Académique Documents
Professionnel Documents
Culture Documents
Meds Acls
Transféré par
junejune1793Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Meds Acls
Transféré par
junejune1793Droits d'auteur :
Formats disponibles
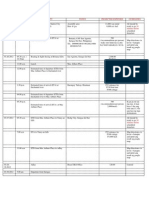
ACLS MEDICATIONS 1. Epinephrine - is the primary drug used in the pulseless arrest algorithm.
It is used for its potent vasoconstrictive effects and also for its ability to increase cardiac output. Epinephrine is considered a vasopressor. Indications for ACLS 1.Vasoconstriction effects: epinephrine binds directly to alpha-1 adrenergic receptors of the blood vessels (arteries and veins) causing direct vasoconstriction, thus, improving perfusion pressure to the brain and heart. 2.Cardiac Output: epinephrine also binds to beta-1-adrenergic receptors of the heart. This indirectly improves cardiac output by: Increasing heart rate Increasing heart muscle contractility Increasing conductivity through the AV nodeDosing Intravenous Push/IO: 1mg epinephrine IV is given every 3-5 minutes. IV infusion for bradycardia: 1mg epinephrine is mixed with 500ml of NS or D5W. The infusion should run at 2-10 micrograms/min (titrated to effect). Endotracheal Tube: 2-2.5mg epinephrine is diluted in 10cc NS and given directly into the ET tube. Epinephrine should be used with caution in patients suffering from myocardial infarction since epinephrine increases heart rate and raises blood pressure. This increase in HR and BP can increase myocardial oxygen demand and worsen ischemia. Note: There is no clinical evidence that the use of epinephrine, when used during cardiac arrest, increases rates of survival to discharge from the hospital. However, studies have shown that epinephrine and vasopressin improve rates of ROSC (return of spontaneous circulation). 2. Vasopressin -is a primary drug used in the pulseless arrest algorithm. In high concentrations, it raises blood pressure by inducing moderate vasoconstriction, and it has been shown to be more effective than epinephrine in asystolic cardiac arrest -One major indication for vasopressin over epinephrine is its lower risk for adverse side effects when compared with epinephrine. With epinephrine, some studies have shown a risk of increased myocardial oxygen consumption and post arrest arrhythmias because of an increase
in heart rate and contractility (beta 1 effects). Vasopressin also is thought too cause cerebral vessel dilation and theoretically increase cerebral perfusion. -Trivia: Another name for vasopressin is antidiuretic hormone (ADH). Routes -Vasopressin may be given IV/IO or by endotracheal tube Dosing - 40 units of vasopressin IV/IO push may be given to replace the first or second dose of epinephrine, and at this time, there is insufficient evidence for recommendation of a specific dose per the endotracheal tube. In the ACLS pulseless arrest algorithm, vasopressin may replace the first or second dose of epinephrine 3. Amiodarone -is considered a class III antiarrhythmic agent and is used for various types tachyarrhythmias. Because of its associated toxicity and serious side-effects it should be used cautiously and care should be taken to ensure that cumulative doses are not exceeded. Indications for ACLS Amiodarone is an antiarrhythmic that is used to treat both supraventricular arrhythmias and ventricular arrhythmias. The mechanism of action of amiodarone remains unknown, but within the framework of ACLS, amiodarone is used primarily to treat ventricular fibrillation and ventricular tachycardia that occurs during cardiac arrest and is unresponsive to shock delivery, CPR, and vasopressors. Amiodarone should not be used in individuals with polymorphic VT as it associated with a prolonged QT interval which is made worse with antiarrhythmic drugs. Amiodarone should only be used after defibrillation/cardioversion and first line drugs such as epinephrine and vasopressin have failed to convert VT/VF. Route Amiodarone can be administered by intravenous, IO route Dosing The maximum cumulative dose in a 24 hour period should not exceed 2.2 grams. Within the VT/VF pulseless arrest algorithm, the dosing is as follows: 300mg IV/IO push (if no conversion) 150 mg IV/IO push (after conversion) Infusion #1 360 mg IV over 6 hours (1mg/min) Infusion #2 540 mg IV over 18 hours (0.5mg/min)
For tachyarrhythmias other than life threatening, expert consultation should be considered before use. For Tachycardia other than pulseless VT/VF, Amiodarone dosing is as follows: (see above note) 150 mg over 10 minutes repeat as needed if VT recurs maintenance infusion of 1mg/min for 6 hours Amiodarone should only be diluted with D5W and given with an in-line filter. 4. Although lidocaine was removed from the 2010 Simplified Pulseless Arrest Diagram, it is still considered a suitable alternative if amiodarone is ineffective in cardiac arrest from VT/VF. Lidocaine was removed in the AHA Simplified Pulseless Arrest Diagram to help reduce emphasis on the use of medications and place more emphasis on high quality CPR and early defibrillation. Indications for ACLS In ACLS, Lidocaine is used intravenously for the treatment of ventricular arrhythmias. (VT/VF) It is also useful for the treatment of stable monomorphic VT with preserved ventricular function and for stable polymorphic VT with preserved left ventricular function, normal QT interval, and correction of any electrolyte imbalances. Side Effects Lidocaine should be used with caution due to negative cardiovascular effects which include hypotension, bradycardia, arrhythmias, and/or cardiac arrest. Some of these side effects may be due to hypoxemia secondary to respiratory depression. Lidocaine Toxicity Symptoms of lidocaine toxicity progress in the following predictable pattern. It begins with numbness of the tongue, lightheadedness, and visual disturbances and progresses to muscle twitching, unconsciousness, and seizures, then coma, respiratory arrest, and cardiovascular depression. There are several conditions that increase the potential for lidocaine toxicity: 1.Liver dysfunction increases the risk of toxicity due to lidocaine being metabolized by the liver. 2.Low protein increases the risk of toxicity because lidocaine is protein bound. 3.Acidosis can also increase the risk of toxicity since acidosis increase the potential of lidocaine to dissociate from plasma proteins
Dosing Cardiac Arrest from VT/VF: Initial dose: 1 to 1.5 mg/kg IV/IO For refractory VF may give additional 0.5 to 0.75 mg/kg IV push, repeat in 5 to 10 minutes; maximum 3 doses or total of 3mg/kg Perfusing Arrhythmia: For stable VT, wide-complex tachycardia of uncertain type and significant ectopy: Doses Range from 0.5 to 0.75 mg/kg and up to 1 to 1.5mg/kg Repeat 0.5 to 0.75 mg/kg every 5-10 minutes with maximum total dose of 3 mg/kg Maintenance infusion: 1 to 4 mg/min (30-50 mcg/kg/min) Discontinue a lidocaine infusion immediately if signs of toxicity develop
5. Atropine Atropine is the first drug used to treat bradycardia in the bradycardia algorithm. It is classified as an anticholinergic drug and increases firing of the SA Node by blocking the action of the vagas nerve on the heart resulting in an increased heart rate. Atropine should be used cautiously in the presence of myocardial ischemia and hypoxia since it increases oxygen demand of heart and can worsen ischemia The dosing for Atropine is 0.5 mg IV every 3-5 minutes as needed, and the maximum total dosage that can be give is 3 mg. 6. Adenosine -should be used within the tachycardia algorithm when vagal maneuvers fail to terminate stable narrow-complex SVT -When given as a rapid IV bolus, adenosine slows cardiac conduction particularly effecting conduction through the AV node. The rapid bolus of adenosine also interrupts reentry (SVT causing) pathways through the AV node and restores sinus rhythm in patients with SVT. -When injected into the body, adenosine is rapidly absorbed by red blood cells and blood vessel endothelial cells and metabolized for natural uses throughout the body. In light of this adenosine should be administered by RAPID intravenous bolus so that a significant bolus of adenosine reaches the heart before it is metabolized.
Dosing The first dose of adenosine should be 6 mg administered rapidly over 1-3 seconds followed by a 20 ml NS bolus. If the patients rhythm does not convert out of SVT within 1 to 2 minutes, a second 12 mg dose may be given in similar fashion. All efforts should be made to administer adenosine as quickly as possible. Precautions Some side effects of adenosine administration incude flushing, chest pain/tightness, brief asystole or bradycardia. 7. Dopamine -stimulates adrenergic receptors. Increase cardiac ourput and bp -2nd line drug for symptomatic bradycardia, hypotension with signs and symptoms of shock. Dose: infusion of 5-20 mcg/kg/min titrate to patient response Use caution with cardiogenic shock associated with CHFmay cause tachydyrythmiass- monitor heart rate. 8. MgSO4 -Torsade De Pointe VT; Hypomagnesmia hinders the cellular movement of K+ and thereby makes the heart prorrhythmic. May cause hypotension with rapid administration, caution in renal failure. Dose: 1-2gm IV push over 1-2 minutes. Torsade with pulse = 1-26mg in 100ml D5W over 5-60 minutes 9. Sodium Bicarb -Indication: Acidosis reversal. Initial dose without a blood gas: 1meq/kg IV push w/ half dose administered q10min Mainlyh used for TCA OD, Hyperkalemia, pre-existing metabolic acidosis
10. Allerfin -anti histamine drug -may cause drowsiness.do not take with alcohol,sedatives as it may increase drowsiness effect 11. Ventolin - Selective beta-2 agonist that stimulates adrenergic receptors of the sympathetic nervous system resulting in smooth muscle relaxation in the bronchial tree and peripheral vasculature - Treatment of bronchospasm in patients with reversible obstructive airway disease (COPD/asthma). Prevention of exercise-induced bronchospasm. -monitor heart rate as it may cause tachycardia Dosage: Adult: Administer 2.5 mg. Dilute 0.5 mL of 0.5% solution for inhalation with 2.5 mL NS in nebulizer and administer over 10-15 minutes. MDI: 1-2 inhalations (90-180g). Five minutes between inhalations.
12. Calcium Chloride
-Indication: Magnesium Toxicity or Calcium Channel blocker Over Dose 500-100mg IV Be careful with patients on Digitalis 13. Verapamil -is a calcium channel blocker used to treat angina,arrhythmias. - 2.5 to 5 mg IV over 2 minutes. May repeat dose of 5-10mg 15-30 minutes after 1st dose. Alternative initial choice in stable patients. Decrease dose by 30-50% in hepatic insufficiency. Adverse reactions: Severe hypotension; bradycardia; ventricular standstill in digitalized patients; asystole; respiratory failure. Hypotension can be reversed with calcium chloride 0.5-1 gram over 5 minutes 14.Aminophyyline - Aminophylline is a bronchodilator - Aminophylline is a nonselective adenosine receptor antagonist and phosphodiesterase inhibitor capable of reversing ischemia-induced bradyasystole2 . It does this by improving the rate of return of spontaneous circulation (ROSC). During atropine-resistant out-of-hospital cardiac arrest, all aspects of attempted resuscitation must proceed in accordance with standard Advanced Cardiac Life Support (ACLS) guidelines3 . After exhaustive conventional therapy, aminophylline is administered early in resuscitation efforts to re-establish cardiac rhythm4 . With aminophylline administration, the patient may have immediate resumption of cardiac electrical
activity5 . Aminophylline should be an intervention with the ACLS treatment of atropine-resistant asystolic out-of-hospital cardiac arrest6 . 15. Phenytoin - Phenytoin sodium (/fnton/) is a commonly used antiepileptic. Phenytoin acts to suppress the abnormal brain activity seen in seizure by reducing electrical conductance among brain cells by stabilizing the inactive state of voltage-gated sodium channels. Aside from seizures, it is an option in the treatment of trigeminal neuralgia in the event that carbamazepine or other first-line treatment seems inappropriate 16. D50 -tx of hypoglycaemia.volume expander
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Accounting Information System - Chapter 1Document41 pagesAccounting Information System - Chapter 1Lizette OlivaPas encore d'évaluation
- ThreatDocument1 pageThreatjunejune1793Pas encore d'évaluation
- AIS01Document49 pagesAIS01Fitriyah Az-zahraaPas encore d'évaluation
- 2012 AICPA Financial QuestionsDocument60 pages2012 AICPA Financial Questionsjunejune1793Pas encore d'évaluation
- Date Time Activity Venue Projected Expenses GuidelinesDocument1 pageDate Time Activity Venue Projected Expenses Guidelinesjunejune1793Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Dvanced Cardiac Life SupportDocument72 pagesDvanced Cardiac Life Supportolivia100% (1)
- EpinephrineDocument4 pagesEpinephrinegovind_soni_15Pas encore d'évaluation
- Pha-Bls 2H2019Document3 pagesPha-Bls 2H2019Abram BunoanPas encore d'évaluation
- Acls FixDocument20 pagesAcls Fixluthfi adityaPas encore d'évaluation
- BLS For TeacherrDocument166 pagesBLS For TeacherrGavinKarl Mianabanatao100% (1)
- MylatestSOS BLS ACLS LectureDocument87 pagesMylatestSOS BLS ACLS LectureArmin MercadoPas encore d'évaluation
- CPR MCQ 03Document21 pagesCPR MCQ 03Ryam Taif100% (1)
- 2013 Eman Ramadan Abdel Moniem AliDocument5 pages2013 Eman Ramadan Abdel Moniem AliEug UlepPas encore d'évaluation
- Philippine Heart AssociationDocument2 pagesPhilippine Heart AssociationNURSES' PADPas encore d'évaluation
- Rahal ResumeDocument2 pagesRahal Resumeapi-503911568Pas encore d'évaluation
- Approved Abbreviations: Administrative 1.0Document12 pagesApproved Abbreviations: Administrative 1.0jhoniPas encore d'évaluation
- User Manual CardiostartDocument113 pagesUser Manual CardiostartLouie Jay AmantePas encore d'évaluation
- Professional Development Plan: By: Isabella RahalDocument10 pagesProfessional Development Plan: By: Isabella Rahalapi-503911568Pas encore d'évaluation
- Basic Life Support (BLS) in AdultsDocument13 pagesBasic Life Support (BLS) in AdultsElena ChitoiuPas encore d'évaluation
- ACLS SubhankarDocument87 pagesACLS SubhankarMarc Andreo MalalaPas encore d'évaluation
- Basic Life Support Written ReportDocument8 pagesBasic Life Support Written ReportLovely Ann AviadoPas encore d'évaluation
- ACLS Precourse Self-AssessmentDocument3 pagesACLS Precourse Self-AssessmentHollan GaliciaPas encore d'évaluation
- Managemen Disritmia: Dr. Rofika Hanifa, SPPDDocument20 pagesManagemen Disritmia: Dr. Rofika Hanifa, SPPDavivlabirdPas encore d'évaluation
- Emergency and Disaster Nursing 2012Document218 pagesEmergency and Disaster Nursing 2012Darran Earl Gowing100% (2)
- ACLS Online Training Material: Unit One: General ConceptsDocument34 pagesACLS Online Training Material: Unit One: General ConceptsJohn JenjinsPas encore d'évaluation
- ACLS Secondary Survey For A Patient in Respiratory ArrestDocument2 pagesACLS Secondary Survey For A Patient in Respiratory ArrestLady MuffinsPas encore d'évaluation
- Emergency Cart ProcedureDocument20 pagesEmergency Cart ProcedureAyiessa_AJPas encore d'évaluation
- American Heart Association Acls Post Test AnswersDocument4 pagesAmerican Heart Association Acls Post Test AnswersArun Jude Alphonse0% (9)
- Cardiology USMLE 2CK (Cardio Clinical Care) Flashcards - MemorangDocument4 pagesCardiology USMLE 2CK (Cardio Clinical Care) Flashcards - MemorangMohamed Abbas0% (2)
- AHA Program Administration ManualDocument69 pagesAHA Program Administration ManualMohammad AbdUllah TahirPas encore d'évaluation
- AclsDocument13 pagesAclsAllah YarPas encore d'évaluation
- 12 - Chapter 2Document39 pages12 - Chapter 2Add KPas encore d'évaluation
- Pals Pediatric BradycardiaDocument1 pagePals Pediatric BradycardiadarlingcarvajalduquePas encore d'évaluation
- Management of Cardiac ArrestDocument10 pagesManagement of Cardiac ArrestAhmed VelićPas encore d'évaluation
- Updatesincardiacarrest Resuscitation: Vivian Lam,, Cindy H. HsuDocument15 pagesUpdatesincardiacarrest Resuscitation: Vivian Lam,, Cindy H. HsuFia Bella KusumaPas encore d'évaluation