Académique Documents
Professionnel Documents
Culture Documents
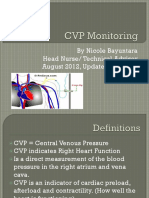
CVP
Transféré par
Jen GarzoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CVP
Transféré par
Jen GarzoDroits d'auteur :
Formats disponibles
Central Venous Pressure (CVP for short) is defined as the pressure of blood in the thoracic vena cava just
before it (the blood) enters the right atrium of the heart. Normal CVP is 5 to 10 cm H2O. CVP measurements are important in clinical cardiology because the CVP is a major determinant of the filling pressure of the right ventricle of the heart. The filling pressure of the right ventricle determines the stroke volume i.e. the amount of blood pumped with each contraction of the heart. Background: Central Venous Pressure is an accurate indicator of the amount of blood returning to the heart from the head, body and limbs via the superior and inferior vena cava. If and when there is blood loss then the CVP reading will be altered (will fall) almost immediately as the amount of blood returning to the heart will have decreased. Central Venous Pressure is also an accurate indicator of the ability of the heart (myocardialpump strength) to pump out blood to maintain normal blood pressure and tissue perfusion. Last but not least, the CVP is an accurate indicator of right ventricular end diastolic volume. In most institutions CVP is measured in cm of water (H2O). On this scale the normal value of CVP is 5 to 10 cm H2O. Some, (very few) institutions measure CVP in mm. Hg (millimetres of mercury). On this scale the normal value is approximately 4 to 8 mm Hg.
CVP measurements are important in clinical cardiology because the CVP is a major determinant of the filling pressure of the right ventricle of the heart. The filling pressure of the right ventricle determines the stroke volume i.e. the amount of blood pumped with each contraction of the heart. Background: Central Venous Pressure is an accurate indicator of the amount of blood returning to the heart from the head, body and limbs via the superior and inferior vena cava. If and when there is blood loss then the CVP reading will be altered (will fall) almost immediately as the amount of blood returning to the heart will have decreased. Central Venous Pressure is also an accurate indicator of the ability of the heart (myocardialpump strength) to pump out blood to maintain normal blood pressure and tissue perfusion. Last but not least, the CVP is an accurate indicator of right ventricular end diastolic volume. In most institutions CVP is measured in cm of water (H2O). On this scale the normal value of CVP is 5 to 10 cm H2O. Some, (very few) institutions measure CVP in mm. Hg (millimetres of mercury). On this scale the normal value is approximately 4 to 8 mm Hg. Generally, when the CVP is rising to unsafe (unhealthy) levels the patient may display difficulties with breathing. Conversely, when the CVP is falling there may be a decrease in urinary output and the patient may complain of feeling excessively thirsty. To correct over hydration, as illustrated by a rising CVP the physician may choose to restrict fluids or to administer a diuretic. To deal with a falling CVP the physician might choose to give the patient more fluids or blood as the case may be.
Indications for Central Venous Pressure Lines A central venous catheter is inserted by a qualified person into one of the central or peripheral veins and then threaded to the exterior of the right atrium where the superior vena cava meets the inferior vena cava. This is only done where medically indicated and qualified nursing staff is available to care, manage, and support the patient. Reading the CVP correctly is essential for the results to be useful therapeutically. The following are some of the general indications for inserting a CVP line.
1.
Monitoring of Central Venous Pressure in the acutely ill patient. This allows the care giver to have an insight into the fluid balance status of the patient. High CVP would indicate fluid overload or a failing heart. Low CVP would indicate a degree of dehydration or blood loss. Exact fluid status can only be evaluated by correlating Hb, Cardiac Functioning and all other lab results and clinical history of the patient. 2. Total Parenteral Nutrition (TPN) Administration. When an acutely ill patients GI tract is not able to absorb nutrients then the treatment team may decide to give the patient nutrition. This is called TPN and TPN can be given safely only via a CVP line or a peripherally inserted central line (PICC). Generally TPN is administered via a central intravenous catheter which is inserted in the subclavian or jugular vein. In infants the Umbilical vein is used most frequently. The rationale for using big deep veins for the administration is the fact that TPN causes phlebitis in peripheral veins because it is contains many caustic components. Examples include Calcium Chloride and Potassium chloride. 3. Medication Administration. Certain medications can be given safely only via a central line. Hence a CVP may be inserted for this purpose. Drugs that are likely to cause phlebitis include Chemotherapeutic Agents used in the treatment and management of malignant conditions. Amiodarone is used extensively in the management and treatment of acute life-threatening arrhythmias as well as for the suppression of chronic arrhythmias. It is useful both for supraventricular and ventricular arrhythmias because it has a low incidence of pro-arrhythmic effects. In arrest trials amiodarone has shown to improve survival rates (when compared to placebo) in individuals who suffer a cardiac arrest. 4. Lack of peripheral access. In some acutely ill patients, when there is no peripheral venous access, then a CVP line may be inserted. This is usually done for the purposes of re-hydration, medication administration, administration of blood and blood products.
Prior to insertion of a CVC catheter it is good practice to clean and set up a trolley with the following equipment.
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13.
CVP catheter Sterile gown for physician or practitioner Sterile gloves and masks. Local anaesthetic Hypodermic needles Silk sutures with needle. CVP insertion kit (with drape, chlorohexidine). Manometer or transducer with monitor and pressure bag Normal saline or heparinised saline according to Hospital policy. Sterile Scissors Op site or other transparent dressing(s). Writing (non-lead) pen Patients chart
When the physician is inserting the CVC catheter the nurse may need to elevate the foot of the bed to increase venous distension so that the physician is able to visualise the blood vessel better. Further, the draped patient may need emotional support too because he may be anxious and it is not comfortable lying there with the face covered and the bright lights shining on the face. The CVC insertion procedure is completed when the CVC is inserted, has been verified with a chest x-ray, adequately secured (stitched in placed) and covered with a sterile dressing. It is the physicians responsibility to place all sharps in the sharps container.
Measuring and Recording the Central Venous Pressure Measuring and recording the CVP is a highly skilled procedure and must be done correctly. Incorrect readings and recordings can result in wrong medical diagnosis and wrong treatments and interventions with disastrous consequences for all care givers, the patient and family. In most institutions Registered Nurses who have had special training perform this procedure. In the acute setting CVP is measured and recorded each hour. Measuring the CVP is done by two methods depending upon availability of equipment. Both methods are accurate if done correctly and are outlined below.
Manometer Method This is a low tech. method and is more frequently done in remote facilities and in poorer countries. All that is needed is a CVC line, fluid, manometer and a skilled team of doctors and nurses. The big disadvantage of this method is that continuous monitoring is impossible and therefore it is of limited value. 1. The procedure is explained to the conscious patient in simple language which he can understand. In instances where the patient is unable to understand the Institutional language an interpreter must be used. This constitutes informed consent and is an important nursing process.
Place the patient in a flat horizontal (supine) position. Use the spirit level indicator on the bed to insure that the patient is horizontal. Older beds may not be equipped with this facility. You may then use a manual spirit level or use your personal (visual) judgment to insure that the bed is truly horizontal. The rational for this is that fluids find their own level and spread out evenly when the patient is horizontal. Please see picture 1 which shows a patient in a horizontal position. Picture 2 shows the spirit level bubble in the middle to signify that the bed is perfectly horizontal. 3. CVC measurements can be taken with the patient in an upright or semi-upright position. The important point to remember is that all CVC measurements must be done with the patient in the same position for the readings to be comparable. It is for this reason that the supine position is the gold standard for recording CVP readings. 4. Flush the CVC to insure that the device is patent. Turn off or pause all fluids which are running through the CVC except medications like noradrenaline which may continue to run because the effective volumes are extremely small. 5. Do not flush any medication lines. This is particularly important because the amount of medication in the line may be sufficient to raise the blood pressure if there is Noradrenaline in the line. The patient may become hypoglycaemic if there is insulin in the line.
2.
6. The zero mark on the manometer is aligned with the phlebostatic axis. This is
called zeroing the CVP. It is done with the aid of a spirit level or a tube containing a fluid with air and water. Zeroing the CVP must be done before every reading otherwise the readings will not be accurate. 7. Clamp off the fluid bag. Rotate the three way tap to connect the fluid and the manometer. Fill the manometer with fluid (Normal Saline should be use unless otherwise indicated) up to the 20 cm mark. Now rotate the three way clamp to connect the manometer to the patient. 8. The fluid level in the manometer falls to the same level as the patients CVP. If the CVP line is not dampened then the level of the CVP should rise and fall with the patients respirations. Please see CVP waveform for more details. 9. Read the CVP when the patient is taking a breath in (at the end of inspiration). This will be the lowest point during a swing cycle. If you ever end up working in the intensive care of a hospital where the patient is on a ventilator you may be able to note that patients who are on ventilators have a lower CVP because the intrathoracic pressure is higher the CVP is elevated artificially. 10. Once a reading is obtained turn the three way tap to allow fluid to connect to patient. This will insure that the CVP line (CVC) remains patent for future use. 11. Document the CVP on the patients chart. Observe it with the previous reading and report changes and abnormal readings to the physician or treatment team. REFER TO PG.4 and PG.5 for pictures
Electronic Transducer Method This method is high tech but is not necessarily more accurate than the manual manometer method described above. The equipment that is required include a CVC, pressured bag of normal saline, electronic transducer, monitor, connecting cables and a skilled team of nurses and doctors. The big advantage of this method is that continuous monitoring is possible and is often done in intensive care units.
1. The CVC is inserted by a duly qualified practitioner. The insertion procedure is the same as that for the manometer method. Informed consent must be obtained from the patient or legal custodian of the patient. 2. The procedure is explained to the conscious patient in simple language which he can understand. In instances where the patient is unable to understand the Institutional language an interpreter must be used. This constitutes informed consent and is an important nursing process. 3. A pressured bag of saline is hung up and connected to the CVC line, the transducer and the CVP lumen of the CVC line. This is generally the proximal lumen most suitable for measuring the CVP. 4. The patient is placed in supine position (flat, horizontal). Use the spirit level indicator on the bed to insure that the patient is horizontal. Older beds may not be equipped with this facility. You may then use a manual spirit level or use your personal (visual) judgment to insure that the bed is truly horizontal. The rationale for this is that fluids find their own level and spread out evenly when the patient is horizontal. 5. The three-way tap is located and the CVP line is connected to the transducer. Most modern transducers give a continuous reading and are routine left in the on position for continuous readings. 6. CVC Catheters differ between manufacturers, however, the white or proximal lumen is the port which is used for measuring the CVP. 7. Turn the tap off to the patient. Open it to air by removing the cap from the three-way port by opening the system to the atmosphere. This will allow the zeroing process. 8. Press the zero button of the monitor and wait until calibration occurs. The time and date of calibration will be displayed. When zeroed time is displayed on the monitor replace the cap of the three-way tap. Maintain sterility at all times. Finally turn the tap on to the patient. 9. Observe the CVP trace on the monitor. The waveform undulates as the right atrium contracts and relaxes, emptying and filling with blood. 10. Document the measurement and report any significant changes to the physician. Reading the CVP.
There are two methods for reading the CVP. The first is to read the high point of the a wave and then the low point of the a. Finally add the two numbers and obtain the average. The result is the mean CVP. Nowadays computers do this for the nurse. All the nurse has to do is to look at the computer and read the CVP off the screen. When using a manual manometer reads the high point and the low point of a respiratory cycle. Add these two and obtain the arithmetic mean. This is the patients CVP. If there is no swinging of the meniscus with the inspiratory and expiratory cycle then the CVP is dampened and the reading is probably less accurate. The second method consists of finding the Z-point which occurs mid to end QRS. The Z-point is read. Since the Z-point occurs just before the closure of the tricuspid valve it is a good indicator of CVP (right ventricular end diastolic pressure). The Z-point is useful when A waves are not visible. This often occurs when the patient is in atrial fibrillation. Again, if a transducer and monitor is being used the computer will do the
calculations. The CVP will be displayed as a digital number and the waveform will be visible below the ECG tracing. Common Causes of Altered Central Venous Pressure The Central Venous Pressure of an individual patient can vary from normal the normal range of between 5 and 10 cm H2O due to a variety of reasons. Some of the common causes of raised (elevated) and lowered CVP are given below. Causes of Elevated CVP Readings 1. Occlusion or kink in central venous catheter. These are the most common causes of wrong readings and all nurses should make sure that the meniscus rises and falls when a reading is being taken. 2. Heart failure. When a patients heat is failing it is unable to pump the blood which is being brought to it by the SVC and the IVC. The backlog of blood causes the CVP to rise. The back pressure is due to the failing heart which results in decreased cardiac output. 3. Therapeutic of accidental fluid overload. The pathophysiology is exactly the same as explained above in number 2. Essentially, the rise in CVP is due to the increased blood volume. 4. Pulmonary embolism. During this disease process the embolus restricts movement of blood through the lungs. The back pressure causes the CVP to rise. 5. Fluid overload. This may be the result of vasoconstriction due to medications or arteriosclerosis. These two factors cause the blood vessels to narrow and a backlog of fluid is produced. This fluid backlog causes CVP to rise. 6. Increased intra-thoracic pressure. This does not occur naturally but occurs when a patient is placed on a ventilator following respiratory failure. The causes of respiratory failure are not discussed here because they are beyond the scope of this article. IPPV and CPAP cause raised intrathoracic pressures which in turn cause the CVP to rise. 7. Dampening of the air filter (getting the air filter wet) can cause the CVP reading to rise because the wet filter does not allow the escape of air from the manometer. This is often referred to as erroneous reading and does not have anything to with the patients physiological processes. 8. Changing a patients position from standing to supine will cause the CVP to rise. 9. Valsalva manoeuvre (forced expiration) will cause the CVP to rise because there is a change in compliance. 10. Contractions of the abdominal and limb muscles alter compliance and circulating fluid returning to the heart. These contractions will generally cause the CVP to rise. Causes of Lowered CVP Readings 1. Blood loss (haemorrhage) and fluid losses caus the CVP to fall. Burns and vomiting are common causes of fluid loss.
2. Excessive use of diuretics causes fluid loss too. This will cause the CVP reading to be low. 3. Vasodilation due to excessive heat, medications, sepsis and neurogenic shock will cause the CVP to fall.
CVP Waveforms
Diagram 1. CVP Waveform Typical. Typical Waveforms: The central venous waveforms seen on the cardiac monitor show the pressure changes in the SVC and IVC (at the location of the tip of the CVC). These are pressure variations which occur during the cardiac cycle. These pressure changes are transmitted in the form of characteristic waves. Typically, there are three positive waves. These are the a, c, and v waves. There are two negative waves. These are the x and y waves. These waves correlate with different phases of the cardiac cycle and EKG . 1. + a wave : This positive wave is due to the increased atrial pressure. During normal right atrial contraction it correlates with the P wave on an EKG. 2. + c wave : This is another positive wave. It is caused by a slight elevation of the tricuspid valve into the right atrium during normal early ventricular contraction. It correlates with the end of the QRS segment on an EKG. The QRS complex is due to ventricular contraction. 3. - x descent : This negative wave is less well understood. It is probably produced by the downward movement of the ventricles during systolic contractions. On the ECG, it occurs before the t-wave. 4. + v wave : This positive wave occurs from the pressure produced during the filling of the right atrium rises becomes it has to deal with the closed tricuspid valve. On the 12 lead ECG this wave correlates with the ending of the T wave. The T wave on the ECG is produced by the repolarisation of the myocardium. 5. - y descent : This is another negative wave. It is the result of the tricuspid valve opening in diastole and with blood flowing into the right ventricle. This wave occurs prior to the P wave on an ECG Cautionary Advice: Since the CVC line is always located in the central part of the thoracic cavity, central venous pressures and waveforms are influenced by changes in intrathoracic pressure during both spontaneous and assisted (ventilated) respirations. All of these changes are small however they can be seen clearly in well functioning CVC lines. As discussed elsewhere the CVP decreases slightly with spontaneous inspiration. It increases slightly with forced exhalation as well as positive pressure mechanical inspiration. A patient on PEEP (positive end expiratory pressure) will have an elevated CVP. These changes are most noticeable when the PEEP is greater than 7.5cm H2O.
Pathologic CVP Waveforms
Variations of the normal central venous waveform can provide information about cardiac pathology physiology e.g. in atrial fibrillation. 1. During AF: a waves will be absent, and in atrioventricular disassociation, a waves will be dramatically increased. When this happens these waves are called cannon waves. The cannon waves are produced because the atrium contracts when the tricuspid valve is closed. 2. During tricuspid regurgitation the c wave and the x wave will be negative. They will be replaced by large positive waves of regurgitation as the blood flows back into the right atrium during ventricular contraction. This generally elevates the average central venous pressure, but it is not an accurate measurement. A better way of obtaining an accurate CVP in similar cases would be by looking at the pressure between the regurgitation waves. 3. In cardiac tamponade, all pressure will be elevated, and the y descent will be nearly absent.
Correctly Interpreting the Patients CVP
The CVP does not measure blood volume or heart functioning directly. However, CVP readings are altered when blood volume alters (e.g. Blood loss or circulatory overload) or when there is heart muscle failure. CVP readings should be interpreted with other clinical data like heart rate, blood pressure, urine output, level of consciousness, and respiratory rate. The absolute value is less significant than serial measurements which reflect the changes in response to therapy. As stated before the normal value during spontaneous breathing is 5-10cm water cmH2O. During mechanical ventilation it rises to by 3-5cmH2O depending upon the PEEP (Positive end of expiration pressure) and ventilator pressure. In some situations the CVP measurement may be in the normal range even when there is Hypovolemia due to vaso/veno constriction. A summary guide to CVP interpretation is shown in below.
Vous aimerez peut-être aussi
- Healing with Herb: Cannabis and HydrocephalusD'EverandHealing with Herb: Cannabis and HydrocephalusPas encore d'évaluation
- Central Venous PressureDocument4 pagesCentral Venous Pressuremike_steven12Pas encore d'évaluation
- Christian Ian A DialysisDocument4 pagesChristian Ian A DialysisMc LagulaPas encore d'évaluation
- Measuring Central Venous Pressure: Elaine ColeDocument8 pagesMeasuring Central Venous Pressure: Elaine ColednllkzaPas encore d'évaluation
- Clinical Cases in Chronic Thromboembolic Pulmonary HypertensionD'EverandClinical Cases in Chronic Thromboembolic Pulmonary HypertensionWilliam R. AugerPas encore d'évaluation
- CVPDocument3 pagesCVPAudreySalvadorPas encore d'évaluation
- Central Venous PressureDocument39 pagesCentral Venous PressureJelly Rose Bajao Otayde100% (2)
- Flashcard Critical CareDocument11 pagesFlashcard Critical CaresnehaPas encore d'évaluation
- Central Venous Preasure: By: Engkus Kusnadi, S.Kep., M.KesDocument26 pagesCentral Venous Preasure: By: Engkus Kusnadi, S.Kep., M.KesShofarie AhmadPas encore d'évaluation
- Central Venous Preasure: By: Engkus Kusnadi, S.Kep., M.KesDocument22 pagesCentral Venous Preasure: By: Engkus Kusnadi, S.Kep., M.KesNenazNaziahPas encore d'évaluation
- 106 Prefi Critical Care Nclex ReviewDocument10 pages106 Prefi Critical Care Nclex ReviewraigenePas encore d'évaluation
- Central Venous PreasureDocument22 pagesCentral Venous PreasureD ZamiatPas encore d'évaluation
- Central Venous Pressure MeasurementDocument6 pagesCentral Venous Pressure MeasurementghalaalsolumiPas encore d'évaluation
- Sub - Medical Surgical Nursing: Assignment On CVP MonitoringDocument11 pagesSub - Medical Surgical Nursing: Assignment On CVP Monitoringkamini ChoudharyPas encore d'évaluation
- CVP and Total Parenteral NutritionDocument4 pagesCVP and Total Parenteral Nutritionkenjam89mbPas encore d'évaluation
- Central Venous Pressure MonitoringDocument13 pagesCentral Venous Pressure MonitoringKris TejereroPas encore d'évaluation
- CVP ReportDocument37 pagesCVP ReportJulienne Sanchez-SalazarPas encore d'évaluation
- Central Venous Pressure (CVP)Document38 pagesCentral Venous Pressure (CVP)Kimberly Abella CabreraPas encore d'évaluation
- Seminar On Hemodynamic Monitoring: BY UMA Iind Year MSC NursingDocument52 pagesSeminar On Hemodynamic Monitoring: BY UMA Iind Year MSC NursingAyen AlingPas encore d'évaluation
- Take5 Hemodynamic1Document2 pagesTake5 Hemodynamic1est03Pas encore d'évaluation
- Hemodynamics MonitoringDocument12 pagesHemodynamics MonitoringBhawna Joshi100% (3)
- Central Venous PressureDocument22 pagesCentral Venous Pressurejhong100% (1)
- Activtiy UntitledDocument6 pagesActivtiy UntitledJan Cyrel ColomaPas encore d'évaluation
- CVP PPPDocument13 pagesCVP PPPYep Yep100% (1)
- Central Venous Pressure and Central LinesDocument13 pagesCentral Venous Pressure and Central Linesaims2099Pas encore d'évaluation
- Hemodynamic MonitoringDocument39 pagesHemodynamic MonitoringNor Jeannah PolaoPas encore d'évaluation
- CVP MonitoringDocument4 pagesCVP Monitoringسانو روديلPas encore d'évaluation
- CVP Evaluation Interpretation PDFDocument3 pagesCVP Evaluation Interpretation PDFMegan LewisPas encore d'évaluation
- Central Venous PressureDocument2 pagesCentral Venous PressureRazaele ManaloPas encore d'évaluation
- Case Study - Cardio FunctionDocument3 pagesCase Study - Cardio FunctionJrBong Semanero100% (1)
- Meds-Study GuideDocument3 pagesMeds-Study Guidejackli21Pas encore d'évaluation
- CVP MonitoringDocument16 pagesCVP MonitoringVictor Elvis0% (1)
- Pulmonary Artery Catheterization and MonitoringDocument31 pagesPulmonary Artery Catheterization and MonitoringVhince Norben PiscoPas encore d'évaluation
- Chapter 65: Critical Care Lewis: Medical-Surgical Nursing, 10th EditionDocument15 pagesChapter 65: Critical Care Lewis: Medical-Surgical Nursing, 10th EditionCrystal LynaePas encore d'évaluation
- Hemodynamic MonitoringDocument10 pagesHemodynamic MonitoringDivya Joy100% (1)
- kh7 CVPDocument50 pageskh7 CVPأبوأحمد الحكيمPas encore d'évaluation
- Hemodynamic Monitoring For NursesDocument29 pagesHemodynamic Monitoring For NursesMahalakshmi Prabhu100% (1)
- Central Venous Monitoring 2022Document17 pagesCentral Venous Monitoring 2022AngiePas encore d'évaluation
- Ramilo, Sheena Patricia M. Ncenh06Document4 pagesRamilo, Sheena Patricia M. Ncenh06JaysellePuguonTabijePas encore d'évaluation
- CVP 3rd YearDocument11 pagesCVP 3rd YearChonkayshek Rias BarrunPas encore d'évaluation
- Monitoring Hemodynamic StatusDocument50 pagesMonitoring Hemodynamic StatusShafiq Ur RahmanPas encore d'évaluation
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 66Document15 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 66sarasjunkPas encore d'évaluation
- Swan Ganz Catheterization: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduDocument24 pagesSwan Ganz Catheterization: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduArchana Maharjan100% (1)
- CVP LineDocument26 pagesCVP LineÂbdàlláh Âl Ñàjjár0% (1)
- Abdominal Compartment SyndromeDocument7 pagesAbdominal Compartment Syndromemezgebu alemnehPas encore d'évaluation
- CVP MonitoringDocument24 pagesCVP MonitoringChoji Heiwajima100% (1)
- 2 Understanding ICU EquipmentDocument45 pages2 Understanding ICU EquipmentAbhinav DuttaPas encore d'évaluation
- Haemodynamic MonitoringDocument6 pagesHaemodynamic MonitoringAnusha Verghese100% (1)
- CVP Care (Swapnil (Document18 pagesCVP Care (Swapnil (SWAPNIL WANJARIPas encore d'évaluation
- CVP Final 2021Document11 pagesCVP Final 2021Ahmed AshrafPas encore d'évaluation
- Central Venous PressureDocument10 pagesCentral Venous PressureAngelo ArquizaPas encore d'évaluation
- Hemodynamic Monitoring Pocket CardDocument5 pagesHemodynamic Monitoring Pocket CardFitz JaminitPas encore d'évaluation
- Measurement of CENTRAL VENOUS PRESSURE Via A TransducerDocument22 pagesMeasurement of CENTRAL VENOUS PRESSURE Via A TransducerJasleen KaurPas encore d'évaluation
- WECOC - Diagnosing HypertensionDocument37 pagesWECOC - Diagnosing HypertensionDhira 'Princess Kalonk' AninditaPas encore d'évaluation
- CVPDocument23 pagesCVPShalini KaluraPas encore d'évaluation
- 3730 Monitoring Hemodinamik-2019Document52 pages3730 Monitoring Hemodinamik-2019ojika olandaPas encore d'évaluation
- Pitfalls in Anesthesia MonitoringDocument56 pagesPitfalls in Anesthesia MonitoringDr.Sandeep Kumar Kar100% (1)
- Daily Patient Assignment SheetDocument1 pageDaily Patient Assignment SheetJen GarzoPas encore d'évaluation
- Vital Signs and I&O SheetDocument1 pageVital Signs and I&O SheetJen GarzoPas encore d'évaluation
- College of The Holy Spirit Manila: WWW - Holyspirit.edu - PHDocument5 pagesCollege of The Holy Spirit Manila: WWW - Holyspirit.edu - PHJen GarzoPas encore d'évaluation
- BCA With Brain Mets PathoDocument2 pagesBCA With Brain Mets PathoJen GarzoPas encore d'évaluation
- Schizophrenia UndifferentiatedDocument64 pagesSchizophrenia UndifferentiatedJen GarzoPas encore d'évaluation
- Assessment Nursing Diagnosis Planning Intervention EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention EvaluationJen GarzoPas encore d'évaluation
- NCI Stages of Grief For Cancer Patients and Their Families - Bear, 2011Document2 pagesNCI Stages of Grief For Cancer Patients and Their Families - Bear, 2011Jen GarzoPas encore d'évaluation
- College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Document2 pagesCollege of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Jen GarzoPas encore d'évaluation
- Bed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Document1 pageBed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Jen GarzoPas encore d'évaluation
- College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Document1 pageCollege of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Jen GarzoPas encore d'évaluation
- Casa Ibiza Resort & Events Place. All Rights ReservedDocument10 pagesCasa Ibiza Resort & Events Place. All Rights ReservedJen GarzoPas encore d'évaluation
- Bed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Document2 pagesBed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Jen GarzoPas encore d'évaluation
- D E N G U E F E V E R: Pathophysiology Dengue Hemorrhagic FeverDocument2 pagesD E N G U E F E V E R: Pathophysiology Dengue Hemorrhagic FeverJen GarzoPas encore d'évaluation
- GordonsDocument2 pagesGordonsJen Garzo100% (1)
- NCP Risk For BleedingDocument1 pageNCP Risk For BleedingJen Garzo75% (4)
- GordonsDocument2 pagesGordonsJen Garzo100% (1)
- Central Venous PressureDocument8 pagesCentral Venous PressureJen GarzoPas encore d'évaluation
- Coping Mechanisms of Students of The College of The Holy Spirit of Manila With Ofw Parents (Print)Document109 pagesCoping Mechanisms of Students of The College of The Holy Spirit of Manila With Ofw Parents (Print)Jen Garzo79% (14)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainD'EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainÉvaluation : 4 sur 5 étoiles4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4 sur 5 étoiles4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (60)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesD'EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesÉvaluation : 4.5 sur 5 étoiles4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (45)