Académique Documents
Professionnel Documents
Culture Documents
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition. CHP 29pdf
Transféré par
jokazelDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition. CHP 29pdf
Transféré par
jokazelDroits d'auteur :
Formats disponibles
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only.
No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
436
CHAPTER 29 Musculoskeletal Care KEY TERMS Angulated injury
An injury that is deformed (bent) at the site.
436 437
Closed injury
An injury that does not break the continuity of the skin.
Crepitation
The sound made when bone ends rub together or there is air inside the tissue.
Direct injury
An injury that results from a force that comes into direct contact with an area of the body.
Indirect injury
An injury in one body area that results from a force that comes into contact with a different part of the body.
Mechanism of injury
The force that acts upon the body to produce an injury.
Open injury
An injury that breaks the continuity of the skin.
Pneumatic splints
Devices such as air or vacuum splints that conform to the injury.
Position of function
The relaxed position of the hand or foot in which there is minimal movement or stretching of muscle.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 1 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Rigid splints
A type of splint that does not conform to the body.
Sling and swathe
Bandaging used to immobilize a shoulder or arm injury.
Traction splints
A special device used to immobilize a midfemur injury.
Twisting injury
An injury that results from a turning motion of the body in opposite directions.
437 438
IN THE FIELD
Varun and Tony were dispatched to a hockey rink late on a Friday evening. The injured man was awake and oriented, and complained only of pain in his left upper thigh. He reported that he was the coach of a team and an angry player swung a hockey stick at his leg. He felt a cracking noise and immediately fell to the ice. Police on scene report that the scene is safe and the angry player has been restrained. Upon assessment, Tony finds that the only injury to the coach is a midshaft deformity in his left upper thigh. The coach's distal pulse is weak and the skin is pale and cool. Varun gets the traction splint while Tony explains the process to the patient. He tells him that by pulling on the leg, the bone might move back into place, relieving him of pain and improving his distal circulation. The patient agrees to the application of the traction splint. Varun carefully holds the leg around the ankle and applies gentle manual traction. Tony applies the splint, and then reassesses the leg, finding the circulation to be improved. Minutes later they have the coach immobilized on the long backboard and are en route to the emergency department. Dealing with musculoskeletal injuries is a common occurrence in the life of most EMTs. Many musculoskeletal injuries are not complicated and will only require careful assessment, splinting, and a trip to the emergency department. Other injuries can threaten the patient's life or limb and will require emergent treatment.
MUSCULOSKELETAL REVIEW
Before we begin discussing these injuries, let's briefly review the musculoskeletal system. For more detailed information, see Chapter 4.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 2 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
THE MUSCULAR SYSTEM
The muscular system performs several specific functions. Muscles give the body shape, protect internal organs, and provide movement. There are three different types of muscle (Fig. 29-1). Voluntary, or skeletal, muscles are attached to bones. These muscles form the major muscle mass of the body and are controlled by the nervous system and brain. They can be contracted and relaxed at will and are responsible for movement. Involuntary, or smooth, muscles are found in the walls of the hollow structures of the gastrointestinal tract and urinary system, as well as the blood vessels and bronchi. Involuntary muscles control the flow of blood, body fluids, and other substances through these structures, and there is generally no conscious control of these muscles. They carry out the automatic muscular functions of the body and respond to stimuli such as heat or cold or the stretching produced when an organ is full. Cardiac muscle exists only in the heart and has automaticity, the ability of the muscle to contract on its own. Cardiac muscle is involuntary muscle that has its own supply of blood through the coronary artery system. This muscle can tolerate only short interruptions of blood supply.
THE SKELETAL SYSTEM
The skeletal system helps provide body shape, protects internal organs, and assists in body movement. The skeletal system consists of the bones of the skull and face, the spinal column and thorax, the pelvis, the lower extremities, and the upper extremities. The skull and face are made up of numerous fused bones. The spinal column consists of 33 bones: 7 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 4 coccygeal vertebrae. The thorax consists of 12 ribs and a sternum. The lower extremities are composed of the femur (thigh); the tibia and fibula; and the tarsals, metatarsals, and phalanges, which make up the ankle and foot. The upper extremities are composed of the humerus; the radius and ulna; and the carpals, metacarpals, and phalanges, which make up the wrist and hand. Muscles and bones, together with other connective tissue, allow for body movement. Extremities move at the joints where bones are connected to other bones. There are ball-and-socket joints such as the shoulder, and there are hinge joints such as the elbow (Fig. 29-2).
REVIEW QUESTIONS
MUSCULOSKELETAL REVIEW 1. List three functions of the muscular system. 1. Give the body shape, protect organs, provide for movement 2. What type of muscle is found in the walls of the gastrointestinal tract?
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 3 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
2. Smooth muscle 3. Muscles that we can control are called ________. 3. voluntary (skeletal) muscles
438 439
Fig. 29-1 The three types of muscles. A, Voluntary (skeletal). B, Involuntary (smooth). C, Cardiac muscles.
INJURIES TO BONES AND JOINTS
Various injuries to bones and joints are described in the following sections. To help you treat the injuries, you must understand the forces that can cause damage to bones. Some injuries are much more traumatic and serious than others and must be cared for as such. If the forces that caused the injury are very serious, you would expect the injuries to also be more serious.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 4 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
The elderly are often more susceptible to bone injury because of osteoporosis, a disease in which bone matter is lost and there is greater air space within a bone, making them more brittle. Immobilization in the elderly may also be complicated by arthritis. Arthritis is the inflammation of the joints and may produce an angulation that cannot be straightened, such as a curvature of the spine. The bones of children are more flexible and pliable than the bones of adults. Children can sustain serious injuries to the organs and structures underlying bones without having any injuries to the bones themselves. There are even case reports of children with obvious tire tracks on their chests from being run over by a car without breaking any of the bones in the chest.
ALERT!
Lack of musculoskeletal trauma in a child does not indicate there is no serious underlying injury.
MECHANISM OF INJURY
The mechanism of injury can help you determine the severity of the injury. Musculoskeletal injuries usually result from a force applied to an area of the body. Some injuries result from a direct force onto an area of the body. Such a direct injury can be caused by a baseball
439 440
Fig. 29-2 Skeleton of the human body.
440
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 5 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
440 441
Fig. 29-3 A, A direct mechanism of injury. B, An indirect mechanism of injury. C, A twisting mechanism.
bat swung into a person's arm. The arm's injury results from direct contact with the baseball bat (Fig. 29-3, A). Other injuries are caused by indirect forces. An example of indirect injury is an auto collision in which a patient's knees are thrown forward into the dashboard. The knees are directly injured from contact with the dash, but indirect injury can occur from forces transmitted from the knees through the legs to the hips and pelvis (Fig. 29-3, B). If an extremity is pulled and turned beyond its normal range of motion, a twisting injury may result. For instance, a wrestler who becomes entangled in an opponent's hold may pull and twist his body. This force may produce an injury to the muscles and bones that are twisted (Fig. 29-3, C). Always consider the force that was involved in the cause of the injury. It takes a much greater force to injure a femur (thigh), for example, than it takes to injure the ulna (forearm) because the bone is much larger, more dense, and protected by larger muscles. Gather as much information as possible regarding the mechanism of injury, and include this in your report to the receiving facility. Patients who sustain a serious mechanism of injury but don't have any obvious injuries to their bodies should be carefully evaluated at a trauma center. If the mechanism of injury is serious, always suspect that serious hidden injuries are present and transport the patient to a trauma center.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 6 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
BONE OR JOINT INJURIES
Musculoskeletal injuries are either open or closed. An open injury involves a break in the continuity of the skin and usually produces some external bleeding (Fig. 29-4). Open injuries have the added complication of possible infection due to the break in the skin. A closed injury does not involve a break in the skin or external bleeding, although it may produce internal bleeding (Fig. 29-5). Various signs and symptoms are characteristic of bone or joint injuries. The area of injury may have some deformity or angulation and may be painful to move and tender to touch. If the bone ends are separated, some crepitation (grating) may be heard or felt during the examination, caused by the bone ends
441 442
Fig. 29-4 An open injury involves a break in the continuity of the skin.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 7 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Fig. 29-5 A closed injury, such as this fractured pelvis, does not involve a break in the skin but may produce internal bleeding.
rubbing together. However, do not purposefully seek this sign, and do not try to repeat it if you note it during the assessment because it may produce further injury. Bone ends can be very sharp and cause damage to nearby blood vessels, nerves and muscle if they are allowed to move. The area of injury may be swollen, appearing larger than the same area on the other side of the body, and may be discolored. In an open bone injury, the ends of the bones that are injured may be protruding through the skin and exposed to the outside environment. Sometimes the bone ends have protruded through the skin, creating an open wound and then have withdrawn back inside the skin and no bone ends will be visible. With a joint injury, the joint may be locked in position and unmovable. Box 29-1 summarizes the signs and symptoms of a bone or joint injury.
BOX 29-1 Signs and Symptoms of a Bone or Joint Injury
Deformity or angulation Pain and tenderness
Page 8 of 28
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Crepitation (grating) Swelling Bruising (discoloration) Exposed bone ends (open injury) Joints locked into position
BOX 29-2 Types of Fractures
Comminuted: Involves multiple breaks creating bone fragments Greenstick: An incomplete fracture in children where the bone is bent but not broken completely Spiral: A fracture caused by a twisting mechanism of injury Stress: A fracture caused by repeated pressure on a bone, such as a tibia stress fracture in a runner
There is some terminology that you may hear associated with musculoskeletal trauma. Fractures occur when the bone is actually cracked or broken. Box 29-2 lists various types of fractures. Dislocations occur when the bone ends do not meet appropriately at a joint. Sprains are partial tearing of ligaments (tissues that connect bones to other bones). Strains are injuries to tendons (tissue that connects bones to muscles) or muscles due to overstretching. In the field, it is impossible to distinguish these various types of injuries from one another, and they all should be treated and splinted as though they are fractures. In the hospital, definitive tests will be performed to determine the specific type of injury and the appropriate treatment.
EMERGENCY CARE FOR PATIENTS WITH BONE OR JOINT INJURIES
Emergency medical care for bone or joint injuries consists of both basic techniques and specialized techniques. First, always use appropriate personal protective equipment (PPE) for body substance isolation precautions before examining the patient. Even a closed injury that is not bleeding may become an open injury because of movement or pressure. Establish a patent airway and administer high-flow oxygen to all patients as indicated. Extremity injuries can be quite horrific to look at, but they rarely cause life-threatening problems on their own. Make sure you assess the airway, breathing, and circulation before addressing individual bone or joint injuries. Any major bleeding or life-threatening situations should be controlled using the methods, such as direct pressure, described in Chapter 27.
442 443
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 9 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
ALERT!
Always care for life-threatening injuries before focusing on a painful, swollen, deformed extremity. Do not waste scene time on an extremity if the patient is not breathing adequately or has other threats to life! Splint the injury appropriately to prevent movement of bone ends or fragments (described later in this chapter), and prepare the patient for transport. During transport, a cold pack may be applied to the injured area to reduce swelling and pain. An injured extremity should be elevated to reduce blood flow to that area, unless other injuries are present and would cause complications. If elevating the extremity causes the patient more pain, do not elevate. Monitor the patient's vital signs en route to the receiving facility. Any changes in the patient's condition or vital signs should be reported to the receiving facility.
REVIEW QUESTIONS
INJURIES TO BONES AND JOINTS 1. A(n) _______ injury occurs when the force is transmitted from one body area injuring another body area. 1. indirect 2. The sound that is produced when bone ends grate together is called ________. 2. crepitation 3. To help determine the potential severity of a wound, you should consider the forces that were applied to the body, called the ________. 3. mechanism of injury
SPLINTING AN INJURY
The specialized emergency medical care provided for a painful, swollen, deformed extremity includes applying a splint to immobilize the injury and prevent further damage. This chapter describes various types of splints and how they are used.
REASONS FOR SPLINTING
Splinting a painful, swollen, deformed extremity prevents movement of bone fragments, bone ends, or injured joints. The splint minimizes damage to muscles, nerves, and blood vessels caused by broken
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 10 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
bones. Immobilization helps to prevent a closed injury from becoming an open injury. It also minimizes the restriction of blood flow resulting from bone ends compressing blood vessels and limits the bleeding caused by tissue damage from the bone ends. Splinting reduces pain by limiting the movement of bone ends. Paralysis resulting from spinal damage is also minimized. Box 29-3 summarizes the reasons for splinting.
PRINCIPLES OF SPLINTING
When caring for an extremity injury, always evaluate the pulse, motor function, and sensation distal to the injury both before and after applying a splint, and record the findings. It is important to know the circulatory and sensory status of the extremity before splinting. A splint that is placed improperly or secured too tightly may impede circulation. If there is a change in distal circulation, loosen the splint and reassess. If the circulation does not return, the extremity may need to be resplinted.
BOX 29-3 Reasons for Splinting
Prevent movement of bone fragments, bone ends, or injured joints Minimize damage to muscles, nerves, and blood vessels Minimize the chance of converting a closed injury into an open injury Minimize the restriction of blood flow resulting from bone ends compressing blood vessels Minimize bleeding from damaged tissue caused by bone ends Minimize the pain associated with movement of bone ends Minimize chance of paralysis of extremities due to spinal damage
443 444
The bones and joints above and below an injury site must be immobilized with the splint to minimize muscle movement near the injury. For example, if the injury is to the forearm, the joint below (the wrist) and the joint above (the elbow) must be splinted. Before splinting, cut clothing away to expose the area and make the splint more effective. Open injuries should be dressed and bandaged before application of the splint. If there is a severe deformity or if the distal extremity is cyanotic or lacks a pulse, the injury should be aligned with gentle traction before splinting in an attempt to regain circulation. If resistance is felt, splint the extremity in the position in which you find it. If no pulse returns distal to the injury, rapid transport is indicated to prevent possible loss of the extremity. If any bones are protruding through the skin, do not try to replace them, although they may retract when the splint is applied. Splints should be padded to prevent pressure and discomfort to the patient. When splinting a hand or foot, immobilize it in the position of function. This is the most comfortable position for the hand or foot and requires the least amount of muscle use or stretching. This is the resting position for the hand or foot. For the hand, place a roll of gauze in the palm to support the hand, and for the foot, support the sole (Figs. 29-6 and 29-7).
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 11 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Splint the injury before transporting only if there are no life-threatening situations present. If life-threatening problems with the airway, breathing, or circulation are present, you can simply splint the extremity to the long backboard as you prepare the patient for transport. If you are in doubt whether to splint an injury, err on the side of caution and apply a splint. It is acceptable to splint an extremity that was not actually fractured, but it is unacceptable to fail to splint a fractured extremity. Without an X-ray, it is impossible to differentiate between a broken ankle and a sprain or strain; therefore, you should assume the ankle is broken. Do not waste time trying to identify the actual injury. See Principle 29-1 for the general rules of splinting.
Fig. 29-6 For a hand injury, place a roll of gauze in the palm to support and immobilize the hand in the position of function.
If the patient is showing the signs and symptoms of shock, align the patient in the normal anatomical position and transport using total body immobilization, including backboard and cervical collar. Do not waste time splinting each injury separately. Chapter 30 describes full-body immobilization.
PRINCIPLE 29-1 Principles of Splinting
1. Assess pulse, motor function, and sensation distal to the injury before and after splinting, and record your findings.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 12 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
2. Immobilize the joint above and below the musculoskeletal injury. For a joint injury, immobilize the bone above and below the injury. 3. Remove or cut away clothing before splinting. 4. Cover open wounds with sterile dressings before splinting. 5. Splint the injury in the position found, unless there is severe deformity or the distal extremity is cyanotic or lacks a pulse. Then attempt to align the extremity with gentle traction before splinting. 6. Do not intentionally replace protruding bones, but note them in your prehospital care report. 7. Pad the splint to prevent pressure and discomfort to the patient. 8. Splint the injury before moving the patient unless there are life-threatening situations present. 9. If in doubt whether an injury is present, apply a splint. 10. If the patient has the signs and symptoms of shock, use full-body immobilization, align the patient in the normal anatomical position on a backboard, and transport.
Fig. 29-7 For a foot injury, support the sole and immobilize in the position of function.
444
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 13 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
444 445
Fig. 29-8 Common types of splints include padded-board splints (top and right), ladder splints (middle), and cardboard splints (bottom).
EQUIPMENT AND TECHNIQUES
Many types of splints are used to immobilize various musculoskeletal injuries. For all types of splints, remember the general principles previously described. Rigid splints are nonformable splints used to support a painful, swollen, and deformed extremity and immobilize the joints or bones above and below the injury. Common examples are padded-board splints, cardboard splints, and ladder splints (Fig. 29-8). Technique 29-1 describes one method for using rigid splints. Traction splints are indicated for a closed, painful, swollen deformity at the midthigh (femur) when there is no joint or lower leg injury. A direct force to the femur may cause this injury. Although traction splints may look like they would cause pain, most patients report diminished pain after the leg has been realigned with
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 14 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Fig. 29-9 Hare traction splint (left) and Sager splint (right).
traction. Do not use a traction splint if the injury is close to the knee; if the knee, hip, pelvis, lower leg, or ankle is injured; or if bone ends are protruding through the skin. Also, do not use the traction splint if there is partial amputation or avulsion with bone separation or if the distal limb is connected only by marginal tissue such as a thin piece of skin. Traction in such cases would risk separation. Technique 29-2 details the use of the Hare traction splint, one type of bipolar splint (Fig. 29-9). Other types of traction splints use different techniques. Consult the directions supplied with the device. Pneumatic splintssuch as vacuum splintsare flexible, conforming splints that are used commonly with angulated injuries. The air splint and pneumatic antishock garments (PASG) are other types of pneumatic splints that are used for nonangulated injuries (Fig. 29-10).
445 447
TECHNIQUE 29-1 Splinting a Long Bone with a Rigid Splint
1. Use appropriate personal protective equipment for body substance isolation precautions. Check the patient's pulse, motor functions, and sensation distal to the injured area.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 15 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
2. Provide manual stabilization and support to the injured extremity and maintain gentle traction if indicated while applying the rigid splint. Measure the rigid splint to the extremity.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 16 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
3. Pad the open spaces between the splint and the extremity to place pressure evenly over the entire area of the extremity.
4. Secure the rigid splint to the extremity with cravats or roller gauze tied snugly. Tie the knots over the splint, not the skin, for comfort. Immobilize the joints above and below the injury site. Secure and immobilize the hand or foot in the position of function. Secure the entire injured extremity to the body. Repeat the assessment of pulse, motor function, and sensation distal to the injury.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 17 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
TECHNIQUE 29-2 Use of the Hare Traction Splint
1. Use appropriate personal protective equipment for body substance isolation precautions. Manually stabilize the injured leg by supporting the extremity with hands underneath to prevent movement or bumping. Assess pulse, motor functions, and sensation distal to the injured area and record the findings.
2. Apply manual traction to the injured area; this procedure is required when using a Hare traction splint. Prepare or adjust the splint to the proper length. Measure the splint on the uninjured leg with the ischial pad at the ischium, and the end of the splint 20 to 30 centimeters (8 to 12 inches) longer than the heel. Lock the splint in place.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 18 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
3. Open the support straps, position the splint under the injured leg.
4. Position the straps as shown. Apply the proximal securing device (ischial strap).
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 19 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
5. Apply the distal securing device (ankle hitch). Apply mechanical traction by tightening the ankle hitch to the splint.
6. Position and secure the support straps. Reevaluate the proximal and distal securing devices to ensure tightness. Reassess the patient's pulse, motor function, and sensation distal to the injury site and record the findings. If these findings are diminished compared with those before splinting, adjust the tension of the traction being applied. Secure the patient's torso to the long backboard to immobilize the hip. Secure the splint to the long backboard to prevent movement of the extremity.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 20 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
The air splint is applied to the injured area and then inflated with air until snug. The air splint usually has a zipper and is used primarily for injuries below the elbow and the knee. The advantages of the air splint include pressure on bleeding areas, comfort to the patient, and uniform contact. The disadvantage of the air splint is that air may leak from the splint or the pressure may change with changes in temperature or altitude. Air splints are difficult to clean, and the method of inflation (blowing into a small tube) may compromise body substance isolation precautions. When using an air splint, cover all wounds with clean dressings before applying the splint. Place the injured
447 448
Fig. 29-10 Vacuum splints (left) and air splints (right) are commonly used pneumatic splints.
Fig. 29-11 An injured arm immobilized by an air splint.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 21 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
extremity within the splint, and inflate the splint by blowing into the valve (Fig. 29-11). The port for the air may be cleansed with an alcohol wipe prior to inflation. Some air splints may come with an adapter and a pump to inflate them with air. This process requires two rescuers, one to support the extremity and one to apply the splint. As when applying any splint, check patient pulse, motor function, and sensation distal to the injury before and after application. PASGs can also be used as immobilization devices. They are indicated for the emergency medical care of pelvic instability and long bone injuries of the legs with signs and symptoms of shock. They are usually applied by placing them open on a long backboard and moving the patient onto them by log roll or scoop stretcher. The appropriate compartments are then inflated. For example, if the patient has a painful, swollen, deformed left femur, the PASG is inflated in the leg compartment on the side of the injury to act as an air splint. If the patient has pelvic instability and the signs and symptoms of shock, all compartments are inflated to immobilize the
Fig. 29-12 A vacuum splint conforms to the injured area.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 22 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Fig. 29-13 A pillow splint is an improvised splint that provides support for an injured ankle or foot.
lower half of the body. The PASG may be used as a splint on a lower-leg injury only if the ankle is securely immobilized as well. This is possible using a pillow splint applied over the end of the PASG and around the foot and secured. As always, check pulse, motor function, and sensation distal to the injury before and after applying the PASG as a splint. The appropriate uses of PASG remain controversial. Local protocols may differ and must be followed in the application of the PASG. The vacuum splint is wrapped around the injured area, and then the air is removed with a pump so that the splint conforms to the injured area (Fig. 29-12). The splint becomes very rigid and lacks the disadvantages of the air splint. Vacuum splints can be used with angulated injuries. Improvised splints, such as pillows, may be used to support joint injuries and are commonly used for ankle injuries. The pillow is wrapped completely around the ankle and secured. The toes are left visible so that assessment may be made of the pulse, motor function, and sensation (Fig. 29-13). Cardboard
448
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 23 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
448 449
Fig. 29-14 A sling and swathe is a common splinting technique for a shoulder injury to prevent movement of the arm and shoulder.
splints may also be cut to form to an angle and then secured in place. The sling and swathe is the common splinting technique for a shoulder injury. The arm is placed into the sling and the swathe is wrapped around the arm and the body so that the arm and shoulder cannot move (Fig. 29-14). The sling and swathe may be used along with other types of splints for arm injuries. See Principle 29-2 for the proper method in splinting joint and bone injuries.
ALERT!
Always use properly sized splints. Some devices, such as PASG and traction splints, come in infant and child sizes. Familiarize yourself with all the available equipment provided on your ambulance and with local protocols.
RISKS OF SPLINTING
Using splints improperly can lead to complications. If they are not used correctly, they may cause more harm than benefit. A splint can compress nerves, tissues, and blood vessels; therefore, the pressure of the splint should be monitored continuously along with the pulse, motor function, and sensation distal to the injury. A splint applied too tightly on an extremity can reduce distal circulation. An improperly applied
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 24 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
splint can increase bleeding and tissue damage associated with the injury, cause permanent nerve damage or disability, convert a closed injury to an open injury, or increase the pain caused by excessive movement.
PRINCIPLE 29-2 Splinting
1. Use appropriate personal protective equipment for body substance isolation precautions. 2. Apply manual stabilization to the injured area. 3. Assess the pulse, motor function, and sensation distal to the injury. 4. Align the bones with gentle traction only if the distal extremity is cyanotic or lacks pulse and if no resistance is met. 5. Immobilize the injury site with the splint. 6. If the injury is to a joint, immobilize the bone above and below the injury. If the injury is to a bone, immobilize the joint above and below the injury. 7. Reassess the distal pulse, motor function, and sensation and record the findings. Splinting an injury takes time. Do not delay treating or transporting a critical patient to splint an extremity injury. Splinting may be done en route or not at all if the patient has any life-threatening injuries. You can always use the long backboard to splint an injured extremity for critically injured patients. When moving the patient, take extreme care to keep the injury stable.
ALERT!
Injuries to bones and joints require splinting prior to moving the patient unless life-threatening injuries are present. In this case, splinting should be done en route to the receiving facility if possible.
REVIEW QUESTIONS
SPLINTING AN INJURY 1. Before applying a splint, you should check ________, ________ and ________. 1. pulse, sensation, motor function 2. When splinting a hand or foot, you should immobilize them in the _________ _________ ________ to prevent further injury. 2. position of function 3. Traction splints are used for what type of injury?
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 25 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
3. Isolated midshaft femur fracture without involvement of the knee or pelvis 4. A sling and swathe is used to ________ 4. immobilize shoulder or arm injuries 5. If you apply a splint and the distal pulse or sensation is decreased, you should __________ 5. loosen or reposition the splint
449 450
CHAPTER SUMMARY MUSCULOSKELETAL REVIEW
The musculoskeletal system functions to give the body shape, provide for movement, and protect vital internal organs. There are three types of muscle in the human body. Voluntary (skeletal) muscles attach bone to bone and create movement. These muscles are under voluntary control of the individual. Involuntary (smooth) muscles are primarily found in the hollow organs of the digestive system and blood vessels and control the flow of blood and body fluids and substances through them. These muscles are not under conscious control. Cardiac muscle is the muscle of the heart and has automaticity, which is the ability to contract on its own. The skeletal system, in conjunction with muscles, tendons, and ligaments, provides for movement, body shape, and protection. The skeleton is composed of the bones of the skull and face; the spinal column consisting of the cervical, thoracic, lumbar, sacral, and coccygeal vertebrae; the thorax (rib cage); and the lower and upper extremities. Bones are jointed primarily in two different ways: ball-and-socket joints, such as the shoulder, and hinge joints, such as the elbow or knee.
INJURIES TO BONES AND JOINTS
The mechanism of injury is important as an indication of the possible severity of the injury. A musculoskeletal injury is usually the result of a force that has been applied to an area of the body. Direct, indirect, and twisting are some types of forces that can produce injuries to the muscle and bone. Musculoskeletal injuries can be either open or closed. Closed injuries do not break the continuity of the skin, whereas open injuries do break the skin. Excessive movement may cause a closed injury to become an open injury. Signs and symptoms of injury include deformity, angulation, pain, tenderness, grating (crepitation), swelling, bruising, exposed bone ends, and joints that are locked. Emergency medical care of musculoskeletal injuries includes body substance isolation precautions. The airway should always be protected and assessed. High-flow oxygen is indicated for the treatment of these patients. Any major bleeding and life-threatening situations should be cared for immediately. The injured area may be elevated to reduce blood flow to that area, and cold packs may be applied to reduce swelling.
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 26 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Splints can be used to restrict movement and prevent further damage to the injured tissue. Never delay transport of a critical patient to splint an extremity.
450 451
SPLINTING AN INJURY
Splinting a painful, swollen, deformed extremity prevents movement of bone fragments, bone ends, or injured joints; minimizes damage to muscles, nerves, and blood vessels; minimizes the risk of converting a closed injury to an open injury; minimizes the restriction of blood flow resulting from bone ends compressing blood vessels; minimizes excessive bleeding and pain from damaged tissue caused by bone ends or fragments; and minimizes the chance of paralysis of extremities caused by spinal damage. The principles of splinting include: assess the pulse, motor function, and sensation distal to the injury before and after splinting the injury; manually stabilize the joint or bone above and below the injury; remove or cut away clothing on the extremity before splinting the injury; and cover open wounds with clean dressings. Splint the extremity in the position found, unless there is severe deformity or the distal pulse is absent. In this case, use gentle traction to align the extremity before splinting. Do not intentionally replace protruding bones. Pad the splint to prevent pressure and discomfort to the patient. Splint the injury before moving unless life-threatening situations are present. If in doubt about splinting an injury, splint it. If the patient is in shock, use full-body immobilization, align in the normal anatomical position on the backboard, and transport. Rigid splints are nonformable, such as padded-board splints. Traction splints are indicated for a closed, painful, swollen deformity at the midthigh with no joint or lower-leg injury. Do not use a traction splint if the injury is close to the knee; if there is injury to the knee, hip, pelvis, lower leg, or ankle; or if the bone ends are protruding through the skin. Also do not use the traction splint if there is partial amputation or avulsion with bone separation or if the distal limb is connected only by marginal tissue. Pneumatic splints, such as vacuum splints, are flexible, conforming splints used commonly with angulated injuries. A PASG can be used as an immobilization device also. They are indicated in the emergency medical care of pelvic instability and long bone injuries of the femur with signs and symptoms of shock. The sling and swathe is the common splinting technique for the shoulder injury. The arm is placed into the sling, and the swathe is wrapped around the arm and the body so that the arm and shoulder cannot move. The sling and swathe can be used in conjunction with other splints for arm and elbow injuries. Because a splint might compress nerves, tissues, and blood vessels, the pressure of the splint should be checked continually along with the pulse, motor function, and sensation distal to the injury. Excessive movement may cause or aggravate tissue, nerve, vessel, or muscle damage. Do not delay treating or transporting a critical patient to splint.
451 452
United States Department of Transportation National Highway Traffic Safety Administration EMT-Basic Objectives
Check your knowledge. The National Registry of EMTs and many state EMS agencies use the objectives below to develop EMT-Basic certification examinations. Can you meet them?
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition Page 27 of 28
PRINTED BY: Ahed Al Najjar <najjarahed@gmail.com>. Printing is for personal, private use only. No part of this book may be reproduced or transmitted without publisher's prior permission. Violators will be prosecuted.
Cognitive
1. Describe the function of the muscular system. 2. Describe the function of the skeletal system. 3. List the major bones or bone groupings of the spinal column; the thorax; the upper extremities; the lower extremities. 4. Differentiate between an open and a closed painful, swollen, deformed extremity. 5. State the reasons for splinting. 6. List the general rules of splinting. 7. List the complications of splinting. 8. List the emergency medical care for a patient with a painful, swollen, deformed extremity.
Affective
1. Explain the rationale for splinting at the scene versus load and go. 2. Explain the rationale for immobilization of the painful, swollen, deformed extremity.
Psychomotor
1. Demonstrate the emergency medical care of a patient with a painful, swollen, deformed extremity. 2. Demonstrate completing a prehospital care report for patients with musculoskeletal injuries.
452
Mosby's EMT Textbook - Revised Reprint, 2011 Update, 2nd Edition
Page 28 of 28
Vous aimerez peut-être aussi
- Extreme Measure - SummaryDocument1 pageExtreme Measure - SummaryjokazelPas encore d'évaluation
- Skill: Assessing The Breasts and Axillae: AssessmentDocument2 pagesSkill: Assessing The Breasts and Axillae: AssessmentjokazelPas encore d'évaluation
- Analytic MemoDocument4 pagesAnalytic MemojokazelPas encore d'évaluation
- Governance in Health Care Practice ReportDocument7 pagesGovernance in Health Care Practice ReportjokazelPas encore d'évaluation
- Epidemiology Perspective in NursingDocument6 pagesEpidemiology Perspective in NursingjokazelPas encore d'évaluation
- Ethical Dimension of DiversityDocument6 pagesEthical Dimension of DiversityjokazelPas encore d'évaluation
- Bio StatisticsDocument3 pagesBio StatisticsjokazelPas encore d'évaluation
- Bed BathDocument10 pagesBed BathjokazelPas encore d'évaluation
- 01 GlossaryDocument2 pages01 GlossaryjokazelPas encore d'évaluation
- Lunar ExplorationDocument15 pagesLunar ExplorationjokazelPas encore d'évaluation
- Governance in Health Care Practice ReportDocument7 pagesGovernance in Health Care Practice ReportjokazelPas encore d'évaluation
- DOH Manual (Hospital Design)Document6 pagesDOH Manual (Hospital Design)Deven Garcia88% (8)
- Epidemiology Perspective in NursingDocument6 pagesEpidemiology Perspective in NursingjokazelPas encore d'évaluation
- SituationDocument1 pageSituationjokazelPas encore d'évaluation
- Illness - Wellness ContinuumDocument10 pagesIllness - Wellness Continuumhalleyworld93% (29)
- Pedia Theory, G & DDocument323 pagesPedia Theory, G & DjokazelPas encore d'évaluation
- Bed BathDocument10 pagesBed BathjokazelPas encore d'évaluation
- Quizzes OPDDocument1 pageQuizzes OPDjokazelPas encore d'évaluation
- Arellano University Jose Abad Santos Campus 3058 Taft Avenue, Pasay City, Metro ManilaDocument32 pagesArellano University Jose Abad Santos Campus 3058 Taft Avenue, Pasay City, Metro ManilajokazelPas encore d'évaluation
- CoparDocument5 pagesCoparjokazelPas encore d'évaluation
- Quizzes OPDDocument1 pageQuizzes OPDjokazelPas encore d'évaluation
- Philo ProjDocument2 pagesPhilo ProjjokazelPas encore d'évaluation
- 01 GlossaryDocument2 pages01 GlossaryjokazelPas encore d'évaluation
- Copar Hand OutsDocument5 pagesCopar Hand OutsjokazelPas encore d'évaluation
- Prelim SkillsDocument4 pagesPrelim SkillsjokazelPas encore d'évaluation
- Copar Hand OutsDocument5 pagesCopar Hand OutsjokazelPas encore d'évaluation
- CoparDocument5 pagesCoparjokazelPas encore d'évaluation
- CoparDocument5 pagesCoparjokazelPas encore d'évaluation
- Prelim TFNDocument5 pagesPrelim TFNjokazelPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Articular Fractures of The Distal HumerusDocument9 pagesArticular Fractures of The Distal HumerusJoha DavilaPas encore d'évaluation
- Autopsy Report: DECEDENT: John AndersonDocument5 pagesAutopsy Report: DECEDENT: John AndersonjilliankadPas encore d'évaluation
- Closed Fractures of The Tibial Diaphysis: David L. Rothberg, MD Erik N. Kubiak, MDDocument64 pagesClosed Fractures of The Tibial Diaphysis: David L. Rothberg, MD Erik N. Kubiak, MDtilahunthmPas encore d'évaluation
- Zimmer Traction HandbookDocument92 pagesZimmer Traction HandbookMohd Saufee0% (1)
- Musculoskeletal-System NLE ReviewDocument124 pagesMusculoskeletal-System NLE ReviewRitamaria0% (1)
- Lesson 5 Health of The Skeletal SystemDocument21 pagesLesson 5 Health of The Skeletal SystemReynaBaquillerPas encore d'évaluation
- Julius Bishop CVDocument30 pagesJulius Bishop CVAlways At workPas encore d'évaluation
- All Pages v3Document142 pagesAll Pages v3luh martaniPas encore d'évaluation
- FixinDocument44 pagesFixinJaime EscobarPas encore d'évaluation
- Clavicle FractureDocument121 pagesClavicle FractureMuhamad Agung SupriyantoPas encore d'évaluation
- Bone InjuriesDocument35 pagesBone InjuriesSharmaine CabreraPas encore d'évaluation
- Maslaris 2018Document15 pagesMaslaris 2018Jairo GuevaraPas encore d'évaluation
- Generating Report of Bone Fracture and Bleeding Using X-Ray ImagesDocument7 pagesGenerating Report of Bone Fracture and Bleeding Using X-Ray ImagesIJRASETPublicationsPas encore d'évaluation
- Fractures of The Scapula: Charles D. NewtonDocument12 pagesFractures of The Scapula: Charles D. NewtonasheneyPas encore d'évaluation
- Terrible Triad Injury of The ElbowDocument15 pagesTerrible Triad Injury of The ElbowkenthepaPas encore d'évaluation
- Mapeh: Music - Arts - Physical Education - HealthDocument13 pagesMapeh: Music - Arts - Physical Education - HealthGelina TibayanPas encore d'évaluation
- Orthopedic MCQ (Group 5)Document4 pagesOrthopedic MCQ (Group 5)Law YouPas encore d'évaluation
- CH 6 - Bones and Skeletal TissuesDocument119 pagesCH 6 - Bones and Skeletal Tissuesleul amlekePas encore d'évaluation
- Hsin10542 25 06 2014Document136 pagesHsin10542 25 06 2014Anil KumarPas encore d'évaluation
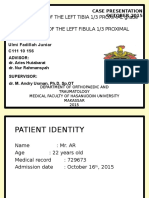
- Ulmi Fadillah - Case Report (Open Fracture Tibia Fibula) Revisi 2Document27 pagesUlmi Fadillah - Case Report (Open Fracture Tibia Fibula) Revisi 2leonardPas encore d'évaluation
- Parasite Electrocution 5.5x8.5 Manual 2 1Document24 pagesParasite Electrocution 5.5x8.5 Manual 2 1Jerry Laviña100% (1)
- 024344Document6 pages024344Aravind DesaiPas encore d'évaluation
- New Trends and Techniques in Open Reduction and Internal Fixation of Fractures of The Tibial PlateauDocument8 pagesNew Trends and Techniques in Open Reduction and Internal Fixation of Fractures of The Tibial PlateauCosmina BribanPas encore d'évaluation
- SCIENCE Cambridge 4th Grade TestDocument7 pagesSCIENCE Cambridge 4th Grade TestLejla Eminovic Niksic73% (33)
- Clou T2 Stryker 15Document56 pagesClou T2 Stryker 15rosette MarcePas encore d'évaluation
- Early Detection of Pediatric Orthopedic DisordersDocument35 pagesEarly Detection of Pediatric Orthopedic Disordersdina hapsariPas encore d'évaluation
- Femur Shaft Fractures in Children: An Epidemiological and Biomechanical StudyDocument71 pagesFemur Shaft Fractures in Children: An Epidemiological and Biomechanical StudyVidini Kusuma AjiPas encore d'évaluation
- Fractures: A. Pusey-Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)Document68 pagesFractures: A. Pusey-Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)okaciaPas encore d'évaluation
- FRACTURE First AidDocument15 pagesFRACTURE First AidAdrian CadaPas encore d'évaluation
- Musculoskeletal Pathology Notes PDFDocument20 pagesMusculoskeletal Pathology Notes PDFvevestephaniPas encore d'évaluation