybunnyfeelin,
Swpb, Sxeraverx, Syncategoremata, T.vanschaik, Tabby, Taemyr, Taliska, Tarquin, Tarret, Taw, Tawker, Technopat, Telekenesis, Temporaluser, TenOfAllTrades, Tetracube, The Letter J, The
Thing That Should Not Be, The chemistds, The last username left was taken, Thegamecreator1, Thingg, Thricecube, Tide rolls, Tim Starling, Tim1357, Tiptoety, Titoxd, Tobias Bergemann, Tom
harrison, Tony port, Tpbradbury, Triesault, True Pagan Warrior, Trusilver, Tsemii, Twir, Txbangert, Uga71234, Ugen64, Ulric1313, Umweb, Unschool, User119, UtpalC, V8rik, VASANTH
S.N., VMS Mosaic, Varlaam, Vavrik, Vegaswikian, Velella, Verma parikshit, Vsmith, Vuo, Vuong Ngan Ha, Walkerma, Wapcaplet, Wavelength, WaysToEscape, Wdfarmer, Werdan7,
Wfgiuliano, Why Not A Duck, Wickey-nl, Widr, Wik, Wiki alf, Will Beback, William Avery, Wimvandorst, Wizzard2k, Wjejskenewr, Woodsstock, Woohookitty, Xact, Xaosflux, Yamamoto
Ichiro, YanA, Yath, You a fool, Youssefsan, Z koochoolooo, Zapadap, Zbxgscqf, Zidonuke, Ziphon, ZooFari, , , , 1288 anonymous edits
Urine Source: https://en.wikipedia.org/w/index.php?oldid=581971745 Contributors: 123901ab, 21655, 2D, 4twenty42o, 5 albert square, 9oo9, A Stop at Willoughby, A$$merkin69, A1r, ASk,
Aaami111, Aamonroe, Aaronblahah, Abcolleenz79, Acroterion, Action Jackson IV, Adrian J. Hunter, Adz657, Aelius28, Aeris-chan, Afroshock, Agateller, Ahuskay, Aiken drum,
Airforcerules222, Airplaneman, Aitias, Alan Liefting, Alansohn, Albert Krantz, Albievdmorkel, Ale jrb, Aleksa Lukic, Alessgrimal, Alex roy08, Alex43223, Alexcrook15, Alexdamad,
Alexius08, AlexiusHoratius, Aliento, Allen4names, Allstarecho, Alpha 4615, Alphachimp, Altadena, Alucard (Dr.), Alwaysfruche, Alwaysfrush, Alwaysgrammar, Alxeedo, Amaenjea, Amaury,
American Eagle, Amigan, Anchoress, Andrew3345, AndrewHZ, Androstachys, Andy Dingley, Andycjp, Andyjsmith, Angelo Michael, Anna Frodesiak, Annand541, Antandrus, Anthony
Appleyard, Anupamsr, Apers0n, Apothecia, Aquaninja32, Arakunem, Aranea Mortem, Arcadian, Arima, Asdfsdtgtrg, Atlan, AutomatedPwner, Avenged Eightfold, Avicennasis, Awesumkid,
B15nes7, Baba gump, Backslash Forwardslash, Badgernet, Bagelboyz711, Bakilas, BarkerJr, Barneca, BarretB, Basketball203, Bassbonerocks, Battlebruvaz, Bean 246, Beauty1287, Beeblebrox,
Behaafarid, Bellerophon, Bender235, Bentogoa, Bernnybc, Betswiki, Betty.explosive, Bex Dew, Beyond My Ken, Bgwhite, Big pnis vandaI, BigDunc, Bigblueplanet, Bill102, Blackzerox2,
Blanchardb, Bleeblublahblafflesnifflesnork, Blehfu, Blurpeace, Bmfluff123, Bob Castle, Bob Weiss, Bob123321bob, Bobby "big" balls, Bobjameson, Bobo192, Bobtbuilder, Bolivar2008,
Bonadea, Bongwarrior, Boobmania, BookSquirrel, Booooobsaget, Borissimo, Brainslug, BrainyBabe, Brandon, Breawycker, Bremerenator, Brewhaha@edmc.net, Brian Crawford,
Brianaissocoollike, Broadwayblue222, Btharper1221, Bturner4, Buckeyetigre, Butholelicker123, Buthwiki, Cacycle, Cai-444, Caiaffa, Caknuck, Can't sleep, clown will eat me, Cantaloupe2,
Canterbury Tail, Capricorn42, Car salesman, Carolbird, CaryssEvanss, Caseyateme, Catsmeat, Causa sui, Ccgrimm, Celeste6566, Celestra, Charles Elliotte, Cheeseynips, Chick850, Chiu
frederick, Chocolateir, Cholmes75, Chongalicious, Christian75, Chzz, Clicketyclack, Closedmouth, Clq, Coasterlover1994, Cocoapups, Coeus559, Coffee, Cole Jester, Cool3634, Cordell,
Corkupyourbutt, Corpx, Corvus cornix, CouchTomato25, Courcelles, Cpcheung, Crackbaby101, Craig Pemberton, Crazy Boris with a red beard, CrazyChemGuy, Crazymario27397,
Crosstemplejay, Crusoe8181, Csigabi, Cst17, Cubbyblue20, Cue the Strings, Cursedkakashi, CutOffTies, DARTH SIDIOUS 2, DH85868993, DVD R W, DVdm, DX-MON, DaNinjaDude4269,
Dac04, Daedalus969, Daft punkette, Damirgraffiti, Dan D. Ric, Dan Harkless, Dan6hell66, DanBradshaw007, Daniel J. Leivick, DanielCD, Danielpursehouse, Danimadi, Dapurpoopnub,
Darkwhistle, Darren23, Darth Panda, DarthVader, DarwinPeacock, Daven200520, Davewho2, Davewild, David Battle, David Shankbone, Deathawk, Debeo Morium, Debresser, Deedeedee
Steven, Defender of torch, Delicious carbuncle, Delldot, DennyColt, Der lektor, DerHexer, Deusxechelon, Dffgd, Dgw, Diannaa, Dilster82, Dinesh smita, Dirac1933, Discospinster, Dj funnybun,
Doc.mari, Doczilla, Domoorigato, Donalfredo, Donbert, DoubleBlue, Dougweller, Doulos Christos, DoversCHAMP, Download, Downtown dan seattle, Downwards, Dp76764,
Dr.HaNaWaNaLaYa, Dr.suhasini, Dragon tamer21, Drake222, Dreadstar, Dreftymac, Drinhaus10, Dtrebbien, Dublinflorg231, Dumrance, DuncanHill, Duy Huu Nguyen, Dystopos, E2eamon,
E71, ERK, ESkog, EdEColbert, Edgar181, Edgehead772, Edistomosin, Eekerz, Efe, Eiffelle, Elassint, Elfonice, ElinorD, Elipro, Elm-39, Elockid, Em Mitchell, Emicacd, Emily Jensen,
Emmacookies, Emo1234, Enderminh, Enti342, Enviroboy, Epbr123, Eras-mus, Erff217, Eric-Wester, Erielhonan, Erik9, Escape Orbit, Esscoss, Ethnicmb, Eugene-elgato, Everchanging02,
Excirial, Exert, Ezhiki, FCSundae, Falcon8765, Fangfufu, Fartsallot, Fastsloe21, Favonian, Fggt, Fieldday-sunday, FisherQueen, Flarn2006, Flewis, Floquenbeam, Flowerpotman, Fluri,
Flyaway2341, Flyguy649, Flyingpigchicken, Fomz, Frankenpuppy, Freddy257, Frijole, Fugyoo, Fumitol, Funandtrvl, Funny Muffin, Furrykef, Fusionmix, Fyyer, Fck sht and pss, GDonato,
200
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Article Sources and Contributors
Gaara Steaua, Gail, Garyzx, GavinTing, Gefred7112, Gejan, GenOrl, Georgebushloverzz, Gfrsdgerr, Giants27, Gilliam, Ginsengbomb, Gogo Dodo, Googoobah, Grasshead123, Green caterpillar,
GregorB, Grenonator, Greswik, Grika, Grimwwr, GrizzlySound, Grundle, Gsa10, Gscshoyru, Gunnar Hendrich, Gurch, Gurchzilla, Guymclaren, Gwernol, H2g2bob, HCA, Hadgoat, HairyPerry,
Hallows AG, Hammer1980, Hans Dunkelberg, Harry, Hatton123, HendrixEesti, Herecomespattypoo, Hesaiddestroy, HexaChord, Hezzy140, Hfricke, Hmains, Hmdpsych, Hohenheim117,
HokieRNB, Homoland66, Honette, Horse24, Htews, Huji, Hydrogen Iodide, I m dude2002, I42, II MusLiM HyBRiD II, IRP, Iamsexy7, Ianp321, Icairns, Ice Czar, IceCreamAntisocial,
Ieatpolarbears, Iknowsitall, Ilgiz, Imagemonth, Immie 93, InShaneee, Ipwnedyouallwithamelon, Iridescent, Irishguy, Irock57, Ironholds, It Is Me Here, Ixfd64, J Di, J.delanoy, J0nj0nr0b4rt,
JD554, JEN9841, JForget, JFreeman, JGabbard, JNW, JPMcGrath, JaGa, Jaanwy, Jackollie, Jacobfoo918, Jake Wartenberg, Jakio202, Jaksmata, JamesBWatson, Jamoche, Janejellyroll, January,
Jarble, Jareth86, Jasonkaye, Jauerback, Jauhienij, Jaw959, Jay Gatsby, Je.rrt, Jedi Master Dil, Jeff G., Jeffrey Mall, Jfdwolff, Jguard18, Jidanni, Jiggley puff, Jikepaddy, JimVC3, Jimbob136925,
Jimmysauce, Jj137, Jjthunder, Jmlk17, John, John Hay, John254, JohnCD, Johner, Jojhutton, Jojotheindian, Jonathan2400, Jonemerson, Josef12290, JoshuaZ, Jpers36, Jslayton34, Julesd,
Juliancolton, June12, Juniebugg2000, Jusdafax, Just plain Bill, Justpassin, Jxl180, K2turbervill, KGV, KGasso, KVDP, Ka Faraq Gatri, Kaaphi, Kablammo, Kafka Liz, Kartano, Kasjanek21,
Katalaveno, Katieh5584, Kaylawormack1993, Keegscee, Keenan Pepper, Keke101092, Kennedybrankin, KerrySims, Khullah, Kickbutluke, Killer213, KillerChihuahua, Kimo p, KingGusII,
Kingmidasband, Kingpin13, Kitty2cute6546, Kiwi128, Kjane214, Kmao10987654321, KnowledgeOfSelf, Korg, Kotjze, Kukini, Kurt Shaped Box, Kurykh, L Kensington, L.tak, LOL,
Ladygaga020, LairepoNite, Lamro, Landon1980, Lankiveil, LasticMan, Lateg, Laurawrr, Laurencanbatterboys, Lawrence Cohen, Laxboy764, Lazulilasher, Lcarsdata, LeaveSleaves, Lectonar,
LeeLeepooleaver, Leeb603, Leenewton, Legge1996, Legion fi, Leszek Jaczuk, Liam22, Life of Riley, Lightmouse, Lil.ninja.ladd, Lithorien, Logan, Longhair, Loopylizard333, Lotje,
Louissanchez, Lova Falk, Lovevoltage, LovleyPeople, Lrusso99, Lsu131, Luk, Lukobe, Luna Santin, Lurlock, MBisanz, MER-C, MPerel, Maayan1111, Mad Pierrot, Magic Cannibal,
Makeemlighter, Mandarax, Manticore, Manufracture, Manutdlost3-0tofulham, Manytexts, Marek69, Martin451, Marvinmillsjr, Masterchefsp, Mat8989, Materialscientist, Matt.T,
MattTheGreat13, Matthewcgirling, Matthewrbowker, MattieTK, Matty456789, Maxis ftw, Mbc362, McSly, Mcflie, Mchughc1233, Mcstrother, Mdwyer, Meaghan, Meeples, Merovingian,
Metropolitan90, Michael 26, Michaelsbll, Mikael Hggstrm, Mike Rosoft, Millermk, Millionsandbillions, Miquonranger03, Mlpearc, Mmxx, Mogism, Mojo Hand, Mono, Monty845,
Moosemichael, Moshe Constantine Hassan Al-Silverburg, Movingboxes, MrDurham, Msuspartans1855, MuZemike, Muchness, Mushroom, Musouwine, Mutterfutter111, Mygerardromance,
N2e, N419BH, NHRHS2010, Nabokov, Nageeb, Nagy, Narob, Narutolovehinata5, Nathanielboy, NawlinWiki, NealIRC, Nedron12, Neelix, NellieBly, Neo139, NerdyScienceDude, Nesodak,
Newportm, Newt Winkler, Nibuod, Nick C, Nick123, Nick252, Nidhis1234, Nifky?, NigelR, Nishkid64, Norm mit, Noroom9, Northumbrian, NotAnonymous0, Nsaa, Numbahh9, Number one
maximum ride fan, Nutsnfruge, Obsidian Soul, Oda Mari, Official Newscast Today, Ofjudinmh, Ohnoitsjamie, OlavN, Old Moonraker, Oliver202, Om my gosh, Omicronpersei8, Omnibus,
Onthegogo, Opelio, Oreo Priest, Ormomack, Otisjimmy1, OverlordQ, Paddongle, ParisianBlade, Paste, Patris Magnus, Patstuart, Paul-Kirkland, Pax85, Pbmaise, Pdcook, Pdogg98, Pepetehpepe,
Peridon, Persian Poet Gal, Peruvianllama, Peter Deer, PeterEastern, PeterSymonds, Ph.d Carl edenburgh, Pharaoh of the Wizards, Philip Trueman, Philipp670, Piano non troppo, Pinethicket,
Pinkadelica, Pinkkeith, Piss4eva, PokemonFan102, Pol098, Polik4, Pololokouni, Polylerus, Pooponmyface, Pooponmyhand, Poopstainers, Possum, Postdlf, Postlewaight, Pouletic,
Princessstrawberry, Prioryman, Professor Ninja, Ptaorumcyh92, Puffin, PullUpYourSocks, Pwner0 0, Pyfan, Qrc2006, Quail123, Quercus solaris, Quicksand10, Quintote, Qwyrxian,
ROBert4512xXx, RTG, RYBOUL, Ralmin, RandomXYZb, Raphite, RaseaC, Raven in Orbit, Raven4x4x, Rcsprinter123, Reach Out to the Truth, RealGrouchy, Reaper Eternal, ReconTanto,
Reconsider the static, Red King, Redroxtoo, Redsxfenway, Reguiieee, RenamedUser01302013, Res2216firestar, RetiredWikipedian789, RexNL, Rigurat, Riodelpiss, Riventree, Rjwilmsi,
Rmhermen, Rmosler2100, Rnb, Robma, Rod57, Roleplayer, Romit3, Ron Ritzman, Ronhjones, Ronmore, Rrburke, Rror, Runningsquid, Ryan032, Ryan1114, S Marshall, S h i v a (Visnu), SD5,
SDS, SMC, SV Resolution, Sahuagin, Saibhaskar, Sakkura, Saladin.zero, Salander86, Samclarke9, Samd thomas, Samtheboy, Sanjeev.singh3, Sapanza, Saros136, Saturn star, Saturn-78,
Sc0ttkclark, Scarian, Scetoaux, SchfiftyThree, SchmuckyTheCat, Scorpian ad, ScottSteiner, Scottalter, Scoutersig, Sean7777, Seanwilliams98, Seany577, Seaphoto, Selena1234, Senator
Palpatine, SenorSprinkles, Seraphimblade, Setanimalammit, Shablog, Shadowjams, Shahzeb1119, Shandris, Sheogorath, Shinpah1, Shirik, Shmally101, Shpoon, Shureg, Sirpinesol, Slakr,
SlamDiego, Slashr20, Slon02, SluggoOne, Smaug123, Smithr01, Smokefoot, Smokizzy, Smshbrosfreak247, Snan, Snigbrook, Snow Blizzard, Snowolf, Snowolfd4, SoCalSuperEagle, Soap,
Some jerk on the Internet, Sonic3KMaster, SpaceFlight89, Sparkmonkey7, SparsityProblem, Sparta300xps, Spartansrock74, SpeedyGonsales, Spellmaster, Spider1357, Spilla, Srose, Sslurth,
Sstteevvee, St34m1ng, StaceyAngelastro, StaticGull, Stephenb, SteveBaker, StevenhawkingsII, Stevey7788, Stickee, StickyWikiRicky, Strageworld, Sturm br, Stwalkerster, Suffusion of Yellow,
Sunkissed435, Supakill1328, Super-Magician, SuperHamster, Supermanpop3, Superruss, Sven Manguard, Swainstonation, Swimmingchicken, Symane, Synchronism, Synergism,
THEDOMINATOR 2340, THEN WHO WAS PHONE?, Tainted Drifter, Tanthalas39, Tbhotch, Tcncv, Tdkenny19, Teabagger101, Techman224, Tempodivalse, Tercero, Terdsarefat, Terence,
TerriersFan, TexasAndroid, ThatOneAsianKid, The Anome, The Grevonator, The Lucky Puppy, The Obento Musubi, The Thing That Should Not Be, The Universe Is Cool, The grim sniper,
TheBigZzz, TheFarix, TheOldJacobite, Thebagman, Theboogog, Theboss48506, Theda, Thedjatclubrock, Themightyhawk, Therealmen, Theresa knott, Thingg, Thistheman, Thrindel, Tiddly
Tom, Tide rolls, Tiger Khan, Tigerray2000, TimVickers, Timavegas, Timmytheuser, Timrem, Tins128, Tofutwitch11, Tom harrison, Tommy2010, Tommyjoewood, Tony1711123, Tortoisex,
Toryt0821, Totz mcgoof, Trangor, Trevor MacInnis, Tribe16, Triona, Trusilver, Tstormcandy, Tterrag, TucsonDavid, TutterMouse, Twat13, Twipley, TylerDurden8823, Tyw7, Tzheriki,
Uchihasharingan, Uhessler99, Una Smith, Uncle Dick, Uncle Milty, Undead warrior, Unschool, Unused0030, Us.marrines, Useight, Usuckeggs, Ute in DC, VMS Mosaic, Valley2city, Vancouver
Outlaw, VandalCruncher, Vanished User 1004, Vanished user 342562, Vanished user uih38riiw4hjlsd, Varaaki, VasilievVV, Vector Potential, Vegetarianbchris419, Venu62, Versus22, Vianello,
Vionau, Virus326, Von Jellyberg, Vranak, Vssun, WJBscribe, WLU, WWGB, WadeSimMiser, Wayne Slam, Wdaloz, Wespanol, West4949, Whayward4, Where, Whipped E Dog, Whispering,
White Shadows, Whouk, WhyBeFeet, Wicker1, WikHead, Wiki alf, WikiMazter, Wikiale, Wikidudeman, Wikipelli, Wikiuser100, Will789456123, William Avery, Willking1979, Wily wonka,
Winchelsea, Wine Guy, Wingo, Wissahickon, Wknight94, WookieInHeat, Wootness24, X1987x, XJaM, XP1, Xeltopius, Xeno, Xxbtrxx, Ybbor, Yellowpoostain, Yescomeon, Yidisheryid,
Ynhockey, Yournameheresugar, ZX81, Zaneselvans, Zealander, Zilklol, Zionandbabylon, Zoth12, ZR, uman, , 1697 anonymous edits
Clearance (medicine) Source: https://en.wikipedia.org/w/index.php?oldid=583461214 Contributors: Ark25, Chaldor, Countincr, DS Belgium, Edwin, EnabledDanger, Heracles31, Irene U,
JerroldPease-Atlanta, Jmlk17, Khazar2, Krash, Madhero88, Mikael Hggstrm, Nephron, Nick Number, Pinethicket, Quercus solaris, Radiojon, Rcsprinter123, Sfahey, Superoxiddismutasa,
Vldscore, 18 anonymous edits
Blood pressure Source: https://en.wikipedia.org/w/index.php?oldid=584020692 Contributors: 28421u2232nfenfcenc, 4wajzkd02, 5-HT8, 5Q5, A8UDI, Abdmy011, Abeg92, Abrech,
Aceofhearts1968, Adam Zivner, Addshore, Adh30, Adville, Aitias, Ajh16, Ale jrb, Alex.tan, Alexius08, Algumacoisaqq, Ali, Amoooorlin, Anaselshamy, Andre Engels, AndrewHowse,
AndrewWTaylor, Anfieldroad, Angus Lepper, Anim8cme, Ann Stouter, Anna Lincoln, Anthonyhcole, Antonio Lopez, Arakunem, Arcadian, Arch dude, ArielGenesis, Arjayay, Arjun01,
Ashishbhatnagar72, Ashraf khan99, Assume5, AugPi, Avi8tor, AxelBoldt, B. Wolterding, BOMBINI, Barek, Bear and Dragon, Beetstra, Bemoeial, Bencherlite, Bensaccount, Bensin, Bfesser,
Bffsrliars, BigNate37, BillC, Biyer, Bjkeefe, BlaiseFEgan, Blood Pressure Association Publications Officer, Blue Tie, Bob K31416, BobKawanaka, Bobo192, Bollyjeff, Bongwarrior,
Brainmachine, Braksb, Brandon, Brendan Moody, Brighterorange, BruceBlaus, Bubba hotep, Buchskj, Burlywood, Butwhatdoiknow, Byeitical, Bcherwrmlein, CIreland, CMBJ, CWenger,
Calabe1992, Can't sleep, clown will eat me, Canihaveacookie, CanuckViking, CapitalR, Carlydan, Carmichael, Cburnett, Ccacsmss, Celarnor, Chafe66, Chamal N, Charles Gaudette, Chowbok,
Chuckmoran7, Ckdsiteckd, CliffC, Closedmouth, CoJaBo, Colenso, Cometstyles, CopperSquare, Correogsk, Crystallina, Csdorman, Cst17, DBigXray, DFS454, DMacks, DRosenbach, DVD R
W, Dan Gluck, DanConnolly, Daniel.Cardenas, Dank, Darth Panda, David Henderson, DavidSmith8888, Davidoff, Davidruben, DeadEyeArrow, DeathHamster, Defender of torch, Deli nk,
Delldot, Deor, DerHexer, Diberri, Difu Wu, Dionysia, Djgregory, Djk3, Dlohcierekim, Docu, Dog Eat Dog World, Dominus, Doops, Dovid, Dr Bilal Alshareef, DrMacrophage, DragonLord,
Dreamyshade, Dwinner, E Wing, E rulez, Eastchester, Edgar181, Eekerz, EhJJ, Eiler7, Ekko, ElKevbo, Eleassar, Eliazar, Emote, Emperorbma, Enigma55, Epbr123, Eric-Wester, Erik9, Fabrcio
Kury, Facts707, Falcon8765, Faradayplank, Fenggegecn, FisherQueen, Flewis, FlyingToaster, Fnielsen, Founders4, Fraggle81, Frap, Fredrik, Freestyle-69, FreplySpang, Frietjes, Frmatt,
Fulkkari, Fyrael, G0dsweed, Gabbe, Gary King, Gene Nygaard, GermanX, Giftlite, Gilliam, Ginsuloft, Gizz, Glacialfox, Gogo Dodo, GoingBatty, GordonMarjory, GorillaWarfare, Gro-Tsen,
Grubber, HMSSolent, HTGuru, Hadal, Haham hanuka, HappyInGeneral, Harej, Healy24, Heimoma, Heron, Hiberniantears, Holdspa, Hooperbloob, HorsePunchKid, Housecarl, Hu12, Hut 8.5,
IW.HG, Icairns, Ice Cold Beer, Iggydawn, Iridescent, Isidore, Ixfd64, J Di, J.delanoy, J04n, JForget, JHP, Jack-A-Roe, Jackhynes, Jacqui M, James086, JamesAM, Jared Hunt, Jasonkodat,
Jecowa, Jeff Silvers, Jeffq, Jeremygbyrne, Jfdwolff, Jim1138, JimmyAndRobert!, Jimp, Jjron, Jkgray, Jmarchn, Jmh649, Jmor7, John Kaduwanema, John of Reading, JohnCub, Johnduffell,
Jojhutton, Jonathunder, Jonny-mt, Jorvik, Josep sola, Joyous!, Jprey, JuliaHavey, JulieADriver, Julo, Just plain Bill, Justinstroud, Kansas Sam, Karlhahn, Kartano, Kelliel@iinet.net.au, Keron
Cyst, Kevino62, Kilbosh, King of Hearts, Kitty bean, Klausness, Knowledge Seeker, Kosebamse, Ksheka, Kukini, Kuyabribri, Kwiki, Kylet, Kyoko, LAX, Lactotripeptide, Lalchand91,
Larrymcp, LeadSongDog, Lear's Fool, LeaveSleaves, Lenitudent, Lexicontra, Lheydon, LilHelpa, LimpThis, LittleDan, Lkinkade, Lmuenchen, LordRae, Losmog, Luk, Lupinoid,
M1ss1ontomars2k4, MAlvis, MER-C, MONGO, Macaddct1984, Maderchoud334, Maderchoudsala44, Madhero88, Magioladitis, Mansoornbangash, Marek69, MarkSutton, Martin451, Master
Jay, Masterchiefthespartan117, Matt povey, Mattaidepikiw, Me, MeVsAll, Mentifisto, Merube 89, Mesoderm, Mfranck, Michael V Hayes, Mig174, Mikael Hggstrm, Mike Magowan, Mike
Rosoft, Minimac, Miranda, Miyagawa, Mjharrison, Moe Epsilon, Mootros, Morning277, Mortense, Mr Goulash, MrOllie, Mrdocjb, Mtynerod, Muchclag, Muszek, Myadav, Mzcrazybitch, N-k,
Naniwako, Nastajus, Natkeeran, Nehrams2020, Neptune5000, Nfu-peng, Nick C, Nicnic m, Nikzbitz, Nmg20, Notepadpage, Nutcrakerr, Ocdcntx, Oguk, Ohnoitsjamie, Okedem, Olorin28,
Orangedwarf, OrgasGirl, Osbus, Oshwah, Oxymoron83, PEBill, PRONIZ, Paiamshadi, Pandaassassin7, Patrick, PatronSaintOfEntropy, Peruvianllama, PeteThePill, Pgan002, Phansen, Phgao,
Phil Wardle, Philip Trueman, Piano non troppo, Pilarian, Pinethicket, Piplicus, Pol098, Polacrilex, Postmeta, Pratyya Ghosh, PreThinker, Prodego, ProfBondi, Pseudomonas, Puffball, Puffin,
Quaint and curious, Quercus solaris, Qwyrxian, RDBrown, RNchoo, Rajah, Rdsmith4, Red Act, Remi0o, Renato Caniatti, Res2216firestar, RexNL, Rich Farmbrough, Rishigupta02445, Rjwilmsi,
Rob Hooft, Robert P. O'Shea, Roberta F., Rojypala, Romanm, Ronz, RoyBoy, Rsduhamel, Ryancormack, Ryguasu, SJP, SMC, Sampi, Sango123, Scarian, Scohoust, Sean.hoyland, Selket,
Septine, Seuwin, Shanes, Shawn in Montreal, Sho Uemura, Silvrous, Sinkker, Sixtythirdy, Sjakkalle, Skarebo, Skizzik, Sljaxon, Snowmanradio, Someone else, Sonett72, Spiff666, Spongefrog,
SportWagon, SqueakBox, Srich32977, SstrykerR, Stack, Statkit1, Stephen, Steve2011, Steven Zhang, Stevenfruitsmaak, Strasburger, Supten, Surturz, Svadhisthana, TSoprano, Tarquin,
TastyPoutine, Tefomaste, Tempodivalse, Tentinator, Terrytibbs1983, TexasAndroid, Tgeairn, The Rambling Man, The Thing That Should Not Be, TheEgyptian, TheNewPhobia, Thickycat,
Thomas Blomberg, Thumperward, Tide rolls, TigerShark, Tkessler, Todd Vierling, Tom Morris, Tom Yates, TonyHagale, Toreau, Tpaba, Tpbradbury, Traw187, Traxs7, Tresiden, Troop350,
TruthIsStrangerThanFiction, Tsujigiri, UISKuwait, Uknowme imbehindu, Ulric1313, Uncle Bill, Unused0029, Uploadvirus, User38934, Uthbrian, Utopianheaven, V.narsikar, Van helsing,
Vanished user 39948282, Vary, VasilievVV, Vgviz1001, WDM27, WadeSimMiser, Waimate01, Wap, Wavelength, Wayunga, Wayward, Weeksgo, Westendgirl, WhatamIdoing, Wikipelli,
Wikiperson0202, Will Beback Auto, Wimt, Wisdom89, Woohookitty, Wouterstomp, Wraithdart, Wtshymanski, Wyferltd, Xlegiofalco, Xris0, Yidisheryid, Yintan, Ymaziar, Yobol, Yoweigh,
Yuanchosaan, Zephalis, Zuff, Zureks, Zzuuzz, , 1291 anonymous edits
Erythropoietin Source: https://en.wikipedia.org/w/index.php?oldid=582793507 Contributors: Alex.tan, Alteripse, Andrew Su, Angela, Anir1uph, Anrnusna, Anthonymhowarth, Anypodetos,
Arcadian, Arcenciel, Asamudra, Asthapawar, Badgettrg, Bejnar, Bemoeial, Bender235, Beyond My Ken, Bignoter, Bikeroo, BillpSea, BitQuirky, Blainster, Bluemoose, Boghog, Caliper, Can't
sleep, clown will eat me, Captain-n00dle, Captainandrewwiggins, Charlie1995aza89r, ChillyMD, Chirlu, Chowbok, Chris Roy, Chris the speller, Christian75, Chrysaor, Ciar, Clementine2009,
201
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Article Sources and Contributors
Ctu2485, DGG, Dahoss, Dale Arnett, David D., David Santucci, David.Monniaux, Davidlwinkler, Decora, Deflective, Dekimasu, Delldot, Demantos, Dhara75, Dickandharry, Dinarabaggy,
Doelleri, Dominantprefix, Dr.michael.benjamin, DrComplement, DrGabriela, Drbobvan, Drphilharmonic, Duncan.france, Duncharris, E A S, EVula, Edcolins, Egil, Einstein9073, Eklir, Elb2000,
Ellis2ca, Equendil, Ericoides, Eug, Everything Is Numbers, Exercisephys, Facts707, Gak, Gareth Owen, Gene Nygaard, Gigemag76, Glotris173, Ground Zero, Habj, HaeB, Happily ever after,
Hdt83, Hede2000, HenkvD, HighIntellectual, Hu12, ImperfectlyInformed, J.delanoy, Jackhammer111, Jackson Peebles, Jfdwolff, Job314, John R Rodgers, John Reaves, Julesd, KTo288,
Kaiserkarl13, Katnap01, Kitkat21, Knowledge keen, Kpjas, Ktrenskow, Kwamikagami, L.tak, L509alumni, Lambiam, Law, Leafyplant, Leemorrison, Lensi, Lkinkade, Lurker27, Lvangundy,
MBisanz, MEDICCGR, MER-C, Macdorman, Mahendern, Marycontrary, Materialscientist, Matt Gies, Medstudent29, Meewam, Mellery, Meodipt, Michael Devore, Mikael Hggstrm,
Monkeyontheloose, Montgomery '39, MrOllie, MrTroy, MuZemike, NawlinWiki, Nbauman, Nephron, Nexus 215, Nyttend, Nyxos, Ocean57, Ost316, Paiamshadi, PaoloNapolitano, Patentpedant,
Patrick-br, Peoplesunionpro, Philip Trueman, Philosopheratrest, Pne, Portillo, Pramanick, Quonston, Qwfp, RDBrown, Rcgy, Remedios44, Rewguy, Rich Farmbrough, Richard Arthur Norton
(1958- ), RidinHood25, Riffle, Rjwilmsi, Rknrobin, Roboo.jack, S&W Sciences, SMC, Sballal, Scottalter, SeanMack, Serenity forest, Sk741, Slashme, Sliu2013, Smithbrenon, Some standardized
rigour, Spaully, Spouima, Squids and Chips, StuffOfInterest, Sushbiotech, Svick, Tbuzz, Techelf, The Illusive Man, TheAMmollusc, Thirureddy, ThujaSol, Tide rolls, Timwhit, Tooto,
Topnaman, Tpbradbury, Trekphiler, Tristanb, Unsweet Tea, VKemyss, Vanished user kijsdion3i4jf, VetPsychWars, Wavelength, Wayland, Wernher, Windwardside, Wingman4l7, Wiwaxia,
Wmahan, Wolfgang Jelkmann, Woohookitty, Xmp, Xurei, Yeast2Hybrid, Young Pioneer, Zack wadghiri, ZayZayEM, Zeamays, Zoe, , , 369 anonymous edits
Calcium metabolism Source: https://en.wikipedia.org/w/index.php?oldid=582717366 Contributors: Allmightyduck, Apollo1758, Arcadian, Ark7, Arripay, Bensaccount, BrightStarSky, Brim,
Bryan Derksen, Corpet, Drcarlos, Dreadstar, Eleassar777, Generic Player, Gildindaimoth, Gobonobo, Headbomb, IONTRANSP, Inferior Olive, Jasonasosa, Jfdwolff, Jimw338, Jonathan.viney,
K.nirujan, Lir, LittleHow, MIRROR, Materialscientist, Mikael Hggstrm, Mike2vil, Moez, MooresLaw, Nen, Ntsimp, Nutriveg, ObjectivismLover, Pinethicket, R'n'B, RDBrown, RJFJR,
Rhombus, Riley Huntley, Rjwilmsi, RoyBoy, Sam Hocevar, Snowolf, Sturders, Theolatic, Thine Antique Pen, Ururu, WQUlrich, WatchAndObserve, Westin, Zmandel, 82 anonymous edits
Fluid balance Source: https://en.wikipedia.org/w/index.php?oldid=579961553 Contributors: Aeluwas, Andyzweb, Arcadian, Braeden.peters, Brandmeister (old), Cmdrjameson, Daughter of
Mmir, Donner60, Dwrmal, Epolk, Erudecorp, Eubulides, Fishystick, Frozenevolution, Glane23, Hoverflysmiles, Jim1138, John Broughton, Ketiltrout, LizardJr8, MacStep, Methecooldude,
Mikael Hggstrm, Morning277, Mrt3366, Naniwako, Pearle, RN for life, Rjwilmsi, Skapur, Skier Dude, Steveprutz, Vanished user uih38riiw4hjlsd, Wyvyrn, Zalery, 54 , anonymous edits
Vasopressin Source: https://en.wikipedia.org/w/index.php?oldid=582978913 Contributors: A314268, A3camero, AaronM, Abtinb, Adolphie, AlbertHall, Alex.tan, Alousybum, Als022,
Amovrvs, Andrux, Antelan, Arcadian, Armando Navarro, Artur Lion, Aude, AxelBoldt, Axl, Aytrus, Backwardtoes, Bensaccount, Blackmarketpenguin, Bobo192, Boghog, Bomac, BorisTM,
Bowman, Bwrs, CDN99, Caltas, Caseyisahobo69, Cezarika1, Chaldor, Chemgirl131, Chris the speller, Chymra, Csobankai Aladar, DRosenbach, Dab2108, Darth Panda, Dcirovic, Denis
tarasov, DerHexer, Dhatfield, Diberri, Drphilharmonic, Edgar181, EerieNight, EhJJ, Electric goat, EmlivOlcano, EmmetCaulfield, Epingchris, Eug, Expergefactionist, Fantumphool, Feral mage,
Flyer22, Forluvoft, FrozenMan, Fvasconcellos, Geetarmainiac, GermanX, Giftlite, Gleng, Guillaume2303, Gurch, Harriv, Hattaway, Hodja Nasreddin, I9606, IO Device, IONTRANSP, Inferior
Olive, Inoculatedcities, Invalidsyntax, InverseHypercube, JForget, JakobSteenberg, James McNally, Javierstroud, JesseAlanGordon, Jfdwolff, Jmoneydizzle, Joel7687, John, John.mapleview,
Jonathan.s.kt, Juliecarver, Katoa, Kelson, Kilo-Lima, Krylonblue83, Lepidoptera, M1ss1ontomars2k4, MPerel, Magioladitis, ManiF, Mark Knepper, Matdaddy, MauriceTrainer, Mav,
Mboverload, Medevo, Medicineman84, Mikael Hggstrm, Mike2vil, Mimihitam, Minnsurfur2, Misskidney, Mthteh, Nagy, Nathan Johnson, Netopoa, Nishkid64, Nyq, Odoketa, Olegkolesnikov,
Osm agha, Philip Trueman, Pit, Pranks16, Prayingmantis78, Puckly, RDBrown, RadicalHarmony, Raghuram.chimata, Rich Farmbrough, Rjwilmsi, RyanGerbil10, SPhotographer, Sammyj,
Sgtpepper66, Shrimppesto, Slimjimno1, Someone else, Spaully, Stepanka, Stismail, Tameeria, Tavilis, Tbhotch, Techfiend, Tgilhou, The Determinator, The Legendary Douglas Butcher,
Theodore Kloba, Tide rolls, Tony Mach, Tpjv86b, Uncle G, Vanv2642, Vogelbacherr, Vokesk, Wavelength, Wiki.saeid, WordyGirl90, Xris0, Zain Arshad, dipus sic, , , 263
anonymous edits
Aldosterone Source: https://en.wikipedia.org/w/index.php?oldid=576647686 Contributors: A3camero, AdoreMila, Adun12, Alansohn, Altenmann, Ambience3, Andre Engels, Animeronin,
Antandrus, Anthonyhcole, Anypodetos, Arcadian, Arctic Kangaroo, Arripay, AxelBoldt, Beetstra, Benjah-bmm27, Benlisquare, Bensaccount, Bignoter, Bobo192, Bogwhistle, Brianf711, Bryan
Derksen, Bsehn, Bubbachuck, Cab.jones, Cajolingwilhelm, Chem-awb, Chemgirl131, Chris the speller, Chrisgj, Codsears, CopperKettle, Courcelles, Csmith0434, Dan100, DancingMan,
Dcirovic, DemonicPartyHat, DerBorg, Diberri, Dr Bilal Alshareef, Drbreznjev, Drphilharmonic, Edgar181, Eleassar777, Emperorbma, Epipelagic, Epop fr, Eshywiki, Facts707, Faldizzle,
Frehley, FrozenMan, Fvasconcellos, Giftlite, Gregnz, H12321, Hamsterlopithecus, HansThane, Hede2000, Herizora, Isoptera, Jabronimus, Jepoirrier, Jeremy112233, Jfdwolff, Jonesey95, Karsten
Adam, KnightRider, Ksheka, KugelaP, Lanternix, Leyo, Ling.Nut, Louisajb, Luckydhaliwal, MER-C, Mac, Mbc362, Meclee, Michael Devore, Mikael Hggstrm, Mike2vil, Mowtown philippe,
Mr Bound, N5iln, Nbauman, Nono64, OlaIsacsson, Orenburg1, Orlandoturner, Pashihiko, Peter morrell, Petersam, Philip Trueman, Physchim62, Princessamoeba, RDBrown, Razol2, Rich
Farmbrough, Rich257, Rjwilmsi, Rob Hurt, SS1981, Sarindam7, Settersr, Shaddack, Shakiestone, SoCal, Spaully, Spencer, Spuntyb, Ssschhh, Stewartadcock, Thatfeel, The wub, Theda, Tpjv86b,
Triviaa, UberMD, Ugen64, Unschool, Uthbrian, Vedran12, WhatamIdoing, Whcernan, Wimt, Woochiao, Wood Thrush, Xerophon, Yelyos, , , 184 anonymous edits
Countercurrent multiplication Source: https://en.wikipedia.org/w/index.php?oldid=576217290 Contributors: Amalas, Andersat, Anomalocaris, BradBeattie, Camrn86, Capit, Chibibrain,
David Eppstein, Desmond Tsui, Dilane, ErrantX, Ethan Mitchell, Folajimi, Insanity Incarnate, InverseHypercube, J04n, Jeepday, Jrtayloriv, Mandarax, Nagle, Pashute, Retired username, Rich
Farmbrough, Woohookitty, 30 anonymous edits
Osmoregulation Source: https://en.wikipedia.org/w/index.php?oldid=580785496 Contributors: A8UDI, Aaron Brenneman, Akababa, Akrukowski, Amkilpatrick, Anticipation of a New Lover's
Arrival, The, AqibAqeel259, ArchStanton69, Arthena, BD2412, Bluerasberry, Butros, Can't sleep, clown will eat me, CatPath, Chris the speller, Christian75, Communisthamster, DARTH
SIDIOUS 2, Daughter of Mmir, Dawn Bard, Diannaa, Drahkrub, Drphilharmonic, E Wing, Earthdirt, Easchiff, Emw, EncycloPetey, Fascinoma, Fish and karate, Forschung, Gilderien, Grafen,
Hemanshu, Hemmer, Hopetocome, It Is Me Here, J.delanoy, Jaberwocky6669, Jacj, Jesse V., JodyB, Junkyardprince, Just69me, Khvalamde, KittyKat, Kkmurray, Kookookook, Lan360, Lexor,
Luna Santin, MagnInd, ManyueGPH, Master of Puppets, Mifter, Mikael Hggstrm, Mustangs125, Naniwako, Nick Number, Novangelis, Objectivesea, Ockrn, PaddyM, Pinethicket, Pinkadelica,
Rafaledeguerre, Razaawais141, Secretlondon, Smartse, Snigbrook, Spindocter123, Steel, Steveprutz, StuRat, Thane, Thesuzerain, Thunsaker, Timmeh, Vbhubeny, Vicpeters, Widr, Wik, William
Avery, Woohookitty, Xizengm, Yk Yk Yk, 129 anonymous edits
Loop of Henle Source: https://en.wikipedia.org/w/index.php?oldid=577953533 Contributors: AC+79 3888, Alex.tan, Antedon, Arcadian, Auric, Axl, Beeswaxcandle, David.Monniaux,
Devilsjumper, Diberri, Easyer, Eleven even, Eras-mus, F.chiodo, Flyguy649, Fuzheado, Giftlite, HELvet, Haakon K, Hemsleydale, JakobSteenberg, Jared999, Jfdwolff, Jfmantis, Jhinman, Jim
Douglas, Jmarchn, Jrtayloriv, Kiousu, Luckydhaliwal, Makeemlighter, Mcstrother, Merideth, Mgp28, Mikesta178, Mithrandirthewise, Mj455972007, Moniem musa, MrArifnajafov, NeilN, Nlu,
Nn123645, Omar35880, PamD, Pashute, Pwash01, Quintin1992, Rdub8, Rjwilmsi, Rsc227, SFK2, Sahehco, Scottalter, SimonPerera, Sonnejw0, Spaully, Stepa, TimVickers, Tiptoety, Uncle
Dick, Waggers, 104 anonymous edits
Water-electrolyte imbalance Source: https://en.wikipedia.org/w/index.php?oldid=561481160 Contributors: AThing, Arcadian, Arunsingh16, Cacycle, CanisRufus, Chris83, Davidruben,
Diberri, Dylan Lake, Eequor, Eewild, Erich gasboy, Everynewmorning, Fethroesforia, FirstPrinciples, Fyrael, Gail, GermanX, Infamous Castle, Jfdwolff, Julia W, Karsten Adam, Keenan Pepper,
Lexor, Lsd123, Magioladitis, Philip Trueman, Pinethicket, Rcej, Skier Dude, Stevertigo, Tabletop, Technopilgrim, The Anome, Truffle200, Vedran12, Wouterstomp, 42 anonymous edits
Hyponatremia Source: https://en.wikipedia.org/w/index.php?oldid=582409014 Contributors: A2Kafir, ACEOREVIVED, AManWithNoPlan, Alex, Alvis, Andrew Benton, Andrewman327,
Andypandy.UK, Angelito7, Anrnusna, AntiVan, Apollo1758, Arcadian, Arripay, Ashleyleia, Athomeonarock, Axl, Ben Ben, Bigsnake 19, Bork, Bryantilton, Burhan Ahmed, Buxtor, Chris
Capoccia, ChrisGualtieri, Ckujau, Clementdiabetesdoc, Cowabunga5587, Cybergoth, Cypher Aod, DJ Craig, Daniel Case, Danielil, Denisarona, Dieter Simon, Diptanshu.D, Docu,
Drphilharmonic, Eequor, Elkman, Emloo, Erich gasboy, Esprit15d, F Notebook, FirstPrinciples, FlynnUK, Fubar Obfusco, Funandtrvl, Fursday, Gabbe, Gaussgauss, GeorgeN512, Ghakko,
Grayshi, Guillaume2303, HDCase, Hadal, Haitchnash, Happy B., Hayne, Hnsn, Hojasmuertas, Hydrargyrum, IveGoneAway, J.delanoy, James Bedford, James pic, Jan Pospil, Jcs2b, Jfdwolff,
JimVC3, Jmh649, Jon the id, Jonesey95, Julia W, Jylothr, Kfogel, Kibbitzer, Kilcoyne, Last Lost, Lindsay.falvey, Logan, Luci Sandor, Lumberguy1028, Mace, Mandarax, Markewilliams,
Mdriver1981, Mfagan, Mikael Hggstrm, Mike hayes, Mild Bill Hiccup, Monkeyget, Nick Number, Nmg20, Novangelis, Nunh-huh, Nunquam Dormio, Ocdnctx, Per Olofsson, Phatom87, Plrk,
Prabhujoseph, Puchiko, RDBrown, Radiant chains, Rcej, Rhcastilhos, Rhombus, Rich Farmbrough, Richiez, Rjwilmsi, RodC, Rsg, SFK2, Sardmeta1, Sghayes, Sgpsaros, Shawn in Montreal,
Shrimppesto, Skier Dude, Slyjackalope, Smartse, Smooth O, Some standardized rigour, Ssetd, Stannered, Staszek Lem, Stevenfruitsmaak, Sweikart, Technopilgrim, The Determinator, The1anton,
Thealliedhacker, Tooki, Treshnell, Truth's Advocate, Tyciol, TylerDurden8823, User27091, Vedran12, Vincentmsf, Wikiuser100, Wouterstomp, Yugyug, 230 , anonymous edits
Hypernatremia Source: https://en.wikipedia.org/w/index.php?oldid=584188666 Contributors: Allen3, Angelito7, Arcadian, Ariel., Arripay, Bdiscoe, Bo hessin, Cactus.man, Cburnett,
Chillinvillain, Cybergoth, DR.R.MAR, Danielil, Driftwoodzebulin, Eequor, FirstPrinciples, GDallimore, GermanX, Happy B., HarishV, Jarble, Jmh649, Kyng, LeaveSleaves, Leevclarke,
Marknagel, MastCell, Master of Puppets, Phayla, Rcej, RickK2, Sardmeta1, Sasquatchmd, Skier Dude, Srays, Syedrali, Theindianreincarnated, TylerDurden8823, Vedran12, Wervi,
Wouterstomp, Zephalis, 45 anonymous edits
Acidbase homeostasis Source: https://en.wikipedia.org/w/index.php?oldid=565862035 Contributors: Alansohn, Arcadian, Ariel., Charlesdrakew, Cmcnicoll, Cst17, Daughter of Mmir,
Discospinster, Domsicj, Draeco, Drphilharmonic, Freekozak, Fulanokochman, F, Gorthian, GreysAnatomy, Huckfinne, Iaconome, InverseHypercube, Jason7825, Je.rrt, Jsfouche, KerryB,
Kostisl, Liam Skoda, Luke13579, Mikael Hggstrm, Moletrouser, NawlinWiki, Newport Backbay, Ossip Groth, Petergans, Plutix, RDBrown, Rjwilmsi, Rm w a vu, Saintswithin, Sakkura,
Saludtotem, Scottalter, Scray, Tomas e, Tomaxer, TylerDurden8823, Vinograd19, Zlir'a, 37 anonymous edits
Acidosis Source: https://en.wikipedia.org/w/index.php?oldid=567566035 Contributors: AaronM, AdjustShift, Alai, Angelito7, Anonymousphrase, Anthonyhcole, Arcadian, Ash, BadCannstatt,
Beland, Bensaccount, BigHairRef, Bluemask, Bubbawest, Chasingsol, Cpt ricard, Crystallina, DSRH, Dictabeard, DrMtl, Drphilharmonic, Edgar181, Eequor, Erich gasboy, EvgenyGenkin,
GTBacchus, Gaius Cornelius, Gene Nygaard, Gioto, Glane23, Gobonobo, Grondin, Gurch, Gustave G., Hede2000, HexaChord, Iridescent, Jason7825, Jfdwolff, Jsfouche, Karsten Adam,
Kauczuk, Khobler, Kmmalloyzz, Kunstgebit, Lamro, Magioladitis, MarcoTolo, MattKingston, Mikael Hggstrm, Mikez, Modify, Mr.Rocks, Mroseman4, NOchotny, Nephron, Nescio, Nmg20,
202
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Article Sources and Contributors
Nulzilla, Nuttycoconut, Papte, Pb30, Pdcook, Rapsar, Rcej, Rjwilmsi, RoyBoy, Salud pH, Saludtotem, Sanfranman59, SciberDoc, Scottalter, Secretlondon, SentientSystem, Shiney, Skier Dude,
SpuriousQ, Stillnotelf, Str1977, Tainter, Tannkrem, Taooo, Theakrillianlunchbox, Thefinalprophecy, Timo Honkasalo, Wood Thrush, ZayZayEM, , 92 anonymous edits
Alkalosis Source: https://en.wikipedia.org/w/index.php?oldid=577978517 Contributors: Alansohn, Alexf, Angelito7, Arcadian, Bensaccount, Bobblewik, Cacycle, CalJW, Careless hx, Cburnett,
ChrisGualtieri, Eequor, Erich gasboy, Falcon8765, GregorB, Hariva, Headbomb, Hschiong, JDspeeder1, JJIG, Jefdstahr, Jmarchn, Jsfouche, Karsten Adam, Lucien504, Mikael Hggstrm,
Minimac, Nathan.e.lee, Nulzilla, Physchim62, Poltergeist EN, Rcej, Rich Farmbrough, Rustavo, Saccharomyces, Scottalter, Secretlondon, SimonP, Skier Dude, Stemonitis, Tjc, Una Smith,
WaterCrane, WhatamIdoing, Widr, Wouterstomp, Zack wadghiri, 48 anonymous edits
Glomerulonephritis Source: https://en.wikipedia.org/w/index.php?oldid=584237228 Contributors: 2004-12-29T22:45Z, Adeliine, Ahoerstemeier, Americanluck, Andrew Benton,
Androuwaheeb, Angelito7, AnjaManix, Anteskalle, Anypodetos, Arcadian, Avono, Beetstra, Bogwhistle, CDN99, Cacycle, CambridgeBayWeather, Centenarian, Charles Matthews, Darklilac,
Dayoung000, Dcabrilo, Devahn58, Diberri, Diptanshu.D, Dmitrei, Dmoreira, Dominicanpapi82, Dr.robertg, Drsriku, Dryphi, GermanX, Goawayfast, Gszilins, Habj, Istillma, Jfdwolff, Jmarchn,
Joshmax, Jtdaugir, Kauczuk, Ketiltrout, Khazar2, KnightRider, Kunstgebit, LT910001, Lankiveil, LearnMed, Mark ong, Matthias.hilty, MauchoEagle, Mdanciu, Mendalus, Michaledwardmarks,
Mike2vil, Miracle Pen, MistyMorn, MusikAnimal, Mysdaao, Nabihovich, Neilymon, Niceguyedc, Nonagonal Spider, Papte, Peter Chastain, Phlegm Rooster, Qetuth, Reza luke, Rod57, Ryanaxp,
Sanya3, Sarindam7, Serrin, Snafje, Stevenfruitsmaak, Teammm, The Thing That Should Not Be, The1anton, Tide rolls, Tlabshier, Trabelsiismail, Triddle, Unckc, Vedran12, WCFrancis, Wine
Guy, Wouterstomp, 121 ,55 anonymous edits
Interstitial nephritis Source: https://en.wikipedia.org/w/index.php?oldid=580719874 Contributors: AnjaManix, Arcadian, Badgettrg, Cglenn1, Coinmanj, Gaff, Garmenkell, GermanX,
Huang588021, Hydro, Master Scott Hall, MrDarcy, NCurse, NawlinWiki, Obaid221, Parkwells, Ratel, Rjwilmsi, RobinHood70, Stephenwanjau, Thehelpfulone, Tomas e, 19 anonymous edits
Diabetic nephropathy Source: https://en.wikipedia.org/w/index.php?oldid=582371977 Contributors: (), Afaprof01, Allens, Alpheus, Angelito7, Arcadian, Axl, Baxter9, Breadified,
BrownHairedGirl, BruceBlaus, Chickenboner, Chris the speller, Cmichael, Coffee, CyberknightMK, Danielcrockett, Davidruben, Discospinster, Draeco, El33th4x0r, Faigl.ladislav, GermanX,
Gobonobo, Graham87, Grannos, GregorB, Headbomb, Jamesdpalmer, Jetman, Jfdwolff, Jmh649, Kazem.fa, Korg, Liaocyed, LinaNordquist, Loudsox, Mhmd-lallo, Nephron, Niels Olson,
Nihiltres, Nono64, Ntsimp, PaperTruths, PhiJ, Pmchitongco, Pranay2000, R. S. Shaw, RDBrown, Rhcastilhos, Riturajan1026, Rjwilmsi, Roberta F., Rsabbatini, Rsrikanth05, Scientest, Shahab
13, Skagedal, Swatjester, Tabletop, TheIrishWarden, 88 anonymous edits
Acute kidney injury Source: https://en.wikipedia.org/w/index.php?oldid=581153857 Contributors: 3!3X, Accurizer, Adashiel, Adnan saqib, Aeusoes1, Alex.tan, Alice Person, Andrew73,
Anrnusna, Anupam, Aqadir149, Arcadian, Asamau, Axl, Aymatth2, Babajobu, BillpSea, Binary TSO, Bobjgalindo, Broississy, Checkingfax, Cst17, Davidlwinkler, Davidruben, Dexter prog,
Diberri, Doug Bell, Dr farajov, Drphilharmonic, Ellusion, Felix-felix, Fleester, Gaff, Gaius Cornelius, Gene Nygaard, GermanX, Goodnightmush, Haymanj, Hswapnil, Huckfinne, Hydro,
InvictaHOG, JByrd, Jalan z, Jfdwolff, Jim1138, Jimw338, Jrew86, Karmosin, Ketiltrout, Kiwiski, Knuckles, Kolbasz, Kyoko, Madhero88, MarcoTolo, Matanya, McPat, McSly, Mike2vil,
Minkchawla, Mlaszlo, MrBell, Muad, MuanN, Nbauman, Nephron, Nescio, Neutrality, Opelio, Osm agha, PDH, Passion83, Petersam, Pinethicket, Pratap.sps, Qwyrxian, RDBrown, Razghandi,
Reatlas, RedWolf, Reynardo, Rich Farmbrough, Rjwilmsi, Rod57, Rsva, Russthomas1515, Saintcatherine77, Shinkolobwe, Stevenfruitsmaak, Suspasioso, Taxman, The Anome, The Thing That
Should Not Be, Thomasimov, ToNToNi, Tonytypoon, TylerDurden8823, Volney, W.D., Wcd480, Woohookitty, Wouterstomp, Wsiegmund, Yobol, Yoshm, 135 ,12 anonymous edits
Acute tubular necrosis Source: https://en.wikipedia.org/w/index.php?oldid=560868640 Contributors: A. Rad, Angelito7, Arcadian, ArturoJurezFlores, Beaware101, CanisRufus, Charles
Matthews, Chris Capoccia, Countincr, Diptanshu.D, Docmojo, Edward, Finlay McWalter, Fkhury, GabeIglesia, Gizmo.AT, Goodnightmush, Hanay, Hoverflysmiles, Jfdwolff, Keegan,
Magioladitis, Mdanciu, Medic, Mikael Hggstrm, NCurse, Nerdseeksblonde, Nescio, Pearle, RJFJR, Rcej, Rich Farmbrough, Sam5253, Sbmehta, Serrin, Stevenfruitsmaak, TimVickers, Tomas
e, Woohookitty, Wouterstomp, 16 anonymous edits
Chronic kidney disease Source: https://en.wikipedia.org/w/index.php?oldid=584248212 Contributors: 422e148, ACRoginiel, Ahernconsulting, Ajrsferreira, Alan2005, Alchewizzard, Aleenf1,
Aleksandr Grigoryev, Alex.tan, AlfonsVH, Arcadian, Aris berd, Armeria, Arunsingh16, Ashwinhgtx, Barefootguy, Beachdude2k, Bebofpenge, Ben Ben, Bender235, Bentogoa, BillpSea, Blehfu,
Bluerasberry, Bry9000, Bsrngeorge, Burntout123, CWii, Ceemai, Chaldor, Chester Markel, Chet Gray, Christeletina, Ckd0, Ckdsite, Ckdsiteckd, Ckdsss, CliffC, Crisco 1492, Danielil, David
from Downunder, Davidruben, Deadk82, Dhp1080, DoubleBlue, Earlypsychosis, Elpuellodiablo, Ex50ex, Favonian, Fluffernutter, Folduprabbit, Fred Bauder, FunPika, Fythrion, GB fan, Gaff,
GermanX, Gobonobo, Gogo Dodo, Gtrab, Guido1980, Guptan99, Gwib, Gyuftuvtugb, HOUNDDAWG, Habj, Headbomb, HelenoBR, Hswapnil, Hu12, Hydro, Icseaturtles, Illogicalpie,
Imhoteppaluzzi, Imsomniac2, Indiajal, IvanLanin, J.delanoy, JRPG, Jakew, JamesAM, Jenstcl, Jer5150, Jfdwolff, Jihadcola, Jmh649, JohnCD, JohnnyMyself, Jonathan.s.kt, Jschnur, Jtdaugir,
Kainaw, Kaleem1892, Karissa 25, Karmosin, Karolfranks, Kyoko, Laddiet4e, LeaveSleaves, Limjason, Lugia2453, Lunagato, MarcoTolo, Mark Arsten, MatchingDonors, Matt Strickland,
Maxxicum, Mboverload, McSly, Mdwyer, Micki, Mikael Hggstrm, Mike2vil, Millahnna, Mlaszlo, Mogism, Nephron, Neutrality, Nihiltres, Novangelis, Nutriveg, Ohnoitsjamie, Paleorthid,
Papte, Physio.UoK, Piast93, Pilarian, Quercus solaris, Qwfp, RDBrown, RainbowOfLight, Ramdrake, Ranjeevmishra, RenamedUser01302013, ReyBrujo, Rgoodermote, Rich Farmbrough,
Ripogenus77, Riturajan1026, Rjwilmsi, Robert A West, RockOut25, Rod57, Rory 20 uk, Runkidney, Samar, Scottalter, Sherilynb, Shijiazhuangckd, Singhalawap, Skippyjones, Spydoc,
Squallwc, Stevenfruitsmaak, Susfele, Theroadislong, Tide rolls, Tina312, ToNToNi, Unschool, WarrenKent, WhatamIdoing, Wikih101, Woohookitty, Wouterstomp, Yamamoto Ichiro, Zad68,
Zhenqinli, Zvar, 230 ,12 anonymous edits
Dialysis Source: https://en.wikipedia.org/w/index.php?oldid=582035518 Contributors: AHRtbA==, Abanima, Academic Challenger, Accuruss, Acroterion, Actualpirate, Adirays99, Adrian,
Aeusoes1, Afr77, Ahernconsulting, Ahmednh, Alan2005, Alansohn, Ali, Allgoodnamesalreadytaken, Allstarecho, Andrux, Andyabides, Angela, Angelito7, Animum, Ann Stouter, Anna
Frodesiak, Antandrus, Anthonyhcole, Arcadian, Art Carlson, Assasinator24, Avono, AxelBoldt, Ayman Qasrawi, BRUTE, Beast 99, BeerGeek, Beetstra, Begoon, Bellemonde, Bemoeial,
Bensaccount, BillpSea, Biologos, Bloodshedder, Bob1960evens, Bobet, Bongwarrior, Brandon, BrightStarSky, CSharpMinor, Can't sleep, clown will eat me, Capricorn42, Chaldor, Challiovsky,
Chinneeb, Christian75, Chrysaor, Cohenjm3, Contempo1254, Corticopia, CptUnconscious, Cptmurdok, Crywalt, D Dinneen, DARTH SIDIOUS 2, DBigXray, DMahalko, Dark Samus,
Davidruben, Dcpeters, DeadEyeArrow, Delirium, Delldot, Dialysiscenters, Diberri, Dicklyon, Dirac1933, Discospinster, DocWatson42, Dontworry, DoriSchatell, Drphilharmonic, Dwstultz,
DzWiki, ESkog, Ed Poor, Edgar181, El C, ElTyrant, Entheta, Epbr123, EvelinaB, Evercat, Everyking, Falcon Kirtaran, Fckskwl, Felix-felix, Floyd311, Flyingidiot, Forschung, Fosterche,
FunPika, Gaff, Gene Nygaard, Geoffrey Wickham, George415, GermanX, Germnrottie, Gioto, Gogo Dodo, GoingBatty, Gracenotes, Graham87, GreatWhiteNortherner, Gwernol, HPJoker,
Hancong, Hauskalainen, Hobbema, Hswapnil, Hu12, I dream of horses, IW.HG, Icseaturtles, Ike9898, ImperfectlyInformed, Indiajal, Istomas, Iwu001, J.delanoy, JDspeeder1, JNW,
Jackehammond, James086, Jarseen, JayC, Jayjg, Jazzbeer27, Jclemens, Jeff G., Jepitts, Jfdwolff, Jncraton, Job314, John254, Joyous!, Jtdaugir, JuneGloom07, Jusdafax, KBrown, Karpov33,
Kaszeta, Katherine, Katoa, Kbir1, Kjramesh, Ksyrie, Kummi, Kungfuadam, Kurtis, KyleB, KylieTastic, Kyoko, Lamro, Lawinslow, Lazarus1907, LedgendGamer, Limjason, Lisatwo, Lupo,
M1ss1ontomars2k4, M7, MER-C, Mani1, McSly, MementoVivere, Metju, Michael Schubart, Minkchawla, MistyMorn, Mlpearc, Mmxx, Mohandasalle, Moonside, Munkee, Myanw, Najafhaider,
Natalya, Ndkartik, Nephron, Nickky60, Nicoledeath, Nikthestunned, Noq, Nsaa, Onco p53, Oniscoid, Pakaran, Panscient, Papte, Pathoschild, Pauli100, Peter Chastain, Peter in s, Pikiwyn,
Pinethicket, Pinkadelica, Piyeye, PizzaMargherita, Poeloq, Prad7187, Qasinka, QuizzicalBee, R'n'B, R3m0t, RA0808, RG2, RJaguar3, RattleMan, Razorflame, Rbanzai, Realm of Shadows,
Reconsider the static, Renaldialysis, ReyBrujo, Richardarcher, Rjarm0, Rjwilmsi, Rkaufman13, Roberthilley@hotmail.com, Rodney Boyd, Ronark, Rror, RudolfCardinal, Runkidney,
RussellEngland, S spiegel, SHAHINOVE, SJP, Salamurai, Scarwing, SchnitzelMannGreek, SconeHead, Sdicastro, Sdornan, Seaphoto, Sherryshang, Shinkolobwe, Silvermask, SimonP,
Sjakkalle, Skraz, Snaxe920, SpaceFlight89, SpuriousQ, StaceyGrove, Stephan Leeds, Stevietheman, Stillnotelf, Superm401, Templarion, Tempodivalse, The Thing That Should Not Be,
Theroadislong, Thingg, Tide rolls, TigEer, Timc, Tipiac, Tom davies, Triacylglyceride, TubularWorld, Twatblock, Typhoonchaser, Ubergeek1027, Ucucha, Unckc, Veinor, Velella, Versus22,
Vinsfan368, Virginia-American, Viriditas, Vsmith, Wavelength, WazzaMan, Wik, Xaosflux, Xeno, Xgenei, Yanamad, Yaris678, YassineMrabet, Yintan, Zackkelly, Zidane tribal, ,
, 634 anonymous edits
Kidney transplantation Source: https://en.wikipedia.org/w/index.php?oldid=582005646 Contributors: A More Perfect Onion, Adrian J. Hunter, Alansohn, Allisonamy, Amiliuus, Anas Khalid,
Angelito7, Anrnusna, Applecider42, Arcadian, Arjayay, ArmadilloFromHell, Arx Fortis, BackSpo, BarretB, Bcody80, Beetstra, Beland, Beno1000, Bobo192, Bongomatic, Brainboy109, Bremen,
BrightStarSky, Bry9000, Btl, C'est moi, Cagliost, Carnun, Ccht, Ceyockey, Cindery, Coastergeekperson04, Cocytus, Cool3, Countincr, Crowsnest, Dale Arnett, Danielil, Dararivera, Dasjkl, Dave
Messina, David Kernow, DavidWBrooks, Deathawk, Disavian, DiverDave, Doc.mari, Docvips, Donner60, EchetusXe, Echofish21, Entheta, FastLizard4, Fbv65edel, Feedmecereal, Felix-felix,
FelsenVonEngland, Firien, Florentino floro, For the Laugh of God, Frank A W, Gabbe, Gak, GermanX, Gigi Lincoln, GirlForLife, Gowmoya, Graham87, GreytFolly, Gwernol, HCUP US,
HHarper1976, Haeinous, Halpaugh, Hasban, Hemanshu, Hoppyh, Howcheng, Hydro, Imjustmatthew, InvictaHOG, Islander, J.delanoy, J04n, Jamesontai, Jarviss64, Jazzbeer27, JeffreyN,
Jeremiah, Jessedle, Jesup, Jfdwolff, Joan Lando, Job314, JohnBlack, Justinfreid, KC Panchal, Kablammo, KarenFK, Karolfranks, Kbdank71, Kbik, Kelly, Kuteni, Kyoko, LanguageMan,
LeaveSleaves, Lifeonahilltop, Living Donor, Lybbar12, Magioladitis, Magister Mathematicae, Makemi, Marcika, MatchingDonors, Materialscientist, McSly, Medicalcdl, Michael Devore, Mikael
Hggstrm, Motyka, Mrpaulshen, N5iln, NawlinWiki, Neotarf, Nephron, Neurolysis, NewEnglandYankee, Nick, Noozgroop, Novangelis, Nsaa, Nummer29, Oatmeal batman, Omlakhani,
PFHLai, Papte, Patxi lurra, Persian splendour, Philip Trueman, Piano non troppo, Plutonium27, Porturology, Prosenzweig, Psommerfeld, Qst, Reaper Eternal, Redddogg, Reecesel, Relib,
Remember, Rich Farmbrough, Riznstar, Rjwilmsi, Rklawton, Roastedpepper, Ronhjones, Rrburke, RussAllenUSMA82, Ryulong, SFK2, SYSS Mouse, Scientificwriter, Sdolan1225, SilkTork,
SlaveToTheWage, Sorens, Spiritia, Sticky Parkin, Stoddo1, Suffusion of Yellow, Sun Creator, SundanceXP, TBAmes, Takuro1202, Tassedethe, Tbhotch, Tobias Bergemann, Tom davies,
Tomwsulcer, Tony Fox, Tpesa, Trabelsiismail, Unckc, Wadester10, Wantsarevolution, Wavelength, WelshAlec, Widr, Wikimk, Willhb, World, Wouterstomp, Yonahk, Yworo, Zigger, Zsm101,
Zuhayr09, Zvika, ., 398 anonymous edits
203
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Image Sources, Licenses and Contributors
Image Sources, Licenses and Contributors
File:Gray1123.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1123.png License: Public Domain Contributors: Arcadian, German, Magnus Manske
File:Surface projections of the organs of the trunk.png Source: https://en.wikipedia.org/w/index.php?title=File:Surface_projections_of_the_organs_of_the_trunk.png License: Public Domain
Contributors: Mikael Hggstrm
File:CTscankidney.jpg Source: https://en.wikipedia.org/w/index.php?title=File:CTscankidney.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: RGshredfox
File:KidneyStructures PioM.svg Source: https://en.wikipedia.org/w/index.php?title=File:KidneyStructures_PioM.svg License: Creative Commons Attribution-ShareAlike 3.0 Unported
Contributors: Piotr Micha Jaworski; PioM ENDEPL
File:3D rendered CT of abdominal aortic branches and kidneys.svg Source:
https://en.wikipedia.org/w/index.php?title=File:3D_rendered_CT_of_abdominal_aortic_branches_and_kidneys.svg License: GNU Free Documentation License Contributors: Mikael Hggstrm
from original image created and uploaded by by Dr. I-Chen Tsai ()
File:Kidney-medulla.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Kidney-medulla.JPG License: Public Domain Contributors: File:Kidney-Cortex.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Kidney-Cortex.JPG License: Public Domain Contributors: Jmarchn
File:Hunter enlarged kidney.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Hunter_enlarged_kidney.jpg License: Public Domain Contributors: McLeod
File:Kidney.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Kidney.JPG License: Creative Commons Attribution 3.0 Contributors: Pll
File:1407871818 5c7f215934 o.jpg Source: https://en.wikipedia.org/w/index.php?title=File:1407871818_5c7f215934_o.jpg License: Creative Commons Attribution-Sharealike 3.0,2.5,2.0,1.0
Contributors: Jonathan Koertge
File:Slide22222.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Slide22222.JPG License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Slide42222.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Slide42222.JPG License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Kidney Cross Section.png Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_Cross_Section.png License: Creative Commons Attribution 3.0 Contributors: Anmats,
Dmalicke, Trijnstel
File:Slide4nn.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Slide4nn.JPG License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Slide5pp.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Slide5pp.JPG License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Slide3ppp.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Slide3ppp.JPG License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Right kidney.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Right_kidney.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Left kidneys.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Left_kidneys.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Kidneys.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Kidneys.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Left kidney.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Left_kidney.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: User:Anatomist90
File:Physiology of Nephron.png Source: https://en.wikipedia.org/w/index.php?title=File:Physiology_of_Nephron.png License: Creative Commons Attribution 3.0 Contributors: Madhero88
File:Renal corpuscle.svg Source: https://en.wikipedia.org/w/index.php?title=File:Renal_corpuscle.svg License: Creative Commons Attribution-Sharealike 3.0 Contributors: MKomorniczak
-talk- (polish Wikipedist)
File:Gray1129.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1129.png License: Public Domain Contributors: Arcadian, German, Jmarchn, Magnus Manske, Marcus Cyron,
1 anonymous edits
Image:Gray1130.svg Source: https://en.wikipedia.org/w/index.php?title=File:Gray1130.svg License: Public Domain Contributors: Mysid
File:Nephron illustration.svg Source: https://en.wikipedia.org/w/index.php?title=File:Nephron_illustration.svg License: Creative Commons Zero Contributors: User:Burton Radons
File:Kidney Nephron.png Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_Nephron.png License: Creative Commons Attribution 3.0 Contributors: Anmats, Dmalicke, Marcus
Cyron, Trijnstel
Image:Gray1129.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1129.png License: Public Domain Contributors: Arcadian, German, Jmarchn, Magnus Manske, Marcus
Cyron, 1 anonymous edits
Image:Kidney tubules.png Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_tubules.png License: GNU Free Documentation License Contributors: Original uploader was
JWSchmidt at en.wikipedia
Image:PhysiologieGlomrulaire.png Source: https://en.wikipedia.org/w/index.php?title=File:PhysiologieGlomrulaire.png License: Creative Commons Attribution-ShareAlike 1.0 Generic
Contributors: Tieum at fr.wikipedia
Image: Kidney Nephron Cells.png Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_Nephron_Cells.png License: Creative Commons Attribution 3.0 Contributors: Anmats,
Dmalicke, Marcus Cyron, Trijnstel
Image: Kidney Glomerulus Cell Types.png Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_Glomerulus_Cell_Types.png License: Creative Commons Attribution 3.0
Contributors: Anmats, Dmalicke, Trijnstel
File:Gray1130.svg Source: https://en.wikipedia.org/w/index.php?title=File:Gray1130.svg License: Public Domain Contributors: Mysid
File:Filtration barrier.svg Source: https://en.wikipedia.org/w/index.php?title=File:Filtration_barrier.svg License: Creative Commons Attribution-Sharealike 3.0 Contributors: MKomorniczak
-talk-, polish wikipedist.
Image:Histology-kidney.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Histology-kidney.jpg License: Creative Commons Attribution-ShareAlike 3.0 Unported Contributors:
--Uwe Gille 13:16, 13 May 2006 (UTC)
Image:Glomerulus pas.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Glomerulus_pas.JPG License: Copyrighted free use Contributors: Arcadian, German, Jmarchn, Marcus
Cyron
Image:Gray1132.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1132.png License: Public Domain Contributors: Arcadian, German, Jmarchn, Magnus Manske, Marcus
Cyron, Origamiemensch
Image:Glomerulum of mouse kidney in Scanning Electron Microscope, magnification 1,000x.GIF Source:
https://en.wikipedia.org/w/index.php?title=File:Glomerulum_of_mouse_kidney_in_Scanning_Electron_Microscope,_magnification_1,000x.GIF License: GNU Free Documentation License
Contributors: SecretDisc
Image:Glomerulum of mouse kidney in Scanning Electron Microscope, magnification 5,000x.GIF Source:
https://en.wikipedia.org/w/index.php?title=File:Glomerulum_of_mouse_kidney_in_Scanning_Electron_Microscope,_magnification_5,000x.GIF License: Creative Commons
Attribution-Sharealike 3.0 Contributors: SecretDisc
Image:Glomerulum of mouse kidney with broken capillary in Scanning Electron Microscope, magnification 10,000x.GIF Source:
https://en.wikipedia.org/w/index.php?title=File:Glomerulum_of_mouse_kidney_with_broken_capillary_in_Scanning_Electron_Microscope,_magnification_10,000x.GIF License: Creative
Commons Attribution-Sharealike 3.0 Contributors: SecretDisc
Image:Inner view of fenestrae in capillary of glomerulus in Scanning Electron Microscope, magnification 100,000x.GIF Source:
https://en.wikipedia.org/w/index.php?title=File:Inner_view_of_fenestrae_in_capillary_of_glomerulus_in_Scanning_Electron_Microscope,_magnification_100,000x.GIF License: Creative
Commons Attribution-Sharealike 3.0 Contributors: SecretDisc
Image:Renal corpuscle.svg Source: https://en.wikipedia.org/w/index.php?title=File:Renal_corpuscle.svg License: Creative Commons Attribution-Sharealike 3.0 Contributors: MKomorniczak
-talk- (polish Wikipedist)
Image:Renal Diuretics.gif Source: https://en.wikipedia.org/w/index.php?title=File:Renal_Diuretics.gif License: Creative Commons Attribution-Sharealike 3.0,2.5,2.0,1.0 Contributors:
Haisook at en.wikipedia
File:Nephrocalcinosis.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Nephrocalcinosis.jpg License: Public Domain Contributors: Felix-felix
File:XrayRicketsLegssmall.jpg Source: https://en.wikipedia.org/w/index.php?title=File:XrayRicketsLegssmall.jpg License: Creative Commons Attribution-ShareAlike 1.0 Generic
Contributors: Original uploader was Mrich at en.wikipedia
204
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Image Sources, Licenses and Contributors
File:Aldosterone-2D-skeletal.svg Source: https://en.wikipedia.org/w/index.php?title=File:Aldosterone-2D-skeletal.svg License: Public Domain Contributors:
Image:Aldosterone-2D-skeletal.png by Ben Mills, vectorized by
File:Alpha Intercalated Cell Cartoon.svg Source: https://en.wikipedia.org/w/index.php?title=File:Alpha_Intercalated_Cell_Cartoon.svg License: Creative Commons Attribution 3.0
Contributors: Rswarbrick
Image:Ammonia-dimensions-from-Greenwood&Earnshaw-2D.png Source: https://en.wikipedia.org/w/index.php?title=File:Ammonia-dimensions-from-Greenwood&Earnshaw-2D.png
License: Public Domain Contributors: Ben Mills
File:Ammonia-3D-balls-A.png Source: https://en.wikipedia.org/w/index.php?title=File:Ammonia-3D-balls-A.png License: Public Domain Contributors: Ben Mills
File:Ammonia-3D-vdW.png Source: https://en.wikipedia.org/w/index.php?title=File:Ammonia-3D-vdW.png License: Public Domain Contributors: Benjah-bmm27, Luigi Chiesa
File:Yes check.svg Source: https://en.wikipedia.org/w/index.php?title=File:Yes_check.svg License: Public Domain Contributors: Anomie
Image:GHS-pictogram-bottle.svg Source: https://en.wikipedia.org/w/index.php?title=File:GHS-pictogram-bottle.svg License: Public Domain Contributors: Torsten Henning
Image:GHS-pictogram-acid.svg Source: https://en.wikipedia.org/w/index.php?title=File:GHS-pictogram-acid.svg License: Public Domain Contributors: Torsten Henning
Image:GHS-pictogram-skull.svg Source: https://en.wikipedia.org/w/index.php?title=File:GHS-pictogram-skull.svg License: Public Domain Contributors: Torsten Henning
Image:GHS-pictogram-pollu.svg Source: https://en.wikipedia.org/w/index.php?title=File:GHS-pictogram-pollu.svg License: Public Domain Contributors: Torsten Henning
Image:Hazard_T.svg Source: https://en.wikipedia.org/w/index.php?title=File:Hazard_T.svg License: Public Domain Contributors: BLueFiSH.as, Csium137, Ies, KES47, MarianSigler,
Matthias M., Maxima m, Natr, Phrood, Trelio, W!B:, 12 anonymous edits
Image:Hazard_C.svg Source: https://en.wikipedia.org/w/index.php?title=File:Hazard_C.svg License: Public Domain Contributors: Amishaa, Augiasstallputzer, BLueFiSH.as, Bangin,
Cosmo1976, Csium137, Herbythyme, MarianSigler, Matthias M., Pavel92, Phrood, W!B:, , 12 anonymous edits
Image:Hazard_N.svg Source: https://en.wikipedia.org/w/index.php?title=File:Hazard_N.svg License: Public Domain Contributors: See historic
File:X mark.svg Source: https://en.wikipedia.org/w/index.php?title=File:X_mark.svg License: Public Domain Contributors: User:Gmaxwell
Image:Equilibrium.svg Source: https://en.wikipedia.org/w/index.php?title=File:Equilibrium.svg License: Public Domain Contributors: L'Aquatique
File:Tetraamminediaquacopper(II)-3D-balls.png Source: https://en.wikipedia.org/w/index.php?title=File:Tetraamminediaquacopper(II)-3D-balls.png License: Public Domain Contributors:
Ben Mills and Jynto
File:Ammoniak Reaktor BASF.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Ammoniak_Reaktor_BASF.jpg License: Creative Commons Attribution-Sharealike 3.0
Contributors: Drahkrub
File:AmmoniacalGasEngineStreetcarARWaud.jpeg Source: https://en.wikipedia.org/w/index.php?title=File:AmmoniacalGasEngineStreetcarARWaud.jpeg License: Public Domain
Contributors: Alfred Rudolph Waud, 1828 - 1891
File:x-15.jpg Source: https://en.wikipedia.org/w/index.php?title=File:X-15.jpg License: Public Domain Contributors: Courtesy photo
File:Meth ammonia tank Otley iowa.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Meth_ammonia_tank_Otley_iowa.JPG License: Public Domain Contributors: Bill Whittaker
(user Billwhittaker)
File:Ammiakoprovod NS.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Ammiakoprovod_NS.jpg License: Creative Commons Attribution-Sharealike 2.5 Contributors:
(Azh7)
Image:Hydrochloric acid ammonia.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Hydrochloric_acid_ammonia.jpg License: Public Domain Contributors: User:Walkerma
File:Production of ammonia.svg Source: https://en.wikipedia.org/w/index.php?title=File:Production_of_ammonia.svg License: Public Domain Contributors: Ammoniakproduktion.svg: Orci
derivative work: Leyo
File:Symptoms of hyperammonemia.svg Source: https://en.wikipedia.org/w/index.php?title=File:Symptoms_of_hyperammonemia.svg License: Public Domain Contributors: Mikael
Hggstrm
File:Reference ranges for blood tests - by molarity.png Source: https://en.wikipedia.org/w/index.php?title=File:Reference_ranges_for_blood_tests_-_by_molarity.png License: Public Domain
Contributors: Mikael Hggstrm
File:Magnify-clip.png Source: https://en.wikipedia.org/w/index.php?title=File:Magnify-clip.png License: Public Domain Contributors: User:Erasoft24
Image:Jupiter.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Jupiter.jpg License: Public Domain Contributors: NASA/JPL/USGS
Image:Diamminesilver(I)-3D-balls.png Source: https://en.wikipedia.org/w/index.php?title=File:Diamminesilver(I)-3D-balls.png License: Public Domain Contributors: Benjah-bmm27
File:PD-icon.svg Source: https://en.wikipedia.org/w/index.php?title=File:PD-icon.svg License: Public Domain Contributors: Alex.muller, Anomie, Anonymous Dissident, CBM, MBisanz,
PBS, Quadell, Rocket000, Strangerer, Timotheus Canens, 1 anonymous edits
File:Weewee.JPG Source: https://en.wikipedia.org/w/index.php?title=File:Weewee.JPG License: Public domain Contributors: en:User:Markhamilton
File:Urea.png Source: https://en.wikipedia.org/w/index.php?title=File:Urea.png License: Public Domain Contributors: Ben Mills
File:De urinarum differencia negocium between 1210 and 1230 ..JPG Source:
https://en.wikipedia.org/w/index.php?title=File:De_urinarum_differencia_negocium_between_1210_and_1230_..JPG License: Public Domain Contributors: Hmdpsych
File:IMAG0466.jpg Source: https://en.wikipedia.org/w/index.php?title=File:IMAG0466.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: Rmosler2100
File:Bigot, Trophime - A Doctor Examining Urine.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Bigot,_Trophime_-_A_Doctor_Examining_Urine.jpg License: Public Domain
Contributors: DenghiComm, Ecummenic, Ham, Mattes, Oxxo, Thib Phil, Wst
File:Blutdruck.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Blutdruck.jpg License: Creative Commons Attribution-ShareAlike 3.0 Unported Contributors: User:Peng
File:Blausen 0092 BloodPressureFlow.png Source: https://en.wikipedia.org/w/index.php?title=File:Blausen_0092_BloodPressureFlow.png License: Creative Commons Attribution 3.0
Contributors: User:BruceBlaus
File:Arterial-blood-pressure-curve.svg Source: https://en.wikipedia.org/w/index.php?title=File:Arterial-blood-pressure-curve.svg License: Public domain Contributors: Benutzer:Lupino.
Original uploader was Lupino at de.wikipedia
File:MMSA Checking Blood Pressure.JPG Source: https://en.wikipedia.org/w/index.php?title=File:MMSA_Checking_Blood_Pressure.JPG License: Creative Commons
Attribution-Sharealike 3.0 Contributors: Kilbosh
File:Correcta posicin para la toma de presin arterial.webm Source: https://en.wikipedia.org/w/index.php?title=File:Correcta_posicin_para_la_toma_de_presin_arterial.webm License:
Creative Commons Attribution-Sharealike 3.0 Contributors: User:Manuarteaga
File:Sphygmomanometer.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Sphygmomanometer.jpg License: Public Domain Contributors: BrokenSphere, Edward, EugeneZelenko,
GreyCat, Ranveig, Saperaud
File:Mercury manometer.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Mercury_manometer.jpg License: GNU Free Documentation License Contributors: Original uploader
was Michael V Hayes at en.wikipedia
File:Main complications of persistent high blood pressure.svg Source: https://en.wikipedia.org/w/index.php?title=File:Main_complications_of_persistent_high_blood_pressure.svg License:
Public Domain Contributors: Mikael Hggstrm
File:Circumferential stress.svg Source: https://en.wikipedia.org/w/index.php?title=File:Circumferential_stress.svg License: Creative Commons Zero Contributors: Mikael Hggstrm
file:erythropoietin.png Source: https://en.wikipedia.org/w/index.php?title=File:Erythropoietin.png License: Public Domain Contributors: Cwbm (commons), Delwarl, E A S, Nagy, 4
anonymous edits
file:PBB_GE_EPO_207257_at_tn.png Source: https://en.wikipedia.org/w/index.php?title=File:PBB_GE_EPO_207257_at_tn.png License: GNU Free Documentation License Contributors: file:PBB_GE_EPO_217254_s_at_tn.png Source: https://en.wikipedia.org/w/index.php?title=File:PBB_GE_EPO_217254_s_at_tn.png License: GNU Free Documentation License
Contributors: Image:Ca-TableImage.png Source: https://en.wikipedia.org/w/index.php?title=File:Ca-TableImage.png License: GNU Free Documentation License Contributors: user:Schneelocke
File:Calcium regulation.png Source: https://en.wikipedia.org/w/index.php?title=File:Calcium_regulation.png License: Public Domain Contributors: Mikael Hggstrm
file:Arginine vasopressin3d.png Source: https://en.wikipedia.org/w/index.php?title=File:Arginine_vasopressin3d.png License: Public Domain Contributors: Fvasconcellos
file:PBB_GE_AVP_207848_at_tn.png Source: https://en.wikipedia.org/w/index.php?title=File:PBB_GE_AVP_207848_at_tn.png License: GNU Free Documentation License Contributors: File:AVP, ISH, periventricular region of the hypothalamus, adult mouse.jpg Source:
https://en.wikipedia.org/w/index.php?title=File:AVP,_ISH,_periventricular_region_of_the_hypothalamus,_adult_mouse.jpg License: Creative Commons Attribution 1.0 Generic Contributors:
205
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
Image Sources, Licenses and Contributors
Allen Institute for Brain Science
File:vasopressin labeled.png Source: https://en.wikipedia.org/w/index.php?title=File:Vasopressin_labeled.png License: Public Domain Contributors: Edgar181
File:Oxytocin with labels.png Source: https://en.wikipedia.org/w/index.php?title=File:Oxytocin_with_labels.png License: Public Domain Contributors: Edgar181
Image:Aldosterone-2D-skeletal.svg Source: https://en.wikipedia.org/w/index.php?title=File:Aldosterone-2D-skeletal.svg License: Public Domain Contributors:
Image:Aldosterone-2D-skeletal.png by Ben Mills, vectorized by
File:Steroidogenesis.svg Source: https://en.wikipedia.org/w/index.php?title=File:Steroidogenesis.svg License: GNU Free Documentation License Contributors: David Richfield (User:Slashme)
and Mikael Hggstrm Derived from previous version by Hoffmeier and Settersr.
File:Renin-angiotensin system in man shadow.svg Source: https://en.wikipedia.org/w/index.php?title=File:Renin-angiotensin_system_in_man_shadow.svg License: Public Domain
Contributors: Mikael Hggstrm
Image:Corticosteroid-biosynthetic-pathway-rat.png Source: https://en.wikipedia.org/w/index.php?title=File:Corticosteroid-biosynthetic-pathway-rat.png License: Creative Commons
Attribution-Sharealike 2.5 Contributors: Jean-Etienne Poirrier
Image:Corticosterone.svg Source: https://en.wikipedia.org/w/index.php?title=File:Corticosterone.svg License: Public Domain Contributors: User:Bryan Derksen
Image:Osmoseragulation Carangoides bartholomaei bw en2.png Source: https://en.wikipedia.org/w/index.php?title=File:Osmoseragulation_Carangoides_bartholomaei_bw_en2.png License:
Creative Commons Attribution-Sharealike 3.0 Contributors: Kare Kare modified by Biezl translation improved by smartse
Image:Bachforelle osmoregulatoin bw en2.png Source: https://en.wikipedia.org/w/index.php?title=File:Bachforelle_osmoregulatoin_bw_en2.png License: Public Domain Contributors:
Raver, Duane; modified by Biezl translation improved by User:smartse
File:Paramecium contractile vacuoles.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Paramecium_contractile_vacuoles.jpg License: GNU Free Documentation License
Contributors: derivative work: Hmbrger (talk) Paramecium.jpg: User:Josh Grosse
File:Gray1128.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1128.png License: Public Domain Contributors: Arcadian, German, Jmarchn, Magnus Manske, Marcus Cyron,
Origamiemensch
File:Countercurrentmultiplier.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Countercurrentmultiplier.jpg License: Creative Commons Zero Contributors: User:Pashute
Image:Gray1133.png Source: https://en.wikipedia.org/w/index.php?title=File:Gray1133.png License: Public Domain Contributors: Arcadian, German, Jmarchn, Magnus Manske, Marcus
Cyron, Origamiemensch, 1 anonymous edits
Image:Kidney nephron molar transport diagram.svg Source: https://en.wikipedia.org/w/index.php?title=File:Kidney_nephron_molar_transport_diagram.svg License: Creative Commons
Attribution-Sharealike 3.0 Contributors: Nephron-urine.svg: MKomorniczak -talk-, polish wikipedist. Kidney_nephron_molar_transport_diagram.png: *Nephron-urine.svg: MKomorniczak
-talk-, polish wikipedist. derivative work: Juvo415 (talk) derivative work: Mcstrother (talk)
File:Na-TableImage.png Source: https://en.wikipedia.org/w/index.php?title=File:Na-TableImage.png License: GNU Free Documentation License Contributors: Ahoerstemeier, Atanamir,
Jacek FH, Mav, Paddy, Pieter Kuiper, Saperaud
Image:Management of Hypernatremia.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Management_of_Hypernatremia.jpg License: Creative Commons Attribution-ShareAlike
3.0 Unported Contributors: en:User:HarishV
File:Acetic-acid-dissociation-3D-balls.png Source: https://en.wikipedia.org/w/index.php?title=File:Acetic-acid-dissociation-3D-balls.png License: Public Domain Contributors: Ben Mills
File:Acid-base nomogram.svg Source: https://en.wikipedia.org/w/index.php?title=File:Acid-base_nomogram.svg License: Public Domain Contributors: Huckfinne
File:Symptoms of acidosis.png Source: https://en.wikipedia.org/w/index.php?title=File:Symptoms_of_acidosis.png License: Public Domain Contributors: Mikael Hggstrm
File:Crescentic glomerulonephritis HE stain.JPEG Source: https://en.wikipedia.org/w/index.php?title=File:Crescentic_glomerulonephritis_HE_stain.JPEG License: Creative Commons
Attribution 2.0 Contributors: Arunachalam Ramaswami, Thiraviam Kandaswamy, Tholappan Rajendran, Kizhake Pisharam Jeyakrishnan, Hla Aung, Mohammaed Iqbal, Chakko K Jacob, Haji
Shaukat Zinna and Gazala Kafeel.
File:Filtration_barrier.svg Source: https://en.wikipedia.org/w/index.php?title=File:Filtration_barrier.svg License: Creative Commons Attribution-Sharealike 3.0 Contributors: MKomorniczak
-talk-, polish wikipedist.
Image:Crescentic glomerulonephritis PAS and IF.gif Source: https://en.wikipedia.org/w/index.php?title=File:Crescentic_glomerulonephritis_PAS_and_IF.gif License: Creative Commons
Attribution 2.0 Contributors: Daisuke Koya, Kazuyuki Shibuya, Ryuichi Kikkawa and Masakazu Haneda.
Image:Crescentic glomerulonephritis Periodic acid silver methanamine stain.JPEG Source:
https://en.wikipedia.org/w/index.php?title=File:Crescentic_glomerulonephritis_Periodic_acid_silver_methanamine_stain.JPEG License: Creative Commons Attribution 2.0 Contributors:
Arunachalam Ramaswami, Thiraviam Kandaswamy, Tholappan Rajendran, Kizhake Pisharam Jeyakrishnan, Hla Aung, Mohammaed Iqbal, Chakko K Jacob, Haji Shaukat Zinna and Gazala
Kafeel.
File:Nodular_glomerulosclerosis.jpeg Source: https://en.wikipedia.org/w/index.php?title=File:Nodular_glomerulosclerosis.jpeg License: Public Domain Contributors: Jmarchn,
Nachcommonsverschieber
File:Blausen 0310 DiabeticNephropathy.png Source: https://en.wikipedia.org/w/index.php?title=File:Blausen_0310_DiabeticNephropathy.png License: Creative Commons Attribution 3.0
Contributors: User:BruceBlaus
Image:Diabetic glomerulosclerosis (1) HE.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(1)_HE.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (2) HE.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(2)_HE.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (3) HE.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(3)_HE.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (4) PAS.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(4)_PAS.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (5) PAS.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(5)_PAS.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (7) PAM.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(7)_PAM.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
Image:Diabetic glomerulosclerosis (8) PAM.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Diabetic_glomerulosclerosis_(8)_PAM.jpg License: Creative Commons
Attribution-ShareAlike 3.0 Unported Contributors: Alex brollo, KGH, 1 anonymous edits
File:Kidney acute cortical necrosis.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Kidney__acute_cortical_necrosis.jpg License: Public Domain Contributors: Haymanj
File:Uremic frost on forehead and scalp of young Afro-Caribbean male.jpg Source:
https://en.wikipedia.org/w/index.php?title=File:Uremic_frost_on_forehead_and_scalp_of_young_Afro-Caribbean_male.jpg License: GNU Free Documentation License Contributors: Fythrion
File:Combined hyperkalemia and hypocalcemia.png Source: https://en.wikipedia.org/w/index.php?title=File:Combined_hyperkalemia_and_hypocalcemia.png License: Creative Commons
Attribution-Sharealike 3.0 Contributors: User:Jer5150
File:Patient receiving dialysis 03.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Patient_receiving_dialysis_03.jpg License: Public Domain Contributors: Anna Frodesiak
File:Dialysis - arm - 01.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Dialysis_-_arm_-_01.jpg License: Creative Commons Zero Contributors: User:Anna Frodesiak
File:Hemodialysismachine.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Hemodialysismachine.jpg License: GNU Free Documentation License Contributors: Greg g, Landstuhli,
Moscvitch, Smooth O, 2 anonymous edits
Image:Hemodialysis-en.svg Source: https://en.wikipedia.org/w/index.php?title=File:Hemodialysis-en.svg License: Creative Commons Attribution 3.0 Contributors: Adert, Ingolfson,
Nanoxyde, Smooth O, YassineMrabet, 2 anonymous edits
Image:Peritoneal dialysis.gif Source: https://en.wikipedia.org/w/index.php?title=File:Peritoneal_dialysis.gif License: Public Domain Contributors: National Kidney and Urologic Diseases
Information Clearinghouse, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, USA
File:kidtransplant.jpg Source: https://en.wikipedia.org/w/index.php?title=File:Kidtransplant.jpg License: Public Domain Contributors: NIH
File:Schema der Pankreas-Nierentransplantation mit portalvenser Anastomose des Pankreastransplantats.tif Source:
https://en.wikipedia.org/w/index.php?title=File:Schema_der_Pankreas-Nierentransplantation_mit_portalvenser_Anastomose_des_Pankreastransplantats.tif License: Creative Commons
Attribution-Sharealike 3.0 Contributors: User:Herecomesdoc
206
IVMS Basic Mecdial Science of the Kidney, The Scientific Basis of Clinical Disease
License
License
Creative Commons Attribution-Share Alike 3.0
//creativecommons.org/licenses/by-sa/3.0/
207
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Drug-Drug Interactions (DDIs)Document63 pagesDrug-Drug Interactions (DDIs)Marc Imhotep Cray, M.D.100% (3)
- Prepared and Presented by Marc Imhotep Cray, M.DDocument30 pagesPrepared and Presented by Marc Imhotep Cray, M.DMarc Imhotep Cray, M.D.100% (1)
- HIV and AIDSDocument75 pagesHIV and AIDSMarc Imhotep Cray, M.D.100% (1)
- Drug Metabolism and Drug InteractionsDocument52 pagesDrug Metabolism and Drug InteractionsMarc Imhotep Cray, M.D.100% (1)
- Endocrine System Pathology PPT Lecture SeriesDocument285 pagesEndocrine System Pathology PPT Lecture SeriesMarc Imhotep Cray, M.D.100% (6)
- Host Defense and Microbial PathogenesisDocument72 pagesHost Defense and Microbial PathogenesisMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Clinical History and Examination of Patients With Infectious DiseaseDocument43 pagesClinical History and Examination of Patients With Infectious DiseaseMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Renal Pathology Lectures - PPT SeriesDocument267 pagesRenal Pathology Lectures - PPT SeriesMarc Imhotep Cray, M.D.100% (12)
- Mechanisms of Antibiotic ActionDocument15 pagesMechanisms of Antibiotic ActionMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Pulmonary Tuberculosis, With Leprosy and HIV-Tuberculosis CoinfectionDocument74 pagesPulmonary Tuberculosis, With Leprosy and HIV-Tuberculosis CoinfectionMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Drugs Used in Disorders of The Respiratory SystemDocument100 pagesDrugs Used in Disorders of The Respiratory SystemMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Pneumonia and Lung AbscessDocument50 pagesPneumonia and Lung AbscessMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Gram Positive RodsDocument15 pagesGram Positive RodsMarc Imhotep Cray, M.D.Pas encore d'évaluation
- 6-Pharmacokinetics and Pharmacokinetics SynopsisDocument60 pages6-Pharmacokinetics and Pharmacokinetics SynopsisMarc Imhotep Cray, M.D.100% (2)
- Gastrointestinal Physiology-A Global OverviewDocument76 pagesGastrointestinal Physiology-A Global OverviewMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Renal Insufficiency - Dialysis, Urinary Incontinence - CalculiDocument27 pagesRenal Insufficiency - Dialysis, Urinary Incontinence - CalculiMarc Imhotep Cray, M.D.Pas encore d'évaluation
- 4-Pharmacokinetics IDocument88 pages4-Pharmacokinetics IMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Pharmacodynamics II Dose Response RelationshipsDocument35 pagesPharmacodynamics II Dose Response RelationshipsMarc Imhotep Cray, M.D.Pas encore d'évaluation
- General Principles of Pharmacology - Approach To Learning PharmacologyDocument65 pagesGeneral Principles of Pharmacology - Approach To Learning PharmacologyMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Bacterial Pneumonia PharmacologyDocument70 pagesBacterial Pneumonia PharmacologyMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Basic Pharmacology of DiureticsDocument46 pagesBasic Pharmacology of DiureticsMarc Imhotep Cray, M.D.100% (3)
- Renal Physiology and Regulation of Water and Inorganic IonsDocument73 pagesRenal Physiology and Regulation of Water and Inorganic IonsMarc Imhotep Cray, M.D.67% (3)
- History Taking and Physical Examination - An Overview PDFDocument31 pagesHistory Taking and Physical Examination - An Overview PDFMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Respiratory Pathology and Pathophysiology-Global OverviewDocument90 pagesRespiratory Pathology and Pathophysiology-Global OverviewMarc Imhotep Cray, M.D.100% (1)
- Pulmonary Tuberculosis PharmacologyDocument48 pagesPulmonary Tuberculosis PharmacologyMarc Imhotep Cray, M.D.Pas encore d'évaluation
- POMR and SOAP NotesDocument44 pagesPOMR and SOAP NotesMarc Imhotep Cray, M.D.100% (1)
- Interviewing and The Health History - Rapid ReviewDocument17 pagesInterviewing and The Health History - Rapid ReviewMarc Imhotep Cray, M.D.Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Instilling Otic/Ear Drops Procedure RationaleDocument12 pagesInstilling Otic/Ear Drops Procedure RationaleBSN2-F MASINING NA PAGPAPAHAYAGPas encore d'évaluation
- Nodular Goiter Concept MapDocument5 pagesNodular Goiter Concept MapAllene PaderangaPas encore d'évaluation
- NCPDocument7 pagesNCPJo Chiko FlorendoPas encore d'évaluation
- Dr. Naitik D Trivedi & Dr. Upama N. Trivedi: Pharmacology and Toxicology PracticalDocument2 pagesDr. Naitik D Trivedi & Dr. Upama N. Trivedi: Pharmacology and Toxicology PracticalAnjali RaulPas encore d'évaluation
- Atlas of Common Oral Mucosal Lesions (Final) AIN SHAMS UNIVERSITY IN EgyptDocument92 pagesAtlas of Common Oral Mucosal Lesions (Final) AIN SHAMS UNIVERSITY IN EgyptAbdEl-latifM.Al-smaryPas encore d'évaluation
- Nephrectomy Nov16Document7 pagesNephrectomy Nov16Devanshi JoshiPas encore d'évaluation
- Drug StudyDocument4 pagesDrug StudyAilah Mae Dela Cruz0% (1)
- Scabies Tinea Cruris Pityriasis Versicolor: Semangat!Document11 pagesScabies Tinea Cruris Pityriasis Versicolor: Semangat!Fitriah Nur SyamiatiPas encore d'évaluation
- TFCBT Training GuidelinesDocument3 pagesTFCBT Training GuidelinespolPas encore d'évaluation
- 14 Factitious Disorders and MalingeringDocument13 pages14 Factitious Disorders and Malingeringkrysdana22100% (1)
- Heamatology Dr. Osama PDFDocument94 pagesHeamatology Dr. Osama PDFRaouf Ra'fat Soliman80% (5)
- Care of Postpartum PatientsDocument35 pagesCare of Postpartum PatientsCHi NAi100% (1)
- Hallux Valgus PDFDocument26 pagesHallux Valgus PDFDeny EvanderPas encore d'évaluation
- Pulpotomy Pediatric Prevention Diagnosis Treatment PlanningDocument122 pagesPulpotomy Pediatric Prevention Diagnosis Treatment PlanningTamara Nitya ArianiPas encore d'évaluation
- Heparin - ClinicalKeyDocument85 pagesHeparin - ClinicalKeydayannaPas encore d'évaluation
- Homeostasis Booklet: Done By: Sonali AmbasanaDocument4 pagesHomeostasis Booklet: Done By: Sonali AmbasanaambasanaPas encore d'évaluation
- HSV1 HSV2 R-Gene & VZV R-GeneDocument2 pagesHSV1 HSV2 R-Gene & VZV R-GeneSachinPas encore d'évaluation
- 3-Ammar Notes (Ob - Gyn)Document6 pages3-Ammar Notes (Ob - Gyn)Dr-Hashem Al-ShareefPas encore d'évaluation
- Management of Anembryonic Pregnancy Loss: An Observational StudyDocument6 pagesManagement of Anembryonic Pregnancy Loss: An Observational StudyAnonymous ORleRrPas encore d'évaluation
- Headache: Differential Diagnosis of HeadacheDocument139 pagesHeadache: Differential Diagnosis of Headachemero1983Pas encore d'évaluation
- Restrospective Study Inguinal HerniaDocument6 pagesRestrospective Study Inguinal HerniaDaniela VidalPas encore d'évaluation
- 4th Meeting of GTFCC Working Group On Surveillance 2019 List of ParticipantsDocument4 pages4th Meeting of GTFCC Working Group On Surveillance 2019 List of ParticipantsSteve NjengaPas encore d'évaluation
- Hazard Identification & Analysis Work Sheet For Cake Rusk (Process) - UpdatedDocument12 pagesHazard Identification & Analysis Work Sheet For Cake Rusk (Process) - Updatedsajid waqas100% (1)
- No. Name Position Monday Administration: Alternative Work Arrangement Jose C. Payumo Jr. Memorial High SchoolDocument35 pagesNo. Name Position Monday Administration: Alternative Work Arrangement Jose C. Payumo Jr. Memorial High SchoolJeremy Desoyo TorresPas encore d'évaluation
- Core Surgical Training CT1 Person SpecificationsDocument10 pagesCore Surgical Training CT1 Person SpecificationsRajin MaahiPas encore d'évaluation
- Dental Radiology CurriculumDocument11 pagesDental Radiology CurriculumkarolynaPas encore d'évaluation
- 1 Labor and Delivery ProcessDocument13 pages1 Labor and Delivery ProcessBardiaga JmayPas encore d'évaluation
- B Blab 6 Crossmatch SP 05Document14 pagesB Blab 6 Crossmatch SP 05Rutchelle Joyce PugoyPas encore d'évaluation
- Module 4 - Alcohol AbuseDocument17 pagesModule 4 - Alcohol AbuseMark Johnuel DuavisPas encore d'évaluation
- 06 Luka Kanker 2022Document34 pages06 Luka Kanker 2022mesi purnamaPas encore d'évaluation