Académique Documents
Professionnel Documents
Culture Documents
Abortion
Transféré par
Gabriella ChafrinaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Abortion
Transféré par
Gabriella ChafrinaDroits d'auteur :
Formats disponibles
ABORTION |Tutorial F-4
Definition Termination of pregnancy by any means (either spontaneously or intentionally) before the fetus is sufficiently developed by survive Termination of pregnancy before 20 weeks gestation or less than 500 g birth weight (conventional)
A) Spontaneous Abortion
Definition When abortion occurs without medical or mechanical means to empty the uterus, another widely used term is miscarriage Pathology Early Abortion Hemorrhage into the decidua basalis followed by necrotic of tissues adjacent to the bleeding The ovum becomes detached Stimulates uterine contractions Result in expulsion Blood or carneous mole => an ovum that is surrounded by a capsule of clotted blood, the capsule is of varying thickness with degenerated chorionic villi scattered through it Later Abortion Several outcomes: (the retained fetus may undergo maceration) The bones of the skull collapse The abdomen becomes distended with blood-stained fluid The skin softens and peels off in utero or at the slightest touch, leaving behind the corium Internal organs degenerate and undergo necrosis Amniotic fluid may be absorbed when the fetus becomes compressed upon itself and desiccated to form a fetus compressus Occasionally, the fetus eventually becomes so dry and compressed that it resembles parchment => fetus papyraceous Etiology The risk of spontaneous abortion increases with parity, maternal, and paternal age The exact mechanisms are not always apparent In the first trimester, spontaneous expulsion of the ovum is nearly always preceded by death of the embryo or fetus => etiological considerations of early abortion involve ascertaining whenever possible the cause of fetal death In the subsequent months, the fetus frequently does not die in utero before expulsion, and othe explanations for its expulsion must be invoked
A. Fetal Factors
1. Abnormal Zygotic Development The most common morphological finding in early spontaneous abortions is an abnormality of development of the zygote, embryo, early fetus, or at times the placenta
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
2. Aneuploid Abortion Chromosomal abnormalities are common among embryos and early fetuses that are aborted spontaneously Autosomal trisomy The most frequently trisomies, can be result of an isolated nondisjunction, maternal or paternal balanced translocation, or balanced chromosomal inversion Monosomy X (45, X) The second most common, autosomal monosomy is rare and incompatible with life Triploidy Is often associated with hydropic placental degeneration Tetraploid Rarely live born and are most often aborted very early in gestation Chromosomal Structural Abnormalities Unusual causes of abortion, some of these infants are live born with balanced translocations can be normal Sex chromosomal polysomy (47, XXX or 47, XXY) Unusual in abortus material but is commonly seen in live births 3. Euploid Abortion Euploid fetus tend to abort later is gestation than anuploid Incidence of euploid abortions increases dramatically after the maternal age of 35 years The reasons for euploid abortions are generally unknown, but the following are possibilities: 1. A genetic abnormality such as an isolated mutation or polygenic factors 2. Various maternal factors 3. Possibly some paternal factors
B. Maternal Factors
1. Infections Some chronic infections have been implicated in causing abortion => uncommon cause 2. Chronic Debilitating Disease In early pregnancy, chronic wasting diseases (such as tuberculosis or carcinomatosis) have seldom caused abortion. Celiac sprue has been reported to cause both male and female infertility and recurrent abortions 3. Endocrine Abnormalities Hypothyroidism Iodine deficiency may be associated with excessive miscarriages. There done appear to be an increased incidence if abortion with clinical hypothyroidism Diabetes Mellitus (insulin-dependent diabetes) Poor glucose control resulted in a market increase in the abortion rate Progesterone Deficiency Insufficient progesterone secretion by the corpus luteum or placenta (luteal phase defect), Insufficient progesterone production usually the consequence rather than the cause of early pregnancy failure
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
4. Nutrition There is no conclusive evidence that dietary deficiency of any one nutrient or moderate deficiency of all nutrients is an important cause of abortion 5. Drug Use and Environment Factors Tobacco Increased risk for euploidic abortions, women who smoked more than 14 cigarettes a day, the risk was approximately two fold compared with controls Alcohol Frequent alcohol use during the first 8 weeks of pregnancy have been associated with spontaneous abortion and fetal The abortion rate was doubled in women drinking twice weekly and tripled in women who consumed alcohol daily compared with nondrinkers Caffeine (paraxanthine) Coffee consumption at greater than 5 cups per day (equivalent to 500mg caffeine) => the risk appears to increase with increasing amounts Radiation In sufficient doses Contraceptives Intrauterine devices are associated with an increased incidence of septic abortion after contraceptive failure Environmental Toxins There was an increased risk of spontaneous abortion for women occupationally exposed to anesthetic gases, dental assistants exposed to 3 or more hours of nitrous oxide in offices without scavenging equipment Arsenic, lead, formaldehyde, benzene, and ethylene oxide may cause abortion 6. Immunological Factors Two primary pathophysiological models are the autoimmune theory (immunity against self) and the alloimmune theory (immunity against another person) Autoimmune factors Antiphospholipid antibodies have been implicated in spontaneous abortion Antiphospholipid antibodies => family of antibodies that bind to a negatively charged phospholipids, phospholipid-binding proteins, or a combination of the 2 Antiphospholipid antibodies: lupus anticoagulant, antiocardiolipin antibody, IgG, IgA, IgM The mechanism of pregnancy loss involves placental thrombosis and infarction Antibodies inhibit prostacyclin (a potent vasodilator and inhibitor of platelet aggregation) release Platelets produce thromboxane A2 (a vasoconstrictor and platelet aggregator) Reduce prostacyclin production Facilitating a thromboxane dominant milieu Leads to thrombosis In addition, antibody inhibits protein C activation
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
Treatment: low-dose aspirin alone, combination of heparin and low dose aspirin, prednisone, and intravenous immunoglobulin Treatments begin when pregnancy is diagnosed, is continued until labor or delivery Alloimmune factors Diagnosis of an alloimmune factor has centered on several tests: 1. Maternal or paternal HLA comparison 2. Assessment of maternal serum for the presence of cytotoxic antibodies to paternal leukocytes 3. Maternal serum testing for blocking factors for maternal-paternal mixed lymphocyte reactions The diagnosis determined to have significant HLA-type homology, or in which the women were found to have minimal antipaternal antibodies => judged to represent an alloimmune disorder Treatment: paternal cell immunization, third-party donor leukocytes, throphoblast membrane, and IV Ig 7. Inherited Thrombophilia Several genetic disorders of blood coagulation (factor V Leiden mutation) may increase the risk of thrombosis) Treatment: - Heparin (including low molecular weight heparin) for treatment of antithrombin III deficiency, protein C, and S deficiency - Aspirin plus heparin for treatment of factor V Leiden mutation and antiphospholipid syndrome 8. Laparotomy No evidence that surgery performed during early pregnancy causes increased abortions 9. Physical Trauma Major abdominal trauma can precipitate abortion but general trauma contributes minimally to abortion 10. Uterine Defects Acquired uterine defects Uterine leiomyomas are associated with abortion with their location than their size and amount Uterine synechiae (Asherman syndrome) are caused by destruction of large areas of endometrium by curettage => results in amenorrhea and recurrent abortions because of insufficient endometrium to support implantation Treatment: - Ahesiolysis via hysteroscopy and placement of an intrauterine contraceptive device to prevent recurrence - Continous high-dose estrogen therapy 60 to 90 days following adhesiolysis Developmental uterine defects Defects are the consequence of abnormal mullerian duct formation of fusion (occurs spontaneously or induced by in utero exposure to diethylstilbestrol) Treatment: corrective procedures
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
11. Incompetent Cervix Characterized by painless cervical dilation in the second trimester with prolapse and ballooning of membranes into the vagina, followed by rupture of membranes and expulsion of an immature fetus Etiology 1. Previous trauma to the cervix: - Dilatation and curettage - Conization - Cauterization - Amputation 2. Abnormal cervical development (exposure to diethylstilbestrol in utero) Treatment The treatment of cervical incompetence is cerclage (surgically reinforce the weak cervix by some type of purse-string suturing) Contraindication of cerclage: bleeding, uterine contractions, or ruptured membranes Preoperative Evaluation Sonography to confirm a living fetus and to exclude major fetal anomalies should precede cerclage Cervical specimens are tested, if positive cervical infections, treatment is given Cerclage may be performed prophylactically before cervical dilatation, or emergently after the cervix has dilated Cerclage is performed between 12 and 16 weeks The more advanced the pregnancy, the more likely surgical interventions will stimulate preterm labor or membrane rupture => after midpregnancy prefer bed rest rather than cerclage, do not perform cerclage after 23 to 26 weeks If cerclage is performed, the woman may be advised to decreased physical activity and abstain from intercourse (a week before and after surgery) Cervical examinations are performed each week or every two weeks to asses cervical effacement and dilatation Cerclage Procedures Two types of vaginal operations are commonly used during pregnancy: - First, the simple procedure recommended by McDonald - Second, is the more complicated Shirodkar operation (modification of the original procedure described by Shirodkar) The modified Shirodkar procedure is often reserved for previous McDonald cerclage failures and structural cervical abnormalities Success rates are higher when cervical dilatation was minimal and membrane prolapse was absent Transabdominal cerclage => the suture placed at the level of the uterine isthmus is used in some cases of severe anatomical defects af the cervix or cases of prior transvaginal cerclage failure Complications 1. Infection => much less frequent when cerclage was performed by 18 weeks 2. Membrane rupture, chorioamnionitis, and intrauterine infection => if cerclage is performed after 20 weeks
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
C. Paternal Factors
Little is known about paternal factors in the genesis of spontaneous abortion Certainly, chromosomal translocations in sperm can lead to abortion
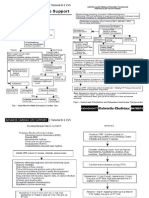
Categories of Spontaneous Abortion
A. Threatened Abortion
Clinical Diagnosis: - Bloody vaginal discharge (spotting) or bleeding through a closed cervical os may persist for days or weeks (during the first half or pregnancy) - Cramping abdominal pain (anterior and rhythmic) - Persistent low backache - Dull, midline, suprapubic discomfort Even without abortion, fetus are at increased risk for preterm delivery, low birthweight, and perinatal death Therapy: bed rest and analgesia to help relieve the pain Vaginal sonography (fetal sac can usually be seen between 33 and 35 days form the last menstrual period), serial serum quantitative hCG levels, and serum progesterone values, measured alone or in various combinations can help ascertain in fetus is alive and its location Ectopic pregnancy should always be considered in the differential diagnosis of threatened abortion Women who are D negative with a threatened abortion probably should receive anti-D immunoglobulin
B. Inevitable Abortion
Clinical diagnosis: - Moderate effacement of the cervix - Cervical dilatation greater than 3 cm - Rupture of the membrane - Bleeding for more than 7 days - Persistent of cramps despite narcotic analgesics - Other signs of termination of pregnancy (e.g: partial extrusion of products of conception)
C. Complete and Incomplete Abortion Complete Abortion
- Complete detachment of placenta and expulsion of the conceptus - Internal cervical os closed - Cessation of pain and termination of risk bleeding Incomplete Abortion - Incomplete detachment of placenta and expulsion of the conceptus - Internal cervical os remains open - Persistent bleeding and cramping, patulous cervix, enlarge uterus
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
D. Missed Abortion
Uterus retains dead products of conception behind a closed cervical os for days or even weeks Clinical diagnosis: - Loss of symptoms of pregnancy - Decrease in uterine size - Embryo or fetus has succumbed - Pain or tenderness in unusual - Brownish vaginal discharge - Cervix remains closed and firm - No adnexal abnormality
E. Recurrent Abortion
Three or more consecutive spontaneous abortions Two types of test as having a clear value in the investigation of recurrent miscarriage: - Parental cytogenetic analysis - Lupus anticoagulant and anticardiolipin antibodies assays
B) Induced Abortion
Definition The medical or surgical termination of pregnancy before the time of fetal viability Indications Disease that commonly lead to the operation: - Persistent heart disease after previous cardiac decompensation - Advanced hypertensive vascular disease - Invasive carcinoma of the cervix When continuation of pregnancy may threaten the life of the women or seriously impair her health When pregnancy has resulted from rape or incest When continuation of pregnancy is likely to result in the birth of a child with severe physical deformities or mental retardation
A. Elective (Voluntary) Abortion
The interruption of pregnancy before viability at the request of the women but not for reasons of impaired maternal health or fetal disease Abortion techniques: Surgical techniques a) Cervical dilatation followed by uterine evacuation - Curettage (sharp and suction curettage) -> before 14 to 15 weeks - Dilatation and evacuation (D&E) -> at 16 weeks - Dilatation and extraction (D&X) b) Menstrual aspiration c) Laparotomy
130110110177 | Gabriella Chafrina| 09/04/12
ABORTION |Tutorial F-4
Medical techniques a) Intravenous oxytocin b) Intra-amnionic hyperosmotic fluid (20% saline, 30% urea) c) Prostaglandin E2, F2, E1, and analogues - Intra-amniotic injection - Extraovular injection - Vaginal insertion - Parenteral injection - Oral ingestion d) Antiprogesterones mifepristone and epostane e) Methotrexate intramuscular and oral f) Various combinations of the above Consequences of Elective Abortion - Maternal mortality - Impact on future pregnancy Fertility does not appear to be diminished by an elective abortion, except infrequently as a consequence of infection - Septic abortion Septic hemorrhage, sepsis, bacterial shock, acute renal failure, uterine infection Resumption of Ovulation after Abortion Ovulation may resume as early as 2 weeks after an abortion
130110110177 | Gabriella Chafrina| 09/04/12
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Life Style Wellness Coaching PDFDocument275 pagesLife Style Wellness Coaching PDFSundar Prabhu71% (7)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Emr408 A2 KL MarkedDocument21 pagesEmr408 A2 KL Markedapi-547396509Pas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Security & Safety Hand BookDocument110 pagesSecurity & Safety Hand BookIts Mind's Eye100% (22)
- Foreign Body EarDocument34 pagesForeign Body EarGabriella ChafrinaPas encore d'évaluation
- Chapter 27 GuytonDocument6 pagesChapter 27 GuytonGabriella ChafrinaPas encore d'évaluation
- Sehatvan Fellowship ProgramDocument8 pagesSehatvan Fellowship ProgramShivam KumarPas encore d'évaluation
- Relapse PreventionDocument10 pagesRelapse PreventionDawn FarmPas encore d'évaluation
- Pathogenesis of LeprosyDocument13 pagesPathogenesis of LeprosyNurul AinPas encore d'évaluation
- Cvs4-Clinical Aspects of Serum Cholesterol LevelDocument2 pagesCvs4-Clinical Aspects of Serum Cholesterol LevelGabriella ChafrinaPas encore d'évaluation
- RS7 InfluenzaDocument6 pagesRS7 InfluenzaGabriella ChafrinaPas encore d'évaluation
- Rs4-Gas Exchange and TransportDocument5 pagesRs4-Gas Exchange and TransportGabriella ChafrinaPas encore d'évaluation
- GUS4 Antihypertensive DrugsDocument7 pagesGUS4 Antihypertensive DrugsGabriella ChafrinaPas encore d'évaluation
- Group A Β-Hemolytic Streptococcus: - Tutorial B-1 RSDocument2 pagesGroup A Β-Hemolytic Streptococcus: - Tutorial B-1 RSGabriella ChafrinaPas encore d'évaluation
- Tutorial D-1 CVS: Advance Cardiac Life SupportDocument4 pagesTutorial D-1 CVS: Advance Cardiac Life SupportGabriella ChafrinaPas encore d'évaluation
- Deep Vein Thrombosis (DVT) : - Tutorial D-1 CVSDocument1 pageDeep Vein Thrombosis (DVT) : - Tutorial D-1 CVSGabriella ChafrinaPas encore d'évaluation
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaPas encore d'évaluation
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaPas encore d'évaluation
- Advance Life Support (Resuscitation Council (Uk) 2000) : - Tutorial D-1 CVSDocument1 pageAdvance Life Support (Resuscitation Council (Uk) 2000) : - Tutorial D-1 CVSGabriella ChafrinaPas encore d'évaluation
- Advance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSDocument1 pageAdvance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSGabriella ChafrinaPas encore d'évaluation
- Cvs4-Clinical Aspects of Serum Cholesterol LevelDocument2 pagesCvs4-Clinical Aspects of Serum Cholesterol LevelGabriella ChafrinaPas encore d'évaluation
- Leptospirosis WHODocument122 pagesLeptospirosis WHOabhinaya2006100% (1)
- Iodine Deficiency Disorders (IDD) and Congenital HypothyroidDocument44 pagesIodine Deficiency Disorders (IDD) and Congenital HypothyroidGabriella ChafrinaPas encore d'évaluation
- 4th Year MBBS Batches & GroupsDocument2 pages4th Year MBBS Batches & GroupsSohail Abbas KhanPas encore d'évaluation
- Drug Ana Surgery WardDocument11 pagesDrug Ana Surgery WardJames QuilingPas encore d'évaluation
- Deep Sleep ExperimentsDocument12 pagesDeep Sleep ExperimentsCristina Lemoing100% (1)
- Can Cognitive Therapy Be Conducted by Computers. Eells, Barrett, Wrigh, ThaseDocument7 pagesCan Cognitive Therapy Be Conducted by Computers. Eells, Barrett, Wrigh, ThaseAylin Lidsay Feria GPas encore d'évaluation
- List of Private Hospitals and Diagnostic Centers Approved by INSADocument16 pagesList of Private Hospitals and Diagnostic Centers Approved by INSAvijay sainiPas encore d'évaluation
- Hearing Loss in Adults Assessment and Management PDF 1837761878725 PDFDocument20 pagesHearing Loss in Adults Assessment and Management PDF 1837761878725 PDFxtinePas encore d'évaluation
- Msds - AdditiveDocument9 pagesMsds - AdditivedanalabPas encore d'évaluation
- SCI - Learning Packet - Biology Week 5Document13 pagesSCI - Learning Packet - Biology Week 5Pal, Julia HannePas encore d'évaluation
- MLP Registration FormDocument6 pagesMLP Registration FormDoll JonesPas encore d'évaluation
- Chest Physiotherapy ReportDocument8 pagesChest Physiotherapy ReportPatricia G ChiuPas encore d'évaluation
- Kitir Proposal Penelitian 2014 SIDocument32 pagesKitir Proposal Penelitian 2014 SIclarazettiraPas encore d'évaluation
- Evolution of Spaces With Respect To Child PsychologyDocument28 pagesEvolution of Spaces With Respect To Child PsychologyDevvrat ChowdharyPas encore d'évaluation
- MastoiditisDocument3 pagesMastoiditisPrincess GyasiPas encore d'évaluation
- Puskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraDocument6 pagesPuskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraicaPas encore d'évaluation
- 3390 3396 PDFDocument7 pages3390 3396 PDFXavier Alexandro Ríos SalinasPas encore d'évaluation
- Ncezid FRM Pass Attest Eng 508Document5 pagesNcezid FRM Pass Attest Eng 508GO STUDY ABROAD OFFICIALPas encore d'évaluation
- NHS Change ManagementDocument20 pagesNHS Change ManagementMary NjeriPas encore d'évaluation
- Reva Rubin Dan Ramona MercerDocument8 pagesReva Rubin Dan Ramona MercerFifi FruitasariPas encore d'évaluation
- Literature Review On UTIDocument31 pagesLiterature Review On UTINishchal Dhakal0% (1)
- Drug Study: Phinma University of PangasinanDocument1 pageDrug Study: Phinma University of PangasinanVoid LessPas encore d'évaluation
- Exercise Science Honours 2016Document22 pagesExercise Science Honours 2016asdgffdPas encore d'évaluation
- Introduction of Air Ambulance Services in IndiaDocument5 pagesIntroduction of Air Ambulance Services in Indiaprithvinatarajan100% (1)
- Power of Plants 1Document14 pagesPower of Plants 1api-399048965Pas encore d'évaluation
- Drug Formulary HospitalDocument98 pagesDrug Formulary HospitalahmshmPas encore d'évaluation
- Surgery KGMU Proff Chapterwise by Arif Naseem 2009-2021Document4 pagesSurgery KGMU Proff Chapterwise by Arif Naseem 2009-2021DR. PARDEEP SHARMAPas encore d'évaluation