Académique Documents
Professionnel Documents
Culture Documents
Universitas Indonesia
Transféré par
Ramadhan AkmalDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Universitas Indonesia
Transféré par
Ramadhan AkmalDroits d'auteur :
Formats disponibles
UNIVERSITAS INDONESIA
RHEUMATOID ARTHRITIS
CASE PRESENTATION
ADLY NANDA AL FATTAH, 0606065125 DINI
Supervisor:
INTERNAL MEDICINE FACULTY OF MEDICINE UNIVERSITAS INDONESIA JANUARY 2011
CHAPTER 1 Case Illustration
Identity Name Age Address Religion Occupation : Mrs. A : 35 years old : Rangkasbitung, West Java : Moslem : midwife
Anamnesis (autoanamnesis 28th December 2010) Chief Complaint Pain and swollen on her shoulder, elbow, wrist, finger, knee, and ankle joints since 2 years before hospital admission. Present History Illness Since approximately 2 years ago (beginning of 2009), patient complaints morning stiffness on her shoulder, elbow, wrist, finger, knee, and ankle joint. The complaint was appear almost every day and persisted for about an hour. Patient also complaints that she had her proximal part of the right index finger, the joint of the right little finger, and the left knee swelling, redness, and tense. There was also pain on those joints. The pain is persisted, not moving to the other joints. Patient tells that she was not being able in wearing her own trouser and holding the comb. The patient went to the internist at Rangkasbitung and underwent several laboratory tests. The results are the positive rheumatoid factor (RF), 105 mm of erythrocyte sedimentation rate (ESR), and normal limit of uric acid. Patient given Methylprednisolone 3 x 4 mg for 2 months and then the complaints was subsided. Patient also received Meloxicam 2x7.5 mg, Ranitidine 2 x 1 tab, CaCO3 2x1 tab. At that time (19 months ago), the patient is being pregnant. After delivery, the patient wants to continue to check-up at RSCM regarding the internist opinion. Even though the complaints were being subsided on the therapy given, she still wants to find better therapy at rheumatologist at RSCM. At this time, patient is coming to the clinic to check up for her disease (for previous 10 months, the patient also checked up at RSCM regularly). The patient is still complaining of pain on her left knee, both of wrists, and left little finger joints. The pain is persisted and felt especially on the movement of the joint. The drugs taken regularly are Methotrexate 6 tablets for 1 week, Methylprednisolone 2 x 1 tablet, folic acid 2 x 1 tab, CaCO3 3x1 tablet, Lansoperazole 1x1 tablet, Actonel 2x20 mg/week. There was no history
of nausea, vomiting, diarrhea, mouth sores and hair loss. Now the patient is being able to drive the motorcycle, but the pain is still felt when she is walking. Past History Illness She denied any history of hypertension, DM, asthma, and allergy Family History Illness There is history of hypertension from the mother. She denied any history of DM, asthma, allergy, and heart disease in her family. There are no histories of rheumatoid arthritis or the other joint diseases in the family. Physical Examination General status: CM, moderately Ill Vital signs: Blood Pressure 100/70 mmHg Heart Rate 88x/min, regular, enough filling Temperature 36,6oC Respiratory Rate 16 x/min
Body Height: 152 cm Body Weight: 57 kg BMI : 24.6
Status Generalis Head Eye : : Normocephali Anemic conjunctival (-/). Icteric sclera (-/-). Direct Pupils Reflexes +/+, Indirect Pupils Reflects +/+ deformity -, wide, secrete -/-, secrete -/-, septum deviation -/-, conchae hypertrophy -/Tonsil T1/T1, hiperemis (-) good mucosal, bad oral hygiene, caries dentis (+) JVP 5-2cmH20, trachea is in the middle, lymph nodes not palpable, thyroid is not palpable
Ear Nose
: :
Throat : Mouth : Neck :
Thorax:
Lung I P P A Heart I P P line A Abd Ext wrist.
: : Statically and dynamically symmetric : Symmetric left and right fremitus : Sonor above all lung field :vesicular, rhonchi (-/-), wheezing (-/-) : : Ictus cordis is not visualized : Ictus cordis is palpable on 1 finger medial from left midclavicular line : Right border : Right parasternalis linne, Left border: 1 finger medial from left mudclavicular
: Normal heart sound S1 & S2, murmur (-), Gallop (-) :flat, supple, ascites (-), pain (-), bowel sound (+) normal :Oedema (-), warm acral, CRT < 2, swollen on left knee, right proximal interphalanges, and left
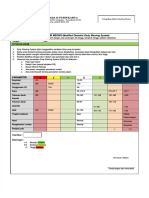
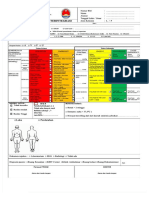
Local Status (28/12/2010)
Local Status (24/1/2010)
Laboratory Findings (27/12/2010) Items Hemoglobin Hematocryte Leukocyte Diff. count Basophiles Eosinophile Neutrophile Lymphocytes Monocyte Thrombocyte Erythrocyte Sedimentation Rate SGOT (AST) SGPT (ALT) Anti CCP serum Problems list: Rheumatoid Arthritis Plan Diagnostic Plan: - CBC, ALT/AST, Ureum/Creatinine Treatment Plan: Oral Methotrexate 1x15 mg/week 7 tablets once weekly Oral Methylprednisolone 1x4 mg/day Folic acid 2 x 1 tablet/day CaCO3 3 x 1 tablet/day Lansoperazole 1 x 30 mg /day Patient 13.6 g/dl 42.7 % (35-43) 15.800/uL 0 % 0 % 90 % 9 % 1 % 428.000/ul 27 mm 14 12 2066.5 RU/ml Normal limit 13-16 40-48 5000-10000 0-1 1-3 52-76 20-40 2-8 150.000-440.000 0-10 < 33 < 46
Education Plan: Exercise: regular, dynamic physical activity Weight Control: weight control and dietary modification Disease monitoring and co morbidities : o o o o eating plenty of fruit, vegetables and whole grain cereal foods eating foods rich in fish oil (omega-3) eating a diet low in fat eating only a moderate amount of sugars and foods containing added sugars, and
o o o
choosing low salt foods and using salt sparingly Monitor at least 3 times per year: CVS, GIT, liver, and renal function
Inform about the side effects of the drugs; Use contraception to prevent pregnancy for until 3 months stop taking methotrexate
CHAPTER 2 LITERATURE REVIEW
REFERENCES
Vous aimerez peut-être aussi
- Resusitasi Jantung Paru Berkualitas: Dr. Ichwan Zuanto 3 FEBRUARI 2018 Rsia Setya BhaktiDocument12 pagesResusitasi Jantung Paru Berkualitas: Dr. Ichwan Zuanto 3 FEBRUARI 2018 Rsia Setya BhaktiIchwan Zuanto SjamanPas encore d'évaluation
- 2608 Pedoman Pws Kia 2Document93 pages2608 Pedoman Pws Kia 2bibit herawatiPas encore d'évaluation
- Dapsa EngDocument1 pageDapsa EngwawanpecelPas encore d'évaluation
- Pengkajian Triase: Resusitasi (P1) Emergency (P2) Less Urgent (P4)Document1 pagePengkajian Triase: Resusitasi (P1) Emergency (P2) Less Urgent (P4)Obet BassangPas encore d'évaluation
- Lta FiveDocument100 pagesLta FiveEchy RahmadhaniPas encore d'évaluation
- Manajemen HipertensiDocument46 pagesManajemen HipertensiYeni BelawatiPas encore d'évaluation
- Alkes Kit Emergency NeonatusDocument2 pagesAlkes Kit Emergency NeonatusgusmargonoPas encore d'évaluation
- Pengaruh Penyuluhan Kesehatan Terhadap PDocument8 pagesPengaruh Penyuluhan Kesehatan Terhadap PEdith LauraPas encore d'évaluation
- LABIOPALATOSCHIZISDocument25 pagesLABIOPALATOSCHIZISEya Prepti SerraPas encore d'évaluation
- Form Telaah RM ExelDocument9 pagesForm Telaah RM ExelBlack BoxPas encore d'évaluation
- Formulir Meows (FORMULIR MEOWS (Modified Obstetric Early Warning System Modified Obstetric Early Warning System) )Document2 pagesFormulir Meows (FORMULIR MEOWS (Modified Obstetric Early Warning System Modified Obstetric Early Warning System) )miraPas encore d'évaluation
- Makalah Keselamatan PasienDocument17 pagesMakalah Keselamatan Pasiensinta widhiePas encore d'évaluation
- ISMOAC - 20241 - Read-OnlyDocument30 pagesISMOAC - 20241 - Read-Onlyaditya galih wicaksonoPas encore d'évaluation
- Lembar Balik Cuci TanganDocument7 pagesLembar Balik Cuci TanganKristo FaniPas encore d'évaluation
- Hubungan Preeklamsi Berat Dengan Kelahiran Preterm Di Rumah Sakit Umum Provinsi Nusa Tenggara Barat 2013Document10 pagesHubungan Preeklamsi Berat Dengan Kelahiran Preterm Di Rumah Sakit Umum Provinsi Nusa Tenggara Barat 2013Vera Andri YaniPas encore d'évaluation
- Logbook Obeserver E3Document28 pagesLogbook Obeserver E3Ricky PebriansyahPas encore d'évaluation
- Introduction Pno: Afia Halida Nadiaty, S.TRDocument12 pagesIntroduction Pno: Afia Halida Nadiaty, S.TRIsa doraPas encore d'évaluation
- Etnografi KesehatanDocument3 pagesEtnografi KesehatanAkri SarumahaPas encore d'évaluation
- Format Lplpo 2020Document32 pagesFormat Lplpo 2020Syarif HalimPas encore d'évaluation
- Peran KomunikasiDocument10 pagesPeran KomunikasiIndra Mawan MawanPas encore d'évaluation
- Modul 2 - 3 PDFDocument70 pagesModul 2 - 3 PDFTarmidi MidziPas encore d'évaluation
- ID Faktor Faktor Yang Mempengaruhi PerilakuDocument11 pagesID Faktor Faktor Yang Mempengaruhi PerilakuM Ekmal Yusuf PutraPas encore d'évaluation
- Proker NewDocument40 pagesProker Newnahdia100% (1)
- Demam TifoidDocument32 pagesDemam TifoidMageswari SelvarajooPas encore d'évaluation
- Materi SEPSISDocument42 pagesMateri SEPSISdellanurainiPas encore d'évaluation
- Data SDMK PKM Ciparay 2019Document12 pagesData SDMK PKM Ciparay 2019heryanzPas encore d'évaluation
- Promkes PPDocument56 pagesPromkes PPwisnuPas encore d'évaluation
- Kel 3 TPNDocument32 pagesKel 3 TPNTriliantari Siregar0% (1)
- Code Sisrute 5Document41 pagesCode Sisrute 5Bayu BimarthaPas encore d'évaluation
- Poster 5 Moment Cuci TanganDocument2 pagesPoster 5 Moment Cuci TanganalfonsaPas encore d'évaluation
- Cranial Nerve Examination 231109 191528Document43 pagesCranial Nerve Examination 231109 191528najlaxd2002Pas encore d'évaluation
- First Year 2019docxDocument262 pagesFirst Year 2019docxCherry100% (1)
- NBS Law FinalDocument33 pagesNBS Law Finalkissiah Cajetas100% (1)
- Kebutuhan Alat Alat AnestesiDocument5 pagesKebutuhan Alat Alat AnestesiidrisPas encore d'évaluation
- Jurnal CA. MammaeDocument7 pagesJurnal CA. MammaeNengahOktaVianyPas encore d'évaluation
- Jadwal Acara PIT POGI 25 Padang Update 3 Sept 2021Document8 pagesJadwal Acara PIT POGI 25 Padang Update 3 Sept 2021daniel_alexander_susenoPas encore d'évaluation
- Askep Preeklampsia - CoverDocument6 pagesAskep Preeklampsia - CoverARPas encore d'évaluation
- Format JurnalDocument16 pagesFormat JurnalRetno puspitariniPas encore d'évaluation
- SRF934 PDFDocument2 pagesSRF934 PDFDidyPas encore d'évaluation
- Tor Iht Manajemen NyeriDocument5 pagesTor Iht Manajemen NyeriheriiskandarPas encore d'évaluation
- 18-Article Text-35-3-10-20190830Document9 pages18-Article Text-35-3-10-20190830ariefPas encore d'évaluation
- Fidratul Khasanah-FKIK PDFDocument127 pagesFidratul Khasanah-FKIK PDFsinarPas encore d'évaluation
- Dosen Pembimbing Jeni Cesi Cintiani, SSTDocument1 pageDosen Pembimbing Jeni Cesi Cintiani, SSTitaPas encore d'évaluation
- Format Triage RSTDocument1 pageFormat Triage RSTnovia swPas encore d'évaluation
- Formulir Laporan Insiden Internal Di PuskesmasDocument3 pagesFormulir Laporan Insiden Internal Di Puskesmassandal sanglirPas encore d'évaluation
- Dyspepsia PDFDocument14 pagesDyspepsia PDFCdma Nastiti FatimahPas encore d'évaluation
- Form Triage RevisiDocument2 pagesForm Triage RevisiRSUD SUMBAWAPas encore d'évaluation
- Perlindungan Hukum Terhadap Peserta BpjsDocument22 pagesPerlindungan Hukum Terhadap Peserta BpjsRizal Saputra100% (1)
- Brosur Klinik VCTDocument2 pagesBrosur Klinik VCTNila WatiPas encore d'évaluation
- Contoh Rundown Basic Life SupportDocument2 pagesContoh Rundown Basic Life SupportElok Faiqotul Umma100% (1)
- Skenario Asfiksia UNSRI 4Document43 pagesSkenario Asfiksia UNSRI 4opi neanPas encore d'évaluation
- JakNEWS 8 2nd Announcement FixDocument66 pagesJakNEWS 8 2nd Announcement FixFerdy HalimPas encore d'évaluation
- Jurnal Pisang Ambon Pada Hipertensi PDFDocument6 pagesJurnal Pisang Ambon Pada Hipertensi PDFVivoraroPas encore d'évaluation
- Tuberkulosis (Batuk Darah) : Bagaimana Pengobatannya?Document2 pagesTuberkulosis (Batuk Darah) : Bagaimana Pengobatannya?Wildan'z CreedPas encore d'évaluation
- Diabetes Melitus DAN Puasa Ramadhan: Dr. Andravina Pranathania Puskesmas Kelurahan SelongDocument38 pagesDiabetes Melitus DAN Puasa Ramadhan: Dr. Andravina Pranathania Puskesmas Kelurahan SelongRima Indah Sari LubisPas encore d'évaluation
- Meatotomy/meatoplasty: Procedure-Specific InformationDocument7 pagesMeatotomy/meatoplasty: Procedure-Specific Informationsyaiful rinantoPas encore d'évaluation
- National Cholesterol Education Program: Adult Treatment Panel III (ATP III) GuidelinesDocument103 pagesNational Cholesterol Education Program: Adult Treatment Panel III (ATP III) GuidelinesAdil AhmedPas encore d'évaluation
- Artikel SaraaaaaDocument8 pagesArtikel SaraaaaaArdiantiWulandariHusenPas encore d'évaluation
- Neurology Writeup - 2Document9 pagesNeurology Writeup - 2Bo GuanPas encore d'évaluation
- Patan Academy of Health Sciences School of Medicine Lagankhel, LalitpurDocument12 pagesPatan Academy of Health Sciences School of Medicine Lagankhel, LalitpurSARMITA SHRESTHAPas encore d'évaluation
- Booms Ma 2019Document48 pagesBooms Ma 2019Ramadhan AkmalPas encore d'évaluation
- The Origins of Genome Complexity: Science December 2003Document6 pagesThe Origins of Genome Complexity: Science December 2003Ramadhan AkmalPas encore d'évaluation
- Siam 2012Document7 pagesSiam 2012Ramadhan AkmalPas encore d'évaluation
- The Effect of Intrauterine Insemination Time On Semen ParametersDocument4 pagesThe Effect of Intrauterine Insemination Time On Semen ParametersRamadhan AkmalPas encore d'évaluation
- Editorial: Sperm Differentiation and Spermatozoa Function: Mechanisms, Diagnostics, and TreatmentDocument4 pagesEditorial: Sperm Differentiation and Spermatozoa Function: Mechanisms, Diagnostics, and TreatmentRamadhan AkmalPas encore d'évaluation
- Accepted Manuscript: 10.1016/j.cbi.2018.07.002Document28 pagesAccepted Manuscript: 10.1016/j.cbi.2018.07.002Ramadhan AkmalPas encore d'évaluation
- Timing 2018Document4 pagesTiming 2018Ramadhan AkmalPas encore d'évaluation
- LymphedemaDocument47 pagesLymphedemaRamadhan Akmal100% (2)
- Timingyavas 2004Document10 pagesTimingyavas 2004Ramadhan AkmalPas encore d'évaluation
- HormonesDocument9 pagesHormonesRamadhan AkmalPas encore d'évaluation
- Influenza Vaccines For The FutureDocument8 pagesInfluenza Vaccines For The FutureRamadhan AkmalPas encore d'évaluation
- Anal Dilatations PDFDocument3 pagesAnal Dilatations PDFRamadhan AkmalPas encore d'évaluation
- Kuliah NeurodiagnostikDocument4 pagesKuliah NeurodiagnostikRamadhan AkmalPas encore d'évaluation
- Medicine 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS-1 PDFDocument24 pagesMedicine 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS-1 PDFAditya Barman100% (1)
- Rheumatoid Arthritis Nursing Care PlanDocument3 pagesRheumatoid Arthritis Nursing Care PlanCyrus De Asis95% (22)
- GeriaDocument78 pagesGerianikki_sia_150% (2)
- Buildup of Fatty Plaque in The Arteries, Is The MostDocument7 pagesBuildup of Fatty Plaque in The Arteries, Is The MostCherry Bobier100% (1)
- Diagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDateDocument20 pagesDiagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDateDannyGutierrezPas encore d'évaluation
- Nutrition Interventions in Rheumatoid ArDocument11 pagesNutrition Interventions in Rheumatoid ArJULIETAPas encore d'évaluation
- Rheumatoid ArthritisDocument21 pagesRheumatoid ArthritisKatrene LequiganPas encore d'évaluation
- Nursing PresentationDocument63 pagesNursing PresentationDeekayPas encore d'évaluation
- Model Answer: Important Instructions To ExaminersDocument31 pagesModel Answer: Important Instructions To Examinersmannuu00Pas encore d'évaluation
- Aseklofenak MonografDocument132 pagesAseklofenak MonografAbdurrahimPas encore d'évaluation
- Venom Book ReviewDocument17 pagesVenom Book ReviewgnjidaPas encore d'évaluation
- DVDGGDocument10 pagesDVDGGSilviPas encore d'évaluation
- Presentation of RaDocument47 pagesPresentation of RaRutashobya Manara TopManyotaPas encore d'évaluation
- HBC q4 2022 Financial ReportDocument18 pagesHBC q4 2022 Financial ReportMaria PolyuhanychPas encore d'évaluation
- Clinical Tutorial 2008.11.05Document31 pagesClinical Tutorial 2008.11.05Ywagar Ywagar100% (1)
- List of Autoimmune DiseasesDocument11 pagesList of Autoimmune DiseasesDuwa AhmadPas encore d'évaluation
- A Dictionary of Rheumatology PDFDocument235 pagesA Dictionary of Rheumatology PDFTeodora PolgarPas encore d'évaluation
- Ra Case StudyDocument52 pagesRa Case StudyMiracle Guillermo100% (4)
- 3365460Document3 pages3365460Mohamed NabilPas encore d'évaluation
- Basic of Manual TherapyDocument30 pagesBasic of Manual Therapycamy bhagatPas encore d'évaluation
- Rheumatoid ArthritisDocument52 pagesRheumatoid ArthritisArun NingarajappaPas encore d'évaluation
- MJP Tips and InfoDocument4 pagesMJP Tips and InfonatyaPas encore d'évaluation
- Chapter-08 - Examination of Musculoskeletal SystemDocument9 pagesChapter-08 - Examination of Musculoskeletal SystemAnnahi BcPas encore d'évaluation
- Krok 2 - 2014 (Therapy)Document74 pagesKrok 2 - 2014 (Therapy)areenPas encore d'évaluation
- Rheumatoid ArthritisDocument28 pagesRheumatoid ArthritisNisya Andesita HPas encore d'évaluation
- Clinical Case JiaDocument28 pagesClinical Case JiaShymaPas encore d'évaluation
- Rheumatoid ArthritisDocument2 pagesRheumatoid ArthritisRiena Austine Leonor NarcillaPas encore d'évaluation
- Management of Pregnancy in Women With Rheumatoid Arthritis: Clinical Focus Clinical FocusDocument3 pagesManagement of Pregnancy in Women With Rheumatoid Arthritis: Clinical Focus Clinical FocusLatifa Tistanty Permadi AlchairidPas encore d'évaluation
- Orthodontics in Medically CompromisedDocument189 pagesOrthodontics in Medically CompromisedAshish MathewPas encore d'évaluation
- DataDocument207 pagesDatamikhael muaneoPas encore d'évaluation
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainD'EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainÉvaluation : 4 sur 5 étoiles4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4 sur 5 étoiles4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesD'EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesÉvaluation : 4.5 sur 5 étoiles4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (45)