Académique Documents
Professionnel Documents
Culture Documents
CSIM2.26 - Pituitary Function
Transféré par
AinahMahaniTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CSIM2.26 - Pituitary Function
Transféré par
AinahMahaniDroits d'auteur :
Formats disponibles
CSIM2.
26 Pituitary function
Pituitary tumours
Pathology
1. pituitary adenoma
a. functional tumours
b. non-functional
2. craniopharyngioma
3. tumours around the pituitary
4. secondary tumours
a. metastases
Local effects
1. Hypopituitarism
2. Chiasmal compression
a. Neuro-opthalmic dysfunction
b. Loss of visual acuity
c. Visual field defects
Bitemporal hemianopia
3. CN palsy
4. Obstructive hydrocephalus
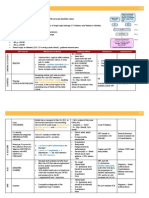
Anterior pituitary
Thyroid
Adrenal
Pituitary
hormone
TSH
ACTH
Gonadal
FH, LSH
GH
GH
System
System
Thyroid
Adrena
l
Gonada
l
GH
Hormo
ne
TSH
Target
Hormone
T4, T3
ACTH
Cortisol
FH, LSH
GH
Target
Hormone
T4, T3
Cortisol
Testosterone,
E2
IGF-1
Testosterone,
E2
IGF-1
Insufficiency
Primary
Secondary
TSH, FT4/T3
TSH, FT4/T3
ACTH, cortisol
ACTH, cortisol
LH/FSH, Testo/E2
LH/FSH,
Testo/E2
Doesnt apply
Excess
Insufficient
Thyrotoxicosis
Cushings Disease
Reproductive Dysf(x)
Acromegaly
A. Prolactin Excess Hyperprolactinaemia
Causes
Clinical Features
1. drug induced
a. dopamine antagonists
b. antidepressants
c. opiates
2. functional pituitary tumour
a. microadenoma
b. macroadenoma
3. non-functioning tumour
a. disruption of hypophyseal-portal
tract
1. hypogonadism
a. secondary ammenorrhoea
b. sub-fertility
c. loss of libido
2. galactorrhoea (milk when not lactating)
Funtional Pituitary Tumour
Management
1. Dopamine agonist; Bromocriptine, cabergoline
2. Tumour control; Prolactin, tumour size, hypogonadism (testosterone)
B. Growth Hormone Excess
GH secreting pituitary tumour
Clinical features
Soft tissue overgrowth: Hand, feet, face, linear growth if pre-pubertal
Headache
Sweating
HPT
Hyperglycaemia
OA
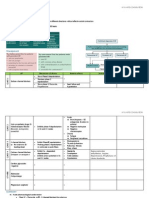
Posterior
System
Pituitary
hormone
Kidney/Arteri
oles
AVP
Uterus
Oxytoxin
Target
Hormone
Insufficiency
Primary
Secondary
Diabetes Insipidus
1.
2.
3.
4.
5.
Coordinated physiology of AVP and thirst
Maintenance of plasma Na+
Balancing water input & output (AVP, thirst)
Defect in AVP production or action
Polyuria with dilute urine. 3 types: hypothalamic AVP deficiency (absolute vs relative),
nephrogenic (renal AVP resistance), and dipsogenic (excess fluid intake)
Hypothalamic DI
Acquired
1. tumour
a. craniopharyngioma
b. germ cell tumour
2. trauma
3. vascular
4. inflammatory
a. hypophysitis
b. LCH & sarcoid
5. idiopathic
a. autoimmune
Congenital/genetic
1. developmental
a. SOD
2. autosomal dominant
3. autosomal recessive
4. syndromic
a. Wolframs syndrome
Key points to remember:
1. Diabetes Insipidus: There is a low level of ADH produced
- Low Level of ADH equals excessive urinary output
2. SIADH: There is a high level of ADH produced
- High Level of ADH equals low urinary output
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Csim2.26 - Pituitary F (X) Unusual DiabetesDocument2 pagesCsim2.26 - Pituitary F (X) Unusual DiabetesAinahMahaniPas encore d'évaluation
- Penilaian Bahan TamhidiDocument3 pagesPenilaian Bahan TamhidiAinahMahaniPas encore d'évaluation
- Urinary IncontinenceDocument1 pageUrinary IncontinenceAinahMahaniPas encore d'évaluation
- Csim2.26 - Pituitary F (X)Document1 pageCsim2.26 - Pituitary F (X)AinahMahaniPas encore d'évaluation
- CPTP - Pud + Altered Bowel HabitDocument3 pagesCPTP - Pud + Altered Bowel HabitAinahMahaniPas encore d'évaluation
- Csim2.94 - Interstitial Lung DiseaseDocument3 pagesCsim2.94 - Interstitial Lung DiseaseAinahMahaniPas encore d'évaluation
- Csim2.25 - Electrolyte Imbalance Iron Metabolism & StorageDocument1 pageCsim2.25 - Electrolyte Imbalance Iron Metabolism & StorageAinahMahaniPas encore d'évaluation
- Csim2.25 - Iron Metabolism & StorageDocument4 pagesCsim2.25 - Iron Metabolism & StorageAinahMahaniPas encore d'évaluation
- Csim2.25 - Electrolyte ImbalanceDocument4 pagesCsim2.25 - Electrolyte ImbalanceAinahMahaniPas encore d'évaluation
- Csim2.92 - HypoventilationDocument1 pageCsim2.92 - HypoventilationAinahMahaniPas encore d'évaluation
- CSIM2.24 - Signal TransductionDocument6 pagesCSIM2.24 - Signal TransductionAinahMahaniPas encore d'évaluation
- CPTP - Pregnancy & LactatingDocument1 pageCPTP - Pregnancy & LactatingAinahMahaniPas encore d'évaluation
- Csim2.25 - Electrolyte Imbalance Calcium and BoneDocument7 pagesCsim2.25 - Electrolyte Imbalance Calcium and BoneAinahMahaniPas encore d'évaluation
- Csim2.71 - The Patient With Proteinuria and HaematuriaDocument11 pagesCsim2.71 - The Patient With Proteinuria and HaematuriaAinahMahaniPas encore d'évaluation
- CSIM2.91 - COPD and Pulmonary HypertensionDocument2 pagesCSIM2.91 - COPD and Pulmonary HypertensionAinahMahaniPas encore d'évaluation
- CSIM2.90 - Occupational AsthmaDocument1 pageCSIM2.90 - Occupational AsthmaAinahMahaniPas encore d'évaluation
- CPTP - Infection and Antibiotics 2Document3 pagesCPTP - Infection and Antibiotics 2AinahMahaniPas encore d'évaluation
- CPTP - Poisonig MH Misuse of DrugsDocument5 pagesCPTP - Poisonig MH Misuse of DrugsAinahMahaniPas encore d'évaluation
- CPTP - PainDocument3 pagesCPTP - PainAinahMahaniPas encore d'évaluation
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniPas encore d'évaluation
- Penilaian Bahan MUAYYIDDocument3 pagesPenilaian Bahan MUAYYIDAinahMahaniPas encore d'évaluation
- CPTP - Parkinson & MVMT DisordersDocument2 pagesCPTP - Parkinson & MVMT DisordersAinahMahaniPas encore d'évaluation
- CPTP - HPT & HFDocument4 pagesCPTP - HPT & HFAinahMahaniPas encore d'évaluation
- CPTP - EpilepsyDocument4 pagesCPTP - EpilepsyAinahMahaniPas encore d'évaluation
- CPTP - Diabetes and Lipid Lowering DrugsDocument4 pagesCPTP - Diabetes and Lipid Lowering DrugsAinahMahaniPas encore d'évaluation
- CPTP - Asthma & CopdDocument5 pagesCPTP - Asthma & CopdAinahMahaniPas encore d'évaluation
- CPTP - Af & Anti CoagulationDocument4 pagesCPTP - Af & Anti CoagulationAinahMahaniPas encore d'évaluation
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniPas encore d'évaluation
- Themed Week 7 - LIVERDocument24 pagesThemed Week 7 - LIVERAinahMahaniPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Fisiologi Saraf OtonomDocument32 pagesFisiologi Saraf OtonomNiaPas encore d'évaluation
- Changes To Breast Structure and Function Across ADocument12 pagesChanges To Breast Structure and Function Across AMauricio MoncadaPas encore d'évaluation
- 5.-Pancreatita-Cronica ...Document12 pages5.-Pancreatita-Cronica ...Enache MihaiPas encore d'évaluation
- Cardiovascular Physiology 4 - Gomez MD PDFDocument65 pagesCardiovascular Physiology 4 - Gomez MD PDFMelissa SalayogPas encore d'évaluation
- Breathing For Singing-The Anatomy of RespirationDocument11 pagesBreathing For Singing-The Anatomy of RespirationAnurrag Kumar100% (3)
- DAMS CBT 2015 Test -1 ReviewDocument173 pagesDAMS CBT 2015 Test -1 ReviewMitvinder SinghPas encore d'évaluation
- First M.B.B.S. Examination January - 2021 Physiology Paper-I - (Old)Document2 pagesFirst M.B.B.S. Examination January - 2021 Physiology Paper-I - (Old)veerkokani2005Pas encore d'évaluation
- L11 - Anatomy of The SkullDocument36 pagesL11 - Anatomy of The SkullSivakumar Kathuu KarthikeyanPas encore d'évaluation
- Triangles FlowChartDocument1 pageTriangles FlowChartDjalel ChkounPas encore d'évaluation
- Holes Human Anatomy and Physiology 12Th Edition Shier Test Bank Full Chapter PDFDocument53 pagesHoles Human Anatomy and Physiology 12Th Edition Shier Test Bank Full Chapter PDFJakeOwensbnpm100% (9)
- Referat Carpal Tunnel SyndromeDocument25 pagesReferat Carpal Tunnel Syndromegede andreasPas encore d'évaluation
- Lower Back PainsDocument35 pagesLower Back PainsMary Les RN100% (1)
- NEET Chemical Control and Coordination Important QuestionsDocument14 pagesNEET Chemical Control and Coordination Important QuestionsAditiPas encore d'évaluation
- Histology DigestiveDocument87 pagesHistology DigestiveAnang Yanuar RamadhanPas encore d'évaluation
- Shoulder Muscles Origin and FunctionDocument8 pagesShoulder Muscles Origin and FunctionSyeda Bint E KhalilPas encore d'évaluation
- Sullivan Siegelman Retention Exam With AnswersDocument9 pagesSullivan Siegelman Retention Exam With AnswersJed A. MartirPas encore d'évaluation
- Anatomy State Exam1Document12 pagesAnatomy State Exam1Manisanthosh KumarPas encore d'évaluation
- Endocrine System Anatomy and Physiology - NurseslabsDocument29 pagesEndocrine System Anatomy and Physiology - NurseslabsAlyssum Marie50% (2)
- Muscular SystemDocument41 pagesMuscular SystemGem Rose UretaPas encore d'évaluation
- The Heart Has Several Pacemakers Known As Autonomic FociDocument1 pageThe Heart Has Several Pacemakers Known As Autonomic FociAnonymous mLYupGyNPas encore d'évaluation
- SCR January 2021 SampleDocument13 pagesSCR January 2021 SampleDima KotPas encore d'évaluation
- Enteric Nervous SystemDocument5 pagesEnteric Nervous Systemmehdi mafakheriPas encore d'évaluation
- Mastering Handstands and Beyond by Lee WeilandDocument74 pagesMastering Handstands and Beyond by Lee WeilandRayen HamrouniPas encore d'évaluation
- 34 Pictures That Show You Exactly What Muscles You'Re StretchingDocument20 pages34 Pictures That Show You Exactly What Muscles You'Re StretchingAnkit DalmiaPas encore d'évaluation
- Bill Starr - Strong To The Core 3Document6 pagesBill Starr - Strong To The Core 3TomSusPas encore d'évaluation
- PNF Techniques in The Upper ExtremityDocument27 pagesPNF Techniques in The Upper ExtremitysanalcrazyPas encore d'évaluation
- CH 7 The Nervous SystemDocument4 pagesCH 7 The Nervous Systemapi-267543553Pas encore d'évaluation
- Blanko Permintaan Pemeriksaan RadiologiDocument4 pagesBlanko Permintaan Pemeriksaan Radiologijoko suhartonoPas encore d'évaluation
- Ent Trauma DanuDocument52 pagesEnt Trauma Danudanu100% (1)
- Pron 1993Document10 pagesPron 1993Javiera Paz Rios CarmonaPas encore d'évaluation