Académique Documents
Professionnel Documents
Culture Documents
Git
Transféré par
Gretchen SotoDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Git
Transféré par
Gretchen SotoDroits d'auteur :
Formats disponibles
Radiology is a medical specialty that employs the use of imaging to both diagnose and treat disease visualised within
the human body. Radiologists use an array of imaging technologies (such as x-ray radiography, ultrasound, computed tomography (CT), nuclear medicine, positron emission tomography (PET) and magnetic resonance imaging (MRI) to diagnose or treat diseases. Interventional radiology is the performance of (usually minimally invasive) medical procedures with the guidance of imaging technologies. The acquisition of medical imaging is usually carried out by the radiographer or radiologic technologist. Madura Foot X-Ray Main article: Projectional radiography Radiographs (or roentgenographs, named after the discoverer of x-rays, Wilhelm Conrad Rntgen) are produced by transmitting x-rays through a patient. A capture device then converts x-rays into visible light which then forms an image for review and diagnosis. The original - and a still common imaging procedure uses silver-impregnated films. In Film-Screen radiography, an x-ray tube generates a beam of x-rays which is aimed at the patient. The x-rays that pass through the patient are filtered by placing a device called x-ray filter, made of aluminium to reduce scatter and noise, and strike an undeveloped film, which is held tightly to a screen of light-emitting phosphors in a light-tight cassette. The film is then developed chemically and an image appears on the film. Now replacing Film-Screen radiography is Digital Radiography (DR), in which x-rays strike a plate of sensors that converts the signals generated into digital information and an image that is displayed on a computer screen. Plain radiography was the only imaging modality available during the first 50 years of radiology. Due to its availability, speed, and lower costs compared to other modalities, radiography is often the first-line test of choice in radiologic diagnosis. [edit] Fluoroscopy Main article: Fluoroscopy Fluoroscopy and angiography are special applications of X-ray imaging, in which a fluorescent screen and image intensifier tube is connected to a closed-circuit television system.[1]:26 This allows real-time imaging of structures in motion or
augmented with a radiocontrast agent. Radiocontrast agents are usually administered by swallowing or injection into the body of the patient to delineate anatomy and functioning of the blood vessels, the genitourinary system, or the gastrointestinal tract. Two radiocontrast agents are presently in common use. Barium sulfate (BaSO4) is given orally or rectally for evaluation of the GI tract. Iodine, in multiple proprietary forms, is given by oral, rectal, intra-arterial or intravenous routes. These radiocontrast agents strongly absorb or scatter X-ray radiation, and in conjunction with the real-time imaging allows demonstration of dynamic processes, such as peristalsis in the digestive tract or blood flow in arteries and veins. Iodine contrast may also be concentrated in abnormal areas more or less than in normal tissues and make abnormalities (tumors, cysts, inflammation) more conspicuous. Additionally, in specific circumstances air can be used as a contrast agent for the gastrointestinal system and carbon dioxide can be used as a contrast agent in the venous system; in these cases, the contrast agent attenuates the X-ray radiation less than the surrounding tissues. [edit] Interventional radiology Main article: Interventional radiology Interventional radiology (abbreviated IR or sometimes VIR for vascular and interventional radiology) is a subspecialty of radiology in which minimally invasive procedures are performed using image guidance. Some of these procedures are done for purely diagnostic purposes (e.g., angiogram), while others are done for treatment purposes (e.g., angioplasty). The basic concept behind interventional radiology is to diagnose or treat pathology, with the most minimally invasive technique possible. Interventional radiologists diagnose and treat several disorders including peripheral vascular disease, renal artery stenosis, inferior vena cava filter placement, gastrostomy tube placements, biliary stents and hepatic interventions. Images are used for guidance and the primary instruments used during the procedure are needles and tiny tubes called catheters. The images provide road maps that allow the interventional radiologist to guide these instruments through the body to the areas containing disease. By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery time as well as shorten hospital stays. To be a trained interventionalist in the United States, an individual completes a five year residency in Radiology and a one or two year fellowship in Interventional Radiology.[2]
[edit] Computed tomography (CT) Main article: X-ray computed tomography
Image from a CT scan of the brain CT imaging uses X-rays in conjunction with computing algorithms to image the body.[3] In CT, an X-ray generating tube opposite an X-ray detector (or detectors) in a ring shaped apparatus rotate around a patient producing a computer generated cross-sectional image (tomogram). CT is acquired in the axial plane, while coronal and sagittal images can be rendered by computer reconstruction. Radiocontrast agents are often used with CT for enhanced delineation of anatomy. Although radiographs provide higher spatial resolution, CT can detect more subtle variations in attenuation of X-rays. CT exposes the patient to more ionizing radiation than a radiograph. Spiral Multi-detector CT uses 8, 16, 64 or more detectors during continuous motion of the patient through the radiation beam to obtain much finer detail images in a shorter exam time. With rapid administration of IV contrast during the CT scan these fine detail images can be reconstructed into 3D images of carotid, cerebral, coronary or other arteries. CT scanning has become the test of choice in diagnosing some urgent and emergent conditions such as cerebral hemorrhage, pulmonary embolism (clots in the arteries of the lungs), aortic dissection (tearing of the aortic wall), appendicitis, diverticulitis, and obstructing kidney stones. Continuing improvements in CT technology including faster scanning times and improved resolution have dramatically increased the accuracy and usefulness of CT scanning which may partially account for increased use in medical diagnosis. The first commercially viable CT scanner was invented by Sir Godfrey Hounsfield at EMI Central Research Labs, Great Britain in 1972. EMI owned the distribution rights to The Beatles music and it was their profits which funded the research.[4] Sir Hounsfield and Alan McLeod McCormick shared the Nobel Prize for Medicine in 1979
for the invention of CT scanning. The fi [edit] Ultrasound Main article: Ultrasound Medical ultrasonography uses ultrasound (high-frequency sound waves) to visualize soft tissue structures in the body in real time. No ionizing radiation is involved, but the quality of the images obtained using ultrasound is highly dependent on the skill of the person (ultrasonographer) performing the exam and patient body habitus. Larger patients may have a decrease in image quality due to sound wave absorption in the subcutaneous fat layer. This results in less sound wave penetrating to organs and reflecting back to transducer ultimately causing a poorer quality image. Ultrasound is also limited by its inability to image through air (lungs, bowel loops) or bone. The use of ultrasound in medical imaging has developed mostly within the last 30 years. The first ultrasound images were static and two dimensional (2D), but with modern-day ultrasonography 3D reconstructions can be observed in real-time; effectively becoming 4D. Because ultrasound does not use ionizing radiation, unlike radiography, CT scans, and nuclear medicine imaging techniques, it is generally considered safer. For this reason, this modality plays a vital role in obstetrical imaging. Fetal anatomic development can be thoroughly evaluated allowing early diagnosis of many fetal anomalies. Growth can be assessed over time, important in patients with chronic disease or gestation-induced disease, and in multiple gestations (twins, triplets etc.). Color-Flow Doppler Ultrasound measures the severity of peripheral vascular disease and is used by Cardiology for dynamic evaluation of the heart, heart valves and major vessels. Stenosis of the carotid arteries can presage cerebral infarcts (strokes). DVT in the legs can be found via ultrasound before it dislodges and travels to the lungs (pulmonary embolism), which can be fatal if left untreated. Ultrasound is useful for image-guided interventions like biopsies and drainages such as thoracentesis). Small portable ultrasound devices now replace peritoneal lavage in the triage of trauma victims by directly assessing for the presence of hemorrhage in the peritoneum and the integrity of the major viscera including the liver, spleen and kidneys. Extensive hemoperitoneum (bleeding inside the body cavity) or injury to the major organs may require emergent surgical exploration and repair. [edit] Magnetic resonance imaging (MRI)
Main article: Magnetic resonance imaging Image from an MRI examination of the knee with a displaced patella MRI uses strong magnetic fields to align atomic nuclei (usually hydrogen protons) within body tissues, then uses a radio signal to disturb the axis of rotation of these nuclei and observes the radio frequency signal generated as the nuclei return to their baseline states. The radio signals are collected by small antennae, called coils, placed near the area of interest. An advantage of MRI is its ability to produce images in axial, coronal, sagittal and multiple oblique planes with equal ease. MRI scans give the best soft tissue contrast of all the imaging modalities. With advances in scanning speed and spatial resolution, and improvements in computer 3D algorithms and hardware, MRI has become an important tool in musculoskeletal radiology and neuroradiology. One disadvantage is that the patient has to hold still for long periods of time in a noisy, cramped space while the imaging is performed. Claustrophobia severe enough to terminate the MRI exam is reported in up to 5% of patients. Recent improvements in magnet design including stronger magnetic fields (3 teslas), shortening exam times, wider, shorter magnet bores and more open magnet designs, have brought some relief for claustrophobic patients. However, in magnets of equal field strength there is often a trade-off between image quality and open design. MRI has great benefit in imaging the brain, spine, and musculoskeletal system. The modality is currently contraindicated for patients with pacemakers, cochlear implants, some indwelling medication pumps, certain types of cerebral aneurysm clips, metal fragments in the eyes and some metallic hardware due to the powerful magnetic fields and strong fluctuating radio signals the body is exposed to. Areas of potential advancement include functional imaging, cardiovascular MRI, as well as MR image guided therapy. [edit] Nuclear medicine Main article: Nuclear medicine Nuclear medicine imaging involves the administration into the patient of radiopharmaceuticals consisting of substances with affinity for certain body tissues labeled with radioactive tracer. The most commonly used tracers are Technetium-99m, Iodine-123, Iodine-131, Gallium-67, Indium-111, Thallium-201 and 18F-FDG. The heart, lungs, thyroid, liver, gallbladder, and bones are commonly evaluated for particular conditions using these techniques. While anatomical detail is limited in these studies, nuclear medicine is useful in displaying physiological
function. The excretory function of the kidneys, iodine concentrating ability of the thyroid, blood flow to heart muscle, etc. can be measured. The principal imaging device is the gamma camera which detects the radiation emitted by the tracer in the body and displays it as an image. With computer processing, the information can be displayed as axial, coronal and sagittal images (SPECT images, single-photon emission computed tomography). In the most modern devices Nuclear Medicine images can be fused with a CT scan taken quasi-simultaneously so that the physiological information can be overlaid or co-registered with the anatomical structures to improve diagnostic accuracy. Positron emission tomography (PET), scanning is a nuclear medicine procedure that deals with positrons. The positrons annihilate to produce two opposite traveling gamma rays to be detected coincidentally, thus improving resolution. In PET scanning, a radioactive, biologically active substance, most often Fludeoxyglucose (18F), is injected into a patient and the radiation emitted by the patient is detected to produce multi-planar images of the body. Metabolically more active tissues, such as cancer, concentrate the active substance more than normal tissues. PET images can be combined (or "fused") with an anatomic imaging study (currently generally CT images), to more accurately localize PET findings and thereby improve diagnostic accuracy. The fusion technology has gone further to combine PET and MRI similar to PET and CT. PET/MRI fusion, largely practiced in academic and research settings, could potentially play a crucial role in fine detail of brain imaging, breast cancer screening and small joint imaging of foot. The technology recently blossomed following passing a technical hurdle of altered positron movement in strong magnetic field thus affecting the resolution of PET images and attenuation correction. [edit] Teleradiology Main article: Teleradiology Teleradiology is the transmission of radiographic images from one location to another for interpretation by a radiologist. It is most often used to allow rapid interpretation of emergency room, ICU and other emergent examinations after hours of usual operation, at night and on weekends. In these cases the images are often sent across time zones (i.e. to Spain, Australia, India) with the receiving radiologist working his normal daylight hours. Teleradiology can also be used to obtain
consultation with an expert or sub-specialist about a complicated or puzzling case. Teleradiology requires a sending station, high speed Internet connection and high quality receiving station. At the transmission station, plain radiographs are passed through a digitizing machine before transmission, while CT scans, MRIs, Ultrasounds and Nuclear Medicine scans can be sent directly as they are already a stream of digital data. The computer at the receiving end will need to have a high-quality display screen that has been tested and cleared for clinical purposes. Reports are then transmitted to the requesting physician. The major advantage of teleradiology is the ability to use different time zones to provide real-time emergency radiology services around-the-clock. The disadvantages include higher costs, limited contact between the ordering physician and the radiologist, and the inability to cover for procedures requiring an onsite radiologist. Laws and regulations concerning the use of teleradiology vary among the states, with some states requiring a license to practice medicine in the state sending the radiologic exam. Some states require the teleradiology report to be preliminary with the official report issued by a hospital staff radiologist. [edit] Professional training [edit] United States Radiology is an expanding field in medicine. Applying for residency positions in radiology has become increasingly competitive. Applicants are often near the top of their medical school class, with high USMLE (board) scores. The field is rapidly expanding due to advances in computer technology, which is closely linked to modern imaging. Diagnostic radiologists must complete prerequisite undergraduate education, 4 years of medical school to earn a medical degree (D.O. or M.D.), one year of internship, and 4 years of residency training.[5] After residency, radiologists often pursue one or two years of additional specialty fellowship training. To be certified by the American Board of Radiology (ABR), the radiology resident must pass a multiple choice medical physics board exam during training (usually taken after the second year of radiology residency) covering the science, technology and radiobiology of ultrasound, CTs, x-rays, nuclear medicine and MRI. A second multiple choice exam ("written board") on clinical aspects is then subsequently taken usually one year later. After passing these two tests and being in good standing, the
resident is eligible to take the oral examination or eligible to "sit for the Boards", taken about a month before graduating from the radiology residency. To complete the oral section of the ABR certification, a radiologist must pass all eleven sections. An applicant who passes fewer than eight sections has failed and must re-take the entire exam. An applicant who passes at least eight of the eleven sections of the ABR oral boards is considered "conditioned" and can retake the last three or fewer sections again at a later date to become ABR certified. Once successful in passing all sections, the physician then becomes a diplomate of the American Board of Radiology. Beginning with the residency class that started in 2010, the ABR's board examination structure will be changed to include two computer-based exams, one given after the third year of residency training covering both physics and clinical aspects with increasing emphasis on images, and the second exam to be taken 15 months after graduating from residency. The current oral examination is eliminated. Recertification examination is taken every 10 years with additional continuing medical education as outlined in the Maintenance of Certification (MOC) document. Certification may also be obtained from the American Osteopathic Board of Radiology (AOBR) and the American Board of Physician Specialties (ABPS). Following completion of residency training, radiologists may either begin practicing or enter into sub-specialty training programs known as fellowships. Examples of sub-speciality training in radiology include abdominal imaging, thoracic imaging, cross sectional/ultrasound, MRI, musculoskeletal imaging, interventional radiology, neuroradiology, interventional neuroradiology, paediatric radiology, nuclear medicine, emergency radiology, breast imaging and women's imaging. Fellowship training programs in radiology are usually 1 or 2 years in length.[6] Some medical schools in the US have started to incorporate a basic radiology introduction into their core MD training. New York Medical College, The Wayne State University School of Medicine, the Uniformed Services University, and the University of South Carolina School of Medicine offer an introduction to radiology during their respective MD Programs.[7][8][9][10] Radiographic exams are usually performed by radiologic technologists, (also known as diagnostic radiographers) who in the United States have a 2-year Associates Degree or 4 year Bachelors of Science Degree and, in the UK, a 3 year Honours Degree.
Veterinary radiologists are veterinarians that specialize in the use of X-rays, ultrasound, MRI and nuclear medicine for diagnostic imaging or treatment of disease in animals. They are certified in either diagnostic radiology or radiation oncology by the American College of Veterinary Radiology. Chiropractic Radiologists are doctors of chiropractic that have completed a minimum of 3 years of residency training, and are board certified Diplomates of the American Chiropractic Board of Radiology (ACBR).[11][12] Chiropractic radiology includes, but is not limited to, diagnostic interpretation of plain film radiography, digital radiography,[13] fluoroscopy, computed tomography, ultrasonography, radioisotope imaging and magnetic resonance imaging.[14] Some chiropractic radiologists also complete post-graduate fellowships to specialize in a specific area of radiology. Chiropractic radiologists practice and teach in a variety of institutions including chiropractic schools, medical schools,[15] hospitals, group practices,[16] imaging centers,[17][18][19] and private practices.[20] Achlorhydria - Literally without hydrochloric acid. Refers to lack of acid production by the stomach. Breath tests - Tests that detect abnormalities of CO2 and H2 elimination in the breath due to abnormalities of digestion, absorption, or bacterial overgrowth. Celiac disease (Gluten-Sensitive Enteropathy) - a malabsorption syndrome precipitated by the ingestion of gluten-containing foods, leading to destructive interaction of gluten with intestinal mucosa Chyme - The semifluid, homogenous, creamy or gruel-like material produced by gastric digestion of food; also called chymus. Crohns disease - A chronic inflammatory disease affecting any part of the gastrointestinal tract from the mouth to the anus. Cystic fibrosis - a genetic disorder characterized by widespread dysfunction of exocrine glands, characterized by chronic pulmonary disease, pancreatic deficiency and high levels of electrolytes in sweat Dumping syndrome - Condition in which, after gastric surgery, hyperosmolar chyme is dumped into the small intestine, causing rapid hypovolemia and hemoconcentration.
Fecal occult blood - The presence of blood in the feces in concentrations in excess of 2 mL per day, suggesting the possibility of malignant or premalignant lesions in the colon. GERD - gastroesophageal reflux disease Gluten - A protein found in wheat and wheat products. Helicobacter pylori - A bacterium found in the mucous layer of the stomach that has been implicated in the development of duodenal and gastric ulcers. Malabsorption - An abnormality of the small intestine that causes a disorder of the absorptive process. Maldigestion - An abnormality of the digestive process due to dysfunction of the pancreas or small intestine. Postgastrectomy syndrome - A syndrome that occurs after surgery for peptic ulcer disease and includes the dumping syndrome, diarrhea, maldigestion, weight loss, anemia, bone disease, and gastric cancer. Steatorrhea - A condition of excessive fat in feces (>7 g/day). Ulcerative colitis - A recurrent inflammatory disease of the large bowel that is also known as inflammatory bowel disease. Zollinger-Ellison (Z-E) syndrome - A condition resulting from a gastrin-secreting tumor (gastrinoma) of the pancreatic islet cells that results in an overproduction of gastric acid, leading to fulminant ulceration of the esophagus, stomach, duodenum, and jejunum. BACKGROUND/SIGNIFICANCE The GI tract is a vast and diverse system subject to a plethora of disorders. Many different laboratory tests have been developed that are invaluable tools that clinicians use to diagnosis and manage these disorders. Drug therapy is well established for the treatment of many diseases of the GI tract and it is essential that
pharmacists understand how to interpret laboratory tests related to GI function in order to recommend appropriate medications. GERD The most common disorder in the esophagus It affects up to 10% of the population The commonly used laboratory test is based on the measurement of the amount of HCl produced by the stomach Gastric Function Tests Measurement of the amount of HCl produced by the stomach under basal (resting) and fasting conditions and without exposure to visual, auditory or olfactory stimuli. This is followed by testing after maximal stimulation. The measurement of pepsin activity or pepsinogen I concentration of the gastric juice is possible, but their production so closely parallels the secretion of acid that testing for pepsin activity does not add significant clinical information about the function of the stomach. The standard methods now in use are as follows: A) Basal gastric secretion One hour morning aspiration Following a 12 hour overnight fast, the patient is intubated under fluoroscopic guidance and the residual gastric secretion is aspirated with a syringe with the patient leaning slightly to the right. The four 15 minute samples are taken and segregated in separate containers. Sudden pH changes would suggest regurgitation of intestinal contents. B) Pentagastrin stimulation test Pentagastrin is a synthetic pentapeptide containing the four C-terminal amino acids of gastrin coupled to alanine. It has biologic activity similar to gastrin, stimulating HCl and pepsin secretion. After completion of the basal secretion collection, pentagastrin (Peptavlon, Ayerst) is injected subcutaneously (4 g/kg). The peak acid output (PAO) is determined by collecting 6 serial 15 minute specimens and calculating the acid output on the basis
of the two highest specimens. The maximum acid output (MAO) is determined on the basis of four successive 15 minute specimens. Table 1
Gastric Acid
Young people > Old people Gastric carcinoma < Controls
Men > Women Gastric ulcer < Controls
Duodenal ulcer > Controls Jejunal ulcer > Controls
Table 2: Basal and Maximal Acid Output in Various Conditions
Conditions Sex Number of Patients
Acid Output (mEq./hour)
Basal Maximal
Controls Male Female 35 26 4.2 1.8 22.6 15.2
Medical students Male Female 145 16 5.3
3.3 26.7 21.4
Duodenal ulcer Male Female 256 64 7.1 4.2 35.2 25.7
Gastric ulcer Male Female 117 43 2.9 1.6 19.6 13.1
Gastric carcinoma Male Female 74 32 1.3 0.7 6.7 3.0
Jejunal ulcer Male Female Male 10 4 4 7.9 5.5 9.1 25.1 16.4 36.1
From Marks, I.N., et al: S. Afr. J. Surg. 1:53, 1963.
Following partial gastrectomy with gastrojejunostomy. Following gastroenterostomy alone.
C) Laboratory examination The volume of each sample is measured, a few drops of a pH indicator dye are added, and the pH is titrated to neutrality with 0.1 mol/L NaOH. The millimoles of acid are calculated per 15 minute sample and recorded. The total acid output for the basal and augmented test hours is calculated and reported. D) Clinical interpretation Achlorhydria (anacidity) after stimulation is seen in all cases of pernicious anemia, and in some patients with advanced carcinoma of the stomach. It may also be seen in a variety of other conditions, such as hypochromic anemia, aplastic anemia, hypothyroidism, nutritional megaloblastic anemia and in relatives of patients with pernicious anemia. Low values are found in gastric carcinoma, benign gastric ulcers, in females and in aging persons. Hyperacidity is seen in duodenal ulcer, but there is considerable overlap with the normal range. Gastrin is produced by the antral G cells of the stomach and stimulates HCl secretion by the parietal cells of the stomach. The Zollinger-Ellison (Z-E) syndrome is caused by a non-beta islet cell gastrin-secreting tumor of the pancreas. In this condition there is also a high ratio of basal/maximal acid output. Causes of Gastric Disorders vs. Hypergastremia Table 3: Serum Gastrin Concentrations in Various Disorders
Disorder Gastric acid secretion
Zollinger-Ellison syndrome greatly
Hypersecretion of gastrin by antral G-cells greatly
Pernicious anemia
Post vagotomy
Chronic renal failure variable
Drugs Important in Hyperacidity A) H2 antagonists (e.g., cimetidine, ranitidine) Inhibit gastric acid secretion due to histamine stimulation B) Proton-pump inhibitors (e.g., lansoprazole, omeprazole) Irreversibly inhibit pump that produces H+ (H+-K+ ATPase)
Little effect on intrinsic factor, pepsin or overall volume of secretion C) Antacids (e.g., Mg(OH)3, Al(OH)3, CaCO3) Neutralize HCl Helicobacter Pylori Helicobacter pylori has been implicated in many gastrointestinal diseases including duodenal and gastric ulcer, gastritis, and possibly gastric cancer. In asymptomatic individuals colonization by Helicobacter pylori increases with age up to 50% in the elderly. A) Diagnostic tests 1.Biopsy 1.Culture 2.Detection of urease enzyme activity by placing the biopsy specimen onto a substrate containing urea and monitoring change in pH. 2.13C-breath test Helicobacter pylori is a bacterium that is capable of living in the low pH environment of the stomach; as part of its adaptation to this hostile environment, it produces high levels of urease (which can help raise the local pH). Based on urease production by Helicobacter pylori, a patient ingests a 13C-labeled urea, and the breath of the patient is monitored for the appearance of 13C-labeled CO2. Within minutes after ingesting the labeled urea, the 13C to 12C ratio of respiratory CO2 starts to increase, reflecting the addition of the 13CO2 from the labeled urea. The maximum ratio of 13C to 12C peaks at 1.5 hours and then decreases to baseline. Using the 13C methodology, detection of Helicobacter pylori infection is determined with a clinical sensitivity of 94% and a specificity of 94.7%. 3.Immunoassay for IgG antibody There is a strong correlation between serum antibody and the presence of Helicobacter pylori in culture material obtained by biopsy. However, the test may remain positive for several years, even after successful treatment. Sample of Gastric Analysis Results (click to enlarge)
B) Preferred therapies for Helicobacter pylori infection
Triple therapy includes a proton-pump inhibitor (twice a day) and plus two of the following: amoxicillin, clarithromycin or metronidazole Quadruple therapy includes a proton-pump inhibitor (twice a day), tetracycline, bismuth, and metronidazole MALABSORPTION/MALDIGESTION A variety of diseases causes a disturbance in digestion and absorption. Maldigestion: Dysfunction of the digestive process that can occur in a number of sites in the gastrointestinal tract. Malabsorption: Dysfunction of the absorptive process by the gut caused by gluten, inflammation, infection, surgical resection, vitamin deficiency and other factors. Both conditions lead to one common syndrome called malabsorption. Thus, the diagnostic process is designed to: 1.Demonstrate the presence of malabsorption 2.Identify the type of disease process All major phases of absorption may simultaneously be affected, i.e. fats, proteins, carbohydrates, vitamins, minerals, etc. This syndrome, called general malabsorption, is characterized by amylorrhea (excess starch), steatorrhea (excess fat), and creatorrhea (meat fibers, protein). General Malabsorption/Maldigestion In this syndrome all major phases of absorption may be involved. This syndrome may be due to: 1.Pancreatic disease such as chronic pancreatitis, carcinoma, cystic fibrosis 2.Zollinger-Ellison syndrome (gastrinoma of the non-beta islet cells in the pancreas) 3.Liver disease with blockage of bile flow 4.Intestinal diseases Celiac disease [gluten (gliadin) sensitivity] Tropical sprue Idiopathic steatorrhea Crohns disease Whipples disease (caused by Tropheryma whippeli)
Scleroderma Amyloidosis Lymphoma Intestinal resection Blind Loop Syndrome Carcinoid syndrome 5.Resin treatment A) Tests of nonspecific biochemical abnormalities seen in malabsorption Serum calcium is usually low because of decreased absorption and decreased serum albumin to which normally 55% of the calcium in serum is bound Serum alkaline phosphatase is elevated; its source may be the gut but usually is the bone; chronically decreased vitamin D and calcium absorption lead to osteomalacia, a condition accompanied by inadequate mineralization of osteoid and elevations of serum alkaline phosphatase Serum proteins are decreased Serum urea nitrogen usually is low due to the decreased protein absorption Hypocholesterolemia is seen in the full syndrome of malabsorption, presumably due to decreased absorption of lipids and decreased synthesis of cholesterol The prothrombin time may be markedly prolonged, and the patient may even present with hemorrhages; a combination of reduced vitamin K absorption and decreased synthesis of clotting factor due to protein deficiency or decreased liver synthesis is responsible The glucose tolerance curve often is flat because of defective glucose absorption Vitamin A is decreased B) Specific malabsorption/maldigestion defects Disaccharidase deficiencies: lactase deficiency sucrase deficiency maltase deficiency Glucose-galactose malabsorption Pernicious anemia Protein-losing enteropathy Blind-loop syndrome Jejunal diverticulum Parasitic infestations
C) Tests used in the evaluation of malabsorption/maldigestion 1.Carbohydrate malabsorption D-xylose absorption test (decreased) Disaccharidase test (decreased) Breath hydrogen test (increased) 2.Fat malabsorption Fecal fat determination (elevated) 14C-triolein breath test (decreased) 3.Bacterial overgrowth 14C-Xylose breath test (increased) 4.Specific disorders Celiac disease (Endomysial antibody present) Pernicious anemia (Schilling test) Cystic fibrosis (sweat test)
Carbohydrate Malabsorption D-Xylose absorption test This test evaluates carbohydrate absorption and differentiates proximal intestinal from pancreatic malabsorption. D-xylose, a pentose, normally not present in urine, is given by mouth in doses of either 25 g or 5 g. Its excretion in a 5-hour urine sample and its levels in plasma at 1 or 2 hours are measured. The absorption of D-xylose in the intestine does not require phosphorylation or pancreatic secretions, and it is not metabolized by the liver. Thus, the urinary excretion of xylose is a reliable measure of intestinal absorption, provided renal function is normal. Plasma levels serve to ascertain if renal function is normal. Decreased D-xylose absorption is observed in celiac disease, tropical sprue, Crohns disease, immunoglobulin deficiency, pellagra, ascariasis, blind loop syndrome, radiation enteritis, surgical bowel resection, after vomiting, delayed gastric emptying, inadequate hydration, decreased circulation, renal disease, thyroid disease, sequestration in body fluids. Reference values > 4.1 g/5 h urine sample on 25 g dose > 1.2 g/5 h urine sample on 5 g dose 1 h plasma level: > 25 mg/dL on 25 g dose 2 h plasma level: > 15 mg/dL on 25 g dose
Some patients have abdominal discomfort with the 25 g dose. In these individuals (and in children) the 5 g dose is used. Interpretation of low urine levels of D-xylose Urine (U), plasma (P) 1.Intestinal malabsorption (P U) 2.Renal retention (renal failure) (nl or P, U) 3.Myxedema and bacterial overgrowth (poor absorption) (P, U) 4.Incomplete urine collection (nl P, U) Disaccharide test Individual disaccharides are administered orally and the blood glucose response is measured every 30 min for 2 h. To differentiate between disaccharidase deficiency and general malabsorption the test is performed with 50 g of each specific disaccharide. If the test is normal, disaccharidase deficiency is excluded. If it is abnormal an equivalent quantity of each constituent monosaccharide (25 g) is tested. Normal absorption of the monosaccharides excludes general carbohydrate malabsorption, and the lesion is identified as a disaccharidase deficiency. Acquired lactase deficiency is the most common with the congenital form being rare. Sucrase and maltase deficiencies are less common. The normal reponse should be an increase of serum glucose >20 30 mg/dL over fasting glucose levels. An increase of <20 mg/dL suggests a deficiency. Breath hydrogen test for carbohydrate intolerance This test is based on the principle that hydrogen is not produced by mammalian cells and its presence in expired air is due to bacterial fermentation of carbohydrates. A deficiency of one or more enzymes can lead to retention of sugars in the intestinal lumen, which are a source of bacterial fermentation in the large intestine. The bacteria ferment the sugars to hydrogen gas which is absorbed systemically and expired in air. Fat Malabsorption
Fecal fat determination In general malabsorption, steatorrhea is a consistent finding. High fecal fat is the best confirmatory test for steatorrhea; but, it gives no information as to the cause. The fecal lipids normally are derived from: 1.Mucosal cells 2.Gastrointestinal flora 3.Excretions into the intestinal lumen 4.Diet In health the normally small contribution of dietary fat to the total fecal lipids remains fairly constant despite variations in dietary fat intake. In malabsorption the fraction of unabsorbed dietary fat increases markedly. The standard total fecal fat determination should be carried out on the specimens pooled over 72 h. In our institution, feces for this purpose are collected in a pre-weighed gallon paint can, and kept refrigerated during the collection period. In the laboratory the entire sample is diluted with water, well blended to the point of emulsification and then small samples are removed for fat extraction by organic solvents, followed by drying and weighing. Results are reported in grams/24 h.
Reference range: 1-5 g/24 h
Questionable: 5-7 g/24 h
Abnormal:
>7 g/24 h
Fecal fat determinations are cumbersome and also entail unpleasantries for patients, ward and laboratory personnel alike, and they should be ordered only for stringent and appropriate clinical indications. However, a qualitative fecal fat by microscopic examination of stool for fat globules can be useful without the problems of a quantitative test. 14C-Triolein breath test This test is based on the principle that orally administered 14C-labeled triglycerides are digested and absorbed, and some of the labeled 14C is expired in the breath. This test measures the specific activity of 14CO2 and it assumes that there is a constant rate of CO2 production from other sources. The patient must be fasting and at rest during the study. The 14C-triolein breath test is not reliable in patients with diabetes, obesity, thyroid disease, or chronic respiratory insufficiency. The results correlate well with the fecal fat determination. Both tests are not specific for the cause of malabsorption. Specific Disorders Celiac Disease Celiac disease can be triggered after surgery, pregnancy, emotional stress or viral infections. Of particular high risk are those individuals with other autoimmune diseases. Diagnosing celiac disease can be difficult because some of its symptoms are similar to other illnesses such as Crohns disease, ulcerative colitis, diverticulosis, intestinal infections, chronic fatigue syndrome and depression. Diagnosis Accurate diagnosis of celiac disease requires gluten in the patients diet at the time of testing. The initial test is detection of IgA endomysial antibody (EMA) against tissue transglutaminase. The sensitivity of this test is close to 100% and specificity is around 95%. If this test is positive, the patient should have multiple small bowel biopsies from the second part of the duodenum and beyond to establish the diagnosis. The diagnosis is then confirmed by a resolution of symptoms following the
introduction and maintenance of a strictly gluten-free diet. In those patients that appear to have celiac disease but dont have an elevated EMA, consider that 2% of patients with celiac disease will be IgA deficient and unable to make IgA antibodies. A total IgA quantitation is indicated in these cases. These patients, and patients under the age of 3, should be tested for IgG antibodies to tissue transglutaminase. Since celiac disease is a relatively common disease associated with long-term complications that are treatable by a gluten-free diet, it has been considered for public-health screening. Arguments for this are the antibody testing is inexpensive, sensitive, and specific. However, the rebuttal is that we do not know the clinical significance of an asymptomatic individual found on screening to have the disease. Will these patients have the same long-term consequences? Additionally, a single negative test does not necessarily exclude possibility of disease in the future. Treatment The only treatment for the disease is a lifelong gluten-free diet. This is difficult due to the wide use of gluten in products ranging from bread to salad dressings and beer. Oats have general been considered safe for patients with celiac disease; however, recent studies indicate that the grain does contain some T-cell-stimulatory epitopes and that symptoms develop in some patients after consumption. Others contend that the oats are implicated due to contamination with wheat during packaging and transportation. Tef, a cereal traditionally grown in Ethiopia for making flat bread (injera), has been suggested as substituted for wheat flour in almost all applications and has similar nutritional value. Tef is only distantly related phylogenetically to wheat, barley and rye. Thus, tef could be considered for patients with celiac disease. (NEJM 2005;353:1748-9). Pernicious Anemia Schilling Test - absorption of vitamin B12 Vitamin B12 (cobalamin) is an essential cofactor for DNA synthesis. It requires gastric synthesis of intrinsic factor and proper ileal function for its absorption. B12 deficiency can be due to decreased intrinsic factor or decreased absorption due to pancreatic or ileal disease.
The Schilling test is performed by orally administering 57Co-radiolabeled B12 and quantitating its appearance in the serum, feces or (most commonly) in the urine. A reference population excretes > 8% of the ingested dose in a 24 hour urine collection while < 7% is excreted in pernicious anemia. If the abnormality corrects with the co-administration of intrinsic factor with B12, the defect is due to deficiency of intrinsic factor rather than malabsorption due to pancreatic or ileal causes. Cystic Fibrosis The sweat test is the most reliable laboratory test for the diagnosis of cystic fibrosis. In cystic fibrosis, sweat chloride values are 60-120 mmol/L; normal values are < 60 mmol/L. The test becomes positive within 3 to 5 weeks of age. Only 1 to 2 % of affected patients have sweat chloride values below 60 mmol/L and only 1 in 1000 has values below 50 mmol/L. Positive tests are observed in a number of other diseases; however, those are rare and are generally clinically distinct from cystic fibrosis. The Cystic Fibrosis Foundation of the U.S. accepts only the sweat test done by iontophoresis with direct determination of chloride or sodium. Use of ion-specific electrodes applied directly to the skin or agar plates for the determination of Cl- is no longer accepted. A) Collection of sample A 0.3% solution of pilocarpine (a cholinergic drug) is introduced into the skin by iontophoresis to induce sweating. Sweat is collected with a gauze pad, weighed, eluted, and analyzed for Cl- and less often Na+. B) Test for sweat chloride and sodium Gauze pad is weighed, eluted with measured amount of distilled water, and electrolytes are determined. C) Normal values Chloride: < 60 mmol/L Sodium: 10-90 mmol/L D) Elevated values are indicative of cystic fibrosis Chloride 60-120 mmol/L (no overlap of normal) Sodium 60-180 mmol/L (overlaps normal; less useful) DETECTION OF OCCULT BLOOD (HEME) Principle The detection of blood in feces is an important diagnostic aid in establishing the occurrence of internal bleeding resulting from gastrointestinal malignant growths or from gastric and duodenal ulcers. Severe gastrointestinal bleeding (60-90 mL blood
per day) is visually recognizable because "tarry" (black) stools are excreted and further microscopic examination of these stools reveals the presence of erythrocytes. In those instances where much smaller quantities of blood are not visually or microscopically apparent, more sensitive techniques are required to detect this hidden, or so-called "occult," blood. Because heme-containing substances possess peroxidase activity, this property can be used to detect the presence of occult blood in feces or urine. Colorless, aromatic substances (such as guaiacol, o-tolidine, di-orthoanisidine) are catalytically oxidized to blue chromogens by heme in the presence of H2O2 when the reaction is performed in an acid medium. The sensitivity of the test is adjusted in such a way that a physiologic amount of blood loss will not give a positive reaction. To establish that occult blood in feces is due to gastrointestinal hemorrhages, other possible sources of blood from hemorrhoids, menstrual flow, ingested blood derived from the nose or mouth, and perianal bleeding must be excluded. In addition, ingested meat contains hemoglobin and myoglobin and the presence of heme in stool derived from these foodstuffs may give false positive tests for fecal occult blood. Thus, for best results patients should be placed on meat-free or low-meat diets for three days before evaluation for occult blood in their stools. Normally, up to 2.5 mL of blood may be lost daily in the stools. Drugs (such as salicylates, steroids, reserpine, indomethacin, colchicine, iron) often cause increased gastrointestinal blood loss, resulting in positive occult blood tests. Potent reducing agents such as ascorbic acid may quench the reaction (false negative). False positives may be seen following ingestion of horseradish (peroxidase). To reduce the number of false negative results, the test should be requested on several different occasions.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Robin's DIY FMD Menu and RecipesDocument8 pagesRobin's DIY FMD Menu and RecipesmPas encore d'évaluation
- Clinical NutritionDocument175 pagesClinical NutritionCristianaParvanPas encore d'évaluation
- ReportDocument17 pagesReportBùi Văn PhúPas encore d'évaluation
- Lab Report For MonossacharideDocument15 pagesLab Report For MonossacharideSay Cheez100% (1)
- Primal Testosterone EbookDocument44 pagesPrimal Testosterone Ebook7nvzs8wn24Pas encore d'évaluation
- Beggs Mechanotherapy Ortho / Orthodontic Courses by Indian Dental AcademyDocument130 pagesBeggs Mechanotherapy Ortho / Orthodontic Courses by Indian Dental Academyindian dental academy100% (6)
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFDocument9 pages3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailPas encore d'évaluation
- ENG 105 SEC 37 Research PaperDocument20 pagesENG 105 SEC 37 Research PaperMushfique AhmedPas encore d'évaluation
- Brochure Physical ActivityDocument2 pagesBrochure Physical Activityapi-340126515Pas encore d'évaluation
- Biology 11 BODY SYSTEMSDocument13 pagesBiology 11 BODY SYSTEMSkatwal09Pas encore d'évaluation
- The Effect of Probiotic Biscuit On Faecal Microbiota in Malnourished ChildrenDocument11 pagesThe Effect of Probiotic Biscuit On Faecal Microbiota in Malnourished ChildrenAhmad DexPas encore d'évaluation
- Nutrition Diet Therapy for Cardiac PatientDocument27 pagesNutrition Diet Therapy for Cardiac PatientTina TalmadgePas encore d'évaluation
- Why We Get SickDocument32 pagesWhy We Get SickOne Clip100% (4)
- Diabetes MellitusDocument59 pagesDiabetes Mellitusuzzal ahmedPas encore d'évaluation
- Bulking Up: The Warfighter Nutrition GuideDocument10 pagesBulking Up: The Warfighter Nutrition GuideKim PetersenPas encore d'évaluation
- OB AssessmentDocument3 pagesOB AssessmentJoshua D ParkerPas encore d'évaluation
- Collagen Types 1Document24 pagesCollagen Types 1hayiwadaPas encore d'évaluation
- Exchange ListDocument16 pagesExchange ListSaira JabeenPas encore d'évaluation
- Real Food Althetes PlateDocument4 pagesReal Food Althetes Plateapi-236684744Pas encore d'évaluation
- System of Linear InequalitiesDocument7 pagesSystem of Linear InequalitiesDominic SavioPas encore d'évaluation
- Nutrition Labeling Questions L1 Through L153: Guidance For Industry: A Food Labeling GuideDocument18 pagesNutrition Labeling Questions L1 Through L153: Guidance For Industry: A Food Labeling GuidesrinuvoodiPas encore d'évaluation
- Brand Image Study of HorlicksDocument23 pagesBrand Image Study of HorlicksM.E. Prakash100% (1)
- Weight Gain SmoothiesDocument23 pagesWeight Gain SmoothiesDaEruditePas encore d'évaluation
- WINGS Corporation's Growth into a Market LeaderDocument9 pagesWINGS Corporation's Growth into a Market LeaderERna Permana PrasodjoPas encore d'évaluation
- Best Wii Games For Weight L...Document2 pagesBest Wii Games For Weight L...Maria CabritaPas encore d'évaluation
- Influence of Jackfruit Pulp On The Quality and Shelf Life of Jackfruit CakeDocument6 pagesInfluence of Jackfruit Pulp On The Quality and Shelf Life of Jackfruit Cakeokta misro'iPas encore d'évaluation
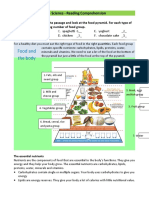
- Food Pyramid Word WorksheetDocument2 pagesFood Pyramid Word WorksheetAnabelPas encore d'évaluation
- Gapan City College Entrepreneurship DepartmentDocument10 pagesGapan City College Entrepreneurship DepartmentElisha EstiloPas encore d'évaluation
- 1.2 Growth and Production: 1.2.1 Tree SpacingDocument9 pages1.2 Growth and Production: 1.2.1 Tree SpacingGiza FirisaPas encore d'évaluation
- Manual of Homeopathic Practice (1876)Document864 pagesManual of Homeopathic Practice (1876)Dr. JimPas encore d'évaluation