Académique Documents
Professionnel Documents
Culture Documents
1034 Types of Muscle Fuel
Transféré par
DanniLi0 évaluation0% ont trouvé ce document utile (0 vote)
7 vues5 pages1034 Types of Muscle Fuel
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce document1034 Types of Muscle Fuel
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
7 vues5 pages1034 Types of Muscle Fuel
Transféré par
DanniLi1034 Types of Muscle Fuel
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 5
Types of exercise
Type 1 suited to aerobic exercise, mitochondria rich, good blood
supply, stores more TAG, resistant to fatigue, moderate glycolytic
cacpity, high oxidative capacity, slow myosin ATPases
Type 2 suited to anaerobic exercise, mitochondria poor, moderate
blood supply, stores more glycogen, easily fatigued, rapid myosin
ATPases, low oxidative capacity, high glycolytic capacity
Exercise types
Aerobic sustained for long periods, low moderate intensity e.g.
marathon
Anaerobic short duration, high intensity e.g. weight lifting/
sprinting
Sources of fuel
- Muscle and liver glycogen: used during fasting or exercise esp.
high intensity. Exhaustion coincides with depletion of muscle
glycogen.
- Plasma glucose: uptake increases during fed state, exercise and
after exercise
- Muscle and adipose TAG: usage increases during fasting and
exercise esp. low intensity
- Plasma lipoproteins: muscle secretes lipoprotein lipase during
fasting, and after exercise, to replenish TAG store.
- Ketone bodies: usage increases during very prolonged exercise,
or very prolonged fasting depends on supply by liver.
Muscle Metabolism in the Fed State
- insulin stimulates an increase in glucose uptake glycogenesis
and glycolysis increase, while fatty acid oxidation is inhibited
- liver senses high [glucose] uptake increases, used for synthesis
of glycogen/ TAG
- pancreas beta cells sense high [glucose] uptake increases,
insulin release stimulated
- insulin favours lipogenesis and inhibits lipolysis
Muscle Metabolism in the Fasting State (at rest)
- decrease in insulin causes decrease in glucose uptake in
muscles. Fatty acid oxidation increases. Amino acids may be
released
- pancreatic beta cells sense low [glucose] uptake decreases,
insulin release decreases
- Low insulin favours release of fatty acids
- Liver senses low [glucose] glucose is released from glycogen
stores and gluconeogenesis.
Muscle Metabolism during exercise
- glycogenolysis and glucose uptake increase. Uptake of fatty
acids and breakdown of TAG increase.
- Adrenaline stimulates glycogenolysis in liver, so glucose is
released. Lactate released by muscle is converted back to
glucose.
- Adrenaline favours release of fatty acids.
High Intensity Exercise
High intensity contractions require a high rate of ATP replenishment.
Glycolysis is the pathway most suited to this, due to its lack of
reliance on oxygen diffusion into the tissue.
Type II muscle fibres are recruited for these types of contractions. In
the five seconds before the rate of glycolysis can be increased, the
stores of phosphocreatine are used to replenish ATP, via creatine
kinase.
ADP is also used to replenish ATP via adenylate kinase. The AMP
produced is an allosteric effector for several enzymes.
Adenylate kinase catalyses the formation of ATP from ADP, and
helps to maintain the ATP: ADP ratio. This reactions also results in an
increase in [AMP].
This helps to maintain the ATP concentration, and the increase in
AMP is used as a signal that ATP production needs to increase.
[AMP] is therefore a sensitive indicator of the cells energy status.
AMP is an important allosteric effector.
Phosphocreatine
Phosphocreatine is an energy store that replenishes ATP in the first
5s of maximal exertion. It also acts as a more diffusible form of high
energy phosphate.
Skeletal muscle contains high levels of phosphocreatine, at 30mM,
compared to 7mM in other cell types.
As pH decreases (anaerobic glycolysis producing lactic acid), [ADP]
increases and reaction goes forward.
After exercise is over, adenylate kinase works to convert AMP to
ADP, so it can be converted to ATP, and phosphocreatine is
replenished from ATP.
Glucose availability: glucose needed for exercise, esp. high intensity
exercise for contracting muscles.
Breakdown of muscle glycogen stimulated by the activation of
glycogen phosphorylase.
Breakdown of liver glycogen is stimulated by a similar process.
Muscle contraction causes translocation of GLUT4 transporters to
the membrane, allow it to take up glucose from the blood. The
amount of glucose made available is affected by other factors, and
there is a limit to the rate glucose can be made available.
Phosphorylase kinase.
Phosphorylase kinase activates glycogen phosphorylase, and is itself
partially activated by calcium ions or phosphorylation, or maximally
activated by both.
In muscle, adrenaline stimulates PKA, while contractions are
associated with the release of calcium ions into the cytosol.
In the liver, glucagon stimulates PKA, adnrealine stimulates PKA ad
calcium release into the cytosol, supplying glucose for the muscles.
Upregulation of glycolysis
Apart from increasing the supply of glucose, the regulatory enzymes
of glycolysis must also increase their availability.
Hexokinase: inhibited by glucose 6 P, inhibition is relieved as the
rate of glucolysis is increased.
Phosphofructokinase 1: activated by the increase in AMP
(adenylate kinase). Any fructose 6 P buildup is converted to F2,6
bisP, a potent activator.
Pyruvate kinase: activated by the increase in AMP. Any buildup in
F1,6 bisP also activates it (feedforward activation)
The occurrence of fatty acid oxidation has a negative effect on the
rate of glycolysis, causing glycogen to last longer.
Phosphofructokinase 1
PFK is the central regulatory enzyme in glycolysis, because it
determines the activity of hexokinase and pyruvate kinase. ATP is a
substrate of PFK-1, but high [ATP] inhibits PFK-1
When [ATP] is high, and [phosphocreatine] is high, inhibition of PFK1 shuts down glycolysis. If fatty acids are being oxidized, citrate also
inhibits PFK-1.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Grade 8 Science Unit 1 Force, Motion and EnergyDocument68 pagesGrade 8 Science Unit 1 Force, Motion and EnergyKeil Morada73% (26)
- Fox 7th ISM ch07-13Document1 079 pagesFox 7th ISM ch07-13Ismar GarbazzaPas encore d'évaluation
- Transferring Stock and Sales Data Process SAP StandardDocument3 pagesTransferring Stock and Sales Data Process SAP StandardrksamplaPas encore d'évaluation
- Easy Stretching PosturesDocument118 pagesEasy Stretching Postures김종빈100% (3)
- Management Controls in Family-Owned Businesses (Fobs) : A Case Study of An Indonesian Family-Owned UniversityDocument13 pagesManagement Controls in Family-Owned Businesses (Fobs) : A Case Study of An Indonesian Family-Owned UniversityAgustPas encore d'évaluation
- Subaltern Voice in The Novel of Anita Nair's Lessons in Forgetting: A Female PerspectiveDocument2 pagesSubaltern Voice in The Novel of Anita Nair's Lessons in Forgetting: A Female PerspectiveIJELS Research JournalPas encore d'évaluation
- WilkersonDocument4 pagesWilkersonmayurmachoPas encore d'évaluation
- Module 4 - Instruction Set Architecture (ISA) v2 (Student) PDFDocument49 pagesModule 4 - Instruction Set Architecture (ISA) v2 (Student) PDFnedunilavanPas encore d'évaluation
- NamdarDocument38 pagesNamdarthe next miamiPas encore d'évaluation
- CVE 202 Lecture - 28062021Document11 pagesCVE 202 Lecture - 28062021odubade opeyemiPas encore d'évaluation
- Usm StanDocument5 pagesUsm StanClaresta JanicePas encore d'évaluation
- Ca1 Pu 12Document100 pagesCa1 Pu 12Shabbeer ZafarPas encore d'évaluation
- Analisis Penerapan Prinsip Prinsip Koperasi Dalam UUDDocument10 pagesAnalisis Penerapan Prinsip Prinsip Koperasi Dalam UUDSaikhudinPas encore d'évaluation
- Penguatan Industri Kreatif Batik Semarang Di Kampung Alam Malon Kecamatan Gunung Pati SemarangDocument10 pagesPenguatan Industri Kreatif Batik Semarang Di Kampung Alam Malon Kecamatan Gunung Pati SemarangAllo YePas encore d'évaluation
- Duncan Reccommendation LetterDocument2 pagesDuncan Reccommendation LetterKilimanjaro CyberPas encore d'évaluation
- Developing Training Program For Effective and Quality Volleyball PlayersDocument13 pagesDeveloping Training Program For Effective and Quality Volleyball PlayersDeogracia BorresPas encore d'évaluation
- ID Analisis Tingkat Kesehatan Perusahaan BeDocument7 pagesID Analisis Tingkat Kesehatan Perusahaan BeAjna RossaPas encore d'évaluation
- English Practice 1: C. Carried D. Sugar B. Underline A. Danger A. CharacterDocument3 pagesEnglish Practice 1: C. Carried D. Sugar B. Underline A. Danger A. CharacterKeisaPas encore d'évaluation
- List of HEIsDocument2 pagesList of HEIsNadine MercadoPas encore d'évaluation
- The Influence of Beauty Projected in The Mass Media On Female Students.Document7 pagesThe Influence of Beauty Projected in The Mass Media On Female Students.Maggie SamsudinPas encore d'évaluation
- How To Configure Checklists in SAP Solution Manager 7.1Document12 pagesHow To Configure Checklists in SAP Solution Manager 7.1singhashwiniPas encore d'évaluation
- Indirectness and Euphemism PDFDocument30 pagesIndirectness and Euphemism PDFmgar10Pas encore d'évaluation
- Introduction To Forensic Science Questioned DocumentsDocument50 pagesIntroduction To Forensic Science Questioned DocumentsLyka C. De Guzman100% (2)
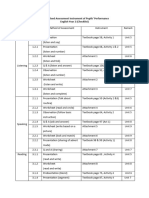
- Penyelarasan Instrumen Pentaksiran PBD Tahun 2 2024Document2 pagesPenyelarasan Instrumen Pentaksiran PBD Tahun 2 2024Hui YingPas encore d'évaluation
- History 541gDocument21 pagesHistory 541gkarl1802Pas encore d'évaluation
- RCA 1 and 2 Wafer CleanDocument3 pagesRCA 1 and 2 Wafer CleanJoonhyuk HwangPas encore d'évaluation
- SCHLEICH - Advanced Test Technologies - GLP1-e - PE+IR+HVAC PDFDocument4 pagesSCHLEICH - Advanced Test Technologies - GLP1-e - PE+IR+HVAC PDFRakesh Kumar VermaPas encore d'évaluation
- SMT Syllabus 2018 19Document90 pagesSMT Syllabus 2018 19sanjanaPas encore d'évaluation
- Pathway Foundation T'SDocument113 pagesPathway Foundation T'SDo HuyenPas encore d'évaluation
- Enterprise Exam Style QuestionsDocument2 pagesEnterprise Exam Style Questionsapi-301785352Pas encore d'évaluation