Académique Documents
Professionnel Documents
Culture Documents
Pathophysiology and Pathogenesis of Type 2 Diabetes
Transféré par
Gladys SorianoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pathophysiology and Pathogenesis of Type 2 Diabetes
Transféré par
Gladys SorianoDroits d'auteur :
Formats disponibles
Type 2 Diabetes
About 90% of diabetic Americans have type 2 diabetes. The prevalence of type 2 diabetes is higher in African Americans, Native Americans, Hispanics, and Pacific Islanders than it is in Caucasians. Most type 2 diabetes patients are overweight, and most are diagnosed as adults. The genetic influence in type 2 diabetes is greater than that seen with type 1. While concordance rates between monozygous twins for type 1 diabetes are about 30 to 50%, the rate is approximately 90% for type 2 diabetes. Although the genetic predisposition to type 2 diabetes is strong, no single genetic defect has been found. In addition to genetic influences, acquired risk factors for type 2 diabetes include obesity, advancing age, and an inactive lifestyle. The underlying pathophysiologic defect in type 2 diabetes does not involve autoimmune beta-cell destruction. Rather, type 2 diabetes is characterized by the following three disorders: (1) peripheral resistance to insulin, especially in muscle cells; (2) increased production of glucose by the liver; and, (3) altered pancreatic insulin secretion. Increased tissue resistance to insulin generally occurs first and is eventually followed by impaired insulin secretion. The pancreas produces insulin, yet insulin resistance prevents its proper use at the cellular level. Glucose cannot enter target cells and accumulates in the bloodstream, resulting in hyperglycemia. The high blood glucose levels often stimulate an increase in insulin production by the pancreas; thus, type 2 diabetic individuals often have excessive insulin production (hyperinsulinemia). Over the years, pancreatic insulin production usually decreases to below normal levels. In addition to hyperglycemia, type 2 diabetic patients often have a group of disorders that has been called "insulin resistance syndrome" or syndrome X. Obesity contributes greatly to insulin resistance, even in the absence of diabetes. In fact, weight loss is a cornerstone of therapy for obese type 2 diabetic patients. Insulin resistance generally decreases with weight loss. Obesity also may explain the dramatic increase in the incidence of type 2 diabetes among young individuals in the United States in the past 10 to 20 years. Once considered a disease of adults, type 2 diabetes has increased among America's youth in direct correlation with the increase in the average weight of children and young adults during that time period. Type 2 diabetes usually has a slow onset and may remain undiagnosed for years. Approximately half of those who have type 2 diabetes are unaware of their disease. Unfortunately, the insidious nature of the disease allows prolonged periods of hyperglycemia to begin exerting negative effects on major organ systems. By the time many type 2 diabetic patients are diagnosed, diabetic complications have already begun. Type 2 diabetic patients do not require exogenous insulin for survival since they still produce insulin. However, insulin injection is often an integral part of medical management for type 2 diabetes. Unlike type 1 diabetic patients, individuals with type 2 diabetes are generally resistant to DKA because their pancreatic insulin production is often sufficient to prevent ketone formation. Severe physiologic stress may induce DKA in those with type 2 diabetes. Long periods of severe hyperglycemia may result in hyperosmolar nonketotic acidosis. Hyperglycemia results in the urinary excretion of large amounts of glucose, with attendant water loss. If fluids are not replaced, the dehydration can result in electrolyte imbalance and acidosis.
Pathophysiology and Pathogenesis of Type 2 Diabetes
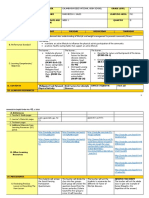
Type 2 diabetes is the most common form of diabetes, with more than 90% of diabetics being Type 2, and 5%-10% being Type 1. Type 2 diabetes mellitus is a heterogeneous disorder with varying prevalence among different ethnic groups. In the United States the populations most affected are Native Americans, particularly in the desert Southwest, Hispanic-Americans, African-Americans, and AsianAmericans. However, Caucasian-Americans are also affected, but not at the same disproportionate percentage levels. The pathophysiology of Type 2 diabetes mellitus is characterized by peripheral insulin resistance (insulin insensitivity), cell damage, impaired
regulation of hepatic glucose production, and later on: declining beta () cell function, eventually leading to possible -cell failure. The primary events are believed to be an initial insensitivity of insulin resulting in peripheral insulin resistance; and, later on, relative insulin deficiency. The key message here is that the key cellular dysfunction that occurs in Type 2 diabetes is notdue to the cells (as in Type 1 diabetes) -- it's the muscle, liver, and fat cells, and also the damage to the red blood cells (due to glycation)! Author's Note: During my medical workshops with doctors, nurses, and other healthcare professionals, they were shocked to discover that cell dysfunction is NOT the primary issue with Type 2 diabetics -especially when I show them the data from thousands of Type 2 diabetics. In fact, I was one of those Type 2 diabetics who was put on a drug protocol of 4 insulin shots a day because the doctors believed I was either a Type 1 diabetic, or a Type 2 diabetic with cell dysfunction. But, because of my biochemistry background I knew enough to ask for specific blood/urine/hormone tests that verified that I wasn't Type 1 and didn't have beta cell dysfunction, i.e. insulin serum test, cpeptide, urine ketone test, hemoglobin A1C, glutamic acid decarboxylase (GAD) antibody tests, islet cell antibody (ICA) tests, insulin antibody tests, GTT. Unfortunately, most Type 2 diabetics don't know this, and are led to take diabetic drugs that don't really help in the long run. If I had not recognized this discrepancy I would still be diabetic today and I would be taking even more insulin. Overview: Diabetes at the Cellular Level The key cells that are affected when Type 2 diabetes initially develops (due to hyperinsulinemia) include the glycated red blood cells, and the muscle, fat, andliver cells, which are designed to take glucose (sugar) out of the blood, pull it into the cells and change it into energy. These cells require insulin to absorb glucose. When these cells fail to respond adequately to circulating insulin, these cells lose their sensitivity to insulin (a condition known as insulin resistance) and blood glucose levels rise. The body responds to this situation by signaling the pancreas to produce more insulin, causing insulin levels in the blood to become too high. This condition is known as hyperinsulinemia. The cells in the liver also become insulin resistant and respond by making too much blood sugar. Because blood sugar is not absorbed by the cells, it stays in the blood, causing blood sugar levels to rise a condition known as hyperglycemia. Red blood cells are damaged due to the high glucose levels, as sugar molecules are appended to the exterior part of the red blood cells, forming a crystalline (coarse) crust -- this is known as glycation (which creates AGEs). These coarse red blood cells cause damage throughout the circulatory system, damaging arteries and capillaries. This damage is repaired by the cholesterol produced by the liver, leading to arterial plaque formation -- all triggered by an inflammatory response. These coarse red blood cells cause greater damage in dense capillary areas such as the hands and feet, and fragile capillaries such as those that feed the kidneys and eyes. All of this leads to diabetic complications that can lead to blindness, kidney failure, amputation, heart attack and stroke. Other health issues include high blood pressure, high cholesterol, high inflammation markers, periodontal disease, and erectile dysfunction. Key Point!: Given the cellular dysfunction of the muscle cells, fat cells, and the liver cells, once can see that diabetic drugs are not going to help defeat or reverse your diabetes! Why? Because the majority of diabetic drugs are designed either to make the pancreas secrete more insulin or prevent the liver from releasing stored glycogen. The drugs do nothing to address the insulin resistance of the muscle and fat cells, or the inflammatory damage caused by the coarse (glycated) red blood cells. You don't have to be a scientist to figure out that you need to reduce the insulin resistance (by increasing the insulin sensitivity of the cells) and reduce the cellular inflammation -- by reducing blood
glucose
levels
and
insulin
levels.
Insulin Resistance The presence of hyperinsulinism in type 2 diabetes, insulin resistance has been considered to play an integral role in the pathogenesis of the disease. As chronic hyperinsulinemia inhibits both insulin secretion and action, and hyperglycemia can impair both the insulin secretory response to glucose as well as cellular insulin sensitivity, the precise relation between glucose and insulin level as a surrogate measure of insulin resistance has been questioned. Lean type 2 diabetic patients over 65 years of age have been found to be as insulin sensitive as their age-matched non-diabetic controls. Moreover, in the majority of type 2 diabetic patients who are insulin resistant, obesity is almost invariably present. As obesity or an increase in intra-abdominal adiposetissue is associated with insulin resistance in the absence of diabetes, it is believed by some that insulin resistance in type 2 diabetes is entirely due to the coexistence of increased adiposity. Additionally, insulin resistance is found in hypertension, hyperlipidemia, and ischemic heart disease, entities commonly found in association with diabetes, again raising the question as to whether insulin resistance results from different pathogenetic disease processes or is unique to the presence of type 2 diabetes. Prospective studies have demonstrated the presence of either insulin deficiency or insulin resistance before the onset of type 2 diabetes. Two studies have reported the presence of insulin resistance in non-diabetic relatives of diabetic patients at a time when their glucose tolerance was still normal. In addition, first degree relatives of patients with type 2 diabetes have been found to have impaired insulin action upon skeletal muscle glycogen synthesis due to both decreased stimulation of tyrosine kinase activity of the insulin receptor and reduced glycogen synthase activity. Other studies in this high risk group have failed to demonstrate insulin resistance, and in the same group, impaired early phase insulin release and loss of normal oscillatory pattern of insulin release have been described. Based upon these divergent studies, it is still impossible to dissociate insulin resistance from insulin deficiency in the pathogenesis of type 2 diabetes. However,both entities unequivocally contribute to the fully established disease. Cortisol Insulin resistance creates high levels of insulin which then signal the release of cortisol (from the adrenal glands). Cortisol is responsible for releasing fatty acids into the blood stream. These fatty acids are very high energy fats or lipids. These systematic responses are normal in situations of high stress, such as running from a bear in the woods or fighting a tiger. What would naturally follow is the lowering of these hormones back down to a stable state. But, because we are leading stressful lives through worries and fears with very little physical activity and very poor eating habits, this leads to sustained high levels of cortisol, blood sugar and insulin. Excessive levels of cortisol leads to excessive levels of fatty acids in our blood stream. Oxidation of fatty acids is a natural part of the bodies immune response, but when we have excessive amounts, we cause an over reaction of our immune response, and attack our own tissues. This causes an inflammatory state in our bodies. These excessive fatty acids oxidize and lead to a build up of fatty tissue. This build up leads to plaque and fatty streaks as well as calcification. This is whycardiovascular disease and hardening of the
arteries is a major result of this metabolic syndrome. Consequently, when the cell isnt converting blood sugar for energy, its converted to fat for storage. Fat cells are responsible for hormone synthesis and storage of toxins. Our environment is full of toxins from chemicals, detergents, pollution, drugs, food additives, pesticides, etc. When our fat cells get too big, they leak these toxins back into the blood stream. These toxins also inhibit the insulin function of the cells and stimulate inflammation. Belly fat is also a predictor of insulin resistance. Belly fat, also known as visceral fat, has the highest amount of cortisol receptors. Visceral fat is found around the organs. This fat is a power house for immune function. This high immune type of tissue is critical for keeping viruses, bacteria and other foreign bodies out of our vital organs. High levels of cortisol from insulin resistance creates a high level of fatty acid release around these organs. Subsequently, more oxidation occurs and this causes a large immune response, sending out white blood cells to destroy the invaders. This causes the body to be in a constant state of inflammation which can lead to the attack of all types of tissues in the body. The Liver The ability of insulin to suppress hepatic glucose production both in the fasting state and postprandially is normal in first degree relatives of type 2 diabetic patients . It is the increase in the rate of postprandial glucose production that heralds the evolution of IGT. Eventually, both fasting and postprandial glucose production increase as type 2 diabetes progresses. Hepatic insulin resistance is characterized by a marked decrease in glucokinase activity and a catalytic increased conversion of substrates to glucose despite the presence of insulin. Thus, the liver in type 2 diabetes is programmed to both overproduce and under-use glucose. The elevated free fatty acid levels found in type 2 diabetes may also play a role in increased hepatic glucose production. In addition, recent evidence suggests an important role for the kidney in glucose production via gluconeogenesis, which is unrestrained in the presence of type 2 diabetes. Inflammation Blood sugar control is important because the body is normally destroyed by increased levels of sugar in the blood which results in inflammation. The following text explains why inflammation is caused by increased levels of sugar in the body. An increase in levels of sugar in the blood results in the creation of a bond between the sugar and the red blood cells. Normally this sugar appends itself to the hemoglobin molecule contained in the red blood cells. The amount of sugar appended to the hemoglobin molecule decreases if the levels of sugar in your blood are controlled; otherwise the amount of sugar appended to the hemoglobin molecule increases [Ref: Hemoglobin A1C test]. Sugar appended to the exterior part of the red blood can be compared to the way sand attaches itself to a moist object. A crystalline crust which is very coarse is created. Try to envision that there are millions of very coarse red blood cells in your body and the harm that would happen to your circulatory system. Arteries that are destroyed are sealed off by cholesterol and this can result in strokes and heart attacks in people suffering from Type 2 diabetes. Fragile capillary beds can also be damaged by these coarse red blood cells. Capillaries are the minute blood vessels in our bodies. that feed our kidneys, eyes, and feet Patients with poor blood sugar control can experience greater damage in dense capillary areas such as the hands and feet. Poor flow of blood caused by damaged capillary beds can result in infections and more serious problems such as amputations in people with Type 2 diabetes. These coarse red blood cells can also cause damage to the delicate capillaries that feed the retina and the kidneys. This damage can lead to cataracts, blindness, and kidney failure (kidney dialysis). If you imagine what your body will go through due to the inflammation and damage caused by these coarse red blood cells, you will be able to understand why diabetic patients experience so many terminal problems.
Good blood sugar control is very important since our bodies cannot stand that kind of mistreatment for a long time without severe consequences.Unfortunately, during a recent survey, more than 80% of diabetics did not believe that they will face blindness, amputation, heart attack, stroke, or kidney failure! The primary reasons for this is due to the denial by the patient and a lack of understanding of the science of diabetes by the patient and some doctors. Advanced Glycation End Products (AGEs) Hyperglycemia is still considered the principal cause of diabetes complications. Its deleterious effects are attributable, among other things, to the formation of sugar-derived substances called advanced glycation end products (AGEs). AGEs form at a constant but slow rate in the normal body, starting in early embryonic development, and accumulate with time. However, their formation is markedly accelerated in diabetes because of the increased availability of glucose. AGEs are a heterogeneous group of molecules formed from the nonenzymatic reaction of reducing sugars with free amino groups of proteins, lipids, and nucleic acids. The initial product of this reaction is called a Schiff base, which spontaneously rearranges itself into an Amadori product, as is the case of the well-known hemoglobin A1c (A1C). These initial reactions are reversible depending on the concentration of the reactants. A lowered glucose concentration will unhook the sugars from the amino groups to which they are attached; conversely, high glucose concentrations will have the opposite effect, if persistent. A key characteristic of certain reactive or precursor AGEs is their ability for covalent crosslink formation between proteins, which alters their structure and function, as in cellular matrix, basement membranes, and vessel-wall components. Other major features of AGEs relate to their interaction with a variety of cell-surface AGE-binding receptors, leading either to their endocytosis and degradation or to cellular activation and pro-oxidant, pro-inflammatory events. A large body of evidence suggests that AGEs are important pathogenetic mediators of almost all diabetes complications, conventionally grouped into micro- or macroangiopathies. For instance, AGEs are found in retinal vessels of diabetic patients, and their levels correlate with those in serum as well as with severity of retinopathy. Aminoguanidine, an inhibitor of AGE formation, is shown to prevent retinopathy in diabetic animals. Also, it is known that AGEs accumulate in peripheral nerves of diabetic patients and that the use of anti-AGE agents improves nerve conduction velocities and neuronal blood flow abnormalities. The characteristic structural changes of diabetic nephropathy, thickened glomerular basement membrane and mesangial expansion, are accompanied by accumulation of AGEs, leading to glomerulosclerosis and interstitial fibrosis. Prolonged infusion of nondiabetic rats with AGEs has led to the development of similar morphological changes and significant proteinuria. Here again, AGE inhibitors such as aminoguanidine prevented diabetic nephropathy in diabetic animal models and were recently shown to do the same in one clinical trial on diabetic patients. Atherosclerosis is significantly accelerated in diabetic patients and is associated with greater risk of cardiovascular and cerebrovascular mortality. Animal and human studies have shown that AGEs play a significant role in the formation and progression of atherosclerotic lesions. Increased AGE accumulation in the diabetic vascular tissues has been associated with changes in endothelial cell, macrophage, and smooth muscle cell function. In addition, AGEs can modify LDL cholesterol in such a way that it tends to become easily oxidized and deposited within vessel walls, causing streak formation and, in time, atheroma. AGE-crosslink formation results in arterial stiffening with loss of elasticity of large vessels. This arterial stiffness has recently been shown to be reversed by the administration of another anti-AGE class of compounds called AGE-breakers. In addition to those endogenously formed, AGEs can also be introduced in the body from exogenous sources. Tobacco smoke, for example, is a well-known exogenous source of AGEs. The combustion of
various pre-AGEs in tobacco during smoking gives rise to reactive and toxic AGEs. Serum AGEs or LDL-linked AGEs are significantly elevated in cigarette smokers. Diabetic smokers, as a result, are reported to exhibit greater AGE deposition in their arteries and ocular lenses. More importantly, recent studies have provided evidence that diet is a significant exogenous source of highly reactive AGEs. Food processing, heating in particular, has a significant accelerating effect in the generation of glyco- and lipoxidation products. Heat helps create tasteful flavors that humans have learned to enjoy. In recent decades, food manufacturers have been using this knowledge to boost the flavor of natural foods by incorporating synthetic AGEs into foods. Consequently, the AGEs content of the Western diet has increased vastly in the past 50 years, as has the quantity of food consumed. A significant proportion (10%) of ingested AGEs is absorbed with food. There is apparently a direct correlation between circulating AGE levels and those consumed. Studies in animals have demonstrated an important relationship between high dietary AGE intake and development or progression of diabetes-related tissue damage, e.g., vascular and renal. In all instances, this was prevented by dietary AGE restriction. A similarly significant contribution to the human body AGE pool by diet was demonstrated recently. More importantly, its effective reduction by a restriction of dietary AGEs was associated with a significant suppression of circulating levels of vascular disease markers (e.g., adhesion molecules) as well as of inflammatory mediators. This new evidence suggests that modulation of food-AGE content could become an important ingredient of the therapeutic armamentarium in the management of diabetic patients. Until effective and safe drugs become available, physicians and dietitians can, for instance, advise increased reliance on fresh foods, cooked by brief applications of heat, in the presence of ample water or humidity. A diet designed to be low in AGEs is apparently not lacking in taste, while not requiring compromises in important nutrients. Such a regimen can decrease AGE intake by more than 50%; this in turn was shown to reduce circulating AGEs by 30% within a month without a change in A1C. On the contrary, short-term euglycemia or temporary normalization of A1C are not sufficient means for reducing serum AGEs; instead this requires extended periods of time, e.g., months or years. In conclusion, current evidence points to glucose not only as the bodys main short-term energy source, but also as the long-term fuel of diabetes complications, mainly in the form of oxidative, proinflammatory AGEs. Food commonly consumed after exposure to heat contains a significant amount of pre-formed AGEs, a fact that offers a new perspective on food as a major environmental risk factor. It may be necessary, for instance, to restructure our guidelines to include methods of food preparation along with or in addition to routine recommendations about food quantity and composition. It is reasonable to consider that good glycemic control, in combination with a careful diet in terms of reduced AGE consumption, should be among the new goals for optimal management of diabetic patients. Addressing dietary habits from a new perspective, while difficult, could achieve the best long-term effects as novel drug interventions become available for clinical use in the future. The -cell Dysfunction After many years of the pancreas secreting high levels of insulin to keep up with the high levels of blood glucose, the pancreas begins to wear out, leading to -Cell dysfunction. This dysfunction is initially characterized by an impairment in the first phase of insulin secretion during glucose stimulation and may precede the onset of glucose intolerance in type 2 diabetes. Initiation of the insulin response depends upon the transmembranous transport of glucose and coupling of glucose to the glucose sensor. The glucose/glucose sensor complex then induces an increase in glucokinase by stabilizing the protein and impairing its degradation. The induction of glucokinase serves as the first step in linking intermediary metabolism with the insulin secretory apparatus. Glucose transport in -cells of type 2 diabetes patients appears to be greatly reduced, thus
shifting the control point for insulin secretion from glucokinase to the glucose transport system. Later in the course of the disease, the second phase release of newly synthesized insulin is impaired, an effect that can be reversed, in part at least in some patients, by restoring strict control of glycemia. This secondary phenomenon, termed desensitization or -cell glucotoxicity, is the result of a paradoxical inhibitory effect of glucose upon insulin release and may be attributable to the accumulation of glycogen within the -cell as a result of sustained hyperglycemia. Other candidates that have been proposed are sorbitol accumulation in the -cell or the non-enzymatic glycation of cell proteins. Other defects in -cell function in type 2 diabetes mellitus include defective glucose potentiation in response to non-glucose insulin secretagogues, asynchronous insulin release, and a decreased conversion of proinsulin to insulin. An impairment in first phase insulin secretion may serve as a marker of risk for type 2 diabetes mellitus in family members of individuals with type 2 diabetes mellitus and may be seen in patients with prior gestational diabetes. However, impaired first phase insulin secretion alone will not cause impaired glucose tolerance. Autoimmune destruction of pancreatic -cells may be a factor in a small subset of type 2 diabetic patients and has been termed the syndrome of latent autoimmune diabetes in adults.This group may represent as many as 10% of Scandinavian patients with type 2 diabetes and has been identified in the recent United Kingdom study, but has not been well characterized in other populations. Glucokinase is absent within the -cell in some families with maturity-onset diabetes of young . However, deficiencies of glucokinase have not been found in other forms of type 2diabetes. In summary, the delay in the first phase of insulin secretion, although of some diagnostic import, does not appear to act independently in the pathogenesis of type 2 diabetes. In some early-onset patients with type 2 diabetes (perhaps as many as 10%), there may be a deficiency in insulin secretion that may or may not be due to autoimmune destruction of the -cell and is not due to a deficiency in the glucokinase gene. In the great majority of patients with type 2 diabetes (90%), the delay in immediate insulin response is accompanied by a secondary hypersecretory phase of insulin release as a result of a compensatory response to peripheral insulin resistance. Over a prolonged period of time, perhaps years, insulin secretion gradually declines, possibly as a result of intra-islet accumulation of glucose intermediary metabolites. In view of the decline in -cell mass, sulfonylureas and other diabetic drugs appear to serve a diminishing role in the long term management of type 2 diabetes. Unanswered is whether amelioration of insulin resistance with earlier detection or newer insulin-sensitizing drugs will retard the progression of -cell failure, obviating or delaying the need for insulin therapy. Mitochondria Dysfunction Given their essential function in aerobic metabolism, mitochondria are intuitively of interest in regard to the pathophysiology of diabetes. Qualitative, quantitative, and functional perturbations in mitochondria have been identified and affect the cause and complications of diabetes. Moreover, as a consequence of fuel oxidation, mitochondria generate considerable reactive oxygen species (ROS). Evidence is accumulating that these radicals per se are important in the pathophysiology of diabetes and its complications. Insulin resistance in skeletal muscle is a major hallmark of type 2 diabetes mellitus (T2D) and obesity that is characterized by impaired insulin-mediated glucose transport and glycogen synthesis and by increased intramyocellular content of lipid metabolites. Several studies have provided evidence for mitochondrial dysfunction in skeletal muscle of type 2 diabetic and pre-diabetic subjects, primarily due to a lower content of mitochondria (mitochondrial biogenesis) and possibly to a reduced functional capacity per mitochondrion -- but, more research and studies need to be performed.
http://nurseslabs.com/diabetes-mellitus-type-2-pathophysiology-schematic-diagram/
Read more:Diabetes Pathophysiologyhttp://www.health.am/db/diabetes-pathophysiology/#ixzz0KGAFz7bj
Vous aimerez peut-être aussi
- How EXERCISE Helps Control DiabetesDocument23 pagesHow EXERCISE Helps Control DiabetesApurba MukherjeePas encore d'évaluation
- What is diabetes? Types, symptoms and complicationsDocument11 pagesWhat is diabetes? Types, symptoms and complicationsTonee Marie Gabriel100% (1)
- 222 Diabetes FinalDocument61 pages222 Diabetes Finalrajatsgr100% (1)
- Diabetes Facts: Types, Causes and Symptoms ExplainedDocument13 pagesDiabetes Facts: Types, Causes and Symptoms ExplainedShelly_Ann_Del_9959Pas encore d'évaluation
- Type 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]D'EverandType 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]Évaluation : 5 sur 5 étoiles5/5 (7)
- What Is Diabete1Document134 pagesWhat Is Diabete1Icha AjaPas encore d'évaluation
- Diabetes Overview: Aerobic Exercise ClassDocument13 pagesDiabetes Overview: Aerobic Exercise Classpak3maPas encore d'évaluation
- DM Report1Document16 pagesDM Report1Wendy EscalantePas encore d'évaluation
- DM ThyroidDocument184 pagesDM ThyroidtentenPas encore d'évaluation
- Diabetes Mellitus 1Document16 pagesDiabetes Mellitus 1Ajet AsaniPas encore d'évaluation
- Jaya's BiochemistryDocument13 pagesJaya's BiochemistryJKKP HPJBPas encore d'évaluation
- Type 1 vs Type 2 Diabetes: Causes and TreatmentsDocument3 pagesType 1 vs Type 2 Diabetes: Causes and TreatmentsTvisha PatelPas encore d'évaluation
- Controlling Blood Glucose 2 (AutoRecovered)Document3 pagesControlling Blood Glucose 2 (AutoRecovered)Tvisha PatelPas encore d'évaluation
- Type 1 vs Type 2 Diabetes: Causes and TreatmentsDocument3 pagesType 1 vs Type 2 Diabetes: Causes and TreatmentsTvisha PatelPas encore d'évaluation
- Controlling Blood Glucose 2 (AutoRecovered)Document3 pagesControlling Blood Glucose 2 (AutoRecovered)Tvisha PatelPas encore d'évaluation
- Diabetes MellitusDocument13 pagesDiabetes Mellitusdreneavalentinstefan100% (1)
- Diabetes OverviewDocument38 pagesDiabetes OverviewKye GarciaPas encore d'évaluation
- Diabetes MellitusDocument8 pagesDiabetes MellitusJaja RamosPas encore d'évaluation
- Diabetes MellitusDocument8 pagesDiabetes MellitusJaja RamosPas encore d'évaluation
- Diabetes MellitusDocument8 pagesDiabetes MellitusJaja RamosPas encore d'évaluation
- Type 1 Diabetes Mellitus: PathoDocument6 pagesType 1 Diabetes Mellitus: PathoMary JoycePas encore d'évaluation
- Pathophysiology of Diabetes MellitusDocument2 pagesPathophysiology of Diabetes MellitusShelly_Ann_Del_9959Pas encore d'évaluation
- What Is Diabetes? What Causes Diabetes?Document8 pagesWhat Is Diabetes? What Causes Diabetes?Khaleda FatmawatiPas encore d'évaluation
- The Diabetes Code Cookbook: Delicious, Healthy, Low-Carb Recipes to Manage Your Insulin and Prevent and Reverse Type 2 DiabetesD'EverandThe Diabetes Code Cookbook: Delicious, Healthy, Low-Carb Recipes to Manage Your Insulin and Prevent and Reverse Type 2 DiabetesÉvaluation : 1 sur 5 étoiles1/5 (1)
- Introduction To DiabetesDocument9 pagesIntroduction To DiabetesSameer Saurabh100% (1)
- Pathophysiology ScribdDocument8 pagesPathophysiology ScribdTamil VillardoPas encore d'évaluation
- DM ReportDocument16 pagesDM ReportWendy EscalantePas encore d'évaluation
- Diabetus Mellitus, LeoDocument11 pagesDiabetus Mellitus, LeoinnyPas encore d'évaluation
- Bka Case FinalDocument26 pagesBka Case FinalJayson SorianoPas encore d'évaluation
- Diabetes MellitusDocument19 pagesDiabetes MellitusHaleelu Abdul JaleelPas encore d'évaluation
- Presentation On Diabetes Mellitus in Pharmacology LabDocument35 pagesPresentation On Diabetes Mellitus in Pharmacology Labpurwo yuhantoPas encore d'évaluation
- Ero Diabetes Type IIDocument4 pagesEro Diabetes Type IINocReyes100% (1)
- Illness Narrative Type 2 Diabetes - EditedDocument8 pagesIllness Narrative Type 2 Diabetes - EditedLando Amit FeisalPas encore d'évaluation
- Diabetes Mellitus, Disorder Of: Institute For BiotechnologyDocument10 pagesDiabetes Mellitus, Disorder Of: Institute For BiotechnologyAndre Jonathan Siàńsàkà IIPas encore d'évaluation
- Diabetes Perspectives and TreatmentsDocument32 pagesDiabetes Perspectives and TreatmentsyellahfellahPas encore d'évaluation
- Case Study - Diabetes Mellitus (Nutrition&Dietetics)Document10 pagesCase Study - Diabetes Mellitus (Nutrition&Dietetics)Summer Suarez100% (1)
- Pathophysiology of Diabetes Mellitus: Normal Pathology of The Human BodyDocument4 pagesPathophysiology of Diabetes Mellitus: Normal Pathology of The Human BodyMelodia Turqueza GandezaPas encore d'évaluation
- Antidiabetic Plants Reduce Blood SugarDocument77 pagesAntidiabetic Plants Reduce Blood SugarUrmi Joshi100% (2)
- Case Study On Diabetes MellitusDocument12 pagesCase Study On Diabetes Mellitusferdz02Pas encore d'évaluation
- Discover Natural -Alternative Therapies for Managing Type 2 DiabetesD'EverandDiscover Natural -Alternative Therapies for Managing Type 2 DiabetesPas encore d'évaluation
- Chapter-5_DMDocument8 pagesChapter-5_DMFitri YaniPas encore d'évaluation
- Types of Diabetes Mellitus ExplainedDocument5 pagesTypes of Diabetes Mellitus ExplainedKlinik MaleoPas encore d'évaluation
- DM Grand Case PresDocument24 pagesDM Grand Case PresBing Howell de GuzmanPas encore d'évaluation
- Diabetes Type 2 and How It ArisesDocument9 pagesDiabetes Type 2 and How It Arisesayankotlai099Pas encore d'évaluation
- Diabetes Mellitus Is A Group of Metabolic Diseases Characterized byDocument67 pagesDiabetes Mellitus Is A Group of Metabolic Diseases Characterized byBivek TimalsinaPas encore d'évaluation
- Correlation Between Diabetes and Coronary Artery DiseaseDocument18 pagesCorrelation Between Diabetes and Coronary Artery Diseaserahmat safryansyahPas encore d'évaluation
- Vol-2 DiabetesDocument50 pagesVol-2 DiabetesVishwanath SomaPas encore d'évaluation
- Diabetes: Causes, Symptoms and TreatmentsDocument4 pagesDiabetes: Causes, Symptoms and TreatmentsAbdullah BazryPas encore d'évaluation
- Diabeties NewDocument54 pagesDiabeties NewDipti SharmaPas encore d'évaluation
- Ultimate Diet Plan for Diabetic Patients: Revolutionizing Diabetic NutritionD'EverandUltimate Diet Plan for Diabetic Patients: Revolutionizing Diabetic NutritionPas encore d'évaluation
- Diabetes Truth 2Document11 pagesDiabetes Truth 2gibrambo5770Pas encore d'évaluation
- Diabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inDocument3 pagesDiabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inGanesh BalaPas encore d'évaluation
- IntroductionDocument22 pagesIntroductionjayrana40Pas encore d'évaluation
- Diabetes Report: Causes, Types & SymptomsDocument8 pagesDiabetes Report: Causes, Types & SymptomsKristina RoblesPas encore d'évaluation
- Diabetes Mellitus Case StudyDocument5 pagesDiabetes Mellitus Case StudyRainier Rhett Concha86% (7)
- Medical Information of The DiseaseDocument8 pagesMedical Information of The Diseasecharibel torresPas encore d'évaluation
- CasestudyDocument10 pagesCasestudyPunam Patel100% (2)
- Diabetes MellitusDocument21 pagesDiabetes MellitusJuri GallosPas encore d'évaluation
- DR Anuj Raj BijukchheDocument60 pagesDR Anuj Raj BijukchheMUHAMMAD JAWAD HASSANPas encore d'évaluation
- PSY 22 ABPSYCH 1st Exam REVIWERDocument14 pagesPSY 22 ABPSYCH 1st Exam REVIWERCresiel PontijonPas encore d'évaluation
- Atom Electrosurgical SystemDocument40 pagesAtom Electrosurgical SystemOgut AjaPas encore d'évaluation
- Academic Year: 2021/2022 Semester: Fall 2021Document27 pagesAcademic Year: 2021/2022 Semester: Fall 2021Marwa abbassPas encore d'évaluation
- GallstonesDocument17 pagesGallstonesع ب و دPas encore d'évaluation
- q2 Grade 9 Pe DLL Week 1Document11 pagesq2 Grade 9 Pe DLL Week 1Airaa A. Baylan88% (8)
- Living Life With Copd Booklet EngDocument32 pagesLiving Life With Copd Booklet EngPrplknitePas encore d'évaluation
- Cervical Cancer Literature ReviewDocument6 pagesCervical Cancer Literature Reviewaflskeqjr100% (1)
- IMCIDocument21 pagesIMCIAnonymous h2EnKyDbPas encore d'évaluation
- Brain Tumor Segmentation and Detection Using Nueral NetworksDocument9 pagesBrain Tumor Segmentation and Detection Using Nueral Networksjoshi manoharPas encore d'évaluation
- Aminoff's Neurology and General Medicine 6th Ed - Chapter 60. Neuromuscular Complications of General MedDocument28 pagesAminoff's Neurology and General Medicine 6th Ed - Chapter 60. Neuromuscular Complications of General MedYenny MaharaniPas encore d'évaluation
- History Taking and Physical ExaminationDocument53 pagesHistory Taking and Physical ExaminationBoruuf If GammachuuPas encore d'évaluation
- Automated Peritoneal Dialysis: Clinical Prescription and TechnologyDocument8 pagesAutomated Peritoneal Dialysis: Clinical Prescription and Technologyamalia puspita dewiPas encore d'évaluation
- Otc DrugsDocument71 pagesOtc DrugsEthan Morgan100% (2)
- Cutaneous Leishmania: Dr. Vijayakumar Unki Asst Professor VCGDocument16 pagesCutaneous Leishmania: Dr. Vijayakumar Unki Asst Professor VCGLohith MCPas encore d'évaluation
- GHC Gut Health Course Syllabus - MKTGDocument23 pagesGHC Gut Health Course Syllabus - MKTGKat HerreraPas encore d'évaluation
- The Real Anthony Fauci PDFDocument14 pagesThe Real Anthony Fauci PDFRocco Lampone100% (1)
- MiscellaneousDocument487 pagesMiscellaneoussalah subbahPas encore d'évaluation
- Neonatal Exchange TransfusionDocument33 pagesNeonatal Exchange TransfusionedrinsnePas encore d'évaluation
- Pulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Document9 pagesPulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Akash AkashPas encore d'évaluation
- RespiratoryDocument18 pagesRespiratoryReneé Camille50% (2)
- Total Abdominal Hysterectomy Bilateral Salpingo OophorectomyDocument3 pagesTotal Abdominal Hysterectomy Bilateral Salpingo OophorectomyLouise BravoPas encore d'évaluation
- Cushing's Disease PathophysiologyDocument3 pagesCushing's Disease PathophysiologyAj MacotoPas encore d'évaluation
- 50 Studies Every Anesthesiologist Shoud Know 2019Document305 pages50 Studies Every Anesthesiologist Shoud Know 2019pcut100% (2)
- Management of Anembryonic Pregnancy Loss: An Observational StudyDocument6 pagesManagement of Anembryonic Pregnancy Loss: An Observational StudyAnonymous ORleRrPas encore d'évaluation
- Immunization Case-Based Register: DHIS2 Tracker Data Model in PracticeDocument11 pagesImmunization Case-Based Register: DHIS2 Tracker Data Model in PracticeGerald ThomasPas encore d'évaluation
- Mata Merah Visus TurunDocument27 pagesMata Merah Visus TurunErinPas encore d'évaluation
- Peran Ipp - Bu CostyDocument13 pagesPeran Ipp - Bu Costysahrun runtiPas encore d'évaluation
- ScccvyDocument7 pagesScccvyDavy JonesPas encore d'évaluation
- QUIZDocument14 pagesQUIZhahaha0% (1)




![Type 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]](https://imgv2-1-f.scribdassets.com/img/word_document/616633879/149x198/173640cf06/1710278044?v=1)