Académique Documents
Professionnel Documents
Culture Documents
Cleft Palate and Cleft Lip Introduction
Transféré par
CLaui SagibalDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cleft Palate and Cleft Lip Introduction
Transféré par
CLaui SagibalDroits d'auteur :
Formats disponibles
Cleft Palate and Cleft Lip Introduction Cleft lip and cleft palate are facial and oral
malformations that occur very early in pregnancy, while the baby is developing inside its mother. Clefting results when there is not enough tissue in the mouth or lip area, and the tissue that is available does not join together properly. A cleft lip is a physical split or separation of the two sides of the upper lip and appears as a narrow opening or gap in the skin of the upper lip. This separation often extends beyond the base of the nose and includes the bones of the upper jaw and/or upper gum. A cleft palate is a split or opening in the roof of the mouth. A cleft palate can involve the hard palate (the bony front portion of the roof of the mouth), and/or the soft palate (the soft back portion of the roof of the mouth). Cleft lip and cleft palate can occur on one or both sides of the mouth. Because the lip and the palate develop separately, it is possible to have a cleft lip without a cleft palate, a cleft palate without a cleft lip, or both a cleft lip and cleft palate together. Who Gets Cleft Lip and Cleft Palate? Cleft lip, with or without cleft palate, affects one in 700 babies annually, and is the fourth most common birth defect in the U.S. Clefts occur more often inchildren of Asian, Latino, or Native American descent. Compared with girls, twice as many boys have a cleft lip, both with and without a cleft palate. However, compared with boys, twice as many girls have cleft palate without a cleft lip. What Causes a Cleft Lip and Cleft Palate? In most cases, the cause of cleft lip and cleft palate is unknown. These conditions cannot be prevented. Most scientists believe clefts are due to a combination of genetic and environmental factors. There appears to be a greater chance of clefting in a newborn if a sibling, parent, or relative has had the problem. Another potential cause may be related to a medication a mother may have taken during her pregnancy. Some drugs may cause cleft lip and cleft palate. Among them: anti-seizure/anticonvulsant medications, acnemedications containing Accutane, and methotrexate, a drug commonly used for treating cancer, arthritis, and psoriasis. Cleft lip and cleft palate may also occur as a result of exposure to viruses or chemicals while the fetus is developing in the womb. In other situations, cleft lip and cleft palate may be part of another medical condition. What Problems Are Associated With Cleft Lip and/or Cleft Palate?
Eating problems. With a separation or opening in the palate, food and liquids can pass from the mouth back through the nose. Fortunately, specially designed baby bottles and nipples that help keep fluids flowing downward toward the stomach are available. Children with a cleft palate may need to wear a man-made palate to help them eat properly and ensure that they are receiving adequate nutrition until surgical treatment is provided.
Ear infections/hearing loss. Children with cleft palate are at increased risk of ear infections since they are more prone to fluid build-up in the middle ear. If left untreated, ear infections can cause hearing loss. To prevent this from happening, children with cleft palate usually need special tubes placed in the eardrums to aid fluid drainage, and their hearing needs to be checked once a year.
Speech problems. Children with cleft lip or cleft palate may also have trouble speaking. These children's voices don't carry well, the voice may take on a nasal sound, and the speech may be difficult to understand. Not all children have these problems and surgery may fix these problems entirely for some. For others, a special doctor, called speech pathologist, will work with the child to resolve speech difficulties.
Dental Problems. Children with clefts are more prone to a larger than average number of cavities and often have missing, extra, malformed, or displaced teeth requiring dental and orthodontic treatments. In addition, children with cleft palate often have an alveolar ridge defect. The alveolus is the bony upper gum that contains teeth. A defect in the alveolus can (1) displace, tip, or rotate permanent teeth, (2) prevent permanent teeth from appearing, and (3) prevent the alveolar ridge from forming. These problems can usually be repaired through oral surgery.
. Description 1. Cleft lip (cheiloschisis) is a congenital anomaly that occurs at a rate of 1 in 800 births. a. If the cleft does not affect the palate structure of the mouth it is referred to as cleft lip. b. Cleft lip is formed in the top of the lip as either a small gap or an indentation in the lip (partial or incomplete cleft) or it continues into the nose (complete cleft) c. Cleft lip can be unilateral or bilateral. d. It is due to the failure of fusion of the maxillary and medial nasal processes (formation of the primary palate). 2. Cleft palate (palatoschisis) is a congenital anomaly that occurs in approximately 1 of every 2000 births, and it is more common in boys than girls.
a. It is a condition in which the two plates of the skull that form the hard palate (roof of the mouth) are not completely joined. b. It ranges in severity from soft palate involvement alone to a defect including the hard palate and portions of the maxilla. c. Cleft palate may or may not be associated with cleft lip. 3. Children with these structural disorders may have associated dental malformations, speech problems, and frequent otitis media, the latter resulting from improper functioning of the Eustachian tubes. B. Etiology 1. Many factors are associated with the development of cleft lip and cleft palate, and cleft lip with or without cleft palate is developmentally and genetically different from isolated cleft palate. 2. Most cases appear to be consistent with the concept of multifactorial inheritance as evidenced by an increase incidence in relatives and monozygotic twins. C. Pathophysiology 1. During embryonic development the lateral and medial tissues forming the upper lip palates fuse between weeks 7 and 8 of gestation; the palatal tissues forming the hard and soft palates fuse between weeks 7 and 12 gestation. 2. Cleft lip and cleft palate result when these tissues fail to fuse. D. Assessment findings 1. Clinical manifestations a. Cleft lip and cleft palate are readily apparent at birth. Careful physical assessment should be performed to rule out other midline birth defects. b. Cleft lip and cleft palate appear as incomplete or complete defects, and may be unilateral or bilateral. 2. Laboratory and diagnostic study findings. Obstetric ultrasound will reveal cleft lipwhile the infant is in utero. E. Nursing management 1. Assess for problems with feeding, breathing parental bonding, and speech. 2. Ensure adequate nutrition and prevent aspiration. a. Provide special nipples or feeding devices (eg, soft pliable bottle with soft nipple with enlarged opening) for a child unable to suck adequately on standard nipples. b. Hold the child in a semiupright position; direct the formula away from the cleft and toward the side and back of the mouth to prevent aspiration.
c. Feed the infant slowly and burp frequently to prevent excessive swallowing of air and regurgitation. d. Stimulate sucking by gently rubbing the nipple against the lower lip. 3. Support the infants and parents emotional and social adjustment. a. Help facilitate the familys acceptance of the infant by encouraging the parents to express their feelings and concerns and by conveying an attitude of acceptance toward the infant. b. Emphasize the infants positive aspects and express optimism regarding surgical correction. 4. Provide preoperative care. a. Depending in the defect and the childs general condition, surgical correction of the cleft lip usually occurs at 1 to 3 months of age; repair of the cleft palate is usually performed between 6 and 18 months of age. Repair of the cleft palate may require several stages of surgery as the child grows. b. Early correction of cleft lip enables more normal sucking patterns and facilitates bonding. Early correction of cleft palate enables development of more normal speech patterns. c. Delayed closure or large defects may require the use of orthodontic appliances. d. The responsibilities of the nurse are to: 1. Reinforce the physicians explanation of surgical procedures. 2. Provide mouth care to prevent infection. 5. Provide postoperative care.
a. Assess airway patency and vital signs; observe for edema and respiratory distress. b. Use a mist tent, if prescribed, to minimize edema, liquefy secretions, and minimize distress. c. Position the child with cleft lip on her back, in an infant seat, or propped on a side to avoid injury to the operative site; position the child with a cleft palate on the abdomen to facilities drainage. d. Clean the suture line and apply an antibacterial ointment as prescribed to prevent infection and scarring. Monitor the site for signs of infection. e. Use elbow restraints to maintain suture line integrity. Remove them every 2 hours for skin care and range-of-motion exercises. f. Feed the infant with a rubber-tipped medicine dropper, bulb syringe, Breck feeder, or soft bottle-nipples, as prescribed, to help preserve suture integrity. For older children, diet progresses from clear fluids; they should not use straws or sharp objects. g. Attempt to keep the child from putting tongue up to palate sutures. h. Manage pain by administering analgesic as prescribed. 6. Provide child and family teaching. Demonstrate surgical wound care. Show proper feeding techniques and positions. Explain that temperature of feeding formulas should be monitored closely because new palate has no nerve endings; therefore; the child can suffer a burn to the palate easily and without knowing it. Explain handling of prosthesis if indicated. Stress the importance of long-term follow up, including speech therapy, and preventing or correcting dental abnormalities. Discuss the need for, at least, annual hearing evaluations because of the increased susceptibility to recurrent otitis. The child may require myringotomy and surgical placement of drainage tubes. Teach infection control measures
Cause
The development of the face is coordinated by complex morphogenetic events and rapid proliferative expansion, and is thus highly susceptible to environmental and genetic factors, rationalising the high incidence of facial malformations. During the first six to eight weeks of pregnancy, the shape of the embryo's head is formed. Five primitive tissue lobes grow: a) one from the top of the head down towards the future upper lip; (Frontonasal Prominence) b-c) two from the cheeks, which meet the first lobe to form the upper lip; (Maxillar Prominence) d-e) and just below, two additional lobes grow from each side, which form the chin and lower lip; (Mandibular Prominence) If these tissues fail to meet, a gap appears where the tissues should have joined (fused). This may happen in any single joining site, or simultaneously in several or all of them. The resulting birth defect reflects the locations and severity of individual fusion failures (e.g., from a small lip or palate fissure up to a completely malformed face). The upper lip is formed earlier than the palate, from the first three lobes named a to c above. Formation of the palate is the last step in joining the five embryonic facial lobes, and involves the back portions of the lobes b and c. These back portions are called [19] palatal shelves, which grow towards each other until they fuse in the middle. This process is very vulnerable to multiple toxic substances, environmental pollutants, and nutritional imbalance. The biologic mechanisms of mutual recognition of the two cabinets, and the way they are glued together, are quite complex and obscure despite intensive scientific research
Vous aimerez peut-être aussi
- Cleft Lip and Palate CareDocument16 pagesCleft Lip and Palate CareIsmail LubisPas encore d'évaluation
- EJMCM - Volume 7 - Issue 10 - Pages 470-474Document5 pagesEJMCM - Volume 7 - Issue 10 - Pages 470-474Ayu Nur FadilahPas encore d'évaluation
- Cleft Lip and PalateDocument18 pagesCleft Lip and Palateicywitch100% (1)
- Cleft Lip Pregnancy BabyDocument2 pagesCleft Lip Pregnancy BabySamrah ManibpelPas encore d'évaluation
- Cleft Lip and PalateDocument20 pagesCleft Lip and Palatejapzee1988100% (1)
- Chrisanthopoulos Marika 300453 Cleft Lip and PalateDocument14 pagesChrisanthopoulos Marika 300453 Cleft Lip and PalateCharles IppolitoPas encore d'évaluation
- Cleft Lip Palate CareDocument6 pagesCleft Lip Palate CarekrishnasreePas encore d'évaluation
- Cleft LipDocument5 pagesCleft LipGraziePas encore d'évaluation
- About Oral Clefting: Birth DefectsDocument7 pagesAbout Oral Clefting: Birth DefectsWilly TenjayaPas encore d'évaluation
- Cleft Lip and Palate FactsDocument9 pagesCleft Lip and Palate FactsJahzel CallinoPas encore d'évaluation
- Cleft Lip and Palate TreatmentDocument3 pagesCleft Lip and Palate TreatmentnarutomoviePas encore d'évaluation
- Cleft Palate Pregnancy Mouth: Slideshow: Migraine Dos and Don'tsDocument6 pagesCleft Palate Pregnancy Mouth: Slideshow: Migraine Dos and Don'tsBenedictus HanjayaPas encore d'évaluation
- Cleft Lip and Cleft PalateDocument22 pagesCleft Lip and Cleft PalateOm VaishNav0% (1)
- Cleft and Lip PalateDocument6 pagesCleft and Lip PalateShane PangilinanPas encore d'évaluation
- Cleft Lip and Palate Disorders ExplainedDocument20 pagesCleft Lip and Palate Disorders ExplainedKaka SalvatorePas encore d'évaluation
- Syndrome Cleft Lip and PalateDocument8 pagesSyndrome Cleft Lip and PalateValentina Lakhsmi PrabandariPas encore d'évaluation
- Cleft Lip or Cleft PalateDocument2 pagesCleft Lip or Cleft PalateKueenmae Unza SolivenPas encore d'évaluation
- Cleft Lip and Palate CareDocument4 pagesCleft Lip and Palate CareJulliza Joy PandiPas encore d'évaluation
- PalatoschisisDocument4 pagesPalatoschisisInge Sandrie PhutriPas encore d'évaluation
- Maternal First Quiz ReviewerDocument15 pagesMaternal First Quiz ReviewerRay Ann BorresPas encore d'évaluation
- Types of cleft palate surgeries and side effects explainedDocument91 pagesTypes of cleft palate surgeries and side effects explainedahmad shaddadPas encore d'évaluation
- Cleft Lip and Cleft PalateDocument16 pagesCleft Lip and Cleft Palatemacuka08100% (3)
- Cleft Lip PalateDocument29 pagesCleft Lip PalatelisalovPas encore d'évaluation
- Cleft Lip and Palate Care GuideDocument7 pagesCleft Lip and Palate Care GuideUday Kumar0% (1)
- Nursing Care of The Child Born With PhysicalDocument55 pagesNursing Care of The Child Born With PhysicalJoy kimmPas encore d'évaluation
- Physical and Developmental Disorders of The Gastrointestinal SystemDocument10 pagesPhysical and Developmental Disorders of The Gastrointestinal SystemJo Marchianne PigarPas encore d'évaluation
- Cleft Lip and Cleft PalateDocument12 pagesCleft Lip and Cleft PalateNadieya SafiyaPas encore d'évaluation
- 6 Cleft Palate Cleft LipDocument2 pages6 Cleft Palate Cleft LipLidya DiandraPas encore d'évaluation
- Cleft Lip and PalateDocument25 pagesCleft Lip and PalateRahul Dhaker100% (1)
- Health Brochure Comprehensive OverviewDocument12 pagesHealth Brochure Comprehensive Overviewعبدالرحمن سالم بن مخاشنPas encore d'évaluation
- Baba Jaswant Singh Dental College and Research Institute, LudhianaDocument40 pagesBaba Jaswant Singh Dental College and Research Institute, LudhianaPalak VashistPas encore d'évaluation
- Oral Development PathologyDocument6 pagesOral Development PathologyKathyWPas encore d'évaluation
- Role of Feeding Plate in Cleft Palate: Case Report and Review of LiteratureDocument9 pagesRole of Feeding Plate in Cleft Palate: Case Report and Review of Literatureimroatul hasanahPas encore d'évaluation
- Cleft Lip and Palate GuideDocument4 pagesCleft Lip and Palate GuideMaricel DefiestaPas encore d'évaluation
- Cleft Lip BrochureDocument15 pagesCleft Lip BrochureValentina Cerón ZúñigaPas encore d'évaluation
- Cleft lip and palate treatment guideDocument19 pagesCleft lip and palate treatment guideAnkita Rathi AgrawalPas encore d'évaluation
- Lecture 19 Rampant CariesDocument12 pagesLecture 19 Rampant CariesKhaled Al-haddadPas encore d'évaluation
- Cleft Palate BookletDocument8 pagesCleft Palate BookletsalamredPas encore d'évaluation
- Cleft Lip and Cleft Palate: College of Health Science Department of Midwifery Course Newborn Care For PostbasicDocument42 pagesCleft Lip and Cleft Palate: College of Health Science Department of Midwifery Course Newborn Care For PostbasicmichaelPas encore d'évaluation
- Lesson 16Document20 pagesLesson 16Twinamasiko DanielPas encore d'évaluation
- Polygenetic Traits: Presented by Archa SasikumarDocument30 pagesPolygenetic Traits: Presented by Archa SasikumarArcha SasikumarPas encore d'évaluation
- Cleft Lip and Palate GuideDocument8 pagesCleft Lip and Palate GuideRAJU33% (3)
- 15.3 Cleft Lip and PalateDocument41 pages15.3 Cleft Lip and PalateChristina YounasPas encore d'évaluation
- Cleft Lip PalateDocument1 pageCleft Lip PalateBara pawanaPas encore d'évaluation
- Special Needs Research PaperDocument8 pagesSpecial Needs Research Paperapi-660191691Pas encore d'évaluation
- Dental Care For The Patient With A Cleft Lip and Palate. Part 2: The Mixed Dentition Stage Through To Adolescence and Young AdulthoodDocument4 pagesDental Care For The Patient With A Cleft Lip and Palate. Part 2: The Mixed Dentition Stage Through To Adolescence and Young AdulthoodMostafa FayadPas encore d'évaluation
- Submucuos Cleft Palate BrochureDocument2 pagesSubmucuos Cleft Palate Brochurecleft_palatePas encore d'évaluation
- Labioschizis Dan Palatoskisis Persentasi Kelompok 1Document17 pagesLabioschizis Dan Palatoskisis Persentasi Kelompok 1Hengky HanggaraPas encore d'évaluation
- Oral Perif ExamDocument18 pagesOral Perif ExamElena LOgoPas encore d'évaluation
- GASTROINTESTINAL DISORDERS Cleft Palate - Esophageal Atresia - Oral MoniliasisDocument7 pagesGASTROINTESTINAL DISORDERS Cleft Palate - Esophageal Atresia - Oral MoniliasisMikasa AckermanPas encore d'évaluation
- Cleft Lip and Palate Causes and CareDocument26 pagesCleft Lip and Palate Causes and CareRohit ThetePas encore d'évaluation
- Kliegman: Nelson Textbook of Pediatrics, 18th Ed.: 2007 Saunders, An Imprint of ElsevierDocument14 pagesKliegman: Nelson Textbook of Pediatrics, 18th Ed.: 2007 Saunders, An Imprint of ElseviermelindamentariPas encore d'évaluation
- Cleft Lip Cleft Palate: Presented By: Ivan AvenadoDocument16 pagesCleft Lip Cleft Palate: Presented By: Ivan AvenadoIvan Liquiran AvenadoPas encore d'évaluation
- Asynch DabucolDocument4 pagesAsynch DabucolKatelinne DabucolPas encore d'évaluation
- Bad HabitsDocument7 pagesBad HabitsAnonymous itwv6oMPas encore d'évaluation
- Cleft Formation. Double Lip - Case ReportDocument6 pagesCleft Formation. Double Lip - Case Reportval362Pas encore d'évaluation
- Cleft Lip And Palate, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCleft Lip And Palate, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÉvaluation : 4.5 sur 5 étoiles4.5/5 (3)
- How to address breastfeeding difficulties due to tongue-tieD'EverandHow to address breastfeeding difficulties due to tongue-tiePas encore d'évaluation
- Breastfeeding and tongue tie: How it can affect feedingD'EverandBreastfeeding and tongue tie: How it can affect feedingPas encore d'évaluation
- Typhoid Fever PamphletDocument3 pagesTyphoid Fever PamphletCLaui SagibalPas encore d'évaluation
- Surgical TermsDocument10 pagesSurgical TermsCLaui SagibalPas encore d'évaluation
- AromatherapyDocument3 pagesAromatherapyCLaui SagibalPas encore d'évaluation
- Emergency Crash Cart ContentsDocument15 pagesEmergency Crash Cart ContentsCLaui SagibalPas encore d'évaluation
- Balanced Diet: Includes Foods From All Food Groups During The DayDocument19 pagesBalanced Diet: Includes Foods From All Food Groups During The DayMayuri VohraPas encore d'évaluation
- Pancha Karma (Sree Subramania Ayurvedic Nursing Home)Document15 pagesPancha Karma (Sree Subramania Ayurvedic Nursing Home)Sanand Ratnam Thekkayil100% (1)
- Brochure - Cs9300-System-201302 PDFDocument12 pagesBrochure - Cs9300-System-201302 PDFjesusPas encore d'évaluation
- Legal Medicine Review PDFDocument10 pagesLegal Medicine Review PDFGhie TangonanPas encore d'évaluation
- Sputum Culture TestDocument5 pagesSputum Culture TestpraveenASPPas encore d'évaluation
- Nasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyDocument4 pagesNasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyEditor IJTSRDPas encore d'évaluation
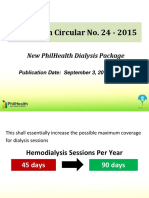
- 09 Dialysis DataDocument11 pages09 Dialysis DataThinkingPinoyPas encore d'évaluation
- Friedberg Wilt 2010 CT and MetaphorsDocument16 pagesFriedberg Wilt 2010 CT and MetaphorsAlexandra HuhPas encore d'évaluation
- Lifestyle, Genetics and Environment Predispose to DiseaseDocument4 pagesLifestyle, Genetics and Environment Predispose to DiseaseJohnnette BedoniaPas encore d'évaluation
- Mental Health CH 2Document6 pagesMental Health CH 2Gina GiammalvoPas encore d'évaluation
- Air Gets Inside The Chest CavityDocument2 pagesAir Gets Inside The Chest CavityLore Anne Mhae SantosPas encore d'évaluation
- Sandip Das Naukri CVDocument3 pagesSandip Das Naukri CVShreya SinghPas encore d'évaluation
- Innovations in Medical ElectronicsDocument10 pagesInnovations in Medical Electronicsapi-3837905100% (5)
- Fluid and Electrolyte BalanceDocument295 pagesFluid and Electrolyte BalanceAnuchithra RadhakrishnanPas encore d'évaluation
- The Benefits of ExerciseDocument3 pagesThe Benefits of ExerciseAtet KurniadiPas encore d'évaluation
- CPC PowerpointDocument36 pagesCPC Powerpointapi-277377339Pas encore d'évaluation
- Pharmacokinetics & Drug Metabolism LectureDocument78 pagesPharmacokinetics & Drug Metabolism LectureJoseph ChanPas encore d'évaluation
- Malaria Control ProgramDocument17 pagesMalaria Control ProgramCaliso RichmondPas encore d'évaluation
- Greenberg 2021Document5 pagesGreenberg 2021SALMA HANINAPas encore d'évaluation
- Perioperative Nursing Care PhasesDocument5 pagesPerioperative Nursing Care PhasesanjiePas encore d'évaluation
- Absence of A Menstrual PeriodDocument2 pagesAbsence of A Menstrual PeriodDragan PetrovicPas encore d'évaluation
- Clinical Approach To Syncope in ChildrenDocument6 pagesClinical Approach To Syncope in ChildrenJahzeel Gacitúa Becerra100% (1)
- Ist Bams Internal Exam (Winter - 2021 Batch)Document2 pagesIst Bams Internal Exam (Winter - 2021 Batch)Shubham PandarePas encore d'évaluation
- Behavior Therapy For ChildrenDocument72 pagesBehavior Therapy For ChildrenJaveria Danish100% (3)
- 09 SterilizationDocument34 pages09 Sterilizationitung2350% (2)
- Marketing Research MethodologyDocument3 pagesMarketing Research MethodologyAniket SinghPas encore d'évaluation
- Development Economics II Summary: Health, Calories, and ProductivityDocument9 pagesDevelopment Economics II Summary: Health, Calories, and Productivityshabrina larasatiPas encore d'évaluation
- Callista Roy Adaptation TheoryDocument11 pagesCallista Roy Adaptation Theoryandre_delitua100% (6)
- Hutzell Workbook 2009 PDFDocument48 pagesHutzell Workbook 2009 PDFPedro Almeida100% (2)
- BSSP Course DescriptionsDocument3 pagesBSSP Course DescriptionsJilliane LagusPas encore d'évaluation