Académique Documents
Professionnel Documents
Culture Documents
Patho
Transféré par
EmWongDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Patho
Transféré par
EmWongDroits d'auteur :
Formats disponibles
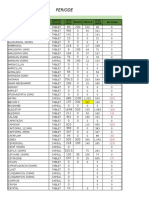
PATHOPHYSIOLOGY A.
Ideal Group A Hemolytic Streptococcal Infection
Cross reacting antibody formation
Binding to connective and heart tissue
Inflammation damage
Involvement of joints/ skin/ nervous system
Cardiac involvement
Endocarditis
Myocarditis
Faulty mitral and aortic semilunar valve function
Aschoff bodies
Pulmonary and Right heart involvement
Myocardial dysfunction
Chronic heart failure
Acute rheumatic fever can develop only as a sequel to pharyngeal infection by group A -hemolytic streptococcus. Streptococcal skin infections do not progress to acute rheumatic fever, although both skin and pharyngeal infections can cause acute glomerulonephritis. This is because the strains of the microorganism that affect the skin do not have the same antigenic molecules in their cell membranes as those that cause pharyngitis and, therefore, do not elicit the same kind of immune response. Acute rheumatic fever affects the heart, joints, central nervous system, and skin through an abnormal humoral and cellmediated immune response to group A streptococcal cell membrane antigens called M proteins. These antigens can bind to receptors on heart, muscle, and brain cells and have an affinity for membrane receptors within synovial joints, where they trigger an autoimmune response. Diffuse, proliferative, and exudative inflammatory lesions develop in the connective tissues, especially in the heart, joints and skin. The inflammation may subside before the treatment leaving behind damage to the heart, valves and increasing the individuals susceptibility to recurrent acute rheumatic fever after any subsequent streptococcal infections. Repeated attacks of acute rheumatic fever cause chronic proliferative changes in the previously mentioned organs as a result of scarring, granulomas, and thromboses. Approximately 10% of individuals with rheumatic fever develop rheumatic heart disease. It begins as carditis, or inflammation of the heart, called rheumatic heart disease. Rheumatic heart disease (RHD) continues to be a common health problem in the developing world, causing morbidity and mortality among both
children and adults. Even mild cases of rheumatic fever can cause carditis in all three layers of the heart wall. The primary lesion usually involves the endocardium, which lines the heart chambers and includes the heart valves. Endocardial inflammation causes of swelling of the valve leaflets, with secondary erosion along the lines of leaflet contact. Small, beadlike clumps of vegetation containing platelets and fibrin are deposited on eroded valvular tissue and on the chordate tendineae cordis. These lesions can become progressively adherent. Scarring and shortening of the involved structures occur over time. The valves lose their elasticity, and the leaflets may adhere to each other. If inflammation penetrates the myocardium, localized fibrin deposits develop that are surrounded by areas of necrosis. These fibrinoid necrotic deposits are called Aschoff bodies. Pericardial inflammation is usually characterized by serofibrinous effusion within the pericardial cavity.
Cardiomegaly and left heart failure may occur during episodes of untreated acute or recurrent rheumatic fever. Conduction defects and atrial fibrillation often are associated with rheumatic heart disease.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Biodata Format FinalDocument5 pagesBiodata Format FinalCharles Saurus PacomaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Mosh RoomDocument21 pagesMosh RoomBrandon DishmanPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- 9401-Article Text-17650-1-10-20200718Document5 pages9401-Article Text-17650-1-10-20200718agail balanagPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Insomnia: Management of Underlying ProblemsDocument6 pagesInsomnia: Management of Underlying Problems7OrangesPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- TinnitusDocument34 pagesTinnitusHnia UsmanPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Wa0094.Document9 pagesWa0094.lider vigilanciaPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- h2s Hand BookDocument34 pagesh2s Hand BookJorge Eliecer Ferro Cotes100% (4)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Klübersynth UH1 14-151: Safety Data SheetDocument16 pagesKlübersynth UH1 14-151: Safety Data SheetLiliana BeruPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- CLC - Good Copy Capstone ProposalDocument6 pagesCLC - Good Copy Capstone Proposalapi-549337583Pas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- PIIS0261561422000668 Micronitrientes: RequerimientosDocument70 pagesPIIS0261561422000668 Micronitrientes: Requerimientossulemi castañonPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Regulatory Compliance Planning GuideDocument70 pagesRegulatory Compliance Planning GuideriestgPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Shivashaki Organic Menure and TransportDocument3 pagesShivashaki Organic Menure and TransportShivashakthi MaheshPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Satvik DietDocument3 pagesSatvik DietDisha TPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Botswana Ref Ranges PaperDocument7 pagesBotswana Ref Ranges PaperMunyaradzi MangwendezaPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Urosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFDocument11 pagesUrosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFOLga A. Thigpen100% (4)
- AL Bio 2008 Marking SchemeDocument31 pagesAL Bio 2008 Marking Schemes200410400% (4)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 1.3.1 The Autopsy-1Document4 pages1.3.1 The Autopsy-1Alyssa robertsPas encore d'évaluation
- Boracay Rehabilitation: A Case StudyDocument9 pagesBoracay Rehabilitation: A Case StudyHib Atty TalaPas encore d'évaluation
- CSEC Biology June 2012 P2Document17 pagesCSEC Biology June 2012 P2Joy BoehmerPas encore d'évaluation
- Office: The of The SecretaryDocument20 pagesOffice: The of The SecretaryJustine KimPas encore d'évaluation
- 7 Contoh Analytical Exposition Pendek Bahasa InggrisDocument6 pages7 Contoh Analytical Exposition Pendek Bahasa InggrisDarsi YujiwatiPas encore d'évaluation
- Ozone As A Disinfecting Agent in The Reuse of WastewaterDocument9 pagesOzone As A Disinfecting Agent in The Reuse of WastewaterJoy Das MahapatraPas encore d'évaluation
- Nfpa 791-R2024Document20 pagesNfpa 791-R2024Ivan MarquezPas encore d'évaluation
- REFERENCES in APA Style 7th EditionDocument2 pagesREFERENCES in APA Style 7th EditionReabels FranciscoPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- 3.3.2.4 Love AnimalDocument8 pages3.3.2.4 Love AnimalRina ErnawatiPas encore d'évaluation
- 16-23 July 2011Document16 pages16-23 July 2011pratidinPas encore d'évaluation
- Format OpnameDocument21 pagesFormat OpnamerestutiyanaPas encore d'évaluation
- BB - Self AuditDocument18 pagesBB - Self AuditFe Rackle Pisco JamerPas encore d'évaluation
- ErpDocument31 pagesErpNurul Badriah Anwar AliPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- School Form 2 (SF2) Daily Attendance Report of LearnersDocument4 pagesSchool Form 2 (SF2) Daily Attendance Report of LearnersRyan A. CabalidaPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)