Académique Documents
Professionnel Documents
Culture Documents
Technology in Nursing Final Paper
Transféré par
api-272621489Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Technology in Nursing Final Paper
Transféré par
api-272621489Droits d'auteur :
Formats disponibles
Running head: ALARM FATIGUE
Technology in Nursing: Alarm Fatigue
Cameron Verkaik
Ferris State University
ALARM FATIGUE
Abstract
This paper examines alarm fatigue, a desensitizing to alarm sounds, which can affect nurses in
the healthcare setting. Advantages and disadvantages of current technologies are discussed to
present a rather complex issue. Applying alarm fatigue to both an environmental and
psychological theory promotes several informative perspectives. The assessment of the
healthcare environment in connection to technology and alarms is examined through various
study statistics, systems framework, policies, assumptions, and quality and safety issues. Using
root cause analysis, the problems surrounding alarm fatigue are outlined. The American Nurses
Association (ANA) Standards of Practice as well as the QSEN Institutes competencies are
reviewed and provide beneficial guidelines to review the implications and consequences to alarm
fatigue. Several strategies of implementation are discussed such as removing scope-of-barrier
practices, collaboration, lifelong learning and leadership and deciphering current alarm sounds.
These strategies have proven to lower the risk of alarm fatigue in several healthcare settings and
promote a safer patient environment.
Keywords: technology, alarm fatigue, nursing, informatics, safety, patient risk, healthcare,
environment
ALARM FATIGUE
Technology in Nursing: How Technology is Changing Healthcare
Technology is changing the world at warp speed and nowhere is this more evident than
in the health care setting (Huston, 2013, p. 1). This statement by Huston is one few would
argue. The world of technology seems to have no end in many professions, and medical
professionals are being bombarded with many technologies to create greater work efficiency,
more mature patient analysis, and safer healthcare environments. But are all technologies
advantageous? Technology has been described as both part of the problem and part of the
solution for safer health care, and some observers warned of the introduction of yet-to-be errors
after the adoption of new technologies (Powell-Cope, Nelson, Patterson, 2008, p. 1). Many of
these technologies that the health care environment has implemented have alarms, many times
multiple, with various sounds, warnings, and signals. Common sense would tell us these alarms
are beneficial to all involved, granting efficiency to the nurses supervision, yielding warning to
possible health threats for the patient, while putting the patients family at ease knowing their
loved one is being carefully monitored. Yet what if these alarms were actually creating an
opposite effect? Due to the constant barrage of noise, patient families may be feeling trapped in a
disruptive, anxiety-filled environment and clinicians may becoming desensitized or immune to
the sounds, overwhelmed by information, and suffering from a condition called alarm fatigue.
Alarm Fatigue
With nearly five thousand types of medical devices used by millions of health care
providers, alarm fatigue is a widespread issue that can affect any hospital with technology
(Powell-Cope, Nelson, Patterson, 2008). The more advanced and widespread the technology, the
more likely the clinicians in this setting suffer from some level of alarm fatigue. Technology
allows for greater efficiency and many times lower costs, yet needs to be balanced with the
ALARM FATIGUE
importance of human interaction, and not devalue the human element (Huston, 2013, p. 10).
Nursing professionals should be well informed of alarm fatigue so that they can evaluate their
own behavior and work environment, and also work towards possible solutions, in order to
minimize risks and give all patients the best care possible.
Theory
Alarm fatigue can be studied through multiple theoretical frameworks. This type of
analysis can lead to a greater understanding of the issue as well as develop deeper awareness and
education.
Florence Nightingale: Environmental Theory
Florence Nightingales environmental theory discusses the importance of environmental
conditions and the direct relation to patient outcome. Two of the ten canons of the environmental
theory relate to technology in nursing. First, observation is a key component to promoting a
healing environment for the patient (Environmental Theory, 2013). Now pulse oximetry allows
nurses to identify decreased oxygenation before clinical symptoms appear, and thus more
promptly diagnose and treat underlying causes (Powell-Cope, et al., 2008). Thus, many
technologies allow for close monitoring of patient status, complementing this component. The
second canon related to alarm fatigue discusses the importance of light and noise of the patients
environment (Environmental Theory, 2013). Excess alarms can affect the noise and light levels,
causing stress to both the patient and family members, which reduces their ability to cope with
their circumstance.
It is also important to remember that Florence Nightingale believed nursing to be both an
art and a science. The science comes in the use of technology to diagnose and treat patients
according to the data that is obtain. The art is concerned with how nurses interact with patients.
ALARM FATIGUE
Technology is here to stay and more incredible advances are arriving daily. We, as nurses, must
make certain that these technological wonders do not become more important than the human
beings we are caring for (Nash, 2014, p.12). We cannot allow technology to take over clinical
skills or personal interaction.
Abraham Maslow: Hierarchy of Needs Theory
Complementing Nightingales theory, psychologist Abraham Maslow believed that there
are basic needs that must be satisfied in humans before higher-order needs are met. One of these
basic foundational needs is safety, including security of environment (McLeod, 2007). Many
technologies have been implemented into health care due to their attractiveness of increased
safety and security. All individuals, whether patient or nurse, desire to feel they are in a secure
environment.
The advancement of technological alarms started out supporting this secure environment,
but is now creating danger to the patient.
For example, a 60-year-old man died in the intensive care unit of a hospital not
from the injury he suffered but from a system failure that resulted in delayed
response to an alarm signal that indicated significant changes in his condition.
Serious changes that included rapidly increasing heart rate and falling blood
oxygen levels. Staff responded only after one hour, when a critical alarm
condition signaled that the patient had stopped breathing. (Joint Commission,
2013).
The environment of each patient is directly correlated to their safety, as well as their overall
health improvement during their time in the health care setting.
ALARM FATIGUE
Assessment of the Healthcare Environment
Alarm fatigue is a complex issue that requires careful, on-going assessment of the
healthcare environment. Because technology is being introduced consistently, the healthcare
environments are also consistently changing, therefore healthcare organizations should be
regularly assessing their nursing staffs behavior when working alongside many alarms.
The Association for the Advancement of Medical Instrumentation, the Food and Drug
Administration, and the Joint Commission came to this conclusion during a 2012 summit
hearing:
Medical alarm systems are out of control. Every day, around the clock, hundreds
of auditory alarm signals sound for every patient, thousands of alarm signals
chime in every unit, tens of thousands of alarm signals blare throughout every
hospital. Clinicians are fatigued, confused and overloaded with sensory alerts or
left in the dark without actionable information from this cacophony of sounds
and signals. (Ferenc, 2012, p.1).
Systems Framework
Organization Policies
Due to its severity, the Joint Commission has announced alarm fatigue as a 2014 patient
safety goal. Between January 2009 and June 2012, there were ninety eight events of alarms
ignored due to sheer volume, with eighty of those resulting in death and thirteen resulting in loss
of function, as well as five unexpected additional care or extended stays (Nault & Sincox, 2014).
In order to complete the alarm fatigue safety goal, several phases are occurring. Phase one began
in January 2014, with hospitals being required to establish alarms as an organization priority and
ALARM FATIGUE
identify the most important alarms to manage based on their own internal situations. Phase two
will begin in January 2016 when hospitals will be expected to develop and implement specific
components of policies and procedures. Alarm system management education will also be
required of those in the organization (Joint Commission, 2013).
Resources
Boston Medical is facing the alarm fatigue problem head on by creating a task force
made up of nurses, physicians, and residents. After taking time to compile their alarm data
through frontline user input and nurse evaluations, they discovered 67% of the alarms came from
violations in heart rate default settings (McKinney & Maureen, 2014). These individuals were
asked to explain, in their opinions, why there were so many unanswered alarms, the obstacles to
alarms, and determine what the cause of the problem is. From the start, their focus was on
standardizing devices default settings across units. They adjusted heart rate monitors, while still
within clinically acceptable ranges, as well as changing heart rate alarm levels from warning to
crisis so they could not automatically reset. Boston Medicals clinical service manager of
cardiology, Deborah Whalen stated, Staff were used to warning alarms resetting so if they went
off, they often waited to see if they went away (McKinney et al., 2014, p. 2). Rather than
addressing the alarm and assessing the patient immediately, many nurses were experiencing
alarm fatigue. The task force did develop a process in which nurses have authority to raise or
drop certain heart-rate parameters in certain patient circumstances. In order to allow this change,
two registered nurses must review patient data together and agree to make the change. In
addition, nurse professionals are also required to have a thorough understanding of heart-rate
knowledge, scoring at least ninety percent on their exams. Audible cardiac alarms are now down
ALARM FATIGUE
eighty nine percent from nearly ninety thousand to roughly ten thousand over a six week starting
period (McKinney et al, 2014).
Assumptions
In the nursing profession, the patient is the highest priority. The patients safety, feelings,
and rights are the nurses main concern. The respectfulness of privacy is also a high priority, as
call lights are used to allow patients to call the nurse when needed. In the health care setting, the
element of team is encouraged, as the acuity of patients increases, the work of the nurse
increases and makes it hard to address every alarm. Nurses may assume others will respond to
the purpose of the alarm. In a system where teamwork and collaboration are in place, this nurse
may be able to depend on fellow staff to answer the alarm. However, assumptions should not be
made as this may put the patient in great danger if no one, in fact, responds.
Inference, Implications and Consequences
Consequences of Alarm Fatigue
The consequences of alarm fatigue can be very costly to any organization. Extended
hospital stay, injury, and even death can result. Such an instance occurred in 2007 when a 77 year
old who had been admitted to a cardiac unit passed away due to cardiac arrest after a low
battery alarm had gone unanswered for an extended period of time (Sendelbach & Funk, 2013).
This type of consequence is much more costly than the education and high exam standards that
could be implemented for all nurses.
Recommendations for Quality and Safety Improvements
Removing scope-of-barrier practices. All nurses and other health care providers must
be able to practice to the full extent of their education and training (Cipriano & Murphy, 2011,
p. 3). By removing scope-of-practice barriers, nurses will better be able to collect and analyze
ALARM FATIGUE
patient data as well as make informative decisions that can decrease the number of alarms being
used.
Collaboration. By encouraging collaboration in the nursing setting, teamwork will
become the norm and allow for responsible decision-making for all patient-related technology
decisions. More importantly, before making widespread initiatives, it is important to include
nurses in testing of new models of care and new technology. Selecting wrong equipment and
technology can be costly and expose the patient to errors (Powell-Cope, 2008, p.7).
Lifelong learning and leadership. Ensuring that nurses engage in lifelong learning will
promote technology in the healthcare setting. In turn, nurses will be better equipped to lead
change and advance health. Ideally, all nurses will be able to lead in technology, rather than only
technically competent staff members. If lifelong learning is occurring, all nurses will feel
competent to lead.
Alarm setting improvement. By setting alarms to have different tones, nurses can
anticipate the severity of the alarm. All of these warning systems depend on the ability of the
nurse to notice the warning, process the alarm and comprehend what is happening, and finally
take the appropriate action to decrease risk to the patient (Powell-Cope, 2008, p.6). For
example, when a code is called, the alarm that rings overhead is very distinct so that everyone is
informed of the patients status. Thus, nurses and other staff can act quickly on the situation and
decrease the risk and harm that may have otherwise occurred.
American Association of Critical-Care Nurses (AACN). The AACN has implemented
a practice alert to help nurses decrease the amount of alarms they may experience. The AACN
practice alert is focused on ECG monitoring as 80% to 99% are false alarms for of minimal
clinical significance. They include proper skin preparation for ECG placement, daily changes,
ALARM FATIGUE
10
individualized alarm settings including threshold settings for oxygen saturation, educating new
nurses on the proper use of the equipment, monitoring only patients who have clinical
indications for it, and establishing teams to address alarms issues and develop policies directly
related to them (AACN, 2013). Following these guidelines will help nurses troubleshoot alarm
issues as well as enhance the patients experience.
American Nurses Association (ANA) Standards
Standard 1: assessment. The registered nurse collects comprehensive data pertinent to the
healthcare consumers health and/or the situation (ANA, 2010, p.32). Today, nurses use many
different types of technology to determine the health status of the patient. These various
technologies can include IV pumps, telemetry monitoring, electronic medical records, and
barcode scanning. Both application and interpretation of data is necessary in order for clinicians
to make wise decisions. When determining which data is pertinent to the patients health, it is
also important to document in a timely and accurate manner. Rather than relying on technology,
the nurse should rely on their own assessment and consider technology a complementing tool.
Standard 5: implementation. The registered nurse utilizes technology to measure, record,
and retrieve healthcare consumer data, implement the nursing process, and enhance nursing
practice (ANA, 2010, p.38). Operating equipment effectively and efficiently protects the
patient from harm and allows the nurse to use only equipment that is necessary. Therefore,
feelings of anxiety are avoided for the patient and family that can arise from an overuse of
technology that includes many alarms.
Standard 8: education. The registered nurse attains knowledge and competence that
reflects current nursing practice (ANA, 2010, p.49). Continuing education allows the nurse to
ALARM FATIGUE
11
gain awareness of the issue of alarm fatigue as well as strategies to control it. If all nurses stay
current in their field, patients will be better cared for in a calmer, quieter environment.
Standard 9: evidence-based practice and research. The registered nurse integrates
evidence and research findings into practice (ANA, 2010, p.51). Nurses should find evidence
based on research that shows alarm fatigue is a serious issue that may cause harm to the patient,
therefore working to develop ways that alarms can be diminished is a priority that may require
re-training as well as various alarm settings for each individual patient.
Quality and Safety Education for Nurses (QSEN) Competencies
Patient centered care. The QSEN definition of patient centered care focuses on
including patients in all decisions and providing compassionate care that's based on a patient's
needs and values (Hunt, 2012, p.2). Applying this practice is crucial in maintaining a positive
relationship with the patient and patients family. By asking the patient how the alarms are
making them feel, a nurse can perform a more accurate assessment of the patients health and
improve the quality of environment.
Teamwork and collaboration. Teamwork and collaboration is define as
interdisciplinary collaboration and shared decision making among the healthcare team (Hunt,
2012, p.2). By collaborating with other nurses in regards to alarm parameters and settings, both
nurses and patients can feel secure that the correct decisions are being made.
Evidence-based practice (EBP). QSENs EBP focuses on the use of research and
evidence in the development of nursing practice (Hunt, 2012). Research has shown that alarm
fatigue is a serious issue that needs to be address. The American Association of Critical-Care
Nurses (AACN) has shown that the implementation of the practice alert has decreased the
number of alarms (AACN, 2013).
ALARM FATIGUE
12
Quality improvement. QSEN defines quality improvement as it relates to data
collection, evaluation, and improvement of patient outcomes (Hunt, 2012, p.2). It is important
to continue evaluating the healthcare setting through patient outcomes even after alarm
improvements are made. This type of data collection will provide necessary feedback for the
healthcare setting trying to make improvements.
Safety. The S of QSEN, safety, focuses on preventing harm to patients as it relates to the
Joint Commissions National Patient Safety Goals (Hunt, 2012). This education is the most
critical when applied to alarm fatigue. Nurses must prevent harm, and if technology is harming
patients, that technology needs to be re-evaluated or changed in some way.
Informatics. The QSEN definition of informatics relates to the utilization of
technology to promote safety and quality (Hunt, 2012, p.2). When using equipment properly,
the number of alarms does decrease. The idea that technology is harmful because of the alarm
fatigue effect must be balanced with the usefulness technology provides for all patients.
Conclusion
In conclusion technology will continue to be a prevalent and beneficial tool in many
healthcare settings. It is the responsibility of medical professionals to continue to gain awareness
of the disadvantages to technology as well. The value of technology hinges on how its used and
whether it helps or hinders care (Cipriano & Hamer, 2013, p. 2). Alarm fatigue is a consequence
to alarm technology that can affect anyone, and nurses must work to assess their own behavior as
well as their patients environment to stay on top of this issue. If nurses continue to keep patient
safety as a first priority, they will engage in lifelong learning that will benefit them for many
reasons and technology will continue to be a complementing tool to their medical knowledge and
ALARM FATIGUE
13
experience. Technology enables care and enhances safety by automating functions both simple
and complex. It doesnt replace nurses (Cipriano & Hamer, 2013, p. 2)
References
Alarm management. (2013). In American Association of Critical-Care Nurse. Retrieved from
http://www.aacn.org/wd/practice/content/practicealerts/alarm-management-practicealert.pcms?menu=practice
American Nurses Association [ANA]. (2010). Nursing: Scope and standards of practice
(2nd ed.). Silver Spring, MD: Nursesbooks.org, (pgs. 52-55).
Cipriano, P. F., & Murphy, J. (2011). Nursing Informatics. The Future of Nursing and Health IT:
The Quality Elixir. Nursing Economic$, 29(5), 286-282.
Cipriano, Pamela F., and Susan Hamer. (2013). Enabling the ordinary: More time to care.
American NursesToday 8.11: 2-4. Web. 27 Apr. 2015.
Environmental Theory. (2013). In Nursing Theory. Retrieved from http://www.nursingtheory.org/theories-and-models/nightingale-environment-theory.php
Ferenc, Jeff. (2012). Alarm fatigue to get heightened attention. H&HN: Hospitals & Health
Networks, 86(5), 18.
Hunt PhD, RN, D. (2012, September). QSEN competencies: A bridge to practice. Nursing Made
Incredibly Easy!. Retrieved from
http://journals.lww.com/nursingmadeincrediblyeasy/Fulltext/2012/09000/QSEN_compete
ncies__A_bridge_to_practice.1.aspx
Huston, C. (2013). The impact of emerging technology on nursing care: Warp speed ahead.
Online Journal Of Issues In Nursing, 18(2), 1. doi:10.3912/OJIN.Vol18No02Man01
ALARM FATIGUE
14
Kenny, P. E. (2011). Message from the President. Alarm Fatigue and Patient Safety.
Pennsylvania Nurse, 66(1), 3-22.
McLeod, S. (2007). Maslow's hierarchy of needs. Simply Psychology. Retrieved from
http://www.simplypsychology.org/maslow.html
McKinney, M. (2014). Hospital's simple interventions help reduce alarm fatigue. Modern
Healthcare, 44(5), 26-27.
Nash, B. A. (2014). Maintaining the art of nursing in an age of technology. Ohio Nurses Review,
89(6), 12-13.
Powell-Cope, G., Nelson, A. L., & Patterson, E. S. (2008). Chapter 50 patient care technology
and safety. Patient Safety and Quality: An Evidence-Based Handbook for Nurses (pp. 113). Rockville, MD: Hughes RG. Retrieved from
http://www.ncbi.nlm.nih.gov/books/NBK2686/
Rice, S. (2015). Health IT among ECRI's top 10 patient-safety concerns. Modern Healthcare,
45(14), 8.
Sincox, A.K, Nault, D.S (2014). Raising the alarm: Patient care at risk from too many... bells,
beeps & buzzers. Michigan Nurse, 87(2), 11-16.
The Joint Commission Announces 2014 National Patient Safety Goal. (2013, January). Joint
Commission Perspectives, 33(7), 1-4. Retrieved from
http://www.jointcommission.org/assets/1/18/JCP0713_Announce_New_NSPG.pdf
ALARM FATIGUE
15
Vous aimerez peut-être aussi
- Nursing As A Prof, HistoryDocument51 pagesNursing As A Prof, Historymags_abad09Pas encore d'évaluation
- The Impact of Emerging Technology On Nursing Care: Warp Speed AheadDocument16 pagesThe Impact of Emerging Technology On Nursing Care: Warp Speed Aheadphoenix180Pas encore d'évaluation
- Trends in NursingDocument8 pagesTrends in NursingVjs MrunaliniPas encore d'évaluation
- 07 Nurse-Patient Ratios As A Patient Safety Strategy PDFDocument7 pages07 Nurse-Patient Ratios As A Patient Safety Strategy PDFAmanda DavisPas encore d'évaluation
- Nursing As An Art Nursing As An Art Nursing As An Art Nursing As An ArtDocument14 pagesNursing As An Art Nursing As An Art Nursing As An Art Nursing As An Artraj100% (3)
- The Future of Nursing EducationDocument10 pagesThe Future of Nursing EducationAimee GutierrezPas encore d'évaluation
- The Analysis of Nurse Compliance in Documenting of Nursing Care in Islamic Hospital PalembangDocument11 pagesThe Analysis of Nurse Compliance in Documenting of Nursing Care in Islamic Hospital PalembangInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Orem's Self-Care Deficit TheoryDocument6 pagesOrem's Self-Care Deficit TheoryMary ShiksPas encore d'évaluation
- UnderstaffingDocument13 pagesUnderstaffingIrish Docoy PatesPas encore d'évaluation
- The Effect of Nurse Staffing On Patient-Safety Outcomes A Cross-Sectional SurveyDocument9 pagesThe Effect of Nurse Staffing On Patient-Safety Outcomes A Cross-Sectional SurveyLuoya houPas encore d'évaluation
- Summary On Evidence Based PracticeDocument1 pageSummary On Evidence Based Practiceteena17Pas encore d'évaluation
- History of NursingDocument8 pagesHistory of NursingNazareth Narisma PatindolPas encore d'évaluation
- Ethical Issues in NursingDocument30 pagesEthical Issues in NursingUpendra Yadav100% (2)
- Nursing in 21st CenturyDocument41 pagesNursing in 21st CenturyCarissa De Luzuriaga-Balaria0% (2)
- Patterns of Knowing EssayDocument6 pagesPatterns of Knowing Essayapi-282992446100% (2)
- Nurse Case StudyDocument6 pagesNurse Case Studyprateeksha16Pas encore d'évaluation
- Research NursingDocument20 pagesResearch NursingMimi Lizada BhattiPas encore d'évaluation
- Florence NightingaleDocument18 pagesFlorence NightingaleCarolina Alejandra Hernández GálvezPas encore d'évaluation
- Unit 2 Evidence Based Nursing PracticeDocument94 pagesUnit 2 Evidence Based Nursing Practicenoo.wann100% (2)
- PAPER 3 Nursing PhenomenonDocument7 pagesPAPER 3 Nursing PhenomenonMhel Es QuiadPas encore d'évaluation
- Level of Knowledge and Attitude Among Nursing Students Toward Patient Safety and Medical ErrorsDocument125 pagesLevel of Knowledge and Attitude Among Nursing Students Toward Patient Safety and Medical ErrorshanadiPas encore d'évaluation
- Autism, It Is Discussed Why People Started Believing That Vaccines Cause Autism. There Was ADocument8 pagesAutism, It Is Discussed Why People Started Believing That Vaccines Cause Autism. There Was Aapi-301643808Pas encore d'évaluation
- Current Trends in Nursing EducaionDocument14 pagesCurrent Trends in Nursing EducaionArchana SahuPas encore d'évaluation
- Analyse Nursing Data PDFDocument22 pagesAnalyse Nursing Data PDFRika FatmadonaPas encore d'évaluation
- Case Study CovidDocument6 pagesCase Study CovidAngel Faith TirolPas encore d'évaluation
- Perceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesDocument14 pagesPerceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesRhod Bernaldez EstaPas encore d'évaluation
- Nursing ImageDocument10 pagesNursing Imageapi-392400343Pas encore d'évaluation
- PJN Jan June 2021 Final Version CompleteDocument130 pagesPJN Jan June 2021 Final Version CompleteJohn Vincent LacuestaPas encore d'évaluation
- Scope of NursingDocument27 pagesScope of NursingBlanche Gonzalez100% (2)
- Evidence Based Practice in NursingDocument3 pagesEvidence Based Practice in NursingThrift Advisory100% (2)
- Lifelong Learning TheoryDocument21 pagesLifelong Learning TheoryXieng TiocoPas encore d'évaluation
- Ethical PrinciplesDocument6 pagesEthical PrinciplesSammy ChegePas encore d'évaluation
- ICU Admission, Discharge, and Triage GuidelinesDocument9 pagesICU Admission, Discharge, and Triage Guidelinesugi 23Pas encore d'évaluation
- Ethical CompetenceDocument28 pagesEthical CompetenceRysanPas encore d'évaluation
- Caring in NursingDocument60 pagesCaring in NursingChadrie SanchezPas encore d'évaluation
- Ethical Dilemmas Experienced by Nurses in Providing Care For Critically Ill Patients in Intensive Care Units, Medan, IndonesiaDocument9 pagesEthical Dilemmas Experienced by Nurses in Providing Care For Critically Ill Patients in Intensive Care Units, Medan, Indonesiaravibunga4489Pas encore d'évaluation
- Nurse ManagerDocument10 pagesNurse Managerapi-282133920100% (1)
- Thesis Male in NursingDocument64 pagesThesis Male in Nursingljago278512Pas encore d'évaluation
- The Lived Experience of NursesDocument161 pagesThe Lived Experience of NursesGermán AchuryPas encore d'évaluation
- Rawls' Theory of JusticeDocument13 pagesRawls' Theory of JusticeLarry MagallanoPas encore d'évaluation
- Journal 1 - Technology in Nursing - FinalDocument47 pagesJournal 1 - Technology in Nursing - FinalEmilio Antang JrPas encore d'évaluation
- Work-Related Stress in NursingDocument49 pagesWork-Related Stress in Nursinga_l_y_nPas encore d'évaluation
- Nursing DefinitionDocument30 pagesNursing Definitionaibuty100% (2)
- Human To Human Relationship ModelDocument4 pagesHuman To Human Relationship Modelrj carpsonPas encore d'évaluation
- Integrative Literature ReviewDocument23 pagesIntegrative Literature Reviewapi-428103455100% (1)
- Hospital Management Services, Inc - Medical Center Manila, Petitioner, vs. EmployeesDocument2 pagesHospital Management Services, Inc - Medical Center Manila, Petitioner, vs. EmployeesPrhyllePas encore d'évaluation
- Role Development AssignmentDocument9 pagesRole Development AssignmentElizabeth HoPas encore d'évaluation
- Nursing Theory PaperDocument5 pagesNursing Theory Paperapi-268670617Pas encore d'évaluation
- The Future of Nursing Service RegulationDocument81 pagesThe Future of Nursing Service RegulationthatiePas encore d'évaluation
- Nurses' Job Burnout and Job Satisfaction During The COVID-19 Pandemic in The PhilippinesDocument14 pagesNurses' Job Burnout and Job Satisfaction During The COVID-19 Pandemic in The PhilippinesShan AlejosPas encore d'évaluation
- Nursing TheoristsDocument18 pagesNursing TheoristsDanielle Elizabeth Andres100% (1)
- Global Trends and Issues in NursingDocument27 pagesGlobal Trends and Issues in NursingDolly Jiljith100% (1)
- Fields of Specialization in NursingDocument6 pagesFields of Specialization in NursingBella IsananPas encore d'évaluation
- Quantitative Research DesignDocument19 pagesQuantitative Research DesignAli Ahmed GhouriPas encore d'évaluation
- Huacasi White Paper WeeblyDocument11 pagesHuacasi White Paper Weeblyapi-397532577Pas encore d'évaluation
- Essential Iii-2Document12 pagesEssential Iii-2api-318152697Pas encore d'évaluation
- Lauren Vandaniker Technology Impact On Nursing PracticeDocument19 pagesLauren Vandaniker Technology Impact On Nursing PracticeAllysaPas encore d'évaluation
- Removal of Sharp Object Patient SaftyDocument6 pagesRemoval of Sharp Object Patient SaftyAlibaba AlihaihaiPas encore d'évaluation
- Alarm Safety Anf FatigueDocument16 pagesAlarm Safety Anf FatigueRaquel Olivares SanchezPas encore d'évaluation
- WFCCN Chapter 4 Safety-and-Quality-in-the-ICU 2nd EditionDocument13 pagesWFCCN Chapter 4 Safety-and-Quality-in-the-ICU 2nd EditionJuan Carlos Mora TorresPas encore d'évaluation
- Cee 2005 - 06Document129 pagesCee 2005 - 06iloveeggxPPas encore d'évaluation
- Gerin Bagaslino - 52417512Document13 pagesGerin Bagaslino - 52417512Gerin BagaslinoPas encore d'évaluation
- Fichas Slate HoneywellDocument1 pageFichas Slate HoneywellING CARLOS RAMOSPas encore d'évaluation
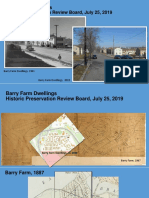
- Barry Farm Powerpoint SlidesDocument33 pagesBarry Farm Powerpoint SlidessarahPas encore d'évaluation
- Augmented FeedbackDocument54 pagesAugmented FeedbackAhmad KhuwarizmyPas encore d'évaluation
- M4-Lesson Transitional SignalDocument50 pagesM4-Lesson Transitional SignalJeneros PartosPas encore d'évaluation
- JurnalDocument24 pagesJurnaltsania rahmaPas encore d'évaluation
- DBR G+24 Building ProjectDocument28 pagesDBR G+24 Building ProjectShobhit Mohta100% (1)
- BharathDocument2 pagesBharathbharath kumarPas encore d'évaluation
- Affective DomainDocument3 pagesAffective DomainJm Enriquez Dela Cruz50% (2)
- Project PlanDocument8 pagesProject PlanRodsheen100% (1)
- Specification of SGP InterlayerDocument3 pagesSpecification of SGP InterlayerHAN HANPas encore d'évaluation
- Potential Application of Orange Peel (OP) As An Eco-Friendly Adsorbent For Textile Dyeing EffluentsDocument13 pagesPotential Application of Orange Peel (OP) As An Eco-Friendly Adsorbent For Textile Dyeing EffluentsAnoif Naputo AidnamPas encore d'évaluation
- Morning Report: Supervisor: Dr. H. Doddy Ak., Spog (K)Document10 pagesMorning Report: Supervisor: Dr. H. Doddy Ak., Spog (K)vika handayaniPas encore d'évaluation
- Computer Graphics Question For Final ExamDocument3 pagesComputer Graphics Question For Final ExamMd Rifat BhuiyanPas encore d'évaluation
- Control Panel Manual 1v4Document52 pagesControl Panel Manual 1v4Gustavo HidalgoPas encore d'évaluation
- IBRO News 2004Document8 pagesIBRO News 2004International Brain Research Organization100% (1)
- Tips Experiments With MatlabDocument190 pagesTips Experiments With MatlabVishalPas encore d'évaluation
- Cultural GlobalizationDocument16 pagesCultural Globalizationee0785Pas encore d'évaluation
- Internship Report On Service IndustryDocument50 pagesInternship Report On Service Industrybbaahmad89Pas encore d'évaluation
- Gender InequalityDocument9 pagesGender InequalityRhzPas encore d'évaluation
- (Herbert Kitschelt, Steven I. Wilkinson) Patrons, PDFDocument387 pages(Herbert Kitschelt, Steven I. Wilkinson) Patrons, PDFClemente Tomás Sánchez BarjaPas encore d'évaluation
- D027B OmronDocument141 pagesD027B OmronirfanWPKPas encore d'évaluation
- Multithreading AlgorithmsDocument36 pagesMultithreading AlgorithmsAsna TariqPas encore d'évaluation
- Network Management Systems 10CS834 PDFDocument113 pagesNetwork Management Systems 10CS834 PDFSarfraz AhmedPas encore d'évaluation
- Spinning CalculationDocument178 pagesSpinning Calculationamboklate69% (16)
- Sop For RetailDocument13 pagesSop For Retailkarthika suresh100% (6)
- PERFORM Toolkit 3 1 Release Notes 1.0 OnlinePDFDocument18 pagesPERFORM Toolkit 3 1 Release Notes 1.0 OnlinePDFJose HugoPas encore d'évaluation
- The Doppler EffectLDocument2 pagesThe Doppler EffectLintan100% (1)
- The Structure of Deception: Validation of The Lying Profile QuestionnaireDocument16 pagesThe Structure of Deception: Validation of The Lying Profile QuestionnaireNancy DrewPas encore d'évaluation