Académique Documents
Professionnel Documents
Culture Documents
Hematology System
Transféré par
Nurse DianneDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hematology System
Transféré par
Nurse DianneDroits d'auteur :
Formats disponibles
HEMATOLOGICAL SYSTEMS
I Blood forming organs 1. Thymus removed myasthenia gravis 2. Liver largest gland 3. Lymph nodes 4. Lymphoid organs payers patch 5. Bone marrow 6. Spleen destroys RBC II Blood vessels 1. Veins SVC, IVC, Jugular vein blood towards the heart 2. Artery carries blood away from the 1. Aorta, carotid 3. Capillaries III Blood - 45% formed elements 55% plasma fluid portion of vlood. Yellow color. Serum Plasma CHONs (Produced in Liver) 1. Albumin- largest, most abundant plasma Maintains osmotic pressure preventing edema FXN: promotes skin integrity 2. Globulins alpha transports steroids Hormones & bilirubin - Transports iron & copper Gamma transport immunoglobulins or antibodies 3. Prothrombin fibrinogen clotting factor to prevent bleeding
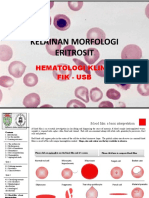
Formed Elements: 1. RBC (erythrocytes) Spleen life span = 120 days (N) 3 6 M/mm3 - Anucleated - Biconcave discs - Has molecules of Hgb (red cell pigment) Transports & carries O2
SICKLE CELL ANEMIA
sickle shaped RBC. Should be round. Impaired circulation of RBC. -immature cells hemolysis of RBC decreased hgb 3 NURSING PRIORITY: 1. a/w avoid deoxygenating activities - High altitude is bad 2. Fluid deficit promote hydration 3. Pain & comfort HGB ( HEMOGLOBIN) F= 12 14 gms % M = 14-16 gms %
Hct 3x hgb 12 x 3 = 36 (HAMATOCRIT) F 36 42% 14 x 3 = 42 M 42 48%
Average 42% - Red cell percentage in whole red Substances needed for maturation of RBC a.) Folic acid b.) Iron c.) Vit C d.) Vit B12 (cyanocobalamin) e.) Vit B6 (Pyridoxine) f.) Intrinsic factor Pregnant: 1st trimester- Folic acid prevent neural tube deficit 3rd tri iron Life span of rbc 80 120 days. Destroyed at spleen. NON-GRANULOCYTES 1. Monocytes (macrophage) - largest WBC - involved in long term phagocytes - For chronic inflammation - Other name macrophage Macrophage Macrophage Macrophage Macrophage in CNS- microglia in skin Histiocytes in lungs alveolar macrophage in Kidneys Kupffer cells
WBC leucocytes 5,000 10,000/mm3 GRANULOCYTES 1. Polymorphonuclearneutrophils Most abundant 60-70% WBC - fx short term phagocytosis For acute inflammation 2. PM Basophils -Involved in Parasitic infection - Release of chem. Mediator for inflammation Serotonin, histamine, prostaglandin, bradykinins 3. PM eosinophils - Allergic reactions
2. Lymphocytes B Cell L bone marrow or bursa dependent T cell devt of immunity- target site for HIV NK cell natural killer cell Have both antiviral & anti-tumor properties 3.Platelets (thrombocytes) N- 150,000 450, 000/ mm3 it promotes hemostasis prevention of blood loss by activating clotting - Consists of immature or baby platelets known as megakaryocytes target of virus dengue - Normal lifespan 9 12 days
Drug of choice for HIV Zidovudine (AZT or Retrovir) Standard precaution for HIV gloves, gown, goggles & mask Malaria night biting mosquito Dengue day biting mosquito Signs of platelet dysfunction: a.) Petecchiae b.) Ecchemosis/ bruises c.) Oozing or blood from venipuncture site
ANEMIA
1.) IRON DEFICIENCY ANEMIA
chronic normocytic, hypocromic (pale), microcytic anemia due to inadequate absorption of iron leading to hypoxemic injury. INCIDENCE RATE: 1. Common developed country due to high cereal intake Due to accidents common on adults 2. Common tropical countries blood sucking parasites 3. Women 15 35yo reproductive yrs 4. Common among the poor poor nutritional intake
Predisposing factor: 1. Chronic blood loss a.Trauma b. Mens c.GIT bleeding: i. Hematemesisii. Melena upper GIT duodenal cancer iii. Hematochezia lower GIT large intestine fresh blood from rectum 2. Inadequate intake of food rich in iron 3. Inadequate absorption of iron due to : a. Chronic diarrhea b. Malabsorption syndrome celiac disease-gluten free diet. Food for celiac pts- sardines c. High cereal intake with low animal CHON ingestion d. Subtotal gastrectomy 4. Improper cooking of food Signs & Symptoms: 1. Asymptomatic 2. Headache, dizziness, dyspnea, palpitations, cold sensitivity, gen body malaise, pallor 3. Brittle hair, spoon shaped nails (KOILONYCHIA)=Dec O2=hypoxia=atrophy of epidermal cells 4. Atropic glossitis, dysphagia, stomatitis 5. Pica abnormal craving for non edible food (caused by hypoxia=dec tissue perfusion=psychotic behavior) Brittle hair, spoon shaped nail atrophy of epidermal cells N = capillary refill time < 2 secs N = shape nails biconcave shape, 180 Atrophy of cells Plummer Vinsons Syndrome due to cerebral hypoxia 1. Atropic glossiti inflammation of tongue due to atrophy of pharyngeal and tongue cells 2. Stomatitis mouth sores 3. Dysphagia Diagnostic Exam: 1. RBC 2. Hgb 3. Reticulocyte 4. Hct 5. Iron 6. Ferritin Nursing Management: 1. Monitor signs of bleeding of all hema test including urine & stool 2. Complete bed rest dont overtire pt =weakness and fatigue=activity intolerance 3. Encourage iron rich food 2. Raisins, legumes, egg yolk 4. Instruct the pt to avoid taking tea - impairs iron absorption 5. Administer meds a.) Oral iron preparation Ferrous SO4 Fe gluconate Fe Fumarate Nursing Management: oral iron meds: 1. Administer with meals to lessen GIT irritation 2. If diluting in iron liquid prep adm with straw Straw 1. Lugols 2. Tetracycline 3. Oral iron 4. Macrodantine 3. Give Orange juice for iron absorption 4. Monitor & inform pts S/E a. Anorexia
b. c. d. e.
n/v Abdominal pain Diarrhea or constipation Melena
If pt cant tolerate oral iron prep administer parenteral iron prep example: 1. Iron dextran (IV, IM) 2. Sorbitex (IM) Nursing Management: parenteral iron prep 1. Administer of use Z tract method to prevent discomfort, discoloration leakage to tissues. 2. Dont massage injection site. Ambulate to facilitate absorption. 3. Monitor S/E: a.) Pain at injury site b.) Localized abscess (nana) c.) Lymphadenopathy d.) Fever/ chills e.) Urticaria itchiness f.) Hypotension anaphylactic shock Anaphylactic shock give epinephrine
2. PERNICIOUS ANEMIA
- megaloblastic, chronic anemia due to deficiency of intrinsic factor leading to * Hypochlorhydria decrease Hcl acid secretion. - Lifetime B12 injections. With CNS involvement. Predisposing factor 1. Subtotal gastrectomy removal stomach 2. Hereditary 3. Infl dse of ileum 4. Autoimmune 5. Strict vegetable diet STOMACH Parietal or ergentaffen Oxyntic cells Fxn produce intrinsic factor For reabsorption of B12 For maturation of RBC Diet high caloric or CHO to correct wt loss Signs & Symptoms: 1. Headache dizziness, dyspnea, palpitations, cold sensitivity, gen body malaise, pallor 2. GIT changes a. Red beefy tongue PATHOGNOMONIC mouth sores b. Dyspepsia indigestion c. Wt loss d. Jaundice 3. CNS Most dangerous anemia: pernicious due to neuroglogic involvement. a. Tingling sensation b. Paresthesia c. (+) Rombergs test Ataxia d. Psychosis Diagnostic Exam: Fxn secrets Hcl acid Fx aids in digestion
- Shillings test Nursing Management: 1. Enforce CBR 2. Administer B12 injections at monthly intervals for lifetime as ordered. IM- dorsogluteal or ventrogluteal. Not given oral due pt might have tolerance to drug 3. Diet high calorie or CHO. Increase CHON, iron & Vit C 4. Avoid irritating mouthwashes. Use of soft bristled toothbrush is encouraged. 5. Avoid applying electric heating pads can lead to burns
3. APLASTIC ANEMIA
stem cell disorder due to bone marrow depression leading to pancytopenia all RBC are decreased PANCYTOPENIA Decrease RBC Anemia decrease WBC leukopenia decrease platelets thrombocytopenia
Increase WBC leukocytocys Increase RBC polycythemia vera complication stroke, CVA, thrombosis Predisposing factor: 1. 2. 3. 4. Chemicals Banzene & its derivatives radiation Immunologic injury Drugs cause bone marrow depression a. Broad spectrum antibiotic - Chlorampenicol - Sulfonamides bactrim b. Chemo therapeutic agents Methotrexate alkylating agents Nitrogen mustard anti metabolic Vincristine plant alkaloid
Signs & Symptoms: 1. Anemia: a. Weakness & fatigue b. Headache, dizziness, dyspnea c. cold sensitivity, pallor d. palpitations 2. Leucopenia increase susceptibility to infection 3. Thrombocytopenia Peticchiae Oozing ofblood from venipuncture site ecchymosis Diagnostic Exam: 1. CBC pancytopenia 2. Bone marrow biopsy/ aspiration at post iliac crest reveals fatty streaks in bone marrow Nursing Management: 1. Removal of underlying cause 2. Blood transfusion as ordered 3. Complete bed rest 4. O2 inhalation 5. Reverse isolation due leukopenia 6. Monitor signs of infection 7. Avoid SQ, IM or any venipuncture site = HEPLOCK 8. Use electric razor when shaving to prevent bleeding 9. Administer meds Immunosuppresants
Anti lymphocyte globulin (Alg) given via central venous catheter, 6 days 3 weeks to achieve max therapeutic effect of drug.
DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
- Acute hemorrhagic syndrome char by wide spread bleeding & thrombosis due to a def of clotting factors (Prothrombin & Fibrinogen). Predisposing factor: 1. Rapid BT 2. Massive trauma 3. Massive burns 4. Septicemia 5. Hemolytic reaction 6. Anaphylaxis 7. Neoplasia growth of new tissue 8. Pregnancy Signs & Symptoms: 1. Petechiae widespread & systemic (lungs, lower & upper trunk) 2. Ecchymosis widespread 3. Oozing of blood from venipunctured site 4. Hemoptysis cough blood 5. Hemorrhage 6. Oliguria late sx Diagnostic Exam: 1. CBC reveals decrease platelets 2. Stool for occult blood (+) Specimen stool 3. Opthalmoscopic exam sub retinal hemorrhage 4. ABG analysis metabolic acidosis pH pH ph ph ph HCO3 PCO2 PCO2 HCO3 HCO3
R O M E
respiratory alkalosis respiratory acidosis metabolic alkalosis metabolic acidosis
Diarrhea metabolic acidosis Vomitting metabolic alkalosis Pyloric stenosis metabolic alkalosis vomiting Ileostomy or intestinal tubing metabolic acidosis Cushings metabolic alkalosis DM- metabolic acid Chronic bronchitis respiratory acid with hypoxemia, cyanosis Nursing Management 1. Monitor signs of bleeding hema test + urine, stool, GIT 2. Administer isotonic fluid solution to prevent shock. 3. Administer O2 inhalation 4. Administer meds a. Vit K aquamephyton b. Pitressin or vasopressin to conserve water. 5. NGT lavage - Use iced saline lavage 6. Monitor NGT output 7. Provide heplock 8. Prevent complication: hypovolemic shock Late signs of hypovolemic shock : anuria
BLOOD TRANSFUSION
Objectives: 1. To replace circulating blood volume 2. To increase O2 carrying capacity of blood 3. To combat infection if theres decrease WBC 4. To prevent bleeding if theres platelet deficiency
Nursing Management& Principles:
1. Proper refrigeration 2. Proper typing & crossmatching Type O universal donor AB universal recipient 85% of people is RH (+) 3. Asceptically assemble all materials needed: a.) Filter set b.) Isotonic or PNSS or .9NaCl to prevent Hemolysis Hypotonic sol swell or burst Hypertonic sol will shrink or crenate c.) Needle gauge 18 - 19 or large bore needle to prevent hemolysis. d.) Instruct another RN to recheck the following . Pts name, blood typing & cross typing expiration date, serial number. e.) Check blood unit for presence of bubbles, cloudiness, dark in color & sediments indicates bacterial contamination. Dont dispose. Return to blood bank. f.) Never warm blood products may destroy vital factors in blood. - Warming is done if with warming device only in EMERGENCY! For multiple BT. - Within 30 mins room temp only! g.) Blood transfusion should be completed < 4hrs because blood that is exposed at room temp for > 2h causes blood deterioration. h.) Avoid mixing or administering drug at BT line leads to hemolysis i.) Regulate BT 10 15 gtts/min KVO or 100cc/hr to prevent circulatory overload j.) Monitor VS before, during & after BT especially q15 mins(local board) for 1st hour. NCLEX-q5min for 1st 15min. - Majority of BT reaction occurs within 1h.
BLOOD TRANSFUSION REACTIONS
H hemolytic Reaction A allergic Reaction P pyrogenic Reaction C circulatory overload A air embolism T - thrombocytopenia C citrate intoxication expired blood =hyperkalemia H hyperkalemia
1.HEMOLYTIC REACTION
Signs & Symptoms: Headache Dizziness Dyspnea Palpitation Lumbar/ sterna/ flank pain hypotension, flushed skin , (red) port wine urine.
Nursing Management: 1. Stop BT 2. Notify Doc 3. Flush with plain NSS 4. Administer isotonic fluid sol to prevent acute tubular necrosis & conteract shock 5. Send blood unit to blood bank for reexamination 6. Obtain urine & blood samples of pt & send to lab for reexamination 7. Monitor VS & Allergic Rxn
2.ALLERGIC REACTION
Signs & Symptoms: 1. Fever/ chills 2. Urticaria/ pruritus 3. Dyspnea 4. Laryngospasm/ bronchospasm 5. Bronchial wheezing Nursing Management: 1. Stop BT 2. Notify Doc 3. Flush with PNSS 4. Administer antihistamine diphenhydramine Hcl (Benadryl). Give bedtime.SE-Adult-drowsiness. Childhyperactive If (+) Hypotension anaphylactic shock administer epinephrine 5. Send blood unit to blood bank 6. Obtain urine & blood samples send to lab 7. Monitor VS & IO 8. Adm. Antihistamine as ordered for AllergicRxn, if (+) to hypotension indicates anaphylactic shock 3. administer epinephrine 9. Adm antipyretic & antibiotic for pyrogenic Rxn & TSB
3.PYROGENIC REACTION
Signs & Symptoms: a.) Fever/ chills b.) Headache c.) Dyspnea d. tachycardia e. palpitations f. diaphoresis
Nursing Management: 1. Stop BT 2. Notify Doc 3. Flush with PNSS 4. Administer antipyretics, antibiotics 5. Send blood unit to blood bank 6. Obtain urine & blood samples send to lab 7. Monitor VS & IO 8. Tepid sponge bath offer hypothermic blanket
4. CIRCULATORY OVERLOAD
Signs & Symptoms: b. Dyspnea c. Orthopnea d. Rales or crackles e. Exertional discomfort Nursing Management: 1. Stop BT 2. Notify Doc. Dont flush due pt has circulatory overload. 3. Administer diuretics
PRIORITY CASES Hemolytic Rxn 1st due to hypotension 1st priority attend to destruction of Hgb O2 brain damage Allergic 3rd Pyrogenic 4th Circulatory 2nd Hemolytic 2nd Anaphylitic 1st priority
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- OncologyDocument3 pagesOncologyNurse DiannePas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Neuro SystemDocument22 pagesNeuro SystemNurse DiannePas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- E. A. D. A.: Gastrointestinal SystemDocument9 pagesE. A. D. A.: Gastrointestinal SystemDominic ReambonanzaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Circulatory SystemDocument9 pagesCirculatory SystemNurse DiannePas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Integumentary SystemDocument2 pagesIntegumentary SystemNurse DiannePas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- 6sterss Adaptation, Homeostasis PHYSIOLOGIC RESPONSESDocument6 pages6sterss Adaptation, Homeostasis PHYSIOLOGIC RESPONSESNurse DiannePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Gut SystemDocument8 pagesGut SystemNurse DiannePas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Endo SystemDocument21 pagesEndo SystemNurse DiannePas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- NutritionDocument1 pageNutritionNurse DiannePas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- 5asepsis & Infection ControlDocument9 pages5asepsis & Infection ControlNurse DiannePas encore d'évaluation
- 3concepts of Man & His Basic Human NeedsDocument2 pages3concepts of Man & His Basic Human NeedsNurse DiannePas encore d'évaluation
- 4concepts of Health and IllnessDocument2 pages4concepts of Health and IllnessNurse DiannePas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- 2nursing Leaders in The PhilippinesDocument1 page2nursing Leaders in The PhilippinesNurse DiannePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- 1nursing Basic TheoriesDocument3 pages1nursing Basic TheoriesNurse DiannePas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hepatobiliary DisorderDocument19 pagesHepatobiliary DisorderNurse DiannePas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Wave of WisdomDocument104 pagesWave of WisdomRasika Kesava100% (1)
- Method Statement For Wall Panels InstallationDocument11 pagesMethod Statement For Wall Panels InstallationChristos LoutrakisPas encore d'évaluation
- DDAL05-02 The Black RoadDocument45 pagesDDAL05-02 The Black Roadlpokm100% (1)
- Questions DR JekyllDocument4 pagesQuestions DR JekyllMaRiePas encore d'évaluation
- Promotion From Associate Professor To ProfessorDocument21 pagesPromotion From Associate Professor To ProfessorKamal KishorePas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Modulo InglesDocument8 pagesModulo InglesJames Mosquera GarciaPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Checklist For HR Audit Policy and ProceduresDocument3 pagesChecklist For HR Audit Policy and ProcedureskrovvidiprasadaraoPas encore d'évaluation
- Chrome Settings For CameraDocument6 pagesChrome Settings For CameraDeep BhanushaliPas encore d'évaluation
- 2006 - Bykovskii - JPP22 (6) Continuous Spin DetonationsDocument13 pages2006 - Bykovskii - JPP22 (6) Continuous Spin DetonationsLiwei zhangPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- KG Technologies Inc Metric: K119X-DX024P-1AT-90A-C399Document2 pagesKG Technologies Inc Metric: K119X-DX024P-1AT-90A-C399Bhushan PAwarPas encore d'évaluation
- Something About UsDocument18 pagesSomething About UsFercho CarrascoPas encore d'évaluation
- Modern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFDocument37 pagesModern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFRichardThompsonpcbd100% (9)
- Vaccination Consent Form: Tetanus, Diphtheria / Inactivated Polio Vaccine (DTP) & Meningococcal ACWY (Men ACWY)Document2 pagesVaccination Consent Form: Tetanus, Diphtheria / Inactivated Polio Vaccine (DTP) & Meningococcal ACWY (Men ACWY)meghaliPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Relation of Sociology with other social sciencesDocument4 pagesRelation of Sociology with other social sciencesBheeya BhatiPas encore d'évaluation
- Subject Object Schede PDFDocument28 pagesSubject Object Schede PDFanushhhkaPas encore d'évaluation
- People V Gona Phil 54 Phil 605Document1 pagePeople V Gona Phil 54 Phil 605Carly GracePas encore d'évaluation
- Ohp (2171912)Document8 pagesOhp (2171912)rajushamla9927Pas encore d'évaluation
- Doña PerfectaDocument317 pagesDoña PerfectadracbullPas encore d'évaluation
- 6 Holly Fashion Case StudyDocument3 pages6 Holly Fashion Case StudyCaramalau Mirela-Georgiana0% (1)
- Endoplasmic ReticulumDocument4 pagesEndoplasmic Reticulumnikki_fuentes_1100% (1)
- 5528 L1 L2 Business Admin Unit Pack v4Document199 pages5528 L1 L2 Business Admin Unit Pack v4Yousef OlabiPas encore d'évaluation
- All Over AgainDocument583 pagesAll Over AgainJamie Kris MendozaPas encore d'évaluation
- 13 Years of Unremitting Tracking of Chinese Scientists To Find The Source of SARS Virus - NewsDocument14 pages13 Years of Unremitting Tracking of Chinese Scientists To Find The Source of SARS Virus - NewsWillSmathPas encore d'évaluation
- Times Leader 04-10-2013Document37 pagesTimes Leader 04-10-2013The Times LeaderPas encore d'évaluation
- Leaflet STP2025 LightDocument2 pagesLeaflet STP2025 LightNoel AjocPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Kelainan Morfologi EritrositDocument19 pagesKelainan Morfologi EritrositAdel shbelPas encore d'évaluation
- Topic 8 - Managing Early Growth of The New VentureDocument11 pagesTopic 8 - Managing Early Growth of The New VentureMohamad Amirul Azry Chow100% (3)
- Sarawak Energy FormDocument2 pagesSarawak Energy FormIvy TayPas encore d'évaluation
- Full Download Test Bank For Macroeconomics 11th Edition Arnold PDF Full ChapterDocument36 pagesFull Download Test Bank For Macroeconomics 11th Edition Arnold PDF Full Chaptervitalizefoothook.x05r100% (17)
- Specification For Diesel Engines: AugustDocument19 pagesSpecification For Diesel Engines: AugustSerge RINAUDOPas encore d'évaluation