Académique Documents
Professionnel Documents
Culture Documents
Outcome of SQ .Cell CA of Gingiva
Transféré par
karmayagnaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Outcome of SQ .Cell CA of Gingiva
Transféré par
karmayagnaDroits d'auteur :
Formats disponibles
Journal of Cranio-Maxillofacial Surgery (2000) 28, 331335
# 2000 European Association for Cranio-Maxillofacial Surgery
doi:10.1054/jcms.2000.0177, available online at http://www.idealibrary.com on
Outcome of squamous cell carcinoma of the gingiva: a follow-up
study of 83 cases
Dominique Gomez,1 Alain Faucher,1 Veronique Picot,1 Francois Siberchicot,2 Jean-Louis Renaud-Salis,1
Emmanuel Bussie`res,1 Jacques Pinsolle2
1
Institut Bergonie, Regional Cancer Center, Bordeaux Cedex, France; 2Department of Maxillofacial and
Plastic Surgery, Centre Hospitalier Universitaire, Bordeaux Cedex, France
SUMMARY. Background: Squamous cell carcinomas of the gingiva are relatively rare tumours. Standard
treatment is based on surgery and radiotherapy. The extent of bone involvement affects mandibulectary indications.
Purpose: A retrospective review of squamous cell carcinomas of the gingiva was performed to evaluate the
incidence of mandibular or maxillary bone involvement. Indications for marginal and segmental bone resections are
specified. Material: From 1985 to 1996, 83 patients with squamous cell carcinoma of the gingiva were treated at the
Department of Surgery (Institut Bergonie, Bordeaux, France) and at the Department of Maxillofacial and Plastic
Surgery (Centre Hospitalier Universitaire, Bordeaux, France). Forty-three underwent surgery plus postoperative
radiotherapy. Twenty-two had flap reconstructions. Clinical evaluation and panorex rntgenography were the
means used to evaluate bony invasion and to decide on the extent of bone resection. Methods: A retrospective
review of 83 consecutive patients was performed. This series is unusual in its homogeneity: surgery was performed
by only two individuals and the radiotherapy was the responsibility of just two physicians. Outcome was calculated
using the Kaplan-Meier method. Results: Primary local control was achieved in 72 patients (87%). Overall survival
and rate of recurrence were comparable to those of other squamous cell carcinomas of the oral cavity and
oropharynx. Conclusion: Surgical resection continues to be the mainstay of treatment and this study tends to
confirm the validity of modified neck dissection and marginal bone resection in suitably selected patients. # 2000
European Association for Cranio-Maxillofacial Surgery
Universitaire, Bordeaux, France) were reviewed.
Adequate clinical information was available in 87
patients. Four patients who had previously received
treatment for another head and neck primary tumour
were excluded, leaving 83 patients.
All patients had histologically proven squamous
cell carcinoma. Lesions of the retromolar triangle
were excluded because the origin could be buccal
mucosa or tonsillar pillar (Cady & Catlin, 1969).
Furthermore, the thin layer of submucosal connective
tissue between the gingival mucosa and the underlying bone is thicker in the retromolar area, thus
possibly modifying local extension of the tumours
(Totsuka et al., 1990).
Surgery was the only treatment used in 26 patients
(31%) of whom 15 had no neck dissection (these
patients were classified T1N0 or T2N0 or T3N0).
Forty-three patients (52%) underwent surgery and
postoperative radiotherapy and 14 were treated by
radiotherapy alone.
There were 56 neck dissections, of which 11 were
bilateral (45 patients). Amongst the indications
for the various types were: supraomohyoid neck
dissection for tumours classified N0 (40 performed),
modified neck dissection for tumours classified N1
or N2 (14 performed) and radical neck
dissection for tumours classified N3 (2 undertaken).
Marginal mandibulectomy (horizontal resection
of upper portion of mandible) was performed in
INTRODUCTION
Squamous cell carcinoma of the gingiva is relatively
rare and represents less than 10% of squamous cell
carcinomas of the oral cavity (Cady & Catlin, 1969;
Byers et al., 1981; Soo et al., 1988; Eicher et al., 1996).
The initial symptoms are similar to those of other
primary sites in the oral cavity (Cady & Catlin, 1969;
Byers et al., 1981). Standard treatment is based on
surgery and radiation therapy (Fletcher & Jessee,
1977; Vikram et al., 1980; Byers et al., 1981; Soo
et al., 1988). We performed a retrospective review of
83 consecutive, previously untreated patients with
carcinoma of the gingiva to assess outcome and to
evaluate the incidence of mandibular or maxillary
bone involvement, since this affected the extent of
bone resection (Byers et al., 1981; Totsuka et al.,
1990; Loree & Strong, 1990; Totsuka et al., 1991;
Overholt et al., 1996).
PATIENTS AND METHODS
The medical records of 96 patients with previously
untreated squamous cell carcinoma of the gingiva,
seen between 1 January 1985 and 31 December 1996
at either the Department of Surgery (Institut Bergonie, Bordeaux, France) or at the Department of
Maxillofacial and Plastic Surgery (Centre Hospitalier
331
332 Journal of Cranio-Maxillofacial Surgery
25 patients and segmental mandibulectomy (en bloc
resection of a variable length of mandible) in 16
patients. One patient had a hemimandibulectomy. The decision on which technique was made
according to Totsuka et al. (1991), Greer et al. (1953),
Wald and Calcaterra (1983), Gilbert et al. (1986) and
Randall et al. (1987). Six patients had hemimaxillectomies.
Reconstruction required 22 flaps, including
five nasolabial flaps (23%), four pectoralis major
flaps (18.5%), three infrahyoid flaps (13.5%), three
lateral osteocutaneous trapezius flaps (13.5%), two
latissimus dorsi flaps (9%), two osteocutaneous fibula
flaps (9%), one temporofrontal flap (4.5%), one
lateral trapezius flap (4.5%) and one forearm
flap (4.5%). Of these patients requiring flaps,
twelve underwent reconstruction with a mandibular
reconstruction plate. Reconstruction required a
plate without flap cover in one segmental mandibulectomy.
Postoperative radiotherapy was used in 43 patients.
It was felt to be indicated for tumours classified T3
and T4, histologically proven neck disease, and
positive surgical margins (there was no reoperation
for these patients). Radiotherapy was commenced as
soon as possible even when healing was incomplete.
Mean delay was 20 days following surgery (range 12
31 days) except for one patient who began radiotherapy 77 days after surgery because of several
postoperative complications. The median dose was
55 Gy (range 5080 Gy) and the median number of
fractions given was 28. Neck areas with extracapsular
spread or positive surgical margins received an
additional 10 Gy boost. Among the 16 patients
classified T1N0 or T2N0, seven received radiotherapy
alone (8.5% of the complete series). In these cases,
the median dose to the primary and the neck areas
was 63 Gy (range 5074 Gy) and the median number
of fractions given was 31. A palliative treatment plan
was offered for seven other patients (8.5% of the
complete series) on account of tumour extension and
poor general status. None of these underwent
surgery; instead treatment comprised chemotherapy
(5-FU and cisplatin) with or without locoregional
radiotherapy.
Locoregional control was assessed 1 month after
completion of therapy. Patients were reviewed every
3 months up to 18 months, then every 6 months up to
5 years and then annually. Recurrence was defined as
a lesion at the primary site, lymph node metastasis or
distant metastasis compatible with the previously
treated tumour. Confirmation was assessed histologically whenever possible.
Results were evaluated according to the KaplanMeier method to calculate survival probabilities regarding the period between first and last
consultations or death. Univariate analysis by the
log-rank method was used to assess significance.
Multivariate analysis using the Cox model of
proportional hazards was used to determine the
covariates that best predicted survival and recurrence
rates.
RESULTS
There were 52 men (63%) and 31 women (37%) who
ranged in age from 4090 years (mean age 68 years).
Mean follow-up was 61 months. Accurate evaluation
of tobacco and alcohol consumption was available in
50 patients. Tobacco was used regularly by 31
patients. Twenty-five patients consumed alcohol
daily. Irritation from ill-fitting dentures was present
in 20 patients. The prevailing initial symptom was an
intraoral mass or swelling in 31 patients (37%).
Ulceration was noted in 27 patients (33%), whereas
pain was reported by only 5 (6%). Mobility of teeth
was seen in two patients (2.5%), there being no link
between the extraction of teeth and carcinoma of the
gingiva. The pre-treatment evaluation usually included clinical history, physical examination, biopsy,
chest rntgenography, endoscopy and a full blood
count. Panorex rntgenography was used in all
patients. Facial bone scans were performed in only
15 patients.
Primary tumour site was the lower alveolar ridge in
53 patients (64%) and the upper in 30 patients (36%).
Forty lesions were located on the left side (48%), 28
on the right side (34%) and 15 were midline (18%).
Tumours were staged according to the 1987 recommendations of the Union Internationale Contre le
Cancer (U.I.C.C.; Table 1) and the American Joint
Committee on Cancer (1988). Tumours of patients
admitted before 1987 were reclassified. Among the 58
patients with tumours classified as T4, 48 had clinical
or radiological evidence of bone invasion. No patient
was found to have a distant metastasis at the first
consultation. The tumours were categorized as well
differentiated in 67 (81%) and moderately differentiated in 14 patients (17%). The tumour grade was
not classified in two patients (2%).
Among the 69 patients treated surgically, there was
one postoperative death due to general complications
Table 1 Tumour and node staging for the complete series of
gingival carcinomas (UICC, 1987)
N0
N1
N2a
N2b
N2c
N3
Total
T1
T2
T3
T4
TX
Total
6
1
10
1
39
12
2
60
14
2
1
2
4
83
72
17
2.5
1
2.5
5
100
1
7
11
2
3
58
1
2
Table 2 Fifteen complications in 12 patients out of 69 patients
who had surgery with/without postoperative irradiation
Postoperative complications
Total
Fistula
Wound infection
Wound haematoma
Partial flap necrosis
Total flap necrosis
Systemic complications
Total
4
3
1
3
1
3
15
27
20
6.5
20
6.5
20
100
Squamous carcinoma of the gingiva 333
(1.4%). Twelve patients (17.4%) experienced postoperative complications (Table 2).
Histological examination of tumour specimens
from 69 patients revealed tumour-free margins in 59
patients (86%) and margins with tumour invasion in
10 (14%). Surgical margins were positive in 19% of
patients in whom resection of the jaws was marginal
and in 12.5% of patients in whom segmental
resection was chosen. There was no significant
difference between marginal and segmental mandibulectomy for local control (p 0.42). Histological
findings in neck dissection specimens (45 patients)
showed no lymph node invasion in 22 patients (50%),
lymph node invasion without extracapsular spread in
12 patients (26%), and lymph node invasion with
extra-capsular spread in 11 patients (24%). We
focused on the relationship between clinical and
preoperative radiological evaluation of bone invasion
and histologically proven bone invasion. Suspicion of
preoperative bone invasion was confirmed in 28
patients (58%) and was refuted in 20 others (42%)
by histological examination. There was no significant
statistical relationship between clinical and radiological evidence of bone involvement and pathologic
findings (p 0.093).
Locoregional disease control for the complete
series was achieved in 72 patients (87%) at the first
post-therapeutic consultation (1 month after completing treatment). For the complete series, the
overall 1- and 5-year survival rates were 72.9% and
42.7% respectively; the disease-specific 1- and 5-year
survival rates were 80.5% and 60% respectively
(Figs 1 & 2). On univariate analysis, neither age,
sex, primary site (upper or lower gingiva) nor clinical
nor radiologic evidence of bone invasion had a
significant impact on overall survival. Only tumour
stage (p50.001), tumour invasion of surgical margins
(p 0.03) and histologically proven node invasion
(p 0.004) were significant. The difference between
patients with or without histologically proven bone
invasion was not significant (p 0.059). Multivariate
analysis was used to assess variables that seemed to
Fig. 2 Disease-specific survival probability for complete series.
influence survival amongst T stage, N stage, histologically proven bone involvement, surgical margins
and lymph node involvement: in this series T stage
(p 0.05), N stage (p50.001) and surgical margins
(p 0.016) emerged as significant predictors of
survival.
Among the 72 patients with primary disease
control, recurrences occurred in 29 patients
(40.3%): there were 13 local recurrences, four local
with cervical recurrences, one local recurrence plus
distant metastasis, seven lymph node recurrences in
the neck, one local plus lymph node in the neck plus
distant metastasis, and three distant metastases.
T stage (T1, T2 and T3 vs. T4: p 0.05), surgical
margins (p 0.006), and lymph node invasion
(p 0.005) predicted a statistically significant risk of
recurrence. One- and 5-year survival rates following
detection of recurrence were 47.3% and 18.8%,
respectively. On multivariate analysis, only lymph
node involvement emerged as a significant predictor
of recurrence (p 0.016).
DISCUSSION
Fig. 1 Overall survival probability for complete series.
This consecutive series of patients is particularly
homogeneous in terms of their management. These
patients whose age is comparable to those in other
reports of gingival carcinoma (Cady & Catlin, 1969;
Soo et al., 1988; Overholt et al., 1996) are older than
those treated for other upper aerodigestive tract
primary sites (Barrelier & Granon, 1997). Unlike
another report (Soo et al., 1988), no relationship was
found between dental extraction and result of
treatment of gingival carcinoma. The coincidence
with alcohol and tobacco consumption is not as close
as in other series (Cady & Catlin, 1969; Soo et al.,
1988; Eicher et al., 1996; Overholt et al., 1996;
Barrellier & Granon, 1997). The role of dental
prostheses is not proven (Campbell et al., 1997).
Unlike other studies most of our patients (70%) were
staged as T4 (Cady & Catlin, 1969; Byers et al., 1981;
334 Journal of Cranio-Maxillofacial Surgery
Wald & Calcaterra, 1983; Soo et al., 1988; Totsuka
et al., 1991; Eicher et al., 1996; Overholt et al., 1996).
In this series, 60 patients (72%) were staged as N0;
there was no known distant metastasis initially.
Totsuka (Totsuka et al., 1990; Totsuka et al., 1991)
has defined and compared two basic patterns of
radiological and histological bone involvement. On
radiological analysis, he found an erosive and an
invasive bone defect. On histological analysis he
discovered an expansive and an infiltrative kind of
invasion. If panorex rntgenography were to show
an erosive bone defect not extending beyond the
inferior alveolar canal or an invasive bone defect
confined to a superficial area of the alveolar bone, or
no bone involvement at all, then marginal resection
of the mandible might be indicated. Segmental
resection is indicated when radiologic bone involvement is more extensive. Our mandibulectomy indications are based on the experience of Totsuka (Totsuka
et al., 1991) and other authors (Greer et al.,
1953; Wald & Calcaterra, 1983; Gilbert et al., 1986;
Randall et al., 1987). Retrospectively, it was impossible to evaluate these two basic patterns of radiologic
and histologic bone involvement. To assess mandibular invasion by intraoral carcinoma, panorex rntgenography, CT scan, bone scintigraphy and MRI
may be used. While extremely sensitive (100%), bone
scintigraphy is non-specific (60%; Bergstedt et al.,
1981; Higashi et al., 1996). CT scan is associated with
10 or 15% of false positives, just like panorex
rntgenography (Baker et al., 1982; Weisman &
Kimmelman, 1982; Schaefer et al., 1984; Close et al.,
1986). MRI seems to be superior to other imaging
modalities but the reported series are not large enough
to draw valid conclusions (Ator et al., 1990; Pellissier
et al., 1994). Therefore, clinical evaluation and
panorex rntgenography (sensitivity: 87%) remain as
our methods of reference to evaluate bone invasion.
Standard treatment is based on surgery with or
without postoperative radiotherapy. Only 9% of our
patients received radiotherapy alone. This is equivalent to or more frequent than in other reports (Cady
& Catlin, 1969; Soo et al., 1988; Eicher et al., 1996;
Overholt et al., 1996). Postoperative radiotherapy was
indicated for T3 and T4 tumours, when surgical
margins were positive or when lymph node involvement was present. In carefully selected patients,
marginal bone resection seems to be as effective as
segmental resection in the local control of gingival
carcinoma (Byers et al., 1981; Soo et al., 1988).
Overall surival was comparable to other series (Cady
& Catlin, 1969; Byers et al., 1981) and depended on
tumour stage, node stage, lymph node involvement
and surgical margins (Loree & Strong, 1990; Eicher
et al., 1996). Whilst bone invasion was not a
significant factor, there was a slight trend in favour
of a difference: (p 0.059) although bone invasion
was correlated with T4 tumour stage which influences
overall survival. In a recent retrospective study
(Wong et al., 2000), it is unclear whether the
difference in survival is due to the histological pattern
of mandibular invasion or whether it is a consequence
of the higher number of positive surgical margins
found in the infiltrative lesions. Also, certain data
concerning the treatment modalities (particularly the
number of patients having postoperative radiation
therapy in each group) are missing. Therefore, it is
difficult to compare and to draw definitive conclusions.
CONCLUSION
Squamous cell carcinomas of the gingiva are rare
tumours and preoperative radiological assessment of
bone invasion is not easy. Overall survival and rate of
recurrence are comparable to those of other squamous cell carcinomas of the oral cavity and
oropharynx. Surgical resection remains the mainstay
of treatment. This study tends to confirm the validity
of modified neck dissection and marginal bone
resection in properly selected patients as the results
achieved were similar to those of other authors.
References
American Joint Committee on Cancer. Manual for staging of
cancer, Ed. 3.3 B. Lippincott, Philadelphia, 1988
Ator GA, Abemayor E, Lufkin RB, Hanafee WN, Ward PH:
Evaluation of mandibular tumour invasion with magnetic
resonance imaging. Arch Otolaryngol Head Neck Surg 116:
454459, 1990
Baker HL, Woodbury DH, Krause CJ, Saxon KG, Stewart RC:
Evaluation of bone scan by scintigraphy to detect subclinical
invasion of the mandible by squamous cell carcinoma of the
oral cavity. Otolaryngol Head Neck Surg 90: 327336, 1982
Barrellier P, Granon C: Epidemiologie des cancers de la cavite
buccale. Encycl Med Chir Stomatol Odontol 22-063-B10, 1997
Bergstedt HF, Lind MG, Silfversward C: Facial bone scintigraphy
VII. Diagnosis of malignant lesions in the mandible. Acta
Radiol Diag 22: 485493, 1981
Byers RM, Newman R, Russel N, Yue A: Results of treatment for
squamous carcinoma of the lower gum. Cancer 47: 22362238,
1981
Cady B, Catlin D: Epidermoid carcinoma of the gum. A 20-year
survey. Cancer 23: 551569, 1969
Campbell BH, Mark DH, Soneson EA, Freife JE, Schultz CJ: The
role of dental prostheses in alveolar ridge squamous
carcinomas. Arch Otolaryngol Head Neck Surg 124: 1112
1115, 1997
Close LG, Burns DK, Merkel M, Burns DK, Schaefer SD:
Computed tomography in the assessment of mandibular
invasion by intraoral carcinoma. Ann Otol Rhinol Laryngol
95: 383388, 1986
Eicher SA, Overholt SM, El-Naggar AK, Byers RM, Weber RS:
Lower gingival carcinoma: clinical and pathologic
determinants of regional metastases. Arch Otolaryngol Head
Neck Surg 122: 634638, 1996
Fletcher GH, Jessee RH: The place of irradiation in the
management of the primary lesion in head and neck cancers.
Cancer 39: 862867, 1977
Gilbert S, Tzadik A, Leonard G: Mandibular involvement by oral
squamous cell carcinoma. Laryngoscope 96: 96101, 1986
Greer DB, Smith RR, Klopp CT: A surgical method of treatment
of carcinoma of the floor of the mouth. Surgery 34: 279287,
1953
Higashi K, Wakao H, Ikuta H, Kashima I, Everhart FR: Bone
scintigraphy in detection of bone invasion by oral carcinoma.
Ann Nuclear Med 10: 5761, 1996
Loree TR, Strong EW: Significance of positive margins in oral
cavity squamous carcinoma. Am J Surg 160: 410414, 1990
Squamous carcinoma of the gingiva 335
Overholt SM, Eicher SA, Wolf P, Weber RS: Prognostic factors
affecting outcome in lower gingival carcinoma. Laryngoscope
106: 13351339, 1996
Pellissier S, Duvoisin B, Fontolliet C, Monnier P: Magnetic
resonance imaging and X-ray computed tomography in
advanced cancer of the oral cavity. A comparative clinical,
radiological and morphological study. J Radiol 75: 577583,
1994
Randall CJ, Eyre J, Davies D, Walsh-Waring GP: Marginal
mandibulectomy for malignant disease: indications, rationale
and results. J Laryngol Otol 101: 676684, 1987
Schaefer SD, Merkel M, Burns DK, Close LG: Computed
tomography of upper aero-digestive tract squamous cell
carcinoma. Arch Otolaryngol 110: 236240, 1984
Soo KC, Spiro RH, King W, Harvey W, Strong EW: Squamous
carcinoma of the gum. Am J Surg 156: 281285, 1988
Totsuka Y, Usui Y, Tei K et al.: Mandibular involvement by
squamous cell carcinoma of the lower alveolus: analysis and
comparative study of histologic and radiologic features. Head
Neck 13: 4050, 1990
Totsuka Y, Usui Y, Tei K et al.: Results of surgical treatment for
squamous carcinoma of the lower alveolus: segmental vs
marginal resection. Head Neck 13: 114120, 1991
Vikram B, Strong EW, Sha J, Spiro RH: Elective postoperative
radiation therapy in stages III and IV epidermoid carcinoma of
the head and neck. Am J Surg 140: 580584, 1980
Wald RM, Calcaterra TC: Lower alveolar carcinoma: segmental vs
marginal resection. Arch Otolaryngol 109: 578582, 1983
Weisman RA, Kimmelman CP: Bone scanning in the assessment of
mandibular invasion by oral cavity carcinomas. Laryngoscope
92: 14, 1982
Wong RJ, Keel SB, Glynn RJ, Varvares MA: Histological pattern
of mandibular invasion by oral squamous cell carcinoma.
Laryngoscope 110: 6572, 2000
Dominique Gomez MD
17, rue Charles Laterrade
33400 Talence
France
Tel: +33 5 56 84 95 38
E-mail: emmanuelle.scottogomez@libertysurf.fr
Paper received 27 March 2000
Received 28 November 2000
Vous aimerez peut-être aussi
- Spiritual Development Through The Chakra Progression: Jennifer Drapkin, Clayton Mcclintock, Elsa Lau, Lisa MillerDocument16 pagesSpiritual Development Through The Chakra Progression: Jennifer Drapkin, Clayton Mcclintock, Elsa Lau, Lisa MillerkarmayagnaPas encore d'évaluation
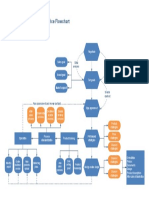
- Flowchart of The Industrial Process For The Manufacturing of Plastic Yogurt CupsDocument1 pageFlowchart of The Industrial Process For The Manufacturing of Plastic Yogurt CupskarmayagnaPas encore d'évaluation
- Borders Crossed: Vibhishana in The Ramayana and Beyond: South Asia: Journal of South Asian StudiesDocument22 pagesBorders Crossed: Vibhishana in The Ramayana and Beyond: South Asia: Journal of South Asian StudieskarmayagnaPas encore d'évaluation
- BhagavadGita theArtofLeadership OldTextNewContextDocument19 pagesBhagavadGita theArtofLeadership OldTextNewContextkarmayagnaPas encore d'évaluation
- Ecommerce FlowchartDocument1 pageEcommerce FlowchartkarmayagnaPas encore d'évaluation
- Flow Chart of The Manufacturing Process Used by Arena Software Numbers Indicating BatchDocument1 pageFlow Chart of The Manufacturing Process Used by Arena Software Numbers Indicating BatchkarmayagnaPas encore d'évaluation
- Manufacturing WorkflowDocument1 pageManufacturing WorkflowDidik HariadiPas encore d'évaluation
- Main Functions of The Operative Manufacturing Execution LevelDocument1 pageMain Functions of The Operative Manufacturing Execution LevelkarmayagnaPas encore d'évaluation
- Manufacturing Process MapDocument1 pageManufacturing Process MapkarmayagnaPas encore d'évaluation
- Beer Production ProcessDocument1 pageBeer Production ProcesskarmayagnaPas encore d'évaluation
- Logical Flow Diagram of The Production Process OperationsDocument1 pageLogical Flow Diagram of The Production Process OperationskarmayagnaPas encore d'évaluation
- Manufacturing Process MapDocument1 pageManufacturing Process MapkarmayagnaPas encore d'évaluation
- Order FlowchartDocument1 pageOrder FlowchartkarmayagnaPas encore d'évaluation
- Flowchart of The Industrial Process For The Manufacturing of Plastic Yogurt CupsDocument1 pageFlowchart of The Industrial Process For The Manufacturing of Plastic Yogurt CupskarmayagnaPas encore d'évaluation
- Beer Processing PFDDocument1 pageBeer Processing PFDkarmayagnaPas encore d'évaluation
- Server WorkflowDocument1 pageServer WorkflowkarmayagnaPas encore d'évaluation
- Logical Flow Diagram of The Production Process OperationsDocument1 pageLogical Flow Diagram of The Production Process OperationskarmayagnaPas encore d'évaluation
- Order WorkflowDocument1 pageOrder WorkflowkarmayagnaPas encore d'évaluation
- Logical Flow Diagram of The Production Process OperationsDocument1 pageLogical Flow Diagram of The Production Process OperationskarmayagnaPas encore d'évaluation
- Manufacturing WorkflowDocument1 pageManufacturing WorkflowDidik HariadiPas encore d'évaluation
- Services FlowchartDocument1 pageServices FlowchartLuis Fernando Sanchez TapiaPas encore d'évaluation
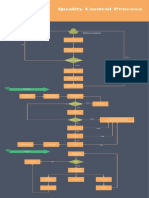
- Quality Control Process: Material SupplierDocument1 pageQuality Control Process: Material Supplieralva10 vaPas encore d'évaluation
- Statistical Study For Sonographic Differential Diagnosis ofDocument8 pagesStatistical Study For Sonographic Differential Diagnosis ofkarmayagnaPas encore d'évaluation
- Intra Arterial ChemotherapyDocument6 pagesIntra Arterial ChemotherapykarmayagnaPas encore d'évaluation
- Ecommerce FlowchartDocument1 pageEcommerce FlowchartkarmayagnaPas encore d'évaluation
- Oral CancerDocument5 pagesOral CancerkarmayagnaPas encore d'évaluation
- Secondary Orbital MlanomasDocument5 pagesSecondary Orbital MlanomaskarmayagnaPas encore d'évaluation
- Survival After Oral CancerDocument5 pagesSurvival After Oral CancerkarmayagnaPas encore d'évaluation
- Relationship of Tumor Thickness in Punch Biopsy and SubsequentDocument4 pagesRelationship of Tumor Thickness in Punch Biopsy and SubsequentkarmayagnaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Interpretarea Holter TADocument37 pagesInterpretarea Holter TAburdihanPas encore d'évaluation
- Treatment Planning Heterogeneity Vs Homogeneity Lung ProjectDocument13 pagesTreatment Planning Heterogeneity Vs Homogeneity Lung Projectapi-299138743Pas encore d'évaluation
- ABA Techniques for Exceptional NeedsDocument6 pagesABA Techniques for Exceptional NeedsSunny Bautista100% (4)
- Chapter 2 Review of Related Literature RevisedDocument13 pagesChapter 2 Review of Related Literature RevisedJun Ace S. Biete80% (15)
- Epilepsy Sleep Disturbance PDFDocument7 pagesEpilepsy Sleep Disturbance PDFFadila Amalina AriputriPas encore d'évaluation
- Clinical Teaching PlanDocument12 pagesClinical Teaching PlanEden Natividad100% (3)
- Stephanie's CVDocument3 pagesStephanie's CVmadcat1425Pas encore d'évaluation
- 2021 Master Competency ListDocument1 page2021 Master Competency Listapi-574059920Pas encore d'évaluation
- Renal DiseaseDocument18 pagesRenal Diseaseapi-262638118Pas encore d'évaluation
- D G Model Making Sense of Clinical Examination of The Adult Patient Hands-On GuideDocument313 pagesD G Model Making Sense of Clinical Examination of The Adult Patient Hands-On GuidevaidyamPas encore d'évaluation
- Project On Lupin PhrmaDocument47 pagesProject On Lupin PhrmaUmesh AmanPas encore d'évaluation
- 6 How To Run An OSCE Session - For OrganisersDocument8 pages6 How To Run An OSCE Session - For Organisersroryj78Pas encore d'évaluation
- Casestudy UTIDocument53 pagesCasestudy UTIRuja Shakya100% (3)
- Autism Spectrum Disorder (Asd) : PRESENTED BY: Ms Mamta BishtDocument21 pagesAutism Spectrum Disorder (Asd) : PRESENTED BY: Ms Mamta BishtRudra prasad SahuPas encore d'évaluation
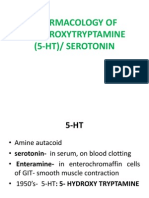
- Pharmacology of SerotoninDocument52 pagesPharmacology of SerotoninSunilPas encore d'évaluation
- 13 Potential Health Benefits of DandelionDocument3 pages13 Potential Health Benefits of DandelionaniruskPas encore d'évaluation
- Upper Limb Amputee Rehabilitation and Prosthetic RestorationDocument19 pagesUpper Limb Amputee Rehabilitation and Prosthetic RestorationkUt'S1031Pas encore d'évaluation
- Litigating The Omnicare Kickbacks Qui Tam Case - The ComplaintDocument121 pagesLitigating The Omnicare Kickbacks Qui Tam Case - The ComplaintBehn and Wyetzner, CharteredPas encore d'évaluation
- Soap NoteDocument5 pagesSoap NoteSolange Wilson100% (1)
- Disease ResearchDocument2 pagesDisease ResearchabilPas encore d'évaluation
- DentistryDocument16 pagesDentistryMeka Syahputra56% (9)
- Title Page Chapter I RevisedDocument9 pagesTitle Page Chapter I RevisedAvashti LontokPas encore d'évaluation
- Nutrition Services Volume 1 Issue 1Document10 pagesNutrition Services Volume 1 Issue 1api-343888842Pas encore d'évaluation
- Pulmonary EdemaDocument28 pagesPulmonary EdemaMohammed Elias100% (1)
- Journal Club Gut PrepDocument14 pagesJournal Club Gut PrepMohammad NomanPas encore d'évaluation
- Executive Order 032 Series of 2018Document10 pagesExecutive Order 032 Series of 2018elayPas encore d'évaluation
- Lilavati V/s KEMDocument35 pagesLilavati V/s KEMAshita Doshi100% (1)
- HCP Endor Faciales enDocument2 pagesHCP Endor Faciales enrijascp1Pas encore d'évaluation
- Selenium Yeast Gras PDFDocument76 pagesSelenium Yeast Gras PDFGopalaKrishnan SivaramanPas encore d'évaluation
- Dementia Beyond Drugs: Changing The Culture of Care, Second Edition (Excerpt)Document8 pagesDementia Beyond Drugs: Changing The Culture of Care, Second Edition (Excerpt)Health Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.Pas encore d'évaluation