Académique Documents
Professionnel Documents
Culture Documents
Nurs 464 - Nis Kritzman - Final
Transféré par
api-2595911650 évaluation0% ont trouvé ce document utile (0 vote)
48 vues25 pagesTitre original
nurs 464- nis kritzman- final
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
48 vues25 pagesNurs 464 - Nis Kritzman - Final
Transféré par
api-259591165Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 25
Running head: ACUTE MI 1 1
Nursing Intervention Synthesis
Chelsea Kritzman
Saginaw Valley State University
ACUTE MI 2
Nursing Intervention Synthesis/Patient Summary
Events leading to admission (ER, Cath Lab, SICU)
Patient, A.B., is a 61 year old Caucasian male who presented to the St. Marys emergency
department via EMS after having a sudden onset of severe left precordial chest pain and
associated shortness of breath. Patient stated he noticed the onset of this pain after he was lifting
a basket of laundry. He described the pain as sharp, intense and rated it a 10/10. The patient has a
history of valvular heart disease and ascending aortic aneurysm. Due to his history of valvular
heart disease, the patient has been on Coumadin therapy since 2000. A.B. stated he recently has
been holding his Coumadin in order to receive back injections for a pinched nerve.
Presenting Symptoms/Assessment: per ER documentation: Patient presented with shortness
of breath, nausea, lightheadedness, diaphoresis and was tachycardic with heart rates in the 120-
130s.
Vital Signs: HR 126, BP 170/101, Temp. 98.6 degrees F (oral), RR 28, O2 Sat 97% on 15L via
100% nonrebreather mask.
EKG 4-6-2014 @ 17:26: Sinus tachycardia with occasional ventricular premature complexes,
moderate intraventricular conduction delay, ST elevation, consider inferior injury marked ST
elevation, consider anterolateral injury. ***ACUTE MI*** Result interpretation EKG #1: Sinus
tachycardia with acute anterolateral, inferior wall MI moderate intraventricular conduction delay.
(Rate was 114; PR, QRS, QT, and ST elevation in specific lead was not found on the EKG
report).
Chest X-ray 4-6-2014 @ 17:39: Poststernotomy changes noted. There is poor inspiration. Heart
size is at the upper limits of normal. Poor inspiratory effort accentuates cardiovascular,
ACUTE MI 3
pulmonary markings. Mild congestion is not excluded. No lobar pneumonia seen. Subtle
interstitial infiltrates are difficult to exclude on the right side.
Lab Results: For 4-6-2014 (day of admission) is on the chart below
Treatment provided in ER: Patient was evaluated immediately on arrival, a STEMI alert was
paged prior to his arrival based on paramedics report. A 12-lead EKG was obtained at the time of
arrival that showed an acute inferolateral MI. The case was discussed with the patients
cardiologist. The cardiologist came to evaluate the patient. The patient was maintained on the
cardiac monitor and on 15L of oxygen via nonrebreather. STEMI orders were initiated, and the
patient was given IV heparin, nitroglycerin, Aspirin, Lopressor, morphine, and Zofran. (No exact
doses of these medications given were obtained from the chart and documentation of the
treatment provided in the ER was straight from the ER admitting note).
Patient Information:
Patient Initials: A.B. Height: 170.1 cm / 57 Weight: 86.2 kg / 189.6 lbs.
Allergies: Cipro
Past Medical History: hypertension, hyperlipidemia, and aortic aneurysm.
Past Surgical History: A.B. had an aortic valve replacement in 2000.
Home Medications:
Coumadin: 2.5 mg, PO once daily, on M/W/F and 5 mg on Su/T/R
o Taken in order to prevent clotting from his previous valve replacement.
Lisinopril: 20 mg, PO once daily
ACUTE MI 4
o Taken to treat high blood pressure.
Simvastatin: 20 mg, PO once daily at bedtime
o Taken to treat high cholesterol.
Primary Diagnosis: Acute Inferior and Anterolateral Myocardial Infarction
Pathophysiology:
Myocardial infarction, also known as MI, is the most serious type of acute coronary
syndrome. Acute coronary syndrome occurs when an atherosclerotic plaque in an artery ruptures.
When the plaque ruptures, platelets rush to this area and clump together which in turn forms a
clot in the artery along with vasoconstriction. The greater the plaque injury determines the
severity of the obstruction within the artery. The artery has to have at least 40% plaque
accumulation before it starts to block blood flow (Ignatavictus & Workman, 2010). In this
patient, the MI can be linked to his medical diagnoses of hypertension and hyperlipidemia. Both
of these diagnoses can play a major role in plaque formation which is linked to acute coronary
syndrome. Typically the plaque that is formed ruptures when a person does some type of
strenuous activity that causes enough stress on the plaque to eventually burst. In this patients
case, he was lifting a clothes basket up and down which could have been enough to cause the
rupture that led to his MI.
An MI occurs after the onset of acute coronary syndrome, as described above. Other
factors that lead to a MI include coronary artery spasm, platelet aggregation, and emboli from
mural thrombi that lines the walls of the cardiac chamber. When acute coronary syndrome occurs
the myocardial tissue is abruptly and severely oxygen deprived. When the heart is not getting the
ACUTE MI 5
appropriate amount of oxygen it needs to survive ischemia occurs. Prolonged ischemia can lead
to cell injury and necrosis of the myocardial tissue if the oxygen is not restored in an adequate
amount of time. Once cell death occurs, there is no way to reverse the effects from a MI so time
is crucial when treating these types of patients. Hypoxia, or decreased oxygen occurs from
prolonged ischemia, which then can causes vasodilation of blood vessels and acidosis. The
contractile functions of the heart can be dramatically impacted by potassium, calcium, and
magnesium imbalances, as well as acidosis at the cellular level. Also, catecholamines are
released, such as epinephrine and norepinephrine, because of the hypoxia. The pain response
increases heart rate, contractility, and afterlord. All of these factors increase the oxygen
requirements in tissue that is already oxygen deprived. When this oxygen demand occurs, life-
threatening ventricular dysrhytmias can also occur (Ignatavictus & Workman, 2010).
Patients who present with signs and symptoms of a MI are classified into one of three
categories depending on the presence or absence of a ST- segment elevation and/or positive
troponin levels. The first category is a ST-elevation MI (STEMI) that is diagnosed using an
electrocardiogram. The second category is Non-ST elevation MI (NSTEMI) and occurs when the
electrocardiogram shows no signs of ST-elevation. If the patient has no ST-elevation along with
normal troponin levels then the patient is put into the last category which is unstable angina.
Statistics show that between 10% and 30% of patients who are diagnosed with unstable angina
develop into a MI within one year, and 29% die from a MI within five years of being diagnosed
with unstable angina (Ignatavictus & Workman, 2010). This patient had a ST- segment elevation
along with increased troponin levels.
Signs and symptoms of a myocardial infarction vary from patient to patient. Some people
present with very few symptoms, whereas some people have many. In one study, one-third of
ACUTE MI 6
patients experiencing a MI had no chest pain. These patients were older, female, or diabetic
(What Are the Symptoms of a Heart Attack, n.d.) . For this circumstance it is important to know
the type of patient they are and their common signs and symptoms. Symptoms can start slowly
and cause only mild pain or discomfort, and it can even be mild or more intense and sudden.
Symptoms also may come and go over several hours. Other facts that are important to remember
are that patients who have diabetes may have no symptoms or very mild ones, the most common
symptom, in both men and women, is chest pain or discomfort, and women are more likely to
present with shortness of breath, nausea and vomiting, unusual tiredness (sometimes for days),
and pain in the back, shoulders, and jaw (What Are the Symptoms of a Heart Attack, n.d.). This
patient presented with signs and symptoms such as shortness of breath, nausea, lightheadedness,
diaphoresis, and tachycardia. These specific symptoms can help the healthcare team reach a
diagnosis along with other diagnostic tests.
This patient had a blockage to the left anterior descending (LAD) artery and the
circumflex artery. Obstruction of the LAD artery causes anterior or septal MIs because it is
responsible for perfusing the anterior wall of the heart and most of the septum of the left
ventricle. This patient is extremely lucky because patients who experience this type of MI have
the highest mortality rate because of the decrease perfusion to the left side of the heart. If the left
side of the heart isnt being perfused, then the rest of the body isnt as well. A patient that has
this type of MI is most likely to have left ventricular failure and dysrhythmias from the severe
damage. The circumflex artery supplies the lateral wall of the left ventricle and portions of the
posterior wall along with the SA and AV nodes. A patient with this type of MI may experience a
posterior wall MI or lateral wall MI and sinus dysrhythmias.
ACUTE MI 7
There are many risk factors that can predispose a person to getting a myocardial
infarction. Atherosclerosis is the primary factor in the progression of coronary artery disease that
can lead to a MI. There are non-modifiable and modifiable risk factors that can put a patient at
risk. The non-modifiable risk factors include personal characteristics that cannot be changed.
These include age, gender, family history, and ethnic background. The modifiable risk factors
include smoking and obesity (Ignatavictus & Workman, 2010). In this patients case, he had a
non-modifiable risk factor such as family history. He also had hypertension and hyperlipidemia
that can have a strong correlation with a MI if it is not properly treated. His biggest risk factor
that put him at greatest risk was that he stopped his Coumadin therapy. He did not have any
modifiable risk factors. All these factors can be individualized from patient to patient and it is
extremely important that the risks are being identified as early as possible in order to help
prevent a MI.
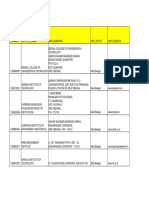
Diagnostic Testing/Lab Results: For 4-6-2014 (Day of admission in the ER) 4-7-2014 (day I
took care of A.B.)
Lab Test Results
for
4-6-2014
Results
for
4-7-2014
Normal
Range
Patient Correlation
WBC
15.9 17.2 5-10 mm3 High due to the tissue necrosis from the acute myocardial
infarction that the patient experienced.
This should be monitored in all hospitalized patients
because of the risk of infections, along with monitoring and
diagnosing other health problems such as an MI. WBCs
could also be high due to stress from the MI and also being
in the hospital.
RBC
5.5 4.5 4.5-5.5 WNL. It is important to monitor RBC because it tells you
how many red blood cells are circulating in the blood
stream. It can be an indicator that the patient is anemic,
dehydrated, or even over hydrated.
Hgb
16.1 13.2 13.5-18
g/dL
WNL on 4-6. Low on 4-7 due to moderate bleeding during
heart catheterization. Hemoglobin is a protein substance
found in red blood cells and it is also composed of iron,
ACUTE MI 8
which is an oxygen carrier. Serum osmolarity on 4-6 was
295 and on 4-7 was 293.1. This finding doesnt necessarily
match with the hemoglobin since you would expect to find a
decreased hemoglobin when there is dehydration and a
normal hemoglobin when the patient is hydrated.
Hct
48.0% 38.1% 39-50 % WNL on 4-6. Low on 4-7 due to moderate bleeding during
heart catheterization. This could indicate slight anemia.
Hematocrit is the volume of red blood cells found in 100
mL of blood, expressed as a percentage.
Platelet
Count
264 219 150-400 WNL. Basic elements in the blood that promote
coagulation.
However this should definitely be continued to be closely
monitored due to the significant decrease in the platelet
count within one day. This significant decrease in platelets
could be due to the patient having an angioplasty (Labriolle,
Bonello, & Lemesle, 2010)
Neutrophils
80% 75% 50-70 % High due to the patient having a MI. Most numerous
circulating WBC. Bodys first line of defense. They respond
to inflammatory and tissue injury. Since the patient had a
MI, the inflammatory response is initiated to help repair the
damaged area.
Lymphocyte
14.9% 4.1% 30-40 % Low due to the patients MI. Immune response with T cells
and B cells. Studies show that low lymphocyte count
obtained within the first 96 hours of a STEMI predicts the
risk of re-MI (Nez, Llcer, Darmofal, & Merlos, 2010).
Monocyte
7.2% 6.8% 4-6% Increased due to the patients MI. They ingest large
particles of debris. Second line of defense.
Eosinophil
2.2% 1.7% 1-3% WNL. They are responsible for combating
multicellular parasites and certain infections.
Basophil
0.4% 0.4% 0.4-1.0% WNL. Increase during the healing process.
PT
12.9 13.5 9.1-12.3
seconds
High due to the patient stopping his Coumadin therapy. PT
measures the clotting ability of the blood and is used to
monitor oral anticoagulant therapy to make sure it is at a
therapeutic level.
INR
1.2 1.3 2-3.5 Low due to the patient stopping his Coumadin in order to
get back injections. Coumadin takes awhile to respond in
the body, so even though he started taking his Coumadin
again, it may take awhile to see the therapeutic results.
This is used to monitor more correctly anticoagulant therapy
for patients receiving Coumadin therapy.
ACUTE MI 9
APTT
22 36 18-36
seconds
1.5-2 x
normal
value
WNL. APTT is affected by medications such as Heparin,
however this patient is not taking Heparin so is not at a
great risk at this time.
BUN
21 21 5-25 mg/dL WNL. Used to detect renal disorder or dehydration. It is
important to monitor renal function in this patient because
of the decreased ejection fraction that he is experiencing. If
the kidneys arent being profused adequately then renal
failure could occur.
Creatinine
1.1 1.1 0.5-1.5
mg/dL
WNL. Used to diagnose renal dysfunction. It is important to
monitor renal function in this patient because of the
decreased ejection fraction that he is experiencing. If the
kidneys arent being profused adequately then renal failure
could occur.
GFR
>60 >60 >60 WNL. This test is a good indication of kidney function and
would be important to monitor in this patient because of his
decreased ejection fraction.
Ca++
9.6 8.0 8.5-10.5
mEq/L
Calcium could have dropped from the patients MI. It is
necessary for the calcium level to be within normal limits
because it is responsible for nerve impulses and contraction
of the myocardium and skeletal muscles. With a calcium
deficit, there is an increased capillary permeability which
causes fluid to pass through the capillary. Since the patient
is already at risk for fluid overload due to his heart failure it
is important to keep calcium regulated.
K+
4.4 4.7 3.5-5.0
mEq/L
WNL. The majority of our bodies potassium (K
+
) is found
in the intracellular space. It aids in the transmission of
electrical impulses in cardiac and skeletal muscle.
Symptoms of elevated K+ include irritability, diarrhea,
cramps, oliguria, and cardiac arrhythmias, such as peaked T
waves and ventricular fibrillation. Muscle weakness,
dizziness, thirst, confusion, changes in the
electrocardiogram, and life-threatening arrhythmias may
develop during potassium deficiency. Low levels of K+ can
be caused by diarrhea & vomiting, eating disorders,
draining wounds, diuretic therapy and licorice.
Hyperkalemia levels can be caused by renal failure, cell
damage, diabetic ketoacidosis, and hemolysis. It would be
important to continue to monitor this patients K+ level
because he is on Lasix that can cause a decrease in this
level.
Na+
140 138 135-145
mEq/L
WNL. Sodium (Na
+
) is the major cation in the extracellular
fluid and plays a major role in maintaining osmotic pressure
of extracellular fluid, regulating potassium and chloride
levels, stimulating neuromuscular reactions, and
ACUTE MI 10
maintaining systemic blood pressure. Low levels can cause
confusion, irritability, convulsions, tachycardia, nausea,
vomiting, and loss of consciousness. Elevated levels of Na
+
include restlessness, intense thirst, weakness, swollen
tongue, seizures, and coma. It would be important to
continue to monitor patients Na+ levels because he is on
Lasix, which can cause hyponatremia.
Mg 2.0 1.9 1.7-2.5 WNL. Magnesium is most plentiful in the cells. One-third
of the magnesium ingested is absorbed through the small
intestine, and the remaining unabsorbed magnesium is
excreted in the stools. The absorbed magnesium is
eventually excreted through the kidneys. It is also needed
for neuromuscular activity. It would be important to
continue to monitor patients Mg levels because he is on
Lasix, which can cause hypomagnesemia.
Cl-
103 104 98-106
mmol/L
WNL. Chloride is the most plentiful extracellular anion in
the body. It carries a negative charge and serves to maintain
electrically neutrality with cations. It would be important to
continue to monitor patients Cl- levels because he is on
Lasix, which can cause hypochloremia.
CO2
26 29 22-30
mEq/L
WNL.
Albumin
4.4 3.5-4.8
gm/dL
WNL. Component of protein. Makes up half of plasma
proteins. It increases osmotic pressure for maintaining
vascular fluid.
AST
62 Not
obtained
4-36 IU/L Increased due to patients MI and long term statin use.
Enzyme found in the liver and the heart muscle. A
contraindication to statins is a prolong increase in AST,
therefore this should continue to be monitored.
ALT 69 Not
obtained
19-60 IU/L Increased due to patients MI and long term statin use. ALT
is an enzyme found primarily in the liver cells. It is also
found in small amounts in the heart, kidney, and skeletal
muscle. A contraindication to statins is a prolong increase in
ALT, therefore this should continue to be monitored.
Troponin
310 212 0-0.1
>0.120
ischemic
High on both days due to possible damage to the heart from
the patients myocardial infarction. Troponin is a
biochemical marker for cardiac diseases especially for the
diagnosis of acute myocardial infarction. The troponins are
proteins, present in both the heart muscle and skeletal
muscles. The cardiac-specific troponin is released from the
heart into the blood stream 1 to 3 hours after the onset of
symptoms of a MI. Troponin is a more specific for cardiac
muscle injury than CPK-MB. Expect troponin to be
elevated at least 2 weeks after the onset of a MI.
BNP 48 367 5-99 pg/mL WNL on 4-6. High on 4-7 due to myocardial infarction.
ACUTE MI 11
BNP is a neurohormone secretion primarily in the cardiac
ventricles and will increase in response to volume
expansion and pressure overload. Since the patient is
experiencing heart failure from his MI he has an increase in
volume due to the heart not being able to pump adequately.
The afterload is increased due to the backflow of fluid into
the lungs which ultimately increases the pressure overload
in the ventricles causing BNP to increase.
CK >6400 >6400 0-170 unit/L High on both days due to the patient having a myocardial
infarction. CK is an enzyme found in high concentration in
the heart and skeletal muscles and in low concentration in
the brain tissue.
CKMB 585 628 0-3.9
>3.9
ischemic
High on both days because there is damage to specifically
the myocardial cells.
Cholesterol Not
obtained
179 <200 WNL. Cholesterol is a blood lipid synthesized by the liver
and is found in red blood cells, cell membranes, and
muscles. WNL because the patient is taking a statin to help
keep this level reduced.
Triglycerides Not
obtained
154 30-150 Slightly high due to patients myocardial infarction.
HDL Not
obtained
48 40-75 WNL.
LDL Not
obtained
100 30-130 WNL
(Pagana & Pagana, 2011).
Diagnostic Tests:
Coronary Angiogram 4-6-2014 @ 22:06
Successful percutaneous transluminal angioplasty, thrombectomy and bare metal stent
placement to the proximal left anterior descending with 100% occlusion and TIMI 0 flow
distally reduced to 0% stenosis and TIMI 3 flow distally. Successful thrombectomy of the
circumflex artery with large thrombus burden reduced to minimal thrombus burden distally
with thrombectomy using export catheter. Hemodynamics: RA mean was 4, RV systolic was
41, pulmonary capillary wedge pressure was 13. PA was 43/29 with a mean of 31. There was
no significant gradient noted across pulmonic valve. Cardiac output was 3.67 liters per
minute with a cardiac index of 1.85 liters per minute per square meters. Oximetry run RA
saturation was 61%, PA was 63%, and AO was 97 on 100% nonrebreather mask.
Echocardiogram 4-7-2014 @ 06:05:
1.) Left ventricle: the cavity size was normal. Wall thickness was normal. Systolic function
was severely reduced. The estimated ejection fraction was 20-25%. Diffuse hypokinesis.
ACUTE MI 12
Hypokinesis of the anteroseptal myocardium. Hypokinesis of the apical myocardium.
Hypokinesis of the inferior myocardium.
2.) aortic valve: a mechanical prosthesis was present.
3.) mitral valve: mild regurgitation
4.) pericardium, extracardiac: there was no pericardial effusion.
12 lead Electrocardiogram 4-7-2014 @ 05:54:
Sinus tachycardia, possible left atrial enlargement, marked right axis deviation, moderate
intraventricular conduction delay, marked ST elevation, consider anterior injury
Chest X-Ray 4-7-2014 @ 09:40:
1.) Interval significant improvement in the bronchovascular and interstitial prominence as
well as parenchymal opacities in bilateral lung fields with residual disease.
2.) Heart size is stable.
Importance of Diagnostic Tests: The diagnostic tests that are done to confirm and monitor a MI
are vital to the patient and the heart. It is important that any patient who comes in to the hospital
with signs and symptoms of an MI, are being tested in order to try to save as much heart muscle
as possible. If the heart is not perfusing properly, then other parts of the body are being effected
as well.
Medications:
Medication
Indication Dose
Route
Frequency
Side Effect
Contraindications
Patient
Correlation
clopidogrel (Plavix) Reduction of
atherosclerotic events
in patients at risk for
such events including
recent MI, acute
coronary syndrome,
stroke, or peripheral
vascular disease.
75 mg, PO,
once daily
SE: depression,
dizziness, fatigue,
headache, epistaxis,
hypertension
CI:
hypersensitivity;
pathologic bleeding
such as a peptic
ulcer or intracranial
hemorrhage;
lactation
Patient is on
this
medication
because of his
acute MI in
order to help
prevent his
platelets from
sticking
together. He
is also on this
medication
because of his
ACUTE MI 13
aortic valve
replacement.
This will
inhibit
platelets from
sticking to the
new valve and
preventing
more damage.
famotidine (Pepcid) Management of
gastric
hypersecretory states.
20 mg, IV,
q12 hours
SE: confusion,
dizziness,
drowsiness,
headache,
constipation,
nausea, decreased
sperm count and
erectile dysfunction
CI:
hypersensitivity;
some products
contain alcohol and
should be avoided
in patients with
known intolerance
Patient is on
this
medication to
help prevent
stress ulcers.
furosemide (Lasix) Edema due to heart
failure, hepatic
impairment or renal
disease. Also used
for hypertension
20 mg, IV,
once daily
SE: blurred vision,
dizziness,
headache, hearing
loss, hypotension,
dehydration,
hypochloremia,
hypokalemia,
hypomagnesemia,
hyponatremia,
hypovolemia, and
metabolic alkalosis
CI:
hypersensitivity;
cross-sensitivity
with thiazides and
sulfonamides may
occur; hepatic coma
or anuria; some
liquid products may
contain alcohol,
avoid in patients
with alcohol
Patient is on
this
medication to
help control
blood
pressure due
to excess
fluid.
ACUTE MI 14
intolerance.
lisinopril (Prinivil) Alone or with other
agents in the
management of
hypertension.
5 mg, PO,
once daily
SE: hypotension,
cough, taste
disturbances,
dizziness,
drowsiness, fatigue,
headache,
insomnia, and
weakness
CI:
hypersensitivity;
history of
angioedema with
previous use of
ACE inhibitors
Patient is on
this
medication to
help treat his
hypertension.
This
medication is
also a
standard of
care for a
patient who
has an acute
myocardial
infarction.
metoprolol (Lopresor) Hypertension, angina
pectoris, prevention
of MI and decreased
mortality in patients
with recent MI. Also,
management of
stable, symptomatic
heart failure due to
ischemic,
hypertensive, or
cardiomyopathic
origin.
2.5 mg, IV, q6
hours
SE: fatigue,
weakness, anxiety,
depression,
dizziness,
drowsiness,
insomnia, memory
loss, erectile
dysfunction, and
blurred vision.
CI: uncompensated
CHF; pulmonary
edema; cardiogenic
shock, bradycardia,
or heart block.
Patient is on
this
medication to
help treat his
hypertension
and take the
workload off
of the heart
after his MI.
This is a
standard of
care for
someone who
has had a MI.
pravastatin
(Pravachol)
Adjunctive
management of
primary
hypercholesterolemia
and mixed
dyslipidemias. Also,
primary prevention
of CHD in patients
without clinically
evident CHD.
80 mg, PO,
once daily at
bedtime
SE: dizziness,
headache,
insomnia,
weakness, chest
pain, peripheral
edema, abdominal
cramps,
constipation,
diarrhea, flatus,
heartburn, and
rashes
CI:
hypersensitivity;
active liver disease
or unexplained
persistent increase
in AST or ALT;
Patient is on
this
medication to
help treat his
high
cholesterol.
Patient needs
to be
monitored for
his AST and
ALT since a
contradinction
to this
medication is
persistent
increase in
these values. I
ACUTE MI 15
concurrent use of
gemfibrozil or
azole antifungals.
would
question these
medications
in this patient
because of the
drastic
increase.
Since patient
has stable
cholesterol
levels then
maybe a
different plan
of care should
be considered
since the
increase in
AST and
ALT.
warfarin (Coumadin) Prophylaxis and
treatment of venous
thrombosis,
pulmonary
embolism, atrial
fibrillation,
management of MI to
decrease risk of death
and to decrease risk
of subsequent MI.
2.5 mg, PO,
once daily
SE: cramps,nausea,
dermal necrosis,
bleeding, and fever.
CI: uncontrolled
bleeding; open
wounds; active
ulcer disease;
recent brain, eye, or
spinal cord injury
or surgery; severe
liver or kidney
disease;
uncontrolled
hypertension
Patient is on
this
medication
because of his
valvular heart
replacement
to help
prevent clots
and because
of his acute
MI to
decrease risk
of a
subsequent
MI. A goal
INR for this
patient since
he has a valve
replacement is
3 and a goal
PT
acetaminophen
(Tylenol)
Mild pain and fever 650 mg, PO,
q4 hours PRN
SE: hepatic failure,
hepatotoxicity,
renal failure,
neutropenia,
pancytopenia,
leukopenia, and
Patient is on
this
medication to
help treat mild
pain.
ACUTE MI 16
rash.
CI: previous
hypersensitivity;
products containing
alcohol, aspartame,
saccharin, sugar, or
tartrazine should be
avoided in patients
who have
hypersensitivity or
intolerance to these
compounds
alprazolam (Xanax) Treatment of
generalized anxiety
disorder, panic
disorder, and anxiety
associated with
depression.
0.25 mg, PO,
q6 hours PRN
SE: dizziness,
drowsiness,
lethargy, confusion,
hangover,
headache, mental
depression, and
blurred vision.
CI:
hypersensitivity;
cross-sensitivity
with other
benzodiazepines
may exist;
preexisting CNS
depression; severe
uncontrolled pain
Patient is
prescribed
this
medication to
help treat the
anxiety he has
from his acute
MI if needed.
atropine (Atro-Pen) Treatment of sinus
bradycardia and heart
block.
0.5 mg, IV
push, PRN
SE: drowsiness,
confusion,
hyperpyrexia,
blurred vision,
tachycardia, dry
mouth, urinary
hesitancy, and
sweating.
CI:
hypersensitivity;
angle-closure
glaucoma; acute
hemorrhage;
tachycardia
secondary to
cardiac
insufficiency or
Patient is
prescribed
this
medication if
bradycardia or
heart block
occurs.
ACUTE MI 17
thyrotoxicosis;
obstructive disease
of the GI tract.
morphine
(Astramorph)
Severe pain,
pulmonary edema,
and pain associated
with MI. These drugs
bind to the opioid
receptors which are
on the surface of
nerve cells and that
sets off a chain of
chemical reactions
inside the cell which
ultimately causes the
cell membrane to be
less excitable which
decreases painful
stimuli.
2 mg, IV
push, q5
minutes PRN
SE: confusion,
sedation, dizziness,
hypotension,
bradycardia,
constipation,
headache, and
unusual dreams.
CI:
hypersensitivity;
some products
contain tartrazine,
bisulfites, or
alcohol and should
be avoided in
patients with
known
hypersensitivity.
Patient is
prescribed
this
medication to
help treat
severe pain
from his MI
as needed.
nitroglycerin Acute and long-term
prophylactic
management of
angina pectoris. To
improve blood flow
to the heart,
nitroglycerin opens
up (dilates)
the arteries in the
heart (coronary
arteries), which
improves symptoms
and reduces how
hard the heart has to
work.
0.4 mg,
Sublingual, q5
minutes PRN
SE: dizziness,
headache,
restlessness,
hypotension,
tachycardia, and
abdominal pain.
CI:
hypersensitivity;
severe anemia;
pericardial
tamponade;
constrictive
pericarditis; alcohol
intolerance.
Patient is
prescribed
this
medication to
help treat
angina from
his MI as
needed.
procholorperazine
(Compro)
Management of
nausea and vomiting.
5 mg, IV
push, q6
hours PRN
(Not given
during my
shift)
SE: extrapyramidal
reactions, sedation,
blurred vision, dry
eyes, constipation,
and dry mouth.
CI:
hypersensitivity;
cross-sensitivity
with other
phenothiazines may
exist; angle-closure
Patient is
prescribed
this
medication to
help treat his
nausea,
vomiting, and
anxiety as
needed.
ACUTE MI 18
glaucoma; bone
marrow depression;
severe liver or
cardiovascular
disease
zolpidem (Ambien) Insomnia 5 mg, PO, at
bedtime PRN
(Not given
during my
shift)
SE: daytime
drowsiness,
dizziness, abnormal
thinking, amnesia,
nausea, and
vomiting.
CI:
hypersensitivity;
sleep apnea
Patient is
prescribed
this
medication to
help treat
insomnia as
needed.
eptifibatide
(Integrillin)
Acute coronary
syndrome, including
patients who will be
managed medically
and those who will
undergo
percutaneous
coronary intervention
that may consist of
percutaneous
transluminal
angioplasty or
atherectomy.
2 mcg/kg/min,
IV,
continuous
SE: hypotension,
bleeding (including
GI and intracranial
bleeding,
hematuria, and
hematomas.
CI:
hypersensitivity;
active internal
bleeding or history
of bleeding within
previous 30 days;
severe uncontrolled
hypertension; major
surgical procedure
within 6 weeks
Patient is
prescribed
this
medication
because of his
MI and to
help prevent
his platelets
from sticking
together.
Nitroglycerin Acute and long-term
prophylactic
management of
angina pectoris
10 mcg/min,
IV continuous
SE: dizziness,
headache,
restlessness,
hypotension,
tachycardia, and
abdominal pain.
CI:
hypersensitivity;
severe anemia;
pericardial
tamponade;
constrictive
pericarditis; alcohol
intolerance.
Patient is
prescribed
this
medication to
help treat
angina from
his MI and to
help dilate his
blood vessels.
Given also for
his
hypertension
and increased
afterload from
his heart
ACUTE MI 19
failure.
Sodium Chloride
0.9%
This solution is used
to supply water and
salt
(sodium chloride) to
the body. Sodium
chloride solution
may also be mixed
with
other medications giv
en by injection into a
vein.
1000 mL, IV
continuous
SE: Redness, pain ,
or swelling at the
injection site may
occur.
This patient is
receiving
Sodium
Chloride 0.9%
in order to
maintain
proper
hydration at a
set rate while
in the
hospital.
(Deglin &Vallerand 2011)
Assessment:
BP: 110/70 HR: 101 R: 18 Temp: 98.6 (oral) PO2: 100% on 4L of O2 via nasal cannula
Neuro Assessment: Patient is alert and oriented to person, place, and time. Patient states his pain
is 6/10 and is worse when he is laying flat in bed. Pupils are equal, round, and reactive to both
light and accommodation. Face is symmetrical and the patient has firm tone and ROM in all
extremities. Patient also passed the dull/sharp test. Glasgow coma scale = 15.
Cardiovascular: Patient is in normal sinus rhythm, with varying tachycardia. S1 and S2 heard
with no abnormal murmur. There are crisp valve sounds. Pulses are 2+ and are equal bilaterally
in upper extremities and are faint bilaterally in the dorsalis pedis. Jugular vein distension absent
when HOB is elevated at 45 degrees. Capillary refill was less than 3 seconds, nail beds were
pink, and no clubbing was present. Upper and lower extremities were warm and dry to the touch.
The EKG strip below was from 4-7-14.
Rate: 101 PR: 0.12 QRS: 0.12 Interpretation: Sinus Tachycardia
ACUTE MI 20
Pulmonary: Lungs are clear bilaterally with regular rhythm and rate. Prior nursing note stated
that he had some scattered rhonchi and basilar rales. I would continue to monitor pulmonary
function to make sure the Lasix is working to move the fluid off of the patients lungs. Patient
states he is dyspneic when he is laying flat in bed, but it goes away when the HOB is elevated.
Patient is on 4L of O2 via nasal cannula. No cough is present.
GI: Abdomen soft, round, symmetric, and non-tender. Bowel sounds active x 4. Patient did not
have a bowel movement within the 12 hours I took care of him. Patient is on a heart healthy diet
with a restriction of sodium. Since the patient is experiencing heart failure symptoms it would be
important for this patient to restrict sodium because he is already retaining fluid in the lungs.
GU: Patient has a Foley catheter in place that was secured with tape on his thigh. It was patent
with yellow and clear urine. Bladder distention was absent. Urine output was adequate at every
hourly check. Patient had Foley catheter in place because he still had his venous sheath in place
at the time I took care of him. The plan of care was to remove the sheath before the end of the
shift.
Integumentary: The skin is cool, dry, intact, and elastic. The patient appears to be quite pale in
color. Patient is hydrated as evidence by non-tenting skin on his clavicle. No edema noted in
extremities. The patient did not have any bruising present. His backside was checked and no skin
break down or bruising was apparent. Braden Skin integrity risk score- 23 (not a risk for pressure
ulcer at this time)
IV Assess: 18 gage in right and left antecubital area of the arm. Both sites are clean, dry, with
dressing intact. Both IVs are also secured with tape and have good blood return. No redness,
swelling, or signs of infiltration.
ACUTE MI 21
Activity: Patient expressed desire to get out of bed to sit in the chair. The nurse and I helped him
get out of bed. We helped him up slowly, and he stated that he did not feel any lightheadedness
or dizziness. His gait was steady and he had no complaints at the time of getting out of bed. I
came back to assess the patient after a few minutes and he then felt dizzy and lightheaded. I then
helped him back to bed, where after a few minutes of laying back down he felt better again.
Patient did not get out of bed for the remainder of my shift. I discussed the importance of moving
out of bed slowly to prevent further complications and falls, since he just experienced a massive
heart attack and because he is on many blood thinners and anti- platelet medications. Hendrich II
Fall Risk Model score- 3.
Psychosocial/Spiritual: A.B. was really discouraged about having an MI. He was very anxious
and feared the unknown. He also expressed concern about having to take time away from his job.
Patient stated he was very religious and believed that his care was in Gods hands. He expressed
desire to talk to the hospitals Chaplin. He also discussed with me how his wife died in 2003 and
how it has been hard on him and his daughter ever since. He is currently single and lives by
himself in the Saginaw area. He admits to being a former smoker and currently drinks
occasionally.
Educational Needs: Patient needs teaching on the importance of not stopping his Coumadin
therapy. Teaching would include the significance that Coumadin has in preventing future MIs,
since he has a history of hypertension and hyperlipidemia. Another educational need would be
discussing with A.B. the importance of him sticking to a heart healthy diet. He stated that when
he had his heart valve replacement he stuck to a healthy diet for many years, and just recently
started eating non-healthy choices within the past few years.
ACUTE MI 22
Prevention/ Plan: The plan would be to keep patient on Coumadin therapy in order to come to a
therapeutic level to prevent future MIs. Also, patient will have to continue with other
medications that were prescribed in the hospital because of his new diagnosis of heart failure.
Since the patient is becoming very dyspneic with activity and is having a hard time coming to
terms with his diagnosis, cardiac rehab should be highly considered for this individual in order to
reach a positive and functional outcome. Home care should also be considered for the first few
months since the patient was told by his doctor to take off work and to take it easy until he
reaches a more functional level to complete everyday tasks. Also, it would be important for the
patient to stick to his heart healthy diet and sodium restriction. This nutritional change will help
in the prevention of a future MI as well. Patient may also need spiritual support since his daily
role has changed. The overall goal for this patient would be to prevent future MIs and to increase
his level of functioning as much as possible.
Priority NANDAs, NICs, and NOCs:
1.) NANDA:
Cardiac output decreased, related to impaired contractility, as evidence by decreased
activity tolerance, diminished peripheral pulses, and ejection fraction less than 40%.
NIC:
Administer medications as ordered, administer oxygen as ordered, assess for chest pain,
assess heart rate/rhythm, assess respiratory rate/rhythm, auscultate apical pulse, maintain
optimal fluid balance, monitor daily weights, monitor EKG, monitor intake and output,
monitor pulse oximetry, monitor telemetry, arrange for cardiac rehab for the patient.
ACUTE MI 23
NOC:
Expected outcome would be that the patient will have an increased cardiac output
2.) NANDA:
Acute pain, related to MI and heart catheterization, as evidence by reports of pain by the
patient.
NIC:
Administer analgesics as ordered, assess for cause of pain, assess pain score using a
standardized pain scale, encourage use of non-pharmacological measure such as massage,
relaxation techniques, and compress, evaluate response to pain, and monitor
signs/symptoms associated with pain
NOC:
Expected outcome would be that the patient will have a decrease in painful stimuli, and
feel more comfortable during his hospital stay.
NANDA:
Risk for Falls, related to gait instability, limited mobility, and medications, as evidence
by observing the patients gait and stability.
NIC:
Bed in low position/side rails up, assess safety needs, call light within reach, floor
uncluttered, ensure appropriate room lighting
ACUTE MI 24
NOC:
Expected outcome is that the patient will not experience any falls throughout his hospital
stay.
NANDA:
Anxiety, related to hospital stay from myocardial infarction, as evidence by patient
stating I am nervous and anxious as to what will happen next.
NIC:
Calming technique, emotional support, coping enhancement, anxiety reduction by
minimizing apprehension related to fearing the unknown.
NOC:
The expected outcome would be that the patient appears and feels less anxious, has the
ability to focus on a specific stimulus, and can cope by managing stressors.
ACUTE MI 25
References
Deglin, J. H., & Vallerand, A. H. (2011). Davis's drug guide for nurses (12th ed.). Philadelphia:
F.A. Davis.
Ignatavictus, D., & Workman, L. (2010). Medical surgical nursing. (6 ed.). St.Louis, Missouri:
Saunders Elsevier.
Labriolle,, A. D., Bonello, L., & Lemesle, G. (2010). Decline in platelet count in patients treated
by percutaneous coronary intervention: denition, incidence, prognostic importance, and
predictive factors. European Heart Journal, 31, 1079-1087. Retrieved April 14, 2014, from
http://eurheartj.oxfordjournals.org/content/3
Nez, J., Palau, P., Nez, E., Llcer, A., Darmofal, H., Merlos, P., et al. (2010). Low
lymphocyte count in acute phase of ST-segment elevation myocardial infarction predicts
long-term recurrent myocardial infarction. Coronary Artery Disease, 21(1), 1-7.
Pagana, A. D., & Pagana, T. J. (2011). Mosby's diagnostic and laboratory test reference.
(10 ed.). St.Louis, Missouri: Mosby.
What Are the Symptoms of a Heart Attack?. (n.d.). - NHLBI, NIH. Retrieved April 16, 2014,
from https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack/signs.html
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Government College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniqueDocument11 pagesGovernment College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniquepriyankaPas encore d'évaluation
- Canon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFDocument13 pagesCanon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFRita CaselliPas encore d'évaluation
- Cambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022Document15 pagesCambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022ilovefettuccinePas encore d'évaluation
- Music 10 (2nd Quarter)Document8 pagesMusic 10 (2nd Quarter)Dafchen Villarin MahasolPas encore d'évaluation
- Biography Thesis ExamplesDocument7 pagesBiography Thesis Examplesreneewardowskisterlingheights100% (2)
- ChatGpt PDFDocument19 pagesChatGpt PDFsanx2014100% (1)
- Chapter 4 Achieving Clarity and Limiting Paragraph LengthDocument1 pageChapter 4 Achieving Clarity and Limiting Paragraph Lengthapi-550339812Pas encore d'évaluation
- PFEIFER Angled Loops For Hollow Core Slabs: Item-No. 05.023Document1 pagePFEIFER Angled Loops For Hollow Core Slabs: Item-No. 05.023adyhugoPas encore d'évaluation
- SLA in PEGA How To Configue Service Level Agreement - HKRDocument7 pagesSLA in PEGA How To Configue Service Level Agreement - HKRsridhar varmaPas encore d'évaluation
- Canoe Matlab 001Document58 pagesCanoe Matlab 001Coolboy RoadsterPas encore d'évaluation
- Mosfet Irfz44Document8 pagesMosfet Irfz44huynhsang1979Pas encore d'évaluation
- rp10 PDFDocument77 pagesrp10 PDFRobson DiasPas encore d'évaluation
- TriPac EVOLUTION Operators Manual 55711 19 OP Rev. 0-06-13Document68 pagesTriPac EVOLUTION Operators Manual 55711 19 OP Rev. 0-06-13Ariel Noya100% (1)
- Rom 2 - 0-11 (En)Document132 pagesRom 2 - 0-11 (En)Mara HerreraPas encore d'évaluation
- Antena TelnetDocument4 pagesAntena TelnetMarco PiambaPas encore d'évaluation
- Building Services Planning Manual-2007Document122 pagesBuilding Services Planning Manual-2007razanmrm90% (10)
- WBDocument59 pagesWBsahil.singhPas encore d'évaluation
- Astm B19Document6 pagesAstm B19Davor IbarraPas encore d'évaluation
- Assignment of Chemistry For B.sc-B.ed First Semester Session 2019-2023-1Document2 pagesAssignment of Chemistry For B.sc-B.ed First Semester Session 2019-2023-1Payal sahaPas encore d'évaluation
- Kyle Pape - Between Queer Theory and Native Studies, A Potential For CollaborationDocument16 pagesKyle Pape - Between Queer Theory and Native Studies, A Potential For CollaborationRafael Alarcón Vidal100% (1)
- MultiLoadII Mobile Quick Start PDFDocument10 pagesMultiLoadII Mobile Quick Start PDFAndrés ColmenaresPas encore d'évaluation
- NCP - Major Depressive DisorderDocument7 pagesNCP - Major Depressive DisorderJaylord Verazon100% (1)
- Presentation About GyroscopesDocument24 pagesPresentation About GyroscopesgeenjunkmailPas encore d'évaluation
- Test 51Document7 pagesTest 51Nguyễn Hiền Giang AnhPas encore d'évaluation
- Phytotherapy On CancerDocument21 pagesPhytotherapy On CancerSiddhendu Bhattacharjee100% (1)
- DLP - Light Science 7Document6 pagesDLP - Light Science 7Samara M. SalacayanPas encore d'évaluation
- Durex 'S Marketing Strategy in VietnamDocument45 pagesDurex 'S Marketing Strategy in VietnamPham Nguyen KhoiPas encore d'évaluation
- Z-Purlins: Technical DocumentationDocument11 pagesZ-Purlins: Technical Documentationardit bedhiaPas encore d'évaluation
- Micro Lab Midterm Study GuideDocument15 pagesMicro Lab Midterm Study GuideYvette Salomé NievesPas encore d'évaluation
- Acer N300 ManualDocument50 pagesAcer N300 Manualc_formatPas encore d'évaluation