Académique Documents
Professionnel Documents
Culture Documents
Efficacy of Nerve Flossing Technique On Improving Sciatic Nerve Function in Patients With Sciatica - A Randomized Controlled Trial
Transféré par
sphadungkit100%(1)100% ont trouvé ce document utile (1 vote)
747 vues10 pagesStudy aimed to evaluate the efficacy of nerve flossing technique (NFT) in the relief of pain and sensory symptoms, restoration of spinal mobility and minimizing functional disability.
Description originale:
Titre original
Efficacy of Nerve Flossing Technique on Improving Sciatic Nerve Function in Patients With Sciatica – a Randomized Controlled Trial
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentStudy aimed to evaluate the efficacy of nerve flossing technique (NFT) in the relief of pain and sensory symptoms, restoration of spinal mobility and minimizing functional disability.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
100%(1)100% ont trouvé ce document utile (1 vote)
747 vues10 pagesEfficacy of Nerve Flossing Technique On Improving Sciatic Nerve Function in Patients With Sciatica - A Randomized Controlled Trial
Transféré par
sphadungkitStudy aimed to evaluate the efficacy of nerve flossing technique (NFT) in the relief of pain and sensory symptoms, restoration of spinal mobility and minimizing functional disability.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 10
VOL.
18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
13
Key words: sciatica; nerve flossing technique;
passive straight leg raise
Abstract. Objective The purpose of this study
was to evaluate the efficacy of nerve flossing
technique (NFT) in the relief of pain and sensory
symptoms, restoration of spinal mobility and
minimizing functional disability. Design
Randomized Controlled Trial. Setting Department
of Neurophyisotherapy, Pravara Rural Hospital
(Tertiary Hospital), Loni, Tal- Rahata, Dist-
Ahmednagar, Maharashtra, India- 413736.
Participants Thirty-nine participants between 20-
55 years of age having clinical diagnosis of sub
acute sciatica due to prolapsed and extruded
intervertebral disc. Interventions. Study group
received the nerve flossing technique along with
conventional physiotherapy and Control group
received only conventional physiotherapy. In NFT
technique, participant performs knee extension with
neck extension with hold of 5 seconds and then
flexes both the knee and neck simultaneously and
holds it for five seconds. Total five sets of the
above were given for six consecutive days. Main
outcome measurements The outcome was
assessed in terms of Visual Analogue Scale (VAS),
Sciatica Bothersomeness Index, Passive Straight
Leg Raise (PSLR), active lumbar flexion range and
Modified Oswestry Disability Questionnaire
(MODQ) score. Results Study group had
statistically significant improvement in VAS score
(p<0.01), Sciatica Bothersomeness Index score
(p<0.01), PSLR (p<0.01), active lumbar flexion
range (p<0.01), and in MODQ score (p<0.01)
compared to control group after 6 days of treatment.
Conclusion Nerve flossing technique can be
utilized with other modalities in the treatment of
sub-acute sciatic patients due to prolapsed and
extruded disc. Clinical Trial Registration Number
PMT/PIMS/RC/2011/09
Cuvinte cheie: sciatic, tehnica nerve flossing,
ridicarea pasiv a membrului inferior extins
Rezumat. Obiective Scopul acestui studiu este
evaluarea eficienei tehnicii de nerve flossing (TNF)
pentru reducerea durerii i a simptomelor
senzoriale, refacerea mobilitii spinale i
minimizarea dizabilitilor funcionale. Design
Control aleatoriu. Locaie Departamentul de
Neurofizioterapie, Spitalul Rural Pravare (Spital de
gradul trei), Loni, Tal- Rahata, Dist-Ahmednagar,
Maharashtra, India- 413736. Participani 39 de
participani cu vrste ntre 20 i 55 de ani au
diagnosticul clinic de sciatic acut cauzat de
prbuirea sau protruzia discului intervertebral.
Intervenii. Grupului de studiu i s-a aplicat tehnica
de nerve flossing, iar grupului de control i s-a
aplicat kinetoterapie convenional. n tehnica TNF,
participanii execut extensia genunchiului cu
meninere de 5 secunde i apoi flexeaz simultan
att genunchiul ct i gtul i menin 5 secunde. S-a
fcut un total de cinci seturi din exerciiile
menionate anterior, 6 zile consecutive. Msurarea
rezultatelor Rezultatele au fost evaluate conform
Scalei Analog Vizuale (SCV), Indexul
Bothersomeness pentru Sciatic, Ridicarea Pasiv a
Piciorului ntins (RPP), gama de flexii lombare
active i Chestionarul pentru Disabilitatea
Modificat Oswestry (CDMO).
Rezultate. Grupul de studiu a prezentate o
mbuntire semnificativ statistic a scorului (SCV)
(p<0.01), scorul pentru Indexul Bothersomeness
pentru Sciatic (p<0.01), RPP (p<0.01) i la scorul
CDMO (p<0.01) n comparaie cu grupul de
controlk dup 6 zile de tratament. Concluzie
Tehnica de nerve flossing poate fi utilizat
mpreun cu alte modaliti n tratamentul
pacienilor cu sciatic sub-acut din cauza prbuirii
i protruziei discului intervertebral. Numrul de
nregistrare al studiului clinic:
PMT/PIMS/RC/2011/09
EFFICACY OF NERVE FLOSSING TECHNIQUE ON IMPROVING
SCIATIC NERVE FUNCTION IN PATIENTS WITH SCIATICA
A RANDOMIZED CONTROLLED TRIAL
EFICACITATEA TEHNICII NERVE FLOSSING N IMBUNTIREA
FUNCIEI NERVULUI SCIATIC LA PACIENII CU SCIATIC
STUDIU RANDOMIZAT
Kranthi Pallipamula
1
, Singaravelan RM
2
_____________________________________________________________________________
1
Postgraduate Student, College of Physiotherapy, Pravara Institute of Medical Sciences, Loni, Maharastra State,
India 413 736. Web: www.pravara.com, Phone: +91-9561745825, +91-9687006553, Fax No: +91-2422-273413,
E-mail: kranthi259@gmail.com
2
Accociate Professor, College of Physiotherapy, Pravara Institute of Medical Sciences, Loni, Maharastra State,
India 413736.
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
14
Introduction
Sciatica is one of the most common painful, expensive and disabling conditions [1].
Amongst painful diseases and disorders, it occupies a foremost place by reason of its incidence
and prevalence, its production by a great variety of conditions, the great disablement it may
produce, and its tendency to relapse; all of which have long ago led to its recognition as one of
the great scourges of humanity. The life time incidence of LBP is 50-70% and the incidence of
sciatica may be as high as 40%. [2,3] Sciatica is a set of symptoms including radiating pain in
the dermatome of a lumbar or sacral spinal nerve root that may be caused by general
compression and/or irritation of one of five spinal nerve roots that give rise to each sciatic nerve
or the left or right or both sciatic nerves[4]. Sciatica along with back pain accounts for a
disproportionate amount of the costs of medical care and disability compensation and is a major
cause of pain, disability, and social cost affecting the quality of life in most patients [5].
Based on the duration of symptoms, low back pain with radiating pain can be divided into three
stages acute, sub-acute and chronic. Acute sciatica is usually defined as the duration of an
episode of sciatica persisting for less than 6 weeks; sub-acute sciatica persists between 6 and 12
weeks; chronic sciatica persists for 12 weeks or more [8]. Sciatica due to disc pathology creates a
public health burden because of its high incidence and considerable socioeconomic costs. In
approximately 90% of the cases, sciatica is caused by a herniated disc (posterolateral) involving
nerve root compression [6, 7]. While sciatica is usually blamed on a bulging intervertebral disc
pressing on the sciatic nerve, there may be another culprit like lumbar canal stenosis,
spondylolisthesis, spinal tumors, piriformis syndrome, cyst of the hip or lumbar, vascular
malformations and intrapelvic aneurysm [8-12].
Herniated disk is a benign disease with a relatively good prognosis causing pain and functional
loss over a period of some months. A bulging disc is known as a contained disc disorder. Gel-
like center (nucleus pulpous) is still enclosed within the tire-like outer wall (annulus fibrosus) of
the disc. A herniated disc is known as non-contained disc disorder in which the nucleus breaks
through the annulus. Disc material (protruded or herniated disc) can press against an adjacent
nerve root and compress and cause sciatica. Herniated or protruded disc causes both compression
and inflammation of the nerve as it contains an acidic, chemical irritant (hyaluronic acid) leading
to pain, numbness, tingling and muscle weakness. Due to protrusion of nucleus pulposus
chemicals located in the epidural region can seep into the nerve roots through small veins that
can connect the epidural space with the intraneural capillaries in the nerve roots. When nucleus
pulposus is positioned next to the nerve root, without increasing pressure on the root, the
physiology of the nerve root can be profoundly disturbed. This is by way of impaired conduction
and development of intraneural oedema and Schwann cell swelling. This is effectively an
inflammatory response triggered by the mere presence of a specific foreign substance and occurs
in the absence of increased pressure on the neural structure [8, 13].
Various physiotherapy interventions like electrotherapy (laser, mechanical traction, ultrasound,
IFT, TENS), manual therapy (neural mobilization, manipulations, massage, stretching),
therapeutic exercises and corsets are available to deal with sciatica due to protruded and
extruded disc. The currently accepted and wide used treatment used for Sciatica due to protruded
and extruded disc based on the results of past research is mechanical traction, TENS and laser.
Sciatica is an expensive and time consuming problem in terms of direct health care costs
(money) as well as indirect health care costs such as work loss and disability, an intervention
giving immediate results in terms of decreasing pain, other sensory symptoms, functional
disability and also delay the need for the surgery will be a cost effective option. But evidence for
treatments which produce immediate effect in patients with sciatica is still conflicting. Certain
promising studies have suggested that neural mobilization techniques are beneficial to patients
with compressive neuropathies like carpal tunnel syndrome (CTS), cubital tunnel syndrome and
low back dysfunction. An experimental study on rats has been done to find out the efficacy of
neural tissue mobilization in sciatica. Despite the array of randomized controlled studies
investigating the effectiveness of neural mobilization, consensus regarding its effectiveness, use
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
15
and clinical value has not been attained due to heterogeneity among study samples. Nerve
Flossing Technique is a safer, beneficial and cost effective conservative treatment option.
However, there is limited evidence about the nerve flossing technique in sciatica [14-21].
Therefore the purpose of this pragmatic randomized trial study is to investigate the clinical utility
and judge superiority of nerve flossing technique within a specific subpopulation of patients with
sciatica of sub-acute stage caused due to disc prolapse and extrusion. The aim of this study was
to find out the efficacy of nerve flossing technique on improving sciatic nerve function in
patients with sciatica. The primary objective of this study was to investigate the immediate and
short term effect of nerve flossing technique (NFT) in the relief of pain, sensory symptoms and
restoration of spinal mobility. Secondary objective of this study was to find out the short term
effect of nerve flossing technique on sciatica related disability.
Methods
Subjects
A total of eighty seven participants aged 20 to 55 years with sciatica were screened for the
study through the Orthopaedic Department, Pravara Rural Hospital (Tertiary Hospital), Loni,
Tal- Rahata, Dist-Ahmednagar, Maharashtra State, India- 413 736 from Jan 2011 to Nov 2011
considering the inclusion and exclusion criteria of which forty two were eligible and agreed to
participate in the study. Three of these participants dropped out of the study as they lost follow-
up. Study group had 20 participants where as Control group had 19 participants. Criteria for
inclusion in the study were participants of Sciatica due to prolapsed and extruded intervertebral
disc[22] (sub acute stage) seen on MRI and CT Scan aged between 25 to 55 years [4,8,17] with
positive Passive Straight Leg Raise Test (30
0
-70
0
) [23] and only sensory symptoms of sciatica
like radiating pain, tingling, numbness. Participants were excluded if they underwent lumbar
spine surgery in last 12 months, suffered from sciatica along with muscular weakness, sciatica
with vascular disorders and diabetic neuropathy, sciatica due to tumor, acute ligament injury,
fractures, Clinical situations where TENS and Mechanical Traction was contraindicated,
psychological or psychosomatic disorders, infections and inflammation of the spine, known
congenital abnormality of the nervous system and serious comorbidity or indication for
immediate surgical intervention [21,23-27].
Outcome measures
The outcome measures used in this study were Visual analogue scale which was used to
measure the intensity of pain before and after the intervention[28], Sciatica Bothersomeness
Index is a scale from 0 to 6, which assesses bothersomeness (0=not bothersome to 6=extreme
bothersome) of back and leg symptoms[29], Passive Straight Leg Raise Test (Hip flexion range)
which was done passively and the hip flexion range was measured with the help of goniometer
as the leg was raised passively until the participant complaints of pain, tingling and
numbness[30-32], Active lumbar flexion range was measured using Modified Schobers
method[33] and The Modified Oswestry Disability Questionnaire (MODQ) for a patient's
functional disability due to low back pain[34].
Procedure
The study received approval from Ethical Committee of Pravara Institute of Medical
Sciences Deemed University. Loni.413637, Maharashtra, India. Participants were screened based
on the inclusion/exclusion criteria and confirmed the diagnosis of PIVD (disc prolapse and
extrusion) on MRI and CT scan. Those willing to participate were briefed about the nature of the
study, effect and benefit of the intervention in the language best understood by them and the
technique was demonstrated to them and Written Informed Consent was obtained. They were
encouraged to clarify questions regarding the study if any. The detailed assessment of
participants was taken. Participants were then randomized into two groups i.e Study (NFT) and
Control group using simple random sampling. (Figure 1) Allocation of participants to the two
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
16
groups was done on alternate basis. The demographic data, pain rating with Visual Analogue
Scale, Sciatica Bothersomeness Index, Passive Straight Leg Raise (hip flexion range)
measurement of active lumbar flexion range and MODQ score of the participants were recorded
prior to any intervention. Reassessment was done on day 6 after intervention. The two groups
were as follows- Study (NFT) group which received Nerve Flossing Technique, Transcutaneous
Electrical Nerve Stimulation (TENS) [35, 36] and Mechanical Traction and Control Group
which received TENS and Mechanical Traction [26, 37, 38].
Figure 1 Flow diagram of the procedure used in the study
Participants received traction three times a week for 15 minutes with 60/20 hold relax
time and TENS for all six days for 15 minutes along the area of symptoms [26, 35, 36, 37, 38].
All the participants were advised to remain as active as possible.
The nerve flossing technique was performed actively by the participant sitting on a chair. The
participant bent the knee backwards under the chair and lowered the head at the same time and
held the position for 5 seconds. [Fig.2]
Then the participant straightened out the leg on the side in which he experienced sciatic pain and
at the same time extended the neck. The participant lifted the leg out and up in front until he
began to experience pain and did not push beyond that point. As the nerve became less sensitive,
he increased the stretching effect by extending the toes of his foot upward toward the shin and
held the position for 5 seconds. [Fig.3]
Ethical Clearance
Screening (87)
Participants
Included(42)
Written Informed
Consent
Randomisation
n= 42
Study Group
n=21
Baseline Data
Intervention (Nerve Flossing
Technique,Traction, TENS)
Drop Out
n=2
Reassessment of outcome
measures
Control Group
n=21
Baseline Data
Intervention (Traction and
TENS)
Drop Out
n =1
Reassessment of outcome
measures
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
17
Nerve Flossing Technique was repeated 15 times. Patient was re-evaluated after every set of 15
repetitions. Total five sets of the above were given in the presence of the investigator with a gap
of 2 hours between each set. It was continued for six successive days. The physiotherapy
intervention was given for six successive days which included traction for only three days, TENS
and NFT for all six days. The data, thus obtained were considered for statistical analysis.
Fig. 2 Starting position of NFT Fig.3 End position of NFT
Results
Statistical analysis was done by GraphPad InStat software (Trial version 3.03) using
various statistical measures such a mean, standard deviation (SD) and tests of significance such
as paired and unpaired t test. The results were concluded to be statistically significant with p
<0.05 and highly significant with p <0.01. Unpairedt test was used to compare differences
between the two groups i.e. the study group (NFT group) and the control group. The baseline
characteristics were comparable (Table 1). The visual analogue scale score and Sciatica
Bothersomeness Index score showed statistically highly significant difference in the study group
participants treated with NFT than control group participants. PSLR score and active lumbar
flexion range depicted statistically highly significant difference in the average range of PSLR
and lumbar flexion in the study group participants treated with NFT than control group
participants. Functional disability in terms of MODQ score showed statistically highly
significant difference in the average functional disability in study group participants treated with
NFT than control group participants (Table 2, Figure 4).
Table 1: Demographic profile and clinical data of participants of both the groups.
Study Group Control Group p value
Age (years) 42.536.99 40.27.55 0.33
BMI (kg/m
2
) 24.563.05 24.642.42 0.92
Duration of symptom(days) 63.6313.20 62.412.58 0.30
MODQ score (0% to 100%) 39.1310.70 38.759.82 0.91
VAS score (1 to 10 cms) 7.011.10 6.871.08 0.6796
BMI: Body mass index, MODQ: Modified Oswestry Disability Questionnaire, VAS: Visual Analog Scale
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
18
Table 2: Intra group comparison of all outcome measures
of study group between pre and post day 6 of intervention.
Outcome
Measures
Pre Day 6 t value p value Results
VAS 7.011.10 1.390.59 31.941 <0.0.1 Highly Significant
SBl 13.532.17 2.371.12 34.142 <.0.01 Highly Significant
PSLR (Hip
flexion range)
45.216.89 72.324.16 27.771 <0.01 Highly Significant
Active Lumbar
Flexion
4.850.65 7.350.58 16.859 <0.01 Highly Significant
Functional
Disability
39.1310.70 30.136.85 19.170 <0.01 Highly Significant
Graph 1: Intra group comparison of all outcome measures
of study group between pre and post day 6 of intervention.
Table 3: Intra group comparison of all outcome measures
of control group between pre and post day 6 of intervention
Outcome Measures Pre Day 6 t value p value Results
VAS 6.871.08 2.540.76 28.360 <0.01 Highly Significant
SBI 12.952.50 4.20.95 20.137 <0.01 Highly Significant
PSLR (Hip flexion range) 41.47.01 62.255.68 23.763 <0.01 Highly Significant
Active Lumbar Flexion 5.010.61 6.650.73 11.794 <0.01 Highly Significant
Functional Disability 38.759.82 17.53.65 21.447 <0.01 Highly Significant
0
10
20
30
40
50
60
70
80
VAS SBI PSLR Active
Lumbar
Flexion
Functional
Disability
7,01
13,53
45,21
4,85
39,13
1,39 2,37
72,32
7,35
30,13
Study Group
Pre
Day 6
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
19
Graph 2: Intra group comparison of all outcome measures
of control group between pre and post day 6 of intervention.
Table 4: Inter group comparison of all the outcome measures in both the groups
between pre and post day 6 of intervention
Outcome
Measures
Study Group
Mean SD
Control Group
Mean SD
t value p value Results
VAS 5.620.77 4.330.68 5.583 <0.01 Highly significant
SBI 11.161.43 8.751.94 4.394 <0.01 Highly significant
PSLR 27.114.25 20.853.92 4.776 <0.01 Highly significant
Active Lumbar Flexion 2.50.65 1.640.62 4.235 <0.01 Highly significant
MODQ 30.136.85 17.53.65 7.238 <0.01 Highly significant
VAS: Visual Analogue Scale, SBI: Sciatica Bothersomeness Index, PSLR: Passive Straight Leg Raise, MODQ: Modified Oswestry Disability
Questionnaire.
Graph 3: Improvement in Pain, sensory symptoms, PSLR,
active lumbar flexion and functional disability in NFT Group
Discussion
Both the groups showed improvement in the relief of pain and sensory symptoms,
improving spinal mobility, minimizing functional disability but the study group (NFT) showed
greater improvement than control group. The greater relief of pain and improvement in sensory
symptoms and spinal mobility might be due to nerve flossing technique which is done actively
0
10
20
30
40
50
60
70
VAS SBI PSLR Active
lumbar
flexion
Functional
Disability
Control Group
Pre
Day 6
0
10
20
30
40
VAS(cm) SBI PSLR
(Hip
flexion
in deg)
Active
lumbar
flexion
(cm)
MODQ
(%)
5,62
11,16
27,11
2,6
39,24
4,33
8,75
20,85
1,64
25,34
Outcome Measures
Study group
Control group
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
20
and involves large amplitude movements which attempt to take the nerve throughout the
available range of motion potentially affecting the nerve both mechanically and physiologically
sufficient enough to disperse the edema, thus alleviating the hypoxia and reducing the associated
symptoms. NFT also causes proximal sliding of lumbar nerve roots with neck and knee flexion
and causes distal sliding of lumbar nerve roots with neck and knee extension and also improve
the actual excursion of the sciatic nerve [13]. With a dynamic variation in the pressure (by
stretching at one end and relaxing at the other end by neck and knee flexion and vice-versa)
evacuation of intraneural edema may be facilitated and also decrease in adhesions and reducing
symptoms by allowing the nerve to move freely with minimal increase in tension. This technique
may also help to oxygenate the nerve, decreasing ischemic pain. NFT reduces pressure caused by
intraneural and extraneural fibrosis which in turn will increase blood circulation and axonal
transport which are necessary for structural and functional integrity of a neuron. It could also be
because movement may help control pain at a central nervous system level. In the gate control
theory [35], stimulation of mechanoreceptors within the joint capsule and surrounding tissues
causes an inhibition of pain at the spinal cord. It could also be directly associated with the
immobilization reduction in the neurogenic inflammation. In addition, it is hypothesized that the
movement of nerve within pain free variations can help to reduce nerve compression, tension
and friction therefore decreasing its mechanosensitivity. Similar results [39] were found in a
favor of Neural Mobilizations in a study done by McCracking [40] who conducted a study on
LBP with radiculopathy and suggested that neurodynamic treatment techniques has some long
term effects in treating patients with non-specific low back pain and lower extremity pain with
neural tension dysfunction. Devasahayam Augustine Joshua [41] did a case report of 43-yr-old
male patient of discogenic pain with radiculopathy was treated with directional preference
exercise and mobilization for four visits. As the patient complained of increased pain during fifth
visit, the treatment strategy was reconsidered and neural mobility exercises were added
progressively in addition to other exercises during visits fifth through seventh, which gradually
relieved the referred pain completely. Study group showed significant improvement in PSLR
(Hip flexion range) [30,31, 36] and active lumbar flexion range when compared to control group
on day 6 of intervention because the sensory symptoms of sciatica were markedly reduced in
study group which were the main cause of reduced PSLR (Hip flexion range) and active lumbar
flexion. Hence the proposed reason of the enhancement in disability (MODQ) [21, 45] score
might be due to the collective effects of reduction in pain, improvement in PSLR (Hip flexion
range) and in this concern improvement in daily activities. Thus the clinical implications are
nerve flossing technique provides short-term improvement in pain, sensory symptoms, spinal
ROM and functional disability and patients with sciatica will benefit from the addition of nerve
flossing to standard treatment for sciatica. The monetary and temporal cost of performing nerve
flossing technique is minimal. Incorporating these exercises into a home exercise program is
cost-effective. Limitations of the study were limited follow up and the present study has focused
only on patients with subacute sciatica due to lumbar disc protrusion and extrusion so the
findings are applicable to patients within this category only.
Conclusion
Nerve flossing technique can be utilized with other modalities in the treatment of sub-
acute sciatic patients due to prolapsed and extruded intervertebral disc for the relief of pain and
sensory symptoms like tingling and numbness, restoration of spinal mobility and to minimize
functional disability.
Acknowledgements
Ethical approval: Ethical Committee of Pravara Institute of Medical Sciences, Loni,
Maharashtra state, India. (PMT/PIMS/RC/2011/09)
Funding: No funding was gained for the study.
Conflict of interest: None declared.
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
21
References
1. 1. Craig Liebenson. (2005), McKenzie self-treatments for sciatica: Journal of Bodywork and
Movement Therapies;9:4042.
2. Frymoyer J (1988). Back pain and sciatica. N. Eng. j. Med. 1988; 318:291-8.
3. A. Akbar, A.Mahar. (2002), Lumbar Disc Prolapse: Management and Outcome Analysis of 96
Surgically treated Patients: Journal of Pakistan Medical Association;52:62.
4. Wilco C. Peul et al. (2007), Surgery versus prolonged conservative treatment for Sciatica. New
England Journal of Medicine;356(22):2245-2256).
5. Ren XS, SelimAJ , Fincke G, Deyo RA, Linzer M, Lee A et al. (1999), Assessment of functional
status, low back disability, and use of diagnostic imaging in patients with low back pain and
radiating leg pain. J Clin Epidemiol; 52:10631071.
6. B W Koes, M W van Tulder and W C Peul. (2007), Diagnosis and treatment of sciatica: BMJ;
334:1313-1317.
7. Valat J P, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. (2010), Best Pract Res Clin
Rheumatol.; 24:241252.
8. Manish Kumar Gaurav Garg. (2011), Epidemiology, Pathophysiology and Symptomatic
Treatment of Sciatica: A Review. International Journal of Pharmaceutical & Biological Archives;
2(4):1050-1061.
9. Wu KW, Hu MH, Huang SC, Kuo KN. Yang SH (2011), Giant ganglionic cyst of the hip as a rare
cause of sciatica. Journal of neurosurg spine. Apr;14(4):484-7.
10. Lommers E, GilletP. (2010), Clinical case of the month. An uncommon cause of sciatica: lumbar
synovial cyst. Rev Med Liege Dec; 65(12): 665-8.
11. Van Gompel J J et al (2010), Vascular malformations, rare cause of sciatic neuropathy: A case
series. Neurosurgery Oct; 67(4): 1133-42.
12. Dudeney Sean et al (1998): Extraspinal causes of Sciatica: A case Report. Spine Feb; 23(4): 494-
496.
13. Michael Shacklock (2005) Clinical neurodynamics. Elsevier
14. Vroomen PCAJ , de KromMCTFM, Slofstra PD, Knottnerus J A. (2000) Conservative treatment
of sciatica: a systematic review. J Spinal Disord.; 13:463469.
15. C.E.Coxhead Et Al (1981): Multicentre Trial of Physiotherapy in the Management of Sciatic
Symptoms. The Lancet; 317(8229): 1065-1068.
16. Hahne AJ , Ford J J , McMeeken J M. (2010), Conservative management of lumbar disc herniation
with associated radiculopathy: a systematic review. Spine. May; 35(11): 488-504.
17. Andrew J . Schoenfeld and Bradley K. Weiner (2010): Treatment of lumbar disc herniation:
Evidence-based practice. Int J Gen Med.; 3: 209214.
18. Philadelphia P. (2001): Philadelphia Panel evidence-based clinical practice guidelines on selected
rehabilitation interventions for low back pain. Physical Therapy., 81: 164174.
19. Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW (2007) Effectiveness
of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur
Spine J.;16:881899.
20. Richard F. Ellis and Wayne A.Hing: (2008), Neural Mobilization: A systematic review of
randomized controlled trials with an analysis of therapeutic efficacy. Journal of Manual and
Manipulative Therapy.; 16(1): 8-22.
21. Sahar M. Adel. (2011): Efficacy of Neural Mobilization in Treatment of Low Back Dysfunctions.
Journal of American Science; 7(4):566-573.
22. David J . Magee, Orthopaedic Physical Assessment, 5
th
edition, Missouri, Elsevier, (2000): Pages
515-552
23. J ames N. Weinstein, DO: (2006), Surgical vs Nonoperative Treatment for Lumbar Disk
Herniation. The Spine Patient Outcomes Research Trial (SPORT): A Randomized Trial. Journal
of American Science.;296(20):2441.
24. Axel Schafer Toby Hall Gerd Mu ller Kathryn Briffa (2011), Outcomes differ between subgroups
of patients with low back and leg pain following neural manual therapy: a prospective cohort
study. Eur Spine J;20:482490.
25. Patrick C (2002), Predicting the outcome of sciatica at short-termfollow-up. British Journal of
General Practice,; 52:119-123.
VOL. 18/ NR 30/ 2012 REVISTA ROMN DE KINETOTERAPIE
22
26. Annette A Harte (2007), The effectiveness of motorised lumbar traction in the management of
LBP with lumbo sacral nerve root involvement: a feasibility study BMC Musculoskeletal
Disorders;(118):1471-2474.
27. J oel E. (2009), Bialosky et al in their study A Randomized Sham-Controlled Trial of a
Neurodynamic Technique in the treatment of Carpal Tunnel Syndrome Journal Of Orthopaedic
and Sports Physical Therapy. Oct;39(10): 709-723.
28. Anne M Boonstra et al (2008) Reliability and validity of the visual analogue scale for disability
in patients with chronic musculoskeletal pain. International journal of rehabilitation
research;31(2):165-169.
29. Grovle L et al., (2010). The bothersomeness of sciatica: patients' self-report of paresthesia,
weakness and leg pain. European Spine Journal. Feb; 19(2):263-9.
30. Cleland J A, Hunt G, Palmer J A. (2004), Effectiveness of neural mobilization in the treatment of a
patient with lower extremity neurogenic pain: a single-case design. Journal of Manual and
Manipulative Therapy.;12(3):14351.
31. Gurpreet Kaur and Shallu Sharma (2011), Effect of passive straight leg raise sciatic nerve
mobilization on low back pain of neurogenic origin. Indian Journal of Phyisotherapy and
Occupational Therapy. J ul-Sep;5(3):179-184.
32. Chang-Yu Hsieh, J oan M Walker and Kate Gillis. (1983), Straight leg raising test. Comparison of
three instruments. Physical Therapy. September;63(9):1429-1433.
33. Renee Williams et al. (1993(, Reliability of the Modified-Modified Schober and Double
Inclinometer Methods for Measuring Lumbar Flexion and Extension. Physical
Therapy.;73(1):26-44.
34. Fritz J M, Irrgang J J . 2001: A comparison of a modified Oswestry Low Back Disability
Questionnaire and the Quebec Back Pain Disability Scale. Physical Therapy.;81: 77688.
35. Subhash Khatri (2003), Basics of electrotherapy, J aypee brothers, , pg 36-38.
36. Sharma Vijay, Sarkari E, Multani N.K. (2011), Efficacy of neural mobilization in sciatica. Indian
Journal of Physiotherapy and Occupational Therapy J an- March,;5(1):125-127.
37. Michelle H. Cameron (2003), Physical agents in rehabilitation, 2
nd
edition, Elsevier.
38. Hood CB, Chrisman (1968), Intermittent pelvic traction in the treatment of the ruptured
intervertebral disc. Physical Therapy.;48:21-30.
39. J avier Gonzlez-Iglesias et al (2010). Differential Diagnosis and Physical Therapy Management
of a Patient With Radial Wrist Pain of 6 Months Duration: A Case Report Journal of
Orthopaedic & Sports Physical Therapy;40(6):361-368.
40. McCracking HV. (2008), The long-termeffects of a neurodynamic treatment technique using a
treatment-based classification approach to low back pain. Journal of Manual & Manipulative
Therapy.;16(3): 161181.
41. Devasahayam Augustine J oshua (2010), Effectiveness of Symptom Guided Therapeutic
Approach in Treating Discogenic Pain with Radiculopathy Using a Combination of Directional
Preference Exercises, Mobilisation and Neural Mobility Exercises A Case Report. Proceedings
of Singapore Healthcare.;19(3):263-270.
42. Mathews J A, Mills SB, J enkins YM et al (1987), Back pain and sciatica: controlled trials of
manipulation, traction, sclerosant and epidural injection, Journal of Rheumatology.;26:416-423.
43. Onel D, Tuzlaci M, Saritl et al., (1989). Computed tomographic investigation of the effect of
traction on lumbar disc herniations, Spine;14:182-90.
44. J oshua A. Cleland et al. (2006), Slump stretching in the management of non-radicular low back
pain: A pilot clinical trial. Manual Therapy.;11:279286.
Vous aimerez peut-être aussi
- Proprioception in Musculoskeletal Rehabilitation. Part 2: Clinical Assessment and InterventionDocument10 pagesProprioception in Musculoskeletal Rehabilitation. Part 2: Clinical Assessment and InterventionAlejandra VasquezPas encore d'évaluation
- An Essential Guide for Scoliosis and a Healthy Pregnancy: Month-by-month, everything you need to know about taking care of your spine and baby.D'EverandAn Essential Guide for Scoliosis and a Healthy Pregnancy: Month-by-month, everything you need to know about taking care of your spine and baby.Pas encore d'évaluation
- The Effect of Closed Kinetic Chain Exercises And.14Document7 pagesThe Effect of Closed Kinetic Chain Exercises And.14fgomez235Pas encore d'évaluation
- A Simple Guide to Meniscus with Acl Injury, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Meniscus with Acl Injury, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Compton - PsoasDocument25 pagesCompton - PsoasiruizmolinaPas encore d'évaluation
- Everything You Wanted to Know About the Back: A Consumers Guide to the Diagnosis and Treatment of Lower Back PainD'EverandEverything You Wanted to Know About the Back: A Consumers Guide to the Diagnosis and Treatment of Lower Back PainPas encore d'évaluation
- Schroth Basics EbookDocument8 pagesSchroth Basics EbookJo CacerPas encore d'évaluation
- Multifidus ExercicesDocument2 pagesMultifidus Exercicesjo21cu100% (1)
- The Spencer TechniqueDocument11 pagesThe Spencer TechniqueDavidAgelliPas encore d'évaluation
- 9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3Document4 pages9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3LeiltonPas encore d'évaluation
- Lec 6 AcompareDocument2 pagesLec 6 AcomparematshPas encore d'évaluation
- Hari Subedi Physiotherapist: Physiotherapy Equipment ChecklistDocument7 pagesHari Subedi Physiotherapist: Physiotherapy Equipment ChecklistdinuPas encore d'évaluation
- Static Palpation of The Spine FINALDocument13 pagesStatic Palpation of The Spine FINALPrathap KumarPas encore d'évaluation
- Mulligan Concept Manual Therapy Standardizing AnnoDocument6 pagesMulligan Concept Manual Therapy Standardizing AnnoDaniel raja SotardodoPas encore d'évaluation
- A Systematic Review of Rehabilitation Exercises To Progressively Load Gluteus Medius - 2016Document36 pagesA Systematic Review of Rehabilitation Exercises To Progressively Load Gluteus Medius - 2016Bruno HenriquePas encore d'évaluation
- Assisted Stretching 1Document7 pagesAssisted Stretching 1Kostas GhinisPas encore d'évaluation
- Ijspt-Biomechanics and Pathomechanics of The Patellofemoral JointDocument11 pagesIjspt-Biomechanics and Pathomechanics of The Patellofemoral JointDevi MigiekaPas encore d'évaluation
- The Functional Anatomy of Tensor Fascia Latae and Gluteus Medius and Minimus. Janat00044-0181Document11 pagesThe Functional Anatomy of Tensor Fascia Latae and Gluteus Medius and Minimus. Janat00044-0181Itai IzhakPas encore d'évaluation
- Shoulder Rehabilitation: - Anatomy Review - Muscle Testing Review - Common Problems - TreatmentDocument29 pagesShoulder Rehabilitation: - Anatomy Review - Muscle Testing Review - Common Problems - TreatmentStefan VladPas encore d'évaluation
- Rene Cailliet - Shoulder Pain PDFDocument170 pagesRene Cailliet - Shoulder Pain PDFm alfin alfauziPas encore d'évaluation
- Kaltenborn Evjenth Concept of OMTDocument34 pagesKaltenborn Evjenth Concept of OMTJaan100% (1)
- Palpation of Bony LandmarksDocument4 pagesPalpation of Bony LandmarksNur Ashriawati BurhanPas encore d'évaluation
- Pelvic DiaphragmDocument37 pagesPelvic DiaphragmLiew John KhengPas encore d'évaluation
- Clinical Neurodynamics and Sports Medicine: Origins and DevelopmentDocument8 pagesClinical Neurodynamics and Sports Medicine: Origins and DevelopmentWahid NasrudinPas encore d'évaluation
- Overhead Throwing: Biomechanics and PathologyDocument7 pagesOverhead Throwing: Biomechanics and Pathologyrapannika100% (1)
- Efficacy of Neck Stabilization Exercises For Neck Pain: A Randomized Controlled StudyDocument6 pagesEfficacy of Neck Stabilization Exercises For Neck Pain: A Randomized Controlled StudyAnonymous mWAaDZmlJwPas encore d'évaluation
- Biomechanics of The Knee During Closed Kinetic Chain ExercisesDocument31 pagesBiomechanics of The Knee During Closed Kinetic Chain ExercisesJean SantosPas encore d'évaluation
- Hip Impingement FaiDocument8 pagesHip Impingement FaiLev KalikaPas encore d'évaluation
- Rotator Cuff Tears Orthoinfo - Aaos.org TopicDocument7 pagesRotator Cuff Tears Orthoinfo - Aaos.org TopicMontserrat LandaPas encore d'évaluation
- Chiropractic Line AnalysisDocument10 pagesChiropractic Line AnalysisD N BidPas encore d'évaluation
- Muscle and LigamentDocument15 pagesMuscle and LigamentPadma VidyaPas encore d'évaluation
- Proprioceptive Neuromuscular Facilitation (PNF)Document76 pagesProprioceptive Neuromuscular Facilitation (PNF)Hasan KhawaldehPas encore d'évaluation
- Hip Assessment Worksheet Page2Document1 pageHip Assessment Worksheet Page2David GoodwinPas encore d'évaluation
- Geriatric Physical TherapyDocument6 pagesGeriatric Physical Therapyirdasriwahyuni0% (1)
- Working With Rib Restrictions (Myofascial Techniques)Document4 pagesWorking With Rib Restrictions (Myofascial Techniques)Advanced-Trainings.com100% (3)
- Manual Therapy Techniques For The KneeDocument11 pagesManual Therapy Techniques For The KneeSaumitra Phadke100% (2)
- Diastasis Rectus Abdominis: Patient InformationDocument8 pagesDiastasis Rectus Abdominis: Patient InformationJames McInerneyPas encore d'évaluation
- Introduction PhysiotherapistDocument12 pagesIntroduction Physiotherapistapi-371068989Pas encore d'évaluation
- SI Provocative TestsDocument7 pagesSI Provocative TestsGumDrop100% (1)
- Bobath For Musculoskeletal Problem Palembang Online 2020Document128 pagesBobath For Musculoskeletal Problem Palembang Online 2020fisioterapi rsph100% (1)
- FasciaDocument3 pagesFasciaWhisperer BowenPas encore d'évaluation
- Self Myofascial ReleaseDocument22 pagesSelf Myofascial ReleaseMuhammad Fahmy100% (1)
- PhysiotherapyDocument53 pagesPhysiotherapybjpalmer100% (2)
- Manual Therapy: DR - DharmavatiDocument78 pagesManual Therapy: DR - DharmavatiHitesh RohitPas encore d'évaluation
- Balance and Vestibular Rehabilitation KitDocument9 pagesBalance and Vestibular Rehabilitation Kitmsnobody8Pas encore d'évaluation
- Ligaments Positional ReleaseDocument2 pagesLigaments Positional ReleaseFlorence LeoPas encore d'évaluation
- AIS and YogaDocument3 pagesAIS and Yogasale18Pas encore d'évaluation
- Joint MobilizationDocument5 pagesJoint MobilizationnainiswathireddygmaiPas encore d'évaluation
- Effects of Mobilization, Stretching and Traction in Sports Professionals With Cervical Radiculopathies - For MergeDocument20 pagesEffects of Mobilization, Stretching and Traction in Sports Professionals With Cervical Radiculopathies - For MergeVidya VS100% (1)
- Corrective Exercise The Lumbo Pelvic GirdleDocument9 pagesCorrective Exercise The Lumbo Pelvic GirdlealmaformaPas encore d'évaluation
- Bio Mechanics and Motor Control of Human Movement 4editionDocument13 pagesBio Mechanics and Motor Control of Human Movement 4editionStanko.Stuhec8307100% (2)
- Introduction To The Mulligan ConceptDocument6 pagesIntroduction To The Mulligan ConceptPrima Krishna DharmawanPas encore d'évaluation
- The Kinetic Chain Approach To PainDocument4 pagesThe Kinetic Chain Approach To PaincharbelhannaPas encore d'évaluation
- Taping For Knee OsteoarthritisDocument9 pagesTaping For Knee OsteoarthritisLinda SugiartoPas encore d'évaluation
- PNF TableDocument4 pagesPNF Tableblitzkrieg5891Pas encore d'évaluation
- Kinetic ChainsDocument5 pagesKinetic ChainsYermia RashaquatPas encore d'évaluation
- Baseline Bubble Inclinometer User ManualDocument2 pagesBaseline Bubble Inclinometer User Manualphcproducts100% (2)
- MC Kenzie: Diagnostic, Prognostic, Therapeutic, and ProphylacticDocument19 pagesMC Kenzie: Diagnostic, Prognostic, Therapeutic, and ProphylacticEvaPas encore d'évaluation
- McKenzie Classification of Mechanical Spinal PainDocument7 pagesMcKenzie Classification of Mechanical Spinal PainVictor Andrés Olivares Ibarra100% (2)
- Someone Who Believes in YouDocument1 pageSomeone Who Believes in YouMANOLO C. LUCENECIOPas encore d'évaluation
- Material Specification - 077154C-000-JSS-1700-009 - DDocument13 pagesMaterial Specification - 077154C-000-JSS-1700-009 - DStructures ProductionPas encore d'évaluation
- Liver: Anatomy & FunctionsDocument18 pagesLiver: Anatomy & FunctionsDR NARENDRAPas encore d'évaluation
- The Broadband ForumDocument21 pagesThe Broadband ForumAnouar AleyaPas encore d'évaluation
- Grade - 2 Subject - Mathematics Unit - Geometry Topic - Geometrical Shapes School - Army School Roorkee Prepared by Mrs. RanjanaDocument25 pagesGrade - 2 Subject - Mathematics Unit - Geometry Topic - Geometrical Shapes School - Army School Roorkee Prepared by Mrs. RanjanaPenke Mejado BelenPas encore d'évaluation
- Physical and Morphological Characterisation of Typha Australis FibresDocument12 pagesPhysical and Morphological Characterisation of Typha Australis FibresIJAR JOURNALPas encore d'évaluation
- Naming Hydrocarbons Worksheet1 Key 12 26 08 PDFDocument2 pagesNaming Hydrocarbons Worksheet1 Key 12 26 08 PDFMarilyn Castro Laquindanum100% (1)
- BC-6000 Installation Guide V7.0 enDocument111 pagesBC-6000 Installation Guide V7.0 enmentule88Pas encore d'évaluation
- FRP Handrail Fittings CatalogDocument6 pagesFRP Handrail Fittings CatalogAl Adel MorenoPas encore d'évaluation
- TreesDocument69 pagesTreesADITYA GEHLAWATPas encore d'évaluation
- Fundamentals of Pain Medicine: Jianguo Cheng Richard W. RosenquistDocument346 pagesFundamentals of Pain Medicine: Jianguo Cheng Richard W. RosenquistMayPas encore d'évaluation
- PIX4D Simply PowerfulDocument43 pagesPIX4D Simply PowerfulJUAN BAQUEROPas encore d'évaluation
- 9 5 - 358 362 PDFDocument5 pages9 5 - 358 362 PDFمالك مناصرةPas encore d'évaluation
- Port Name: Port of BaltimoreDocument17 pagesPort Name: Port of Baltimoremohd1khairul1anuarPas encore d'évaluation
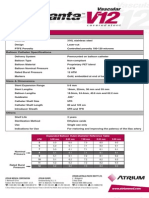
- Advanta V12 Data SheetDocument2 pagesAdvanta V12 Data SheetJuliana MiyagiPas encore d'évaluation
- Cisco 2500 Series RoutersDocument16 pagesCisco 2500 Series RoutersJull Quintero DazaPas encore d'évaluation
- Indor Lighting DesignDocument33 pagesIndor Lighting DesignRajesh MalikPas encore d'évaluation
- Lesson 1 Chapter 9 ErosiondepositionDocument1 pageLesson 1 Chapter 9 Erosiondepositionapi-249320969Pas encore d'évaluation
- Cynosure Starlux 500 Palomar Technical Service ManualDocument47 pagesCynosure Starlux 500 Palomar Technical Service ManualJF SilvaPas encore d'évaluation
- SAT Practice TestDocument77 pagesSAT Practice TestfhfsfplPas encore d'évaluation
- AKI in ChildrenDocument43 pagesAKI in ChildrenYonas AwgichewPas encore d'évaluation
- Tugas Dikumpulkan Pada Hari Sabtu, 11 April 2020. Apabila Email Bermasalah Dapat Mengirimkan Via WA PribadiDocument4 pagesTugas Dikumpulkan Pada Hari Sabtu, 11 April 2020. Apabila Email Bermasalah Dapat Mengirimkan Via WA PribadiFebry SugiantaraPas encore d'évaluation
- From Input To Affordance: Social-Interactive Learning From An Ecological Perspective Leo Van Lier Monterey Institute Oflntemational StudiesDocument15 pagesFrom Input To Affordance: Social-Interactive Learning From An Ecological Perspective Leo Van Lier Monterey Institute Oflntemational StudiesKayra MoslemPas encore d'évaluation
- Owner'S Manual: 2023 Chassis CabDocument444 pagesOwner'S Manual: 2023 Chassis CabDmitry DimasPas encore d'évaluation
- Cambridge IGCSE Paper 2Document4 pagesCambridge IGCSE Paper 2irajooo epik zizterPas encore d'évaluation
- 3rd Quarter Exam (Statistics)Document4 pages3rd Quarter Exam (Statistics)JERALD MONJUANPas encore d'évaluation
- Awakened Citizen Programme-Report-class VII-2014Document4 pagesAwakened Citizen Programme-Report-class VII-2014bhsgeneral r m saraswathi50% (4)
- Table Equivalent Schedule 40 Steel PipeDocument1 pageTable Equivalent Schedule 40 Steel PipeorisPas encore d'évaluation
- Study The Effect of Postharvest Heat Treatment On Infestation Rate of Fruit Date Palm (Phoenix Dactylifera L.) Cultivars Grown in AlgeriaDocument4 pagesStudy The Effect of Postharvest Heat Treatment On Infestation Rate of Fruit Date Palm (Phoenix Dactylifera L.) Cultivars Grown in AlgeriaJournal of Nutritional Science and Healthy DietPas encore d'évaluation
- CBSE DetailsDocument6 pagesCBSE DetailsNARESH KUMARPas encore d'évaluation
- Joey: How a Blind Rescue Horse Helped Others Learn to SeeD'EverandJoey: How a Blind Rescue Horse Helped Others Learn to SeeÉvaluation : 5 sur 5 étoiles5/5 (23)
- Horse Care 101: How to Take Care of a Horse for BeginnersD'EverandHorse Care 101: How to Take Care of a Horse for BeginnersÉvaluation : 4 sur 5 étoiles4/5 (5)
- The Power of the Herd: A Nonpredatory Approach to Social Intelligence, Leadership, and InnovationD'EverandThe Power of the Herd: A Nonpredatory Approach to Social Intelligence, Leadership, and InnovationPas encore d'évaluation
- The Faraway Horses: The Adventures and Wisdom of America's Most Renowned HorsemenD'EverandThe Faraway Horses: The Adventures and Wisdom of America's Most Renowned HorsemenÉvaluation : 4.5 sur 5 étoiles4.5/5 (49)
- Speak Your Horse's Language:: Communicating with the Driving HorseD'EverandSpeak Your Horse's Language:: Communicating with the Driving HorsePas encore d'évaluation
- How Long Can a Fly Fly?: 175 Answers to Possible and Impossible Questions about AnimalsD'EverandHow Long Can a Fly Fly?: 175 Answers to Possible and Impossible Questions about AnimalsPas encore d'évaluation
- Traditional Blacksmithing: The Fine Art of Horseshoeing and Wagon MakingD'EverandTraditional Blacksmithing: The Fine Art of Horseshoeing and Wagon MakingPas encore d'évaluation
- Second-Chance Horses: True Stories of the Horses We Rescue and the Horses Who Rescue UsD'EverandSecond-Chance Horses: True Stories of the Horses We Rescue and the Horses Who Rescue UsPas encore d'évaluation
- The Everything Horse Book: Buying, riding, and caring for your equine companionD'EverandThe Everything Horse Book: Buying, riding, and caring for your equine companionÉvaluation : 2 sur 5 étoiles2/5 (1)
- Wild Horses of the Summer Sun: A Memoir of IcelandD'EverandWild Horses of the Summer Sun: A Memoir of IcelandÉvaluation : 3.5 sur 5 étoiles3.5/5 (4)
- The Winning Horseplayer: An Advanced Approach to Thoroughbred Handicapping and BettingD'EverandThe Winning Horseplayer: An Advanced Approach to Thoroughbred Handicapping and BettingPas encore d'évaluation
- Building Your Dream Horse: Charles Wilhelm's Ultimate Foundation TrainingD'EverandBuilding Your Dream Horse: Charles Wilhelm's Ultimate Foundation TrainingÉvaluation : 4 sur 5 étoiles4/5 (4)
- Lead with Your Heart: Lessons from a Life with HorsesD'EverandLead with Your Heart: Lessons from a Life with HorsesÉvaluation : 4 sur 5 étoiles4/5 (8)
- The USPC Guide to Longeing and Ground TrainingD'EverandThe USPC Guide to Longeing and Ground TrainingÉvaluation : 4.5 sur 5 étoiles4.5/5 (3)
- Project Solomon: The True Story of a Lonely Horse Who Found a Home--and Became a HeroD'EverandProject Solomon: The True Story of a Lonely Horse Who Found a Home--and Became a HeroÉvaluation : 5 sur 5 étoiles5/5 (9)
- Stable Relation: A Memoir of One Woman's Spirited Journey Home, by Way of the BarnD'EverandStable Relation: A Memoir of One Woman's Spirited Journey Home, by Way of the BarnÉvaluation : 5 sur 5 étoiles5/5 (4)
- The Tao Of Horses: Exploring How Horses Guide Us on Our Spiritual PathD'EverandThe Tao Of Horses: Exploring How Horses Guide Us on Our Spiritual PathÉvaluation : 5 sur 5 étoiles5/5 (1)
- Fitness Evaluation of the HorseD'EverandFitness Evaluation of the HorseÉvaluation : 5 sur 5 étoiles5/5 (1)
- Hoof Physics: How to Recognize the Signs of Hoof DistortionD'EverandHoof Physics: How to Recognize the Signs of Hoof DistortionÉvaluation : 5 sur 5 étoiles5/5 (1)
- The Everything Horse Care Book: A Complete Guide to the Well-being of Your HorseD'EverandThe Everything Horse Care Book: A Complete Guide to the Well-being of Your HorsePas encore d'évaluation
- Horses: 101 Super Fun Facts and Amazing Pictures (Featuring The World's Top 18 Horse Breeds)D'EverandHorses: 101 Super Fun Facts and Amazing Pictures (Featuring The World's Top 18 Horse Breeds)Évaluation : 3.5 sur 5 étoiles3.5/5 (11)