Académique Documents
Professionnel Documents
Culture Documents
Heart Failure Essentials
Transféré par
api-275769355Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Heart Failure Essentials
Transféré par
api-275769355Droits d'auteur :
Formats disponibles
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Breathlessness, a cardinal symptom of LV failure, may manifest with progressively increasing
severity as the following:
Exertional dyspnea/ Orthopnea/ PND/ Dyspnea at rest/ Acute pulmonary edema
Other cardiac symptoms of heart failure include chest pain/pressure and palpitations. Common
noncardiac signs and symptoms of heart failure include anorexia, nausea, weight loss, bloating,
fatigue, weakness, oliguria, nocturia, and cerebral symptoms of varying severity, ranging from
anxiety to memory impairment and confusion.
In the recumbent position, decreased pooling of blood in the lower extremities and abdomen
occurs. Blood is displaced from the extrathoracic compartment to the thoracic compartment. The
failing LV, operating on the flat portion of the Frank-Starling curve, cannot accept and pump out
the extra volume of blood delivered to it without dilating. As a result, pulmonary venous and
capillary pressures rise further, causing interstitial pulmonary edema, reduced pulmonary
compliance, increased airway resistance, and dyspnea.
Cough, particularly during laying down, may be an "orthopnea equivalent."
PND- usually occurs at night and is defined as the sudden awakening of the patient, after a
couple of hours of sleep, with a feeling of severe anxiety, breathlessness, and suffocation. The
patient may sit upright in bed and gasp for breath. Bronchospasm with breathing difficulty could
mimic paroxysmal nocturnal dyspnea. On chest auscultation, the bronchospasm associated with a
heart failure exacerbation can be difficult to distinguish from an acute asthma exacerbation,
although other clues from the cardiovascular examination should lead to the correct diagnosis.
Both types of bronchospasm can be present in a single individual.
In contrast to orthopnea, which may be relieved by immediately sitting up in bed, paroxysmal
nocturnal dyspnea may require 30 minutes or longer in this position for relief.
Dyspnea at rest: Dyspnea at rest in heart failure is the result of the following mechanisms:
Decreased pulmonary function secondary to decreased compliance and increased airway
resistance
Increased ventilatory drive secondary to hypoxemia due to increased pulmonary capillary
wedge pressure (PCWP); ventilation/perfusion (V/Q) mismatching due to increased
PCWP and low cardiac output; and increased carbon dioxide production
Respiratory muscle dysfunction, with decreased respiratory muscle strength, decreased
endurance, and ischemia
Acute Pulmonary Edema: Usually sudden increase in wedge pressures(PCWP >25 mm hg)
Gain of ECF volume (Minimum of 5 L in adults) must occur before peripheral edema develops.
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Level
Description
At high risk for heart
A
failure but without
structural heart disease
or symptoms of heart
failure
Examples
Patients with
CAD/LVH/
HTN/DM, geometric
chamber distortion
Structural heart disease
but without
signs/symptoms of
heart failure
Patients who are
asymptomatic but who
have LVH and/or
impaired LV function
Structural heart disease
with current or past
symptoms of heart
failure
Patients with known
structural heart
disease and shortness
of breath and fatigue,
reduced exercise
tolerance
Patients who have
marked symptoms at
rest despite maximal
medical therapy
Refractory heart
failure requiring
specialized
interventions
Notes
Patients with predisposing risk
factors for developing heart failure
Corresponds with patients with
NYHA class I heart failure
The majority of patients with heart
failure are in this stage
Corresponds with patients with
NYHA class II and III heart failure
Patients in this stage may be
eligible to receive mechanical
circulatory support, receive
continuous inotropic infusions,
undergo procedures to facilitate
fluid removal, or undergo heart
transplantation or other procedures
Corresponds with patients with
NYHA class IV heart failure
Stage A: Management focuses on prevention, through reduction of risk factors.
Treat hypertension/ Encourage smoking cessation/Treat lipid disorders
Encourage regular exercise
Discourage alcohol intake and illicit drug use
Patients who have a family history of dilated cardiomyopathy should be screened with a
comprehensive history and physical examination together with echocardiography and
transthoracic echocardiography every 2-5 years.
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Stage B: Patients are asymptomatic, with LV dysfunction from previous MI, LV remodeling
from LV hypertrophy, and asymptomatic valvular dysfunction, which includes NYHA
I.Treatment with an ACEI/ARB and/or beta-blockade is indicated.
Evaluation for coronary revascularization either percutaneously or surgically, as well as
correction of valvular abnormalities, may be indicated. Treatment with an ICD for primary
prevention of sudden death in patients with an LVEF of less than 30% that is more than 40 days
post-MI is reasonable if expected survival is more than 1 year.
There is less evidence for implantation of an ICD in patients with nonischemic cardiomyopathy,
an LVEF less than 30%, and no heart failure symptoms. There is no evidence for use of digoxin
in these populations. Aldosterone receptor blockade with eplerenone is indicated for post-MI LV
dysfunction.
Stage C: Corresponds with NYHA class II and III heart failure. Drugs routinely used in these
patients include ACEI/ARBs, beta-blockers, and loop diuretics for fluid retention. For selected
patients, therapeutic measures include aldosterone receptor blockers, hydralazine and nitrates in
combination, and cardiac resynchronization with or without an ICD.
A meta-analysis performed by Badve et al suggested that the survival benefit of treatment with
beta-blockers extends to patients with chronic kidney disease and systolic heart failure (risk ratio
0.72).
Stage D: Refractory heart failure (NYHA class IV) that requires specialized interventions.
Treatment includes all the measures used in stages A, B, and C. Treatment considerations
include heart transplantation or placement of an LV assist device in eligible patients; pulmonary
catheterization; and options for end-of-life care. For palliation of symptoms, positive inotrope
may be considered.
Evidence-Based BNP and NT-proBNP Cutoff Values for Diagnosing HF
Criterion
>17
>21
2150
5075
>75
Estimated
GFR,
< 60 mL/min
Age,
y
BNP, pg/mL
HF Unlikely (LR- HF Likely (LRNegative)
Positive)
< 100 (0.13)*
>500 (8.1)*
-
NT-proBNP, pg/mL
HF Unlikely (LR- HF Likely (LRNegative)
Positive)
< 300 (0.02)
>450 (14)
>900 (5.0)
< 200 (0.13)
>500 (9.3)
>1800 (3.1)
-
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Besides standard tests for heart failure- below mentioned studies may be indicated in selected
patients.
Screening for hemochromatosis, in which iron overload affects cardiac function
Screening for sleep-disturbed breathing, which affects neurohormonal activation
Screening for human immunodeficiency virus (HIV), which may result in heart failure
from possible direct infectious effects, from disease treatment effects causing CAD
Testing for rheumatologic diseases, amyloidosis, or pheochromocytoma, all of which
may cause cardiomyopathy
Serum and urine electrophoresis for light-chain disease
Genetic testing for at-risk patients with a first-degree relative who has been diagnosed
with a cardiomyopathy leading to heart failure, which may aid in detecting early disease
onset and guide treatment
Holter monitoring, which may reveal arrhythmias or abnormal electrical activity (eg, in
patients with heart failure and a history of MI who are being considered for
electrophysiologic study to document ventricular tachycardia [VT] inducibility)
BNP is mostly limited to the differentiation of heart failure versus other causes of dyspnea in
patients with an atypical presentation.
Plasma BNP comes from cardiac ventricles, and the release of BNP appears to be in direct
proportion to ventricular volume and pressure overload. BNP is an independent predictor of high
LV end-diastolic pressure and is more useful than atrial natriuretic peptide (ANP) or
norepinephrine levels for assessing mortality risk in patients with heart failure.
BNPep has been determined to be the strongest predictor of systolic versus nonsystolic heart
failure (followed by oxygen saturation, history of myocardial infarction, and heart rate), BNP
does not reliably differentiate between heart failure with preserved ejection fraction and heart
failure with reduced ejection fraction. Increased NT-proBNP was found to be the strongest
independent predictor of a final diagnosis of acute heart failure.
BNP levels >100 pg/mL - specificity > 95% and a sensitivity > 98% when comparing patients
without heart failure to all patients with heart failure. Even BNP levels greater than 80 pg/mL
have a specificity greater than 95% and a sensitivity greater than 98% in the diagnosis of heart
failure
BNP and NT-proBNP levels are higher in older patients/ women/ Renal dysfunction and sepsis.
Atrial fibrillation has also been associated with increased BNP levels in the absence of acute
heart failure.
BNP levels may be disproportionately low in obese individuals due to fat metabolism or who
have hypothyroidism or advanced end-stage heart failure (the latter due to increased fibrosis).
NT-proBNP plasma levels are also lower in obese heart failure patients relative to nonobese
patients with heart failure, regardless of whether the etiology is ischemic or nonischaemic.
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Functional Capacity
The European Society of Cardiology (ESC) indicates the 6-minute walk test is a good indicator
of functional status and prognosis in patients with heart failure. It evaluates distance walked,
dyspnea index on a Borg scale from 0 to 10, oxygen saturation, and heart rate response to
exercise. A normal value is walking more than 1500 feet. Patients who walk less than 600 feet
have severe cardiac dysfunction and a worse short- and long-term prognosis.
Cardiopulmonary stress testing (maximal exercise stress testing with measurement of respiratory
gas exchange) can help assess a patients chance of survival within the next year, as well as
determine the need for referral for either cardiac transplantation or implantation of mechanical
circulatory support.ACC/AHA do not recommend routine maximal exercise stress testing but it
may be useful in situations such as the following with measurement of gas exchange:
To distinguish non HF-related causes of functional limitation, specifically cardiac versus
pulmonary
To consider whether patients are candidates for cardiac transplantation or mechanical
circulatory support
To determine the prescription for cardiac rehabilitation
The Heart Failure Society of America (HFSA) suggests that endomyocardial biopsy be
considered in patients with rapidly progressive clinical heart failure or ventricular dysfunction,
despite appropriate medical therapy, as well as in patients suspected of having myocardial
infiltrative processes (eg, sarcoidosis, amyloidosis) or in patients with malignant arrhythmias out
of proportion to their LV dysfunction (eg, sarcoidosis, giant cell myocarditis).
ACC/AHA/HFSA/ESC recommends cardiac catheterization and coronary angiography be
considered for patients with heart failure in the following situations:
When symptoms worsen without a clear cause in patients with heart failure,without
angina, and known coronary artery disease
In heart failure caused by systolic dysfunction in association with angina or regional
wall-motion abnormalities and/or scintigraphic evidence of reversible myocardial
ischemia when revascularization is being considered
When pretest probability of underlying ischemic cardiomyopathy is high and surgical
coronary procedures are being considered
Before cardiac transplantation or left ventricular assist device placement
In cases of heart failure secondary to postinfarction ventricular aneurysm or other
mechanical complications of myocardial infarction
Genetic testing has the highest yield in 3 types of cardiomyopathy: DCM, HCM, and autosomal
dominant ARVD/C. The diagnosis must be established using the specific criteria for each type of
cardiomyopathy, as the genetic testing is different for each type.
The Heart Failure Society of America (HFSA) also has the following recommendations for
genetic evaluation of cardiomyopathy :
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
For all patients with cardiomyopathy, take a detailed family history for at least 3
generations (hypertrophic cardiomyopathy [HCM], dilated cardiomyopathy [DCM],
arrhythmic right ventricular dysplasia [ARVD], left ventricular noncompaction [LVNC],
restrictive cardiomyopathy [RCM], and cardiomyopathies associated with extra-cardiac
manifestations)
Carefully assess the patient's medical history as well as that of asymptomatic first-degree
relatives, with special focus on heart failure symptoms, arrhythmias, presyncope, and
syncope
Screen asymptomatic first-degree relatives for cardiomyopathy (HCM, DCM, ARVD,
LVNC, RCM, and cardiomyopathies associated with extra-cardiac manifestations)
20-50% of idiopathic dilated cardiomyopathy (IDC) may have a genetic basis. Screening firstdegree relatives of a proband with IDC by echocardiography and electrocardiography (ECG)
reveals that 20-48% of probands have affected relatives, consistent with a diagnosis of familial
dilated cardiomyopathy .
HCM, caused by mutation in one of the genes currently known to encode different components
of the sarcomere, is characterized by left ventricular hypertrophy (LVH) in the absence of
predisposing cardiac conditions (eg, aortic stenosis) or cardiovascular conditions (eg, longstanding hypertension).
Autosomal dominant arrhythmogenic right ventricular dysplasia/cardiomyopathy
ARVD is characterized by progressive fibrofatty replacement of the myocardium that
predisposes to ventricular tachycardia and sudden death in young individuals and athletes. It
primarily affects the right ventricle; with time, it may also involve the left ventricle. The
presentation of disease is highly variable even within families, and affected individuals may not
meet established clinical criteria. The mean age at diagnosis is 31 years (13 y; range, 4-64 y).
Management: Multimodal approach( Non pharmacologic/Phramacologic) and Invasive.
Managing other comorbidities including anemia/ CAD/OSA/A fib,.
Atrial fibrillation: Most patients with heart failures also have A fib. AFFIRM trial, there was no
difference in stroke, heart failure exacerbation, or CV mortality in patients treated with rhythm
control (amiodarone) and patients treated with rate control. All of these patients require
anticoagulation for stroke prevention. This can be achieved by using warfarin or a direct
thrombin inhibitor.
Cardiorenal syndrome
Cardiorenal syndrome reflects advanced cardiorenal dysregulation manifested by acute heart
failure, worsening renal function, and diuretic resistance. It is equally prevalent in patients with
heart failure with normal ejection fraction (HFNEF) and those with LV systolic dysfunction.
Worsening renal function is one of the 3 predictors of increased mortality in hospitalized patients
with heart failure regardless of the LVEF.
Cardiorenal syndrome can be classified into the following 5 types:
6
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Type1: rapid worsening of cardiac function leading to acute kidney injury (HFNEF, acute
heart failure, cardiogenic shock, and RV failure)
Type2: worsening renal function due to progression of chronic heart failure
Type3: abrupt and primary worsening of kidney function leading to acute cardiac
dysfunction (heart failure, arrhythmia, ischemia)
Type4: chronic kidney disease leading to progressive cardiac dysfunction, LVH, and
diastolic dysfunction
Type5: combination of cardiac and renal dysfunction due to acute and chronic systemic
conditions(sepsis)
The pathophysiology of CR1 and CR2 is complex and multifactorial, involving neurohormonal
activation (RAAS, sympathetic nervous system, arginine vasopressin, natriuretic peptides,
adenosine receptor activation), low arterial pressure, and high central venous pressure, leading to
lower transglomerular perfusion pressure and decreased availability of diuretics to the proximal
nephron. This results in an increased reabsorption of sodium and water and poor diuretic
responsehence, diuretic resistance despite escalating doses of oral or intravenous diuretics.
Treatment of cardiorenal syndrome in patients with heart failure is largely empirical, but it
typically involves the use of combination diuretics, vasodilators, and inotropes as indicated.
Ultrafiltration is recommended for symptomatic relief by the ACC/AHA guidelines for patients
with heart failure that is refractory to diuretic therapy.
A sudden increase in creatinine can be seen after initiation of diuretic therapy and is often
mistakenly considered evidence of overdiuresis or intravascular depletion (even in the presence
of fluid overload). A common error in this situation is to decrease the dose of ACEI/ARB and/or
diuretics or to even withdraw one of these agents. In fact, when diuresis or ultrafiltration is
continued, patients demonstrate improved renal function, decreased total body fluid, and
increased response to diuretics, as central venous pressure falls.
**Low dose dopamine and lasix infusion- Some benefits in acute heart failure by improving
renal perfusion.
**The Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan
(EVEREST) trial showed that the addition of the vasopressin antagonist tolvaptan to diuretic
therapy facilitates diuresis in acute heart failure. However, tolvaptan had no impact on mortality
or hospitalizations in this setting.
**Adenosine receptor antagonists have been proposed for protecting renal function in acute heart
failure. However, in a double-blind, placebo-controlled trial, the adenosine A1 receptor
antagonist rolofylline demonstrated no benefit for patients hospitalized for acute heart failure
with impaired renal function.
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) updated
guidelines, and the 2008 European Society of Cardiology (ESC) guidelines, with varying levels
of evidence, recommend the following:
Diuretics (to reduce edema by reduction of blood volume and venous pressures) and salt
restriction (to reduce fluid retention) in patients with current or previous heart failure
symptoms and reduced left ventricular ejection fraction (LVEF) for symptomatic relief
Angiotensin-converting enzyme inhibitors (ACEIs) for neurohormonal modification,
vasodilatation, improvement in LVEF, and survival benefit
Angiotensin receptor blockers (ARBs) for neurohormonal modification, vasodilatation,
improvement in LVEF, and survival benefit
Hydralazine and nitrates to improve symptoms, ventricular function, exercise capacity,
and survival in patients who cannot tolerate an ACEI/ARB or as an add-on therapy to
ACEI/ARB and beta-blockers in the black population for survival benefit
Beta-adrenergic blockers for neurohormonal modification, improvement in symptoms
and LVEF, survival benefit, arrhythmia prevention, and control of ventricular rate
Aldosterone antagonists, as an adjunct to other drugs for additive diuresis, heart failure
symptom control, improved heart rate variability, decreased ventricular arrhythmias,
reduction in cardiac workload, improved LVEF, and increase in survival
Digoxin, which can lead to a small increase in cardiac output, improvement in heart
failure symptoms without any mortality benefit.
Anticoagulants to decrease the risk of thromboembolism
Inotropic agents to restore organ perfusion and reduce congestion
Patients with heart failure and depressed LVEF are thought to have an increased risk of thrombus
formation due to low cardiac output. Anticoagulation with an international normalized ratio
(INR) goal of 2-3 is indicated in the presence of left ventricular (LV) thrombus, thromboembolic
event with or without evidence of an LV thrombus, and paroxysmal or chronic atrial
arrhythmias.
Routine anticoagulation with warfarin in patients with normal sinus rhythm, heart failure, and
LV dysfunction has proven not to be superior to aspirin alone in decreasing death, myocardial
infarction (MI), and stroke and was associated with an increased risk of bleeding in the
Coumadin arm of the WATCH trial.
The use of regularly scheduled intermittent intravenous infusions of positive inotropic drugs is
not advisable, given the lack of evidence to support efficacy and concerns about toxicity with an
increase in mortality rate. Rather, the guidelines recommend infusion of a positive inotrope only
as palliation in patients with end-stage disease who cannot be stabilized with standard medical
treatment.
The ACC/AHA guidelines advise that nonsteroidal anti-inflammatory drugs (NSAIDs), calcium
channel blockers, and most antiarrhythmic agents may exacerbate heart failure and should be
avoided in most patients. NSAIDs can cause sodium retention and peripheral vasoconstriction
and can attenuate the efficacy and enhance the toxicity of diuretics and ACEIs.
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Antiarrhythmic agents can have cardiodepressant effects and may promote arrhythmia; only
amiodarone and dofetilide have been shown not to adversely affect survival. Calcium channel
blockers can worsen heart failure and may increase the risk of cardiovascular events; only the
vasoselective calcium channel blockers have been shown not to adversely affect survival.
Digoxin currently occupies places in both US and European guidelines as no more than a
second-line agent for systolic HF. It has not shown to reduce mortality or hospital admissions.
Most patients who present with acute heart failure have exacerbation of chronic heart failure,
with only 15-20% having acute heart failure. Approximately 50% of patients with acute heart
failure have a preserved LVEF (>40%). Less than 5% of patients presenting with acute heart
failure are hypotensive and require inotropic therapy. Pulmonary edema is a medical emergency,
but it is only one of the presentations of acute heart failure.
A systematic and expeditious approach to management of acute heart failure is required, starting
in the outpatient setting (eg, emergency department, urgent care center, office), continuing
during hospitalization, and extending after discharge to the outpatient setting. The clinicians
agenda in these cases is threefold:
Stabilize the patients clinical condition
Establish the diagnosis, etiology, and precipitating factors
Initiate therapies to rapidly provide symptom relief
Administration of oxygen, if oxygen saturation is less than 90%, and noninvasive positive
pressure ventilation (NIPPV) provides patients with respiratory support to avoid intubation.
NIPPV has been shown to decrease the rate of intubation, hospital mortality, and mechanical
ventilation. No difference has been noted between continuous positive airway pressure (CPAP)
and bilevel positive airway pressure (BiPAP). A prospective randomized trial that compared the
use of noninvasive ventilation (NIV) and standard therapy with the use of standard therapy alone
suggested that although NIV may improve dyspnea and respiratory acidosis, it does not appear to
improve mortality.
Medical therapy for heart failure patients, the majority who present with normal perfusion and
evidence of congestion, focuses on the following goals:
Preload and afterload reduction for symptomatic relief using vasodilators (nitrates,
hydralazine, nipride, nesiritide, ACEI/ARB) and diuretics
Inhibition of deleterious neurohormonal activation (renin-angiotensin-aldosterone system
[RAAS] and sympathetic nervous system) using ACEI/ARB, beta-blockers, and
aldosterone antagonists resulting in long-term survival benefit
Preload reduction results in decreased pulmonary capillary hydrostatic pressure and reduction of
fluid transudation into the pulmonary interstitium and alveoli. Preload and afterload reduction
provide symptomatic relief. Inhibition of the RAAS and sympathetic nervous system produces
vasodilation, thereby increasing cardiac output and decreasing myocardial oxygen demand.
Diuretics are effective in preload reduction by increasing urinary sodium excretion and
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
decreasing fluid retention, with improvement in cardiac function, symptoms, and exercise
tolerance.
Once congestion is minimized, a combination of 3 types of drugs (a diuretic, an ACEI or an
ARB, and a beta-blocker) is recommended in the routine management of most patients with heart
failure. This combination can accomplish all of the above goals. ACEIs/ARBs and beta-blockers
are generally used together. Beta-blockers are started in the hospital once euvolemic status has
been achieved.
If there is evidence of organ hypoperfusion, use of inotropic therapies and/or mechanical
circulatory support (eg, intra-aortic balloon pump, extracorporeal membrane oxygenator
[ECMO], left ventricular assist device [LVAD]) and continuous hemodynamic monitoring are
indicated. If arrhythmia is present and if uncontrolled ventricular response is thought to
contribute to the clinical scenario of acute heart failure, either pharmacologic rate control or
emergent cardioversion with restoration of sinus rhythm is recommended.
Diuretics: Cornerstone of standard therapy for acute heart failure. In such patients, IV
administration of a loop diuretic (ie, furosemide, bumetanide, torsemide) is preferred initially
because of potentially poor absorption of the oral form in the presence of bowel edema.
Diuretics can be given by bolus or continuous infusion and in high or low doses. In a study of
patients with acute decompensated heart failure, Felker et al found that there were no significant
differences in effect on symptoms or renal function changes with furosemide given either by
bolus or by continuous infusion; additionally, no differences were found with high versus low
doses. The dose and frequency of administration depend on the diuretic response 2-4 hours after
the first dose is given. If the response is inadequate, then increasing the dose and/or increasing
the frequency can help enhance diuresis.
Diuretic resistance is diagnosed if there is persistent pulmonary edema despite the following :
Repeated doses of 80 mg of furosemide or
Greater than 240 mg of furosemide per day (including continuous furosemide infusion)
or
Combined diuretic therapy (including loop diuretics with thiazide or an aldosterone
antagonist)
Volume status, sodium levels, water intake, and hemodynamic status (for signs of poor
perfusion) need to be reevaluated in case of diuretic resistance. Diuretic resistance is a known
effect of long-term use of diuretics; some approaches to managing resistance to these agents
include increasing the dose and/or frequency of the drug, restricting sodium or water intake,
administering the drug as an IV bolus or IV infusion, and combining diuretics. In addition,
diuretic resistance is an independent predictor of mortality in patients with chronic heart failure.
Eventually, hemodialysis or ultrafiltration, may be used to overcome it. Other agents, such as
vasopressin antagonists(v2r) can be used to assist diuretics.
Transition to oral diuretic therapy is made when the patient reaches a near-euvolemic state. The
oral diuretic dose is usually equal to the IV dose. In most cases, 40 mg/day of furosemide is
10
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
equivalent to 20 mg of torsemide and 1 mg of bumetanide. Weight, signs and symptoms, fluid
balance, electrolyte levels, and renal function have to be monitored carefully on a daily basis.
Vasodilators: Nitrates are potent venodilators. They decrease preload and therefore decrease LV
filling pressure and relieve shortness of breath. They also selectively produce epicardial coronary
artery vasodilatation and help with myocardial ischemia. Although nitrates can be used in
different forms (sublingual, oral, transdermal, IV), the most common route in acute heart failure
is IV. Their use is limited by tachyphylaxis and headache.
Sodium nitroprusside is a potent, primarily arterial, vasodilator resulting in a very efficient
afterload reduction and decrease of intracardiac filling pressures. This agent is particularly
helpful for patients who present with severe pulmonary congestion in the presence of
hypertension and severe mitral regurgitation. Sodium nitroprusside requires not only careful
hemodynamic monitoring, often requiring indwelling catheters, but also monitoring for cyanide
toxicity, especially in the presence of renal dysfunction. The drug should be titrated to off rather
than abruptly stopped because of the potential for rebound hypertension.
Ultrafiltration and refractory heart failure
Ultrafiltration was shown to be an effective alternative to intravenous diuretics in the
Ultrafiltration Versus Intravenous (IV) Diuretics for Patients Hospitalized for Acute
Decompensated Heart Failure (UNLOAD) trial. The ACC/AHA and ESC recommend the use of
ultrafiltration for fluid reduction for patients with refractory heart failure that is not responsive to
medical therapy.
Invasive hemodynamic monitoring
Invasive hemodynamic monitoring is not indicated for stable patients with heart failure
responding appropriately to medical therapy. The Evaluation Study of Congestive Heart Failure
and Pulmonary Artery Catheterization Effectiveness [ESCAPE] trial showed no mortality or
hospitalization benefit in such cases. In patients with acute decompensated heart failure, the
following are indications for invasive hemodynamic monitoring:
Respiratory distress
Signs of impaired perfusion
Inability to determine intracardiac pressures on the basis of clinical examination
No improvement in clinical status despite maximal heart failure therapy
Clinical situations in which invasive hemodynamic monitoring is recommended to guide therapy
include the following :
Persistent symptomatic hypotension despite initial therapy
Worsening renal function despite initial therapy or despite adjustment of recommended
therapies
Need for parenteral vasoactive agents after initial clinical improvement
Presumed cardiogenic shock requiring escalating inotrope and/or pressor therapy and
consideration of mechanical support
Consideration of advanced device therapy or transplantation
11
Heart Failure Essentials for residents/ Dr Subramanian MD FACP
Discharge: The patient must be on a stable oral regimen for at least 24 hours before discharge.
Patients are ready for discharge when they meet the following criteria:
Exacerbating factors have been addressed
Volume status has been optimized
Diuretic therapy has been successfully transitioned to oral medication, with
discontinuation of IV vasodilator and inotropic therapy for at least 24 hours
Oral chronic heart failure therapy has been achieved with stable clinical status
Before discharge, patient and family education should be completed, and extensive postdischarge
instructions and follow-up in 3-7 days should be arranged. Refractory end-stage heart failure
(ACC/AHA stage D, NYHA class IV) is often difficult to manage on an outpatient basis.
Therefore, these patients may be referred to a heart failure program with expertise in
management of refractory heart failure.
To ensure compliance and understanding of a complex medical regimen, a follow-up phone call
can be made 3 days after discharge by a nurse with training in heart failure. Ideally, the patient
should be seen in clinic 7-10 days after discharge.
Different monitoring methods have been implemented by physicians in an attempt to reduce
hospitalization for heart failure. The results have been equivocal, regardless of the severity of
heart failure. No differences in death or hospitalization for heart failure have been found with
either standard outpatient monitoring or intense telemonitoring for heart failure.
An investigational approach to monitoring is the use of a wireless implanted pulmonary artery
pressure sensor. This device permits ambulatory monitoring and is designed to detect early-stage
elevations in pulmonary artery pressure, so that appropriate medical intervention can be provided
before worsening elevation leads to congestion. In a 6-month study in patients with NYHA class
III heart failure, heart failurerelated hospitalizations were approximately 30% lower with use of
the device.
FDA Approval- First permanently implantable wireless hemodynamic monitoring system
(CardioMEMS HF System) for patients with NYHA class III heart failure who have been
hospitalized within the past year. 550 patients from the open-label CHAMPION study
(CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA
Class III Heart Failure Patients), in which the device reduced hospitalizations by 30% compared
with standard care. Measures PA pressures (eg, systolic, diastolic, and mean) heart rate, and
consists of a sensor/monitor implanted permanently in the PA, a transvenous catheter to deploy
the sensor within the distal PA, and an electronics system that acquires and processes the signal
from the sensor/monitor and transfers PA measurements to a secure database.
End-stage heart failure occurs despite maximal medical therapy-> poor prognosis, and when
there is no viable alternative, standard for therapy has been heart transplantation. Discussion
should include palliative and hospice care for appropriate patients. However, mechanical
circulatory devices such as VADs and total artificial hearts (TAHs) can bridge the patient to
transplantation; VADs are increasingly being used as permanent therapy.
12
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Iso 20816 8 2018 en PDFDocument11 pagesIso 20816 8 2018 en PDFEdwin Bermejo75% (4)
- Average Waves in Unprotected Waters by Anne Tyler - Summary PDFDocument1 pageAverage Waves in Unprotected Waters by Anne Tyler - Summary PDFRK PADHI0% (1)
- BGL01 - 05Document58 pagesBGL01 - 05udayagb9443Pas encore d'évaluation
- Database Programming With SQL Section 2 QuizDocument6 pagesDatabase Programming With SQL Section 2 QuizJosé Obeniel LópezPas encore d'évaluation
- The Handmaid's Tale - Chapter 2.2Document1 pageThe Handmaid's Tale - Chapter 2.2amber_straussPas encore d'évaluation
- Unidad 12 (libro-PowerPoint)Document5 pagesUnidad 12 (libro-PowerPoint)Franklin Suarez.HPas encore d'évaluation
- What Is Thesis Plural FormDocument8 pagesWhat Is Thesis Plural Formtracyjimenezstamford100% (2)
- Action List 50Document4 pagesAction List 50hdfcblgoaPas encore d'évaluation
- Music 20 Century: What You Need To Know?Document8 pagesMusic 20 Century: What You Need To Know?Reinrick MejicoPas encore d'évaluation
- Binary SearchDocument13 pagesBinary SearchASasSPas encore d'évaluation
- Approaches To Violence in IndiaDocument17 pagesApproaches To Violence in IndiaDeepa BhatiaPas encore d'évaluation
- Delaware Met CSAC Initial Meeting ReportDocument20 pagesDelaware Met CSAC Initial Meeting ReportKevinOhlandtPas encore d'évaluation
- D5 PROF. ED in Mastery Learning The DefinitionDocument12 pagesD5 PROF. ED in Mastery Learning The DefinitionMarrah TenorioPas encore d'évaluation
- 2nd Form Sequence of WorkDocument7 pages2nd Form Sequence of WorkEustace DavorenPas encore d'évaluation
- Urinary Tract Infection in Children: CC MagbanuaDocument52 pagesUrinary Tract Infection in Children: CC MagbanuaVanessa YunquePas encore d'évaluation
- Claribel Ria MaeDocument19 pagesClaribel Ria MaeGLENN MENDOZAPas encore d'évaluation
- Trigonometry Primer Problem Set Solns PDFDocument80 pagesTrigonometry Primer Problem Set Solns PDFderenz30Pas encore d'évaluation
- Business Administration: Hints TipsDocument11 pagesBusiness Administration: Hints Tipsboca ratonPas encore d'évaluation
- Some Problems in Determining The Origin of The Philippine Word Mutya' or Mutia'Document34 pagesSome Problems in Determining The Origin of The Philippine Word Mutya' or Mutia'Irma ramosPas encore d'évaluation
- 2501 Mathematics Paper+with+solution EveningDocument10 pages2501 Mathematics Paper+with+solution EveningNenavath GaneshPas encore d'évaluation
- Favis vs. Mun. of SabanganDocument5 pagesFavis vs. Mun. of SabanganAyra CadigalPas encore d'évaluation
- Site Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerDocument95 pagesSite Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerKodhamagulla SudheerPas encore d'évaluation
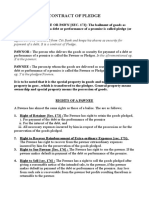
- Contract of PledgeDocument4 pagesContract of Pledgeshreya patilPas encore d'évaluation
- Capstone Report FormatDocument11 pagesCapstone Report FormatAnkush PalPas encore d'évaluation
- The Gower Handbook of Project Management: Part 1: ProjectsDocument2 pagesThe Gower Handbook of Project Management: Part 1: ProjectschineduPas encore d'évaluation
- Research PresentationDocument11 pagesResearch PresentationTeano Jr. Carmelo C.Pas encore d'évaluation
- MOA Agri BaseDocument6 pagesMOA Agri BaseRodj Eli Mikael Viernes-IncognitoPas encore d'évaluation
- 25 ConstitutionDocument150 pages25 ConstitutionSaddy MehmoodbuttPas encore d'évaluation
- Chapter 3 - the-WPS OfficeDocument15 pagesChapter 3 - the-WPS Officekyoshiro RyotaPas encore d'évaluation
- Supporting References in Release 12 SLA PDFDocument8 pagesSupporting References in Release 12 SLA PDFsoireePas encore d'évaluation