Académique Documents
Professionnel Documents
Culture Documents
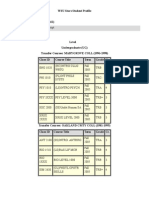
SW 3810 Research I
Transféré par
api-281763711Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
SW 3810 Research I
Transféré par
api-281763711Droits d'auteur :
Formats disponibles
Running head: EVIDENCE BASED RESEARCH
1
Summary
The competencies fulfilled by this assignment are:
2.1.3 Apply critical thinking to inform and communicate professional judgments.
2.1.6
Engage in research-informed practice and practice-informed research.
2.1.10 Engage, assess, intervene, and evaluate with individuals, families, groups, organizations,
and communities evaluate and assess interventions.
In writing this paper I learned about and practiced the steps involved in evidence based
practice (EBP). The first step in the process is to formulate a question to answer a practice need.
Once again, I chose an issue that is, not only of interest to me because of personal experience,
but pervasive in society today; the problem of obesity. I used a theoretical practice setting
(2.1.10) which was a weight loss support group and then used the CIAO acronym to formulate
my research question. For the second step, which is to search for empirical evidence, I used the
bottom-up approach in my research and located eight to ten major articles that I thought would
address the issue of obesity and show that it is indeed a social problem (2.1.3). The third step is
to critically appraise the relevant studies to determine if the treatment outcome is valid, reliable
and if it was done in an unbiased way (2.1.10). In step four I chose three interventions that I felt
could be effective and provide the desired outcome and discussed the research and results of each
one as well as the strengths and limitations and assessed any ethical or cultural issues that may
be present (2.1.6). Since our practice settings were theoretical we could not apply steps five in
which we would obtain any necessary training before implementing the chosen intervention and
formulating measurable treatment goals. We also could not apply step six which is to evaluate,
gather feedback and then share the outcome with interested colleagues.
EVIDENCE BASED RESEARCH
Evidence Based Research: Obesity
Lynda Reimer
SW 3810
Wayne State University
EVIDENCE BASED RESEARCH
3
Obesity
This topic is of interest to me because I have struggled with weight issues since
adolescence. So many of the people in my life. My theoretical practice setting is a weight loss
support group. The group includes eleven women, attendance varies but usually we have seven
or eight members at a bi-weekly meeting. The majority have struggled with their weight since
adolescence, and some have gained weight during a pregnancy. Individually they have tried a
variety of both formal weight loss programs, and self-guided regimens with varying degrees of
success. Unfortunately, none have been able to fully maintain the losses. In discussing why this
happens the group members believed the following issues to be responsible for the inability to
succeed; emotional eating, loss of motivation due to slow weight loss, and difficulty making life
style changes that would help to maintain weight loss. Since nothing thats been tried to date has
worked, it is time to research possible therapies that will help the group members to overcome
these issues and make it possible to maintain the weight loss and lead a healthier, happier life.
CIAO
If obese individuals who have not been successful at losing weight and maintaining
weight loss due to emotional eating, unsustainable motivation, and inability to follow weight loss
regimen follow a behavioral weight-loss program with motivational interviewing or a new
cognitive behavioral therapy or dialectical behavioral treatment, will they be able to control their
emotional eating and maintain lasting weight loss?
Obesity: A Social Problem
The following evidence shows that obesity is a social problem. Obesity has been declared
an epidemic in our country for the past twenty years. According to the Center for Disease
EVIDENCE BASED RESEARCH
Control one-third of all U.S. adults are obese and another one-third are overweight and it affects
seventeen percent of children as well (Ogden, et al, 2012). Government costs of treating obesity
and its related illnesses are estimated at $190 billion annually. Individually the average cost to
an overweight person is $1500 a year in medical expenses alone (Carroll, 2013). Obesity reduces
the quality of life and increases the risk of diseases such as Type 2 Diabetes, heart, lung, and
liver disease and certain cancers. Obesity related diseases are the second leading cause of
preventable death in the U.S. (Fuden, 2013). Although obesity is affects all income levels there
is some disparity. Women with higher income and education levels are less likely to be obese
than low income women with less education. In men, those with higher income are prone to
obesity, regardless of education level (Ogden, et al, 2012).
Research Method
Using the school library system I searched for research using the following key words;
obesity, weight loss therapies, emotional eating, weight loss maintenance, and motivation. I
found a dearth of studies and read through the abstracts of eight to ten articles. I based my
selection on the results shown in the three interventions and whether or not I felt the group
members would be open to using the interventions chosen.
Interventions
The first research article was a randomized controlled study aimed at testing a new form
of cognitive behavioral treatment which was based on CBT-BN, a successful therapy used to
treat eating disorders, in particular, bulimia nervosa. This new form of CBT was intended to help
participants curb overeating and increase their physical activity level. It also concentrated on
thought processes which are believed to block the success of maintaining weight loss. To
EVIDENCE BASED RESEARCH
determine effectiveness it was compared to behavioral therapy (BT), one of the leading
treatments for obesity, and guided self-help (GSH), a minimal intervention therapy. The 150
participants were randomly assigned to the three groups, all groups were guided in lowering their
caloric intake. The CBT and BT groups received weekly individual sessions with the final 14
sessions focusing on maintenance behaviors. The GSH group received two sessions at the start
and a limited number of 20 minute phone sessions throughout. All groups were followed up for
three years after the final session. The study results showed that although program completion
rates were high, most participants lost weight but then regained it; showing that CBT is no better
than BT at helping participants avoid regaining lost weight.
The goal of the second intervention was to improve treatment outcome for behavioral
weight loss programs (BWLP) using a stepped-care (SC) approach. All participants were
enrolled in a behavioral weight loss program (BWLP) with minimal intervention. Participants
who were slow to progress were then enrolled in motivational interviewing (MI) as well.
Motivational interviewing is a method that is designed to improve a persons motivation to make
changes. The BWLP participants attended 20 weekly group sessions of 6-12 people that were
75 minutes long. Those in the BWLP + MI group met weekly in individual sessions that were 4560 minutes long. Study results showed that those who received MI not only had better weight
loss outcomes, but also had more positive change in behaviors, including increased time spent
exercising each week.
The third article was based on four case studies involving participants who were chosen
based on the results of several questionnaires including the Emotional Eating Questionnaire.
Emotional eating is a common barrier, not only to weight loss but to successful maintenance of
lost weight. This study looks to discover whether cognitive behavioral therapy (CBT) and
EVIDENCE BASED RESEARCH
dialectical behavioral therapy (DBT) can alleviate this issue. Of the four participants two
received cognitive behavioral therapy and two received dialectic behavioral therapy. The study
consisted of 22 individual therapy sessions with follow-up sessions at 1, 2, 4, and 8 weeks. The
CBT sessions addressed beginning and maintaining weight loss, barriers to weight loss,
increasing activity level, body image, weight goals and healthy eating. The DBT sessions were
aimed at teaching mindfulness, emotional regulation, distress tolerance, relapse prevention and a
final review of all topics.
At the 4 week follow-up session participants receiving DBT reported having a difficult
time initially with using mindfulness training but improved with practice. By the final 8 week
follow-up they had lost 8-10% of body weight and showed a 4-5 point reduction in BMI. Those
receiving CBT began to have difficulty following the prescribed weight loss regimen by the 4
week session and although they were able to understand that emotional eating is mainly an issue
of distorted thoughts, they were not able to consistently confront those thought processes
effectively. At the 8 week follow-up session they showed a 0.5% reduction in weight and 0.2-0.3
reduction in BMI. Although all participants lost weight, those receiving DBT lost more weight
and were more successful at maintaining their progress.
After reading and comparing the three interventions I immediately eliminated the first
intervention since it was proven that the new CBT and BT did not improve weight loss
maintenance in study participants. Results showed that 98% of participants regained all their lost
weight at the end of the three year follow up. Although the DBT and MI studies were smaller
studies, the results showed some promise. I would suggest the use of a combination of the second
and third interventions. Namely, BWLT plus MI, because those participants showed an increase
of positive changes in adherence and the ability to maintain weight loss, two of the issues
EVIDENCE BASED RESEARCH
reported by support group members. My suggestion to the group would be to begin with
individual MI sessions in order to set individual goals. Then proceed to group sessions using the
LEARN program which is a behavioral therapy that teaches moderate lifestyle changes to
promote weight loss and increase physical activity. During the group sessions I would also teach
some of the DBT modules, specifically the mindfulness, emotional regulation, and distress
tolerance to address emotional eating among group members.
Evidence Based Practice
If used correctly the Evidence Based Practice process can lead to modes of therapy for clients
who have not responded to standard treatments used in social work. In my theoretical practice
setting the clients would likely continue the cycle of losing and regaining weight or they may
have given up altogether. To begin the EBP process I used information gathered from clients in
the group to form a practice question using CIAO format. In my search for evidence based
research I used the bottom-up method and found many research articles related to my practice
question. Not wanting to spend hours reading every study, I chose several that I found
interesting. After thoroughly reading the chosen studies I decided that only two would suit the
clients problem. The final steps are to implement the intervention and evaluate the outcome and
obtain feedback from clients. In this practice setting EBP led me to discover interventions that
show promise where standard therapies had failed in effectiveness.
Some advantages of EBP are improvement in effective interventions that are backed by evidence,
and the opportunity to learn from the expertise of others. It expands our own knowledge base and
promotes life-long learning. Some possible disadvantages are the amount of time required for
research, possible lack of access to necessary databases, and the cost of training to learn
interventions.
EVIDENCE BASED RESEARCH
8
References
Carels, R. A., Darby, L., Cacciapaglia, H. M., Konrad, K., Coit, C., Harper, J., Versland, A.
(2007). Using motivational interviewing as a supplement to obesity treatment: A steppedcare approach. Health Psychology, 26(3), 369-374. doi:10.1037/0278-6133.26.3.369
Carroll, D. (2013, March 13). [Web log message]. Retrieved from
http://www.dailyfinance.com/2013/03/09/the-price-of-americas-obesity-epidemic/
Cooper, Z., Doll, H., Hawker, D., Byrne, S., Byrne, S., Bonner, G., Eeley, E., & O, M. (2010).
Testing a new cognitive behavioral treatment for obesity: A randomized controlled trial
with three-year follow-up. Behavior Research and Therapy, 48(8), 706-713. doi:
10.1016/J.BRAT>2010.03.008
Fuden, S. (2013, April 2). [Web log message]. Retrieved from
http://publichealthonline.gwu.edu/cost-obesity-infographic-nphw/
Glisent, K., & Strodl, E. (2012). Cognitive behavioral therapy and dialectic behavioral therapy
for treating obese emotional eaters. Clinical Case Studies ,11(2), 71-88. doi:
10.1177/1534650112441701
Ogden C., Kit B., Flegal K. Prevalence of Childhood and Adult Obesity in the United States,
2011-2012. JAMA.2014;311(8):806-814. doi:10.1001/jama.2014.732.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Early Signs of AutismDocument27 pagesEarly Signs of AutismErica Alejandra Schumacher100% (1)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Curtain WallDocument11 pagesCurtain WallZameer AhmedPas encore d'évaluation
- Examples: Inability To Sit Still, Pacing, Wringing of Hands, or Pulling of ClothingDocument14 pagesExamples: Inability To Sit Still, Pacing, Wringing of Hands, or Pulling of ClothingFaith Dianasas RequinaPas encore d'évaluation
- Louise L HAY AffirmationsDocument10 pagesLouise L HAY AffirmationsEvi Kutasi100% (2)
- Eng & FLS Standards Rev.1 (Dec. 2018)Document72 pagesEng & FLS Standards Rev.1 (Dec. 2018)Nalan BAHCEKAPILIPas encore d'évaluation
- PPC Production PlantDocument106 pagesPPC Production PlantAljay Neeson Imperial100% (1)
- Personal StatementDocument5 pagesPersonal Statementapi-281763711Pas encore d'évaluation
- Reference EveleenDocument1 pageReference Eveleenapi-281763711Pas encore d'évaluation
- SW 4810 Research IIDocument13 pagesSW 4810 Research IIapi-281763711Pas encore d'évaluation
- SW 4441 Field Seminar IDocument7 pagesSW 4441 Field Seminar Iapi-281763711Pas encore d'évaluation
- Youth Mhfa Certificate LRDocument1 pageYouth Mhfa Certificate LRapi-281763711Pas encore d'évaluation
- SW 4010 Group TheoryDocument7 pagesSW 4010 Group Theoryapi-281763711Pas encore d'évaluation
- Personal Learning GoalsDocument1 pagePersonal Learning Goalsapi-281763711Pas encore d'évaluation
- TranscriptsDocument6 pagesTranscriptsapi-281763711Pas encore d'évaluation
- SW 4710 Policy Analysis IIDocument8 pagesSW 4710 Policy Analysis IIapi-281763711Pas encore d'évaluation
- SW 3710 Policy Analysis IDocument9 pagesSW 3710 Policy Analysis Iapi-281763711Pas encore d'évaluation
- SW 3410 Ethics Moral ReasoningDocument10 pagesSW 3410 Ethics Moral Reasoningapi-281763711Pas encore d'évaluation
- SW 3510 HbseDocument10 pagesSW 3510 Hbseapi-281763711Pas encore d'évaluation
- SW 3020 Theory IIDocument4 pagesSW 3020 Theory IIapi-281763711Pas encore d'évaluation
- SW 3110 DiscriminationDocument6 pagesSW 3110 Discriminationapi-281763711Pas encore d'évaluation
- Jun ReferenceDocument2 pagesJun Referenceapi-281763711Pas encore d'évaluation
- SW 3010 Theory IDocument7 pagesSW 3010 Theory Iapi-281763711Pas encore d'évaluation
- Resume ReimerDocument2 pagesResume Reimerapi-281763711Pas encore d'évaluation
- NewhopereferralletterDocument1 pageNewhopereferralletterapi-281763711Pas encore d'évaluation
- IntroductionDocument1 pageIntroductionapi-281763711Pas encore d'évaluation
- Submission LetterDocument1 pageSubmission Letterapi-281763711Pas encore d'évaluation
- Rorschach y SuicidioDocument17 pagesRorschach y SuicidioLaura SierraPas encore d'évaluation
- Penyakit Palpebra Dan AdneksaDocument39 pagesPenyakit Palpebra Dan AdneksaayucicuPas encore d'évaluation
- We Think About Rotary Valve ReliabilityDocument8 pagesWe Think About Rotary Valve ReliabilityAhmed KhairyPas encore d'évaluation
- EfAD BenchmarkJune2005 UKDocument55 pagesEfAD BenchmarkJune2005 UKCristina Dobrin ClaudiaPas encore d'évaluation
- Soni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyDocument1 pageSoni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyVishalPas encore d'évaluation
- 310 Ta PDFDocument8 pages310 Ta PDFVincent GomuliaPas encore d'évaluation
- Prof Educ 2: Foundation of Special and Inclusive EducationDocument12 pagesProf Educ 2: Foundation of Special and Inclusive EducationNerissa Custosa BastoPas encore d'évaluation
- Refrigeration and Air Conditioning Technology 8th Edition Tomczyk Silberstein Whitman Johnson Solution ManualDocument5 pagesRefrigeration and Air Conditioning Technology 8th Edition Tomczyk Silberstein Whitman Johnson Solution Manualrachel100% (24)
- NTFPP-Module 3 Microwave Processing of Foods - AjitKSinghDocument12 pagesNTFPP-Module 3 Microwave Processing of Foods - AjitKSinghKeshav RajputPas encore d'évaluation
- Exudate Detection For Diabetic Retinopathy With Circular HoughDocument7 pagesExudate Detection For Diabetic Retinopathy With Circular HoughAshif MahbubPas encore d'évaluation
- Excipients As StabilizersDocument7 pagesExcipients As StabilizersxdgvsdgPas encore d'évaluation
- Environmental Stewardship - Sustainability Assignment - Ethan GabrielDocument3 pagesEnvironmental Stewardship - Sustainability Assignment - Ethan GabrielEthan GabrielPas encore d'évaluation
- B152 01 00 00 00Document517 pagesB152 01 00 00 00lsep_bellaPas encore d'évaluation
- Comparative Evaluation of The Diametral Tensile Strength of Four Commercially Available Luting Cements An in - Vitro StudyDocument16 pagesComparative Evaluation of The Diametral Tensile Strength of Four Commercially Available Luting Cements An in - Vitro StudyInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- SureFlo RDocument2 pagesSureFlo RKen NgPas encore d'évaluation
- Bill 192: An Act To Ensure Student Health and Safety in The Classroom by Regulating Ambient Air Quality in SchoolsDocument8 pagesBill 192: An Act To Ensure Student Health and Safety in The Classroom by Regulating Ambient Air Quality in SchoolsCtv MontrealPas encore d'évaluation
- Human Resource Management: Submitted By: Group # 6 Submitted To: Sir Usama NajamDocument23 pagesHuman Resource Management: Submitted By: Group # 6 Submitted To: Sir Usama NajamkamranPas encore d'évaluation
- Funda PharmaDocument9 pagesFunda PharmaShiangPas encore d'évaluation
- Sem-V Principle of Taxation Law PDFDocument3 pagesSem-V Principle of Taxation Law PDFAnantHimanshuEkkaPas encore d'évaluation
- Companies Directory Alternative Fuels and Smart Transportation June 20Document82 pagesCompanies Directory Alternative Fuels and Smart Transportation June 20Mbamali Chukwunenye100% (1)
- CN LSHC The Future of Pharmacy en 031120Document8 pagesCN LSHC The Future of Pharmacy en 031120marina_netPas encore d'évaluation
- Cabuyao Integrated National High School: The Problem and Its BackgroundDocument4 pagesCabuyao Integrated National High School: The Problem and Its BackgroundJohn Carlo MolinaPas encore d'évaluation
- Paper Pet ProjectDocument27 pagesPaper Pet Projectapi-406104878Pas encore d'évaluation
- Fetal Products AllDocument1 pageFetal Products AllIon pasterfPas encore d'évaluation