Académique Documents
Professionnel Documents
Culture Documents
Слайды
Transféré par
Ck KmaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Слайды
Transféré par
Ck KmaDroits d'auteur :
Formats disponibles
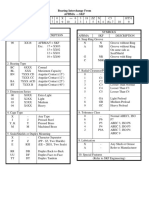
Stratification of risk to quantify prognosis Other risk factors and disease history Normal SBP 120129 or DBP 8084
Average risk Blood pressure (mmHg) High normal SBP 130139 or DBP 8589 Average risk Grade 1 HT Grade 2 HT Grade 3 HT
SBP 140159 SBP 160179 SBP > 180 or DBP 9099 or DBP 100109 or DBP > 110 No other risk Low added risk Moderate added High added factors risk risk 12 risk factors Low added risk Low added risk Moderate added Moderate added Very high risk risk added risk 3 or more risk Moderate added High added High added High added risk Very high factors, MS, risk risk risk added risk OD or diabetes Established High added Very high Very high Very high Very high cardiovascular risk added risk added risk added risk added risk or renal disease OD - subclinical organ damage; SBP - systolic blood pressure; DBP - diastolic blood pressure, MS metabolic syndrome The terms low, moderate, high and very high added risk are calibrated to indicate an approximate absolute 10-year risk of cardiovascular disease of <15%, 1520%, 2030% and >30%, respectively, according to Framingham criteria, or an approximate absolute risk of fatal cardiovascular disease <4%, 45%, 58%, and >8% according to the SCORE chart.
FACTORS INFLUENCING PROGNOSIS Risk factors Subclinical organ damage Diabetes (OD) mellitus 1. Systolic and diastolic 1. Left ventricular Fasting plasma BP levels hypertrophy glucose 7.0 2. Levels of pulse electrocardiogram: mmol/l (126 pressure (in the elderly) mg/dl) on SokolowLyons index 3. Age (Men>55 years, (SV1+RV5-6) >38 mm; repeated Women >65 years) measurements Cornell >2440 mm x ms; 4. Smoking or echocardiogram: 5. Dyslipidaemia: LVMI=left ventricular mass Postprandial total cholesterol: index: M>125, W>110 g/m2 plasma glucose >11.0 mmol/l >5.0 mmol/l 2. Vessels (>190 mg/dl), or Ultrasound evidence of (>198 mg/dl) LDL-cholesterol: carotid wall thickening >3.0 mmol/l (carotid intima-media (>115 mg/dl), or thickness > 0.9 mm) or atherosclerotic plaque HDL-cholesterol: M <1.0 mmol/l Carotid-femoral pulse (<40 mg/dl) wave velocity>12 m/s W <1.2 mmol/l Ankle/brachial BP (<46 mg/dl) index<0,9 Triglycerides: 3. Kidney > 1,7 mmol/l Slight increase in serum
Established cardiovascular or renal disease 1. Cerebrovascular disease: ischaemic stroke; cerebral haemorrhage; transient ischaemic attack 2. Heart disease: myocardial infarction; angina; coronary revascularization; congestive heart failure 3. Renal disease: diabetic nephropathy; renal impairment serum creatinine (M>133 mol/l (>1.5 mg/dl) W>124 mol/l (>1.4 mg/dl) proteinuria (>300 mg/24 h) 4. Peripheral artery disease 5.Advanced retinopathy: haemorrhages or exudates,
(150 mg/dl) 6.Family history of premature cardiovascular disease (M at age <55 years, W <65 years) 7. Abdominal obesity (waist circumference M > 102 cm, W> 88 cm) 8.Fasting plasma glucose 5,6-6,9 mmol/l (102-125 mg/dl) 9. Abnormal glucose tolerance test
creatinine M 115133 mol/l (1.31.5 mg/dl) W 107124 mol/l (1.21.4 mg/dl) Microalbuminuria 30300 mg/24 h; or albumincreatinine ratio M > 22 mg/g (> 2.5 mg/mmol) W >31 mg/g (> 3.5 mg/mmol) Low estimated glomerular filtration rate (MDRD formula): <60 ml/min/1,73 m2 or Low creatinine clearance (Cockroft-Gault formula): <60 ml/min
papilloedema
INITIATION OF ANTIHYPERTENSIVE TREATMENT.
Normal BP Other risk SBP 120-129 factors OD or DBP 80-84 or disease No other No BP risk factors intervention High normal BP SBP 130-139 or DBP 85-89 Grade 1 HT SBP 140-159 or DBP 90-99 Grade 2 HT SBP 160-179 or DBP 100-109 Grade 3 HT SBP > 180 or DBP>110
No BP intervention Lifestyle changes for several months then drug treatment if BP uncontrolled 1-2 risk Lifestyle changes Lifestyle changes Lifestyle changes factors for several weeks then drug treatment if BP uncontrolled >3 risk Lifestyle changes Lifestyle changes Lifestyle changes factors, MS and consider drug +Drug treatment or OD treatment Diabetes
Lifestyle changes Lifestyle changes for several weeks + Immediate drug then drug treatment treatment if BP uncontrolled Lifestyle changes Lifestyle changes for several weeks + Immediate drug then drug treatment treatment if BP uncontrolled Lifestyle changes + Drug treatment Lifestyle changes + Immediate drug treatment Lifestyle changes + Immediate drug treatment
Lifestyle changes Lifestyle changes + Lifestyle changes Lifestyle changes Drug treatment +Drug treatment + Drug treatment
Established Lifestyle changes Lifestyle changes CV or + Immediate drug + Immediate drug + renal treatment treatment disease
Lifestyle changes Lifestyle changes Lifestyle changes + Immediate + Immediate drug + Immediate drug drug treatment treatment treatment
ANTIHYPERTENSIVE TREATMENT: PREFERRED DRUGS
LVH Asympt. atherosclerosis Microalbuminuria Renal dysfunction Previous stroke Previous Ml Angina pectoris Heart failure
Subclinical organ damage ACEl, CA, ARB CA, ACEl ACEl, ARB ACEl, ARB Clinical event any BP lowering agent BB, ACEl, ARB BB, CA Diuretics, BB, ACEl, ARB, antialdosterone agents - ARB, ACEl - BB, non-dihydropiridine CA ACEl, ARB, loop diuretics CA Condition Diuretics, CA ACEl, ARB, CA, modulators of imidazoline receptors ACEl, ARB CA, methyldopa, BB Diuretics, CA
Atrial fibrillation: - Recurrent - Permanent ESRD/proteinuria Peripheral artery disease ISH (elderly) Metabolic syndrome Diabetes mellitus Pregnancy Blacks
Abbreviations: LVH: left ventricular hypertrophy; ISH: isolated systolic hypertension; ESRD: renal failure; ACEl: ACE inhibitors; ARB: angiotensin receptor antagonists; CA: calcium antagonists; BB: b-blockers Aliskiren, a new drug that is targeting the renin system at its point of activation is already available in the USA and may soon be made available in Europe. This drug has been shown to effectively lower blood pressure in hypertension, both alone and in combination with a thiazide diuretic, and also to have an antiproteinuric effect in pre-dinical studies. It has been suggested that renin may have effects not connected to the classical renin-angiotensin cascade and be a prognostic factor independent of angiotensin II production. Conclusive evidence that this is the case as well as data on the cardiovascular protective effects of renin inhibition is not yet available.
Blood pressure thresholds (mmHg) for definition of hypertension with different types of measurement SBP, DBP, systolic blood pressure diastolic blood pressure Office or clinic 140 90 24-hour ambulatory: 125-130 80 - day 130-135 85 -night 120 70 Home (self) 130-135 85
Isolated office (or clinic) hypertension (so-called whitecoat hypertension) Diagnosis Office BP > 140/90 mmHg (at several visits); 24 h ambulatory BP <125/80 mmHg. Investigation Possible metabolic risk factors; possible target organ damage Prescription Lifestyle changes and close follow-up; drug treatment if eviden damage
Blood pressure measurement 1. Blood pressure values measured in the doctors office or the clinic should commonly be used as reference. 2. Twenty-four-hour ambulatory blood pressure monitoring may be considered of additional clinical value, when: considerable variability of office blood pressure is found over the same or different visits; high office blood pressure is measured in subjects otherwise at low global cardiovascular risk; there is marked discrepancy between blood pressure values measured in the office and at home; resistance to drug treatment is suspected; research is involved. 3. Self-measurement of blood pressure at home should be encouraged in order to: provide more information for the doctors decision; improve patients adherence to treatment regimens. 4. Self-measurement of blood pressure at home should be discouraged whenever: it causes patients anxiety; it induces self-modification of the treatment regimen. 5. Normal values are different for office, ambulatory and home blood pressure.
Physical examination for secondary hypertension and organ damage Signs suggesting secondary hypertension and organ damage Features of Cushing syndrome. Skin stigmata of neurofibromatosis (phaeochromocytoma). Palpation of enlarged kidneys (polycistic kidney). Auscultation of abdominal murmurs (renovascular hypertension). Auscultation of precordial or chest murmurs (aortic coarctation or aortic disease). Diminished and delayed femoral and reduced femoral blood pressure (aortic coarctation, aortic disease). Signs of organ damage Brain: murmurs over neck arteries, motor or sensory defects. Retina: funduscopic abnormalities. Heart: location and characteristics of apical impulse, abnormal cardiac rhythms, ventricular gallop, pulmonary rales, dependent oedema. Peripheral arteries: absence, reduction, or asymmetry of pulses, cold extremities, ischaemic skin lesions.
Laboratory investigations
Routine tests Plasma glucose (preferably fasting) Serum total cholesterol Serum high-density lipoprotein (HDL)-cholesterol Fasting serum triglycerides Serum uric acid Serum creatinine Serum potassium Haemoglobin and haematocrit Urinalysis (dipstick test complemented by urinary sediment examination) Electrocardiogram Recommended tests Echocardiogram Carotid (and femoral) ultrasound C-reactive protein Microalbuminuria (essential test in diabetics) Quantitative proteinuria (if dipstick test positive) Funduscopy (in severe hypertension) Extended evaluation (domain of the specialist) Complicated hypertension: tests of cerebral, cardiac and renal function Search for secondary hypertension: measurement of renin, aldosterone, corticosteroids, catecholamines; arteriography; renal and adrenal ultrasound; computer-assisted tomography (CAT); brain magnetic resonance imaging.
Left heart failure_________ ' Causes include: ischaemic heart disease (the most common cause) systemic hypertension (chronic or 'malignant') mitral and aortic valve disease cardiomyopathies. Clinical features predominantly fatigue, tachicardia exertional dyspnoea and paroxysmal nocturnal dyspnoea. Physical signs: Cardiomegaly is demonstrable with a displaced and often sustained apical impulse. Auscultation reveals a left ventricular third or fourth heart sound that, with tachycardia, is described as a gallop rhythm. Dilatation of the mitral anulus results in functional mitral regurgitation. Crackles are heard at the lung bases. In severe left heart failure the patient has pulmonary oedema Right heart failure This syndrome occurs in association with: left heart failure chronic lung disease (cor pulmonale) pulmonary embolism or pulmonary hypertension tricuspid valve disease pulmonary valve disease left-to-right shunts (e.g. atrial or ventricular septal defects) isolated right ventricular cardiomyopathy mitral valve disease with pulmonary hypertension. Clinical features Symptoms (fatigue, breathlessness, anorexia and nausea) relate to distension and fluid accumulation in areas drained by the systemic veins. Physical signs are usually more prominent than the symptoms, with: jugular venous distension ( v waves of tricuspid regurgitation) tender smooth hepatic enlargement dependent pitting oedema development of free abdominal fluid (ascites) pleural transudates (commonly right-sided). Dilatation of the right ventricle produces cardiomegaly and may give rise to functional tricuspid regurgitation. Tachycardia and a right ventricular third heart sound are usual.
Systolic versus diastolic heart failure Systolic ventricular dysfunction is most commonly due to coronary artery disease, usually following myocardial infarction. The left ventricle is usually dilated and fails to contract normally. Diastolic ventricular dysfunction results from impaired myocardial relaxation, with increased stiffness in the ventricular wall and decreased left ventricular compliance leading to impairment of diastolic ventricular filling and hence decreased cardiac output. Coronary artery disease, hypertension and hypertrophic cardiomyopathy are common causes, although infiltrative disease such as amyloid may lead to pure diastolic dysfunction. Up to 30% of patients with heart failure may have normal systolic contraction. Management is similar to systolic heart failure but there may be an additional place for calcium-channel blockers. Diastolic dysfunction appears to carry a better prognosis. Diagnosis of heart failure The diagnosis of heart failure should not be based on history and clinical findings; it requires evidence of cardiac dysfunction with appropriate investigation using objective measures of left ventricular structure and function (usually echocardiography). Diagnosis of heart failure (European Society of Cardiology guidelines) Essential features (criteria 1 and 2) 1. Symptoms and signs of heart failure (e.g. breathlessness, fatigue, ankle swelling) 2. Objective evidence of cardiac dysfunction (at rest) Non-essential features 3. Response to treatment directed towards heart failure cases (in where the diagnosis is in doubt)
INVESTIGATIONS Diagnostic Blood tests - full blood count, liver biochemistry, urea and electrolytes, cardiac enzymes in acute heart failure to diagnose myocardial infarction, thyroid function. Chest X-ray - cardiac size and evidence of pulmonarycongestion, initially upper lobe diversion, then fluid Electrocardiogram - evidence of ischaemia, hypertension or arrhythmia. Natriuretic peptide (B-type NP (BNP) or N terminal (NTproBNP)). A normal plasma level excludes heart failure and is a useful screening test in the investigation of patients with breathlessness. Echocardiography. Two-dimensional and Doppler echocardiography establish the presence of systolic and/ or diastolic impairment of the left or right ventricle. They may also reveal the aetiology (valve disease, regional wall motion abnormalities in ischaemic heart disease, cardiomyopathy, amyloid), and may detect intracardiac thrombus. An ejection fraction of < 0.45 is generally accepted as evidence for systolic dysfunction. Stress echocardiography. Exercise or pharmacologicalstress echocardiography has no radiation hazard and is a reliable technique for detecting ischaemia as a cause of persistent but reversible cardiac dysfunction and in determining the viability of akinetic myocardium in patients with heart failure. Dobutamine sfress-induced sustained contractile improvement is observed when flow reserve is appropriate, in the presence of stunning or non-transmural infarction. Nuclear cardiology. Radionuclide angiography (RNA) provides accurate measurements of left, and to a lesser extent, right ventricular ejection fractions, cardiac volumes and regional wall motion. Left ventricular filling dynamics (diastolic function) can also be analysed. These measurements are not reliable in the presence of atrial fibrillation. Single-photon-emission computed tomography (SPECT) can be performed at rest or during stress, e.g. dobutamine infusion using different radionuclides, e.g. thallium201 or technetium-99m, to detect the presence and extent of ischaemia
INVESTIGATIONS Cardiac MRI. At present, MRI is only recommended in selected patients with heart failure where other investigations do not provide satisfactory diagnosis. Positron emission tomography (PET). When other tests (e.g. stress echocardiography, SPECT) cannot provide satisfactory results, PET scanning can be used, especially to identify potentially viable muscle that is hibernating. The importance of identifying the pathology is that appropriate treatment (surgical or medical) may restore the function. Cardiac catheterization. Cardiac biopsy for infiltrative disease, e.g. amyloid.
Functional/prognostic Cardiopulmonary exercise testing. Peak oxygen consumption (Vo2) is a strong independent predictor of hospital admission and death in patients with heart failure but is not widely available. A 6-minute exercise walk may be used instead. Ambulatory (24-48 hours) ECG monitoring if arrhythmia is suspected. Resting and stress radionuclide angiography (MUGA) - for estimation of ejection fraction, regional wall motion abnormality.
TREATMENT OF HEART FAILURE
Treatment is aimed at relieving symptoms, prevention and control of disease leading to cardiac dysfunction and heart failure, retarding disease progression and improving quality and length of life. Measures to prevent heart failure include cessation of smoking, alcohol and illicit drugs, effective treatment of hypertension, diabetes and hypercholesterolaemia, and pharmacological therapy following myocardial infarction. The management of heart failure requires that any factor aggravating the failure should be identified and treated. Similarly the cause of heart failure must be elucidated and where possible corrected.
The basic medicines: Diuretics: Loop diuretics such as furosemide and bumetanide have a rapid onset of action (i.v. - 5 min; oral - 1-2 h) and generally short-lived (4-6 h) diuresis as the concentrating power of the kidney is reduced. These agents also produce marked potassium loss and promote hyper-uricaemia, and renal function should be monitored. Thiazide diuretics such as bendroflumethiazide have a mild diuretic effect. Metolazone is a powerful thiazide, producing profound. Thiazide diuretics in combination with loop diuretics have a synergistic action and greater diuretic effect. Aldosterons Antagonist (Potassium-sparing diuretics) Spironolactone is a specific competitive antagonist to aldosterone, producing a weak diuresis but with a potassium-sparing action Angiotensin-converting enzyme inhibitors ACEI These drugs improve prognosis in patients with symptomatic heart failure and slowe development of heart failure. ACEI lower systemic vascular resistance and venous pressure, and reduce levels of circulating catecholamines, thus improving myocardial performance. Angiotensin receptor antagonists Angiotensin II receptor antagonists (ARA) ( losartan, ibersartan, candesartan and valsartan) have similar haemodynamic effects to ACEI, but as they do not affect bradykinin metabolism, they do not produce a cough. Digitalis glycosides Digoxin is administered orally (1 mg loading and 0.125-0.25 mg daily according to body mass and renal function). The elderly and patients with hyperthyroidism are more prone to digoxin toxicity. -adrenoblokers metoprolol, bisoprolol, carvedilol. Beta-blockers, ACEI, some statins and spironolactone may reduce sudden cardiac death in patients with coronary heart disease and heart failure.
Additional medicines Anticoagulants Heart failure is associated with a fourfold increase in the risk of a stroke. Oral anticoagulants are recommended in patients with atrial fibrillation and in sinus rhythm with a history of thromboembolism, endocardial thrombus or LV aneurysm. Antiarrhythmic agents Precipitating factors should be treated, in particular electrolyte disturbance. Atrial fibrillation is common in heart failure and leads to a deterioration in symptoms. Restoration of sinus rhythm, either by electrical cardio-version or drugs, is desirable but less successful in the presence of structural heart disease and decompensated heart failure. Rate control with digoxin is often preferred. Arrhythmias are frequent in heart failure and are implicated in sudden death. Patients with sustained episodes of ventricular tachycardia should receive empirical treatment, usually with an implantable cardioverter-defibrillator (ICD). Inotropic agents Intravenous inotropes are frequently used to support myocardial function in patients with acute left ventricular failure and following cardiac surgery. Epinephrine (adrenaline), dobutamine, dopexamine and dopamine are intravenous adrenergic agonists. Statins Summary of treatment All patients with clinical heart failure should receive treatment with diuretics and an ACEI followed by beta-blocker therapy. Spironolactone should be added for severe heart failure. Patients in atrial fibrillation should take digoxin
Investigations for angina Resting ECG This is usually normal between attacks. Evidence of old myocardial infarction (e.g. pathological Q waves), left ventricular hypertrophy or left bundle branch block may be present. During an attack, transient ST depression, T-wave inversion or other changes of the shape of the T wave may appear. Exercise ECG Exercise testing can be very useful both in confirming the diagnosis of angina and in giving some indication as to the severity of the CAD. ST segment depression of > 1 mm suggests myocardial ischaemia, particularly if typical chest pain occurs at the same time Cardiac scintigraphy Myocardial perfusion scans both at rest and after stress (i.e. exercise or dobutamine), are helpful. Redistribution of the contrast agent is a sensitive indicator of ischaemia and can be particularly useful in deciding if a stenosis seen at angiography is giving rise to ischaemia. A normal perfusion scan makes significant CAD unlikely. Echocardiography This can be used to assess ventricular wall involvement and ventricular function. Regional wall motion abnormalities at rest reflect previous ventricular damage. Stress echocardiography, although technically difficult, is useful especially in women with coronary artery disease. Coronary angiography This is occasionally useful in patients with chest pain where the diagnosis is unclear. More often, the test is performed to delineate the exact coronary anatomy in patients being considered for revascularization (i.e. coronary artery bypass grafting or coronary angio-plasty). Coronary angiography should be performed only when the benefit in terms of diagnosis and potential treatment outweighs the small risk of the procedure (a mortality rate of less than 1 in 1000 cases). Acute coronary syndromes (ACS) include ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina. Myocardial infarction occurs when cardiac myocytes die due to myocardial ischaemia, and can be diagnosed on the basis of appropriate clinical history, 12-lead ECG and elevated biochemical markers troponin I and T, creatinine-kinaseMB (CK-MB). STEMI will be covered in the next section
Dose Oxygen Antiplatel et General myocardial oxygenation 35-50% 150-300 mg chewable or soluble aspirin, then 75-100 mg p.o. daily 300 mg p.o, loading dose, then 75 mg p.o. daily Clopidogrel Analgesia Diamorphine 2.5-5.0 mg i.v. Myocardial energy consumption P blockers e.g. Atenolol 5 mg i.v. repeated after 15 min, then 25-50 mg p.o. daily or Metoprolol 5 mg i.v. repeated to a maximum of 15 mg, then 25-50 mg p.o. twice daily Coronary vasodilatation Glyceryl trinitrate 2-10 mg/h i.v./buccal/or sublingual Plaque stabilization/ventricular remodelling HMG-CoA reductase e.g. Simvastatin 20-40 mg p.o. daily inhibitors (statins) Pravastatin 20-40 mg p.o. daily Atorvastatin 80 mg p.o. daily ACE inhibitors e.g. Ramipril 2.5-10 mg p.o. daily Lisinopril 5-10 mg p.o. daily
Notes Check ABG in severe COPD Give PPI with dyspepsia history Caution - increased risk of bleeding, avoid if CABG planned Prescribe with antiemetic, metoclopramide 10 mg i.v. Avoid in asthma, heart failure, hypotension, bradyarrhythmias Avoid in asthma, heart failure, hypotension, bradyarrhythmias Maintain systolic BP above 90 mmHg Combine with dietary advice and modification
Monitor renal function
Plus for non-ST-elevation myocardial infarction (NSTEMI) Antithrombin Enoxaparin 1 mg/kg s.c. twice daily Low-molecularweight heparins Glycoprotein IIB/IIIA inhibitors Abciximab 0.25 mg/kg i.v. bolus, then 0.125 mg/kg/min up to 10 mg/min i.v. for 12 h Eptifibatide 180 mg/kg i.v. bolus, then 2 mg/kg/min i.v. for 72 h Tirofiban 0.4 mg/kg/min i.v. for 30 min, then 0.1 mg/kg/min for 48-108 h
If coronary intervention likely within 24 h Indicated in high-risk patients managed without coronary intervention or during PCI Indicated in high-risk patients managed without coronary intervention or during PCI
Plus for ST-elevation myocardial infarction (STEMI) Thrombolysi s 1 500 000 units i.v. over 60 min Streptokinase or 15 mg i.v. bolus, then 50 mg over 30 min Alteplase (rtand 35 mg over 60 PA) min Tenecteplase (TNKase) 30-50 mg i.v. bolus according to weight or Reteplase 10 units i.v. bolus repeated after 30 min
Antibodies appear after 4 days, which reduces effectiveness Dose modification if < 65 kg or 6-12 h post-MI Prescribe LMW heparin i.v. for 48 h Prescribe LMW heparin i.v. for 48 h or enoxaparin 1 mg/kg twice daily Prescribe LMW heparin i.v. for 48 h
A typical ECG tracing of the cardiac cycle (heartbeat) consists of a P wave, a QRS complex, a T wave, and a U wave which is normally visible in 50 to 75% of ECGs.[23] The baseline voltage of the electrocardiogram is known as the isoelectric line. Typically the isoelectric line is measured as the portion of the tracing following the T wave and preceding the next P wave. Feature Description Duration RR The interval between an R wave and the next R wave is the inverse of 0.6 to 1.2s interval the heart rate. Normal resting heart rate is between 50 and 100 bpm During normal atrial depolarization, the main electrical vector is P wave directed from the SA node towards the AV node, and spreads from the 80ms right atrium to the left atrium. This turns into the P wave on the ECG. The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex. The PR interval reflects the time the PR electrical impulse takes to travel from the sinus node through the AV 120 to 200ms interval node and entering the ventricles. The PR interval is therefore a good estimate of AV node function. The PR segment connects the P wave and the QRS complex. This coincides with the electrical conduction from the AV node to the bundle PR of His to the bundle branches and then to the Purkinje Fibers. This 50 to 120ms segment electrical activity does not produce a contraction directly and is merely traveling down towards the ventricles and this shows up flat on the ECG. The PR interval is more clinically relevant. The QRS complex reflects the rapid depolarization of the right and left QRS ventricles. They have a large muscle mass compared to the atria and so 80 to 120ms complex the QRS complex usually has a much larger amplitude than the P-wave. The point at which the QRS complex finishes and the ST segment J-point begins. Used to measure the degree of ST elevation or depression N/A present. The ST segment connects the QRS complex and the T wave. The ST ST segment represents the period when the ventricles are depolarized. It is 80 to 120ms segment isoelectric. The T wave represents the repolarization (or recovery) of the ventricles. The interval from the beginning of the QRS complex to the apex of the T wave T wave is referred to as the absolute refractory period. The last half of 160ms the T wave is referred to as the relative refractory period (or vulnerable period). ST The ST interval is measured from the J point to the end of the T wave. 320ms interval The QT interval is measured from the beginning of the QRS complex to 300 to QT the end of the T wave. A prolonged QT interval is a risk factor for 430ms[citation interval ventricular tachyarrhythmias and sudden death. It varies with heart rate needed] and for clinical relevance requires a correction for this, giving the QTc. The U wave is not always seen. It is typically low amplitude, and, by U wave definition, follows the T wave. The J wave, elevated J-Point or Osborn Wave appears as a late delta J wave wave following the QRS or as a small secondary R wave . It is considered pathognomic of hypothermia or hypocalcemia.[24] There were originally four deflections, but after the mathematical correction for a
Electrode label (in the USA) Electrode placement RA On the right arm, avoiding bony prominences. LA In the same location that RA was placed, but on the left arm this time. RL On the right leg, avoiding bony prominences. LL In the same location that RL was placed, but on the left leg this time. V1 In the fourth intercostal space (between ribs 4 & 5) just to the right of the sternum (breastbone). V2 In the fourth intercostal space (between ribs 4 & 5) just to the left of the sternum. V3 Between leads V2 and V4. V4 In the fifth intercostal space (between ribs 5 & 6) in the mid-clavicular line (the imaginary line that extends down from the midpoint of the clavicle (collarbone)). V5 Horizontally even with V4, but in the anterior axillary line. (The anterior axillary line is the imaginary line that runs down from the point midway between the middle of the clavicle and the lateral end of the clavicle; the lateral end of the collarbone is the end closer to the arm.) V6 Horizontally even with V4 and V5 in the midaxillary line. (The midaxillary line is the imaginary line that extends down from the middle of the patient's armpit
Electrocardiogram
Main article: Electrocardiography in myocardial infarction
12-lead electrocardiogram showing ST-segment elevation (orange) in I, aVL and V1-V5 with reciprocal changes (blue) in the inferior leads, indicative of an anterior wall myocardial infarction. The primary purpose of the electrocardiogram is to detect ischemia or acute coronary injury in broad, symptomatic emergency department populations. A serial ECG may be used to follow rapid changes in time. The standard 12 lead ECG does not directly examine the right ventricle, and is relatively poor at examining the posterior basal and lateral walls of the left ventricle. In particular, acute myocardial infarction in the distribution of the circumflex artery is likely to produce a nondiagnostic ECG.[65] The use of additional ECG leads like right-sided leads V3R and V4R and posterior leads V7, V8, and V9 may improve sensitivity for right ventricular and posterior myocardial infarction. The 12 lead ECG is used to classify patients into one of three groups:[66] 1. those with ST segment elevation or new bundle branch block (suspicious for acute injury and a possible candidate for acute reperfusion therapy with thrombolytics or primary PCI), 2. those with ST segment depression or T wave inversion (suspicious for ischemia), and 3. those with a so-called non-diagnostic or normal ECG. A normal ECG does not rule out acute myocardial infarction. Mistakes in interpretation are relatively common, and the failure to identify high risk features has a negative effect on the quality of patient care.[67]
[edit] Cardiac markers
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Short-Term and Long-Term Responses To Impaired Cardiac PerformanceDocument10 pagesShort-Term and Long-Term Responses To Impaired Cardiac PerformanceCk KmaPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Medical MnemotechnicsDocument149 pagesMedical MnemotechnicsMaja Maja BułkaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- History Clerking, Physical Examination of Obstetrics PatientsDocument9 pagesHistory Clerking, Physical Examination of Obstetrics PatientsCk Kma0% (1)
- Bronchoobstrustive SyndromeDocument32 pagesBronchoobstrustive SyndromeCk Kma67% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- GOLD Spirometry 2010Document59 pagesGOLD Spirometry 2010Ck Kma100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Lobal Initiative For Chronic Bstructive Ung Isease: G O L DDocument84 pagesLobal Initiative For Chronic Bstructive Ung Isease: G O L DCk KmaPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Obsterics Short CaseDocument10 pagesObsterics Short CasePrincess XarshiniPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- GINA Asthma 2006Document109 pagesGINA Asthma 2006api-3847280Pas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Internal Medicine Practical SkillsDocument8 pagesInternal Medicine Practical SkillsCk KmaPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Presentation Script ObsDocument1 pagePresentation Script ObsCk KmaPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Medicine WorkshopDocument28 pagesMedicine WorkshopCk KmaPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Clinical ClerkshipDocument44 pagesClinical ClerkshipCk KmaPas encore d'évaluation
- Gynaecology Short CaseDocument18 pagesGynaecology Short CaseVasu NallaluthanPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Developmental Milestones How2Document5 pagesDevelopmental Milestones How2Ck KmaPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- DJI F450 Construction Guide WebDocument21 pagesDJI F450 Construction Guide WebPutu IndrayanaPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Conceptual Artist in Nigeria UNILAGDocument13 pagesConceptual Artist in Nigeria UNILAGAdelekan FortunePas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Addtional List Dissertation 040117Document6 pagesAddtional List Dissertation 040117Sagar Kansara100% (2)
- EXCEL For Pump DesignDocument2 pagesEXCEL For Pump Designkad-7Pas encore d'évaluation
- ACR39U-U1: (USB Type A) Smart Card ReaderDocument8 pagesACR39U-U1: (USB Type A) Smart Card Readersuraj18in4uPas encore d'évaluation
- RepaHeel Beeswax-Based Gel For Treating Heel Spurs Has Been Produced in EUDocument2 pagesRepaHeel Beeswax-Based Gel For Treating Heel Spurs Has Been Produced in EUPR.comPas encore d'évaluation
- Statics: Vector Mechanics For EngineersDocument39 pagesStatics: Vector Mechanics For EngineersVijay KumarPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Daftar PustakaDocument3 pagesDaftar PustakaMel DaPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- English Class Vii PDFDocument101 pagesEnglish Class Vii PDFpannapurohitPas encore d'évaluation
- Bulk Material/Part Ppap Process Checklist / Approval: Required?Document32 pagesBulk Material/Part Ppap Process Checklist / Approval: Required?krds chidPas encore d'évaluation
- Nomenclatura SKFDocument1 pageNomenclatura SKFJuan José MeroPas encore d'évaluation
- Asco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Document2 pagesAsco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Khyle Laurenz DuroPas encore d'évaluation
- Ict 2120 Animation NC Ii Week 11 20 by Francis Isaac 1Document14 pagesIct 2120 Animation NC Ii Week 11 20 by Francis Isaac 1Chiropractic Marketing NowPas encore d'évaluation
- FBC MNCS Service-, Error-, Infocodes ENDocument23 pagesFBC MNCS Service-, Error-, Infocodes ENDragos Stoian100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- BIO 201 Chapter 11 LectureDocument34 pagesBIO 201 Chapter 11 LectureDrPearcyPas encore d'évaluation
- Terminals of Ecm: E3 E4 E5 E6Document2 pagesTerminals of Ecm: E3 E4 E5 E6jeremih alhegn100% (1)
- YoungMan EN131 GUIDEDocument16 pagesYoungMan EN131 GUIDErcpawar100% (1)
- Types of Loads Considered For Design of BridgeDocument45 pagesTypes of Loads Considered For Design of BridgeAbhishek100% (1)
- Flusser-The FactoryDocument2 pagesFlusser-The FactoryAlberto SerranoPas encore d'évaluation
- Assessment of Diabetic FootDocument7 pagesAssessment of Diabetic FootChathiya Banu KrishenanPas encore d'évaluation
- AS and A Level: ChemistryDocument11 pagesAS and A Level: ChemistryStingy BiePas encore d'évaluation
- Indoor Air Quality Standard Procedures - 2014 RevDocument12 pagesIndoor Air Quality Standard Procedures - 2014 RevFioriAmeliaHathawayPas encore d'évaluation
- Chillers VoltasDocument4 pagesChillers Voltasanil shuklaPas encore d'évaluation
- GSD Puppy Training Essentials PDFDocument2 pagesGSD Puppy Training Essentials PDFseja saulPas encore d'évaluation
- Psle Science Keywords !Document12 pagesPsle Science Keywords !Aftertea CarousellPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Coding DecodingDocument21 pagesCoding DecodingAditya VermaPas encore d'évaluation
- Islam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamDocument18 pagesIslam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamLoveth KonniaPas encore d'évaluation
- Lima Indiana Oil FieldDocument32 pagesLima Indiana Oil FieldCHARLES PATULAYPas encore d'évaluation
- SAT Practice Test 10 - College BoardDocument34 pagesSAT Practice Test 10 - College BoardAdissaya BEAM S.Pas encore d'évaluation
- Armadio Presentation-2019Document45 pagesArmadio Presentation-2019Subhash Singh TomarPas encore d'évaluation
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissD'EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissÉvaluation : 4.5 sur 5 étoiles4.5/5 (81)