Académique Documents
Professionnel Documents
Culture Documents
EBM Cheat Sheet
Transféré par
NaihtneCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
EBM Cheat Sheet
Transféré par
NaihtneDroits d'auteur :
Formats disponibles
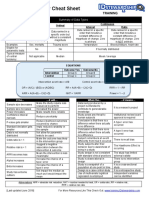
EBM Cheat Sheet- Measurements Card Basic terms Prevalence = Number of existing cases of disease at a point in time / Total
population. Notes: Numerator includes old and new cases Prevalence is cross-sectional and cannot be used to infer causation Useful in determining the burden of disease. Incidence = Number of new cases in a fixed time period / Number of people at risk. When asking Is this association a valid one? Assess the effect of chance and bias: Chance error results from random variation that occurs from sample to sample and can be assessed by the p-value. Bias or systemic error is when an error is introduced due to the design or the conduct of a study. Several types of bias exist (see box below). Validity: how closely the results of a measurement correspond to the actual value that was being measured. Failures of validity are mainly concerned with systematic errors, or bias. Reliability: how reproducible the results are if you were to repeat the measurement. E.g., Intrarater reliability = agreement between repeated results obtained by the same interviewer; Interrater reliability = agreement between results obtained by two or more different interviewers. Unreliability is mainly due to random, or chance variations. The validity of a screening test can be assessed by looking at its sensitivity, specificity, positive predictive value and negative predictive value. Sensitivity: the probability of having a positive test when the disease really is present; it is equal to the true positives divided by the sum of the true positives and the false negatives. A negative result on a highly sensitive test helps rule disease out (SNNOUT). Specificity: the probability of having a negative test when the disease is not present; it is equal to the true negatives divided by the sum of the false positives and the true negatives. A positive test result on a highly specific test helps rule in the disease (SPPIN).
Positive predictive value: the probability of the person having the disease when the test is positive; is equal to the true positives divided by the sum of the true positives and the false positives. Decreases when disease is rare. Negative predictive value: the probability of the person not having the disease when the test is negative; it is equal to the true negatives divided by the sum of the true negatives and false negatives. Forms of Bias that can influence screening results: lead-time bias = the apparent lengthening of survival due to earlier diagnosis in the course of disease without any actual prolongation of life. length-time bias = the tendency of screening to detect a larger number of cases of slowly progressing disease, but miss aggressive disease due to its rapid progression. Study Designs
Observational Designs Case reports: description of an individual patient; often intriguing but not necessarily representative. Case-series: descriptive/observational study of a series of cases. Cross-sectional surveys (aka prevalence studies): a snapshot of health data, such as exposure and disease, assessed simultaneously in a population. Often uses a representative sample and can suggest links between risk factors and disease. Case-control study: a type of observational study designed to identify (but not prove) risk factors or causal influences. People are selected according to whether they have a particular disease (cases) or do not have the disease (controls). The groups are then compared with respect to the presence or absence of the exposure now, or in the past. Indicator of risk is the odds ratio (OR). Cohort study: a type of prospective observational study in which people are selected according to the presence or absence of exposure (e.g., putative causal factors) and followed over a period of time to investigate outcomes. Indicator of risk is based on incidence of disease among exposed and unexposed people. Calculate the relative risk (RR). Experimental Designs Randomized Controlled Trial (RCT): a study in which people are randomly assigned to different exposures or interventions and the outcome of each group is measured and compared.
Case reports/ Case series
Surveys
Case-Control *
Cohort
RCT
Formulation Prevalence of of hypotheses disease; associations of risk factors with health outcomes
Identifying risk factors in rare diseases or diseases with long latency periods; evaluation of multiple exposures Recall Bias due to exposures in the past, Selection Bias if cases and controls chosen from different populations
Provides Strongest estimates of evidence for the incidence, effect of a relative & treatment attributable without the risk; good for effect of evaluating confounders multiple effects (randomness of of one exposure exposure) Selection Bias due to losses to follow-up Lack of generalizabili ty, need to assess compliance, the effect of small samples and losses to follow-up.
Results usually come from one patient or from one center
Causality cannot be inferred
*Causality criteria: These are the elements that suggest a causal relationship between a factor and the onset of disease; they include Temporal sequence, Biologic plausibility, Strength, Consistency, Dose-response, Reversibility (TeBSConDoR)
Issues in interpreting study results:
External validity or generalizability: can the results from this study be applied to other groups not part of the study? Mainly reflects quality of sampling. Internal validity refers to how well the study was undertaken: were there biases, losses to follow-up, etc? A study that is not generalizable does not necessarily mean that it is not internally valid. Confounding occurs when another factor, the confounder, produces an apparent association between an exposure and a disease. E.g., in assessing the association between coffee drinking and myocardial infarction, smoking may be a confounder, if the coffee drinkers also smoke. Confounding variables can be handled either by using randomized or stratified study designs, or by measuring the confounder and analyzing its effect using regression. Efficacy: a measure of the benefit resulting from an intervention for a given health problem under ideal conditions (e.g., all patients took all of the medication prescribed) vs. Effectiveness: a measure of the benefit resulting from an intervention for a given health problem under usual conditions of clinical care for a particular group. In an RCT, intention to treat analyses include patients who did not adhere to the treatment as though they did, making this a study of effectiveness. Clinical versus statistical significance: A result is classified as statistically significant if it is unlikely to be due to chance alone (i.e. the p value obtained upon statistical analysis is less than the critical alpha value, usually 0.05). An outcome is clinically significant if it is meaningful in the clinical setting (i.e. the difference would lead you to change your management). Note: statistical significance increases with sample size, so results can be statistically significant without being clinically significant. Number needed to treat (NNT): A measure of clinical significance. The NNT is number of patients who need to be treated in order to prevent one adverse outcome. Normal distribution: characterized by a bell-shaped and symmetrical curve, with scores more concentrated in the middle than in the ends. It is described by the mean and the standard deviation. Mean: a measure of central tendency for continuous variables. It is the sum of the scores divided by the number of cases.
Median: a measure of central tendency for a continuous variable, but used when the distribution is not normal. It is the score above and below which 50% of the observations fall. Mode: a measure of central tendency for a discrete variable (e.g., eye color). It is the most frequent score in the population (e.g., brown eyes are most common). Variance: a measure of the dispersion among the scores in a given population. First calculate the mean of the scores, then measure the amount that each score deviates from the mean and square each deviation (by multiplying it by itself). Add these squared deviations. The variance equals the average of the squared deviations from the mean. Standard deviation: the square root of the variance. Used to characterize the dispersion among the scores in a given population. Standard error: it is the standard deviation divided by the square root of the number of data values. This gives a measure of the variability of the mean (e.g., if the study were to be repeated). Hypothesis testing: statistical tests used for answering the question Is the mean/median/proportion of this group statistically different (i.e., more than expected by chance) from the value of another group? For continuous measures For discrete proportions Chi-square For medians
z-test and t-test
ANOVA
Non-parametric methods Used when data do not follow a normal distribution. Examples: Wilcoxon Rank test, MannWhitney U Test
Statistical tests used to determine whether a mean differs from the theoretical value or from another mean. Z-test for n>30 and ttest for n<30
ANalysis Of VAriance Statistical test to determine if there are significant differences between variances of multiple samples
Statistical test to determine whether an observed association between 2 categorical variables differs from the theoretical value or from each other
Other statistics often mentioned in clinical studies
Correlation: a statistical measure of the association between two variables (if you know one, how accurately could you predict the other?). Pearsons correlation is designated as r, and ranges from -1 to 1 with r = 0 being defined as no correlation. Note that correlation does not necessarily imply causation. Diseased + a c NOT Diseased d b
Odds Ratio: the odds of having been exposed if you have the disease versus if you do not, often derived from a case-control study; OR= ad/bc Relative Risk: the probability of developing the disease if you are exposed versus if you are not; RR= (a/(a+b)) / (c/(c+d)). A RR of 1.0 indicates no effect, RR=2.0 indicates double the risk; RR=0.5 half the risk. RR can be calculated from a cohort study. Regression Analysis: used to estimate the influence of one or more independent variables on a dependent variable and allows us to control for confounders. Types of regression used are based on the type of data and include: logistic regression for a discrete dependent variable, linear regression for a continuous dependent variable, Poisson regression for certain types of count data, or survival analysis for a continuous dependent variable that records the time to an event.
Vous aimerez peut-être aussi
- Recommendations for Biostatisticians in Managing and Conducting Medical Research ConsultationsD'EverandRecommendations for Biostatisticians in Managing and Conducting Medical Research ConsultationsPas encore d'évaluation
- Hang OutDocument92 pagesHang OutMadhu UpadhyayPas encore d'évaluation
- Statistics & Molecular MRCP1Document87 pagesStatistics & Molecular MRCP1Raouf Ra'fat Soliman100% (2)
- Main Menu - The Hyperlinks Below Take You To The Appropriate WorksheetDocument97 pagesMain Menu - The Hyperlinks Below Take You To The Appropriate WorksheetDineshPas encore d'évaluation
- Hierarchy of Epidemiologic Study Design: Tower & Spector, 2007Document42 pagesHierarchy of Epidemiologic Study Design: Tower & Spector, 2007Aslam BajwaPas encore d'évaluation
- Week 3 Epi Tool KitDocument2 pagesWeek 3 Epi Tool KitRicardo GomesPas encore d'évaluation
- Young Adult Stroke Prediction Using Machine LearningDocument5 pagesYoung Adult Stroke Prediction Using Machine LearningInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Biostatistics Study Cheat SheetDocument1 pageBiostatistics Study Cheat Sheetab100% (1)
- CDC Case Studies in Applied EpidemiologyDocument12 pagesCDC Case Studies in Applied Epidemiologysjab3Pas encore d'évaluation
- Introduction To Epidemiology Presented by L. MuparaDocument107 pagesIntroduction To Epidemiology Presented by L. MuparaArwen WellingtonPas encore d'évaluation
- New Basic Epi IntroDocument52 pagesNew Basic Epi Introaktaruzzaman bethuPas encore d'évaluation
- Clinical EpidemiologyDocument7 pagesClinical EpidemiologyMira Mariana UlfahPas encore d'évaluation
- Unit-I. Epidemiology IntroductionDocument60 pagesUnit-I. Epidemiology IntroductionAny OnePas encore d'évaluation
- Epidemiology ReviewDocument10 pagesEpidemiology ReviewSaurabhPas encore d'évaluation
- Foundations of EpidemiologyDocument106 pagesFoundations of EpidemiologySudaysi AbdisalamPas encore d'évaluation
- RCT Appraisal Sheets 2005 English-2Document4 pagesRCT Appraisal Sheets 2005 English-2Mahardhika AcintyaPas encore d'évaluation
- Stats Test #3 Word Cheat SheetDocument3 pagesStats Test #3 Word Cheat SheetMark StancliffePas encore d'évaluation
- Malaria Disease Prediction and Grading System: A Performance Model of Multinomial Naïve Bayes (MNB) Machine Learning in Nigerian HospitalsDocument14 pagesMalaria Disease Prediction and Grading System: A Performance Model of Multinomial Naïve Bayes (MNB) Machine Learning in Nigerian HospitalsTemitope Olufunmi AtoyebiPas encore d'évaluation
- Cohort StudyDocument37 pagesCohort Studygilbert2691Pas encore d'évaluation
- Nciph ERIC10Document5 pagesNciph ERIC10bejarhasanPas encore d'évaluation
- Epidemic Investigation 2Document10 pagesEpidemic Investigation 2Den Anacay100% (1)
- VIVA PSM 1-Briefing Dec 2014Document22 pagesVIVA PSM 1-Briefing Dec 2014Ko Ka KunPas encore d'évaluation
- Medical Statistics Made Easy For The Medical PractDocument6 pagesMedical Statistics Made Easy For The Medical PractLuming LiPas encore d'évaluation
- 3.3 Case-Control StudiesDocument5 pages3.3 Case-Control StudiesRicardo GomesPas encore d'évaluation
- Therapy - Siti Setiati Evidence Based MedicineDocument33 pagesTherapy - Siti Setiati Evidence Based MedicinejoePas encore d'évaluation
- NCDDocument157 pagesNCDrajnish2555Pas encore d'évaluation
- Epidemiology The Foundation of Public Health PDFDocument34 pagesEpidemiology The Foundation of Public Health PDFgabe18Pas encore d'évaluation
- Epi Biostats ReviewDocument6 pagesEpi Biostats ReviewJohn SobieskiPas encore d'évaluation
- Biostatistics and EpidemiologyDocument44 pagesBiostatistics and Epidemiologyانس ابوهيبة100% (1)
- Disease Surveillance in India: DR Sampath K Krishnan National Professional Officer (Communicable Diseases Surveillance)Document54 pagesDisease Surveillance in India: DR Sampath K Krishnan National Professional Officer (Communicable Diseases Surveillance)Sri Rama Suryatez KattulaPas encore d'évaluation
- ABNGBEDocument74 pagesABNGBEBezan Melese100% (1)
- 25th Edition Park Update PDFDocument34 pages25th Edition Park Update PDFjitendra33% (6)
- BMC Psychiatry: An Animated Depiction of Major Depression EpidemiologyDocument6 pagesBMC Psychiatry: An Animated Depiction of Major Depression Epidemiologyklysmanu93Pas encore d'évaluation
- Biostatistics Lecture - 1 - IntroductionDocument36 pagesBiostatistics Lecture - 1 - IntroductionDr. Mahmoud Abbas Mahmoud Al-Naimi50% (4)
- Measures of Disease Frequency NOTESDocument22 pagesMeasures of Disease Frequency NOTESSJ Jung100% (1)
- Social & Preventive MedicineDocument12 pagesSocial & Preventive Medicinedrsumanthmmc100% (1)
- Health Challenges of NepalDocument19 pagesHealth Challenges of NepalKhadga ShresthaPas encore d'évaluation
- Clinical Evaluation - Pediatrics: General DataDocument2 pagesClinical Evaluation - Pediatrics: General DataColeen VergaraPas encore d'évaluation
- 1-Introduction To EpidemiologyDocument22 pages1-Introduction To EpidemiologyANTHONY KHAOYAPas encore d'évaluation
- Case Control Study DesignDocument15 pagesCase Control Study Designgeorgeloto12Pas encore d'évaluation
- Biostatistics Take Home ExaminationDocument9 pagesBiostatistics Take Home ExaminationUsran Ali BubinPas encore d'évaluation
- My Descriptive EpidemiologyDocument34 pagesMy Descriptive Epidemiologylemon yellowPas encore d'évaluation
- Analytical EpidemiologyDocument28 pagesAnalytical EpidemiologyZuha HundalPas encore d'évaluation
- 3 Summarizing DataDocument71 pages3 Summarizing DataJoevyvamae TorrePas encore d'évaluation
- Exam 2 2002Document7 pagesExam 2 2002Abdi MahamudPas encore d'évaluation
- Biostatistics Final Tests 2017 18-1802 PDFDocument66 pagesBiostatistics Final Tests 2017 18-1802 PDFIvanes IgorPas encore d'évaluation
- Epid Chapt 1 Measurement of Health and DiseaseDocument63 pagesEpid Chapt 1 Measurement of Health and DiseaseAmanuel Maru100% (1)
- Epidemiology: Andre Bencee V. Barimbao, RMT, MLS (ASCP)Document55 pagesEpidemiology: Andre Bencee V. Barimbao, RMT, MLS (ASCP)Alondra Aran100% (2)
- Sample Size Estimation in Clinical ResearchDocument9 pagesSample Size Estimation in Clinical ResearchAshish GuptaPas encore d'évaluation
- Protokol Critical ApraisalDocument16 pagesProtokol Critical ApraisalMustika ayu lestariPas encore d'évaluation
- Study Design ComparisonDocument6 pagesStudy Design ComparisonAri Sri WulandariPas encore d'évaluation
- What Is Evidence-Based Practice (EBP)Document4 pagesWhat Is Evidence-Based Practice (EBP)Nestor BalboaPas encore d'évaluation
- Oral Epidemiology: Epidemiology. Dr. Mohamed Al-MontaserDocument58 pagesOral Epidemiology: Epidemiology. Dr. Mohamed Al-Montaserغلاها عبدوPas encore d'évaluation
- Health ResearchDocument16 pagesHealth ResearchTmanoj PraveenPas encore d'évaluation
- Frankenmuth Disease Detective Test 2014 Answer KeyDocument18 pagesFrankenmuth Disease Detective Test 2014 Answer KeyOjasw UpadhyayPas encore d'évaluation
- Drug Companion Peds 2003Document413 pagesDrug Companion Peds 2003Nisar Shaik100% (1)
- Magacyada Cudurada Iyo Waxa English Lagu Yiraahdo: Home Wararka Baargaal Maqaalo About Baargaal Nala Soo XiriirDocument6 pagesMagacyada Cudurada Iyo Waxa English Lagu Yiraahdo: Home Wararka Baargaal Maqaalo About Baargaal Nala Soo Xiriircankawaab100% (1)
- Meta-Analysis: Montarat Thavorncharoensap, Ph.D. Faculty of Pharmacy, Mahidol UniversityDocument44 pagesMeta-Analysis: Montarat Thavorncharoensap, Ph.D. Faculty of Pharmacy, Mahidol UniversityNanangPas encore d'évaluation
- Study+guide++community+medicine+2010 2011 PDFDocument55 pagesStudy+guide++community+medicine+2010 2011 PDFArvinth Guna SegaranPas encore d'évaluation
- Variables: Mesfin Kote (BSC., MPHDocument28 pagesVariables: Mesfin Kote (BSC., MPHBetii ManduPas encore d'évaluation
- Gage RR Study Quick Reference CardDocument1 pageGage RR Study Quick Reference Cardkc_p21Pas encore d'évaluation
- Class Size and Teaching Competency Template 1 1Document8 pagesClass Size and Teaching Competency Template 1 1noelroajrPas encore d'évaluation
- Masonry& Brick Arch Bridges Condition Appraisal& Remedial TreatmentDocument28 pagesMasonry& Brick Arch Bridges Condition Appraisal& Remedial Treatmentshakirhamid6687Pas encore d'évaluation
- MD Structure Hap Eoc TarapotoDocument11 pagesMD Structure Hap Eoc TarapotoazegarraPas encore d'évaluation
- Ancient History Stage 6 Persepolis ProgramDocument21 pagesAncient History Stage 6 Persepolis ProgramKarlee Whitton100% (2)
- PracressssssssDocument39 pagesPracressssssssAhdelyn ValenciaPas encore d'évaluation
- Storytelling To Enhance Speaking and Listening Skills For English Young Learners: A Case Study at Language Centers in Binh Duong ProvinceDocument8 pagesStorytelling To Enhance Speaking and Listening Skills For English Young Learners: A Case Study at Language Centers in Binh Duong ProvinceHai Hau Tran100% (1)
- Use of Millings in Pavement MaintenanceDocument121 pagesUse of Millings in Pavement MaintenanceMohiuddin AhmadPas encore d'évaluation
- An Exploratory Study To Check The Impact of COVID 19 On Investment Decision of Individual Investors in Emerging Stock Market GROUP 4Document3 pagesAn Exploratory Study To Check The Impact of COVID 19 On Investment Decision of Individual Investors in Emerging Stock Market GROUP 4Keana Cassandra TobiasPas encore d'évaluation
- SMS3033Document4 pagesSMS3033HaooonPas encore d'évaluation
- Increasing The Effectiveness of Reward Management - An Evidence-Based ApproachDocument15 pagesIncreasing The Effectiveness of Reward Management - An Evidence-Based ApproachLu HanPas encore d'évaluation
- Internet Banking in IndiaDocument4 pagesInternet Banking in IndiaMridul RainaPas encore d'évaluation
- C - Proposal ResearchDocument30 pagesC - Proposal ResearchNawaraj GhimirePas encore d'évaluation
- Using Corporate Social Responsibility As InsuranceDocument35 pagesUsing Corporate Social Responsibility As InsuranceAna RamishviliPas encore d'évaluation
- Geothermal Potential Identification of Mount Wilis Area, East Java Based On Landsat 8 by Using Semi-Quantitative and Supervised Classification MethodDocument6 pagesGeothermal Potential Identification of Mount Wilis Area, East Java Based On Landsat 8 by Using Semi-Quantitative and Supervised Classification MethodMuhammad Rizky AshariPas encore d'évaluation
- Chapter 05 A Survey of Probability ConceptsDocument43 pagesChapter 05 A Survey of Probability Conceptswindyuri67% (3)
- Chapter 11Document15 pagesChapter 11Prateek Gupta100% (1)
- Walden University Dissertation ProposalDocument6 pagesWalden University Dissertation ProposalWhoCanWriteMyPaperForMeUK100% (1)
- Finalised Vegetable Value Chain Study1Document94 pagesFinalised Vegetable Value Chain Study1Abdul Malek Sikder100% (1)
- AGMA 2015 915-1-A02Document108 pagesAGMA 2015 915-1-A02danielk32100% (1)
- SPE 525 Field Notes 6Document3 pagesSPE 525 Field Notes 6Kaela IshmaelPas encore d'évaluation
- 4.designfor AASHTO 1997Document18 pages4.designfor AASHTO 1997Aku PalsuPas encore d'évaluation
- Overview of Management Services Exercises and MCDocument3 pagesOverview of Management Services Exercises and MCAbi PiPas encore d'évaluation
- Critical Care Clinical Pharmacists PDFDocument29 pagesCritical Care Clinical Pharmacists PDFMariana RibeiroPas encore d'évaluation
- Term Paper - 113Document29 pagesTerm Paper - 113Ydron SerachPas encore d'évaluation
- Red Label Tea: Group 4Document9 pagesRed Label Tea: Group 4shruti100% (2)
- Lecture 4 - Decline Curve AnalysisDocument41 pagesLecture 4 - Decline Curve Analysisgeber39Pas encore d'évaluation
- Multiple Choice Criteria For A Good QuestionnaireDocument7 pagesMultiple Choice Criteria For A Good QuestionnaireGhitaPas encore d'évaluation
- Chevron Upp Internship Candidate List For Interview Session Chevron UPP Internship AnnouncementDocument1 pageChevron Upp Internship Candidate List For Interview Session Chevron UPP Internship AnnouncementariefPas encore d'évaluation
- Berg Balance TestDocument8 pagesBerg Balance TestMiss AAPas encore d'évaluation