Académique Documents
Professionnel Documents
Culture Documents
Mitchell, C - Occupational Profile and Intervention Plan Edit 1
Transféré par
api-238460511Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Mitchell, C - Occupational Profile and Intervention Plan Edit 1
Transféré par
api-238460511Droits d'auteur :
Formats disponibles
Running head: OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Occupational Profile and Intervention Plan
Sam Mitchell
Touro University Nevada
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Occupational Profile
Pete is a 65 year old pleasant man with a robust medical history. His past medical history
includes chronic obstructive pulmonary disease (COPD), coronary artery disease,
cerebrovascular accident (CVA), diabetes, hypertension, and a colostomy. In June of this year,
Pete was admitted to the hospital for a bowel obstruction, while in the hospital he suffered a right
hemisphere ischemic cerebrovascular accident. He was admitted to Health South Rehabilitation
Hospital six weeks following the CVA. Petes rehabilitation diagnosis is debility. Due to Petes
left side hemiparesis he requires moderate assistance in all transfers and dressing. He requires
minimal assistance in grooming and bed mobility. Pete is right hand dominant, therefore, he is
able to perform many tasks seated using his dominant hand. He is unable to stand independently
due to weakness in his left lower extremity. He has also reported having problems recalling the
correct words, or remembering a specific step when performing tasks that once came natural to
him. Petes current goals are to be able to independently ambulate throughout his home, perform
dressing and grooming tasks, cook for his himself, but ultimately he hopes to return back to
work.
Pete is originally from Hawaii, but has lived in the Las Vegas area for over 40 years. Prior
to his hospitalization, Pete worked as a private investigator. He owns his own business and works
from home. He lives independently in a single story town home. However, following his
discharge he will be moving in with his daughter. She lives in a two story home with her husband
and teenage son. Petes room will be down stairs in the home and is connected to a spacious
bathroom with a walk in shower. Pete also has another child that lives locally that is also able to
help with his care if needed. His daughter works full time as an attorney. She stated that she
would like him to be able to get in and out of bed on his own, as well as dress himself, perform
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
his grooming activities, and be able to move around the home independently. She is willing to
help him shower daily, and is not planning on getting him home care following discharge. Petes
family is very supportive. His daughter has already moved his possessions out of his town home
and into her home. His daughter visits him daily in the hospital and attends his therapy session at
least twice a week.
Pete enjoys bowling, golfing, cooking, and spending time with his family. Prior to his
CVA he bowled for a city league with his daughter and son. He also enjoys cooking for his
family and having them over for Sunday dinner. He is currently not married or in a romantic
relationship. He dedicates a majority of his time to his job. He stated that prior to his stroke he
was often working over 40 hours a week. Pete is a very kind, independent, and a determined
man that has shown great strength throughout his hardships. He is aware of his deficits and is
able to clearly express his expectations for his recovery. His strengths, determination, and family
support will greatly aid him through the rehabilitation process.
Occupational Analysis
Pete was observed during a 90 minute occupational therapy intervention session at Health
South Rehabilitation Hospital. The treatment session took place in his private room and in the
hospitals therapy gym. Pete was located in his room and agreed to work with the occupational
therapist and occupational therapy student. The session began by helping Pete out of bed. Pete
required minimal assistance to transfer supine to edge of bed due to decreased strength on his left
side and verbal queuing to perform the task safely and properly. Pete was able to independently
sit edge of bed. He transferred from the edge of the bed to the wheelchair with moderate
assistance from the therapist. Once in his wheel chair, the therapist asked him to change his
clothes. She retrieved his clothes for him and asked him to change his shirt and pants. He was
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
able to independently remove his pajama t-shirt, but required minimal assistance to put his
affected arm in the arm hole and pull his new shirt over his head. While remaining seated, Pete
was able to remove his pajama pants with minimal assistance. However, he required moderate
assistance in putting his affected leg in the pant hole, standing to pull his pants up, tying his
pants, and putting on his socks and shoes. Once Pete was finished dressing, he performed
grooming activities at the bathroom sink. He began by standing at the sink with moderate
assistance provided by the therapist. He was able to wash his face and comb his hair while
standing for one and a half minutes. He then requested to sit down in his wheelchair to perform
the remainder of the tasks. He required set up to shave using an electric razor and to brush his
teeth. After he finished grooming he agreed to work in the therapy gym. In the therapy gym the
therapist began by having Pete work on upper extremity strengthening exercises while seated in
his wheel chair. He did exercises using a two pound dumbbell in the unaffected arm and no
weight on the affected arm for three repetitions ten times each. Exercise included bicep curls,
bear hugs, wrist turns, and shoulder abduction exercises. After the upper extremity warm up, the
therapist introduced mirror therapy to address compensatory synergy patterns in his affected arm.
The therapist would passively move Petes arm and then instructed him to perform the same
movement and to watch his movements in the mirror. As soon as Pete would show compensatory
synergy patterns the therapist would stop him and have him perform the movement again.
Following ten repetitions using the mirror, the therapist had Pete perform an activity stacking
cones while using the deltoid aid to decrease the weight of his arm when performing the fine
motor tasks.
Pete has suffered a right ischemic cerebrovascular accident. He demonstrates symptoms
including left-side hemiparesis, memory problems, impulsivity, and a decrease in safety
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
awareness. However, deficits in vision, swallowing, or speech have not been noted in his medical
chart. During the occupational therapy treatment session he demonstrated impairments in
activities of daily living including functional mobility, dressing, and personal hygiene and
grooming. The client factors impacted by Petes diagnosis include higher level cognition and
memory. Petes neuromusculoskeletal and movement-related functions have been greatly
impacted since his CVA. His joint mobility, muscle power, muscle tone, and muscle endurance
on the left side of his body interferes with his ability to independently perform his ADLs. The
performance skill that has most impacted Petes occupational performance is his motor skills.
Specifically, he demonstrates problems with alignment, stabilizing, reaching, bending, gripping,
coordinating, walking, and flow of movement. He also shows minimal deficits in process skills
such as sequencing. However, he demonstrates intact social interaction skills. Petes performance
patterns are greatly affected by his physical environment. Since he is currently hospitalized he is
unable to perform his daily routines and personal rituals in the natural environment. He is also
unable to maintain his role as a business owner and private investigator, which is a very
important part of his daily life.
Problem List
Problem statements state the areas of occupation that are limited due to certain underlying
factors. It is a list of problems that can be treated by an occupational therapist and provides a
central understanding of the clients problem areas. Petes functional performance is limited due
to several factors such as left-side hemiparesis, poor dynamic standing balance, decrease safety
awareness, and sequencing deficits.
Problem Statements
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Problem statement one. Client requires Mod (A) for bed to wheelchair transfers due to leftside hemiparesis and a in safety awareness.
Problem statement two. Client requires Mod (A) for LE dressing due to poor dynamic
standing balance and left-side hemiparesis.
Problem statement three. Client requires Min (A) for grooming tasks due to sequencing and
left-side hemiparesis.
Problem statement four. Client requires Mod (A) for shower transfers due to left-side
hemiparesis and a in safety awareness.
Client requires Min (A) for supine to EOB due to left-side hemiparesis and a in safety
awareness.
Problem statement five. Client requires Min (A) in UE dressing due to left-side neglect and
lack of adaptive equipment.
The clients problem statements are prioritized by the problems most greatly inhibiting
him from living independently. In order for Pete to return home he must be able to transfer and
perform his ADLs with modified independence. A majority of Petes problem areas are due to
his left-side hemiparesis, and a decrease in safety awareness. By determining these problem
areas, the occupational therapist will be able to focus on the underlying factors and develop long
and short term goals to improve Petes overall functional performance, thus allowing him to
return home.
Intervention Plan and Outcomes
When writing goals, the occupational therapist must ensure that the goals maintain and
promote function, and prevent dysfunction at all times. Occupational therapy goals are highly
individualized and are based on the clients evident occupational performance problem areas as
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
well as the concerns and priorities of the client. Petes goals have been determined by
information from his medical records, occupational profile, occupational analysis, and his
functional problem statements.
Occupation Therapy Long-term Goal
Client will transfer bed to wheelchair with Mod (I) using FWW within four weeks.
Short-term goal. Client will perform sit to stand with Min (A) using FWW within two
weeks.
Intervention. The approach for this intervention is establish and restore. The
intervention will establish the proper techniques to be used when transferring sit-to-stand or
stand- to-sit. It will help to restore weight-bearing function in the affected lower extremity.
Training Pete in the proper techniques of sit-to-stand and stand-to-sit will ensure his safety and
prevent the risk of falls. Additionally, restoring lower extremity weight bearing will increase
Petes independence in transfers and functional activities. Initially Pete must be educated on the
proper positioning to transfer from sit-to-stand, as well as stand- to-sit. The therapist must
consider the foot position, the starting position of the trunk, the speed of movement, and the
upper limbs in propulsion (Carr & Shepherd, 1998). The therapist will instruct Pete to place his
feet flat on the floor behind his knees, scoot to the edge of his seat and lean forward, to push off
from the bed or walker using his unaffected upper extremity, and to place his affected arm in
front of him when initiating sit-to-stand. A study by Britton, Harris, and Turton (2008) showed
that the implementation of practicing sit-to-stand for 30 minutes, five days a week in addition to
routine therapy showed a ten percent difference in body weight taken through the affected foot
only after one week of practice. Kane and Buckley (2011) expressed the difficulty for patients
following a stroke to control the descent due to compromised muscle strength. They stated that in
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
the initial stages following a stroke, many patients sat by letting go and almost collapsing into a
seated position (Kane and Buckley, 2011). Therefore, practicing stand- to-sit should be done as
often as sit-to stand.
Following blocked repetitive practice of sit-to-stand and stand-to-sit, Pete will participate
in a reaching activity while seated. Practicing forward reaching while seated promotes weightbearing in the affected foot (Dean and Shepherd, 1997). Pete will participate in a bowling
activity that requires him to reach forward and across towards his affected side to retrieve and
roll the bowling ball. Reaching and rolling the ball will be done on the table and on the floor to
promote weight shifting. Dean and Shepherd (1997) administered a study that provided a two
week sitting training protocol that improved sitting ability which was measured by distance
reached and quality of the reaching performance. They also researched the effects of the protocol
on the ability of clients to stand up and walk. The study determined that sitting ability was
significantly improved and the carry over to standing up was evident following the two week
training program (Dean and Shepherd, 1997). During the activity the therapist must provide Pete
with verbal and physical cues to promote weight-bearing on the affected lower extremity while
sitting. Also, Petes feet must be placed flat on the floor, he must be seated on the edge of his
seat, and have proper postural alignment when performing the bowling activity. The main
outcome for this intervention strategy is to improve occupational performance. Providing Pete
with the ability to properly and safely transfer from sit to stand will provide him with the
confidence, strength, and endurance needed to engage in his meaningful occupations and
activities.
Short-term goal. Client will transfer bed to wheelchair with Min (A) within two weeks.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Intervention. The approach for this intervention is establish/restore. The intervention
will establish proper transfer techniques and will help to restore Petes independence in his
occupations. Training him in proper transfer techniques will provide him the skills to safely and
confidently transfer from a wide variety of functional seating surfaces. Lach (2005) reported that
having two or more falls, having feelings of unsteadiness, and reporting fair or poor health status
were risk factors for developing a fear of falling. It is important to implement a program that
addresses fall prevention early in the rehabilitation stage. Pete must be educated on fall risks and
prevention strategies, types of exercises that effectively reduce falls, and proper techniques in his
functional mobility tasks. To ensure proper training the therapist must take into account the
clients learning style and teach the transfer techniques according to his particular learning styles
(Carrier, Levasseur, Bdard & Desrosiers, 2012). Following transfer training the client will then
perform the transfers in order to practice and ensure proper techniques are being used. Bobath
(1990) expressed the need to begin training in transfers from a high seat and progress to a lower
seat. The intervention activity can be graded up by using a variety of functional seating surfaces.
Pete can practice transferring from his wheel chair to a chair with arm rest, to the toilet, shower
chair, standard bed, or onto a couch. The activity can be graded down by using durable medical
equipment including a front wheel walker or grab bars to perform the transfer. It is important to
provide extrinsic feedback during the transfers to provide Pete with knowledge regarding his
performance when transferring. The therapist can also provide physical cueing to ensure
appropriate postural alignment and weight-bearing. The main outcome for this intervention
strategy is to improve occupational performance. Providing Pete with the ability to properly and
safely transfer will provide him with the ability to be independently mobile thus increasing his
occupational performance.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
10
Occupational Therapy Long-term Goal
Client will complete LE dressing with Mod (I) using AE and FWW within four weeks.
Short-term goal. Client will don and doff his socks and shoes with Mod (I) with AE and
extra time within two weeks.
Intervention. The approach for this intervention is establish/restore. The intervention
will establish a new technique for the client to use while performing lower extremity dressing.
By proving the client with the ability to perform this task, it will also restore the clients ability to
independently dress himself. For this intervention the client will be given training on lower body
dressing and the use of adaptive equipment. Providing adequate instruction is a key factor that
influences the use of adaptive devices (Schemm and Gitlin, 1998). The client will be educated
on the proper use of a reacher, dressing stick, pant clip, sock aide, shoe horn and adaptive shoe
laces. Foti and Koketsu (2013) discuss the need for an occupational therapist to explore a variety
of assistive devices in order to find a solution for specific ADL deficits. The therapist will
demonstrate the use of the equipment and teach one handed techniques to use the equipment.
Schemm and Citlin (1998) reported that preparation, interaction, cues, repetition, support, and
rewards are part of effective therapeutic teaching. This involves more than a just a brief
demonstration of the equipment. Following the training and demonstration from the therapist,
Pete will demonstrate dressing his upper and lower body using the adaptive equipment. The
therapist will allow Pete to perform the task independently, but will provide physical and verbal
cueing as needed. At the end of the intervention the therapist and Pete will discuss what adaptive
equipment he found to be beneficial, the equipment he would not like use in his activities of
daily living, and his concerns and questions. According to Gitlin (1995) a lack of knowledge of
how to use a device and inappropriate instruction are the main reasons for underuse of adaptive
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
11
equipment. Therefore, providing Pete with detailed, easy to understand training and the use of
demonstrations and practice will ensure the functional use of the equipment. The main outcome
for this intervention strategy is to improve occupational performance. Providing Pete with
adaptive strategies and equipment to perform lower body dressing with enhance his occupational
performance in independently donning and doffing lower extremity clothing.
Short-term goal. Client will don and doff underwear and pants with Min (A) using a
FWW within two weeks.
Intervention. The approach for this intervention is establish/restore. The intervention
will establish safe and proper techniques for the client to use while performing lower extremity
dressing. By proving the client with the ability to perform this task, it will restore the clients
ability to independently dress himself. Ryan and Sullivan (2011) expressed the need to address
specific deficits when retraining an individual on dressing following a stroke. Impaired postural
stability and balance, decreased endurance, decreased dexterity, impaired ability to stabilize
clothing and body parts, impaired sensory capabilities, and cognitive limitations are all areas that
must be addressed (Ryan and Sullivan, 2011). Pete will participate in therapeutic exercises to
improve strength, balance, weight shifting and control to prepare for standing activities. The
exercises will include body weight exercises such as marching while seated, weigh shifting on all
fours and exercises using resistance bands to increase strength in his lower extremities. Research
has shown that lower extremity strength and power are directly correlated to the patients
functional limitations. Therefore, increasing lower extremity strength will increase independence
in functional activities (Puthoff & Nielson, 2007). Following the therapeutic exercises, Pete will
perform functional static standing to facilitate weight bearing on the affected leg. Kane and
Buckley (2011) express the importance of substantial cueing from the therapist in standing
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
12
activities because clients are often fearful of standing on the affected leg due to decreased muscle
strength, postural control, and sensation. Also it is important for the client to stay concentrated
because the task takes substantial attention to maintain a standing position. Therefore,
distractions should be minimized and frequent breaks should be utilized. While performing
static functional standing the therapist can cue weight shifting on the affected lower leg. The
therapist can place personal items throughout the room and have the client locate the objects in
the room. Performing static standing while scanning the environment or having a conversation
with the therapist is a challenging and meaningful task to the client (Kane and Buckley, 2011).
Next, the therapist will educate and train Pete on the use of adaptive dressing techniques. The
therapist will instruct and demonstrate to Pete the sequencing for upper and lower extremity
dressing with left hemiparesis. Adaptive strategies such as putting the affected arm or leg in first,
clasping hands together to lift the affected leg, bringing the leg up onto the unaffected thigh to
don items, shifting weight when pulling pants up, and using the index finger and thumb to open
the sock with one hand will be addressed. Following training, Pete will complete upper and
lower body dressing. The therapist will provide physical and verbal cueing as needed. At the end
of the intervention the therapist and Pete will discuss what techniques he found to be beneficial
and any questions he may have regarding the treatment session. The main outcome for this
intervention strategy is to improve occupational performance. The intervention is aimed to
increase performance in dressing by improving the clients strength, balance, and postural
stability.
Frequency and Duration of Intervention
Pete will participate in occupational therapy (OT) sessions five days a week for 90
minutes a day. He will receive skilled OT services for a total of four weeks.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
13
Precautions and Contraindications
Before any functional mobility activities are performed, it is important that the therapist
educate the client on safety precautions and proper techniques to be used. The therapist must
ensure the client understands safe and proper techniques prior to participating in the activities.
The clients cognitive status should be evaluated prior to implementing an activity. Also the
clients pain level, activity tolerance, heart rate, respirations and fatigue level should be
monitored throughout the intervention. The therapist must use clinical judgment to determine if
the intervention should be carried out or discontinued if abnormal status or levels are present.
Additionally, the client should always be supervised when performing functional mobility
activities due to the risk of fall.
Primary Theory
The primary framework used to guide this intervention plan is the Person Environment
Occupation Performance (PEOP) Model. The PEOP model takes into account the interaction
between the person, environment, occupations of interest, and occupational performance. The
intervention plan embraces Petes values, interest, skills, and goals. The PEOP model uses a
client centered, top-down approach to treatment. The client must be treated as a whole, taking
into account intrinsic and extrinsic factors that either support or restrict the performance of
activities, tasks, and roles of the person. The primary focus of the intervention plan is on the
factors most inhibiting the clients occupational performance. The performance areas most
affected include the clients inability to functionally ambulate and dress his lower extremities.
Addressing the intrinsic and extrinsic factors inhibiting Pete from performing theses task are
considered when planning a successful intervention plan. The clients psychological, cognitive,
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
14
physiological, spiritual, neurobehavioral, support systems, and environmental factors are
considered when working with the client.
Client and Caregiver Training and Education
Client and caregiver training and education will be completed during the intervention
treatment sessions. The client will be educated on proper and safe transfer techniques, the use of
durable medical equipment and adaptive equipment, and dressing techniques. The therapist will
provide the information verbally, through demonstration, and practice. Also, it is beneficial to
educate the client on the benefits of the participating in interventions. Prior to discharge, the
clients daughter will be educated on the use of durable medical equipment and adaptive devices
that Pete will need at home. Pete and his daughter will both be educated on home modifications
that can be used to ensure Petes safety and independence. Also, the caregiver and client must be
provided with information regarding outpatient rehabilitation services following discharge.
Clients Response to the Interventions
The occupational therapist will monitor and assess Petes progress in achieving his goals
by assessing the occupational therapy daily progress notes and by performing a reassessment.
The therapist will review daily progress notes regarding Petes functional performance. Using
clinical reasoning, the OT will then determine Petes response to the intervention and reassess
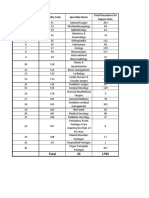
goals and intervention strategies as necessary. Upon initial evaluation, Pete was assessed using
the Functional Independence Measure (FIM). His scores showed that he required moderate
assistance in transfers, lower body dressing, and showering. He required minimal assistance in
upper body dressing, grooming, and bed mobility. Theses scores reflect his performance
regarding muscle strength, endurance, executive functioning, and safety and judgment while
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
15
performing these ADL tasks. Therefore, he will be reassessed throughout treatment and prior to
discharge to determine his progress in these particular areas.
References
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
16
Bobath, B. (1990). Adult hemiplegia: Evaluation and treatment. Oxford, England: ButterworthHeinemann.
Britton, E., Harris, N., & Turton, A. (2008). An exploratory randomized controlled trial of
assisted practice for improving sit-to-stand in stroke clients in the hospital setting.
Clinical Rehabilitation, 22(5), 448-458. doi: 10.1177/0269215507084644
Carrier, A., Levasseur, M., Bdard, D., & Desrosiers, J. (2012). Clinical reasoning process
underlying choice of teaching strategies: A framework to improve occupational
therapists' transfer skill interventions. Australian Occupational Therapy Journal, 59(5),
355-366. doi:10.1111/j.1440-1630.2012.01017.x
Carr, J. H., & Shepherd, R. B. (1998). Neurological rehabilitation: Optimizing motor
performance. Oxford, England: Butterworth-Heinemann.
Dean, C. M, & Shepherd, R. B. (1997). Task-related training improves performance of seated
reaching task after stroke: A randomized controlled trial. Stroke, 28(4), 722-728. doi:
10.1161/01.STR.28.4.722
Foti, D., & Kokestsu, J. (2013). Activities of daily living. In H. Penleton & W. Schultz-Krohn
(Eds. 7), Pedretti's occupational therapy:Practice skills for physical dysfunction (pp.
157-230). St. Louis: Elsevier.
Gitlin, L. N. (1995). Why older people accept or reject assistive technology. Generations, 19(1),
41-46. Retreived from http://web.b.ebscohost.com/ehost/detail/detail?sid=10546cd919aa-4cb5
9921db21697f4708%40sessionmgr110&vid=4&hid=112&bdata=JnNpdGU9ZWhvc3Qtb
Gl2ZQ%3d%3d#db=rzh&AN=1995017821
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
17
Kane, L. A., & Buckley, K. A. (2011). Functional mobility. In G. Gillen (Eds. , Stroke
rehabilitation: A function-based approach (pp. 351-388). St. Louis: Elsevier.
Lach, H. W. (2005). Incidence and risk for developing fear of falling in older adults. Public
Health Nursing, 22(1), 45-52. doi: 10.1111/j.0737-1209.2005.22107.x
Puthoff, M., & Nielsen, D. (2007). Relationships among impairments in lower-extremity strength
and power, functional limitations, and disability in older adults. Physical
Therapy, 87(10), 1334-1347. doi:10.2522/ptj.20060176
Ryan, P. A., & Sullivan, J. W. (2011). Activities of daily living adaptions: Managing the
environment with one-hand techniques. In G. Gillen (Eds. , Stroke rehabilitation: A
function-based approach (pp. 717-734). St. Louis: Elsevier.
Schemm, R. L., & Gitlin, L. N. (1998). How occupational therapists teach older patients to use
bathing and dressing devices in rehabilitation. The American Journal of Occupational
Therapy, 52(4), 272-282. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/?
term=How+occupational+therapists+teach+older+patients+to+use+bathing+and+dressin
g+devices+in+rehabilitation.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Pathfinder 2nd Edition House Rules Compendium - GM BinderDocument119 pagesPathfinder 2nd Edition House Rules Compendium - GM BinderBrandon PaulPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Interpretation of Peripheral SmearDocument34 pagesInterpretation of Peripheral Smearswathi bs100% (1)
- FirstAid SlidesDocument62 pagesFirstAid Slidessamihamaideh100% (1)
- Chessick - The Future of PsychoanalysisDocument283 pagesChessick - The Future of Psychoanalysisuterw100% (1)
- Nutriquizbee-July 2014Document11 pagesNutriquizbee-July 2014naty rodirisPas encore d'évaluation
- An Introduction To NutritionDocument17 pagesAn Introduction To NutritionAlejandra Diaz RojasPas encore d'évaluation
- Ch06 Blocked Fallopian TubesDocument80 pagesCh06 Blocked Fallopian TubesAasia Najaf SoomroPas encore d'évaluation
- Final Eb ReflectionDocument2 pagesFinal Eb Reflectionapi-238460511Pas encore d'évaluation
- Final Reflection Occupation BasedDocument2 pagesFinal Reflection Occupation Basedapi-238460511Pas encore d'évaluation
- Mitchell, Carol - ResumeDocument2 pagesMitchell, Carol - Resumeapi-238460511Pas encore d'évaluation
- Evaluation 4Document2 pagesEvaluation 4api-238460511Pas encore d'évaluation
- Single Evaluation Semester 3Document3 pagesSingle Evaluation Semester 3api-238460511Pas encore d'évaluation
- Semester 2 EvaluationDocument4 pagesSemester 2 Evaluationapi-238460511Pas encore d'évaluation
- Group Model Protocol FinalDocument13 pagesGroup Model Protocol Finalapi-238460511Pas encore d'évaluation
- 526 Evidence Paper 3Document10 pages526 Evidence Paper 3api-238460511Pas encore d'évaluation
- Peperomia PellucidaDocument8 pagesPeperomia PellucidajaninasuzettePas encore d'évaluation
- Locomotor SyllabusDocument5 pagesLocomotor SyllabusAyeshaKhalidPas encore d'évaluation
- Folliculitis Decalvans Update July 2019 - Lay Reviewed July 2019Document4 pagesFolliculitis Decalvans Update July 2019 - Lay Reviewed July 2019sjeyarajah21Pas encore d'évaluation
- QUIZ Classification of Surgery in TableDocument1 pageQUIZ Classification of Surgery in TableMaria Sheila BelzaPas encore d'évaluation
- Medical Decision MakingDocument14 pagesMedical Decision MakingwbothaPas encore d'évaluation
- Welcome To The Celestial Biolabs LimitedDocument8 pagesWelcome To The Celestial Biolabs LimitedsaahilsinghiPas encore d'évaluation
- Research Forms 2Document35 pagesResearch Forms 2api-343437101Pas encore d'évaluation
- Cerebral Blood Flow & StrokeDocument35 pagesCerebral Blood Flow & Stroke-'Henri Djhevon Kaary'-Pas encore d'évaluation
- All PackageRates (ABPMJAY) PDFDocument300 pagesAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- Do You Know Me Flyer-Teacher VersionDocument1 pageDo You Know Me Flyer-Teacher VersionMaria Guy Del DucaPas encore d'évaluation
- Food Saftey PDFDocument22 pagesFood Saftey PDFharsha vardhanPas encore d'évaluation
- Mobicare BrochureDocument4 pagesMobicare Brochuremicrobotica126Pas encore d'évaluation
- LipomaDocument51 pagesLipomaAgnes NiyPas encore d'évaluation
- Csa Z32 - Testing Guideline and Procedures: PO Box 20020 Red Deer, AB T4N 6X5 Phone: 403.986.2939Document8 pagesCsa Z32 - Testing Guideline and Procedures: PO Box 20020 Red Deer, AB T4N 6X5 Phone: 403.986.2939tim4109Pas encore d'évaluation
- OT HoppysAppReviewDocument1 pageOT HoppysAppReviewIris De La CalzadaPas encore d'évaluation
- Application Form (Pledge Form) For Whole Body DonationDocument1 pageApplication Form (Pledge Form) For Whole Body DonationVasanthakumar BasavaPas encore d'évaluation
- AdenomyosisDocument1 pageAdenomyosisVictor GomoiuPas encore d'évaluation
- Importance and Applicability of Strotas in Treatment of DiseaseDocument9 pagesImportance and Applicability of Strotas in Treatment of DiseaseAshutosh JhaPas encore d'évaluation
- Laporan Stock OpnameDocument138 pagesLaporan Stock OpnameAnggunia DeaPas encore d'évaluation
- Medical Needs Fatiguing The Descrpit Social CcienceDocument11 pagesMedical Needs Fatiguing The Descrpit Social Ccienceicicle900Pas encore d'évaluation
- AMINOGLYCOSIDESDocument15 pagesAMINOGLYCOSIDESGareth BalePas encore d'évaluation
- ENT Summery TABLEDocument19 pagesENT Summery TABLEtaliya. shvetzPas encore d'évaluation
- IHSCforAll2024Document510 pagesIHSCforAll2024Gvidas MikalauskasPas encore d'évaluation