Académique Documents
Professionnel Documents
Culture Documents
Meta-Analysis: Method For Quantitative Data Synthesis: Martin Bland
Transféré par
mphil.ramesh0 évaluation0% ont trouvé ce document utile (0 vote)
15 vues14 pagesResearch
Titre original
Hi
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentResearch
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
15 vues14 pagesMeta-Analysis: Method For Quantitative Data Synthesis: Martin Bland
Transféré par
mphil.rameshResearch
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 14
1
Department of Health Sciences
M.Sc. in Evidence Based Practice, M.Sc. in Health
Services Research
Meta-analysis: method for
quantitative data synthesis
Martin Bland
Professor of Health Statistics
University of York
http://martinbland.co.uk/msc/
Adapted from work by Seokyung Hahn
What is a meta-analysis?
An optional component of a systematic review.
A statistical technique for summarising the results of
several studies into a single estimate.
What does it do?
identifies a common effect among a set of studies,
allows an aggregated clearer picture to emerge,
improves the precision of an estimate by making
use of all available data.
2
When can you do a meta-analysis?
When more than one study has estimated the effect
of an intervention or of a risk factor,
when there are no differences in participants,
interventions and settings which are likely to
affect outcome substantially,
when the outcome in the different studies has been
measured in similar ways,
when the necessary data are available.
A meta-analysis consists of three main
parts:
a pooled estimate and confidence interval for the
treatment effect after combining all the studies,
a test for whether the treatment or risk factor effect
is statistically significant or not (i.e. does the effect
differ from no effect more than would be expected
by chance?),
a test for heterogeneity of the effect on outcome
between the included studies (i.e. does the
effect vary across the studies more than would be
expected by chance?).
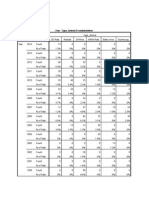
Example: migraine and ischaemic stroke
BMJ 2005; : 63- .
3
Example: metoclopramide compared with
placebo in reducing pain from acute
migraine
BMJ 2004; 329: 1369-72.
Types of meta-analysis
Meta-analysis can be done whenever we have more
than one study addressing the same issue
Interventions: usually randomised
trials to give treatment effect.
Epidemiological: usually case-control and cohort
studies to give relative risk.
Diagnostic: combined estimates of sensitivity,
specificity, positive predictive value.
In this lecture I shall concentrate on clinical trials, but
the principles are the same.
Summary statistics
Calculate a summary statistic for each
trial calculate an estimate of treatment
effect for each trial
Common effect is then calculated by averaging
the individual study effects
BUT a simple average would treat all the trials as if
they were of equal value.
Some trials have more information than others, e.g.
are larger.
We weight the trials before we average them.
4
Weighted average
1. Define weights which reflect the importance of the
trial.
2. E.g. weight = 1/variance of trial estimate
= 1/standard error squared.
3. Multiply each trial difference by its weight and add.
4. Divide by sum of weights.
high variance low amount of information
low weight
low variance high amount of information
high weight
General framework for pooling results
the pooled estimate is basically a summary
measure of the results of the included trials,
the pooled estimate is a weighted combination of
the results from the individual trials,
the weight given to each trial is the inverse of the
variance of the summary measure from each of the
individual trials,
therefore, more precise estimates from larger trials
with more events are given more weight.
Then find 95% confidence interval and P value for
the pooled difference.
Methods of meta-analysis
There are several different ways to produce the pooled
estimate:
inverse-variance weighting,
Mantel-Haenszel method,
Peto method,
DerSimonian and Laird method.
Slightly different solutions to the same problem.
5
Heterogeneity
Studies differ in terms of
Patients
Interventions
Outcome definitions
Design
Clinical heterogeneity
Variation in true treatment effects in magnitude
or direction
Statistical heterogeneity
Heterogeneity
Statistical heterogeneity may be caused by
clinical differences between trials
methodological differences between trials
unknown trial characteristics
Even if studies are clinically homogeneous there
may be statistical heterogeneity
Heterogeneity
How to identify statistical heterogeneity
Test the null hypothesis that the trials all have the
same treatment effect in the population.
The test looks at the differences between observed
treatment effects for the trials and the pooled treatment
effect estimate.
Square, divide by variance, sum.
This gives a chi-squared test with degrees of freedom
= number of studies 1.
6
Heterogeneity
Test for heterogeneity:
2
= 4.91, df = 2, P=0.086.
Heterogeneity
Significant heterogeneity
differences between trials exist
it may be invalid to pool the results and
generate a single summary result
describe variation
investigate sources of heterogeneity
account for heterogeneity
Heterogeneity
Heterogeneity not significant
No statistical evidence for difference between trials
But, test for heterogeneity has low power - the
number of studies is usually low - and may fail to
detect heterogeneity as statistically significant when
it exists.
This cannot be interpreted as evidence of
homogeneity.
To compensate for the low power of the test a
higher significance level is sometimes taken, P < 0.1
for statistical significance.
7
Types of outcome measure
Choice of measure of treatment effect depends on type of
outcome variable:
Dichotomous
e.g. dead/alive, success/failure, yes/no
relative risk or risk ratio (RR), odds ratio (OR), absolute
risk difference (ARD)
Continuous
e.g. weight loss, blood pressure
mean difference (MD), standardised mean
difference(SMD)
Types of outcome measure
Choice of measure of treatment effect depends on type of
outcome variable:
Time-to-event or survival time
e.g. time to death, time to recurrence, time to healing
Hazard ratio
Ordinal (very rare)
outcome categorised with an ordering to the categories
e.g. mild/moderate/severe, score on a scale
Dichotomise, treat as continuous, advanced methods.
Dichotomous outcome measure
Relative risk (RR), odds ratio (OR), absolute risk
difference (ARD).
Relative risk and odds ratio both use logarithmic scales.
Why is this?
Example: ulcer healing (Fletcher et al., 1997)
elastic bandage: 31 healed out of 49 patients
inelastic bandage: 26 healed out of 52 patients.
RR = (31/49)/(26/52) = 1.27 (elastic over inelastic)
RR = (26/52)/(31/49) = 0.79 (inelastic over elastic)
We want a scale where 1.27 and 0.79 are equivalent.
Fletcher A, Nicky Cullum N, Sheldon TA. (1997) A systematic review of
compression treatment for venous leg ulcers. BMJ 315: 576-580 .
8
Dichotomous outcome measure
RR = (31/49)/(26/52) = 1.273 (elastic over inelastic)
RR = (26/52)/(31/49) = 0.790 (inelastic over elastic)
We want a scale where 1.273 and 0.790 are equivalent.
Should be equally far from 1.0, the null hypothesis value.
Logarithmic scale:
log
10
(1.273) = 0.102, log
10
(0.790) = 0.102
log
10
(1) = 0 (null hypothesis value)
log
10
(1/2) = 0.301, log
10
(2) = +0.301
Logarithmic scale, risk ratio:
Interventions for
the prevention of
falls in older
adults, pooled
risk ratio of
participants who
fell at least once.
BMJ 2004; :
680-3.
Logarithmic scale, odds ratios:
Rates of Caesarean section in trials of nulliparous women
receiving epidural analgesia or parenteral opioids.
2004; : 1410-12.
9
Logarithmic scales:
For both relative risk and odds ratio we find the standard
error of the log ratio rather than the ratio. The log ratio
also tends to have a Normal distribution. On the
logarithmic scale, confidence intervals are symmetrical.
Data of Fletcher A, Cullum N, Sheldon TA. (1997) A systematic review of
compression treatment for venous leg ulcers. BMJ 315: 576-580 .
0
1
2
3
4
R
a
t
i
o
o
f
p
e
r
c
e
n
t
a
g
e
h
e
a
l
e
d
1 2 3 Pooled
Study number
RR, natural scale
.
5
1
2
3
4
R
a
t
i
o
o
f
p
e
r
c
e
n
t
a
g
e
h
e
a
l
e
d
1 2 3 Pooled
Study number
RR, logarithmic scale
Logarithmic scales:
For both relative risk and odds ratio we find the standard
error of the log ratio rather than the ratio. The log ratio
also tends to have a Normal distribution. On the
logarithmic scale, confidence intervals are symmetrical.
Data of Fletcher A, Cullum N, Sheldon TA. (1997) A systematic review of
compression treatment for venous leg ulcers. BMJ 315: 576-580 .
.
5
1
5
1
0
O
d
d
s
r
a
t
i
o
,
h
e
a
l
e
d
1 2 3 Pooled
Study number
OR, logarithmic scale
0
2
4
6
8
1
0
O
d
d
s
r
a
t
i
o
,
h
e
a
l
e
d
1 2 3 Pooled
Study number
OR, natural scale
Continuous outcome variable
Measures of treatment effect for continuous outcome:
Weighted Mean Difference:
-- same units as observations.
-- useful when the outcome is always the same
measurement,
-- usually physical measurements.
Standardised Mean Difference:
-- standard deviation units,
-- same as effect size,
-- useful when the outcome is not always the same
measurement,
-- often psychological scales.
10
Continuous outcome variable
Example of weighted mean difference
Blood pressure control by home monitoring.
BMJ 2004; 329: 145-9.
Continuous outcome variable
Data required:
mean,
standard deviation,
sample size,
for each group.
For each study, we then find the difference between
means and its standard error in the usual way.
For standardised differences, we divide the difference
between means by the standard deviation.
Everything is then in the same units, i.e. standard
deviation units.
Continuous outcome variable
Example of standardised mean difference: pain
scales
Non-steroidal anti-inflammatory drugs, including cyclo-
oxygenase-2 inhibitors, in osteoarthritic knee pain.
BMJ 2004; 329: 1317.
11
Continuous outcome variable
Data required: mean, standard deviation, sample size.
Unfortunately, these are not always available for all
published studies.
Trials sometimes report different measure of variation:
standard errors
confidence intervals
reference ranges
interquartile ranges
range
significance test
P value
Not significant or P<0.05.
Continuous outcome variable
Extracting the standard deviation:
standard errors straightforward
confidence intervals straightforward
reference ranges straightforward
interquartile ranges needs assumption about distribution
range estimates unstable and affected by outliers
significance test can work back from a t value
P value can work back to a t value hence to SD.
Not significant or P<0.05 hopeless.
Time to event outcome variables
Time-to-event data arise whenever we have subjects
followed over time until some event takes place.
Often called survival data.
Techniques also used for:
time to recurrence of disease,
time to discharge from hospital,
time to readmission to hospital,
time to conception,
time to fracture,
etc.
12
Time to event outcome variables
Time-to-event data arise whenever we have subjects
followed over time until some event takes place.
Problem: not all subjects have an event.
We know only that they were observed to be event-free up
to some point, but not beyond it.
Usually some of those observed not to have an event were
observed for a shorter time than some of those who did
have an event.
Statistical techniques: survival analysis.
Time to event outcome variables
The main effect measure is the hazard ratio.
Standard outcome measure in survival analysis.
The ratio of the risk of having an event at any given time in
one group divided by the risk of an event in the other.
Time to event outcome variables
Example: time to visual field loss or deterioration of the
optic disc, or both, in patients with ocular hypertension
Hazard ratio = 1.0 represents no difference between the
groups.
(BMJ 2005; 331: 134. )
13
Time to event outcome variables
Hazard ratio is active treatment divided by no treatment, so
if the hazard ratio is less than one, this means that the risk
of visual field loss is less for patients given pressure
lowering treatment.
As for risk ratios and odds ratios, hazard ratios are
analysed by taking the log and the results are shown on a
logarithmic scale.
Individual patient data meta-analysis
In this kind of meta-analysis, we get the raw data from each
trial.
We can combine them into a single data set. We then
analyse them like a single, multicentre clinical trial.
Alternatively, we may use the individual data to extract the
corresponding summary statistics from each study then
proceed as we would using summary statistics from
published reports.
Example: Exercise training meta-analysis of trials in patients
with chronic heart failure (ExTraMATCH) (BMJ 2004; 328:
189 ).
Nine trials identified. Principal investigators provided a
minimum data set in electronic form.
Individual patient data meta-analysis
Example: Exercise training
meta-analysis of trials in
patients with chronic heart
failure --- survival curves
The Kaplan Meier survival
curve shows the estimated
proportion of subjects who
have not yet experienced
the event at each time.
14
More results from ExTraMATCH: outcome variable time to
death
Individual study
results are not
given.
This plot shows
only the effects of
prognostic
variables.
As it is a survival
analysis, the effect
is presented as a
hazard ratio.
Log scale is used.
And finally,
Meta-analysis is straightforward if the data are
straightforward and all available.
It depends crucially on the data quality and the
completeness of the study ascertainment.
Vous aimerez peut-être aussi
- Concise Biostatistical Principles & Concepts: Guidelines for Clinical and Biomedical ResearchersD'EverandConcise Biostatistical Principles & Concepts: Guidelines for Clinical and Biomedical ResearchersPas encore d'évaluation
- EBM Cheat SheetDocument7 pagesEBM Cheat SheetNaihtnePas encore d'évaluation
- 2018 JAMA Random Effects MA Serguiou StylianosDocument2 pages2018 JAMA Random Effects MA Serguiou StylianosOscar PoncePas encore d'évaluation
- Concise Epidemiologic Principles and Concepts: Guidelines for Clinicians and Biomedical ResearchersD'EverandConcise Epidemiologic Principles and Concepts: Guidelines for Clinicians and Biomedical ResearchersPas encore d'évaluation
- What Are Confidence Intervals and P-Values?Document8 pagesWhat Are Confidence Intervals and P-Values?Mostafa Abdelrahman0% (1)
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyD'EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyÉvaluation : 1 sur 5 étoiles1/5 (1)
- Internet Source StatsDocument50 pagesInternet Source StatsDchye DrPas encore d'évaluation
- Biostatistics Explored Through R Software: An OverviewD'EverandBiostatistics Explored Through R Software: An OverviewÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Expe FinalsDocument8 pagesExpe FinalsAirame Dela RosaPas encore d'évaluation
- Patients - Intervention - Comparison - Outcome(s) - Knowledge GapDocument4 pagesPatients - Intervention - Comparison - Outcome(s) - Knowledge GapAmal NajiPas encore d'évaluation
- RCT Appraisal Sheets 2005 English-1 1Document5 pagesRCT Appraisal Sheets 2005 English-1 1api-479716004Pas encore d'évaluation
- Worksheet Appraisal AZALEADocument5 pagesWorksheet Appraisal AZALEAArini NurlelaPas encore d'évaluation
- 5 - Meta-AnalysesDocument20 pages5 - Meta-AnalysesAlvaro SalazarPas encore d'évaluation
- Prettified EBM Notes NUDocument15 pagesPrettified EBM Notes NUCamille DavisPas encore d'évaluation
- 5 How To Analyze Your Data: Nonparametric ParametricDocument18 pages5 How To Analyze Your Data: Nonparametric ParametricSubhankar SanyalPas encore d'évaluation
- Clinical Measurement Categorical and Continuous Data TypesDocument15 pagesClinical Measurement Categorical and Continuous Data TypesConnorPas encore d'évaluation
- Standardized Mortality Ratio (SMR)Document2 pagesStandardized Mortality Ratio (SMR)coolradishPas encore d'évaluation
- RCT Appraisal Sheets 2005 EnglishDocument4 pagesRCT Appraisal Sheets 2005 EnglishAmanda SoebadiPas encore d'évaluation
- Sample Size Determination in Health StudiesDocument88 pagesSample Size Determination in Health Studiesedwinclifford100% (1)
- Evidence Based Medicine & Basic Critical AppraisalDocument47 pagesEvidence Based Medicine & Basic Critical AppraisalMohmmed Abu MahadyPas encore d'évaluation
- EBM Review: B.BarkerDocument86 pagesEBM Review: B.BarkerdioneeliefmanPas encore d'évaluation
- Determination of Sample SizeDocument9 pagesDetermination of Sample SizeSushant SharmaPas encore d'évaluation
- EBP TextbookNotesDocument9 pagesEBP TextbookNotesGeri TohPas encore d'évaluation
- Mbe - Interpreting and Understanding Meta-Analysis GraphsDocument4 pagesMbe - Interpreting and Understanding Meta-Analysis GraphsRaymundoLauroTijerinaGarciaPas encore d'évaluation
- CHAPTER 7 - Research 10 1Document8 pagesCHAPTER 7 - Research 10 1hiroe sagaraPas encore d'évaluation
- Subgroup Analysis TDDocument23 pagesSubgroup Analysis TDapi-535481376Pas encore d'évaluation
- Referat Iktiosis PembahasanDocument4 pagesReferat Iktiosis PembahasanPatih GajahmadaPas encore d'évaluation
- Sample Size: How Many Is Enough?: Elizabeth Burmeister BN, MSC, Leanne M. Aitken RN, PHDDocument4 pagesSample Size: How Many Is Enough?: Elizabeth Burmeister BN, MSC, Leanne M. Aitken RN, PHDnurulaqidahmahadiPas encore d'évaluation
- Robey - 1998 - A Meta-Analysis of Clinical Outcomes in The TreatmDocument4 pagesRobey - 1998 - A Meta-Analysis of Clinical Outcomes in The TreatmJEREMY RAPas encore d'évaluation
- Statistical Significance Versus Clinical ImportanceDocument5 pagesStatistical Significance Versus Clinical ImportanceKaren Sanchez AcostaPas encore d'évaluation
- Critical Appraisal of Articles On TherapyDocument46 pagesCritical Appraisal of Articles On TherapyAditya Rachman Van Der ArjunaqueePas encore d'évaluation
- Centralised Computer Randomisation Is: Critical Appraisal For Therapy ArticlesDocument4 pagesCentralised Computer Randomisation Is: Critical Appraisal For Therapy ArticleshadzaliegPas encore d'évaluation
- Make A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdiDocument12 pagesMake A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdinaotonaoiPas encore d'évaluation
- Meta-Analysis of Screening and Diagnostic TestsDocument12 pagesMeta-Analysis of Screening and Diagnostic TestsLaurens KramerPas encore d'évaluation
- Application of Statistical Test in Clinical ResearchDocument9 pagesApplication of Statistical Test in Clinical ResearchDanny100% (1)
- Critical Apprasial EbmDocument64 pagesCritical Apprasial Ebmmisbah_mdPas encore d'évaluation
- Medpage Guide To Epi and BiostatisticsDocument11 pagesMedpage Guide To Epi and Biostatisticsnet2020100% (1)
- Critical Therapy Study ResultsDocument4 pagesCritical Therapy Study ResultsAinur 'iin' RahmahPas encore d'évaluation
- Patients - Intervention - Comparison - Outcome(s)Document4 pagesPatients - Intervention - Comparison - Outcome(s)sahirbulePas encore d'évaluation
- Kritisi Artikel - Ni Nengah Susilawati - 152191105 - BDocument5 pagesKritisi Artikel - Ni Nengah Susilawati - 152191105 - BShilaPas encore d'évaluation
- Worksheet Therapy-CebmDocument3 pagesWorksheet Therapy-Cebmteddy sPas encore d'évaluation
- Critical Appraisal for Therapy ArticlesDocument4 pagesCritical Appraisal for Therapy ArticlesMahardhika AcintyaPas encore d'évaluation
- Clinical Versus Actuarial Judgment: Methods of Judgment and Means of ComparisonDocument19 pagesClinical Versus Actuarial Judgment: Methods of Judgment and Means of ComparisonanguschandlerPas encore d'évaluation
- Randomised: Differences Between Groups Are Statistically Significant P ValuesDocument6 pagesRandomised: Differences Between Groups Are Statistically Significant P ValuesArga PRPas encore d'évaluation
- ContinuousDocument11 pagesContinuousDinaol TikuPas encore d'évaluation
- Biostatics Freework - Ahlin AshrafDocument16 pagesBiostatics Freework - Ahlin Ashrafab JafarPas encore d'évaluation
- Analisis RCT Continuous Outcome - Google SearchDocument13 pagesAnalisis RCT Continuous Outcome - Google SearchRaudhatulAisyFachrudinPas encore d'évaluation
- IMG EPIDEMIOLOGY STUDY GROUPDocument8 pagesIMG EPIDEMIOLOGY STUDY GROUPManivanh AvalosPas encore d'évaluation
- Higgins 2002Document20 pagesHiggins 2002fengyu1006Pas encore d'évaluation
- Acupoint Stimulation For Fibromyalgia 2013Document15 pagesAcupoint Stimulation For Fibromyalgia 2013silkofosPas encore d'évaluation
- Research Methods Exam NotesDocument9 pagesResearch Methods Exam Notesalana.gordon24Pas encore d'évaluation
- Research Bites 7 PDFDocument1 pageResearch Bites 7 PDFGia Han Hoang HuuPas encore d'évaluation
- RCT Appraisal Sheets 2005 English-2Document6 pagesRCT Appraisal Sheets 2005 English-2tsyrahmaniPas encore d'évaluation
- Analytical StudiesDocument106 pagesAnalytical StudiesPrakash GontiPas encore d'évaluation
- 2015 - Article - 665eficacia EpicondilitiDocument13 pages2015 - Article - 665eficacia EpicondilitimorbreirPas encore d'évaluation
- 2 General Principles of Research Design and AnalysisDocument6 pages2 General Principles of Research Design and AnalysisMohamed Elprince AdelPas encore d'évaluation
- DPS: Evidence Based Medicine and Clinical Epidemiology: Types of Research QuestionDocument37 pagesDPS: Evidence Based Medicine and Clinical Epidemiology: Types of Research Questionarjun.k5796Pas encore d'évaluation
- Best Practice & Research Clinical RheumatologyDocument13 pagesBest Practice & Research Clinical RheumatologydrharivadanPas encore d'évaluation
- Kiss Guide To EBMDocument11 pagesKiss Guide To EBMBob2020Pas encore d'évaluation
- CshaDocument42 pagesCshamphil.rameshPas encore d'évaluation
- Cricket Paper-1Document13 pagesCricket Paper-1mphil.rameshPas encore d'évaluation
- Systematic Review of Infant and Young Child Complementary Feeding Practices in South Asian Families The Pakistan PerspectiveDocument14 pagesSystematic Review of Infant and Young Child Complementary Feeding Practices in South Asian Families The Pakistan Perspectivemphil.rameshPas encore d'évaluation
- Geetha 20160826 WA0008Document961 pagesGeetha 20160826 WA0008mphil.rameshPas encore d'évaluation
- Bayesian MultiparameterDocument15 pagesBayesian Multiparametermphil.rameshPas encore d'évaluation
- Grossman Statistical InferenceDocument483 pagesGrossman Statistical Inferencemphil.ramesh100% (1)
- Review Robotics EducationDocument16 pagesReview Robotics EducationDiana CarolinaPas encore d'évaluation
- Increased Prediction Accuracy in The Game of Cricketusing Machine LearningDocument18 pagesIncreased Prediction Accuracy in The Game of Cricketusing Machine LearningLewis TorresPas encore d'évaluation
- Chapter 3: Central TendencyDocument26 pagesChapter 3: Central TendencyFatimaIjazPas encore d'évaluation
- Review Robotics EducationDocument16 pagesReview Robotics EducationDiana CarolinaPas encore d'évaluation
- WanaparthyDocument12 pagesWanaparthymphil.rameshPas encore d'évaluation
- 4703 07 Notes ARMDocument4 pages4703 07 Notes ARMPhuong HoangPas encore d'évaluation
- Normal DistributionDocument12 pagesNormal Distributionmphil.rameshPas encore d'évaluation
- Data PerentageDocument10 pagesData Perentagemphil.rameshPas encore d'évaluation
- Food BasedapproachDocument8 pagesFood Basedapproachmphil.rameshPas encore d'évaluation
- Cross Over DesignsDocument7 pagesCross Over Designsmphil.rameshPas encore d'évaluation
- Micronutrient Fortification of Food and Its Impact On Woman and Child Health: A Systematic ReviewDocument24 pagesMicronutrient Fortification of Food and Its Impact On Woman and Child Health: A Systematic Reviewmphil.rameshPas encore d'évaluation
- Longitudinal Method KhooWestWuKwokDocument17 pagesLongitudinal Method KhooWestWuKwokmphil.rameshPas encore d'évaluation
- 7.11.2 Vitamin A Deficiency PR MapDocument9 pages7.11.2 Vitamin A Deficiency PR MapRishav RajPas encore d'évaluation
- The American StatisticianDocument10 pagesThe American Statisticianmphil.rameshPas encore d'évaluation
- Calculation of IDDDocument3 pagesCalculation of IDDmphil.rameshPas encore d'évaluation
- Journal of The American Statistical AssociationDocument11 pagesJournal of The American Statistical Associationmphil.rameshPas encore d'évaluation
- 1478 7547 11 18Document6 pages1478 7547 11 18mphil.rameshPas encore d'évaluation
- Fail-Safe-N IDDDocument1 pageFail-Safe-N IDDmphil.rameshPas encore d'évaluation
- Quick Study For Computer Keyboard Short CutsDocument2 pagesQuick Study For Computer Keyboard Short Cutsmahazari100% (3)
- 10Document4 pages10mphil.rameshPas encore d'évaluation
- Fixed Effects Fixed Effects Fixed Effects Random Effects Random EffectsDocument2 pagesFixed Effects Fixed Effects Fixed Effects Random Effects Random Effectsmphil.rameshPas encore d'évaluation
- 1742 5573 1 5Document19 pages1742 5573 1 5mphil.rameshPas encore d'évaluation
- 124 - 2 197 202Document6 pages124 - 2 197 202mphil.rameshPas encore d'évaluation
- 1471 2288 12 125Document15 pages1471 2288 12 125mphil.rameshPas encore d'évaluation
- Hypertensive Emergencies in The Emergency DepartmentDocument13 pagesHypertensive Emergencies in The Emergency DepartmentLuis Lopez RevelesPas encore d'évaluation
- The Concept of NeuropsychiatryDocument10 pagesThe Concept of NeuropsychiatryOscar Adrian Carmona NietoPas encore d'évaluation
- NASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONDocument105 pagesNASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONNguyễn ThànhPas encore d'évaluation
- Chronic Medical IssuesDocument9 pagesChronic Medical IssuesomoshPas encore d'évaluation
- GRANDE ICU CASE SUMMARYDocument3 pagesGRANDE ICU CASE SUMMARYanuzPas encore d'évaluation
- Elevated LDL Triglycerides and Atherosclerotic Risk: BackgroundDocument17 pagesElevated LDL Triglycerides and Atherosclerotic Risk: BackgroundRoxana MariaPas encore d'évaluation
- Borderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergDocument23 pagesBorderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergjuaromerPas encore d'évaluation
- PolycythemiaDocument82 pagesPolycythemiaTiffany Mae Arud100% (3)
- 2024 - ĐỀ 4Document10 pages2024 - ĐỀ 4ellypham1357Pas encore d'évaluation
- Dhatupaushtik ChurnaDocument6 pagesDhatupaushtik ChurnaShoeb MirzaPas encore d'évaluation
- GAD Database DCFDocument26 pagesGAD Database DCFBaby Jane Dedase100% (1)
- Science Learning Sheet 1 RESPIRATORY SYSTEMDocument3 pagesScience Learning Sheet 1 RESPIRATORY SYSTEMexelainedivinePas encore d'évaluation
- Oncology Guidelines For Dogs and CatsDocument24 pagesOncology Guidelines For Dogs and CatsDaniela Loranca ValdovinosPas encore d'évaluation
- Asthma Lesson PlanDocument26 pagesAsthma Lesson PlanBharat Singh BanshiwalPas encore d'évaluation
- Hiv Awareness Project ProposalDocument17 pagesHiv Awareness Project ProposalPrincess Gesa Macula100% (1)
- New Drugs 2014-2018Document31 pagesNew Drugs 2014-2018Prem Goel0% (1)
- Managing Cardiac Patients in the ICUDocument26 pagesManaging Cardiac Patients in the ICUvamshidh100% (2)
- Kelas 3Document5 pagesKelas 3RojPas encore d'évaluation
- Superannuation Benefits SessionDocument49 pagesSuperannuation Benefits SessionfunsharePas encore d'évaluation
- EHSMS Performance and Incident ReportingDocument38 pagesEHSMS Performance and Incident ReportingravimanasPas encore d'évaluation
- Programs of Doh - NCDDocument71 pagesPrograms of Doh - NCDZOVELLA AURORA M. ACURAMPas encore d'évaluation
- Cinnarizine A Contemporary ReviewDocument9 pagesCinnarizine A Contemporary ReviewprimaPas encore d'évaluation
- Rapyuta Robotics PVT LTD - GMC Renewal Quote - 28th Dec2022Document1 pageRapyuta Robotics PVT LTD - GMC Renewal Quote - 28th Dec2022nagarajgnairyPas encore d'évaluation
- AcupunctureDocument15 pagesAcupuncturezextorcPas encore d'évaluation
- Clinical Procedures For Medical Assistants 9th Edition Bonewit Test BankDocument12 pagesClinical Procedures For Medical Assistants 9th Edition Bonewit Test Bankcarriejordanwboriaqmfn100% (16)
- The Function and Anatomy of the LungsDocument20 pagesThe Function and Anatomy of the LungsNkosinathi ShongwePas encore d'évaluation
- Bannock Awareness: Celebrating Aboriginal Culture Through RecipesDocument28 pagesBannock Awareness: Celebrating Aboriginal Culture Through RecipesMaggie SedgemorePas encore d'évaluation
- Addison On The Thing 1982Document14 pagesAddison On The Thing 1982Matheus TomazPas encore d'évaluation
- Disease Prediction Using Machine LearningDocument10 pagesDisease Prediction Using Machine LearningIJRASETPublicationsPas encore d'évaluation
- People Like Us (PLUS) Kolkata, Annual Activity Report 2007-08Document18 pagesPeople Like Us (PLUS) Kolkata, Annual Activity Report 2007-08Agniva LahiriPas encore d'évaluation