Académique Documents
Professionnel Documents
Culture Documents
Medical Systems As A Part of Our Cultural Landscape
Transféré par
Qodarian PramukantoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Medical Systems As A Part of Our Cultural Landscape
Transféré par
Qodarian PramukantoDroits d'auteur :
Formats disponibles
It is impossible to take account of medicine without paying attention to
the place and time of its practice and the social and cultural landscape of which it is part. Medicine and society are not separate, independent forces, one determining the other; they are interdependent, and shape each other. [Susan E. Estroff, Social Medicine Reader, 1997: 3]
Introduction Medicine, in our western point of view, is often seen as a knowledge which represents truth itself. This system of knowledge is built upon large number of terms, symbols and performances which serve to determine the causation of illness and classification of particular diseases in taxonomy (Barfield T., 2006, pg.: 318). However medicine, as is generally understood in EuroNorth American culture, is only one type of many medical systems to be found among different cultures.
The dominant medical system in Europe is called, in its correct terminology, biomedicine, and this term is frequently misunderstood for the term of medicine. Biomedicine is a relatively recent tradition that is technologically sophisticated and often extremely successful in curing. When viewed as a cultural system, biomedicine becomes one ethnomedicine among many others, that is, rooted in cultural presupposition and values, associated with rules of conduct, and embedded in larger context (Hahn 1995 in Barfield 2007 pg.: 319).
Any medical system in the cultural sense is a complex of ideas connected to a certain healing tradition. It involves both the behavioural and cognitive components. There are many different traditions of healing, of which some, for example shamanism, are incorporated into the religious system, while another, for example biomedicine may be more likely to be associated with the scientific system of knowledge. Nevertheless such a system is never culture-free.
This, when adopted to the discipline of medical anthropology, brings us to the statement used by Susan E. Estroff, It is impossible to take account of medicine without paying attention to the place and time of its practice and the social and cultural landscape of which it is part. Medicine and society are not separate, independent forces, one determining the other; they are interdependent, and shape each other. This essay will discuss this statement with reference to selected case studies presented in Byron J. Goods work; Medicine, rationality, and experience and to two case studies from the course reading.
Case studies The first case study this essay will discuss is the case of a young woman, a member of Jehovahs Witnesses religious group. This case is interesting in that it provides us with an understanding that problems arriving from different semiotic relationships and symbolic meanings are not solely restricted to exotic causes. The primary physical problem in this case was rectal bleeding; however within the conversation between the patient and physician another issue arose.
This was an issue of the purity of blood, which is very important to Jehovahs Witnesses. When asked about her view of blood transfusion the woman answered, Jehovahs Witnesses dont take blood, because the blood is, uh, the bible refers to the blood as the life, and we are not to take anybodys life into our own bodies... you wouldnt slice somebodys throat and drink it, so you dont stick it in your veins... really its a filthy product... (Byron J., Good, 1994, pg.:94). In this interview the patient
brought in a complex of symbolic meanings, which refers to a definition beyond the common biomedical meaning of blood. She uses a religious form of knowledge.
When the young woman continued, she talked about her personal and family history and the history of her problems. She also included the use of symbolic oppositions with the references to her faith. The analyses of the interview shows many oppositions of which some, blood is life versus its filthy, or its an individual against its foreign, were closely related to her physical problem. However within the interview other distinct issues arose. Many of them were closely related to her life-change, in the meaning of rite of passage. At the time of her visit, it had been only one week since she was baptized. She invokes her spiritual experience by connecting her old life with Satan, dysfunctional family, diseases including cancer and a filthy environment; and the new life in reference to the Bible, baptism, hope, help or fruits and a garden. Although this young woman went to the physician because of her bleeding, her problem was much more profound. For her, it is almost as if the bleeding is part of her old life. This may resolve the question why she went to see the physician long after the problems began and just a few days after her baptism.
This young woman associated her bleeding with the bad from her past. Her new life was much better and purer, and there was no space for bleeding filthy blood. In this sense the patient uses religious and symbolically opposing expressions of reality as a contrast to the biomedical formulation. Similar uses of symbolic opposition are broadly known, and have been described by Levy-Strauss as crucial for the constitution of the meaning. This
is traceable in many human cultures. For example, the Islamic polarity of the religiously pure and impure was joined to other symbolic oppositions (male/female, right/left) (Byron J., Good 1994, pg.; 110).
Such a polarization when applied to the field of the medical system may bring with it serious consequences. Byron J. Good presents in his work a case study from central Turkey. Its subject focused on interviews with sufferers of suspected epilepsy. Epilepsy is highly stigmatized in many cultures and all the consequences and exclusions which accompany this illness are better understood when narrated by patients. In his book Byron illustrates the importance in exploring how illness narratives are structured in cultural terms, and how these reflect or give form to distinctive modes of lived experience (Byron J. Good 1994, pg.: 136).
In this case, the patient and her family paid significant attention to the description of the family background and to richly describing the circumstances of the first attack. There were people who wanted marry her, and her father wanted to force her to marry one of them. She didnt want to be given to that man... After she went off, her father attacked her with knife... and she saw her father with knife, she received shock,... and from that day until today, she has been fainting (Byron J., Good 1994, pg.:136). A very important point is the significance paid to the settings of the first attack. In the culture under discussion, epilepsy is connected with mental retardation.
Thus, the emphasis on the particulars of the attack and shock which follows was crucial for this patient. The distinction between fainting and epilepsy is also important for maintaining relations within the given society. The previous two case studies were analysed with the concern of the problematic to understanding to different symbolic meanings. The patients and physician confronted their knowledge and we learned that in both cases the affliction has had more complex consequences for the afflicted persons. Those exceed afflicting bodily, physical aspect only. Being diagnosed with epilepsy could mean problems for every member of the family in every generation presented.
Also for the Jehovahs Witness the potential blood transfusion would have the ability to destroy the peace this woman had found in her faith. Such understanding comes through analysis of cultural forms the understanding of the cultural saturation is widely accepted in anthropology today (Byron J., Good 1994, pg.: 139).
The last case study discusses the way in which we perceive reality and how that perception can change as new medical technologies are developed. One of the strongest opposition we can find is the opposition between life and death. As a result of our technological advances, the medical system is capable of keeping patients alive, who in past times would have died. In some cases, such interventions maintain the patient somewhere between life and death. Sharon R. Kaufman in Death with Dignity, explores clinical cases where many patients are in a persistent vegetative state, PVS. These patients are kept alive without higher consciousness, some of them for more than ten
years. Most essential physiologic functions are scrutinized and normalcy must be both produced and regulated by detailed and ongoing surveillance (Kaufman R. 2000).
This opens up questions about how technology and social economic conditions enable a remapping of our understanding of life and the person. Kaufman also argues that in these places new forms of knowledge, practice, the body and even a new category of life are created (Kaufman R. 2000). Because the patients are in the persistent comatose condition, all decisions have to be made by others, usually family members. Youll get a patient who, theres no movement, theres no reaction at all. And then all of sudden youll get a response... every patient has something, no matter what the diagnosis (Kaufman R. 2000). This transcript reveals the view of nurses in the clinic, and it shows that medical science cannot articulate adequately on such grey areas.
There is disagreement over what exact level of awareness the PVS patients are in or even whether they should be considered as dead. These are important moral issues and it could be said that in some cases the patients lose their right to die. Another moral issue we have to face in light of this is the issue of using such technologies to keep alive the dead, while in other places around the globe an enormous insufficiency of the most basic medical treatment exists. However such an inequality is common and may be described as a form of structural violence.
Conclusion This essay analysed three different case studies from the field of medical anthropology. All of them examine stories from different cultural backgrounds and with different primary problems. However, in each, the conflicts reach far beyond the field of medicine. They are connected with the reality as we understand and experience it. The essay has also shown that the limits in how we understand and experience our reality are not in fact constant, but changeable.
Different cultures have evolved various forms of medical systems which are implied in relation to various symbolic forms of expression. Some of these symbols, for example, words like AIDS or epilepsy, may be perceived as taboos. This may have side-effects for the afflicted persons in a very different way to the illness itself. Also with the development of our technologies and globalization of information, our reflection of reality is alternating.
In various places and various times the processes of healing may be understood differently in a wider context than it is in biomedicine. To conclude, we must realise that it is impossible to take account of medicine without paying attention to the place, time and context, because medicine is not an independent system of knowledge, but rather an interaction with the cultural landscape.
Bibliography
Barfield T. (ed.), The dictionary of anthropology, 1997, Blackwell publishing, UK, Oxford
Byron J. Good, Medicine, rationality, and experience, an anthropological perspective, 2007, ninth printing, Cambridge university press, UK, Cambridge
Kaufman R. Sharon, In the shadow of death with dignity: Medicine and cultural quandaries of the vegetative state, American anthropologist, New series, vol. 102, No. 1, (Mar., 2000), pp. 69-83
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1091)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Engineering Stages of New Product DevelopmentDocument20 pagesEngineering Stages of New Product DevelopmentRichard CarsonPas encore d'évaluation
- ME 1403 Computer Integrated ManufacturingDocument20 pagesME 1403 Computer Integrated ManufacturingDhileepan Kumarasamy100% (1)
- The Four Hinges Are The Four Cardinal Virtues: Gec 108: EthicsDocument7 pagesThe Four Hinges Are The Four Cardinal Virtues: Gec 108: EthicsDaniela Kian AyalaPas encore d'évaluation
- 2015 Don C. Benjamin - Social World of Deuteronomy A New Feminist CommentaryDocument108 pages2015 Don C. Benjamin - Social World of Deuteronomy A New Feminist CommentaryPedro RamirezPas encore d'évaluation
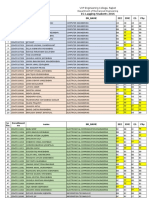
- EG Lagging Students 2016Document30 pagesEG Lagging Students 2016arickPas encore d'évaluation
- JudiciaryDocument21 pagesJudiciaryAdityaPas encore d'évaluation
- Week 3 Lecture Material Isg PDFDocument105 pagesWeek 3 Lecture Material Isg PDFAkhendra KumarPas encore d'évaluation
- EDS261Document8 pagesEDS261micasandogu01Pas encore d'évaluation
- Artificial Intelligence: (Unit 2: Agents)Document5 pagesArtificial Intelligence: (Unit 2: Agents)Lucky sahPas encore d'évaluation
- Sets&StatisticsDocument6 pagesSets&StatisticsFarah AghaverdiyevaPas encore d'évaluation
- The Authentic I Ching The Three Classic Methods of PredictionDocument4 pagesThe Authentic I Ching The Three Classic Methods of Predictionmaximo0% (1)
- 5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryDocument2 pages5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryMikePas encore d'évaluation
- Astro-Diagnosis, A Guide To Healing, Chapters XXX - XXXIIIDocument14 pagesAstro-Diagnosis, A Guide To Healing, Chapters XXX - XXXIIIOmSilence2651100% (1)
- Aruba Controller 650Document2 pagesAruba Controller 650westfiresudamericaPas encore d'évaluation
- Possible Non-Indo-European Elements in HittiteDocument16 pagesPossible Non-Indo-European Elements in HittitelastofthelastPas encore d'évaluation
- MEMORANDUM Statutory RapeDocument5 pagesMEMORANDUM Statutory RapeJing Goal MeritPas encore d'évaluation
- Vistas.1 8 PDFDocument215 pagesVistas.1 8 PDFCool PersonPas encore d'évaluation
- Macbeth-William Shakespeare Study GuideDocument3 pagesMacbeth-William Shakespeare Study GuideBelinda Mirriana LimPas encore d'évaluation
- Strategic Management Final Notes For ExamDocument65 pagesStrategic Management Final Notes For ExamNilesh Mandlik50% (2)
- Quiz GroupingsDocument4 pagesQuiz GroupingsFatima Grace Dela PeñaPas encore d'évaluation
- ME 261 Numerical Analysis: System of Linear EquationsDocument15 pagesME 261 Numerical Analysis: System of Linear EquationsTahmeed HossainPas encore d'évaluation
- Interest GroupsDocument25 pagesInterest GroupsnikkivPas encore d'évaluation
- SLICS Classification DetailedDocument7 pagesSLICS Classification DetailedOj AlimbuyuguenPas encore d'évaluation
- Week 3 CPAR Day 1Document4 pagesWeek 3 CPAR Day 1zessicrel mejiasPas encore d'évaluation
- Part A: 1. Differentiate Among Financial Accounting, Cost Accounting & Management AccountingDocument5 pagesPart A: 1. Differentiate Among Financial Accounting, Cost Accounting & Management AccountingSisir AhammedPas encore d'évaluation
- Unveiling The Factors Shaping Financial Choices Among Women in The Professional Sphere: An Analytical Framework Utilizing Structural Equation Modeling in Behavioral Finance.Document17 pagesUnveiling The Factors Shaping Financial Choices Among Women in The Professional Sphere: An Analytical Framework Utilizing Structural Equation Modeling in Behavioral Finance.International Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- 20 Century Filipino: Traditional ComposersDocument13 pages20 Century Filipino: Traditional ComposersMawi AguiluzPas encore d'évaluation
- Types of Language AssessmentsDocument6 pagesTypes of Language AssessmentsPascual GarciaPas encore d'évaluation
- IDENTIFYING AND FORMING EQUIVALENT FRACTIONS 3RD CO Mrs BiscaydaDocument68 pagesIDENTIFYING AND FORMING EQUIVALENT FRACTIONS 3RD CO Mrs BiscaydaLilibeth BiscaydaPas encore d'évaluation
- Human Medicinal Agents From PlantsDocument358 pagesHuman Medicinal Agents From Plantsamino12451100% (1)