Académique Documents
Professionnel Documents
Culture Documents
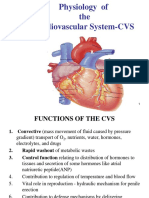
Cardiovascular System
Transféré par
theglobalnursingCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cardiovascular System
Transféré par
theglobalnursingDroits d'auteur :
Formats disponibles
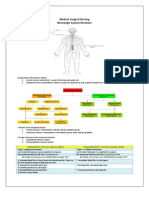
Medical-Surgical Nursing Cardiopulmonary System Anatomy of the Heart
Coverings Pericardium a. fibrous pericardium b. serous Layers 1. 2. 3. Epicardium (visceral pericardium) -protects heart Myocardium cardiac muscle Endocardium epithelial/ connective/ fibers Muscular, pumping organ of the body Left mediastinum Weigh 300 400 grams Resembles a closed fist Covered by serous membrane pericardium
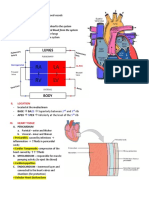
Four chambers A. Upper chambers -Collects blood 1. right atria 2. left atria B. Lower chambers -pumps blood from heart 1. right ventricle 2. left ventricle Arteries carry blood away from heart Veins blood toward heart Valves A. AV valves 1. Tricuspid right atrium 2. Bicuspid or mitral - left atrium Semilunar valves 1. Pulmonary semilunar (pulmonary trunk) 2. Aortic semilunar (aortic arch)
B.
Passage of Blood Through the Heart Blood follows this sequence through the heart: superior and inferior vena cava right atrium tricuspid valve right ventricle pulmonary semilunar valve pulmonary trunk and arteries to the lungs pulmonary veins leaving the lungs left atrium bicuspid valve left ventricle aortic semilunar valve aorta to the body. Blood supply to the heart Arterial supply The heart is supplied with arterial blood by the right and left coronary arteries, which branch from the aorta immediately distal to the aortic valve The coronary arteries receive about 5% of the blood pumped from the heart, although the heart comprises a small proportion of body weight This large blood supply, especially to the left ventricle, highlights the importance of the heart to body function The coronary arteries traverse the heart, eventually forming a vast network of capillaries Venous drainage Most of venous blood is collected into several small veins that join to form coronary sinus, which opens into right atrium
The remainder passes directly into the heart chambers through little venous channels
CARDIAC CYCLE
1. sequence of events that occur when the heart beats There are two phases of this cycle: Diastole - Ventricles are relaxed Systole - Ventricles contract Heart at rest Blood flows from large veins into atria Passive flow from atria into ventricles Atria (R & L) contract simultaneously Blood forced into ventricles Ventricles (R & L) contract simultaneously Atrioventricular valves close lubb sound Blood forced into large arteries Ventricles relax Semilunar valves close dub sound Heart at rest
2.
3. 4.
5. 6.
Heart valves Valves are flap-like structures that allow blood to flow in one direction The heart has two kinds of valves, atrioventricular and semilunar valves
Conducting system of Heart SA node
Acting as the heart's natural pacemaker, the SA node "fires" at regular intervals to cause the heart of beat with a rhythm of about 60 to 70 beats per minute for a healthy, resting heart The electrical impulse from the SA node triggers a sequence of electrical events in the heart to control the orderly sequence of muscle contractions that pump the blood out of the heart The AV node (AV stands for atrioventricular) is an electrical relay station between the atria (the upper) and the ventricles (the lower chambers of the heart) Electrical signals from the atria must pass through the AV node to reach the ventricles
AV node
AV node (bundle of his)
The bundle of His is located in the proximal interventicular septum It emerges from the AV node to begin the conduction of the impulse from the AV node to the ventricles
Purkinje fibers
Purkinje fibers are heart muscle tissues that are specialized to conduct electrical impulses to ventricular cells, which induce the lower chambers of the heart to contract Impulses from the upper chambers of the heart are relayed by this node to large bundles of Purkinje fibers referred to as the Bundle of His These bundles branch into smaller elements and eventually form terminal ends that burrow into left and right ventricular chamber muscles As the impulse is passed to the ventricles, the muscles contract and pump blood The contraction caused by the specialized fibers begins from the bottom of the ventricles and move upwards so that the blood leaves the lower chambers through the pulmonary arteries and the aorta
Electrocardiography Cardiac Output
CO is the amount of blood pumped by each ventricle in one minute CO is the product of heart rate (HR) and stroke volume (SV) HR is the number of heart beats per minute SV is the amount of blood pumped out by a ventricle with each beat
Regulation of Stroke Volume
SV = end diastolic volume (EDV) minus end systolic volume (ESV) EDV = amount of blood collected in a ventricle during diastole ESV = amount of blood remaining in a ventricle after contraction
Blood Vessels
Functions: Distribution of blood Exchange of materials with tissues Return of blood to the heart Structure:
Most have the same basic structure: 3 layers surrounding a hollow lumen
Arteries and veins are composed of three tunics: 1. tunica interna 2. tunica media 3. tunica externa Tunica Intima innermost smooth layer simple squamous epithelium continuous with the endocardium present in all vessels Tunica Media layer of smooth muscle - circular arrangement contains elastin supplied by sympathetic division of the ANS depending on bodys needs lumen is narrowed (vasoconstriction) or widened (vasodilation) Tunica Externa (Adventitia) thin layer of CT elastic & collagen fibres
Vessels Types
1. 2. 3. Arteries carry blood away from the heart Veins carry blood towards the heart Capillaries the most important part of the vascular system; site of exchange of materials
Disorders of the Cardiopulmonary System ATHEROSCLEROSIS
- condition in which an artery wall thickens as a result of the accumulation of fatty materials such as cholesterol
-commonly referred to as a hardening or furring of the arteries. It is caused by the formation of multiple plaques within the arteries
Predisposing Factor 1. Sex male 2. Black race 3. Hyperlipidemia 4. Smoking 5. HPN 6. DM 7. Oral contraceptive- prolonged use 8. Sedentary lifestyle 9. Obesity 10. Hypothyroidism Signs & Symptoms 1. Chest pain 2. Dyspnea 3. Tachycardia 4. Palpitations 5. Diaphoresis Treatment P percutaneous T tansluminar C coronary A angioplasty Objective: 1. To revascularize the myocardium 2. To prevent angina 3. Increase survival rate PTCA done to pt. with single occluded vessel CABAG-for Multiple occluded vessels is CABAG C coronary A arterial B bypass A and G graft surgery Nsg Mgt Before CABAG 1. Deep breathing cough exercises 2. Use of incentive spirometer 3. Leg exercises
ANGINA PECTORIS
- A clinical syndrome characterized by paroxysmal chest pain usually relieved by REST or NGT nitroglycerin, resulting from myocardial ischemia Predisposing Factor 1. sex male 2. black raise 3. hyperlipidemia 4. smoking 5. HPN 6. DM 7. oral contraceptive prolonged 8. sedentary lifestyle 9. obesity 10.hypothyroidism
Precipitating factors 4 Es 1. Excessive physical exertion 2. Exposure to cold environment - Vasoconstriction 3. Extreme emotional response 4. Excessive intake of food saturated fats. Signs & Symptoms 1. Initial symptoms Levines sign hand clutching of chest Chest pain sharp, stabbing excruciating pain. Location substernal -radiates back, shoulders, axilla, arms & jaw muscles -relieve by rest or NGT 2. Dyspnea 3. Tachycardia 4. Palpitation 6.diaphoresis Diagnosis 1.History taking & PE 2. ECG ST segment depression 3. Stress test treadmill = abnormal ECG 4. Serum cholesterol & uric acid - increase Nursing Management 1.) Enforce Complete Bed Rest 2.) Administer medications as ordered NTG small doses venodilator Large dose vasodilator 1st dose NTG give 3 5 min 2nd dose NTG 3 5 min 3rd & last dose 3 5 min Still painful after 3rd dose notify the phycisian, It may be a sign of Myocardial Infaction Medications: A. NTG- Nsg Mgt: 1. Keep in a dry place. Avoid moisture & heat, may inactivate the drug 2. Monitor S/E: a. orthostatic hypotension decrease BP b. transient headache c. dizziness 3. Rise slowly from sitting position 4. Assist in ambulation. 5. If giving NTG via patch: a. avoid placing it near hairy areas because it will decrease drug absorption b. avoid rotating transdermal patches it will decrease drug absorption c. avoid placing near microwave oven or during defibrillation it will burn pt. due aluminum foil in patch B. Beta blockers propanolol C. ACE inhibitors captopril D. Ca antagonist - nefedipine 3.) Administer O2 inhalation 4.) Semi-fowler 5.) Diet- Decrease Na and saturated fats 6.) Monitor VS, I&O, ECG 7.) Health Teaching a. Avoid precipitating factors 4 Es b. Prevent complications MI c. Take meds before physical exertion-to achieve maximum therapeutic effect of drug d. Importance of follow-up care
MYOCARDIAL INFARCTION(MI)
-hear attack terminal stage of CAD -Characterized by necrosis & scarring due to permanent mal-occlusion Types 1. 2.
Trasmural MI most dangerous MI Mal-occlusion of both R&L coronary artery Sub-endocardial MI mal-occlusion of either R & L coronary artery
Most critical period upon diagnosis of MI 48 to 72h Because majority of pt suffers from PVC premature ventricular contraction Predisposing factors sex male black raise hyperlipidemia smoking HPN DM oral contraceptive prolong ed 8. sedentary lifestyle 9. obesity 10. hypothyroidism 1. 2. 3. 4. 5. 6. 7. Signs & symptoms 1. chest pain excruciating, vice like, visceral pain located substernal or precodial area (rare) - radiates back, arm, shoulders, axilla, jaw & abd muscles. - not usually relived by rest r NTG 2. dyspnea 3. erthermia 4. initial increase in BP 5. mild restlessness & apprehensions 6. occasional findings a.) split S1 & S2 b.) pericardial friction rub c.) rales /crackles d.) S4 (atrial gallop) Diagnostic Exam 1. cardiac enzymes a.) CPK MB Creatinine Phosphokinase b.) LDH lactic acid dehydrogenase c.) SGPT (ALT) Serum Glutanic Pyruvate Transaminase- increased d.) SGOT (AST) Serum Glutamic Oxalo-acetic - increased 2. Troponin test increase 3. ECG tracing ST segment increase, widening or QRS complexes means arrhythmia in MI indicating PVC 4. serum cholesterol & uric acid - increase 5. CBC increase WBC
Nursing Management 1. Narcotic analgesics Morphine SO4 to induce vasodilation & decrease levels of anxiety 2. Administer O2 inhalation low inflow (CHF-increase inflow) 3. Enforce Complete Bed Rest without BP a.) Prepare commode at bedside 4. Avoid valsalva maneuver 5. Semi fowler 6. General liquid to soft diet decrease Na, saturated fat, caffeine 7. Monitor VS, I&O & ECG tracings 8. Take 20 30 ml/week wine, brandy/whisky to induce vasodilation 9. Assist in surgical; CABAG 10. Provide pt. Health Teaching a.) Avoid modifiable risk factors b.) Prevent complications: 1. Arrhythmias PVC 2. Shock cardiogenic shock. Late signs of cardiogenic shock in MI oliguria 3. Thrombophlebitis - deep vein 4. CHF left sided 5. Dresslers syndrome post MI syndrome -Resistant to medications -Administer 150,000 450,000 units of streptokinase c.) Strict compliance to medications 1. Vasodilators a. NTG b. Isordil 2. Antiarrythmic a. Lydocaine b. Brithylium 3. Beta-blockers lol a. Propanolol (inderal) 4. ACE inhibitors - pril a. Captopril (enalapril) 5. Ca antagonist a. Nifedipine 6. Thrombolitics or fibrinolytics to dissolve clots/ thrombus
d.) Resume ADL sex/ activity after 4 to 6 weeks
1.)Sex as an appetizer rather then dessert Before meals not after, due after meals increase metabolism heart is pumping hard after meals. 2.) Position non-weight bearing position When to resume sex/ act: When pt can already use staircase, then he can resume sex. e.) Diet decrease Na, Saturated fats, and caffeine f.) Follow up care
CONGESTIVE HEART FAILURE(CHF)
- Inability of heart to pump blood towards systemic circulation - Backflow -CHF can be Left-sided or Right-sided -Left-sided CHF can lead to Right-sided CHF, but Right cannot lead to Left -Lasix is given to both types of CHF -CHF is the inability of the heart to pump blood towards systemic circulation RIGHT-SIDED CHF the #1 cause is TRICUSPID VALVE STENOSIS LEFT-SIDED CHF the #1 cause is MITRAL VALVE STENOSIS
Left sided heart failure
Predisposing factors -Can be caused by Rheumatic Heart Disease: Tonsillitis strep bacteria migrate to mitral valve RHEUMATIC HEART DISEASE mitral stenosis LSHF Complication 1. Right Sided-CHF 2. Aging degeneration / calcification of mitral valve 3. Ischemic heart disease 4. HPN, MI, Aortic stenosis Signs and Symptoms Pulmonary congestion/ Edema 1. Dyspnea 2. Orthopnea 3. Paroxysmal nocturnal dysnea 4. Productive cough with blood tinged sputum 5. Frothy salivation (from lungs) 6. Cyanosis 7. Rales/ crackles due to fluid 8. Bronchial wheezing 9. PMI(Point of Maximal Implant) is displaced laterally due to cardiomegaly 10. Pulsus alternons weak-strong pulse 11. Anorexia & general body malaise 12. S3 extra heart sound (Ventricular gallop) Diagnostic 1. Chest Xray cardiomegaly 2. PAP Pulmonary Arterial Pressure PCWP Pulmonary CapillaryWedge Pressure 3. Echocardiography reveals enlarged heart chamber or cardiomayopathy 4. ABG PCO2 increase, PO2 decrease = = hypoxemia = resp acidosis
Right sided HF
Predisposing factor 1. 90% - tricuspid stenosis 2. COPD 3. Pulmonary embolism 4. Pulmonic stenosis 5. Left sided heart failure Signs and Symptoms 1. Venous congestion 2. Neck or jugular vein distension
3. 4. 5. 6. 7. 8. 9. 10.
Pitting edema Ascites Wt gain Hepatomegalo/ splenomegaly Jaundice Pruritus Esophageal varies Anorexia, gen body malaise
Diagnosis 1. CXR cardiomegaly 2. CVP measures the pressure at R atrium Normal: 4 to 10 cm of water Increase CVP > 10 hypervolemia Decrease CVP < 4 hypovolemia Flat on bed position of pt. when giving CVP Position during CVP insertion Trendelenburg to prevent pulmonary embolism & promote ventricular filling 3. Echocardiography enlarged heart chamber / cardiomyopathy 4.Liver enzyme Increase SGPT ( ALT) Increase SGOT AST Nursing Management 1.Administer medications as ordered Treatment for LSHF: M morphine SO4 to induce vasodilatation A aminophylline & decrease anxiety D digitalis (digoxin) D - diuretics O - oxygen G - gases a.) Cardiac glycosides Increase myocardial = increase CO Digoxin (Lanoxin). Antidote: digivine Digitoxin: metabolizes in liver not in kidneys not given if with kidney failure. b.) Loop diuretics: Lasix takes effect within 10-15 min. Max = 6 hrs c.) Bronchodilators: Aminophillin (Theophyllin). Avoid giving caffeine d.) Narcotic analgesic: Morphine SO4 - induce vasodilaton & decrease anxiety e.) Vasodilators NTG f.) Anti-arrythmics Lidocaine 2. Administer O2 inhalation @ 3 -4L/min via nasal cannula 3. High fowlers 4. Restrict Na 5. Provide meticulous skin care 6. Weigh pt. daily. Assess for pitting edema. Measure abdominal girth daily & notify MD 7. Monitor V/S, I&O, breath sounds 8. Institute bloodless phlebotomy. Rotating tourniquet or BP cuff rotated clockwise q 15 mins to promote decrease venous return 9. Diet decrease salt, fats & caffeine 10. Health Teachings Complications : 1. shock 2. Arrhythmia 3. Thrombophlebitis 4. MI 5. Cor Pulmonale RT ventricular hypertrophy b.) Dietary modifications c.) Adherence to meds
PERIPHERAL MUSCULAR DISEASE Thromboangiitis obliterates/ BUERGER DISEASE
- Acute inflammatory disorder affecting small to medium sized arteries & veins of lower extremities Predisposing factors: Male Smokers Signs and Symptoms 1. Intermittent claudication leg pain upon walking relieved by rest 2. Cold sensitivity & skin color changes 3. Decrease or diminished peripheral pulses - Post tibial, Dorsalis pedis 4. Tropic changes 5. Ulcerations 6. Gangrene formation Dianostic 1. Oscillometry decrease peripheral pulse volume 2. Doppler UTZ decrease blood flow to affected extremities 3. Angiography reveals site & extent of mal-occlusion Nursing Management 1. Encourage a slow progression of physical activity a.) Walk 3 -4 x / day b.) Out of bed 2 3 x a / day 2. Administer medications as ordered a.) Analgesic b.) Vasodilator c.) Anticoagulant 3. Foot care mgt. like DM a.) Avoid walking barefoot b.) Cut toe nails straight c.) Apply lanolin lotion prevent skin breakdown d.) Avoid wearing constrictive garments 4. Avoid smoking & exposure to cold environment 5. Surgery: BKA (Below the knee amputation)
REYNAUDS PHENOMENON
acute episodes of arterial spasm affecting digits of hands & fingers Predisposing factors 1. Female, 40 yrs 2. Smoking 3. Collagen disease a. SLE pathognomonic sign butterfly rash on face 1. Chipmunk face bulimia nervosa 2. Cherry red skin carbon monoxide poisoning 3. Spider angioma liver cirrhosis 4. Caput medusae leg & trunk umbilicus- Liver cirrhosis 5. Lion face leprosy b. Rheumatoid arthritis 4. Direct hand trauma piano playing, excessive typing, operating chainsaw
Signs and Symptoms
1. 2.
Intermittent claudication - leg pain upon walking - Relieved by rest Cold sensitivity
Nursing Management a. Analgesics b. Vasodilators c. Encourage to wear gloves especially when opening a refrigerator d. Avoid smoking & exposure to cold environment
Vous aimerez peut-être aussi
- Cardionursing 110207023802 Phpapp01Document18 pagesCardionursing 110207023802 Phpapp01LudwigJayBarayuga100% (5)
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruPas encore d'évaluation
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruPas encore d'évaluation
- Cardiovascular SystemDocument34 pagesCardiovascular Systemkaz92100% (6)
- 05 Cardiovascular System PhysiologyDocument34 pages05 Cardiovascular System PhysiologyKaye Alyssa EnriquezPas encore d'évaluation
- Physiology Cardiovascular Physiology NotesDocument13 pagesPhysiology Cardiovascular Physiology Noteshedayatamin44Pas encore d'évaluation
- Blood Flow: Right AtriumDocument2 pagesBlood Flow: Right AtriumDaffodelle AnnePas encore d'évaluation
- Cardiovascular System ReviewDocument9 pagesCardiovascular System ReviewsenjicsPas encore d'évaluation
- Anatomy & Physiology Mid-Semster Study Notes PDFDocument32 pagesAnatomy & Physiology Mid-Semster Study Notes PDFsimone dumbrell100% (10)
- Cardiovascular Anatomy Physiology PDFDocument22 pagesCardiovascular Anatomy Physiology PDFMahesh ChendakePas encore d'évaluation
- Lesson 12 HeartDocument9 pagesLesson 12 HeartEly FructuosoPas encore d'évaluation
- Cardiovascular Pharmacology: - Hypertension - Angina Pectoris - Cardiac Arrhythmias - Heart FailureDocument31 pagesCardiovascular Pharmacology: - Hypertension - Angina Pectoris - Cardiac Arrhythmias - Heart Failurelynch775100% (2)
- Anatomy and Physiology Terms: Brief Definitions, Roots & Morphology; An Abecedary; Vol 2-Planes & DirectionsD'EverandAnatomy and Physiology Terms: Brief Definitions, Roots & Morphology; An Abecedary; Vol 2-Planes & DirectionsPas encore d'évaluation
- Handout 5 CardioVascular System Overview PDFDocument7 pagesHandout 5 CardioVascular System Overview PDFGrape JuicePas encore d'évaluation
- Medsurg Cardio Ana&PhysioDocument6 pagesMedsurg Cardio Ana&Physiorabsibala80% (10)
- Anatomy and Physiology DefinedDocument78 pagesAnatomy and Physiology DefinedFhen Farrel100% (5)
- Cardiovascular SystemDocument24 pagesCardiovascular SystemCandice100% (1)
- Appendicular Worksheet With Answers ch.11Document7 pagesAppendicular Worksheet With Answers ch.11Alejandra ReynaPas encore d'évaluation
- Joyce Y. Visitacion NCM 104 Bsn-4Aj SY 2008-2009 Musculoskeletal SystemDocument33 pagesJoyce Y. Visitacion NCM 104 Bsn-4Aj SY 2008-2009 Musculoskeletal Systemyawdle100% (6)
- Cardiovascular NotesDocument23 pagesCardiovascular NotesEmily DongPas encore d'évaluation
- CARDIOLOGYDocument15 pagesCARDIOLOGYPatty RomeroPas encore d'évaluation
- Unit VI Lecture Notes - Respiratory SystemDocument6 pagesUnit VI Lecture Notes - Respiratory SystemSteve Sullivan100% (3)
- Human Anatomy and Physiology NotesDocument19 pagesHuman Anatomy and Physiology NotesRachel Kwong100% (2)
- Between The Erythrocytes and PlasmaDocument5 pagesBetween The Erythrocytes and Plasmajonette carataoPas encore d'évaluation
- Anatomy and Physiology Nursing Mnemonics TipsDocument8 pagesAnatomy and Physiology Nursing Mnemonics TipsariPas encore d'évaluation
- Cardiac DrugsDocument35 pagesCardiac DrugsCristina Centurion100% (3)
- Anatomy and Physiology The HeartDocument21 pagesAnatomy and Physiology The Heartkheng100% (4)
- Exam A-3Document11 pagesExam A-3yapues87Pas encore d'évaluation
- BloodDocument9 pagesBloodCailah Sofia SelausoPas encore d'évaluation
- Endocrine System NotesDocument7 pagesEndocrine System Notesmorganical100% (3)
- Cardiovascular NotesDocument11 pagesCardiovascular NotesJireh Acabal100% (1)
- AnaPhy Lesson 6 Muscular SYstemDocument7 pagesAnaPhy Lesson 6 Muscular SYstemLM KishimotoPas encore d'évaluation
- Heart Circulatory System Study GuideDocument10 pagesHeart Circulatory System Study GuideKyle YiPas encore d'évaluation
- 13th Edition Chapter 4 Test BankDocument61 pages13th Edition Chapter 4 Test BankFirst Last100% (2)
- ECG Review Packet-1Document23 pagesECG Review Packet-1Tori RolandPas encore d'évaluation
- Pharmacology Pharmacokinetics Flash CardsDocument17 pagesPharmacology Pharmacokinetics Flash Cardsbobiome100% (1)
- Nurs 1300 Case Studies and Lab WorkDocument11 pagesNurs 1300 Case Studies and Lab WorkNancy Cummings0% (1)
- Digestive System Anatomy and Physiology - NurseslabsDocument33 pagesDigestive System Anatomy and Physiology - NurseslabsMari FePas encore d'évaluation
- Cardiovascular SystemDocument25 pagesCardiovascular Systemangel_maui100% (22)
- Patho Test Bank 2021Document194 pagesPatho Test Bank 2021wonyoungg5813100% (1)
- CVS Lect 6 Blood Pressure, PathophysiologyDocument13 pagesCVS Lect 6 Blood Pressure, PathophysiologySherwan R Shal100% (5)
- Exam 2 - Neurological Study GuideDocument10 pagesExam 2 - Neurological Study GuideStephaniePas encore d'évaluation
- Cardiac OutputDocument31 pagesCardiac OutputanojPas encore d'évaluation
- Cardiac Cycle NotesDocument20 pagesCardiac Cycle NotesKelly Yeow100% (3)
- Respiratory Physiology NOTESDocument3 pagesRespiratory Physiology NOTESJulienne Sanchez-Salazar100% (1)
- PerfusionDocument9 pagesPerfusionAmanda Brittain100% (2)
- Renal SystemDocument65 pagesRenal Systemxarae23Pas encore d'évaluation
- Cardiac CycleDocument38 pagesCardiac CycleKok HoongPas encore d'évaluation
- A&P Coloring Nervous Worksheet PDFDocument20 pagesA&P Coloring Nervous Worksheet PDFHelen English100% (1)
- Nursing Respiratory SystemDocument254 pagesNursing Respiratory SystemWendy EvansPas encore d'évaluation
- Endocrine System Review Flashcards - QuizletDocument5 pagesEndocrine System Review Flashcards - QuizletDani Anyika100% (1)
- Cardiac CycleDocument30 pagesCardiac CycleNosh AnbreenPas encore d'évaluation
- Reproduction Test For Anatomy & Physiology IIDocument33 pagesReproduction Test For Anatomy & Physiology IIlhayes1234100% (5)
- Chapter 20 - The Lymphatic SystemDocument5 pagesChapter 20 - The Lymphatic SystemTony SnearlyPas encore d'évaluation
- Functional Organization of Cardiovascular SystemDocument19 pagesFunctional Organization of Cardiovascular SystemIbtesam Mohammed100% (2)
- 511-525chapter 6-8 (1) An Introduction To The Skeletal SystemDocument6 pages511-525chapter 6-8 (1) An Introduction To The Skeletal Systemtomorrow.today.yesterday .yesterdayPas encore d'évaluation
- ODY Efenses: Ap Biology Name Animals Form & Function Activity #4 Date HourDocument5 pagesODY Efenses: Ap Biology Name Animals Form & Function Activity #4 Date Hourancientblackdragon0% (1)
- EKG Quick Reference ChartDocument4 pagesEKG Quick Reference ChartMildaPas encore d'évaluation
- NLE 12-2012 ResultsDocument359 pagesNLE 12-2012 ResultsPRC Baguio0% (2)
- Summary Differences Between Dementia and DeliriumDocument4 pagesSummary Differences Between Dementia and Deliriumtheglobalnursing100% (1)
- Disorders of Cranial NervesDocument3 pagesDisorders of Cranial Nervestheglobalnursing100% (2)
- Congenital Heart DiseasesDocument6 pagesCongenital Heart Diseasestheglobalnursing100% (2)
- Perioperative NursingDocument12 pagesPerioperative Nursingtheglobalnursing100% (12)
- Major Fluid and Electrolyte ImbalancesDocument5 pagesMajor Fluid and Electrolyte ImbalancestheglobalnursingPas encore d'évaluation
- Common Eye Problems in ChildrenDocument6 pagesCommon Eye Problems in ChildrentheglobalnursingPas encore d'évaluation
- Disorders of The Lips, Mouth and GumsDocument5 pagesDisorders of The Lips, Mouth and GumstheglobalnursingPas encore d'évaluation
- Common Signs and Symptoms of Diseases (Pathognomonic Sign)Document3 pagesCommon Signs and Symptoms of Diseases (Pathognomonic Sign)theglobalnursing91% (11)
- Emergency Management of Patients With Drug OverdoseDocument6 pagesEmergency Management of Patients With Drug Overdosetheglobalnursing0% (1)
- Gastrointestinal SystemDocument8 pagesGastrointestinal Systemtheglobalnursing100% (1)
- Expanded Program On ImmunizationDocument1 pageExpanded Program On ImmunizationtheglobalnursingPas encore d'évaluation
- Respiratory SystemDocument9 pagesRespiratory Systemtheglobalnursing89% (9)
- Fundamentals of NursingDocument44 pagesFundamentals of Nursingtheglobalnursing100% (2)
- Musculoskeletal System Nursing ReviewerDocument11 pagesMusculoskeletal System Nursing Reviewerposh003850% (2)
- Neurologic NursingDocument14 pagesNeurologic Nursingtheglobalnursing100% (6)
- Endocrine SystemDocument8 pagesEndocrine Systemtheglobalnursing80% (5)
- Pyschiatric NursingDocument40 pagesPyschiatric Nursingtheglobalnursing100% (1)
- Community Health NursingDocument9 pagesCommunity Health NursingtheglobalnursingPas encore d'évaluation
- Classical and Operant Conditioning ExamplesDocument6 pagesClassical and Operant Conditioning ExamplesPersephone355100% (1)
- Implementing Self-Administration of Insulin in Hospital: A Journey of Discovery and Innovation. Part 1: Culture and StorageDocument4 pagesImplementing Self-Administration of Insulin in Hospital: A Journey of Discovery and Innovation. Part 1: Culture and Storagesunrise755Pas encore d'évaluation
- Topic: Going To and Coming From Place of WorkDocument2 pagesTopic: Going To and Coming From Place of WorkSherry Jane GaspayPas encore d'évaluation
- Wax Depilation ManualDocument17 pagesWax Depilation ManualAmit Sharma100% (1)
- Articulo de Las 3 Tesis Por BrowDocument30 pagesArticulo de Las 3 Tesis Por BrowJHIMI DEIVIS QUISPE ROQUEPas encore d'évaluation
- Lecture 2 Types of Fluid FlowDocument29 pagesLecture 2 Types of Fluid FlowMilkias endashawPas encore d'évaluation
- Profile of RespondentsDocument36 pagesProfile of RespondentsPratibha SharmaPas encore d'évaluation
- ICT ContactCenterServices 9 Q1 LAS3 FINALDocument10 pagesICT ContactCenterServices 9 Q1 LAS3 FINALRomnia Grace DivinagraciaPas encore d'évaluation
- Exercise 6Document2 pagesExercise 6Satyajeet PawarPas encore d'évaluation
- AudiometerDocument3 pagesAudiometerVasanth VasanthPas encore d'évaluation
- Case Analysis of Vishal Jeet V. Union of India Trafficking of Women and ChildrenDocument7 pagesCase Analysis of Vishal Jeet V. Union of India Trafficking of Women and ChildrenTrishani NahaPas encore d'évaluation
- Lenovo TAB 2 A8-50: Hardware Maintenance ManualDocument69 pagesLenovo TAB 2 A8-50: Hardware Maintenance ManualGeorge KakoutPas encore d'évaluation
- ProjectxDocument8 pagesProjectxAvinash KumarPas encore d'évaluation
- Human Evolution SE Skull Analysis GizmoDocument9 pagesHuman Evolution SE Skull Analysis GizmoTamia WashingtonPas encore d'évaluation
- Clipsal RCD Tester 486D PDFDocument4 pagesClipsal RCD Tester 486D PDF322399mk7086Pas encore d'évaluation
- Msla Business FeesDocument1 pageMsla Business FeesNBC MontanaPas encore d'évaluation
- COLLOIDAL GOLD RECIPE - CitrateDocument9 pagesCOLLOIDAL GOLD RECIPE - CitrateDevon Narok100% (4)
- All Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationDocument7 pagesAll Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationRakesh KumarPas encore d'évaluation
- MCQSDocument25 pagesMCQSAsifa Liaqat0% (1)
- Learners ' Health and Safety Practices and Their Academic PerformanceDocument10 pagesLearners ' Health and Safety Practices and Their Academic PerformanceHira SaddozaiPas encore d'évaluation
- Peseshet - The First Female Physician - (International Journal of Gynecology & Obstetrics, Vol. 32, Issue 3) (1990)Document1 pagePeseshet - The First Female Physician - (International Journal of Gynecology & Obstetrics, Vol. 32, Issue 3) (1990)Kelly DIOGOPas encore d'évaluation
- Difference Between Gram Positive and GramDocument3 pagesDifference Between Gram Positive and Grambaraa aburassPas encore d'évaluation
- CITEC Genesis & GenXDocument45 pagesCITEC Genesis & GenXPutra LangitPas encore d'évaluation
- Boge FLEX PET SystemsDocument4 pagesBoge FLEX PET SystemsAir Repair, LLCPas encore d'évaluation
- B028-Sayli Kapse B029-Surya Teja B030-Taranum Kaur B032-Yashesh Kothari B034-Sathish Kumar B035-ManeeshDocument24 pagesB028-Sayli Kapse B029-Surya Teja B030-Taranum Kaur B032-Yashesh Kothari B034-Sathish Kumar B035-ManeeshTaranum RandhawaPas encore d'évaluation
- Education - Khóa học IELTS 0đ Unit 3 - IELTS FighterDocument19 pagesEducation - Khóa học IELTS 0đ Unit 3 - IELTS FighterAnna TaoPas encore d'évaluation
- User'S Guide: 5. SpecificationsDocument8 pagesUser'S Guide: 5. SpecificationsNguyễn Xuân VĩPas encore d'évaluation
- 621F 721F Op's ManualDocument362 pages621F 721F Op's ManualMilAuto87100% (1)
- QUIZ7 Audit of LiabilitiesDocument3 pagesQUIZ7 Audit of LiabilitiesCarmela GulapaPas encore d'évaluation
- (PDF) Books Toxic Parents Epub Popular Download - by Susan ForwardDocument1 page(PDF) Books Toxic Parents Epub Popular Download - by Susan Forwardmartagonzalezbordonaba0% (3)