Académique Documents
Professionnel Documents
Culture Documents
2 - Airway and Ventilatory Management
Transféré par
Jessie E. GeeDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2 - Airway and Ventilatory Management
Transféré par
Jessie E. GeeDroits d'auteur :
Formats disponibles
2 - AIRWAY AND VENTILATORY MANAGEMENT
1. What are common causes of early preventable deaths from airway problems after trauma? failure to recognize the need for an airway intervention inability to establish an airway failure to recognize an incorrectly placed airway displacement of a previously established airway failure to recognize the need for ventilation aspiration of gastric contents 2. Outline airway problem recognition. assess level of consciousness anticipate vomiting Particularly close attention paid to: maxillofacial trauma neck trauma laryngeal trauma 3. Airway significance of maxillofacial trauma. midface trauma - fractures and dislocations that compromise the nasopharynx and oropharynx facial fractures - hemorrhage, secretions, dislodged teeth mandibular fractures (especially bilateral) - loss of normal airway support 4. Airway significance of neck trauma. penetrating injury - vascular injury causes hemorrhage that can displace and obstruct the airway disruption of larynx or trachea - obstruction and/or severe bleeding into airways 5. Airway significance of laryngeal trauma. Presents with acute airway obstruction. Triad of clinical signs: hoarseness subcutaneous emphysema palpable fracture 6. How should laryngeal trauma + airway obstruction be managed? intubation required - flexible endoscopic intubation may be helpful if intubation unsuccessful, emergency tracheotomy surgical crichothyroidotomy is easier, though not preferred 7. How should laryngeal fracture be diagnosed? If suspected, CT will confirm. If the patient is talking, no investigation is urgent. 8. What are objective signs of airway obstruction?
Look:
Listen: noisy breathing = partial obstruction snoring, gurgling, stridor - partial occlusion of the pharynx or larynx hoarseness - functional laryngeal obstruction
Agitated or obtunded: - Agitation suggests hypoxia - Obtundation suggests hypercarbia Cyanosis - hypoxia (late sign) Accessory muscle use
Feel:
tracheal deviation 9. Ventilation problem recognition Risk factors: direct trauma to the chest elderly patients patients with preexisting pulmonary dysfunction intracranial injury cervical spinal cord injury or cervical spinal cord transection 10. Objective signs of inadequate ventilation. Look: symmetrical chest wall movement labored breathing Listen: bilateral breath sounds Pulse oximetry 11. How should helmets be removed? Two person technique: 1st person - inline stabilization 2nd person - expands helmet laterally and removes it, ensuring it clears the nose and occiput 1st person then supports the weight of the head, while 2nd person takes over inline stabilization 12. Describe the chin-lift maneuver. fingers of one hand placed under mandible mandible gently lifted upward to bring the chin anterior thumb of same hand lightly depresses the lower lip to open the mouth this maneuver should not extend the neck! 13. Describe the jaw-thrust maneuver. grasp the angles of the lower jaw, one hand on each side displace the mandible forward take care to prevent neck extension 14. Describe insertion of orophagyneal airways. airway inserted into the mouth behind the tongue normally inserted upside down, then turning around to the tip faces down into the laryngopharynx may induce gagging, vomiting and aspiration in conscious patients 15. Describe insertion of nasopharyngeal airways. inserted in one nostril and passed gently into the posterior oropharynx should be well lubricated if obstruction is noted, stop and try the other nostril 16. Role of laryngeal mask airways. established role in difficult airways however, not a definitive airway, so plans for further definitive airway placement should be made 17. Multilumen esophageal airways. used by some prehospital personnel to achieve an airway when a definitive airway is not feasible
one lumen communicates with the esophagus and the other with the airway personnel are trained to observe which lumen is which (capnography helps) requires removal and definitive airway placement ASAP 18. Laryngeal tube airways. extraglottic airway device similar to LMA not a definitive airway device, and will need replacement 19. Gum elastic bougie. also called Eschmann Tracheal Tube Introducer (ETTI) 60cm long, 15 Fr stylette, with angled tip at distal end used when vocal cords cannot be directly visualized GEB passed blindly behind the epiglottis with angled tip anteriorly tracheal position confirmed by: - clicking on tracheal rings - tube rotating left or right when entering bronchi - tube held up in bronchial tree (around 50cm mark) when ready, ETT railroaded over, and GEB removed, then tube position confirmed by conventional means 20. Define "definitive airway". Tube placed in trachea with cuff inflated. Tube connected to some form of oxygen-enric 21. Types of definitive airway. 1. orotracheal tube 2. nasotracheal t 22. What are some indications for a definitive airway. Airway protection: unconscious severe maxillofacial fractures risk of aspiration - bleeding, vomiting risk of obstruction - neck hematoma, laryngeal/tracheal injury, stridor Need for ventilation or oxygenation: apnea - neuromuscular paralysis or unconsciousness inadequate respiratory efforts severe closed head injury warranting forced hyperventilation for raised ICP 23. Outline an airway decision scheme. prepare equipment preoxygenate if unable to oxygenate, definitive or surgical airway if able to oxygenate, predict ease of intubation if easy, proceed with RSI if difficult, call help, consider awake intubation if unsuccessful, use adjunct devices (GEB, LMA, LTA) if all fails, surgical airway 24. What equipment should be ready for airway management? Facilities: suction O2 pulse oximetry
capnography assistant Airways: GEB LMA surgical or needle cricothyroidotomy kit ETT Misc equipment: drugs bag-mask laryngoscope
25. Confirming tube position. equal bilateral breath sounds + no gastric sounds capnography CXR confirmation 26. LEMON assessment for difficult intubation. L = look externally E = evaluate with 3-3-2 rule M = Mallampati O = obstruction N = neck mobility 27. What are external indicators of difficult intubation? small mouth/jaw large overbite facial trauma 28. What is the 3-3-2 rule? Assess the following relationships: distance between patient's incisors should be at least 3 finger breadths distance between hyoid bone + chin should be at least 3 finger breadths distance between thyroid notch and floor of mouth should be at least 2 finger breadths 29. What is the Mallampati score? patient asked to open mouth fully and protrude tongue as far as possible best done in a sitting position examiner looks into mouth to assess degree of hypopharynx visible: - soft palate, uvula, fauces, pillars - soft palate, uvula, fauces - soft palate, base of uvula - hard palate only 30. Describe the technique of rapid sequence induction (RSI). preparation - surgical kit available, suction available, ventilator ready, assistant ready, etc preoxygenate with 100% oxygen apply cricoid pressure give induction agent suxamethonium 1-2 mg/kg IV after fasciculations, intubate as normal inflate cuff + confirm tube placement release cricoid pressure
commence ventilation 31. What are some contraindications to suxamethonium? severe crush injuries major burns and electrical injuries chronic renal failure chronic neuromuscular disease 32. Describe the technique of jet insufflation. Large-calibre plastic cannula (12- to 14-gauge for adults, 16- to 18-gauge for children) through cricothyroid membrane. Cannula connected to oxygen at 15L/min with a Y-connected or side hole cut in tubing. Intermittent insufflation (1 sec on, 4 secs off) allows some time for expiration.
Only suitable for 30-45 minutes, and potentially dangerous due to large pressures that can build up.
Vous aimerez peut-être aussi
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightPas encore d'évaluation
- Acls Pharmacology OverviewDocument11 pagesAcls Pharmacology OverviewzoyaligPas encore d'évaluation
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiPas encore d'évaluation
- Information and Resources For Effective Self-Management of Problem Substance UseDocument52 pagesInformation and Resources For Effective Self-Management of Problem Substance Useedmidler100% (1)
- ToxidromesDocument1 pageToxidromesMayer Rosenberg100% (7)
- Anti Arrhythmic DrugsDocument91 pagesAnti Arrhythmic DrugsAlex beharuPas encore d'évaluation
- ACLS Simulation ScenariosDocument14 pagesACLS Simulation ScenariosVanessa HermionePas encore d'évaluation
- 6 PacuDocument15 pages6 PacuFarrukh Ali KhanPas encore d'évaluation
- ACLS Study GuideDocument28 pagesACLS Study GuideNicole Berry100% (1)
- BarlingFrone 2004 ThePsychologyofWorkplaceSafteyDocument336 pagesBarlingFrone 2004 ThePsychologyofWorkplaceSafteyfitrianiPas encore d'évaluation
- Acute Respiratory Distress: Section I: Scenario DemographicsDocument6 pagesAcute Respiratory Distress: Section I: Scenario DemographicsharasthaPas encore d'évaluation
- ECG InterpretationDocument11 pagesECG InterpretationAndrea AndradaPas encore d'évaluation
- Resusciation Equipments in IcuDocument29 pagesResusciation Equipments in Icuvinoli100% (1)
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDocument49 pagesAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamPas encore d'évaluation
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyPas encore d'évaluation
- PEDIATRIC ASSESSMENT OVERVIEWDocument2 pagesPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- How To Take and Read An ECG ECG BasicsDocument7 pagesHow To Take and Read An ECG ECG BasicsJessica Brittain-GeorgePas encore d'évaluation
- ACLS Drug TherapyDocument8 pagesACLS Drug TherapySahrensPas encore d'évaluation
- Bowel ObstructionDocument48 pagesBowel ObstructionPatrick John100% (1)
- PICU Common ProblemDocument49 pagesPICU Common ProblemRawabi rawabi1997Pas encore d'évaluation
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyPas encore d'évaluation
- DIT High Yield Questions PDFDocument13 pagesDIT High Yield Questions PDFjoshPas encore d'évaluation
- ILS Case Studies COMP 2020.ppsxDocument39 pagesILS Case Studies COMP 2020.ppsxKim Orven KhoPas encore d'évaluation
- Emergency Medical Procedures GuideDocument57 pagesEmergency Medical Procedures GuideDuane Liloc100% (1)
- HeartCode BLSDocument5 pagesHeartCode BLSJohn DiggPas encore d'évaluation
- Paediatric Emergencies NotesDocument6 pagesPaediatric Emergencies NotesJana AldourPas encore d'évaluation
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
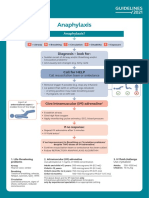
- Anaphylaxis Algorithm 2021Document1 pageAnaphylaxis Algorithm 2021Shawn Gaurav JhaPas encore d'évaluation
- Basic Ecg 2016Document75 pagesBasic Ecg 2016api-284503860Pas encore d'évaluation
- Advance Trauma Life SupportDocument67 pagesAdvance Trauma Life SupportraffellaPas encore d'évaluation
- BLS Guide Dr. Fayyaz Nishtar MedicalDocument42 pagesBLS Guide Dr. Fayyaz Nishtar MedicalShahzeb KhanPas encore d'évaluation
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- Multiple Trauma ATLSDocument36 pagesMultiple Trauma ATLSIkrima Firda MaharaniPas encore d'évaluation
- Emergency NursingDocument46 pagesEmergency NursingJoshua P AloveroPas encore d'évaluation
- Advanced Trauma Life Support RevisedDocument7 pagesAdvanced Trauma Life Support RevisedpaveethrahPas encore d'évaluation
- Emergency Medicine كتاب ايمرجنسي مفيد للروتيترز الجدد وملخص مفيدDocument46 pagesEmergency Medicine كتاب ايمرجنسي مفيد للروتيترز الجدد وملخص مفيدSri PoopasePas encore d'évaluation
- ATLS-9e Trauma Flow Sheet PDFDocument4 pagesATLS-9e Trauma Flow Sheet PDFWaeel HamoudaPas encore d'évaluation
- Bronchoscopy: Dr. Ravi Gadani MS, FmasDocument17 pagesBronchoscopy: Dr. Ravi Gadani MS, FmasRaviPas encore d'évaluation
- Alphabet-Course-Breakdown-Nccp 1Document3 pagesAlphabet-Course-Breakdown-Nccp 1api-232950579Pas encore d'évaluation
- So After ABC - Neuro-IsabilityDocument5 pagesSo After ABC - Neuro-IsabilityXavier FungPas encore d'évaluation
- 2 Approach To The Neuro Exam Feb 2011Document35 pages2 Approach To The Neuro Exam Feb 2011suaqaziPas encore d'évaluation
- CPR AED Choking Guidelines for Healthcare ProvidersDocument2 pagesCPR AED Choking Guidelines for Healthcare Providersreyes markPas encore d'évaluation
- Initial Assessment and Management: Presented by Fayez Abillama, MDDocument53 pagesInitial Assessment and Management: Presented by Fayez Abillama, MDDaniel GhosseinPas encore d'évaluation
- (Advanced Cardiac Life Support) : ACLS Algorithms 2018Document18 pages(Advanced Cardiac Life Support) : ACLS Algorithms 2018cristina100% (1)
- PARAQUAT POISIONING 3rd Block Imed COMPLIEDDocument15 pagesPARAQUAT POISIONING 3rd Block Imed COMPLIEDMohil PratapPas encore d'évaluation
- Electrocardiogramm - Ecg InterpretationDocument56 pagesElectrocardiogramm - Ecg InterpretationKreshnik HAJDARI100% (1)
- 8.the Atls ProtocolDocument57 pages8.the Atls ProtocolReuben DutiPas encore d'évaluation
- PEARS Handout 2016Document8 pagesPEARS Handout 2016Carrie DAndreaPas encore d'évaluation
- Atls MedscapeDocument5 pagesAtls MedscapeCastay GuerraPas encore d'évaluation
- Registered Respiratory TherapistDocument3 pagesRegistered Respiratory Therapistapi-76909521Pas encore d'évaluation
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiPas encore d'évaluation
- Febrile Seizure: Satanun Charoencholvanich, MDDocument10 pagesFebrile Seizure: Satanun Charoencholvanich, MDAPETT WichaiyoPas encore d'évaluation
- Me 1Document74 pagesMe 1Shaz ChindhyPas encore d'évaluation
- ACLS QuizletDocument7 pagesACLS Quizletek.9006001Pas encore d'évaluation
- Approach To PoisoningDocument107 pagesApproach To PoisoningAlex beharuPas encore d'évaluation
- Comparison of Neuromuscular Blocking Drugs: Succinylcholine, Atracurium, Cis-Atracurium, Rocuronium, VDocument1 pageComparison of Neuromuscular Blocking Drugs: Succinylcholine, Atracurium, Cis-Atracurium, Rocuronium, VMarshallMcGoughPas encore d'évaluation
- The Neuro Exam: Yes, You Really Do Have To Wake Them Up and Do ThisDocument12 pagesThe Neuro Exam: Yes, You Really Do Have To Wake Them Up and Do ThisDrGasnasPas encore d'évaluation
- 66 Neonatal Resuscitation Show Notes 1Document3 pages66 Neonatal Resuscitation Show Notes 1Rabbani IcksanPas encore d'évaluation
- Symptom Flow Chart (Difficulty Breathing)Document2 pagesSymptom Flow Chart (Difficulty Breathing)Jeff ZhouPas encore d'évaluation
- ACLS and PALS Certification Practice QuestionsDocument11 pagesACLS and PALS Certification Practice Questionsdyah rahayu hutamiPas encore d'évaluation
- Heart Assessment: Physical ExaminationDocument6 pagesHeart Assessment: Physical Examinationshannon c. lewisPas encore d'évaluation
- Chapter 1 - EMT Intro to RolesDocument2 pagesChapter 1 - EMT Intro to RolesDaniel Kipnis0% (1)
- Table1 ICU DailyGoalsSheetDocument3 pagesTable1 ICU DailyGoalsSheetekrams100% (1)
- PALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908Document3 pagesPALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908YONE LENINPas encore d'évaluation
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Newborn PQDocument6 pagesNewborn PQNurseNancy93Pas encore d'évaluation
- Dr. Ikar J. Kalogjera: Psychiatrist & Clinical Professor of PsychiatryDocument1 pageDr. Ikar J. Kalogjera: Psychiatrist & Clinical Professor of PsychiatryMWWPas encore d'évaluation
- 2.4.B DR Denni Clinical Evidence of Ribociclib Into Clinical PracticeDocument40 pages2.4.B DR Denni Clinical Evidence of Ribociclib Into Clinical Practicetepat rshsPas encore d'évaluation
- Risk Factors and Indications of Orthodontic Temporary Anchorage Devices: A Literature ReviewDocument10 pagesRisk Factors and Indications of Orthodontic Temporary Anchorage Devices: A Literature ReviewSarath KumarPas encore d'évaluation
- Alzheimer's Disease (AD), Also Referred To Simply As Alzheimer's, Is ADocument2 pagesAlzheimer's Disease (AD), Also Referred To Simply As Alzheimer's, Is ASCrIbdPas encore d'évaluation
- Free Journal List For PublicationDocument11 pagesFree Journal List For PublicationSyed Saad AliPas encore d'évaluation
- UNAIDS Core Epidemiology Slides enDocument11 pagesUNAIDS Core Epidemiology Slides enTabarcea VitaliPas encore d'évaluation
- Care of A Bedridden Patient: Prepared by Jannet Reena PuraniDocument25 pagesCare of A Bedridden Patient: Prepared by Jannet Reena PuraniAnn Merlin Jobin100% (1)
- Ejsr 72 3 04Document9 pagesEjsr 72 3 04Khalifa BakkarPas encore d'évaluation
- The Lightning-Fast Quest For COVID Vaccines - and What It Means For Other DiseasesDocument3 pagesThe Lightning-Fast Quest For COVID Vaccines - and What It Means For Other DiseasesKathiravan M NPas encore d'évaluation
- Shock and Hypoperfusion Mechanisms and TreatmentDocument46 pagesShock and Hypoperfusion Mechanisms and TreatmentIgor StefanetPas encore d'évaluation
- Daftar Obat Klinik MPHDocument3 pagesDaftar Obat Klinik MPHxballzPas encore d'évaluation
- Cannabinoids in Neuropathic PainDocument9 pagesCannabinoids in Neuropathic PainZain AmenPas encore d'évaluation
- Starting Injectable RCN PDFDocument40 pagesStarting Injectable RCN PDFPhilip HartleyPas encore d'évaluation
- Compilation Liver Cirrhosis (4) - 1Document45 pagesCompilation Liver Cirrhosis (4) - 1Nagabharana Hm HollattiPas encore d'évaluation
- PVC Unido ConDuplicadosDocument1 181 pagesPVC Unido ConDuplicadosJorge Chachaima MarPas encore d'évaluation
- Supplement-1115 2020Document216 pagesSupplement-1115 2020Laura PaunicaPas encore d'évaluation
- Brain Health Assessment by Dr. Daniel Amen #1 Brain Type QuizDocument1 pageBrain Health Assessment by Dr. Daniel Amen #1 Brain Type Quiz03.wizenedwasterPas encore d'évaluation
- The Sage Encyclopedia of Abnormal and Clinical Psychology - I36172Document5 pagesThe Sage Encyclopedia of Abnormal and Clinical Psychology - I36172Rol AnimePas encore d'évaluation
- What Are Early Indicators of Mesothelioma. Realizing The Early Signs ofDocument2 pagesWhat Are Early Indicators of Mesothelioma. Realizing The Early Signs ofthasyaPas encore d'évaluation
- SepanskiDocument13 pagesSepanskiTammy Utami DewiPas encore d'évaluation
- Isicem 2021Document90 pagesIsicem 2021labbenePas encore d'évaluation
- ICICI Lombard General Insurance Company LimitedDocument22 pagesICICI Lombard General Insurance Company LimitedAmit BansalPas encore d'évaluation
- Systemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Document8 pagesSystemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Jhanu JaguarPas encore d'évaluation
- Goku Notes - Phasmids 2Document9 pagesGoku Notes - Phasmids 2Joulo YabutPas encore d'évaluation