Académique Documents
Professionnel Documents
Culture Documents
Assignment Dia No
Transféré par
Karen T. CeletariaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Assignment Dia No
Transféré par
Karen T. CeletariaDroits d'auteur :
Formats disponibles
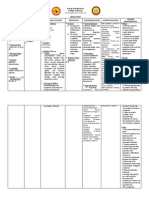
Karen T. Celetaria BSN III-A Group I HEPATIC VS.
HEPATOMA: A research on its management
September 14, 2012 Mrs. Sheila Mae Diano
PATIENT'S PROFILE A case of Orlanda, Ernesto, 71 y/o, male, Filipino, widower, Roman Catholic, born on July 21, 1941 currently residing at Mabolo, Cebu City admitted for the second time at Vicente Sotto Memorial Medical Center. CHIEF COMPLAINTS: jaundice and right upper quadrant pain HISTORY OF PRESENT ILLNESS Few weeks prior to consultation, noted one of undocumented fever, negatives for chills, negative for nausea and vomiting. No consultation done. Condition persisted now associated with right upper quadrant pain, negative for chills, with anorexia plus loose watery, brown stools. Medication taken with temporary relief. Consult done at Cebu City Medical Center due to persistence of symptoms and requested ultrasound wherein it was noted non-specific complex mass at the right hepatic lobe. Referred to VSMMC for further evaluation and management. FRESH FROZEN PLASMA I. Definition Fresh Frozen Plasma (FFP) is the fluid portion of one unit of human blood that has been centrifuged, separated and frozen solid at -18c within eight hours of collection II. PREPARATION & STORAGE Plasma is obtained by centrifugation of whole blood or by apheresis wherein plasma is filtered and the remaining part of the blood is pumped back into the donor.1 unit of FFP is 200ml which is obtained from 1unit of whole blood i.e 450-500ml.Plasma so obtained is frozen at -18C or below. It can be stored at -18C for 24 months, at -36C for 36 months.It is thawed in a water bath at 37C or in a microwave thawing device. III. ADMINISTRATION FFP should be transfused within 24hrs after thawing during this period it has to be stored at 16C.It must be ABO compatible with recipient RBC.The dose is 10-15ml/kg. This constitutes approx. 25-30% replacement therapy for coagulation factors. IV. COMPONENTS Composition FFP contains labile as well as stable components of the coagulation, fibrinolytic and complement systems, the proteins that maintain oncotic pressure and modulate immunity. In addition fats, carbohydrates and minerals are present in concentrations similar to circulation. FFP is a hyperosmolal, hyperglycemic, hypernatremic and hypochloremic solution. It is a less effective volume expander than other albumin containing solutions, due to its lower albumin content.
V. NURSING RESPONSIBILITIES: Before starting the transfusion: Safe practice starts with accurate collection of pretransfusion blood samples for typing and crossmatching. Some facilities may require a second authorized staff member to witness and sign the form as the phlebotomist obtains the specimen. Also take these other key actions before you begin the transfusion: Verify that an order for the transfusion exists. Conduct a thorough physical assessment of the patient (including vital signs) to help identify later changes. Document your findings. Confirm that the patient has given informed consent. Teach the patient about the procedures associated risks and benefits, what to expect during the transfusion, signs and symptoms of a reaction, and when and how to call for assistance. Check for an appropriate and patent vascular access. Make sure necessary equipment is at hand for administering the blood product and managing a reaction, such as an additional free I.V. line for normal saline solution, oxygen, suction, and a hypersensitivity kit. Be sure youre familiar with the specific product to be transfused, the appropriate administration rate, and required patient monitoring. Be aware that the type of blood product and patients condition usually dictate the infusion rate. For example, blood must be infused faster in a trauma victim whos rapidly losing blood than in a 75-year-old patient with heart failure, who may not be able to tolerate rapid infusion. Know what personnel will be available in the event of a reaction, and how to contact them. Resources should include the on-call physician and a blood bank representative. Before hanging the blood product, thoroughly double-check the patients identification and verify the actual product. Check the unit to be transfused against patient identifiers, per facility policy. Infuse the blood product with normal saline solution only, using filtered tubing. Administration and Timing: Use as soon as possible after thawing. Maximum hang time per unit is 6 hours due to risk of bacterial growth. During Administration (things to watch out for): During the transfusion, stay alert for signs and symptoms of a reaction, such as fever or chills, flank pain, vital sign changes, nausea, headache, urticaria, dyspnea, and bronchospasm. Optimal management of reactions begins with a standardized protocol for monitoring and documenting vital signs. As dictated by facility policy, obtain the patients vital signs before, during, and after the transfusion. If you suspect a transfusion reaction, take these immediate actions: Stop the transfusion. Keep the I.V. line open with normal saline solution. Notify the physician and blood bank. Intervene for signs and symptoms as appropriate. Monitor the patients vital signs.
VI. Why is Prothrombin Test indicated in the use of Fresh Frozen Plasma? The prothrombin time (PT) test is ordered to help diagnose unexplained bleeding, often along with a partial thromboplastin time (PTT) test. The PT test evaluates the extrinsic and common pathways of the coagulation cascade, while the PTT test evaluates the intrinsic and common pathways. Using both examines the integrated function of all of the coagulation factors. Interpretation of PT and PTT in Patients with a Bleeding or Clotting Syndrome PT RESULT
PTT RESULT
EXAMPLES OF CONDITIONS THAT MAY BE PRESENT
Liver disease, decreased vitamin K, decreased or defective factor VII, chronic lowgradedisseminated intravascular coagulation (DIC), anticoagulation drug (warfarin) therapy
Prolonged Normal
Normal
Prolonged
Decreased or defective factor VIII, IX, or XI, von Willebrand disease (severe type), presence of lupus anticoagulant
Prolonged Prolonged Normal Normal slightly prolonged
Decreased or defective factor I, II, V or X, severe liver disease, acute DIC or May indicate normal hemostasis; however, PT and PTT can be normal in conditions such as mild deficiencies in other factors and mild form of von Willebrand disease. Further testing may be required to diagnose these conditions.
The patient has a diagnosis of Liver abscess vs. Hepatoma thus clotting factors synthesized/ produced by the liver are compromised which could lead to bleeding. This was verified by his PT result of 44 seconds is relatively longer than 10-14 seconds as the normal range. PALPATION OF ABDOMEN There are two types of abdominal palpation- superficial and deep. The liver is in need of deep palpation since it is not commonly palpable along with the spleen and kidneys. However, it is contraindicated in this case. This is because the metastatic liver is likewise painful. Liver abscesses may cause (frequently severe) pain on tapping. An abscess is a kind of localized infection (only a small area is initially affected) wherein there is a formation of pus and other harmful substances enclosed in a capsule. However, it can spread to nearby organs causing a much more serious inflammation. If frequent deep palpations are practiced on this site, a possibility of bursting the capsule can cause abdominal asepsis. SOURCES: http://en.wikipedia.org/wiki/Abdominal_examination#Palpation http://www.abscesses.org/liver-abscess/
NESTOR: CTT The free end of the tube is usually attached to an underwater seal, below the level of the chest. This allows the air or fluid to escape from the pleural space, and prevents anything returning to the chest. Alternatively, the tube can be attached to a flutter valve. This allows patients with pneumothorax to remain more mobile. British Thoracic Society recommends the tube is inserted in an area described as the "safe zone", a region bordered by: the lateral border of pectoralis major, a horizontal line inferior to the axilla, the anterior border of latissimus dorsi and a horizontal line superior to the nipple[citation needed]. More specifically, the tube is inserted into the 5th intercostal space slightly anterior to the mid axillary line. Chest tubes are usually inserted under local an esthesia. The skin over the area of insertion is first cleansed with antiseptic solution, such as iodine, before sterile drapes are placed around the area. The local anesthetic is injected into the skin and down to the muscle, and after the area is numb a small incision is made in the skin and a passage made through the skin and muscle into the chest. The tube is placed through this passage. If necessary, patients may be given additional analgesicsfor the procedure. Once the tube is in place it is sutured to the skin to prevent it falling out and a dressing applied to the area. Once the drain is in place, a chest radiograph will be taken to check the location of the drain. The tube stays in for as long as there is air or fluid to be removed, or risk of air gathering. Contraindications to chest tube placement include refractory coagulopathy, lack of patient cooperation, and presence of a diaphragmatic hernia, as well as hepatic hydrothorax[3]. Additional contraindications include scarring in the pleural space (adhesions). SPIROMETER A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. It is a precision differential pressure transducer for the measurements of respiration flow rates. The spirometer records the amount of air and the rate of air that is breathed in and out over a specified period
Vous aimerez peut-être aussi
- SP42 Thoracentesis (Adult)Document7 pagesSP42 Thoracentesis (Adult)Adam HuzaibyPas encore d'évaluation
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingD'EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingPas encore d'évaluation
- Drug Study AmoxicillinDocument4 pagesDrug Study AmoxicillinKaren T. Celetaria75% (12)
- Bioreaction Engineering Principles Nielsen Villadsen PDFDocument554 pagesBioreaction Engineering Principles Nielsen Villadsen PDFMuchachos del Rio50% (2)
- Prinsip Penyusunan Gigi Artifisial Kelompok 7Document53 pagesPrinsip Penyusunan Gigi Artifisial Kelompok 7gilangPas encore d'évaluation
- Slave Breakers 2Document167 pagesSlave Breakers 2kjmama100% (1)
- Facial Nerve MCQDocument4 pagesFacial Nerve MCQIqbal Syed100% (1)
- Abdominal ParacentesisDocument5 pagesAbdominal Paracentesisw wPas encore d'évaluation
- Gastrointestinal-Endocrine SystemDocument8 pagesGastrointestinal-Endocrine SystemFritz MirandaPas encore d'évaluation
- Chapter VDocument15 pagesChapter VJellou MacPas encore d'évaluation
- Abdominal Paracentesis.Document4 pagesAbdominal Paracentesis.Sukh Preet100% (1)
- INTRAVENOUSDocument38 pagesINTRAVENOUSLorelyn DelfinPas encore d'évaluation
- Nursing Management of Patient Undergoing Peritoneal DialysisDocument27 pagesNursing Management of Patient Undergoing Peritoneal DialysisHemantPas encore d'évaluation
- ExamDocument7 pagesExamRhabdoPas encore d'évaluation
- IV Therapy SlidesDocument8 pagesIV Therapy SlidesRegean MercadoPas encore d'évaluation
- DIALYSISDocument7 pagesDIALYSISIvy E. LantapePas encore d'évaluation
- Abdominal ParacentesisDocument4 pagesAbdominal ParacentesisRashmi C S100% (1)
- Foreign Body EBook MxncykDocument8 pagesForeign Body EBook MxncykErhan ErtuçPas encore d'évaluation
- IV Therapy SsDocument56 pagesIV Therapy Sssaeed_chohan100% (8)
- Abdominal ParacentesisDocument5 pagesAbdominal ParacentesisVijith.V.kumar100% (1)
- Hainashri MSN ProcedureDocument9 pagesHainashri MSN ProcedureRickjit SadhukhanPas encore d'évaluation
- (Hyperalimentation) Meaning of Total Parental NutritionDocument7 pages(Hyperalimentation) Meaning of Total Parental NutritionSavita HanamsagarPas encore d'évaluation
- Meds-Study GuideDocument3 pagesMeds-Study Guidejackli21Pas encore d'évaluation
- Liver Biopsy and AbdominalDocument25 pagesLiver Biopsy and AbdominalAfiq Mubasyyir AmranPas encore d'évaluation
- A Brief History of IV Infusion Therapy, From The Middle Ages To TodayDocument5 pagesA Brief History of IV Infusion Therapy, From The Middle Ages To TodayJinky Nacar DomingoPas encore d'évaluation
- Patient'S Profile: GROUP 1: Camposano, Cielo, Edem, Ibalin, RodriguezDocument3 pagesPatient'S Profile: GROUP 1: Camposano, Cielo, Edem, Ibalin, RodriguezDivina Gracia Vibal CieloPas encore d'évaluation
- Liver DiseaseDocument8 pagesLiver Diseaseأبوأحمد الحكيمPas encore d'évaluation
- IV InsertionDocument22 pagesIV InsertionRA100% (1)
- Pingen, Kathleen Joy R. BSN 3ADocument3 pagesPingen, Kathleen Joy R. BSN 3AKathleen Joy PingenPas encore d'évaluation
- ERCP Procedure GuideDocument7 pagesERCP Procedure GuideFachrur RodjiPas encore d'évaluation
- Peritoneal DialysisDocument10 pagesPeritoneal DialysisPdianghunPas encore d'évaluation
- Gastro ActDocument6 pagesGastro Actvincent serquenaPas encore d'évaluation
- Intrevenous TherapyDocument5 pagesIntrevenous TherapyCharles DoradoPas encore d'évaluation
- 74 Anaesthesia For Intestinal Obstruction in Children 1Document6 pages74 Anaesthesia For Intestinal Obstruction in Children 1Dr. Anish GolchhaPas encore d'évaluation
- DialysisDocument20 pagesDialysisSiwani rai100% (1)
- Colonoscopy ProcedureDocument3 pagesColonoscopy Procedurejmarcos84Pas encore d'évaluation
- GistDocument5 pagesGistYip Kar JunPas encore d'évaluation
- Procedure AssignmentDocument12 pagesProcedure AssignmentMubarek UmerPas encore d'évaluation
- GI Diagnostic TestsDocument7 pagesGI Diagnostic TestspatziePas encore d'évaluation
- Liver TransplantationDocument6 pagesLiver TransplantationPriyaPas encore d'évaluation
- Hemodialysis PPT 1Document47 pagesHemodialysis PPT 1Edralee VillanuevaPas encore d'évaluation
- Peritoneal DialysisDocument56 pagesPeritoneal DialysisVanet100% (1)
- Acute Respiratory Distress SyndromeDocument4 pagesAcute Respiratory Distress SyndromeBianca WelchPas encore d'évaluation
- Nle Tips 3Document11 pagesNle Tips 3glenard-roble-1251Pas encore d'évaluation
- Abdominal Paracentesis AnpDocument14 pagesAbdominal Paracentesis Anpesther100% (1)
- Intravenous TherapyDocument22 pagesIntravenous TherapyMatt Lao Dionela100% (1)
- Nle Tips May2015Document15 pagesNle Tips May2015Randy100% (2)
- Ov Ov OvDocument15 pagesOv Ov OvHayyana Mae Taguba LadiaPas encore d'évaluation
- Assignment On Abdominal ParacentesisDocument9 pagesAssignment On Abdominal ParacentesisAxsa AlexPas encore d'évaluation
- ParacenthesisDocument5 pagesParacenthesisFatimah AlshareefPas encore d'évaluation
- Peritoneal DialysisDocument29 pagesPeritoneal DialysisMicah Alexis CandelarioPas encore d'évaluation
- Blood TransfusionDocument4 pagesBlood TransfusionmystardokyeomPas encore d'évaluation
- Placenta PreviaDocument54 pagesPlacenta PreviabobtagubaPas encore d'évaluation
- Percutaneous Transhepatic CholangiographyDocument3 pagesPercutaneous Transhepatic CholangiographyRonel UsitaPas encore d'évaluation
- Christine VanguardiaDocument7 pagesChristine VanguardiaJoshua PascasioPas encore d'évaluation
- Abdominal ParacentesisDocument14 pagesAbdominal ParacentesisMonika Joseph75% (4)
- Blood Transfusions - TGH Policies & ProceduresDocument4 pagesBlood Transfusions - TGH Policies & ProceduresMark Anthony FranciscoPas encore d'évaluation
- Ms Flash CardsDocument15 pagesMs Flash CardsMia MalazoPas encore d'évaluation
- Accesory OrganDocument12 pagesAccesory OrganTrisha SuazoPas encore d'évaluation
- Intravenous Parenteral TherapyDocument110 pagesIntravenous Parenteral TherapyDarran Earl Gowing100% (1)
- Peritoneal DialysisDocument5 pagesPeritoneal DialysisJulienne Sanchez-SalazarPas encore d'évaluation
- NCM112 LP1 Rosales - AnswersDocument5 pagesNCM112 LP1 Rosales - AnswersChristine CalleyPas encore d'évaluation
- Pre Analytical ConsiderationsDocument54 pagesPre Analytical ConsiderationsLycah Jyde PechuancoPas encore d'évaluation
- New DSDocument2 pagesNew DSKaren T. CeletariaPas encore d'évaluation
- Commu DiseasesDocument11 pagesCommu DiseasesKaren T. CeletariaPas encore d'évaluation
- Cebu Normal University - College of Nursing Drug Study: AbsorptionDocument2 pagesCebu Normal University - College of Nursing Drug Study: AbsorptionKaren T. CeletariaPas encore d'évaluation
- Cebu Normal University: Progress ReportDocument4 pagesCebu Normal University: Progress ReportKaren T. CeletariaPas encore d'évaluation
- BiperidenDocument3 pagesBiperidenKaren T. Celetaria100% (1)
- FluphenazineDocument3 pagesFluphenazineKaren T. CeletariaPas encore d'évaluation
- Nutrient StandardsDocument16 pagesNutrient StandardsKaren T. CeletariaPas encore d'évaluation
- Anatomy and PhysiologyDocument4 pagesAnatomy and PhysiologyKaren T. CeletariaPas encore d'évaluation
- Progress ReportDocument4 pagesProgress ReportKaren T. CeletariaPas encore d'évaluation
- Activity 2Document7 pagesActivity 2Karen T. CeletariaPas encore d'évaluation
- Blue Cross InsuranceDocument4 pagesBlue Cross InsuranceKaren T. CeletariaPas encore d'évaluation
- Activity 2Document7 pagesActivity 2Karen T. CeletariaPas encore d'évaluation
- Comparative Phytochemical Profiling of Clerodendrum InfortunatumDocument10 pagesComparative Phytochemical Profiling of Clerodendrum Infortunatumupendra1616Pas encore d'évaluation
- Crimson Druid v1.1Document3 pagesCrimson Druid v1.1Carter RobinsonPas encore d'évaluation
- Emergency Nursing Nclex ExamDocument19 pagesEmergency Nursing Nclex ExamsjardioPas encore d'évaluation
- Thehumancerebellum: A Review of Physiologic NeuroanatomyDocument11 pagesThehumancerebellum: A Review of Physiologic NeuroanatomyCan EkerPas encore d'évaluation
- Kara Gianni 2015Document7 pagesKara Gianni 2015devaaPas encore d'évaluation
- Higher Cortical Functions and Basis of LanguageDocument78 pagesHigher Cortical Functions and Basis of Languagelovelots1234Pas encore d'évaluation
- SCIENCE 9-Lesson 1 PhotosynthesisDocument2 pagesSCIENCE 9-Lesson 1 PhotosynthesisTeacher anaPas encore d'évaluation
- Wounds & Wound HealingDocument47 pagesWounds & Wound HealingDrSarmad100% (3)
- Testicular CancerDocument5 pagesTesticular CancerypintohPas encore d'évaluation
- A Visit To A GrandmotherDocument3 pagesA Visit To A GrandmotherHEY ERLPas encore d'évaluation
- PeriodisationDocument6 pagesPeriodisationZahra SativaniPas encore d'évaluation
- Peripheral Nerve Repair and RegenerationDocument15 pagesPeripheral Nerve Repair and RegenerationjaimeaquilesrinconPas encore d'évaluation
- The Workings of The Brain Powers of The MindDocument17 pagesThe Workings of The Brain Powers of The MindLovely ramirezPas encore d'évaluation
- 6.1 Digestion BNDocument24 pages6.1 Digestion BNHana ElattarPas encore d'évaluation
- Neonatal PneumoniaDocument2 pagesNeonatal PneumoniaJustin EduardoPas encore d'évaluation
- TIMI Score For NSTEMI, STEMI and Unstable AnginaDocument8 pagesTIMI Score For NSTEMI, STEMI and Unstable AnginaBenny TrisaktyariPas encore d'évaluation
- Dewey: DecimalDocument888 pagesDewey: Decimalpratiik pyakurelPas encore d'évaluation
- FITT 1 Updated HandoutsDocument25 pagesFITT 1 Updated HandoutsJolina VillalobosPas encore d'évaluation
- Annotated Bibliography (Draft 1)Document2 pagesAnnotated Bibliography (Draft 1)Mitren ThakorPas encore d'évaluation
- The Scarecrow Queen (Excerpt)Document36 pagesThe Scarecrow Queen (Excerpt)I Read YA50% (2)
- 24 Cerebral Blood FlowDocument31 pages24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Metabolism: Anabolism and CatabolismDocument4 pagesMetabolism: Anabolism and CatabolismMedi OmicPas encore d'évaluation
- Client Screening Website FormDocument2 pagesClient Screening Website FormBrett Whipp100% (2)
- Kreisberg-Zakarin Et Al IPNS Antonie Van Leeuwenhoek 1999Document8 pagesKreisberg-Zakarin Et Al IPNS Antonie Van Leeuwenhoek 1999ElPas encore d'évaluation
- The Independence of Combinatory Semantic Processing: Evidence From Event-Related PotentialsDocument21 pagesThe Independence of Combinatory Semantic Processing: Evidence From Event-Related Potentialsdkm2030Pas encore d'évaluation
- NCP Ineffective Gas ExchangeDocument2 pagesNCP Ineffective Gas ExchangeRez ApegoPas encore d'évaluation