Académique Documents
Professionnel Documents
Culture Documents
Back Pain
Transféré par
Nader SmadiDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Back Pain
Transféré par
Nader SmadiDroits d'auteur :
Formats disponibles
Back Pain
Definition
Back pain is a common complaint. Four out of five people in the United States will
experience low back pain at least once during their lives. It's one of the most common
reasons people go to the doctor or miss work.
On the bright side, you can prevent most back pain. If prevention fails, simple home
treatment and proper body mechanics will often heal your back within a few weeks
and keep it functional for the long haul. Surgery is rarely needed to treat back pain.
Causes
Your back is an intricate structure composed of bones, muscles, ligaments, tendons
and disks — the cartilage-like pads that act as cushions between the segments of your
spine. Back pain can arise from problems with any of these component parts. In some
people, no specific cause for their back pain can be found.
Strains
Back pain most often occurs from strained muscles and ligaments, from improper or
heavy lifting, or after a sudden awkward movement. Sometimes a muscle spasm can
cause back pain.
Structural problems
In some cases, back pain may be caused by structural problems, such as:
Bulging or ruptured disks. Disks act as cushions between the vertebrae in
your spine. Sometimes, the soft material inside a disk may bulge out of place
or rupture and press on a nerve. But many people who have bulging or
herniated disks experience no pain from the condition.
Sciatica. If a bulging or herniated disk presses on the main nerve that travels
down your leg, it can cause sciatica — sharp, shooting pain through the
buttock and back of the leg.
Arthritis. The joints most commonly affected by osteoarthritis are the hips,
hands, knees and lower back. In some cases arthritis in the spine can lead to a
narrowing of the space around the spinal cord, a condition called spinal
stenosis.
Skeletal irregularities. Back pain can occur if your spine curves in an
abnormal way. If the natural curves in your spine become exaggerated, your
upper back may look abnormally rounded or your lower back may arch
excessively. Scoliosis, a condition in which your spine curves to the side, also
may lead to back pain.
Osteoporosis. Compression fractures of your spine's vertebrae can occur if
your bones become porous and brittle.
Rare but serious conditions
In rare cases, back pain may be related to:
Cauda equina syndrome. This is a serious neurological problem affecting a
bundle of nerve roots that serve your lower back and legs. It can cause
weakness in the legs, numbness in the "saddle" or groin area, and loss of
bowel or bladder control.
Cancer in the spine. A tumor on the spine can press on a nerve, causing back
pain.
Infection of the spine. If a fever and a tender, warm area accompany back
pain, the cause could be an infection.
Risk factors
Factors that increase your risk of developing low back pain include:
Smoking
Obesity
Older age
Female gender
Physically strenuous work
Sedentary work
Stressful job
Anxiety
Depression
When to seek medical advice
Most back pain gradually improves with home treatment and self-care. Although the
pain may take several weeks to disappear completely, you should notice some
improvement within the first 72 hours of self-care. If not, see your doctor.
In rare cases, back pain can signal a serious medical problem. See a doctor
immediately if your back pain:
Is constant or intense, especially at night or when you lie down
Spreads down one or both legs, especially if the pain extends below the knee
Causes weakness, numbness or tingling in one or both legs
Causes new bowel or bladder problems
Is associated with pain or pulsation (throbbing) in the abdomen, or fever
Follows a fall, blow to your back or other injury
Is accompanied by unexplained weight loss
Also, see your doctor if you start having back pain for the first time after age 50, or if
you have a history of cancer, osteoporosis, steroid use, or drug or alcohol abuse.
Tests and diagnosis
Diagnostic tests aren't usually necessary to confirm the cause of your back pain.
However, if you do see your doctor for back pain, he or she will examine your back
and assess your ability to sit, stand, walk and lift your legs. He or she may also test
your reflexes with a rubber reflex hammer. These assessments help determine where
the pain comes from, how much you can move before pain forces you to stop and
whether you have muscle spasms. They will also help rule out more serious causes of
back pain.
If there is reason to suspect that you have a tumor, fracture, infection or other specific
condition that may be causing your back pain, your doctor may order one or more
tests:
X-ray. These images show the alignment of your bones and whether you have
arthritis or broken bones. X-ray images won't directly show problems with
your spinal cord, muscles, nerves or disks.
Magnetic resonance imaging (MRI) or computerized tomography (CT)
scans. These scans can generate images that may reveal herniated disks or
problems with bones, muscles, tissue, tendons, nerves, ligaments and blood
vessels.
Bone scan. In rare cases, your doctor may use a bone scan to look for bone
tumors or compression fractures caused by osteoporosis. In this procedure,
you'll receive an injection of a small amount of a radioactive substance (tracer)
into one of your veins. The substance collects in your bones and allows your
doctor to detect bone problems using a special camera.
Nerve studies (electromyography, or EMG). This test measures the
electrical impulses produced by the nerves and the responses of your muscles.
Studies of your nerve-conduction pathways can confirm nerve compression
caused by herniated disks or narrowing of your spinal canal (spinal stenosis).
Treatments and drugs
Most back pain gets better with a few weeks of home treatment and careful attention.
A regular schedule of over-the-counter pain relievers may be all that you need to
improve your pain. A short period of bed rest is okay, but more than a couple of days
actually does more harm than good. If home treatments aren't working, your doctor
may suggest stronger medications or other therapy.
Medications
Your doctor may prescribe nonsteroidal anti-inflammatory drugs or in some cases, a
muscle relaxant, to relieve mild to moderate back pain that doesn't get better with
over-the-counter pain relievers. Narcotics, such as codeine or hydrocodone, may be
used for a short period of time with close supervision by your doctor.
Low doses of certain types of antidepressants — particularly tricyclic antidepressants,
such as amitriptyline — have been shown to relieve chronic back pain, independent of
their effect on depression.
Physical therapy and exercise
A physical therapist can apply a variety of treatments, such as heat, ice, ultrasound,
electrical stimulation and muscle-release techniques, to your back muscles and soft
tissues to reduce pain. As pain improves, the therapist can teach you specific exercises
to increase your flexibility, strengthen your back and abdominal muscles, and
improve your posture. Regular use of these techniques will help prevent pain from
coming back.
Injections
If other measures don't relieve your pain and if your pain radiates down your leg, your
doctor may inject cortisone — an anti-inflammatory medication — into the space
around your spinal cord (epidural space). A cortisone injection helps decrease
inflammation around the nerve roots, but the pain relief usually lasts less than six
weeks.
In some cases, your doctor may inject numbing medication into or near the structures
believed to be causing your back pain. Early studies indicate that botulism toxin
(Botox) also may help relieve back pain, perhaps by paralyzing strained muscles in
spasm. Botox injections typically wear off within three to four months.
Surgery
Few people ever need surgery for back pain. There are no effective surgical
techniques for muscle- and soft-tissue-related back pain. Surgery is usually reserved
for pain caused by a herniated disk. If you have unrelenting pain or progressive
muscle weakness caused by nerve compression, you may benefit from surgery. Types
of back surgery include:
Fusion. This surgery involves joining two vertebrae to eliminate painful
movement. A bone graft is inserted between the two vertebrae, which may
then be splinted together with metal plates, screws or cages. A drawback to the
procedure is that it increases the chances of arthritis developing in adjoining
vertebrae.
Disk replacement. An alternative to fusion, this surgery inserts an artificial
disk as a replacement cushion between two vertebrae.
Partial removal of disk. If disk material is pressing or squeezing a nerve,
your doctor may be able to remove just the portion of the disk that's causing
the problem.
Partial removal of a vertebra. If your spine has developed bony growths that
are pinching your spinal cord or nerves, surgeons can remove a small section
of the offending vertebra, to open up the passage.
Prevention
You may be able to avoid back pain by improving your physical condition and
learning and practicing proper body mechanics.
To keep your back healthy and strong:
Exercise. Regular low-impact aerobic activities — those that don't strain or
jolt your back — can increase strength and endurance in your back and allow
your muscles to function better. Walking and swimming are good choices.
Talk with your doctor about which activities are best for you.
Build muscle strength and flexibility. Abdominal and back muscle exercises
(core-strengthening exercises) help condition these muscles so that they work
together like a natural corset for your back. Flexibility in your hips and upper
legs aligns your pelvic bones to improve how your back feels.
Quit smoking. Smokers have diminished oxygen levels in their spinal tissues,
which can hinder the healing process.
Maintain a healthy weight. Being overweight puts strain on your back
muscles. If you're overweight, trimming down can prevent back pain.
Use proper body mechanics:
Stand smart. Maintain a neutral pelvic position. If you must stand for long
periods of time, alternate placing your feet on a low footstool to take some of
the load off your lower back.
Sit smart. Choose a seat with good lower back support, arm rests and a swivel
base. Consider placing a pillow or rolled towel in the small of your back to
maintain its normal curve. Keep your knees and hips level.
Lift smart. Let your legs do the work. Move straight up and down. Keep your
back straight and bend only at the knees. Hold the load close to your body.
Avoid lifting and twisting simultaneously. Find a lifting partner if the object is
heavy or awkward.
Alternative medicine
Many people choose hands-on therapies to ease their back pain:
Chiropractic care. Back pain is one of the most common reasons that people
see a chiropractor. If you're considering chiropractic care, talk to your doctor
about the most appropriate specialist for your type of problem. In addition to
chiropractors, many osteopathic doctors and some physical therapists have
training in spinal manipulation.
Acupuncture. Some people with low back pain report that acupuncture helps
relieve their symptoms. The National Institutes of Health has found that
acupuncture can be an effective treatment for some types of chronic pain. In
acupuncture, the practitioner inserts sterilized stainless steel needles into the
skin at specific points on the body.
Massage. If your back pain is caused by tense or overworked muscles,
massage therapy may help loosen knotted muscles and promote relaxation.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Pharmacology - Anti-Inflammatory DrugsDocument10 pagesPharmacology - Anti-Inflammatory DrugsNader SmadiPas encore d'évaluation
- HyperkalemiaDocument16 pagesHyperkalemiaNader Smadi100% (5)
- Exam 2Document49 pagesExam 2Nader Smadi100% (5)
- Exam 1Document49 pagesExam 1Nader Smadi100% (2)
- Communicable DiseasesDocument161 pagesCommunicable DiseasesNader Smadi95% (20)
- HyponatremiaDocument10 pagesHyponatremiaNader Smadi100% (1)
- Glossary of AbbreviationsDocument38 pagesGlossary of AbbreviationsDaniel VasilePas encore d'évaluation
- Swine FluDocument4 pagesSwine FluNader Smadi100% (2)
- VIDEOS1 (Youtube)Document1 pageVIDEOS1 (Youtube)Nader SmadiPas encore d'évaluation
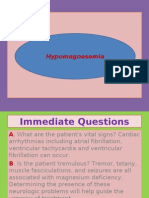
- HypomagnesemiaDocument7 pagesHypomagnesemiaNader SmadiPas encore d'évaluation
- Vital SignsDocument21 pagesVital SignsNader Smadi90% (20)
- Idiopathic Thrombocytopenic PurperaDocument21 pagesIdiopathic Thrombocytopenic PurperaNader Smadi100% (2)
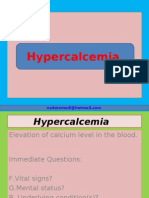
- HypercalcemiaDocument8 pagesHypercalcemiaNader Smadi100% (1)
- Nursing ProcessDocument16 pagesNursing ProcessNader Smadi100% (10)
- HypokalemiaDocument7 pagesHypokalemiaNader SmadiPas encore d'évaluation
- HypernatremiaDocument7 pagesHypernatremiaNader Smadi100% (1)
- Emergency Exam9Document5 pagesEmergency Exam9Nader Smadi100% (2)
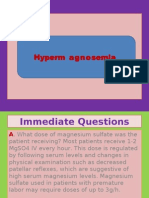
- HypermagnesemiaDocument5 pagesHypermagnesemiaNader Smadi100% (1)
- Emergency Exam7Document8 pagesEmergency Exam7Nader Smadi50% (2)
- Emergency Exam8Document7 pagesEmergency Exam8Nader Smadi100% (1)
- Diabetic ComaDocument15 pagesDiabetic ComaNader Smadi100% (1)
- EpilepsyDocument37 pagesEpilepsyNader Smadi100% (7)
- Cardiovascular Disorders 1Document44 pagesCardiovascular Disorders 1Nader Smadi100% (1)
- Emergency Exam6Document5 pagesEmergency Exam6Nader Smadi100% (1)
- Emergency Exam4Document7 pagesEmergency Exam4Nader Smadi100% (3)
- Emergency Exam5Document6 pagesEmergency Exam5Nader SmadiPas encore d'évaluation
- Emergency Exam3Document5 pagesEmergency Exam3Nader Smadi100% (1)
- Safe Injection TechniquesDocument27 pagesSafe Injection TechniquesNader Smadi100% (1)
- Emergency Exam2Document10 pagesEmergency Exam2Nader Smadi100% (6)
- Peritoneal DialysisDocument15 pagesPeritoneal DialysisNader Smadi100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- BotulismDocument5 pagesBotulismsubhash nayakPas encore d'évaluation
- Advances in Facial Rejuvenation Botox, HA Dermal Fillers, & Combination TherapyDocument26 pagesAdvances in Facial Rejuvenation Botox, HA Dermal Fillers, & Combination Therapybluestes100% (1)
- Your Complete Guide To Choosing The Right Option For You: Dermatology & Skin WellbeingDocument40 pagesYour Complete Guide To Choosing The Right Option For You: Dermatology & Skin WellbeingGanea FlorentinaPas encore d'évaluation
- Diagnosis and treatment approaches for excessive gingival displayDocument9 pagesDiagnosis and treatment approaches for excessive gingival display刘雨樵Pas encore d'évaluation
- Keosha Skin ClinicDocument29 pagesKeosha Skin ClinicGanga BhagirathiPas encore d'évaluation
- Elitox PPT ENG CompressedDocument18 pagesElitox PPT ENG CompressedTom ArdiPas encore d'évaluation
- 02 Padure, L. Spastic Hip in Cerebral PalsyDocument4 pages02 Padure, L. Spastic Hip in Cerebral PalsyminichoixPas encore d'évaluation
- Using Insulin Pens to Treat DiabetesDocument14 pagesUsing Insulin Pens to Treat DiabetesTaran JOtPas encore d'évaluation
- Lower Plant Toxins (Microbial)Document48 pagesLower Plant Toxins (Microbial)Arslan Saeed0% (1)
- Current Use of Cosmetic Toxins To Improve Facial.29Document14 pagesCurrent Use of Cosmetic Toxins To Improve Facial.29Filipe AlbuquerquePas encore d'évaluation
- BotulinumDocument151 pagesBotulinumisabel90% (10)
- JAMADocument5 pagesJAMAmedodido94Pas encore d'évaluation
- Enterotoxemia, Anaerobic Dysentery, Bradsot, Botulism and NecrobacteriosisDocument17 pagesEnterotoxemia, Anaerobic Dysentery, Bradsot, Botulism and NecrobacteriosisNajafova SuadaPas encore d'évaluation
- Bastidas 2021Document13 pagesBastidas 2021ruben dario meza bertelPas encore d'évaluation
- Biopesticide Env JM Mono (2011) 43Document51 pagesBiopesticide Env JM Mono (2011) 43MITHUN KHANDELWALPas encore d'évaluation
- Biological Hazard: Most Common Microbiological Hazards in The Food IndustryDocument19 pagesBiological Hazard: Most Common Microbiological Hazards in The Food IndustryDharanibalan PPas encore d'évaluation
- HACCP PrinciplesDocument106 pagesHACCP PrinciplesJake MelderPas encore d'évaluation
- Holy Name University College of Health and Science Department of NursingDocument37 pagesHoly Name University College of Health and Science Department of NursingZarrick AmielPas encore d'évaluation
- VIVA Training in ENTDocument8 pagesVIVA Training in ENTOpi PippoPas encore d'évaluation
- Statistics: Aesthetic Plastic Surgery National DatabankDocument26 pagesStatistics: Aesthetic Plastic Surgery National DatabankNuka AtabegashviliPas encore d'évaluation
- Phend Pharmaceuticals Double Blind Study Shows NATOX Cream Reduces Wrinkles Without Side EffectsDocument2 pagesPhend Pharmaceuticals Double Blind Study Shows NATOX Cream Reduces Wrinkles Without Side EffectsLiliana LesuPas encore d'évaluation
- (Chapter 7) EvidenceDocument2 pages(Chapter 7) EvidenceK59 LE THI NGOC THAOPas encore d'évaluation
- BACTERIADocument1 pageBACTERIAKumkum MahajanPas encore d'évaluation
- Food-Related Illnesses and Allergies (New)Document57 pagesFood-Related Illnesses and Allergies (New)coosa liquorsPas encore d'évaluation
- Gram Positive BacilliDocument6 pagesGram Positive BacilliSteve ShirmpPas encore d'évaluation
- Tips For Stroke Recovery From Flint RehabDocument9 pagesTips For Stroke Recovery From Flint RehabSaumya99100% (1)
- Dermal Fillers LeafletDocument1 pageDermal Fillers LeafleteidwisamPas encore d'évaluation
- Wanted PosterDocument2 pagesWanted Posterfreakyking68Pas encore d'évaluation
- UntitledDocument24 pagesUntitledDOUGLAS LIEBELPas encore d'évaluation
- Mephisto SignalDocument3 pagesMephisto SignalPatriciaPas encore d'évaluation