Académique Documents
Professionnel Documents
Culture Documents
Somatosensory System
Transféré par
aloepathicDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Somatosensory System
Transféré par
aloepathicDroits d'auteur :
Formats disponibles
Somatosensory Nervous System
General points regarding sensory systems Somatosensory Systems
1. All 1º sensory nerve ending in PNS are a/w specialized receptor end organs which: DC/ML: Dorsal Column/Medial Lemniscal System
a. Transduce sensory signal or aid in transduction ALS: Anterolateral system (aka Spinothalamic tract)
b. Exception: free nerve endings carrying noxious (pain) stimuli Trigeminal (2 systems homologous to DCML and ALS for the head)
2. Sensory info conveyed to cerebral ctx by a series of relay nuclei, incl one in thalamus
Somatosensory Sensations: Keys to clinical testing of one vs other system
a. Major exception: olfaction: no thalamic relay
3. Axons carrying sensory info are organized topographically from relay nuclei to ctx Carried in DCML ONLY Carried in ALS ONLY Carried by both systems
o Somatotopic (sensory) o Viscerotopic (gut layout) Texture Temp Pressure touch
o Tonotopic (auditory) o Retinotopic (visual) Vibration Slow pain Hair-associated touch
4. Cerebral ctx = “center of consciousness” where sensations enter awareness Proprioception Visceral sensations Fast pain
5. Parallel pathways: descending systems govern amt of ascending (i.e. sensory) input
6. Collateral axonal branches may activate other areas of the brain Major differences: DCML vs ALS systems
DCML ALS
Somatosensory sensations: not just the “5 S’s” anymore Medulla:
Somatic: nerves innervating joint capsules and skin 1st synapse occurs at… Gracile nucleus: below T6 Grey matter spinal cord
Touch Temperature: warm/cold Cuneate nucleus: above T6
o Pressure Vibration Large neurons Smaller neurons
o Hair-associated Pain: fast + slow DRG (1º sensory) neurons + Heavily myelinated Less myelination
o Discriminative (texture) Proprioception axons subserving >> # fibers reach cerebrum Fewer # fibers reach
o Stretch localization of sensation cerebrum
Visceral: nerves innervating smooth or cardiac muscle fullness and ischemia Somatosensory information
Caudal medulla Lumbar spinal cord
crosses the midline at…
Receptor end organs
Receptor Major function Composition Location
Modified Just beneath Higher level somatosensory processing
Meissner’s Low-freq vibration
Schwann cells epidermis Primary Somatosensory Cortex (S1): Post-central gyrus of parietal lobe
corpuscles texture (discrim. touch)
Somatotopic organization (point-to-point
Pacinian Subcut. representation/map)
Higher freq vibrations tissue
corpuscle o Lower body = more medial
Deep in skin; o Upper body = more lateral
Ruffini’s
Stretch receptors tendons + Related to pattern of fibers in
corpuscles
ligaments DCML Plasticity: overuse/
Merkel’s Pressure: Irritate 1º afferent Modified underuse of an area
disks w/glutamic acid (NT) AP epidermal cells 2º and 3º Somatosensory Ctx: will cause ∆ in amt
Epidermis ctx dedicated to it
All skin, all
S2: integrates info from 1º
Free nerve Pain chemicals AP somatosensory ctx over time and
Nerves layers?
endings Temperature space: ex. sense a single object (with multiple inputs) as 1 single object
S3: integrates more subtle inputs – texture, etc.
Types of Depolarization
Loss of 2º + 3º ctx tactile agnosia (inability to
Found where in 1º recognize by feel, can still ID visually) S1 S2
Potential type Definition
afferent axon? Location: parietal lobe immediately posterior to 1º
Graded “Analog” – gradations of depolarization Receptor end organs somatosensory ctx
receptor No self-regeneration cannot propagate
potential unless convert into AP above TH level DCML VPL S1 S2 S3
Action potential “Digital” – on or off Axons, begin close to ALS (thalamus)
Self-regenerative carries signal to CNS receptor end organs
Somatosensory Nervous System
DCML pathway
Texture, Vibration, Proprioception (efferent)
Primary somatosensory ctx
Leg (postcentral gyrus)
Trunk
Arm
• Synapse at VPL (Ventral
Posterior limb of internal capsule
posterior lateral nucleus of
thalamus)
• Pass through posterior limb
of internal capsule to 1º VPL nucleus, thalamus
somatosensory ctx
@ Pons:
Shift in orientation from vertical to lateral
distribution of neurons such that most
medial = lower body, lateral = upper body
Medial lemniscus Shift in
somatotopic
Internal arcuate: site of DCML decussation orientation
(both gracile + cuneate axons)
Dorsal column nuclei: Decussation:
internal arcuate fibers Cuneate nuc
• Gracile nucleus: axons from
below T6 (lower limb) Gracile nuc
• Cuneate nucleus: axons from
above T6 (upper limb)
Site of first synapse Dorsal column axons stay separated Cuneate +
in DCML pathway as they ascend in the fasciculi gracile fasciculi
DRG
above T6
• Input from upper and lower Additional synapse @ Clarke’s
body areas (separate DRG nucleus before connecting to
DRG
T6 tracts above and below T6) nucleus gracilis extra neuron
below T6
fibers pass through dorsal spinal
• Make local connections
cerebellar tract in lateral column
(reflexes) in lower body
proprioceptive info from
lower limb
Somatosensory Nervous System
Anterolateral system
Pain and Temperature
Primary somatosensory ctx
Trunk Leg (postcentral gyrus)
Arm
Primary somatosensory cortex
Posterior limb of internal capsule
Thalamus: projects to same nucleus as for DCML
VPL, ventral posterior lateral nucleus
VPL nucleus, thalamus
Reticular activating system Note: arm info switches
Midbrain Location: medulla + pons from medial to lateral @
Function: collateral fibers from ALS and VPL, opposite for limb
trigeminal pain pathways synapse on RAS
o Activate cerebral cortex via relay Part of RAS
Spinothalamic
nucleus in thalamus
tract
o Produce arousal “hyperalertness”
2 major activators: auditory info
Mid-pons
and pain
(Also flash of light, surprise
(sensory stimulus activates),
caffeine!)
Damage to RAS = one cause of
Middle coma (inability to become alert)
medulla Lissauer’s tract:
Dorsal lateral fasciculus
• 1st synapse: in dorsal horn grey matter of Sp cord Significance: for pain relief in
the olden days, would want to
• Synapse in Laminae 1 or 2 cut several levels above site of
Caudal • Axon crosses midline in ventral white pain (ex. T8) because afferent
medulla commissure, turns 90º at jxn of lateral + ventral info spreads out before
funiculi and heads up reaches spinal cord
“ALS”
Pain + temp info from
DRG
upper body (including
Cervical Enter spinal cord
face)
spinal cord starting @ L5 (big toe) Synapse in lamina I: postsynaptic fiber
travels all the way to VPL
Synapse in L2 (substantia gelatinosa)
Pain + temp info from
onto local circuit neurons make
Lumbar lower body
another synapse @ L5 and then crosses
spinal cord midline
Decussation: ventral white commissure
Somatosensory Nervous System
Trigeminal nerve Pain sensation and pain response
Sensory information: Approximate borders between dermatomes
Ophthalmic Pain and temperature: parallels ALS Cervical
o Passes through spinal trigeminal tract to spinal nucleus Thoracic
Maxillary o Decussates at level of spinal cord Lumbar
o Sends fibers to … Sacral
Mandibular Reticular activating system
Facial motor nucleus affects skeletal muscles of
facial expression basis of grimace
Mechanosensory: parallels DCML Pain response:
o Discriminative touch and proprioception (mastication)
o Info enters trigeminal ganglion and synapses on principal sensory nucleus of the
trigeminal nerve
o Decussates @ level of pons
Both systems synapse @ VPM nucleus of thalamus, info projects to facial S1
Nerve endings split cover > territory
(vs finer sensations – more precise)
Chemicals released into extracell. space
activate 1º afferent receptors AP
When AP reaches branch point: some of
AP may spread retrograde causes
NT release at other synaptic terminals
mediating pain response
VPM nucleus of the thalamus
o Substance P
Genu of internal capsule o CGRP leaky RBCs inflamm.
o Mast cells histamine
Mesencephalic Contributes to hyperalgesia (↑ pain response) – for days
Ventral trigeminothalamic tract Proprioceptive info
nucleus
from mm. of mastication
Types of Pain:
Fast Slow Local anesthetic (ex capsaicin):
Principal nucleus ALS ALS Ischemia: Selective block 2nd pain
Discriminative touch
Facial motor nucleus DCML Blocks first pain Short tem pain, LT analgesia
CN VII RAS
Spinal trigeminal
Skeletal muscles of tract Pain
facial expression
Spinal trigeminal
Reticular formation nucleus
Somatosensory Nervous System
Descending control of pain: regulation within brain and spinal cord Effects of unilateral structural destruction on subjective sensations
Some ability to ignore pain (“turn off pain pathways”) until out of danger/acute situation Loss of sensation?
Also site of mechanism of action of some of opioid narcotics Destruction of left…
Proprioception Vibration Pain
Fasciculus gracilis (at C4) L Lower limb L Lower limb –
Higher association cortex:
Cognition, integrated descending pain inputs onto opioid-containing PAG neurons Fasciculus cuneatus (at C4) L Upper limb L Upper limb –
Anterolateral system (at C4) – – R side (exc face)
A dorsal root ganglion (at C4) L neck L neck L neck
Ascending pain info
Caudal spinal trigeminal nucleus – – L face; V1-3???
Lateral 1º somatosensory cortex R arm R arm R arm
Medial primary somatosensory ctx R leg R leg R leg
Lateral pontine medial lemniscus R leg R leg –
Medial pontine medial lemniscus R arm R arm –
Synapse @ PAG, project to serotonergic neurons
in raphé nucleus of rostral medulla
Clinical syndromes involving damage to somatosensory NS (not necc. tissue)
Anesthesia: no sensations (numbness)
Paraesthesias: odd (unnatural) sensations – e.g. pins + needles, bugs under skin, etc.
Project to spinal cord act on 1º afferent neurons – damage to NS, but incomplete damage (arm falls asleep), not painful
Dysesthesias: odd sensations accompanied by discomfort or pain (“shooting,”
“electrical” pain, etc. – sciatica)
Tactile agnosias: inability to recognize objects based on tactile info
C-fibers:
express opioid receptors
Underlying principles RE parasthesia + dysesthesias:
In spinal cord:
o Peripheral axons attempt to regrow following injury; often form neuroma: sensitive
Serotonergic stimulus activates opioid- to non-specific somatosensory stimuli (random firing; NL pain fibers quiescent)
containing neurons in lamina 2
X These neurons act presynaptically on
o Higher ctx sensory areas recognize learned patterns of activity from end organs
Get input that doesn’t match a learned pattern don’t know how to interpret
C fibers projecting to lamina 2
X Dump opioid onto C fibers inhibits
Produce para/dysesthesia (if pain fibers involved)
Dorsal horn projection o Commonly seen in diabetes – loss of nerve sensations in feet, etc.
neuron (L2 L5) neurotransmission onto dorsal horn
projection neuron sending pain signal
to lamina 5 Brown-Séquard Syndrome: hemisection of
Result: analgesia the spinal cord (usually d/t trauma, ice pick)
Damage to:
Utility of opiates and biogenic amine neurotransmitters in the CNS o Ipsilateral dorsal column fibers:
CNS region Receptor expressed Action loss of discriminative touch
Release enkephalin onto µ- o Contralateral pain fibers,
Central gray of the
µ Opioid receptors enkephlinergic R’s on fibers of temperature loss
midbrain (PAG)
reticular formation Complete loss of sensation @ zone of
Raphé nucleus Activate opioid-containing hemisection
Serotonin
(rostral medulla) neurons in Lamina 2
Inhibit C fiber pain transmission
Substantia gelatinosa (L2) µ Opioid receptors to dorsal horn projection
neuron (site of epidural action)
Vous aimerez peut-être aussi
- NeuroTracts - Ascending, Descending, UMN, LMNDocument5 pagesNeuroTracts - Ascending, Descending, UMN, LMNBrandi Allen HensonPas encore d'évaluation
- Tracts of The Spinal CordDocument21 pagesTracts of The Spinal Corddr.a.k.gupta6924100% (10)
- Cranial Nerves (Association & Motor Neurons)Document2 pagesCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- Tracts of Spinal CordDocument4 pagesTracts of Spinal CordBrian HelbigPas encore d'évaluation
- Neuroanatomy Notes 2010Document33 pagesNeuroanatomy Notes 2010Jennifer David InauenPas encore d'évaluation
- 3-Ascending Tracts of Spinal CordDocument28 pages3-Ascending Tracts of Spinal Cordmuhammad altaf100% (2)
- Neuro LesionsDocument7 pagesNeuro Lesionskep1313100% (5)
- Mnemonic For Medical Students For Upper and Lower Motor LesionsDocument1 pageMnemonic For Medical Students For Upper and Lower Motor LesionsLe-Ann Mariamlelue100% (2)
- Descending Tracts: Dr. Niranjan Murthy H L Asst Prof of Physiology SSMC, TumkurDocument23 pagesDescending Tracts: Dr. Niranjan Murthy H L Asst Prof of Physiology SSMC, Tumkurnirilib100% (1)
- Guide To Neural PathwaysDocument1 pageGuide To Neural PathwaysFrancis Kevin SagudoPas encore d'évaluation
- Correlative Neuroanatomy of The Sensory SystemDocument8 pagesCorrelative Neuroanatomy of The Sensory SystemJonathan Gorospe100% (2)
- Brainstem & LesionsDocument4 pagesBrainstem & LesionsErnie G. Bautista II, RN, MDPas encore d'évaluation
- Ascending Descending TractsDocument46 pagesAscending Descending Tractsyasrul izad100% (3)
- Cranial Nerves and Its ExaminationDocument136 pagesCranial Nerves and Its ExaminationNileshPas encore d'évaluation
- Spinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalDocument65 pagesSpinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalKrishna Madhukar100% (1)
- Neuroanatomy TractsDocument4 pagesNeuroanatomy TractsLoveHouseMDPas encore d'évaluation
- D. Brainstem: PONS (Ventral Metencephalon) 1. External Consideration A. Ventral ViewDocument39 pagesD. Brainstem: PONS (Ventral Metencephalon) 1. External Consideration A. Ventral ViewMarvic SueltoPas encore d'évaluation
- Cranial NervesDocument45 pagesCranial Nervesmohanaramesh100% (1)
- (MicroB) 3.6 Brainstem LesionsDocument6 pages(MicroB) 3.6 Brainstem Lesionsnelson lopezPas encore d'évaluation
- Cranial NervesDocument65 pagesCranial NervesatefmaboodPas encore d'évaluation
- Draw It To Know It NotesDocument13 pagesDraw It To Know It Noteskat9210Pas encore d'évaluation
- 21-Spinal Cord TractsDocument23 pages21-Spinal Cord TractsALFAHRUL CAHYADIPas encore d'évaluation
- Functional Areas of Cerebral CortexDocument3 pagesFunctional Areas of Cerebral CortexMatet MonjePas encore d'évaluation
- Anatomic LocalizationDocument9 pagesAnatomic Localizationkid100% (1)
- Brain Areas - Location and FunctionDocument12 pagesBrain Areas - Location and FunctionMattGilmorePas encore d'évaluation
- REFLEXESDocument15 pagesREFLEXESSonali Soumyashree100% (2)
- Descending TractDocument10 pagesDescending TractQairul AzmanPas encore d'évaluation
- Nerve TractsDocument38 pagesNerve TractsAbualauon AlbeblawyPas encore d'évaluation
- MnemonicsDocument34 pagesMnemonicsAleena Stephen100% (2)
- (MicroB) Brainstem Lesions - Dr. Bravo (Nico Castillo)Document4 pages(MicroB) Brainstem Lesions - Dr. Bravo (Nico Castillo)miguel cuevasPas encore d'évaluation
- Cranial NervesDocument17 pagesCranial Nervesdankirsh100% (17)
- Approach To Stroke PatientDocument16 pagesApproach To Stroke PatientNEuRoLoGisT CoFFeeCuP100% (2)
- Study Guide NeurophysiologyDocument2 pagesStudy Guide NeurophysiologyAndrew MajorPas encore d'évaluation
- Neuroanatomy and Cerebrovascular CirculationDocument54 pagesNeuroanatomy and Cerebrovascular CirculationLemuel Pamaran del CastilloPas encore d'évaluation
- Cranial Nerves SummaryDocument3 pagesCranial Nerves SummaryJoash F. Pacquing75% (4)
- Neuroanatomy Brainstem SummaryDocument11 pagesNeuroanatomy Brainstem SummaryStd Dlshsi100% (2)
- Anatomy MnemonicsDocument15 pagesAnatomy Mnemonicskolintang1Pas encore d'évaluation
- UMass Medical School Mind Brain Behavior 1 Spinal Cord Atlas OverviewDocument11 pagesUMass Medical School Mind Brain Behavior 1 Spinal Cord Atlas Overviewnon_zense100% (1)
- CNS Structure and Function - Anatomy of the Brain and Spinal CordDocument18 pagesCNS Structure and Function - Anatomy of the Brain and Spinal CordAnna Marthea V.100% (4)
- Neuroanatomy NotesDocument8 pagesNeuroanatomy NotesJustine May GervacioPas encore d'évaluation
- Gross Brain and Spinal CordDocument36 pagesGross Brain and Spinal CordAmr KandeelPas encore d'évaluation
- Neurology NotesDocument15 pagesNeurology NotesAshley Diane Henry100% (3)
- Spinal Cord LesionsDocument110 pagesSpinal Cord Lesionsgtaha80100% (1)
- Neuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansDocument29 pagesNeuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansAngelaTrinidad100% (2)
- Brainstem Bravo AnnotatedDocument13 pagesBrainstem Bravo AnnotatedMia CadizPas encore d'évaluation
- SMP Neuro Lab ManualDocument37 pagesSMP Neuro Lab Manualsas345sas345Pas encore d'évaluation
- Anatomy MnemonicsDocument2 pagesAnatomy MnemonicsPia Boni0% (1)
- Cranial Nerve Exam Part 1Document9 pagesCranial Nerve Exam Part 1Jennifer Pisco LiracPas encore d'évaluation
- Explore the Nervous System in 40 CharactersDocument31 pagesExplore the Nervous System in 40 CharactersDeology JuaninoPas encore d'évaluation
- Neuroanatomy Practical 2nd ShiftDocument2 pagesNeuroanatomy Practical 2nd Shiftapi-3742802Pas encore d'évaluation
- Neuromuscular DisordersDocument1 pageNeuromuscular DisordersYanaPas encore d'évaluation
- Neurology MnemonicsDocument11 pagesNeurology MnemonicsOstaz100% (1)
- Auditory Brainstem ResponseDocument18 pagesAuditory Brainstem ResponseFree dataPas encore d'évaluation
- UMN Vs LMN Including MnemonicDocument2 pagesUMN Vs LMN Including MnemonicshahzebPas encore d'évaluation
- Visually Memorable Neuroanatomy for BeginnersD'EverandVisually Memorable Neuroanatomy for BeginnersÉvaluation : 5 sur 5 étoiles5/5 (1)
- Physiology FC PainDocument4 pagesPhysiology FC Painiqz saniomePas encore d'évaluation
- Somatic SensationsDocument13 pagesSomatic SensationsStd DlshsiPas encore d'évaluation
- Nutritional Handouts For WebsiteDocument12 pagesNutritional Handouts For WebsiteCaraPas encore d'évaluation
- Nutrilite Body Key Traning DeckDocument92 pagesNutrilite Body Key Traning DeckTapan Chowdhury100% (1)
- Fischer General-CatalogueDocument108 pagesFischer General-Cataloguebo cephusPas encore d'évaluation
- Organic Baby Care Products for Sensitive SkinDocument7 pagesOrganic Baby Care Products for Sensitive SkinNiraj KumarPas encore d'évaluation
- Zombicidegn 1Document4 pagesZombicidegn 1Fran OlmedoPas encore d'évaluation
- Strain Hardening in Aerospace AlloysDocument14 pagesStrain Hardening in Aerospace AlloysAbdelwahab ElaichiPas encore d'évaluation
- CMT2210LC en V0.9 20170817Document20 pagesCMT2210LC en V0.9 20170817Ta ToPas encore d'évaluation
- Gokarna Murudeshwar Vibuthi Falls 3-Day TourDocument3 pagesGokarna Murudeshwar Vibuthi Falls 3-Day TourRama Krishna NaniPas encore d'évaluation
- When To Use Therapeutic Ultrasound TherapyDocument2 pagesWhen To Use Therapeutic Ultrasound TherapyPrakash KulkarniPas encore d'évaluation
- Différence Et Similitudes Entre ASME Et AWSDocument63 pagesDifférence Et Similitudes Entre ASME Et AWSImane KhammouriPas encore d'évaluation
- Health Optimizing Physical EducationDocument18 pagesHealth Optimizing Physical Education95lineVmin BestFriendsForever0% (1)
- Technical specs for Figaro oxygen sensor SK-25FDocument9 pagesTechnical specs for Figaro oxygen sensor SK-25FAbner MorenoPas encore d'évaluation
- Prepearing Teeth For RPDDocument14 pagesPrepearing Teeth For RPDShreyans DamadePas encore d'évaluation
- Lectut-MTN-105-Doc-MT 201A-Tutorial - CH 1 (4 Files Merged)Document9 pagesLectut-MTN-105-Doc-MT 201A-Tutorial - CH 1 (4 Files Merged)Vikhyath KstPas encore d'évaluation
- SBM Level of Practice: Daraetan Integrated SchoolDocument18 pagesSBM Level of Practice: Daraetan Integrated SchoolRose AquinoPas encore d'évaluation
- Vaginal CarcinomaDocument8 pagesVaginal CarcinomaMutiarawati MithrataelúwånzhùPas encore d'évaluation
- BA Sem - 3 English (Core/Elective) - Paper - 201 Notes On Solitude' by PopeDocument2 pagesBA Sem - 3 English (Core/Elective) - Paper - 201 Notes On Solitude' by PopeAnkur AryaPas encore d'évaluation
- Approval Project Manager: Ministry of Electricity (Moe) Republic of IraqDocument5 pagesApproval Project Manager: Ministry of Electricity (Moe) Republic of IraqAlinaIordachePas encore d'évaluation
- Desalination: Yawen Wang, Aimin Li, Hu YangDocument10 pagesDesalination: Yawen Wang, Aimin Li, Hu YangDrFatema HussainPas encore d'évaluation
- Product & Manufacturing Process Audit Checklist: Part NumberDocument6 pagesProduct & Manufacturing Process Audit Checklist: Part NumberDuy Le100% (4)
- IGFR-4: Ground Fault Relay With Adjustable Time Delay Part Number: 1100-0104Document4 pagesIGFR-4: Ground Fault Relay With Adjustable Time Delay Part Number: 1100-0104Brandon Bryan Gomez RodriguezPas encore d'évaluation
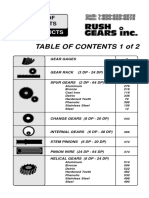
- C 2000 Rush 2Document644 pagesC 2000 Rush 2Rashpal DhanotaPas encore d'évaluation
- SWIGGY's competitive strategies and business modelDocument11 pagesSWIGGY's competitive strategies and business modelARUSHI CHATURVEDI100% (1)
- Thermador DWHD64EFDocument1 pageThermador DWHD64EFPurcellMurrayPas encore d'évaluation
- Why We Fall Ill QuestionsDocument1 pageWhy We Fall Ill Questionsr_phyPas encore d'évaluation
- PM01 - PM Master DataDocument32 pagesPM01 - PM Master DataSandeepPas encore d'évaluation
- Lifting Equipment ChecklistDocument4 pagesLifting Equipment ChecklistRuzaini MohamedPas encore d'évaluation
- Challenges of Catholic Doctors in The Changing World - 15th AFCMA Congress 2012Document218 pagesChallenges of Catholic Doctors in The Changing World - 15th AFCMA Congress 2012Komsos - AG et al.Pas encore d'évaluation
- Fire Hose ReelDocument2 pagesFire Hose Reelkristian08Pas encore d'évaluation
- Worksheet 12.4 Reflex ArcDocument5 pagesWorksheet 12.4 Reflex ArcRay PeramathevanPas encore d'évaluation