Académique Documents
Professionnel Documents
Culture Documents
Neuro Study Guide
Transféré par
NursingSchoolNotesDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Neuro Study Guide
Transféré par
NursingSchoolNotesDroits d'auteur :
Formats disponibles
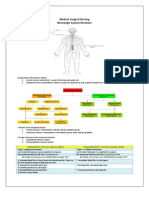
Neurological Study Guide. Neurotransmitters: 1. Chemicals that cross synaptic cleft a. dopamine b. serotonin c. norepinephrine d. GABA e.
Enkephalin, endorphin \ Anatomy of Brain: 1. Cerebrum: higher thought, two hemispheres a. Corpus callosum: nerve fibers that connect the two hemispheres b. four lobes: Frontal: concentration, abstract thought, motor function Parietal: sensory, pain, touch, temperature Temporal: auditory, sensory and speech Occipital: visual 2. Brain Stem: a. midbrain: relay station b. pons: respirations c. medulla: HR, respirations, blood vessel diameter, sneezing, swallowing, vomiting 3. cerebellum: motor function, balance 4. basal ganglia,: asssits cerbral cortex in smooth voluntary movement 5. thalamus: emotions, relay station to other areas of body 6. hypothalamus: regulations of body temp, sleep wake- cycles ect, considered master gland Spinal cord: carries messages from brain to rest of body, 1 st cervical to 2nd lumbar vertebra Afferent fibers: sensory Efferent: motor Structures protecting the brain: 1. Skull 2. Meninges 3. Cerebrospinal fluid: normal pressure is 60 to 180 mmH2O Cerebral circulation: 1. Arteries: 2 internal carotid, 2 vertebral 2. Veins: do not have valves Autonomic Nervous system 1. cardiac, smooth muscle 2. involuntary functions 3. parasympathetic and sympathetic nervous system sympathetic: fight or flight parasympathetic: visceral function, maintains homeostasis Diagnostic Tests: Skull and spinal x ray: bone information such as fractures, dislocation, compressions ect. a. maintaining immobilzation is important when dealing with these injuries!! CT: can be with or without dye, a. detects intracranial bleeding, cerebral edema, infarctions, hydrocephalus, shifts of brain structures b. pre procedure: need informed consent if using dye! c. monitor for allergies for shellfish, iodine (if using dye) d. hold metformin (if using dye) to limit renal damage, need current BUN and creatinine
MRI: Ids tumors and vascular abnormalities, similar to CT but does not need dye a. no metal b. no MRIs on pacemakers ect. c. claustrophobia an issue Lumbar puncture: a. insertion through L3 - L4 b. used to take sample of CSF c. contraindicated with clients with increased intracranial pressure d. empty bladder before e. knee chest position during procedure f. complication is headache due to loss of CSF, must call physician Meylogram: injection of dye or air into subarachnoid space to detect abnormalities of spinal cord and vertebrae, (not used as much due to the use of CT and MRI) ..true dat. a. #1 complication is headache due to loss of CSF similar to lumbar puncture Cerebral Angiography: perfusion study, such as aneurisms EEG: graphic recording of electrical activity a. need to hold stimulants, anticonvulsants, antidepressants ect before procedure
Neurological Assessment:
1. Subjective data: loss of consciousness, dizziness, fainting, numbness, ect., H/A, convulsions 2. mental status a. observation of patient b. asking questions c. objective data: posture, gait, motor movements, dress, hygiene, facial expressions d. mood, thought process, level of consciousness e. length of concentration f. memory g. abstract reasoning, sound judgments ect. 3. Cranial Nerves: I Olfactory: hold scent under nostril II Optic: eye chart III Oculomotor: follow finger, eye movement IV Trochlear: eye movement V Trigeminal: sensory function, light versus sharp touch VI Abducens: eye movement VII Facial: sensory and motor function of face, VIII Acoustic: whisper test IX Glossopharyngeal: say ah X Vagus XI Spinal acessory: shrug shoulders XII Hypoglossal: protude tongue. 4. Cerebellar function 5. Motor assessment: muscle size, tone, movement ect. 6. reflexes Decorticate: flexion in response to pain Decerebrate: extension in response to pain Glasgow coma: score between 1 - 15. score of 8 coma is present (probably needs intubation) a. eye opening b. verbal c. best motor response Respirations: Cheyne-Stokes: periods of apnea Neurogenic hyperventilation: rapid and deep sustaining respirations, dysfunction of midbrain and middle
pons Apneustic: irregular respirations with pauses at end of inspiration and expiration Ataxic: irregular
Altered Level of consciousness
1. Signs and symptoms: a. decreased alertness, decreased consciousness, change in pupils/eye opening, subtle behavior changes b. early sign and symptoms: restlessness and anxiety. 2. complications: a. respiratory failure b. pneumonia c. pressure ulcers d. aspiration 3. medical management: a. airway b. breathing c. circulation d. nutrition 4. 1859! risk for injury is one of the most common nursing diagnosis with altered level of consciousness
Increased intracranial pressure
Caused: Head injury, brain tumors, toxic and viral encephalopathies, subarachnoid hemorrhage earliest sign of ICP is change in LOC Patho: 1. increased ICP leads to decreased cerebral perfusion 2. leads to ischemia and cell death which stimulates further edema 3. shifting of brain tissue 4. herniation 5. death. this is bad. complications: 1. brain stem herniation a. cushings triad: rise in BP with widening pulse pressure, bradycardia, decrease respirations 2. diabetes insipidus: from pressure on the pituitary gland, lack of antidiuretic hormone. 3. syndrome of inappropriate antidiuretic hormone: too much antidiuretic hormone, sodium goes down to due hemodilution Normal CPP is 70 to 100 mmHG, intracranial pressure 0-10 mmHG CPP: MAP - ICP, (cerebral profusion pressure: mean arterial pressure minus ICP) MAP: systolic BP + (2 x diastolic BP)/3 Management of ICP: 1. osmotic diuretics (mannitol) 2. corticosteroids (dexamethasone) 3. fluid restriction 4. hypothermia 5. reduce CSF and intracranial blood volume a. ventriculostomy drain b. hyperventilation will result in vasoconstriction (this reduces ICP) 6. Control temperature a. antipyretic meds b. cooling blanket c. a shivering patient will have increased ICP
7. reduce metabolic demands a. barbiturates: pentobarbital b. paralyzing agents: pavulon c. sedation: diprivan d. analgesia: fentanyl Intracranial surgery: 1. craniotomy: surgical opening of the skull a. to relieve ICP b. evacuate blood clot c. control hemorrhage d. remove a tumor 2. transphenoidal: mouth and nasal sinus to gain access to pituitary glands 3. Burr holes; exploration or diagnosing, evacuate hematoma or abscess 4. craniectomy: removal of portion of skull 5. cranioplasty: repair of cranial defect Preoperative management: 1. antiseizure meds: dilantin, cerebx 2. Corticosteroids 3. fluid restrictions mannitol 4. antibiotics: 5. anxiolytic
Head, Brain, and Spinal cord injuries
1. Primary Injury: injury done to brain from a traumatic event ( initial damage to brain) 2. Secondary injury: damage that evolves, hours to days, that is primarily due to brain swelling or ongoing bleeding. example: ICP Types of Head injuries: 1. Scalp: highly vascular. Abrasion, contusion, laceration, hemotoma 2. Skull Fracture: a. linear: along the fissure b. communiuted: bone fragment, shattering c. Depressed: caved in d. Basilar: base of skull around the ears Signs and symptoms of basilar fracture: Hemorrhage Battles sign: bleeding over mastoid bone, indicative of basilar fracture CSF otorrhea: blood coming out of ear CSF rhinorrhea: blood coming out of nose Halo sign: stain on the pillow from CSF leakage 3. Diagnostic test: CT, MRI, Cerebral angiography 4. S/S of head injury in general: a. altered LOC b. pupil abnormalities c. absent gag reflex d. changes in vital signs 5. Medical management: a. close observation b. surgery
Brain Injury:
1. Closed (blunt) brain injury: head accelerates and rapidly decelerates and collides with another object 2. Open brain injury: objects penetrates the skull, and damages the soft brain tissue
Types of brain injury: 1. Concussion: temporary loss of function with no apparent structural change a. if frontal lobe is affected: bizarre behavior b. temporal: amnesia 2. Contusion a. unconscious for more than a few seconds or minutes b. involuntary evacuation of bowels and bladder c. shallow respirations, cool pale skin d. B/P and temp subnormal e. abnormal eye movement f. body functions will eventually return to normal g. full recovery days to months h. vertigo, seizures, residual h/a are common 3. Diffuse axon injury a. widespread damage to axons in the cerebral hemispheres, corpus callosum, and brain stem b. mild to sever head trauma: axonal swelling and disconnection c. severe, no lucid intervals and experiences immediate coma, decorticate and decerebrate posturing, global cerebral edema d. diagnosis: clinical signs plus CT or MRI e. recovery depends on the severity of the axonal injury 4. Intracranial Hemorrhage: collection of blood, most serious brain injury a. epidural: arterial blood between skull and dura, S/S: loss of consciousness, an apparent recovery, then sudden signs of compression b. Subdural; collection of blood between dura and the brain, can be acute and chronic, elderly and alcoholics more susceptible, number one symptom: change in LOC c. Intracerebral: bleeding into the substance of the brain: force is exerted to the head over a small area (bullet wound), systemic HTN, saccular aneruysm, vascular anomalies. Management if mostly dealing with ICP and supportive care. 5. Management of brain injuries a. all treatment is towars preserving brain homeostasis and preventing secondary injury b. cerebral edema, B/P, respirations, electrolyte imbalance, anti-hypertensives, head of bed 30-45 degrees, diuretics
Spinal Cord Injury
Facts: 1. 4x more in males 2. 16 - 30 3. African American more than caucasians 4. 35% MVA, 30% violence, 19% falls Patho: 1. Transient concussion: usually 100 percent recovery 2. Contusion 3. Laceration 4. Compression 5. Transection: complete cutting of cord Catagories: 1. Primary: initial trauma 2. Secondary: contusion or tear injury after the initial injury Emergency Management: 1. rapid assessment 2. Immobilization 3. extrication (from vehicle if possible)
4. Stabilization 5. Transportation to close location Management of acute phase: 1. Goal is prevent secondary injury 2. high dose of coritcosteroids ASAP 3. O2 therapy, keeps sats high to oxygenate cord 4. Blood transfusions 5. Respiratory therapy: a. dont bend neck to intubate 6. Skeletal fracture reduction and traction Complications: pg 1938 1. Spinal shock and neurogenic shock: develops due to loss of autonomic innervations below area of injury a. the higher the injury on the spinal cord results in more areas that are affected 2. Respirations: especially the higher spinal cord injuries a. decreased vital capacity b. retention of secretions c. increased CO2 levels d. decreased O2 levels e. respiratory failure f. pulmonary edema 3. DVTs: increased risk for blood clots 4. Autonomic dysflexia a. S/S: headache, profound sweating, nasal congestion, bradycardia, HTN, urinary retention b. considered acute emergency from exaggerated autonomic responses to normal stimuli c. occurs after spinal shock is resolved d. triggered by: distended bladder, bowel distention, distention or contraction of visceral organs, simulation of skin (break in skin, rash ect.) e. need to remove triggering stimulus to avoid serious complications (check bladder first) f. put in high fowlers to lower BP
Oncologic disorders of the brain:
1. Primary Brain tumors a. localized lesion that occupies space with the skull b. Shape; spherical mass and grow diffusely and infiltrate tissue c. pathphysiological events d. Origination: often unknown, ionizing radiation, increased ICP 2. Types: a. Gliomas: most common type, can infiltrate any portion of brain, spreads by infiltrating into surrounding neural connective tissue, most deadly, cannot be completely removed b. Angiomas: 83% occur in cerebellum, masses composed largely of abnormal blood vessels, increased risk for CVA, c. Meningiomas: on cover of brain, benign encapsulatd on meninges, can be removed d. Acoustic neuromas: on cranial nerves, grow very slowly, often balance problems, e. Pituitary adenomas: on pituitary, can have pressure effects such as vision or headaches and hormonal effects form the gland itself. Clinical Manifestations: 1. Increased ICP reflect symptoms a. headache b. vomiting c. visual disturbances d. hemiparesis e. seizures f. mental status changes g. personality changes
2. the symptoms you may if the tumor is in the: a. occipital lobe: loss of vision on opposite side of tumor b. cerebellum: dizziness, ataxia, staggering, gait, muscle incoordination d. frontal lobe: higher level thinkingyou may think you have one right now for example after reading 7 pages of this Diagnostics: CT, MRI, PET, EEG, CSF (MRI the most helpful) Medical management: 1. chemo 2. radiation 3. brachytherapy: inplanted radiation into system 4. bone marrow transplant 5. corticosteroids
Cerebral Aneurysm:
1. def: Dilation of the walls of the cerebral artery, often resulting from a weakness in arterial wall. a. usually occurs around circle of willis 2. cause: a. atherosclerosis b. congential defect of vessel wall c. hypertensive vascular disease d. head trauma e. age f. multiple cerebral aneurysms are not uncommon 3. S/S: a. sudden, severe headache, loss of consciousness (if aneurysm ruptures) b. pain and rigidity in back of neck and spine c. visual disturbance d. tinnitus, dizziness, hemiparesis e. coma and death. 4. Management: a. prevent rupturing of aneurysm b. aneurysm can be reinforced or ligated (clipped off) in surgery c. extracranial-intracranial arterial bypass d. bed rest e. analgesics f. elastic compression stockings to prevent DVT while on bed rest.
Vous aimerez peut-être aussi
- MedSurg NeuroDocument8 pagesMedSurg NeuroZachary T Hall100% (1)
- Neuro DisordersDocument13 pagesNeuro DisordersMicz Celiz100% (3)
- Medical Surgical: Nervous SystemDocument90 pagesMedical Surgical: Nervous SystemCatherine G. Borras100% (1)
- Med Surge 2 Mod 3 Study Guide2Document21 pagesMed Surge 2 Mod 3 Study Guide2Dirk Buckner100% (4)
- Chart of Neuro DisordersDocument1 pageChart of Neuro DisordersNursingSchoolNotes100% (2)
- Neurology Nursing Study GuideDocument19 pagesNeurology Nursing Study GuideHayleyLangley100% (5)
- Med Surge 2 Mod 1 CardiacDocument13 pagesMed Surge 2 Mod 1 CardiacDirk Buckner100% (2)
- Musculoskeletal Note1Document34 pagesMusculoskeletal Note1FreeNursingNotes100% (4)
- Endocrine NursingDocument8 pagesEndocrine NursingBunny Bonny100% (5)
- Fundamentals of Nursing ReviewerDocument34 pagesFundamentals of Nursing Reviewerrahkel08100% (1)
- Gi NclexDocument14 pagesGi NclexYoke W Khoo100% (3)
- Neurologic NursingDocument14 pagesNeurologic Nursingtheglobalnursing100% (6)
- Endocrine NursingDocument2 pagesEndocrine NursingUnclePorkchop94% (34)
- Pharm 1.13 Antidepressant Cheat SheetDocument1 pagePharm 1.13 Antidepressant Cheat SheetEunice CortésPas encore d'évaluation
- Med Surg Study GuideDocument98 pagesMed Surg Study Guideprogramgrabber100% (2)
- Medsurg Cardio Ana&PhysioDocument6 pagesMedsurg Cardio Ana&Physiorabsibala80% (10)
- Priority Nursing ActionsDocument4 pagesPriority Nursing ActionsAnn ChenPas encore d'évaluation
- CardioDocument10 pagesCardioMar OrdanzaPas encore d'évaluation
- Med-Surg LEWIS 47 Final Foofed UpDocument10 pagesMed-Surg LEWIS 47 Final Foofed Uphariniliaankhen100% (1)
- Cardio, Respi, GastroDocument11 pagesCardio, Respi, Gastrojeshema100% (1)
- Musculoskeletal MED SURGDocument57 pagesMusculoskeletal MED SURGlolo0880Pas encore d'évaluation
- Cardiovascular Nursing Bullet Points I PDFDocument4 pagesCardiovascular Nursing Bullet Points I PDFKhalid Epping100% (3)
- Med SurgTest2Document17 pagesMed SurgTest2Becca Sanborn100% (2)
- Med Surg ATI1Document97 pagesMed Surg ATI12Ghzchapter88% (17)
- MedSurg Medications & TablesDocument71 pagesMedSurg Medications & TablesSarah PlunkettPas encore d'évaluation
- Medical Surgical Nursing Cardio Vascular System ClassDocument15 pagesMedical Surgical Nursing Cardio Vascular System Classvallal100% (2)
- Cardionursing 110207023802 Phpapp01Document18 pagesCardionursing 110207023802 Phpapp01LudwigJayBarayuga100% (5)
- Exam 2 - Neurological Study GuideDocument10 pagesExam 2 - Neurological Study GuideStephaniePas encore d'évaluation
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- NUR100 Sherpath Oxygenation and PerfusionDocument17 pagesNUR100 Sherpath Oxygenation and Perfusioncaloy2345caloyPas encore d'évaluation
- Chapter 14 Fluid and Electrolytes ChartsDocument7 pagesChapter 14 Fluid and Electrolytes ChartsBNA_RN100% (3)
- Congenital Heart DiseasesDocument6 pagesCongenital Heart DiseasesMox SwanPas encore d'évaluation
- Med Surg Respiration-Cardiac NotesDocument11 pagesMed Surg Respiration-Cardiac Notesorganictallgirl50% (2)
- Nursing 4 Final ReviewDocument41 pagesNursing 4 Final Reviewemeraldwxyz100% (1)
- Med Surg BulletsDocument35 pagesMed Surg Bulletscfournier1982Pas encore d'évaluation
- Med Surg Final Exam MapDocument42 pagesMed Surg Final Exam MapAnais Hall-Garrison100% (1)
- Dysrhythmias NotesDocument23 pagesDysrhythmias NoteskmimmackPas encore d'évaluation
- Handout Medical-Surgical Nursing Fluid and ElectrolyteDocument13 pagesHandout Medical-Surgical Nursing Fluid and ElectrolytePaul Christian P. Santos, RN100% (10)
- Neuro NursingDocument22 pagesNeuro Nursingheiyu100% (6)
- Cardiovascular MneumonicsDocument10 pagesCardiovascular MneumonicsKaly RiePas encore d'évaluation
- Medsurg 3 Exam 1Document55 pagesMedsurg 3 Exam 1Melissa Blanco100% (1)
- Upper Respiratory Drugs #17Document5 pagesUpper Respiratory Drugs #17Gina Giammalvo100% (3)
- Respiratory DiseasesDocument14 pagesRespiratory DiseasesKira100% (6)
- Chapter 35 - Ignatavicius Medical Surgical NursingDocument6 pagesChapter 35 - Ignatavicius Medical Surgical Nursinggrkpanygiri100% (4)
- Med Surge 2 - RESP SYSTEM NOTESDocument26 pagesMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- NCLEX StrokeSeizureDocument9 pagesNCLEX StrokeSeizureArthur Christopher CorpuzPas encore d'évaluation
- Care of Patient With Musculoskeletal DisordersDocument3 pagesCare of Patient With Musculoskeletal DisordersBryan Mae H. DegorioPas encore d'évaluation
- Neurological Med SurgDocument52 pagesNeurological Med Surglolo0880100% (2)
- Physiologic Changes of Aging: System AlterationDocument1 pagePhysiologic Changes of Aging: System Alterationshenric16100% (1)
- PerfusionDocument9 pagesPerfusionAmanda Brittain100% (2)
- Shock With Hemodynamic ChangesDocument2 pagesShock With Hemodynamic ChangesBNA_RN100% (1)
- Medical Surgical Nursing PinoyDocument67 pagesMedical Surgical Nursing Pinoyalfred31191% (23)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Rogers GI Study GuideDocument2 pagesRogers GI Study GuideNursingSchoolNotesPas encore d'évaluation
- ECG StripsDocument5 pagesECG StripsNursingSchoolNotes100% (1)
- GI Study GuideDocument11 pagesGI Study GuideNursingSchoolNotes75% (4)
- Cancer Types, ChartDocument2 pagesCancer Types, ChartNursingSchoolNotesPas encore d'évaluation
- Resp Lecture NotesDocument17 pagesResp Lecture NotesNursingSchoolNotes100% (3)
- Adam's Respiratory Study GuideDocument5 pagesAdam's Respiratory Study GuideNursingSchoolNotesPas encore d'évaluation
- Oncology, HIV, DIC Study Guide.Document6 pagesOncology, HIV, DIC Study Guide.NursingSchoolNotes100% (1)
- Adult III Cardiac Study GuideDocument15 pagesAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Pain Med ChartsDocument4 pagesPain Med ChartsNursingSchoolNotesPas encore d'évaluation
- UNIT 5 Study Guide Part 1Document5 pagesUNIT 5 Study Guide Part 1NursingSchoolNotesPas encore d'évaluation
- Unit 5 Study Guide Part 2Document3 pagesUnit 5 Study Guide Part 2NursingSchoolNotesPas encore d'évaluation
- Endocrine Study GuideDocument4 pagesEndocrine Study GuideNursingSchoolNotes100% (1)
- OB Drug ChartsDocument2 pagesOB Drug ChartsNursingSchoolNotesPas encore d'évaluation
- Psych Med ChartsDocument5 pagesPsych Med ChartsNursingSchoolNotes100% (5)
- Unit 4 Study Guide Part 2Document7 pagesUnit 4 Study Guide Part 2NursingSchoolNotesPas encore d'évaluation
- Pulmonary Med Charts Part 2Document2 pagesPulmonary Med Charts Part 2NursingSchoolNotes100% (3)
- Gastrointestinal System and Nutrition Drug ChartsDocument3 pagesGastrointestinal System and Nutrition Drug ChartsNursingSchoolNotesPas encore d'évaluation
- Hematologic System Drug ChartsDocument2 pagesHematologic System Drug ChartsNursingSchoolNotesPas encore d'évaluation
- Unit 4 Study Guide Part 1Document6 pagesUnit 4 Study Guide Part 1NursingSchoolNotesPas encore d'évaluation
- Cardiac Stuff That You Have To MemorizeDocument1 pageCardiac Stuff That You Have To MemorizeNursingSchoolNotes100% (1)
- Pulmonary Med Charts Part 1Document2 pagesPulmonary Med Charts Part 1NursingSchoolNotes100% (3)
- Unit 3 Study Guide Adult IIDocument7 pagesUnit 3 Study Guide Adult IINursingSchoolNotesPas encore d'évaluation
- Unit 2, Part 2 Study GuideDocument4 pagesUnit 2, Part 2 Study GuideNursingSchoolNotesPas encore d'évaluation
- Lyte ChartDocument3 pagesLyte ChartNursingSchoolNotesPas encore d'évaluation
- Cardiac Med ChartsDocument6 pagesCardiac Med ChartsNursingSchoolNotes100% (15)
- Unit 2 Part 1 Study GuideDocument6 pagesUnit 2 Part 1 Study GuideNursingSchoolNotes100% (1)
- Sound It Out - ElectrolytesDocument2 pagesSound It Out - ElectrolytesNursingSchoolNotes0% (1)
- Unit 1, Part 2 Study GuideDocument4 pagesUnit 1, Part 2 Study GuideNursingSchoolNotes100% (1)
- 3280 4.19MB Strabismus - A Decision Making ApproachDocument206 pages3280 4.19MB Strabismus - A Decision Making ApproachPaulEstrellaPas encore d'évaluation
- Scott-Brown's Vol 2 Benign Neck Disease - Infections & SwellingDocument12 pagesScott-Brown's Vol 2 Benign Neck Disease - Infections & SwellingjessPas encore d'évaluation
- H02E Assignment 8Document4 pagesH02E Assignment 8Good ChannelPas encore d'évaluation
- Pediatric Case StudyDocument29 pagesPediatric Case Studyapi-296281683Pas encore d'évaluation
- Patient and Family Discharge Checklist: Patient Name: Reason For AdmissionDocument7 pagesPatient and Family Discharge Checklist: Patient Name: Reason For Admissiondwirabiatul adwiyahaliPas encore d'évaluation
- 2016 Vol 62 No - 2 - April May 2016 PDFDocument56 pages2016 Vol 62 No - 2 - April May 2016 PDFDanis Diba Sabatillah YaminPas encore d'évaluation
- Physostigmine Antidote FactsDocument1 pagePhysostigmine Antidote FactsLidwina Liniati GeografiPas encore d'évaluation
- Anatomy and Physiology of PlacentaDocument5 pagesAnatomy and Physiology of PlacentaAdrianne Basa100% (1)
- Breast ComplicationsDocument42 pagesBreast ComplicationskurniaPas encore d'évaluation
- Daftar PustakaDocument3 pagesDaftar PustakaBrataAdityaPas encore d'évaluation
- Aneurizma Bazilarke I TrombolizaDocument4 pagesAneurizma Bazilarke I TrombolizaAnja LjiljaPas encore d'évaluation
- Koo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130Document16 pagesKoo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130a b cPas encore d'évaluation
- MEdical Surgical REVEWERDocument86 pagesMEdical Surgical REVEWERennaedPas encore d'évaluation
- 19-06-2017-10-15-0416257 - PD - VMO - Cardiology - Ryde HospitalDocument8 pages19-06-2017-10-15-0416257 - PD - VMO - Cardiology - Ryde HospitalHassamPas encore d'évaluation
- Practical Standard Prescriber, 7th EditionDocument505 pagesPractical Standard Prescriber, 7th EditionTonyScaria60% (5)
- DR - Sreedhar CV 2018 UpdatedDocument11 pagesDR - Sreedhar CV 2018 UpdatedDr Sreedhar TirunagariPas encore d'évaluation
- Hospitalpharmacy PDFDocument13 pagesHospitalpharmacy PDFBhavin DesaiPas encore d'évaluation
- Bryan 3-24-17Document12 pagesBryan 3-24-17Bryan VandentoornPas encore d'évaluation
- Roberto Padlan (Resume)Document5 pagesRoberto Padlan (Resume)Merian PadlanPas encore d'évaluation
- Valleylab ForceTriad - User Manual PDFDocument100 pagesValleylab ForceTriad - User Manual PDFPaulina LekszyckaPas encore d'évaluation
- Basic Surgical Skills Indonesia 2016Document17 pagesBasic Surgical Skills Indonesia 2016'putu' AcaaRyaaPas encore d'évaluation
- Adl IadlDocument20 pagesAdl IadlKrisna Eka Yudha100% (1)
- What Documents Do You Need After A Blood Transfusion?: BT Checklist 1Document5 pagesWhat Documents Do You Need After A Blood Transfusion?: BT Checklist 1Edelweiss Marie CayetanoPas encore d'évaluation
- Healthcare System and Reforms in The United States Revised Essay 3Document4 pagesHealthcare System and Reforms in The United States Revised Essay 3api-272097622Pas encore d'évaluation
- IsosorbideDocument2 pagesIsosorbideSPas encore d'évaluation
- Referat Gangguan Lapang PandangDocument27 pagesReferat Gangguan Lapang PandangIkrima MuhdarmuhallyPas encore d'évaluation
- Daftar PustakaDocument5 pagesDaftar PustakaAgus PratamaaPas encore d'évaluation
- Velopharyngeal Insufficiency and Its Management: DR T BalasubramanianDocument15 pagesVelopharyngeal Insufficiency and Its Management: DR T BalasubramanianDr. T. Balasubramanian100% (2)
- Mental Health Screening ToolsDocument2 pagesMental Health Screening ToolsMinozu AryantiPas encore d'évaluation
- Types of DoctorsDocument29 pagesTypes of DoctorsEduardo Brier VelascoPas encore d'évaluation