Académique Documents
Professionnel Documents
Culture Documents
Case Study
Transféré par
Radenroro Atih Utari RizkyCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Case Study
Transféré par
Radenroro Atih Utari RizkyDroits d'auteur :
Formats disponibles
Running head: NURSING CARE FOR A PATIENT SCENARIO
Case Study Nursing Care for a Patient Scenario (Mrs. Jones)
Customers Name
Academic Institution
NURSING CARE FOR A PATIENT SCENARIO
Case Study Nursing Care for a Patient Scenario (Mrs. Jones)
Nursing Care Plan
Area(s): Nutrition and Hydration
Nursing diagnosis (1). Nutrition: Imbalanced, less than body requirements related to
inability to ingest or digest food or absorb nutrients because of physiologic alterations secondary
to medication regimen, as evidenced by weight loss of 10 kg in the past four months (or 14.3%
weight loss from 70 kg in October 2009).
Goals/desired outcomes. Within the duration of care, Mrs. Jones will be able to:
Demonstrate interest/behaviors to improve her nutrition, thereby paving the way towards
proper nutrition and progressive regain of her previous weight (Doenges, Moorhouse and
Geissler-Murr, 2004).
Nursing interventions based on Doenges, Moorhouse and Geissler-Murr (2004, pp. 347352):
1. Determine the clients ability to chew, swallow, and taste or any dietary restrictions.
Rationale: This determines the factors affecting ingestion, digestion, and food intake.
2. Encourage the client to verbalize her thoughts and feelings about her current situation,
diet, and nutrition.
Rationale: This facilitates assessment and identification of the clients very own needs
and perceptions about her nutrition, thereby leading to individualized care.
3. Encourage the client to choose foods according to her own preferences or foods that are
appealing to her, with due consideration to any prescribed diet.
NURSING CARE FOR A PATIENT SCENARIO
Rationale: This stimulates the clients interest and appetite, at the same time, considering
the recommended diet for the client.
4. Promote pleasant and relaxing environment as well as socialization.
Rationale: Utilization of the environment to enhance food intake.
5. Consult a dietician or nutritionist to cater for the clients nutritional needs.
Rationale: This facilitates experts advice and tailoring of a nutritional plan suited for
Mrs. Joness unique nutritional needs, as well as facilitating collaborative care.
Nursing diagnosis (2). Failure to thrive, adult related to major disease(s) (uterine cancer
and fracture of left neck of femur), as evidenced by apparent unintentional weight loss of 14.3%
for the past 4 months.
Goals/desired outcomes. Within the duration of care, Mrs. Jones will be able to:
Demonstrate interest/behaviors and lifestyle changes to improve her well-being and
nutrition.
Nursing interventions according to doenges, moorhouse and geissler-murr (2004, pp.
214-216):
1. Perform physical and psychosocial assessment.
Rationale: This is to determine the extent of limitations affecting Mrs. Joness ability to
thrive.
2. Explore Mrs. Joness previously used coping mechanisms that may be applied to her
current situation.
Rationale: This refines or further develops the clients coping strategies.
3. Encourage the significant others (SOs) to participate in the management/care of the
client.
NURSING CARE FOR A PATIENT SCENARIO
Rationale: This strengthens the clients support system, thereby enabling her to cope and
thrive.
Area: Skin Integrity
Nursing diagnosis (1). Skin integrity, risk for impaired (Mrs. Joness risk factors: Fractured
left neck of femur, old age, and altered nutrition, as well as braden pressure ulcer risk assessment
tool score of 16 signifying mild risk).
Goals/desired outcomes. Within the duration of care, Mrs. Jones will be able to:
Display interest/behaviors leading to reduced risks for impaired skin integrity.
Nursing interventions based on Doenges, Moorhouse and Geissler-Murr (2004, pp. 465468):
1. Provide information to the client and SOs about the importance of regular observation
and effective skin care as well as proper nutrition and hydration.
Rationale: This promotes skin turgor and reduction of risks for impaired skin integrity.
2. Inspect skin routinely and observe for reddened/blanched areas and implement treatment
promptly, if irregularities are evident.
Rationale: This reduces the likelihood of progression to skin breakdown.
3. Keep the clients bed linen dry and free of wrinkles and crumbs.
Rationale: This reduces the risks of skin injury by preventing pressure and possible
friction.
Area: Continence
Nursing diagnosis (1). Urinary incontinence, urge related to irritation of bladder stretch
receptors causing spasm secondary to Urinary Tract Infection (UTI).
Goals/desired outcomes. Within the duration of care, Mrs. Jones will be able to:
NURSING CARE FOR A PATIENT SCENARIO
Display behaviors/techniques to control/correct situation (incontinence).
Nursing interventions:
1. Measure Mrs. Joness amount of urine voided, especially noting amounts less than 100 cc
or greater than 550 cc (Doenges, Moorhouse and Geissler-Murr, 2004, p.574).
Rationale: This is to assess the degree of bladder disability to control urination.
2. Regulate Mrs. Joness liquid intake at prescheduled times (with and between meals) and
keep a continence record for 3 days (Berman, Snyder, Kozier, & Erb, 2008, p. 1296;
Doenges, Moorhouse and Geissler-Murr, 2004, p. 574).
Rationale: To promote a predictable voiding pattern.
3. Encourage Mrs. Jones to start and stop stream for two or more times during voiding
(Doenges, Moorhouse and Geissler-Murr, 2004, p.574).
Rationale: This isolates muscles involved in voiding process for exercise training.
4. Teach Mrs. Jones about Kegel exercises or the use of vaginal cones (Doenges,
Moorhouse and Geissler-Murr, 2004, p.574).
Rationale: This is to strengthen the pelvic floor and enhance bladder training exercises,
thereby counteracting incontinence and promoting proper urinary elimination.
5. Encourage Mrs. Jones to consciously delay voiding (Doenges, Moorhouse and GeisslerMurr, 2004).
Rationale: To gradually increase intervals between voiding to every 2 to 4 hours.
6. Suggest to Mrs. Joness family to have an adequate lighting during nighttime as well as to
install grab bars and elevated toilet seats as needed (Berman et al., 2008, p. 1298).
Rationale: To promote comfort and safety.
NURSING CARE FOR A PATIENT SCENARIO
Nursing Diagnosis (2). Urinary elimination, impaired related to urinary tact infection (uti),
as evidenced by incontinence.
Goals/desired outcomes. Within the duration of care, Mrs. Jones will be able to:
Display/verbalize understanding of the condition in order to achieve normal elimination
pattern.
Demonstrate behaviors/techniques to prevent the further complication and recurrence of
urinary tract infection (Doenges, Moorhouse and Geissler-Murr, 2004, p.555).
Nursing interventions:
1. Inform the client that women are more susceptible to UTI because of the shorter size of
the urethra (Berman et al., 2008, p. 1297; Doenges, Moorhouse and Geissler-Murr, 2004,
p. 555).
Rationale: To provide knowledge of the clients condition, thereby promoting utmost
understanding.
2. Encourage Mrs. Jones and the SOs to drink adequate amount of fluids, that is, about eight
to ten 8-ounce glasses of water or up to 3000 ml, with cardiac tolerance, daily (Berman et
al., 2008, p. 1298; Doenges, Moorhouse and Geissler-Murr, 2004, p. 557).
Rationale: To promote micturition (or urination), thereby flushing away the
microorganisms from the urethra (Potter and Perry, 2001, p.1411). Including the
family/SOs in the health teaching/education facilitates involvement in the care of the
client. Nevertheless, cardio-clearance must also be taken into consideration to prevent
fluid overload.
NURSING CARE FOR A PATIENT SCENARIO
3. Teach or instruct Mrs. Jones and female family members to wipe from front to back
(from the urinary meatus toward the anus) every after voiding (Berman et al., 2008, p.
1298; Doenges, Moorhouse and Geissler-Murr, 2004, p. 557).
Rationale: Cleaning from dirtiest to cleanest area promotes asepsis, thereby preventing
UTI.
4. Encourage Mrs. Jones to complete the full course of the prescribed medication regimen
for UTI and inform her about the actions, adverse effects and other pertinent information
about the drugs (Berman et al., 2008, p. 1298).
Rationale: This is to ensure effectiveness of the treatment. Educating the client about the
actions and adverse effects of the medications enables the client to promptly report any
untoward reactions that the client may be experiencing.
5. Monitor the effectiveness of the prescribed antibiotics and subsequently send the urine
samples to the laboratory (Doenges, Moorhouse and Geissler-Murr, 2004, p.557).
Rationale: This is to evaluate the effectiveness of the medication regimen.
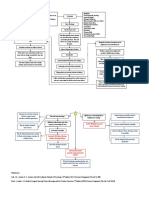
Assessment Tool
Bradens Tool Score for Mrs. Jones pre #NOF: 20 (See Appendix A for further details)
Bradens Tool Score for Mrs. Jones post #NOF: 16 = Mild Risk
Differences between 2 Scores:
The difference between the above 2 scores signifies the apparent alteration of Mrs.
Joness mobility. Her fracture predisposes her to pressure ulcer formation, though it is of mild
risk only (Bradens Tool score of 16).
Comment on Ease of Use (For Tool):
NURSING CARE FOR A PATIENT SCENARIO
The Braden Pressure Ulcer Risk Assessment Tool is somewhat easy to use because it
provides choices that enable us to clearly picture-out or depict the scenario, thereby leading us to
give the appropriate score suitable for the client.
Group Member Agreement/Disagreement of Assessment: The group was completely in
consensus about the scoring and assessment done.
Any Problems with Tool Used:
So far, there are no problems encountered with the use of the tool.
Other Risk Assessment Tools Identified:
1. Norton scale/nortons pressure area risk assessment form scale was the first pressure
ulcer risk assessment reported in the literature. It scores five risk factors namely, physical
condition, mental condition, activity, mobility, and incontinence, wherein the total score
ranges from 5 to 20 (Berman et al., p. 905; Potter and Perry, 2001, p. 1557).
2. Gosnell scale developed from a research on 30 clients in a nursing home, this scale scores
five factors that include mental status, continence, mobility, activity, and nutrition (Potter
and Perry, 2001, p.1557).
Frequency of Assessment:
Constantly (Potter and Perry, 2001, p.1557).
NURSING CARE FOR A PATIENT SCENARIO
Appendix A
PRE #LNOF
NURSING CARE FOR A PATIENT SCENARIO
POST #LNOF
Note: Image taken from Government of Alberta Seniors and Community Supports (2010)
10
NURSING CARE FOR A PATIENT SCENARIO
11
References
Berman, A., Snyder, S. J., Kozier, B. & Erb, G. (2008). Kozier & Erbs fundamentals of nursing:
Concepts, process, and practice (8th ed., p. 905 & pp. 1296-1298). Upper Saddle River,
New Jersey: Pearson Prentice Hall.
Government of Alberta Seniors and Community Supports. (2010). Braden pressure ulcer risk
assessment tool. Retrieved from
http://www.seniors.gov.ab.ca/AADL/AV/manual/PDF/58_braden_assessment_tool.pdf
Doenges, M. E., Moorhouse, M. F., & Geissler-Murr, A. C. 2004). Nurses pocket guide:
Diagnoses, interventions, and rationales (9th ed., pp. 214-216, pp. 347-352, pp. 465-468,
p.555, p.557, & p. 574). Philadelphia: F.A. Davis Company.
Potter, P. A., & Perry, A. G. (2001). Fundamentals of nursing. (5th ed., p.1557). St. Louis:
Mosby.
Vous aimerez peut-être aussi
- Management of Tuberculosis: A guide for clinicians (eBook edition)D'EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Pas encore d'évaluation
- Triamcinolone (Topical) - Drug InformationDocument5 pagesTriamcinolone (Topical) - Drug InformationMauricio Sv0% (1)
- 6 Nursing Care Plan 1Document2 pages6 Nursing Care Plan 1Denise Louise PoPas encore d'évaluation
- USC Case 04 - SinusitisDocument9 pagesUSC Case 04 - SinusitisDisti Damelia SebayangPas encore d'évaluation
- Assessment Pathophysiology Objectives Interventions Rationale EvaluationDocument3 pagesAssessment Pathophysiology Objectives Interventions Rationale Evaluationjesa_olivePas encore d'évaluation
- A Case PresentationDocument50 pagesA Case PresentationAnaleah MalayaoPas encore d'évaluation
- Knowledge DeficitDocument5 pagesKnowledge DeficitteamstrocaPas encore d'évaluation
- NCP For Dehydration 1Document3 pagesNCP For Dehydration 1Khalid KhanPas encore d'évaluation
- ThyroidectomyDocument11 pagesThyroidectomySherina W. EddingPas encore d'évaluation
- Research ProposalDocument22 pagesResearch ProposalKapil LakhwaraPas encore d'évaluation
- Ineffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemDocument5 pagesIneffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemAndrea Albester GarinoPas encore d'évaluation
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument1 pageAssessment Diagnosis Planning Intervention Rationale EvaluationFranz RolfPas encore d'évaluation
- Nursing Care Plan: Subjective: During 8 Hours Nursing Management: (5) After 8 HoursDocument4 pagesNursing Care Plan: Subjective: During 8 Hours Nursing Management: (5) After 8 HoursRawan KhateebPas encore d'évaluation
- 4 Flow Chart PretermDocument4 pages4 Flow Chart PretermYeni PuspitaPas encore d'évaluation
- Post Cesarean Section DeliveryDocument5 pagesPost Cesarean Section Deliveryᒙᕧᖇᕦᙏᖻ ᗴᔛᓦᗩᖆᗩPas encore d'évaluation
- Ortho NCPDocument1 pageOrtho NCPErjohn Vincent Lim100% (1)
- Drug StudyDocument2 pagesDrug Studydwyane0033Pas encore d'évaluation
- Pneumonia Drug StudyDocument3 pagesPneumonia Drug Studyatienza02Pas encore d'évaluation
- HydroxyzineDocument4 pagesHydroxyzineGeorge Smith AbeledaPas encore d'évaluation
- HernioplastyDocument6 pagesHernioplastyCherry Delos ReyesPas encore d'évaluation
- Case Report - Deep Vein ThrombosisDocument12 pagesCase Report - Deep Vein ThrombosisAndi Meidin AnugerahPas encore d'évaluation
- Albendazole - Drug Information PDFDocument7 pagesAlbendazole - Drug Information PDFjjjkkPas encore d'évaluation
- PyelonephritisDocument59 pagesPyelonephritisGheyl GabrielPas encore d'évaluation
- TAHBSO ReportDocument4 pagesTAHBSO ReportsachiiMePas encore d'évaluation
- NCP For AsthmaDocument2 pagesNCP For AsthmawaadPas encore d'évaluation
- Drug-Study NCPDocument5 pagesDrug-Study NCPMURILLO, FRANK JOMARI C.Pas encore d'évaluation
- NCP Alzheimers DiseaseDocument2 pagesNCP Alzheimers DiseaseShawn TejanoPas encore d'évaluation
- Acute Pyelonephritis Nursing Care PlansDocument2 pagesAcute Pyelonephritis Nursing Care PlansJoannah Marie Juloya Kiat-ong100% (1)
- PneumoniaDocument2 pagesPneumoniaPia MedinaPas encore d'évaluation
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityJayson OlilePas encore d'évaluation
- 5 Drug StudyDocument14 pages5 Drug StudyJennyLapitan100% (2)
- ParacetamolDocument2 pagesParacetamolsleep whatPas encore d'évaluation
- Concept Map - Colon CancerDocument2 pagesConcept Map - Colon Cancerbea pegadPas encore d'évaluation
- NCP LeukemiaDocument5 pagesNCP LeukemiaTriciaPas encore d'évaluation
- Asthalin InhalerDocument5 pagesAsthalin InhalerRajib MandalPas encore d'évaluation
- Pathophysiology of FractureDocument2 pagesPathophysiology of Fracturemyer pasandalanPas encore d'évaluation
- NCPDocument2 pagesNCPAnne De VeraPas encore d'évaluation
- Clinical Learning ContractDocument3 pagesClinical Learning ContractKaragire vedastePas encore d'évaluation
- Nursing Care Plan On HypertensionDocument5 pagesNursing Care Plan On Hypertensionbhavana100% (1)
- Regañon - Rle Case # 1Document22 pagesRegañon - Rle Case # 1Darla Janyll RegañonPas encore d'évaluation
- Diphtheria SlideDocument11 pagesDiphtheria Slideandre andrePas encore d'évaluation
- Propranolol 1 PresentationDocument17 pagesPropranolol 1 Presentationapi-284092317100% (1)
- PEDIA CASE 3 FinalDocument9 pagesPEDIA CASE 3 FinalXandra BnnPas encore d'évaluation
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiPas encore d'évaluation
- Deficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Document3 pagesDeficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Vincent Paul SantosPas encore d'évaluation
- Community Mental Health Nursing 9+10Document24 pagesCommunity Mental Health Nursing 9+10Husam AabedPas encore d'évaluation
- NCP 1Document6 pagesNCP 1Maedine Urbano-BrionesPas encore d'évaluation
- LeptospirosisDocument9 pagesLeptospirosisDeepu VijayaBhanuPas encore d'évaluation
- JDM Care PlanDocument5 pagesJDM Care PlangopscharanPas encore d'évaluation
- Nursing Care PlanDocument20 pagesNursing Care PlanZamranosPas encore d'évaluation
- Case Study NCPDocument4 pagesCase Study NCPKelly OstolPas encore d'évaluation
- Oks Na To Thank U Aubs!!: Okiii!!! Wuv U All!Document10 pagesOks Na To Thank U Aubs!!: Okiii!!! Wuv U All!CiaraPas encore d'évaluation
- Drug Study - PiptazDocument1 pageDrug Study - PiptazMutya XDPas encore d'évaluation
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalantePas encore d'évaluation
- Papillary Thyroid Ca: Group. 1 B Grand CaseDocument16 pagesPapillary Thyroid Ca: Group. 1 B Grand CaseAdora Dela CruzPas encore d'évaluation
- Care Plan 2Document11 pagesCare Plan 2api-28474004567% (3)
- Cues Nursing Diagnosis Scientific Reason Planning Intervention Rationale EvaluationDocument6 pagesCues Nursing Diagnosis Scientific Reason Planning Intervention Rationale EvaluationKatrina Ponce86% (7)
- Nursing Care Plan For PostpartumDocument5 pagesNursing Care Plan For PostpartumTheeya Quigao91% (11)
- Nursing Plan of Care ErDocument6 pagesNursing Plan of Care Erapi-642989736Pas encore d'évaluation
- Range of Joint Motion Evaluation Chart: 1. Back 2. Lateral (Flexion)Document2 pagesRange of Joint Motion Evaluation Chart: 1. Back 2. Lateral (Flexion)Radenroro Atih Utari RizkyPas encore d'évaluation
- Penatalaksanaan Keperawatan Covid 19 Di Respiratory Ward AustraliaDocument22 pagesPenatalaksanaan Keperawatan Covid 19 Di Respiratory Ward AustraliaRadenroro Atih Utari RizkyPas encore d'évaluation
- Management of Hypokalaemia Clinical GuidelineDocument13 pagesManagement of Hypokalaemia Clinical GuidelineRadenroro Atih Utari RizkyPas encore d'évaluation
- Konsep EWS Di RSDocument50 pagesKonsep EWS Di RSRadenroro Atih Utari RizkyPas encore d'évaluation
- DokumenDocument3 pagesDokumenRadenroro Atih Utari RizkyPas encore d'évaluation
- UTIDocument57 pagesUTIGireesh NagaruruPas encore d'évaluation
- UTI TreatmentDocument3 pagesUTI TreatmentMaria RezitadinaPas encore d'évaluation
- 5W FeverDocument14 pages5W FeverYork GarcíaPas encore d'évaluation
- Pediatric Urinary Tract Infection: Aprianda Saputra/ANSDocument34 pagesPediatric Urinary Tract Infection: Aprianda Saputra/ANSAkbar DarajatPas encore d'évaluation
- Aromatherapy Essential Oils ChartDocument6 pagesAromatherapy Essential Oils Chartamalya_84100% (9)
- Group1a BSN219 Mothers-Case Final PDFDocument269 pagesGroup1a BSN219 Mothers-Case Final PDFLuis LazaroPas encore d'évaluation
- Abnormalities of The PuerperiumDocument59 pagesAbnormalities of The PuerperiumKENEDYPas encore d'évaluation
- Health Assessment SAS Session 17Document5 pagesHealth Assessment SAS Session 17pw49cbqxnfPas encore d'évaluation
- AUB - Microscopic Analysis of UrineDocument4 pagesAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- BookletDocument14 pagesBookletIndra KelanaPas encore d'évaluation
- Care Plan Risk For Infection 2Document3 pagesCare Plan Risk For Infection 2Chander KantaPas encore d'évaluation
- Bacte MnemonicsDocument10 pagesBacte MnemonicsIan Leo SantosPas encore d'évaluation
- History Taking in Urology-UndergraduateDocument12 pagesHistory Taking in Urology-Undergraduateasmaaburas100% (1)
- NCCLS Manual of Antimicrobial Susceptibility TestingDocument241 pagesNCCLS Manual of Antimicrobial Susceptibility TestingManu SantosPas encore d'évaluation
- Mccqe 1Document42 pagesMccqe 1Vinil Saratchandran100% (4)
- Approach To The Patient With Hematuria: Paul D. Simmons, MD St. Mary's Family Medicine Residency Grand JunctionDocument41 pagesApproach To The Patient With Hematuria: Paul D. Simmons, MD St. Mary's Family Medicine Residency Grand JunctionMichael Spica RampangileiPas encore d'évaluation
- Q-Bank (Micorbiology 1)Document102 pagesQ-Bank (Micorbiology 1)Ali DosaPas encore d'évaluation
- Cefotaxime 1g Powder For Solution For Injection or Infusion PL 14894 0397 Cefotaxime 2g Powder For Solution For Injection or Infusion PL 14894 0398Document48 pagesCefotaxime 1g Powder For Solution For Injection or Infusion PL 14894 0397 Cefotaxime 2g Powder For Solution For Injection or Infusion PL 14894 0398CongluanPas encore d'évaluation
- SHC Antimicrobial Dosing GuideDocument7 pagesSHC Antimicrobial Dosing GuideHelder LopesPas encore d'évaluation
- Antibiotic Pocket GuideDocument19 pagesAntibiotic Pocket GuideNaomi Liang100% (1)
- Pdfshare Prescribing Information: Mechanism of ActionDocument3 pagesPdfshare Prescribing Information: Mechanism of Actionmehul da aviatorPas encore d'évaluation
- Communication and Teaching With Children and FamiliesDocument29 pagesCommunication and Teaching With Children and FamiliesThrecia RotaPas encore d'évaluation
- Approach To A Patient With HaematuriaDocument21 pagesApproach To A Patient With HaematuriaMisbah KaleemPas encore d'évaluation
- Clean Intermittent Catheterization (CIC) : IndicationsDocument2 pagesClean Intermittent Catheterization (CIC) : IndicationsSri HariPas encore d'évaluation
- Notes On Formulation & Evaluation of Floating Microspheres of An Antibiotic DrugDocument66 pagesNotes On Formulation & Evaluation of Floating Microspheres of An Antibiotic DrugkeyurPas encore d'évaluation
- Dosha Gati NotesDocument5 pagesDosha Gati NotesbalatnPas encore d'évaluation
- Pediatric Genitourinary DisordersDocument7 pagesPediatric Genitourinary Disorderscayla mae carlosPas encore d'évaluation
- Nursing Sample Test 6Document5 pagesNursing Sample Test 6Cesar WeePas encore d'évaluation
- News at NUST: ISAK Donates Measuring Equipment To Sports ScienceDocument8 pagesNews at NUST: ISAK Donates Measuring Equipment To Sports ScienceRatanang Rj NokoPas encore d'évaluation
- Renal Nursing - HandoutDocument16 pagesRenal Nursing - HandoutJoms Kim Mina100% (3)