Académique Documents
Professionnel Documents
Culture Documents
Clotting Mechanism
Transféré par
Lindsey SimmonsDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Clotting Mechanism
Transféré par
Lindsey SimmonsDroits d'auteur :
Formats disponibles
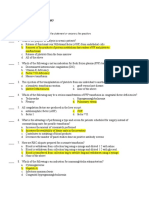
Clotting Mechanism and what helps to absorb clots pg 908-909 in text book Important proteins in the alpha and
beta fractions are the clotting factors which are made in the liver. Clotting factors including fibrinogen remain in an inactive form in the blood plasma until activated by the clotting cascade. Clotting Cascade: -First the tissue is injured resulting in: The extrinsic pathway is activated by the release of thromboplastin from the injured tissue. As a result prothrombin is converted to thrombin, which in turn catalyzes (modify/ increase) the conversion of fibrinogen to fibrin. The intrinsic pathway is activated sequentially until fibrin is ultimately formed. This is a slower process, but is most often responsible for clotting in vivo. As the injured cell is repaired and again covered with endothelial cell (inner layer of blood vessel), the fibrin clot is no longer needed. Fibrin is digested in via two systems: plasma fibrinolytic system and the cellular fibrinolytic system. Plasminogen is required to lyse (break down) the fibrin.
When the clot is no longer needed, after blood vessel is healed, the Plasminogen is activated to form plasmin. Plasmin then digests the fibrinogen and fibrin. The breakdown products are referred to as fibrin degradation products, are released into circulation. With this system clots are dissolved as tissue is repaired, and the vascular system returns to its normal state. Following damage to a blood vessel, vascular spasm occurs to reduce blood loss while other mechanisms also take effect: Blood platelets congregate at the site of damage and amass to form a platelet plug. This is the beginning of the process of the blood "breaking down" from is usual liquid form in such a way that its constituents play their own parts in processes to minimize blood loss
Thrombolytic medications are approved for the immediate treatment of stroke and heart attack. The most commonly used drug for thrombolytic therapy is tissue plasminogen activator (tPA) According to the American Heart Association, you have a better chance of surviving and recovering from a heart attack if you receive a thrombolytic drug within 12 hours after the heart attack starts. Ideally, you should receive thrombolytic medications within the first 90 minutes after arriving at the hospital for treatment. Thrombolytics work by dissolving a major clot quickly. This helps restart blood flow to the heart and helps prevent damage to the heart muscle. Thrombolytics can stop a heart attack that would otherwise be deadly. The drug restores some blood flow to the heart in most patients. However, the blood flow may not be completely normal and there may still be a small amount of muscle damaged. Additional therapy, such as cardiac catheterization or angioplasty, may be needed. Thrombolytics are not given to someone who is having a hemorrhagic stroke. They could worsen the stroke by causing increased bleeding. __________________________________________________________________________________________________ Blood Clotting is one of three mechanisms that reduce the loss of blood from broken blood vessels. 3 mechanisms are: Vascular Spasm - The smooth muscle in blood vessel walls contracts immediately the blood vessel is broken. This response reduces blood loss for some time, while the other hemostatic mechanisms become active. Platelet Plug Formation - When blood platelets encounter a damaged blood vessel they form a "platelet plug" to help to close the gap in the broken blood vessel. The key stages of this process are: platelet adhesion, platelet release reaction, and platelet aggregation
Blood Clotting (Coagulation) - As described below:
Following damage to a blood vessel, vascular spasm occurs to reduce blood loss while other mechanisms also take effect: Blood platelets congregate at the site of damage and amass to form a platelet plug. This is the beginning of the process of the blood "breaking down" from is usual liquid form in such a way that its constituents play their own parts in processes to minimise blood loss. Blood normally remains in its liquid state while it is within the blood vessels but when it leaves them the blood may thicken and form a gel (coagulation).
Blood clotting (technically "blood coagulation") is the process by which (liquid) blood is transformed into a solid state. This blood clotting is a complex process involving many clotting factors (incl. calcium ions, enzymes, platelets, damaged tissues) activating each other. The three stages of this process are: 1. Formation of Prothrombinase 2. Prothrombinase can be formed in two ways, depending of which of two "systems" or "pathways" apply. Intrinsic System o This is initiated by liquid blood making contact with a foreign surface, i.e. something that is not part of the body; or Extrinsic System o This is initiated by liquid blood making contact with damaged tissue. Both the intrinsic and the extrinsic systems involve interactions between coagulation factors. These coagulation factors have individual names but are often referred to by a standardised set of Roman Numerals, e.g. Factor VIII (antihaemophilic factor), Factor IX (Christmas factor). 3. Prothrombin converted into the enzyme Thrombin Prothrombinase (formed in stage 1.) converts prothrombin, which is a plasma protein that is formed in the liver, into the enzyme thrombin. Fibrinogen (soluble) converted to Fibrin (insoluble) In turn, thrombin converts fibrinogen (which is also a plasma protein synthesized in the liver) into fibrin. Fibrin is insoluble and forms the threads that bind the clot. Consequences of Blood Clotting Problems: If blood clots too quickly/easily then thrombosis may occur. This is blood clotting in an unbroken blood vessel, which is dangerous and can lead to strokes or heart-attacks. Conversely, if blood takes too long to clot hemorrhage may occur. In this case much blood may be lost from the blood vessels, which is also dangerous. The hereditary disorder haemophilia is a condition in which certain coagulation factors are missing from the blood, as a result of which the blood cannot form clots (without medical intervention).
Vous aimerez peut-être aussi
- The Vascular Phase: HaemostasisDocument12 pagesThe Vascular Phase: HaemostasisagestaraswitaPas encore d'évaluation
- A Simple Guide to Platelet Disorders, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Platelet Disorders, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Deep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edD'EverandDeep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edÉvaluation : 5 sur 5 étoiles5/5 (1)
- Platelet Protocols: Research and Clinical Laboratory ProceduresD'EverandPlatelet Protocols: Research and Clinical Laboratory ProceduresPas encore d'évaluation
- Laboratory Hematology PracticeD'EverandLaboratory Hematology PracticeKandice Kottke-MarchantÉvaluation : 5 sur 5 étoiles5/5 (1)
- HemophiliaA Research PaperDocument7 pagesHemophiliaA Research PaperShanePoolePas encore d'évaluation
- Topical Hemostatic Agents in Surgery PDFDocument10 pagesTopical Hemostatic Agents in Surgery PDFFernanda SouzaPas encore d'évaluation
- Anticoagulants 2019Document11 pagesAnticoagulants 2019Srijan VermaPas encore d'évaluation
- Cardio-Hepatology: Connections Between Hepatic and Cardiovascular DiseaseD'EverandCardio-Hepatology: Connections Between Hepatic and Cardiovascular DiseaseTatsunori TaniguchiPas encore d'évaluation
- Ethical Challenges of Organ Transplantation: Current Debates and International PerspectivesD'EverandEthical Challenges of Organ Transplantation: Current Debates and International PerspectivesSolveig Lena HansenPas encore d'évaluation
- Urinary System: Cytology, Histology, Cystoscopy, and RadiologyD'EverandUrinary System: Cytology, Histology, Cystoscopy, and RadiologyPas encore d'évaluation
- Haemophilia: DR Y S Vishnu Vardhan, PGDocument64 pagesHaemophilia: DR Y S Vishnu Vardhan, PGVishnu Vardhan100% (1)
- Anorectal Disorders: Diagnosis and Non-Surgical TreatmentsD'EverandAnorectal Disorders: Diagnosis and Non-Surgical TreatmentsEnrique Coss-AdamePas encore d'évaluation
- New Concepts in the Management of Septic Perianal ConditionsD'EverandNew Concepts in the Management of Septic Perianal ConditionsPas encore d'évaluation
- Lung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyD'EverandLung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyPhilip FarrellPas encore d'évaluation
- Necrotizing Fasciitis, (Flesh Eating Disease) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandNecrotizing Fasciitis, (Flesh Eating Disease) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Case Presentations in Arterial DiseaseD'EverandCase Presentations in Arterial DiseaseÉvaluation : 5 sur 5 étoiles5/5 (1)
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Hemostasis and Thrombosis: Practical Guidelines in Clinical ManagementD'EverandHemostasis and Thrombosis: Practical Guidelines in Clinical ManagementHussain I. SabaPas encore d'évaluation
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2D'EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2Pas encore d'évaluation
- Complication of Blood TransfusionDocument5 pagesComplication of Blood TransfusionChey Ochy ApriliaPas encore d'évaluation
- Pathophysiology of Ischemia Reperfusion Injury and Use of Fingolimod in CardioprotectionD'EverandPathophysiology of Ischemia Reperfusion Injury and Use of Fingolimod in CardioprotectionPas encore d'évaluation
- Treatment of Hemostasis DisordersDocument17 pagesTreatment of Hemostasis DisordersDiana HyltonPas encore d'évaluation
- Bleeding Disorders: LCDR Art GeorgeDocument54 pagesBleeding Disorders: LCDR Art Georgesatya_mdsPas encore d'évaluation
- Thrombosis and Bleeding Disorders: Theory and MethodsD'EverandThrombosis and Bleeding Disorders: Theory and MethodsNils U. BangÉvaluation : 2 sur 5 étoiles2/5 (1)
- DR Nilukshi Perera Consultant HaematologistDocument68 pagesDR Nilukshi Perera Consultant HaematologistThaveeshaLindsayWhitePas encore d'évaluation
- Advances in Cattle WelfareD'EverandAdvances in Cattle WelfareCassandra TuckerPas encore d'évaluation
- Management of Hemostasis and Coagulopathies for Surgical and Critically Ill Patients: An Evidence-Based ApproachD'EverandManagement of Hemostasis and Coagulopathies for Surgical and Critically Ill Patients: An Evidence-Based ApproachÉvaluation : 5 sur 5 étoiles5/5 (1)
- Synovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandSynovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Blood Transfusion Services in Sub Saharan Africa: Challenges and ConstraintsD'EverandBlood Transfusion Services in Sub Saharan Africa: Challenges and ConstraintsPas encore d'évaluation
- Practical Gastroenterology and Hepatology Board Review ToolkitD'EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultPas encore d'évaluation
- 1 - Factor ViiiDocument33 pages1 - Factor ViiiSukma EffendyPas encore d'évaluation
- Disseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandDisseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Blood Clotting EnzymologyD'EverandBlood Clotting EnzymologyWalter H. SeegersPas encore d'évaluation
- Scientific Advances in Reconstructive Urology and Tissue EngineeringD'EverandScientific Advances in Reconstructive Urology and Tissue EngineeringMatthias D. HoferPas encore d'évaluation
- Anaerobic Infections in HumansD'EverandAnaerobic Infections in HumansSydney FinegoldÉvaluation : 5 sur 5 étoiles5/5 (1)
- Principles and Practice of Pharmacology for AnaesthetistsD'EverandPrinciples and Practice of Pharmacology for AnaesthetistsÉvaluation : 5 sur 5 étoiles5/5 (1)
- AnemiaDocument11 pagesAnemiacentrino1780% (5)
- Prevention of DVT/PE: Noornadia BT Yahaya 050100841Document32 pagesPrevention of DVT/PE: Noornadia BT Yahaya 050100841Nadia YahayaPas encore d'évaluation
- Concept Strengthening Sheet CSS-03 Zoology: Based On AIATS-03 TYMDocument3 pagesConcept Strengthening Sheet CSS-03 Zoology: Based On AIATS-03 TYMSparsh MehtaPas encore d'évaluation
- Mclarty 2012Document7 pagesMclarty 2012Gisele CanelaPas encore d'évaluation
- Acquired Coagulation AbnormalitiesDocument6 pagesAcquired Coagulation AbnormalitiesDrMohammad MoyassarPas encore d'évaluation
- Reptilase: Haemocoagulase 1 NIH UnitDocument21 pagesReptilase: Haemocoagulase 1 NIH UnitkyawkyawhtayPas encore d'évaluation
- Biology Unit 1 BookletDocument6 pagesBiology Unit 1 Bookletbiology565Pas encore d'évaluation
- CXC Jan - 2015 - HSB 002 - AnswersDocument3 pagesCXC Jan - 2015 - HSB 002 - AnswersKyñg ShākëëlPas encore d'évaluation
- Evaluation of The Automated Coagulation Analyzer SYSMEX CA 6000Document7 pagesEvaluation of The Automated Coagulation Analyzer SYSMEX CA 6000Esther Jara GarcíaPas encore d'évaluation
- Nursing 2020 1.3 Plasma ProteinsDocument20 pagesNursing 2020 1.3 Plasma ProteinsYogesh NerkarPas encore d'évaluation
- Hemostatic Agentshemorrhage ControlDocument75 pagesHemostatic Agentshemorrhage ControlNasraldeen MohamedPas encore d'évaluation
- Hemostatic Disorder in ChildrenDocument4 pagesHemostatic Disorder in ChildrenodiliajessicanpviaPas encore d'évaluation
- Forensic Chemistry Lecture #9Document39 pagesForensic Chemistry Lecture #9kathleenPas encore d'évaluation
- Clinpath-04.-Disorders of Hemostasis and Blood CoagulationDocument11 pagesClinpath-04.-Disorders of Hemostasis and Blood CoagulationCharisse Angelica MacedaPas encore d'évaluation
- Review: Fibrinogen: Biochemistry, Epidemiology and DeterminantsDocument19 pagesReview: Fibrinogen: Biochemistry, Epidemiology and DeterminantsElma Noveria TirandaPas encore d'évaluation
- Nilai Rujukan Pemeriksaan LaboratoriumDocument18 pagesNilai Rujukan Pemeriksaan LaboratoriumHusnul Khatimah100% (1)
- CTH D Dimers May 2 2013 PDFDocument42 pagesCTH D Dimers May 2 2013 PDFRaghu NadhPas encore d'évaluation
- Bleeding Clotting DisordersDocument80 pagesBleeding Clotting DisordersDMnDLPas encore d'évaluation
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLPas encore d'évaluation
- Ncma219 Week 4Document9 pagesNcma219 Week 4Aruxi YoshiPas encore d'évaluation
- Factors Affecting CoagulationDocument4 pagesFactors Affecting CoagulationChristel Bohn GarciaPas encore d'évaluation
- Management of Severe Malaria CasesDocument100 pagesManagement of Severe Malaria CasesAshis karmakarPas encore d'évaluation
- Humaclot JuniorDocument40 pagesHumaclot JuniorJonatan Rolong Ibáñez100% (3)
- Hema2 Finalssssss PDFDocument8 pagesHema2 Finalssssss PDFMarcelino CalataPas encore d'évaluation
- Hematology Laboratory TabulationsDocument6 pagesHematology Laboratory TabulationsNathaniel SimPas encore d'évaluation
- 1 Each 2 CDocument239 pages1 Each 2 CYechale TaferePas encore d'évaluation
- Inflammation in Atrial Fibrillation: Yutao Guo, MDR, Gregory Y. H. Lip, MD, Stavros Apostolakis, MD, P DDocument8 pagesInflammation in Atrial Fibrillation: Yutao Guo, MDR, Gregory Y. H. Lip, MD, Stavros Apostolakis, MD, P DIbrahim HaidarPas encore d'évaluation
- PlateletsDocument12 pagesPlateletsSai KalyanPas encore d'évaluation
- PPT Pemeriksaan D-DIMERDocument25 pagesPPT Pemeriksaan D-DIMERDyan JeanovaPas encore d'évaluation
- Coagulation Control - Level 1 (Coag Control 1) : CAT. NO. CG 5021 Lot No. 331Cg Size: EXPIRY: 2021-10-28 GtinDocument8 pagesCoagulation Control - Level 1 (Coag Control 1) : CAT. NO. CG 5021 Lot No. 331Cg Size: EXPIRY: 2021-10-28 GtinDo PhungPas encore d'évaluation
- Basic Concepts of Hematology (Hemostasis)Document53 pagesBasic Concepts of Hematology (Hemostasis)Hendra SshPas encore d'évaluation
- MUST To KNOW in HematologyDocument45 pagesMUST To KNOW in HematologyDen100% (4)