Académique Documents
Professionnel Documents
Culture Documents
Prevention of Hypotension During Spinal Anesthesia
Transféré par
Ardi FkuiDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Prevention of Hypotension During Spinal Anesthesia
Transféré par
Ardi FkuiDroits d'auteur :
Formats disponibles
Prevention of Hypotension During Spinal Anesthesia: A Comparison of Intravascular Administration of Hetastarch Versus Lactated Ringers Solution
Shiv K. Sharma, MD, FRCA, Noor M. Gajraj, MB, BS, FRCA, and J. Elaine Sidawi,
Department of Anesthesiology and Pain Management, University of Texas Southwestern MD Medical School, Dallas, Texas
This study was designed to compare the efficacy of 6% hetastarch to that of crystalloid administration in reducing the incidence and severity of hypotension during spinal anesthesia. Forty ASA grade I patients scheduled for postpartum tubal ligations under spinal anesthesia were randomly allocated to receive either 500 mL of hetastarch solution or 1000 mL of lactated Ringers solution prior to spinal anesthesia. Spinal anesthesia was managed identically in both groups by anesthesiologists who were unaware of the type of fluid administered. The incidence of hypotension was 11 of 21(52%) in the lactated Ringers solution group and 3 of
19 (16%) in the hetastarch group. The difference in the incidence of hypotension was significant (P < 0.05). The requirement of 5-mg bolus doses of ephedrine to maintain systolic arterial blood pressure > 75% of baseline was significantly greater in the lactated Ringers group than in the hetastarch group (15 vs 4, P < 0.05). We conclude that an intravenous infusion of 500 mL of 6% hetastarch solution is more effective than 1000 mL lactated Ringers solution in attenuating spinal anesthesia induced hypotension in women undergoing postpartum tubal ligation. (Anesth Analg 1997;84:1114)
ypotension during spinal anesthesia is common and can cause significant morbidity and mortality (1,2). Prior to spinal anesthesia crystalloid administration is recommended to reduce the incidence of hypotension, although its value has been questioned (3-6). Crystalloid solutions have a short intravascular half-life and are poor plasma volume expanders, which may explain why hypotension associated with spinal anesthesia cannot be completely eliminated by crystalloid preloading. Large volumes of crystalloid fluid can also decrease oxygen-carrying capacity, and may increase the risk of pulmonary and peripheral edema during the puerperium (7). Colloid solutions which remain in the circulation for a longer period seem to be an effective alternative. The administration prior to spinal anesthesia of 5% albumin for cesarean section and gelatin for transurethral resection are effective in preventing hypotension (8,9). Hetastarch is a colloid solution widely used for plasma volume expansion in patients with trauma,
Presented at the annual meeting of the International Anesthesia Research Society, Honolulu, HI, March 1995. Accepted for publication September 19, 1996. Address correspondence and reprint requests to Shiv K. Sharma, MD, FRCA, Department of Anesthesiology and Pain Management, University of Texas Southwestern Medical School, 5323 Harry Hines Blvd., Dallas, TX 75235-9068.
01996 by the International 0003.2999/97/$5.00 Anesthesia Research Society
shock, or sepsis. A recent study concluded that preloading with 6% hetastarch and lactated Ringers (LR) solution is more effective in reducing the incidence of spinal-induced hypotension during cesarean section than preloading with LR solution alone (10). However, the efficacy of preloading with colloid solutions in reducing the incidence of hypotension after spinal anesthesia in patients undergoing tubal ligation has not been evaluated. The aim of this study was to compare the efficacy of 500 mL of 6% hetastarch solution to that of 1000 mL of LR solution in preventing hypotension during spinal anesthesia in patients undergoing postpartum tubal ligations.
Methods
After institutional review board approval, informed, written consent was obtained from 40 ASA grade I patients undergoing tubal ligation within 15-24 h postdelivery. Patients with obesity, diabetes, pregnancy-induced hypertension, chronic hypertension, and heart disease were excluded from the study. Patients were unpremeditated and did not receive sedatives in the 4-h period prior to anesthesia. Patients were transported to the operating room where an l&gauge intravenous (IV) cannula was inserted into a peripheral vein, and sodium citrate 30 mL orally and
Anesth
Analg
1997;84:1114
111
112
REGIONAL COLLOID
ANESTHESIA AND VERSUS CRYSTALLOID
PAIN MANAGEMENT DURING SPINAL
SHARMA BLOCK
ET AL
ANESTH ANALG 1997;84:111-14
metaclopramide 10 mg IV were administered. Patients were continuously monitored with the usual monitors. Baseline arterial blood pressure was taken as the average of three preoperative recordings. The patients were randomly allocated to receive either 500 mL of 6% hetastarch or 1000 mL of LR solution. The fluid was administered prior to spinal anesthesia over a 15-min period by an anesthesiologist, after which an infusion of LR solution was used for fluid maintenance in all patients. Spinal anesthesia was then managed by another anesthesiologist who was not present in the operating room during the time of prehydration, and who was thus unaware of the type of fluid administered. With the patient in the sitting position, hyperbaric 5% lidocaine 75 mg with fentanyl 10 Fg was injected intrathecally through a 25gauge Whitacre spinal needle at the L2-3 or L3-4 interspace. After the subarachnoid injection, all patients were placed in the supine position and arterial blood pressure and heart rate were recorded at l-min intervals for the first 15 min and subsequently at 3-min intervals. The incidence, timing, severity and duration of hypotension, and the incidence of nausea and vomiting were recorded. Hypotension was defined as a decrease in systolic arterial pressure to less than 75% of the baseline. In both groups of patients, hypotension was treated promptly with a 5-mg IV bolus of ephedrine repeated every 2 min if hypotension persisted. The sensory level was determined by loss of cold sensation and recorded at 10 min after intrathecal injection. All patients received an infusion of LR solution as maintenance fluid during the anesthetic. Values were reported as mean -t SD, y1 (%o), or as median (range) where appropriate. All statistical tests were performed using program SAS for Windows (SAS Institute Inc., Cary, NC). Statistical significance (P < 0.05) was determined using unpaired Students t-test for comparison of parametric data, and Fishers exact test for comparison of nonparametric categorical data. Repeated-measures analysis of variance was used for comparison of serial blood pressure and heart rate measurements during spinal anesthesia. The paired Students t-test and post-hoc Bonferroni multiple comparisons (using P < 0.01) were used for comparison of hemodynamic changes between baseline and subsequent points.
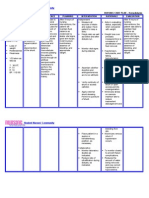
Table
1. Demographic Data and Operative Details
Hetastarch
(n = 19)
Lactated Ringers solution
(n = 21)
Age (yr) Weight (kg) Height (cm) Surgical time (min) Sensory level at 10 min IV fluid during surgery (mL)
Values are mean IV = intravenous. Median (range). L SD.
27.2 + 6.1
61.3 2 4.3 157.1-I 6.1 34.1 + 6.1 T-5 (Tl-7)
567 C 106
27.3 -e 5.2 60.4 + 5.1
156.3t 8.2
32.4 + 5.6
T-6 (T2-8) 565 t 101
+ -a140 -
Hetastarch Lactated Ringers
F E 2 2 h: 120 -
t B 0 m p B I w
100 -
80
I Baselm
I 1 muwte
I
3 mmtes
I
5 mutes
8 mnites
/ 10 mmutes
100 l3 90 3
Figure 1. A, Systolic
Results
Demographic variables, surgical time, intraoperative maintenance fluid and thoracic sensory levels were similar between groups (Table 1). Blood loss during surgery was minimal in all patients. Both groups had similar preinduction systolic blood pressures and heart rates (Figure 1). The incidence of hypotension was significantly greater in the LR solution group than in the hetastarch group (11/21 [52%1
blood pressure and B, heart rate changes at five different time points after spinal anesthesia as compared with the baseline values (mean 2 SD) (Lactated Ringers = lactated Ringers solution).
vs 3/19 [16%1; P < 0.05). There was no difference in the time to hypotension between the hetastarch group and the LR solution group (5 t 2 min and 6 + 3 min, respectively). The episodes of hypotension were transient as they were reversed rapidly by ephedrine. The LR solution group also required significantly more bolus doses of ephedrine (15 vs 4; P < 0.05). Although,
ANESTH ANALG 1997;84:111-14
REGIONAL
ANESTHESIA COLLOID
AND PAIN MANAGEMENT VERSUS CRYSTALLOID DURING
SHARMA SPINAL
ET AL. BLOCK
113
there was no significant difference in the mean systolic blood pressure at each time between the two groups, the two groups were significantly different on average across all times (P < 0.05) (Figure 1). The decrease in systolic blood pressures from baseline to 1 min postanesthesia was significant for the LR solution group (P < O.Ol>, but not for the hetastarch group. In each group, decrease in systolic blood pressures from baseline was significant at 3, 5, 8, and 10 min after spinal anesthesia (P < 0.001) (Figure 1). However, there was no difference in the mean heart rates at each time between the two groups. In each group, change in heart rates from baseline to the five different time points was not significant (Figure 1). There was no difference in the incidence of nausea between the LR solution group and hetastarch group (4/21 [19%1 vs 3/19 [16%1). No patient vomited.
Discussion
Hypotension during spinal anesthesia is the result of sympathetic blockade leading to relative hypovolemia and decreased venous return. The prophylactic administration of crystalloid before regional anesthesia has been considered a safe and effective method of reducing the incidence of hypotension. However, recent reports have suggested that the prophylactic administration of crystalloid is ineffective in eliminating spinal anesthesia-induced hypotension in patients undergoing cesarean section (3,4,6). Since 75% of any crystalloid diffuses into the interstitial space, its efficacy in expanding plasma volume is only transient (11). Although crystalloid administration is safe in most patients, it may be disadvantageous in certain groups, such as those with renal impairment or congestive cardiac failure if infused in large volumes. Excessive crystalloid administration may rarely produce pulmonary and peripheral edema and have little effect on plasma volume. There is evidence to suggest that postpartum patients might be more susceptible to pulmonary edema after the rapid administration of crystalloid, possibly because of an increase in lung water during pregnancy (7). The IV administration of colloid has been shown to be associated with less lung water compared with LR solution (12). Recently, attention has been focused on the prophylactic administration of colloid solutions for the prevention of hypotension during spinal anesthesia. Theoretically, a colloid solution is the more logical choice in preventing hypotension during spinal anesthesia, since it remains in the intravascular compartment for a longer period depending on its physical properties. During cesarean section under spinal anesthesia, LR solution 15 mL/kg with 5% glucose was compared with the same solution containing 5% albumin (8). No
patient given albumin developed significant hypotension, whereas hypotension developed in approximately 30% of patients who received crystalloid. More recently, the prophylactic administration of gelatin was found to be more effective than saline in reducing the incidence of hypotension in a population of patients undergoing transurethral resection of the prostate under spinal anesthesia (9). Hetastarch 6% in 0.9% saline is a synthetic colloid solution with a mean molecular weight of 450,000. The pH of hetastarch is 5.5, the osmolarity is 310 mOsm/L, and the colloid oncotic pressure (34 mm Hg) is similar to that of serum. Its intravascular half-time is 25.5 hours and it has the capacity to expand plasma volume to a volume that is greater than the volume infused (13). Advantages of hetastarch include a lower incidence of anaphylactic reactions as compared to other colloids such as dextran and a better efficacy in preventing venous thrombosis. However, disadvantages related to its use include increased expense, the potential for anaphylactic reactions, and a decreased hemoglobin concentration as well as coagulopathy if infused in excess of 2 L. In recent studies, the administration of hetastarch was found to be superior to LR solution in preventing spinal anesthesia-induced hypotension in patients undergoing cesarean section. Riley et al. (10) demonstrated that the incidence of hypotension during spinal anesthesia for cesarean section was 45% in patients who received hetastarch 500 mL with LR solution 1000 mL versus 85% in those who received only LR solution 1000 mL, and Karinen et al. (14) noted a low incidence of maternal hypotension with hetastarch 500 mL alone (38%) as compared with LR 1000 mL (62%) in patients undergoing cesarean section. However, in both studies the incidence of hypotension during spinal anesthesia with hetastarch administration was only reduced, not completely eliminated. In patients undergoing postpartum tubal ligation the efficacy of hetastarch in reducing the incidence of hypotension has not been demonstrated, and the administration of IV LR solution 15 mL/kg (approximately 1000 mL) before spinal anesthesia has shown to be ineffective in the prevention of hypotension (5). Therefore we chose to compare the efficacy of 1000 mL of LR solution to that of 500 mL of hetastarch in preventing spinal anesthesia-induced hypotension in patients undergoing postpartum tubal ligation. We found that the intravascular administration of 500 mL of hetastarch was associated with a lower incidence of hypotension after spinal anesthesia when compared with 1000 mL of LR solution. Also, the number of ephedrine boluses required to treat hypotension was significantly lower in the hetastarch group. The incidence of hypotension in our study was much lower in both the hetastarch and LR solution groups when compared with the other study comparing hetastarch
114
REGIONAL COLLOID
ANESTHESIA AND VERSUS CRYSTALLOID
PAIN MANAGEMENT DURING SPINAL
SHARMA BLOCK
ET AL.
ANESTH ANALG 1997;84:111-14
with LR solution in preventing spinal anesthesiainduced hypotension (10). This may be explained by the fact that the patient population in our study was nonpregnant. Pregnant patients at term are more prone to develop hypotension due to the occurrence of aortocaval compression by the fetal head and higher level of sympathetic blockade owing to increased spread of local anesthetic in the cerebrospinal fluid. Hypotension was transient and was quickly reversed with ephedrine in our study. The incidence of nausea was very low in both groups and unaffected by the type of fluid administered. The nausea was mostly mild and did not require antiemetics. There was no adverse reaction to hetastarch in this study. In summary, we have found that 500 mL of hetastarch is more effective than 1000 mL of LR solution in preventing hypotension in patients undergoing postpartum tubal ligation under spinal anesthesia. However, the incidence of hypotension was only reduced but not completely eliminated in this study. It is possible that larger volumes of hetastarch might have reduced the incidence of hypotension even further. However, with either type of fluid administration hypotension during spinal anesthesia for tubal ligation was mild and quickly corrected with prompt treatment. Therefore, the routine administration of expensive hetastarch ($50 for 500 mL) compared with LR solution ($1 for 1000 mL) might not be justifiable.
We thank Dr. John Philip for helpful review of the manuscript Richard C. Risser for assisting in statistical analysis. and
References
1. Carpenter RL, Caplan RA, Brown DL, et al. Incidence factors for side effects of spinal anesthesia. Anesthesiology 76:906-16. and risk 1992;
2. McCrae AF, Wildsmith JAW. Prevention and treatment of hypotension during central neural block. Br J Anaesth 1993;70: 672-80. 3. Rout CC, Akoojee SS, Rocke DA, et al. Rapid administration of crystalloid preload does not decrease the incidence of hypotension after spinal anaesthesia for elective Caesarean section. Br J Anaesth 1992;68:394-7. 4. Rout CC, Rocke DA, Levin J, et al. A reevaluation of the role of crystalloid preload in the prevention of hypotension associated with spinal anesthesia for elective cesarean section. Anesthesiology 1993;79:262-9. 5. Gajraj NM, Victory RA, Pace NA, et al. Comparison of an ephedrine infusion with crystalloid administration for prevention of hypotension during spinal anesthesia. Anesth Analg 1993;76:1023-6. 6. Jackson R, Reid JA, Thorburn J. Volume preloading is not essential to prevent spinal-induced hypotension at caesarean section. Br J Anaesth 1995;75:262-5. 7. MacLennan FM, MacDonald AF, Campbell DM. Lung water during the puerperium. Anaesthesia 1987;42:141-7. 8. Mathru M, Rao TLK, Kartha RK, et al. Intravenous albumin administration for prevention of spinal hypotension during cesarean section. Anesth Analg 1980;59:655-8. 9. Baraka AS, Taha SK, Ghabach MB, et al. Intravascular administration of polymerized gelatin versus isotonic saline for prevention of spinal-induced hypotension. Anesth Analg 1994;78: 301-5. 10. Riley ET, Cohen SE, Rubenstein AJ, Flanagan 8. Prevention of hypotension after spinal anesthesia for cesarean section: six percent hetastarch versus lactated Ringers solution. Anesth Analg 1995;81:838-42. 11. Carey JS, Scharsmidt BF, Culliford AT, et al. Hemodynamic effectiveness of colloid and electrolyte solutions for replacement of simulated operative blood loss. Surg Gynecol Obstet 1970; 131:679-86. 12. Wennberg E, Frid I, Haljamae H, et al. Comparison of Ringers acetate with 3% dextran 70 for volume loading before extradural caesarean section. Br J Anaesth 1990;65:654-60. 13. Kroll W, Gerner I, Colombo T, et al. Einfluss von 6% HES 200/0.6-0.66 auf plasmavolumen und blutegerinnung. Infusionstherpie 1992;19:171-80. 14. Karinen J, Rasanen J, Alahuhta S, et al. Effect of crystalloid and colloid preloading on uteroplacental and maternal haemodynamic state during spinal anesthesia for caesarean section. Br J Anaesth 1995;75:531-5.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Tracheal Intubation in Critical Ill Patient PDFDocument8 pagesTracheal Intubation in Critical Ill Patient PDFArdi FkuiPas encore d'évaluation
- Obstetric Postanesthesia Care Unit Stays - Reevaluation of Discharge Criteria After Regional AnesthesiaDocument8 pagesObstetric Postanesthesia Care Unit Stays - Reevaluation of Discharge Criteria After Regional AnesthesiaArdi FkuiPas encore d'évaluation
- Safety Aspects of Postanesthesia Care Unit Discharge Without Motor Function Assessment After Spinal AnesthesiaDocument10 pagesSafety Aspects of Postanesthesia Care Unit Discharge Without Motor Function Assessment After Spinal AnesthesiaArdi FkuiPas encore d'évaluation
- Discharge Times For Knee Arthroscopy in Spinal VsDocument9 pagesDischarge Times For Knee Arthroscopy in Spinal VsArdi FkuiPas encore d'évaluation
- Tracheal Intubation in Critically Ill PatientDocument9 pagesTracheal Intubation in Critically Ill PatientArdi FkuiPas encore d'évaluation
- Tracheal Intubation in Critical Ill PatientDocument8 pagesTracheal Intubation in Critical Ill PatientArdi FkuiPas encore d'évaluation
- Fluid Management in SepsisDocument10 pagesFluid Management in SepsisArdi FkuiPas encore d'évaluation
- PCA in Pediatric PopulationDocument5 pagesPCA in Pediatric PopulationArdi FkuiPas encore d'évaluation
- Tracheal Intubation in Critically Ill PatientDocument9 pagesTracheal Intubation in Critically Ill PatientArdi FkuiPas encore d'évaluation
- Goal-Directed Fluid TherapyDocument9 pagesGoal-Directed Fluid TherapyArdi FkuiPas encore d'évaluation
- v2.0 11+endgültig+12612787 PDFDocument2 pagesv2.0 11+endgültig+12612787 PDFFadil ElbarcaPas encore d'évaluation
- General Principles of Neonatal AnaesthesiaDocument7 pagesGeneral Principles of Neonatal AnaesthesiaArdi FkuiPas encore d'évaluation
- Five Unit Bolus Oxytocin at Cesarean DeliveryDocument7 pagesFive Unit Bolus Oxytocin at Cesarean DeliveryArdi FkuiPas encore d'évaluation
- Fluid Creep PhenomenonDocument9 pagesFluid Creep PhenomenonArdi FkuiPas encore d'évaluation
- Monitoring The Anesthetized PatientDocument6 pagesMonitoring The Anesthetized PatientArdi FkuiPas encore d'évaluation
- Spinal Anaesthesia in Pre-EclampsiaDocument90 pagesSpinal Anaesthesia in Pre-EclampsiaArdi FkuiPas encore d'évaluation
- Preeclampsia Journal2Document12 pagesPreeclampsia Journal2Hieronimus Indra Wira KusumaPas encore d'évaluation
- Ulcer BleedingDocument16 pagesUlcer Bleedingseb2008Pas encore d'évaluation
- Regional Analgesia For Labour Pain ReliefDocument73 pagesRegional Analgesia For Labour Pain ReliefArdi FkuiPas encore d'évaluation
- A Rational Approach To Perioperative Fluid ManagementDocument18 pagesA Rational Approach To Perioperative Fluid ManagementonisarasPas encore d'évaluation
- Intraoperative Fluid TherapyDocument11 pagesIntraoperative Fluid TherapyArdi FkuiPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Vocabulary List - Urdu-400Document59 pagesVocabulary List - Urdu-400Cypto Expert100% (1)
- Case Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D InternDocument35 pagesCase Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D Internsrija vijjapuPas encore d'évaluation
- Amlodipine Drug StudyDocument8 pagesAmlodipine Drug StudyChamCham Aquino75% (4)
- Auspar Sacubitril Valsartan Salt Complex 160923 PiDocument27 pagesAuspar Sacubitril Valsartan Salt Complex 160923 PiMayson BaliPas encore d'évaluation
- Pharmacology Body SystemsDocument159 pagesPharmacology Body SystemsHezielErispeTaligatosPas encore d'évaluation
- Deficient Fluid Volume - Nursing Diagnosis & Care PlanDocument9 pagesDeficient Fluid Volume - Nursing Diagnosis & Care PlanEricsonMitraPas encore d'évaluation
- SyncopeDocument44 pagesSyncopeSap ModulesPas encore d'évaluation
- ACLS DrugsDocument16 pagesACLS Drugstostc100% (2)
- Clinical Pearls in NephrologyDocument5 pagesClinical Pearls in NephrologyEdmilson R. LimaPas encore d'évaluation
- Gunshot WoundDocument57 pagesGunshot Woundnecrophilia090407Pas encore d'évaluation
- Pharm Exam AgianDocument7 pagesPharm Exam AgianyalahopaPas encore d'évaluation
- Head Injury in Pregnancy PDFDocument26 pagesHead Injury in Pregnancy PDFarif_tampan87Pas encore d'évaluation
- Atls Questions and AnswersDocument14 pagesAtls Questions and Answersahmad7mahmoud-1Pas encore d'évaluation
- ATLS 9th Pre-Test 1 - 1Document12 pagesATLS 9th Pre-Test 1 - 1a.e.noushiPas encore d'évaluation
- Pharmacology - Drug Cards (Index Cards)Document272 pagesPharmacology - Drug Cards (Index Cards)Henrietta100% (9)
- Health Assessment Handout 2Document15 pagesHealth Assessment Handout 2ApRil Anne BalanonPas encore d'évaluation
- Orthostatic Hypotension Medical StudentsDocument21 pagesOrthostatic Hypotension Medical StudentsRobMarvinPas encore d'évaluation
- The Effects of Prophylactic Bolus Phenylephrine On Hypotension During Low-Dose Spinal Anesthesia For Cesarean SectionDocument6 pagesThe Effects of Prophylactic Bolus Phenylephrine On Hypotension During Low-Dose Spinal Anesthesia For Cesarean SectionAgus GunardiPas encore d'évaluation
- Workflow of AnesthesiologyDocument2 pagesWorkflow of AnesthesiologyDeng PanPas encore d'évaluation
- Case Scenario - Week 4 - Group 2Document34 pagesCase Scenario - Week 4 - Group 2Angel Hannah100% (1)
- Medication CardsDocument65 pagesMedication CardsMovaliya Ghanshyam80% (5)
- Assisiting Patient To Sit On The Edge of The Bed (DANGLING)Document2 pagesAssisiting Patient To Sit On The Edge of The Bed (DANGLING)Bulajyo Pangngay JolinaPas encore d'évaluation
- Drugs Influence The Peripheral Nervous System: Cholinomimetics. Cholinesterase InhibitorsDocument23 pagesDrugs Influence The Peripheral Nervous System: Cholinomimetics. Cholinesterase Inhibitorslayla kambalaPas encore d'évaluation
- HemodialysisDocument2 pagesHemodialysisRA Ferrer de RomaPas encore d'évaluation
- Insulin Drug StudyDocument6 pagesInsulin Drug StudyRoland YustePas encore d'évaluation
- Blood Loss and Clinical SignsDocument10 pagesBlood Loss and Clinical SignsElias Emmanuel JaimePas encore d'évaluation
- Patofisiologi Syok Hemoragik PDFDocument30 pagesPatofisiologi Syok Hemoragik PDFjsagayPas encore d'évaluation
- Am J Crit Care 2012 Halm 449 52Document5 pagesAm J Crit Care 2012 Halm 449 52Fikri Ulil AlbabPas encore d'évaluation
- Capillary Refill TimeDocument5 pagesCapillary Refill TimeMamata BeheraPas encore d'évaluation
- The Medical Treatment of Cardiogenic Shock: Cardiovascular DrugsDocument7 pagesThe Medical Treatment of Cardiogenic Shock: Cardiovascular DrugsCarlos QuirogaPas encore d'évaluation