Académique Documents
Professionnel Documents
Culture Documents
Nervous Regulation of The Circulation and Rapid Control of Arterial Pressure
Transféré par
mcwnotes100%(2)100% ont trouvé ce document utile (2 votes)
1K vues2 pagesNerve fibers leave the spinal cord through all the thoracic spinal nerves. Sympathetic Nerve Fibers innervate the vasculature of the internal viscera and heart. Sympathetic stimulation markedly increases the activity of the heart.
Description originale:
Titre original
Nervous Regulation of the Circulation and Rapid Control of Arterial Pressure
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOC ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentNerve fibers leave the spinal cord through all the thoracic spinal nerves. Sympathetic Nerve Fibers innervate the vasculature of the internal viscera and heart. Sympathetic stimulation markedly increases the activity of the heart.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC ou lisez en ligne sur Scribd
100%(2)100% ont trouvé ce document utile (2 votes)
1K vues2 pagesNervous Regulation of The Circulation and Rapid Control of Arterial Pressure
Transféré par
mcwnotesNerve fibers leave the spinal cord through all the thoracic spinal nerves. Sympathetic Nerve Fibers innervate the vasculature of the internal viscera and heart. Sympathetic stimulation markedly increases the activity of the heart.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 2
Nervous Regulation of the Circulation, and Rapid Control of Arterial Pressure
Nervous Regulation of the Circulation
• Autonomic Nervous System
o Sympathetic Nervous System
• Sympathetic vasomotor nerve fibers leave the spinal cord through all the thoracic spinal nerves and
through the first one or two lumbar spinal nerves. They then pass immediately to a sympathetic chain.
• Two routes to the circulation: 1) Through specific sympathetic nerves that innervate the vasculature of the
internal viscera and heart and 2) immediately into peripheral portions of the spinal nerves distributed to
the vasculature of the peripheral areas
o Sympathetic Innervation of the Blood Vessels
In most tissues all the vessels except the capillaries, precapillary sphincters, and metarterioles are
innervated
Innervation of small arteries/arterioles allows sympathetic stimulation to increase resistance to blood flow
decrease rate of blood flow through tissues
Innervation of the large vessels/veins makes it possible for sympathetic stimulation to decrease the
volume of these vessels regulate heart pumping.
o Sympathetic Nerve Fibers to the Heart
Sympathetic stimulation markedly increases the activity of the heart, both increasing the heart rate and
enhancing strength/volume of pumping
o Parasympathetic Control of Heart Function, Especially Heart Rate
The parasympathetic nervous system’s most important circulatory effect is to control heart rate by way of
parasympathetic nerve fibers to the heart in the vagus nerves.
o Sympathetic Vasoconstrictor System and Its Control in the Central Nervous System
Vasomotor Center in the Brain and its Control of the Vasoconstrictor System
• Transmits parasympathetic impulses through the vagus nerve to the heart and transmits
sympathetic impulses through the spinal cord and peripheral sympathetic nerves to virtually all
arteries/arterioles/veins of the body.
• Important areas: vasoconstrictor area, vasodilator area, sensory area (tractus solitarius)
Continuous Partial Constriction of the Blood Vessels is Normally Caused by Sympathetic Vasoconstrictor
Tone
• Under normal conditions, the vasoconstrictor area of the vasomotor center transmits signals
continuously to the sympathetic vasoconstrictor nerve fibers over the entire body sympathetic
vasoconstrictor tone vasomotor tone (partial state of contraction in the blood vessels)
Control of Heart Activity by the vasomotor Center
• Heart rate/strength of heart contraction INCREASE when vasoconstriction occurs
• Heart rate/strength of heart contraction DECREASE when vasoconstriction is inhibited
Control of the Vasomotor Center by Higher Nervous Centers
Norepinephrine—The Sympathetic Vasoconstrictor Transmitter Substance
• Vasoconstrictor nerves norepinephrine alpha adrenergic receptors vasoconstriction
Adrenal Medullae and their Relation to the Sympathetic Vasoconstrictor System
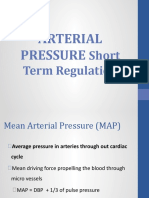
Role of the Nervous System in Rapid Control of Arterial Pressure
• RAPID INCREASES IN ARTERIAL PRESSURE (nervous control of the circulation)
• Three changes to help increase arterial pressure:
o Almost all arterioles of the systemic circulation are constricted increases total peripheral resistance
increases arterial pressure
o Veins are strongly constricted displaces blood toward the heart increases volume of blood in heart
greater pumping increases arterial pressure
o Heart is directly stimulated by the autonomic nervous system enhances cardiac pumping
• Increase in Arterial Pressure During Muscle Exercise and Other Types of Stress
• Reflex Mechanisms for Maintaining Normal Arterial Pressure (NEGATIVE FEEDBACK REFLEX MECHANISMS)
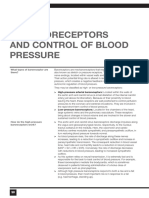
o The Baroreceptor Arterial Pressure Control System—Baroreceptor Reflexes
Stretch receptors: increased arterial pressure baroreceptors stretch signals transmitted to CNS
o Physiologic Anatomy of the Baroreceptors and their Inneration
o Response of the Baroreceptors to Pressure
Baroreceptor feedback mechanism functions most effectively in the pressure range where it is most
needed (100 mm Hg = normal operating pressure)
o Circulatory Reflex Initiated by the Baroreceptors
Baroreceptor signals tractor solitarius of medulla signals inhibit the vasoconstrictor center and
excite the vagal parasympathetic center vasocilation and decreased heart rate/strength of contraction
arterial pressure decreased
o Function of the Baroreceptors During Changes in Body Posture
o Pressure “Buffer” Function of the Baroreceptor Control System
o Are the Baroreceptors Important in Long-term Regulation of Arterial pressure?
o Control of Arterial Pressure by the Carotid and Aortic Chemoreceptors—Effect of Oxygen Lack on Arterial
Pressure
It is at the lower pressures that this reflex becomes important to help prevent still further fall in pressure.
o Atrial and Pulmonary Artery Reflexes that Help Regulate Arterial Pressure and Other Circulatory Factors
Low pressure receptors in atria and pulmonary arteries play an important role in minimizing arterial
pressure changes in response to changes in blood volume.
These receptors do not detect systemic arterial pressure but instead detect simultaneous increases in
pressure in the low pressure areas of the circulation caused by increase in volume and they elicis reflexes
parallel to the baroreceptors.
o Atrial Reflexes that Activate the Kidneys—The Volume Reflex
Stretch of the atria increase glomerular filtration (increased arteriolar resistance in the kidneys) and
decrease in reabsorption of fluid (decreased section of antidiuretic hormone by hypothalamus)
reduction of blood volume toward normal
o Atrial Reflex Control of Heart Rate (the Bainbridge Reflex)
• Central Nervous System Ischemic Response—Control of Arterial Pressure by the Brain’s Vasomotor Center in
Response to Diminished Brain Blood Flow
o Blood flow to the vasomotor center becomes decreased enough to cause nutritional deficiency (cerebral ischemia)
vasoconstrictor and cardioaccelerator neurons excited systemic arterial pressure rises
o Magnitude is TREMENDOUS
o Importance of the CNS Ischemic Response as a Regulator of Arterial Pressure
Acts as an emergency pressure control system that acts rapidly and powerfully to prevent further decrease
in arterial pressure whenever blood flow to the brain decreases close to a lethal level
o Cushing Reaction
Results from increased pressure of the CSF around the brain
CSF pressure rises compresses whole brain (including arteries) cuts off blood supply CNS
ischemic response arterial pressure rises
Special Features of Nervous Control of Arterial Pressure
• Role of the Skeletal Nerves and Skeletal Muscles in Increasing Cardiac Output and Arterial Pressure
o Abdominal Compression Reflex
o Increased Cardiac Output and Arterial Pressure Caused by Skeletal Muscle Contraction During Exercise
• Respiratory Waves in the Arterial Pressure
o During normal respiration there is usually an increase in arterial pressure during the early part of expiration
and a decrease in pressure during the remainder of the respiratory cycle
• Arterial Pressure Vasomotor Waves—Oscillation of Pressure Reflex Control Systems
o Oscillation of the Baroreceptor and Chemoreceptor Reflexes
A higher pressure excites the baroreceptors; this then inhibits the sympathetic nervous system and lowers
the pressure a few seconds later. The decreased pressure in turn reduces the baroreceptor stimulation and
allows the vasomotor center to become active once again, elevating the pressure to a high level
o Oscillation of the CNS Ischemic Response
Vous aimerez peut-être aussi
- Yardi Commercial SuiteDocument52 pagesYardi Commercial SuiteSpicyPas encore d'évaluation
- SWOT AnalysisDocument6 pagesSWOT Analysishananshahid96Pas encore d'évaluation
- Windows Keyboard Shortcuts OverviewDocument3 pagesWindows Keyboard Shortcuts OverviewShaik Arif100% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasD'EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasÉvaluation : 3 sur 5 étoiles3/5 (5)
- Basics of Duct DesignDocument2 pagesBasics of Duct DesignRiza BahrullohPas encore d'évaluation
- Marriage Gift PolicyDocument4 pagesMarriage Gift PolicyGanesh Gaikwad100% (3)
- HeartDocument4 pagesHeartArvin TaylorPas encore d'évaluation
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesPas encore d'évaluation
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesPas encore d'évaluation
- Short and Long Term Regulation and Determinants of BPDocument90 pagesShort and Long Term Regulation and Determinants of BPDan Tristam MicabaloPas encore d'évaluation
- Outstanding 12m Bus DrivelineDocument2 pagesOutstanding 12m Bus DrivelineArshad ShaikhPas encore d'évaluation
- Chap. 18 GuytonDocument4 pagesChap. 18 GuytonMarian Joyce Princess Yuque100% (2)
- Physiological Regulation of Arterial Blood PressureDocument36 pagesPhysiological Regulation of Arterial Blood PressureFrancesPas encore d'évaluation
- Nervous Regulation of Circulation and Arterial Pressure ControlDocument2 pagesNervous Regulation of Circulation and Arterial Pressure ControlOsman NazirPas encore d'évaluation
- Blood Pressure RegulationDocument35 pagesBlood Pressure Regulationبراءة أحمد السلاماتPas encore d'évaluation
- PLJ-8LED Manual Translation enDocument13 pagesPLJ-8LED Manual Translation enandrey100% (2)
- 021SAACK Burner Operating Instructions PDFDocument136 pages021SAACK Burner Operating Instructions PDFmekidmu tadesse100% (1)
- Table of Contents and Executive SummaryDocument38 pagesTable of Contents and Executive SummarySourav Ojha0% (1)
- A. What Is Balanced/objective Review or Criticism?Document11 pagesA. What Is Balanced/objective Review or Criticism?Risha Ann CortesPas encore d'évaluation
- Principles of Marketing Eighth Edition Philip Kotler and Gary ArmstrongDocument17 pagesPrinciples of Marketing Eighth Edition Philip Kotler and Gary ArmstrongJunaid KhalidPas encore d'évaluation
- Blood Pressure Regulation HandoutDocument10 pagesBlood Pressure Regulation Handoutsac50900100% (2)
- Blood Pressure Regulation SummaryDocument42 pagesBlood Pressure Regulation SummaryLouis JinPas encore d'évaluation
- Blood Pressure-For StudentsDocument79 pagesBlood Pressure-For StudentsAshok Kumar P100% (1)
- Long & Short Term Regulation of BPDocument50 pagesLong & Short Term Regulation of BPntambik21Pas encore d'évaluation
- 8 BloodpressuremechanismDocument75 pages8 BloodpressuremechanismNithya SekarPas encore d'évaluation
- Blood Pressure Regulation - SlidesDocument35 pagesBlood Pressure Regulation - Slidesمحمد السنجلاويPas encore d'évaluation
- Arterial Pressure RegulationDocument50 pagesArterial Pressure RegulationareebPas encore d'évaluation
- מצגת4Document24 pagesמצגת4Rahaf MajadlyPas encore d'évaluation
- Cardiovascular Control: Marinette Rumusud-Jambaro, MD Diplomate in Internal MedicineDocument48 pagesCardiovascular Control: Marinette Rumusud-Jambaro, MD Diplomate in Internal MedicineVerlette Roselle Aguisanda LizardoPas encore d'évaluation
- REGULATIONDocument19 pagesREGULATIONADITYAROOP PATHAKPas encore d'évaluation
- CVS PharmacologyDocument19 pagesCVS Pharmacologymug ashPas encore d'évaluation
- Lecture 8 - Neural Regulation of Cardiac Activity and Cardiac ReflexesDocument35 pagesLecture 8 - Neural Regulation of Cardiac Activity and Cardiac ReflexesVishal BalamuruganPas encore d'évaluation
- Blood PressureDocument26 pagesBlood PressureEniola DaramolaPas encore d'évaluation
- Regulasi KV 2020Document45 pagesRegulasi KV 2020Ayu Tiara FitriPas encore d'évaluation
- Blood PressureDocument22 pagesBlood Pressurenaresh sharmaPas encore d'évaluation
- Regulation of BPDocument17 pagesRegulation of BPLemon CatbaganPas encore d'évaluation
- 21 Regulation of Systemic CirculationDocument66 pages21 Regulation of Systemic Circulationsiwap34656Pas encore d'évaluation
- Cardiovascular Regulatory MechanismDocument34 pagesCardiovascular Regulatory Mechanismhia natasyaPas encore d'évaluation
- Blood PressureDocument23 pagesBlood PressuresureshPas encore d'évaluation
- CVS Regulation IIDocument33 pagesCVS Regulation IIbiradarbhagya773Pas encore d'évaluation
- Cvs 4Document4 pagesCvs 4Kim Sa-buPas encore d'évaluation
- Regulation Of ECF Volume Through Kidney FunctionDocument49 pagesRegulation Of ECF Volume Through Kidney FunctionGeorge LusanaPas encore d'évaluation
- Regulation of Arterial Pressure by the Vasomotor CenterDocument6 pagesRegulation of Arterial Pressure by the Vasomotor CenterAIKA BAYAPas encore d'évaluation
- Physiology of Blood PressureDocument4 pagesPhysiology of Blood PressureNoorPas encore d'évaluation
- Physiology of The HeartDocument34 pagesPhysiology of The Heartalyssa_marie_kePas encore d'évaluation
- Physiology of Circulation II: Pavlina Buckova M.D. 5/2014Document25 pagesPhysiology of Circulation II: Pavlina Buckova M.D. 5/2014Yurinda AndriaPas encore d'évaluation
- Heart Rate Blood PressureDocument128 pagesHeart Rate Blood PressureShubhra ShettyPas encore d'évaluation
- Barorecceptori Și Controlul Presiunilor de SângeDocument3 pagesBarorecceptori Și Controlul Presiunilor de SângeAurelia AlexandraPas encore d'évaluation
- Blood PressureDocument57 pagesBlood PressureMatende husseinPas encore d'évaluation
- Blood Pressure HomeostasisDocument7 pagesBlood Pressure HomeostasisHassan Al SinanPas encore d'évaluation
- Homeostasis of The Cardiovascular SystemDocument7 pagesHomeostasis of The Cardiovascular SystemdesbestPas encore d'évaluation
- Blood Pressure Physio AssigmentDocument16 pagesBlood Pressure Physio AssigmentNoorPas encore d'évaluation
- 8.1 Transport System in MammalsDocument41 pages8.1 Transport System in MammalsTheresa IzaPas encore d'évaluation
- Vascular System: - Arteries Arterioles - Capil ExchDocument35 pagesVascular System: - Arteries Arterioles - Capil ExchMikaelle GasparPas encore d'évaluation
- Arterial Blood Pressure and Its RegulationDocument31 pagesArterial Blood Pressure and Its RegulationKELECHI ELEJEPas encore d'évaluation
- Blood Pressure PhysiologyDocument15 pagesBlood Pressure PhysiologyNoorPas encore d'évaluation
- 24 Sistem Homeostatis Jantung DR - NiaDocument22 pages24 Sistem Homeostatis Jantung DR - NiaSurya ArhPas encore d'évaluation
- Cardiac Output & Blood Pressure ControlsDocument33 pagesCardiac Output & Blood Pressure ControlsbakuPas encore d'évaluation
- ANP 1105 Blood VesselsDocument72 pagesANP 1105 Blood VesselsMathios TigerosPas encore d'évaluation
- Untitled NotebookDocument4 pagesUntitled NotebookMohamed HamzaPas encore d'évaluation
- Physiology (Receptors)Document17 pagesPhysiology (Receptors)Omar NuhicPas encore d'évaluation
- Goal of The Cardiovascular System: Deliver Blood To All Parts of The BodyDocument20 pagesGoal of The Cardiovascular System: Deliver Blood To All Parts of The BodyNestor BalboaPas encore d'évaluation
- Shock PresentaionDocument30 pagesShock PresentaionKennedy Ng'andwePas encore d'évaluation
- Lung InflammationDocument44 pagesLung InflammationOnSolomonPas encore d'évaluation
- Cardiovascular Physiology: Cardiac Muscle, Rhythm, Cycle & OutputDocument26 pagesCardiovascular Physiology: Cardiac Muscle, Rhythm, Cycle & OutputPhai KoemhienPas encore d'évaluation
- Cardiovascular Physiology: Cardiac Output, Blood Flow ControlsDocument33 pagesCardiovascular Physiology: Cardiac Output, Blood Flow ControlsLuiz Jorge MendonçaPas encore d'évaluation
- The Cardiovascular System Parts of The Cardiovascular SystemDocument7 pagesThe Cardiovascular System Parts of The Cardiovascular SystemBrent AnosPas encore d'évaluation
- Circulatory Response To ExerciseDocument31 pagesCirculatory Response To ExerciseFarhad GulPas encore d'évaluation
- Cardio Nursing - Course Audit 2Document320 pagesCardio Nursing - Course Audit 2Ciella Dela CruzPas encore d'évaluation
- Lec11 Sem2 Cnsweek3 20110716Document15 pagesLec11 Sem2 Cnsweek3 20110716taharanaPas encore d'évaluation
- 25circulation Part 3Document15 pages25circulation Part 3Jaydave PatelPas encore d'évaluation
- CV RegulatnDocument28 pagesCV RegulatnShahin KhanPas encore d'évaluation
- Circulation II DR PavlinaDocument50 pagesCirculation II DR PavlinaErinaGeraldiPas encore d'évaluation
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesPas encore d'évaluation
- Hormone Thyroid T3, T4 Target Nuclear Receptors Of: MostDocument3 pagesHormone Thyroid T3, T4 Target Nuclear Receptors Of: MostmcwnotesPas encore d'évaluation
- NullDocument53 pagesNullmcwnotesPas encore d'évaluation
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesPas encore d'évaluation
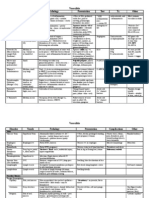
- Organ Hypothalamus Anterior Pituitary Posterior Pituitary Pineal Thyroid ParathyroidDocument1 pageOrgan Hypothalamus Anterior Pituitary Posterior Pituitary Pineal Thyroid ParathyroidmcwnotesPas encore d'évaluation
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesPas encore d'évaluation
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesPas encore d'évaluation
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesPas encore d'évaluation
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesPas encore d'évaluation
- Disorder Hyperprolactinema Adrenal Insufficiency 1° (Addison's) FSH, LHDocument2 pagesDisorder Hyperprolactinema Adrenal Insufficiency 1° (Addison's) FSH, LHmcwnotesPas encore d'évaluation
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesPas encore d'évaluation
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesPas encore d'évaluation
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDocument1 pageHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesPas encore d'évaluation
- NullDocument4 pagesNullmcwnotesPas encore d'évaluation
- People That Meet Clinical Criterion Synonymous DifferencesDocument2 pagesPeople That Meet Clinical Criterion Synonymous DifferencesmcwnotesPas encore d'évaluation
- NullDocument2 pagesNullmcwnotesPas encore d'évaluation
- Male Region Testis Tunica Albuginia Tunica Vasculosa Seminiferous TubuleDocument2 pagesMale Region Testis Tunica Albuginia Tunica Vasculosa Seminiferous TubulemcwnotesPas encore d'évaluation
- People That Meet Clinical Criterion Synonymous DifferencesDocument2 pagesPeople That Meet Clinical Criterion Synonymous DifferencesmcwnotesPas encore d'évaluation
- Changes With Aging Characteristic CV TPR Blood Vessels Renin-AngiotensinDocument2 pagesChanges With Aging Characteristic CV TPR Blood Vessels Renin-AngiotensinmcwnotesPas encore d'évaluation
- Maternal Changes During Pregnancy System Pituitary Hormone/ Parameter GHDocument1 pageMaternal Changes During Pregnancy System Pituitary Hormone/ Parameter GHmcwnotesPas encore d'évaluation
- Hormone Thyroid T3, T4 Target Nuclear Receptors Of: MostDocument2 pagesHormone Thyroid T3, T4 Target Nuclear Receptors Of: MostmcwnotesPas encore d'évaluation
- Adenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)Document2 pagesAdenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)mcwnotesPas encore d'évaluation
- Adenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)Document2 pagesAdenohypophysis Cell Type Somatotrophs (GH/Prolactin Family) Product GH (Somatotrophin)mcwnotesPas encore d'évaluation
- Prevalence The Number of Existing Cases in A PopulationDocument5 pagesPrevalence The Number of Existing Cases in A PopulationmcwnotesPas encore d'évaluation
- Lab 4 Assessment and Analysis of Cardiovascular Function inDocument2 pagesLab 4 Assessment and Analysis of Cardiovascular Function inmcwnotesPas encore d'évaluation
- Lab 4 Assessment and Analysis of Cardiovascular Function inDocument2 pagesLab 4 Assessment and Analysis of Cardiovascular Function inmcwnotesPas encore d'évaluation
- Lab 3: Computer Simulation of Cardiovascular Dynamics 1. CirculatoryDocument3 pagesLab 3: Computer Simulation of Cardiovascular Dynamics 1. Circulatorymcwnotes100% (1)
- Recent Advances in Active Metal Brazing of Ceramics and Process-S12540-019-00536-4Document12 pagesRecent Advances in Active Metal Brazing of Ceramics and Process-S12540-019-00536-4sebjangPas encore d'évaluation
- Reaction CalorimetryDocument7 pagesReaction CalorimetrySankar Adhikari100% (1)
- Sceduling and Maintenance MTP ShutdownDocument18 pagesSceduling and Maintenance MTP ShutdownAnonymous yODS5VPas encore d'évaluation
- Rivalry and Central PlanningDocument109 pagesRivalry and Central PlanningElias GarciaPas encore d'évaluation
- The Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerDocument31 pagesThe Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerCarlos Stuars Echeandia CastilloPas encore d'évaluation
- Microwave: Microwaves Are A Form ofDocument9 pagesMicrowave: Microwaves Are A Form ofDhanmeet KaurPas encore d'évaluation
- Chapter 1Document2 pagesChapter 1Nor-man KusainPas encore d'évaluation
- KG ResearchDocument257 pagesKG ResearchMuhammad HusseinPas encore d'évaluation
- Capex Vs RescoDocument1 pageCapex Vs Rescosingla.nishant1245Pas encore d'évaluation
- Developmen of Chick EmbryoDocument20 pagesDevelopmen of Chick Embryoabd6486733Pas encore d'évaluation
- Marketing of Agriculture InputsDocument18 pagesMarketing of Agriculture InputsChanakyaPas encore d'évaluation
- Ace3 1122.03 GB PDFDocument16 pagesAce3 1122.03 GB PDFArpit VermaPas encore d'évaluation
- ĐỀ CƯƠNG ANH 9 - CK2 (23-24)Document7 pagesĐỀ CƯƠNG ANH 9 - CK2 (23-24)thuyhagl2710Pas encore d'évaluation
- KCL Thesis PrintingDocument4 pagesKCL Thesis PrintingMelinda Watson100% (2)
- Service: Audi A6 1998Document256 pagesService: Audi A6 1998Kovács EndrePas encore d'évaluation
- Bosch Committed to Outsourcing to Boost CompetitivenessDocument4 pagesBosch Committed to Outsourcing to Boost CompetitivenessPriya DubeyPas encore d'évaluation
- IBM Systems Journal PerspectivesDocument24 pagesIBM Systems Journal PerspectivesSmitha MathewPas encore d'évaluation
- An RNA Vaccine Drives Expansion and Efficacy of claudin-CAR-T Cells Against Solid TumorsDocument9 pagesAn RNA Vaccine Drives Expansion and Efficacy of claudin-CAR-T Cells Against Solid TumorsYusuf DemirPas encore d'évaluation
- Irc SP 65-2005 PDFDocument32 pagesIrc SP 65-2005 PDFAjay Kumar JainPas encore d'évaluation