Académique Documents
Professionnel Documents
Culture Documents
Fracture
Transféré par
Vanessa SantosDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Fracture
Transféré par
Vanessa SantosDroits d'auteur :
Formats disponibles
I- Introduction
A fracture is a break in the continuity of bone and is defined according to its type and extent. Fractures occur when the bone is subjected to stress greater that it can absorb. Fractures are caused by direct blows, crushing forces, sudden twisting motions, and even extreme muscle contractions. When the bone is broken, adjacent structures are also affected, resulting in soft tissue edema, hemorrhage into the muscles and joints, joint dislocation, ruptured tendons, severed nerves, and damaged blood vessels. Body organs maybe injured by the force that cause the fracture or by the fracture fragments. There are different types of fractures and these include, complete fracture, incomplete fracture, closed fracture, open fracture and there are also types of fractures that may also be described according to the anatomic placement of fragments, particularly if they are displaced or nondisplaced. Such as greenstick fracture, depressed fracture, oblique fracture, avulsion, spinal fracture, impacted fracture, transverse fracture and compression fracture. A comminuted fracture is one that produces several bone fragments and a closed fracture or simple fracture is one that not cause a break in the skin. Comminuted fracture at the Right Femoral Neck is a fracture in which bones of the Right Femoral Neck has splintered to several fragments. By choosing this condition as a case study, the student nurse expects to broaden her knowledge understanding and management of fracture, not just for the fulfillment of the course requirements in medical-surgical nursing. It is very important for the nurses now a day to be adequately informed regarding the knowledge and skill in managing these conditions since hip fracture has a high incidence among elderly people, who have brittle bones from osteoporosis (particularly women) and who tend to fall frequently. Often, a fractured hip is a catastrophic event that will have a negative impact on the patients life style and quality of life. There are two major types of hip fracture. Intracapsular fractures are fractures of the neck of the femur, Extracapsular fracture are fractures of the trochanteric region and of the subtrocanteric region. Fractures of the neck of the femur may damage the vascular system that supplies blood to the head and the neck of the femur, and the bone may die. Many older adults experience hip fracture that 1
student nurse need to insure recovery and to attend their special need efficiently and effectively. True the knowledge of this condition, a high quality of care will be provided to those people suffering from it.
II. Objectives
General Objectives: After three day of student nurse-patient interaction, the patient and the significant others will be able to acquire knowledge, attitudes and skills in preventing complications of immobility.
Specific Objectives: A. STUDENT-NURSE CENTERED After 8 hours of student nurse-patient interaction, the student nurse will be able to: 1. state the history of the patient. 2. identify potential problems of patient 3. review the anatomy and physiology of the organ affective 4. discuss the pathophysiology of the condition. 5. identify the clinical and classical signs and symptoms of the condition. 6. implement holistic nursing care in the care of patient utilizing the nursing process. 7. impart health teachings to patient and family members to care of patient with fracture. B. PATIENT-CENTERED After 8 hours of student nurse-patient interaction, the patient and the significant others will be able to: 1. explain the goals of the frequent position changes. 2. enumerate the position for proper body alignment. 3. discuss the different therapeutic exercises. 4. practice the different kinds of range of motion. 5. participate attentively during the discussion.
III. Nursing Assessment
1. Personal History 1.1 Patients Profile
Name: Mrs. Torralba, Lourdes Age: 89 years old Sex: Female Civil Status: Widow Religion: Roman Catholic Date and time of admission; March 13, 2008 at 10:10 am Room No.: Room 425, Cebu Doctors University Hospital Complaints: Pain the right hip Impression or Diagnosis: Fracture Close-Comminuted: Femoral Right Neck General Osteoporosis Breast Cancel (Right) Diabetes Mellitus Type II Physician: Dr. F. Vicuna, Dr. E. Lee, Dr. N. Uy, Dr. Ramiro Hospital No: 216 426
1.2. Family and Individual Information, Social and Health History
Mrs. Torralba, Lourdes who resides in 8 Acacia St. Camputhaw Lahug, Cebu City, Cebu Province with 9 successful children ( 6 boys and 3 girls) was admitted to Cebu Doctors University Hospital for further management of the condition. Mrs. Torralba is a college graduate and shes previously working as an assistant of her husband ( Mr. Rodrigo Torrralba ) a doctor. The patient was diagnosed to have Breast Cancer (Right) last 2006 with bone metastasis and on chemotherapy with aromasin.
Two days prior to admission, the patient was standing and was about to open up he umbrella when she got out of balance and landed on her right hip.And had experienced limitation of movement on the right hip. The patient was then admitted due to the persistence of pain. The patient was previously hospitalized due to infected wound at the right ankle last 2002. No familial history of hypertension and bronchial asthma but is positive to diabetes mellitus of paternal side. Has no known food and drug allergies. The patient is non-smoker non-alcoholic beverages drinker.
1.3. Level of Growth and Development
1.3.1. Normal Growth and Development at particular stage Older Adult ( 65 Years old to death)
Physical Development
Perception of well-being can define quality of life. Understanding the older adults perception about health status is essential for accurate assessment and development of clinically relevant interventions. Older adults concepts of health generally depend on personal perceptions of functional ability. Therefore older adults engaged in activities of daily living usually consider themselves healthy, whereas those whose activities are limited by physical, emotional or social impairments may perceive themselves as ill. There are frequently observed physiological changes in order adults that are called normal. Finding these normal changes during and assessment is not an expected. These physiological changes are not always pathological processes in themselves, but they may make older adults more vulnerable to some common clinical conditions and diseases. Some older adults experience all of these physiological changes, and others only experience only a few. The body changes continuously with age, and specific effects on particular older adults depend on health, lifestyle, stressors and environmental conditions.
Cognitive Development
Intellectual capacity includes perception, cognitive, memory, and learning. Perception, or the ability to interpret the environment, depends on the acuteness of the senses. If the aging persons senses are impaired, the ability to perceive the environment and react appropriately is diminished. Perceptual capacity may be affected by changes in the nervous system as well. Cognitive ability, or the ability to know, is related to the perceptual ability. Changes in cognitive structure occur as a person ages. It is believe that there is a progressive loss of neurons. In addition, blood flow to the brain decreases, the meaninges appear to thicken, and brain metabolism slows. As yet, little is known about the effect of these physical changes on the cognitive functioning of the older adult. Older people need addition time for learning, largely because of the problem of retrieving information. Motivation is also important. Older adults have more difficulty than younger ones in learning information they do not consider meaningful. It is suggested that the older person mentally active to maintain cognitive ability at the highest possible level. Life long mental activity, particularly verbal activity, helps the older person retain the high level of cognitive function and may help maintain a long-term memory. Cognitive impairment that interferes with normal life is not considered part of normal aging. A decline in intellectual abilities that interferes with social or occupational functions should always be regarded as abnormal.
Psychosocial Development
According to Erikson, the developmental task at this time is ego integrity versus despair. People who attain ego integrity view with a sense of wholeness and derive satisfaction from past accomplishment. They view death as an acceptable completion. According to Erikson, people who develop integrity accept ones one and only life style. By contrast, people who despair often believe they have made poor choices during life and wish they have made poor choices during life and wish they could live life over. Robert Butler sees integrity and bringing serenity and wisdom, and despair as resulting in 6
the inability to accept ones fate. Despair gives rise of frustration, this couragement, and a sense that ones life has been worthless.
Moral Development
According to Kohlberg, moral development is completed in the early adult years. Most old people stay at Kohlbergs conventional development, and some are at the preconventional level. An elderly person at the preconventional level obeys roles to avoid pain and the displeasure of others. At stage one, a person defines good and bad in relation to self, whereas older persons at stage 7 may act to meet anothers need as well as their own. Elderly people at the conventional level follow societys rules of conduct to expectation of others.
Emotional Development
Well-adjusted aging couples usually thrive on companionship. Many couples rely increasingly on their mates for this company and may have few outside friends. Great bonds if affection and closeness can develop during this period of aging together and nurturing each other. When a mate dies, the remaining partner inevitably experiences feelings of loss, emptiness, and loneliness. Many are capable and manage to live alone; however, reliance, on younger family members increases as age advances and in health occurs. Some widows and widower remarry, particularly the latter, because the widowers are less inclined than widows to maintain a household.
Spiritual Development
Murray and Zentner write that the elderly person with a mature religious outlook striver to incorporate views of theology and religious action into thinking. Elderly people can contemplate new religious and philosophical views and try to understand ideas missed previously or interpreted differently. The elderly person also derives a sense of worth by sharing experiences or views. In contrast, the elderly person who has not 7
matured spiritually may not matured spiritually may feel impoverishment or despair as the drive for economic and professional success wares.
Psychosexual Development Sex drives persist into the 70s, 80s, and 90s, provided that the health is good and an interested partner is available. Interest in sexual activity in old age depends, in large measure, on interest earlier in life. That is, people who are sexually active in young and middle adulthood will remain active during their later years. However, sexual activity does become less frequent. Many factors may play a rate in the ability of an elderly person to engage in sexual activity. Physical problems such as diabetes, arthritis, and respiratory conditions affect energy or the physical ability to participate in sexual activity. Changes in the gonads of elderly women result from diminished secretion of the ovarian hormones. Some changes, such as the shrinking of the uterus, and ovaries, go unnoticed. Other changes are obvious. The breasts atrophy, and lubricating vaginal secretions are reduced. Reduced natural lubrication is the cause of painful intercourse, which often necessities the use of lubricating jellies. 3.1.2. Ill Person at the Particular Age of Patient The older fracture patients showed a higher prevalence of chronic brain syndrome, they were in poorer physical state and their skinfold thickness was less. They also had more unrecognized visual disorders. Those who were younger had a higher prevalence of stroke than comparable controls. The type of fall leading to the fracture varied with agetripping was the commonest cause in the younger patients and drop attacks in the older. Both stroke and partial sightedness were associated with falls due to loss of balance. The older patients had a very high prevalence of pyramidal tract abnormality associated with chronic brain syndromeand it appears that these demented patients fall not because of mental confusion but because of associated motor abnormalities.
Ertra-capsular fractures occur in older patients. They are more likely to have a history of falls but previous fracture is equally common at this age in the fracture and control series.
2. Diagnostic Test Patients Result
Diagnostic test April 10, 2008 Complete Blood Count Hemoglobin Hematocrit WBC RBC
Normal values
Significance
14.0-17.5 g/dL 41.5-50.4% 4.4-11.0x10^ g/uL 4.5-5.9x10^ g/uL
9.1 28.8 5.32 2.8
- Decreased-various anemias, with excessive fluid intake. -Decreased-severe anemias -Normal -Decreased- all anemias and leukemia, when blood volume has been restored. -Normal
Mean Corpuseular Hemoglobin Mean Cell Volume (MCA) Mean Corpuseular Hemoglobin Platelet
27.5-33.2 pg
32.7
80-96 fL
103.6
-Increased-macrocytic anemia
33.4-35.5 %
32
-Decrease-severe hypochronic anemia
150,000-450,000
387
-Normal
Differential Count Neutropihl Basophil Eosinophil Monocyte Lympocyte
40-70 % 0-1 % 0-5 % 0-8% 20-40%
67 0 4 09 20
-Normal -Normal -Normal -Increase-viral infection, collagen and hemolytic disorders -Normal Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2. page 2214-2215 -Normal
Serum
3.6-5
4.7
10
Potassium Creatinine Calcium Protein Albumen Globulin Total Protein GCT(50gms)
6.7-1.5 8.4-10.2 1.2-2.2 3.3-5.5 2 6.8 65-110 8-35 u/mL
6.6 8.2 1.0 2.9 2.9 5.8 145 20
-Decreased-Muscular atrophy, anemia, leukemia -Decreased-vitamin D. deficiency -Decreased-anemia, malnutrition -Decreased-no clinical significance -Increased-chronic infection, multiple myeloma -Decreased-malnutrition -Increased-diabetes mellitus -Normal Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2.page 2217,2219,2221,2224,2229,2230,2232 -Increased-diabetes mellitus Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2.page 2230,2233,
PBS
65-110
118
Uric acid
2.5-7.5
4.4mg/dL
-Normal Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2.page 2225, -Normal
Bleeding time-sim
2.3-9.5
6.31 min.-sec. 10.41 min.-sec. 13.8 sec.
Clotting time
5-15
-Normal
Prothombin time
10-13
-Increased-deficiency of factors I, II, V, VII, and X, fat malabsorption -Normal
% activity
70-120
96.2 %
11
INR
<1.2
1.03
-Normal Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2.page 2214
Urinalysis Macroscopic Examination Color Appearance Plt Specific gravity Protein Glucose Ketones Blood Leukocytes Yellow Clear 4.5-7.8 1.003-1.029 Negative Negative Negative Negative Negative Yellow Clear 6.0 1.010 Trace Trace Negative Negative Negative -Normal -Normal -Normal -Normal -Glomerular disease, nephritic syndrome -Diabetes mellitus -Normal -Normal -Normal
Nitrite Bilirubin Urohilinogen
Negative Negative Normal
Negative Negative 0.2 eu/dL
-Normal -Normal -Normal
Microscopic Examination RBC/hpf WBC/hpf Bacteria Mucus threads 0-5 0-5 Present Present 0-2/hpf 0-2/hpf Few Few -Normal -Normal -Normal -Normal
12
Amorphous Urates Blood cell
Present Negative
Few Few
-Normal Indicates renal or urinary tract disease Source: Brunner and Suddarths. Textbook of Medical-Surgical Nursing.10th Edition Volume 2.page 2224,2225
13
3. Present Profile of Functional Health Patterns
Profile of Functional Health Patterns
3.1. Health Perception / Health Management Pattern
The patient described her usual health before to be fair and body is strong but now she considered it to be poor and weak. This is because of the limited movements she felt, the inability to walk or stand and difficulty in moving the extremities due to the fracture of her right femoral neck. Before the admission, the patient eats more foods rich in fats, sugar or glucose and cholesterol in their meals and she drinks plenty of water everyday. During the patients hospitalization, her diet was changed to low fat and low cholesterol diet because she was diagnosed of having diabetes mellitus type II. The patients attending physician encourages her to take more of calcium and Vitamin D in order for her bones to become stronger. The patient is non-smoker and non-alcoholic drinker and she has no known allergies.
3.2. Nutritional / Metabolic Pattern The patients usual food intake before the hospitalization includes fish, meat, vegetables, fruits, chicken and especially foods rich in fats, sugar/glucose and cholesterol. She consumes more than 8 glasses of water a day. Her maintenance meds were Aromasin, Fosamax, Centrum and Caltrate. Now the patient was advised by her attending physician to restrict foods that can aggravate her condition. The patient was also encourage to take more of Calcium and Vitamin D in order for her bones to become stronger. The patient doesnt smoke or drink alcoholic beverages, has no known allergies. There is a change in her appetite now; she often eats a little only each meal.
14
3.3. Elimination Pattern Before, the patient can freely go to the C.R. to void or defecate but now that shes hospitalized she was advised to wear diaper for her to have difficulty in standing and walking. There is no burning sensation during ur4ination and her stool is brownish formed stool.
3.4. Activity-Exercise Pattern
The patient before hospitalized wakes up early in the morning for her to have fine walking around their house as her exercise. She usually guided her grandsons and granddaughters, but now, shes just on bed lying assisted by her private nurses and CDUH health care providers.
3.5. Cognitive/ Perceptual Pattern
The patient before, can hear, smell, taste and feel well and correctly but the patient cannot read her newspaper without her eyeglasses just the same as now. She speaks slowly English, Tagalog and Bisaya languages as of now but before she speaks fluently all of those languages. She easily communicates, understands questions, instructions and be able to follow and answer them correctly.
3.6. Rest/ Sleep Pattern
Before the hospitalization, the patient usually sleeps late at night at around 10 oclock pm and wakes up early in the morning at 6 oclock am with an hour of sleep of 8 hours. Now, she usually sleeps early at night (8-9 oclock pm) and wakes up at around 7 oclock am with an hour of sleep of 10 hours. The patient usually stays in bed and read newspapers sometimes, she cant take a nap in the afternoon due to her REHAB CARE.
15
3.7. Self- Perception Pattern The patients most concern about right now is her rehabilitation care. The patient wants to stay at the hospital until she improves her mobility so she would be able to stand and walk all alone by herself. The patient never loses the support of her children even if they were not there physically and also her private nurses. Through this, she maybe able to cope up easily from her unhealthy condition. The treatment, managements, medications and all out care rendered by the hospital to the patient assured her for the improvement of her condition.
3.8. Sexuality/ Reproduction The patients husband just recently died. Now, the patient does not allow anyone to see her getting undressed, changing diaper, changing clothes because she believes that as a woman, it should be keep as private.
3.9. Coping- Stress Tolerance Pattern
The patient usually makes her decision as for now since her children were busy in their work abroad, but they make sure they never forget to support and help their mother recover from illness. Sometimes, the patient usually shares her concerns to her private nurses and of course also to the student nurses. She usually reads newspaper for her to be more relaxed.
3.10. Value-Belief Pattern
The patient find source strength and hope with God and her loved ones. God is very much important to the patient. Before, she usually goes to church together with her other children. They were not involved in any religious organizations or practices. The patient knows how to pray and praise God for all the nice things he had given.
16
3.11. Relationship Pattern
The patient understands more on English and Bisaya languages but a little only in Tagalog language. The patient was living all by herself with her private nurses but sometimes, her grandchildren will come over to visit her. She never uses the support of her children even if they were away from their mother they always make sure that their mother is safe and secure. The patient can easily communicate, cooperate, listen and follow instructions easily.
17
4. Pathophysiology and Rationale
4.1 Normal Anatomy and Physiology of Organ/ System Affected
The word skeleton comes from the Greek word meaning dried- up body, our internal framework is so beautifully designed and engineered and it puts any modern skyscraper to shame. Strong, yet light, it is perfectly adapted for its functions of body protection and motion. Shaped by an event that happened more than one million years ago when a being first stood erect on hind legs our skeleton is a tower of bones arranged so that we can stand upright and balance ourselves. The skeleton is subdivided into three divisions: the axial skeleton, the boned that form the longitudinal axis of the body, and the appendicular skeleton, the bones of the limbs and girdles. In addition to bones, the skeletal system includes joints, cartilages, and ligaments (fibrous cords that bind the bones together at joints). The joints give the body flexibility and allow 18
movement to occur. Besides contributing to body shape and form, or bones perform several important body functions such as support, protection, movement, storage and blood cell formation.
Classification of Bones
The diaphysis, or shaft, makes up most of the bones length and is composed of compact bone. The diaphysis is covered and protected by a fibrous connective tissue membrane, the periosteum. Hundreds of connective tissue fibers, called Sharpeys fibers, secure the periosteum to the underlying bone. The epiphyses are the ends of the long bone. Each epiphyses consist of a thin layer of compact bone enclosing the area filled with spongy bone. Articular cartilage, instead of periosteum, covers its external surface. Because the articular cartilage is glassy hyaline cartilage, it provides a smooth, slippery surface that decreases friction at joint surfaces. In adult bones, there is a thin line of bony tissue spanning the epiphyses that looks a bit different from the rest of the bone in that area. This is the epiphyseal line. The epiphyseal line is a remnant of the epiphyseal plate (a flat plate of hyaline cartilage) seen in young, growing bone. Epiphyseal plates cause the lengthwise growth of the long bone. By the end of puberty, when hormones stop long bone growth, epiphyseal plates have been completely replaced by bone, leaving the epiphyseal lines to mark their previous location. In adults, the cavity of the shaft is primarily a storage area for adipose (fat) tissue. It is called the yellow marrow, or medullary, in infants this areas forms blood cells, and red marrow is found these. In adult bones, red marrow is confined to the cavities of spongy bone of flat bones and the epiphyses some long bones. Bone is one of the hardest materials in the body, and although relatively light in weight, it has a remarkable ability to resist tension and other forces acting on it. Nature has given us an extremely strong and exceptionally simple (almost crude) supporting system without up mobility. The calcium salts deposited in the matrix bone its hardness, whereas the organic parts (especially the collagen fibers) provide for bones flexibility and great tensile strength. 19
The femur, or thigh bone, is the only bone in the thigh. It is the heaviest, strongest bone in the body. Its proximal end has a ball-like head, a neck, and greater and lesser trochanters (separrsted anteriorly by the intertrochanteric line and posteriorly by the intertrochanteric crest). The trochanters, intertrochanteric crest and the gluteal tuberosity, located on the shaft, all serve us sites for muscle attachment. The head of the femur articulates with acetabulum of the hip bone in a deep, secure socket. However, the neck of the femur is a common fracture site, especially in old age. The femur slants medially as it runs downward to joint with the leg bones; this brings the knees in line which the bodys center of gravity. The medial course of the femur is more noticeable in females because of the wider female pelvis. Distally on the femur are the lateral and medial condytes, which articulates the tibia below. Posteriorly, these condytes are separated by the deep intercondylar notch. Anteriorly on the distal femur is the smooth patellar surface, which forms a joint with the patella, or kneecap.
20
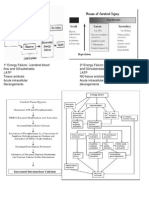
4.2
Schematic Diagram
Predisposing Factors: -Elderly people (85 years or older) - Trauma - Comorbidity - Malnutrition -neurologic problems - Obesity -slower reflexes Precipitating Factors: -Fall - osteoporosis -functional disability - impaired vision and balance
Damage to the blood supply to an entire bone.
Severe circulatory compromise
Avascular (ischemic) necrosis may result
Clinical Manifestations: - Pain (right up) - Loss of function - Deformity - Crepitus - Swelling and discoloration - Paresthesia - Tenderness
Nursing Management: Medical Management: - Repositioning the patient - Temporary skin traction - Promoting strengthening exercise - Bucks extension - Monitoring and managing complications - Open or closed reduction of the fracture and - Health promotion internal fixation - Relieving pain - Replacement of the femoral head with - Promoting physical mobility prosthesis (hemiarthrmoplasty) - Promoting positive psychological response to - Closed reduction with pereutaneous stabilization trauma for an intracapsular fracture. - Patient teaching Surgical Intervention: - Hip Pinning - Hip Hemiarthroplasty - Patients with hip osteonecrosis may require Hip Replacement Surgery
21
4.3 Pathophysiology
Femoral neck fractures occur most commonly after falls. Factors that increase the risk of injuries are related to conditions that increase the probability of falls and those that decrease the intrinsic ability of the person to with stand the trauma. Physical deconditioning, malnutrition, impaired vision and balance, neurologic problems, and shower reflexes all increase the risk of falls. Osteoporosis is the most important risk factor that contributes to hip fractures. This condition decreases bone strength and, therefore, the bones ability to resist trauma. Femoral neck fractures can also be related to chronic stress instead of a single traumatic event. The resulting stress fractures can be divided into fatigue fractures and insufficiency fractures. Fatigue fractures are a result of an increased or abnormal stress placed on a normal bone. Whereas insufficiency fractures are due to normal stresses placed on diseased bone, such as an osteoporotic bone. Trauma sufficient to produce a fracture can result in damage to the blood supply to an entire bone, e.g., the femoral neck in femoral fracture. With seer circulatory compromise, avascular (ischemic) necrosis may result. Particularly vulnerable to the development of ischemic are intracapsular fractures, as occur in the hip. In this location, blood supply is marginal ad damage to surrounding soft tissues may be a critical factor since better results are obtained in cases of hip fracture reduced with in 12 hr. than in those treated after that tine period. In fractures of the femoral neck, bone scans have been recommended as diagnostic tools to determine the orability of the femoral need.
22
4.4 Classical and Clinical Signs and Symptoms Classical Symptoms Pain Clinical Symptoms Manifested - complains of pain on the right hip aggravated by sudden or too much movements of the extremities and relieved by elevation and resting. Manifested - unable to move extremities and unable to stand or walk without assistance. Rationale - The pain is continuous and increases in severity until the bone fragment are immobilized. The muscle spasm that accompanies fracture is a type of natural splinting designed to minimize further movement of he fracture fragments. -After a fracture, the extremity cannot function properly, because normal function of the muscles depends on the integrity of the bones to which they are attached. Pain contributes to the loss of function. In addition, abnormal movement (false motion) may be present.
Loss of function
Deformity
Manifested -Displacement, angulations, or - Bones of the right rotation of the fragments in a fracture femoral neck are of the right femoral neck causes a splintered into small deformity that is detectable when the fragments. limb is compared with the uninjured extremity. Deformity also results from soft tissue swelling. Not Manifested - In fractures of long bones, there is actual shortening of the extremity because of the contraction of the muscles that are attached above ad below the site of the fracture. The fragments often overlap by as much as 2.5 to 5 cm (1 to 2 inches) -When the extremity is examined with the hands, a grating sensation, called crepitus, can be felt. It is caused by the rubbing of the bone fragments against each other. -localized swelling and discoloration 23
Shortening
Crepitus
Manifested
Swelling and
Manifested
Discoloration
of the skin (ecehymosis) occurs after a fracture as a result of trauma and bleeching into the tissues. These signs may not develop for several hours after the injury. Manifested -After fracture, any subjective sensation, experienced as numbness, tingling, or a pins and needles may be felt. These often fluctuate according to such influences as posture, activity, rest, edema, congestion, or underlying disease, it is sometimes identified as acroparesthesia. -Mostly, the affected part responds with a sensation of pain to pressure or touch that would not normally cause discomfort. This happens due to the bones splintered into fragments.
Paresthesia
Tenderness
Manifested
24
IV. Nursing Interventions
1. Medical and Surgical Management Temporary skin traction, Bucks extension, may be applied to reduce muscle spasm, to immobilize the extremity, and to relieve pain. The findings of a recent study suggested that there is no benefit to the routine use of preparative skin traction for patients with hip fractures and that the use of skin traction should be based as evaluation of the individual patient. The goal of surgical treatment of hip fractures is to obtain a satisfactory fixation so that the patient can be mobilized quickly and avoid secondary medical complications. Surgical treatment consists of (1) open or closed reduction of the fracture and internal fixation (2) replacement of the femoral head with a prosthesis (hemiarthroplasty), or (3) closed reduction with pereutaneous stabilization for an intracapsular fracture. Surgical intervention is carried out as soon as possible after injury. The preoperative objective is to ensure that the patient is in as favorable a condition as possible for the surgery. Displaced femoral neck fractures may be treated as emergencies, with reduction and internal fixation performed within 12 to 24 hours after fracture. This minimizes the effects of diminished blood supply and reduces the risk for avascular necrosis. After general or spinal anesthesia, the hip fracture is reduced under x-ray visualization using an image intensifier. A stable fracture is usually fixed with nails, a nail and plate combination, multiple pins, or compression screw devices. The orthopedic surgeon determines the specific fixation device based on the fracture site or sites. Adequate reduction is important for fracture healing (the better the reduction, the better the healing). Hemiarthroplasty (replacement of the head of the femur with prosthesis) is usually reserved for fractures that cannot be satisfactorily reduced or securely nailed or o avoid complications of non-union and avascular necrosis of the head of the femur. Total hip replacement may be used in selected patients with acetabular defects.
25
2. Care Guide of Patient with the Condition (fracture of the right femoral neck) Repositioning the Patient
The nurse may turn the patient onto the effected or unaffected extremity as prescribed by the physician. The standard method involves placing a pillow between the patients legs to keep the affected leg in an abducted position. The patient is then turned onto the side white proper alignment and supported abduction are maintained.
Promoting Strengthening Exercise
The patient is encouraged to exercise as much as possible by means of the overbed trapeze. This device helps strengthening the arms and shoulders in preparation for protected ambulation (e.g., toe touch, partial weight bearing). On the first postoperative day, the patient transfers to a chair with assistance and begins assisted with ambulation. The amount of weight bearing that can be permitted depends on the stability of the fracture reduction. The physician prescribes the degree of weight bearing and the rate at which the patient can progress to full weight bearing. Physical therapists work with the patient on transfers, ambulation, and the safe use of the walker and crutches. The patient who has experienced a fractured hop can anticipate discharge to home or to an extended care facility with the use of an ambulating aid. Some modifications in the home maybe needed to permit safe use of walkers and crutches and for the patients continuing care.
Monitoring and Managing Potential Complications
Elderly people with hip fractures are particularly prone to complications that may require more vigorous treatment than the fracture. In some instances, shock proves fatal. Achievement of homeostasis after injury and surgery is accomplished through careful monitoring and collaborative management, including adjustment of therapeutic interventions as indicated.
26
Health Promotion
Osteoporosis screening of patients who have experienced hip fracture is important for prevention of future fractures. With dual-energy x-ray absorptiometry (DEXA) scan screenings the actual risk for additional fracture can be determined. Specific patient education regarding dietary requirements, lifestyle changes, and exercise to promote bone3 health is needed. Specific therapeutic interventions need to be initiated to retard additional bone loss and to build bone mineral density. Studies have shown that health care providers caring for patient with hip fractures fail to diagnose or treat these patients for osteoporosis despite the probability that hip fractures are secondary to osteoporosis. Fall prevention is also important and maybe achieved through exercises to improve muscle tone and balance and through the elimination of environmental hazards. In addition, the use of hip protectors that absorb or shunt impact forces may help to prevent an additional hip fracture if the patient were to fall.
Relieving Pain
* Secure data concerning pain - have patient describe the pain, location characteristics (dull, sharp, continuous, throbbing, boning, radiating, aching and so forth) - ask patient what causes the pain, makes the pain worse, relieves the pain, and so forth. - evaluate patient for proper body alignment, pressure from equipment (casts, traction, splints, and appliances) * Initiate activities to prevent or modify pain * Administer prescribed pharmaceuticals as indicated. Encourage use of less potent drugs as severity of discomfort diseases. * Establish a supportive relationship to assist patient to deal with discomfort. * Encourage patient to become an active participant in rehabilitative plans.
27
Promoting Self-Care Activities
* Encourage participation in care. * Arrange patient area and personal items for patient convenience to promote independence. * Modify activities to facilitate maximum independence within prescribed limits. * Allow time for patient to accomplish task. * Teach family how to assist patient while promoting independence in self-care
Promoting Physical Mobility
* Perform active and passive exercises to all nonimonobilized joints. * Encourages patient participation in frequent position changes, maintaining supports to fracture during position changes. * Minimize prolonged periods of physical inactivity, encouraging ambulation when prescribed. * Administer prescribed analogies judiciously to decrease pain associated with movement.
Promoting Positive Psychological Response to Trauma
* Monitor patient for symptoms of post from a stress disorder. * Assist patient to more through phases of post-trammatic stress (outery, denied,omtrusiveness, working through, completion). * Establish trusting therapeutic relationship with patient. * Encourages patient to express thoughts and feelings about traumatic event * Encourages patient to participate in decision making to reestablish control and overcome feelings of helplessness. * Teach relaxation techniques to decrease anxiety.
28
* Encourages development of adaptive responses and participation in support groups. * Refer patient to psychiatric liaison nurse or refer for psychotherapy, as needed.
3. Actual Patient Care
3.1 Physical Assessment PHYSIOLOGIC Palpation - Palpable temporal pulse, soft, no evidence of abnormal mass, no protrusions and pond felt upon palpation.
Body part Head
Inspection - Small, round head, normocephalic, no wounds, no rashes present.
Percussion Auscultation
Hair
-Hair is short, white in color, evenly distributed, no scales, wearing a clip, has a fine hair -No dandruff and - Free from lumps, wounds present, pink, lesions, normal bond mobile prominences on the forehead, sides of the parietal bones, behind the ears. - Firm, no scars, no visible bulges, not oily, had wrinkles - Symmetrical, check bones are slightly prominent, no presence of scar, presence of wrinkles, without pimples - Forehead is free of lumps and nodes. -Tempera; pulse is at 82 bpm.
Scalp
Forehead
Face
- No lesions, no tenderness.
29
Eyes
- Symmetrical, round, align with the ears, few discharges seen, with eyeglass - Hair evenly distributed, skin intact, symmetrically aligned, black in color, free from sealing - turn outward, short, black - partially cover the eyelids -Non tender - No lumps and rashes, smooth and no tenderness
Brows
Lashes
Lids-Upper
Lids-Lower
- sometimes cover the -Non tender whole sclerae - whitish in color but red capillaries are slightly seen - pink - transparent, shiny and smooth, night displays at the same spot of the eyes -round, black -black in color but with white opacities near the lacrimal gland , round smooth border, illuminated pupil constricts (pupil equally round reactive to light and decommodation) 30
Sclearae
Cojunction Cornea
Iris Pupil
Muscle Function
-eyes moves slowly as it follows my finger guiding the patient and assessing her 6 cardinal gazes -Move symmetrically the tremors -260/20
Muscle Balance Visual Acuity Peripheral Vision
-able to define correctly the number of fingers showed at the side of the patient nut sometimes its difficult for her. - White, long nose, septum is aligned in midline, no discharge/ flaring, air flows freely. - light color during transillumination -light color during transillumination - no lesions, open and close symmetrically and slowly. -slightly pale in color, soft, moist, symmetry of contour, smooth in texture. -Intact, pink in color, no swelling or bleeding. 31 - no lesions, deformities and deviations
Nose
Frontal Sinuses Maxillary Sinuses Mouth
- non-tender
- nontender - nontender
- non-tender
-free from edema
Lips
- no lumps, lesions and tenderness upon palpation, free from edema
Gums
Teeth
-Yellow teeth with brownish discoloration, the dentures, and teeth are incomplete. Upper- no teeth Lower- 4 -centrally positioned, slightly pale, moist, no lesions. - midline, slightly pale - pinkish, visible veins - bony, whitish - muscular, pinkish - pink, midline, free of lesions - midline, no inflammations - Symmetrical, slightly big, align with the eyes, pinna is in linewith the outer canthus of the ear, no swelling or lesions. - no pain felt, upon palpation of pinna. - no lumps - no palpable nodules
Tongue
Frenulum
Sublingual Area Hard Palate Self Palate Uvula
Tonsils
Ears
External
- Symmetrical, align -Displays no with the eyes, no thickening/ pain. No swelling or lesions, as masses/ bulges. discharges, with slight cerumen and hair.
32
Neck
- Able to do flexion, extension and rotation of neck. -Muscles equal in size, head centered. - no visible bulges, not enlarged - no bulges, not visible
-Carotid pulse palpable
Lymph nodes Thyroid
-Not palpable
-Not palpable, free of nodules, moves up and down as the patient swallows. - central placement in midline of neck, spaces are equal in both sides, nontender, non-palpable - slightly cold, good turgor
Trachea
- not enlarged - centrally located
Skin
- white, with wrinkles, no dryness
Thorax Chest anterior - flat, equal chest expansion, the ride and fall during respiratory is visible - vibrations are equal in both sides - no nodules, retraction or nodules - full, symmetric excursion - resonate down to the 6th rib, flat over areas of heavy muscle and bone, dull on areas over the heart, liver, and stomach percussed. -Lung sounds are clear, no rales and wheezes
Lungs
33
Heart
- no visible pulsations - no nodules, bulges - apical pulse palpable -with breast CA ( R) ( 2006-2007 ) - flat, soft, unblemished skin - non-tenderness
-TR= 80 bpm -no murmurs
Breast
Abdomen
- audible bowel sound of 18 from the normal range of 5-35 bowel sounds. Dull sound at upper quadrant
Spine
- has abnormal curvature -capillary refill time is 2 sec. - white, equal in sizes, fingers were curving downward -35.5 degrees Celsius - no lesions, no lumps palpated in the lungs
Extremities
Upper
- radial pulse palpable- 80 bpm - brachial pulse palpable - no tenderness, slightly cold
- biceps and triceps reflex present
- BP- 120/80 mmHg
Muscle strength Muscle tone
- able to perform ROM exercises - difficulty in overcoming resistance
34
Lower
- white, equal in size, covered with cloth, limited movement on lower extremities - capillary refill is 2 sec - difficulty in performing ROM exercises - inability to overcome resistance
- positive tenderness on the right hip
Muscle strength
Muscle tone
- slightly cold, dry to touch , with pain upon palpation
- patellar reflex not present
35
BRUNSWICK LENS MODEL
36
Needs/ Problem / Cues I. Physiologic A. Deficit 1. Impaired Physical Mobility Cues: - Difficulty in changing position while lying on bed. -Difficulty in moving the extremities. -Inability to walk or stand alone. -limited range of motion in the extremities. -Slowed movement. -Difficulty initiating gait. dili gihapon mu lihok akong tiil day as verbalized by the patient.
Nursing Diagnosis
NURSING CARE PLAN Scientific Basis ObjecNursing Action tives of Care After 8 hours of holistic nursing caring care the patient will be able to: 1. demonst rate increasi ng function of the extremit ies Measures to: 1. Promote adequate mobility of the client. - instruct the 5.0 to keep siderails up or raised. - assist patient to do active ROM exercises on the lower extremities. -Provides comfort measures such as backrub. -Encourage patient to stand or walk as tolerated using parallel bars. -Support affected body parts or joints using pillows or rolls. -administer pain reliever such as areoxia as prescribe by the physician. -Consult with physical or occupational therapist as indicated.
Rationale
Fractures occur when the bone is subjected to Impaired stress greater physical that it can mobility, absorb. When inability the bone is to stand broken, alone adjacent related to structures are skeletal also affected, impairmen resulting in soft t to facture tissue edema, of the hemorrhage into right the muscles and femoral joints, joints neck dislocations, ruptured tendons, severed nerves, and damaged blood vessels. Body organs maybe injured by the force that caused the fracture fragments. After a fracture, the extremities cannot function properly because normal functions of muscle depend on the integrity of the bones which they are attached.
-to avoid patients from falling to sudden movements -to improve muscle strength and joint mobility -in order for the patient to become more relax and comfortable -in order for the muscle to be more relax and relieves the pain
-to relieve pain and motion sickness
-to develop individual exercise or mobility program and identify appropriate adjunctive devices.
37
2. Risk for altered blow flow Risk Factor: Immobility
Risk for altered blood flow right immobilit y to fracture of the right femoral neck
The extremities cannot function properly after a fracture, thus, there is immobility because normal function of the muscle depends on the integrity of the bones to which they are attached. Immobility of a body part may possibly interrupt the circulation of blood through the circuitous network of arteries and veins
2. enhance blood circulati on
2. prevent, blood emboli -note signs of changes in respiratory rate, depth use of accessory muscles purledlip breathing; Note areas of pallor or cynosis. -auscultate breath-sounds Check if there is a decrease or adventitious breath sounds as well as fremitus -monitor ital signs and cardiac rhythm -review risk factors -reinforce need for adequate rest, while encouraging activities within clients limitation -encourage frequent position changes and DBE or coughing exercise. -administer medications as indicated.
-to assess respiratory insufficiency
-serves as a baseline data
-note for any changes -to promote prevention management of risk
-to improve circulation of blood to the body systems.
-to treat underlying conditions
38
B. Overload 3. Risk for additional injury risk factors: *Loss of skeletal integrity * skeletal impartment *Abnormal blood profile *Impaired or altered mobility
Risk for additional injury right loss of skeletal integrity to fracture of the femoral neck.
A fracture occurs when the stress placed on a bone is greater than a bone can absorb. Muscle, blood vessels, nerves, tendons, joints and other organs maybe injured when fracture occurs. This condition may result to a loss of skeletal integrity that may possibly lead to further injury as a result of environmental conditions interacting with the individuals adaptive and defensive resources.
3. to produce risk factors and protect self from injury
3. for the patients to be free from injury -ascertain knowledge of safety needs or injury -assess muscle strength gross and fine motor coordination. -observe for signs of injury -identify interventions or safety devices. -encourage participation in rehab programs, such as gait training -promote education programs geared to increasing the awareness of safety measures
-to reinforce and import knowledge to the patient -to evaluate degree or source of risk. -for early detection. -to promote individual safety. -to improve skeletal integrity.
-to promote wellness.
39
Drug/ Classification/ Dose/ Mechanism Frequency / Route * Aromasin 25 mg T tab-OD C: Antineoplastic M: Binds to estrogen receptors, has anti- estrogen receptorpositives breast cancer cell increased
DRUG THERAPEUTIC RECORD Indication/ Principles of Contraindation/ Care Side effects
Treatment
Evaluation
I. treatment of advanced breast cancer in postmenopaural women whose decreased has progressed FF. Tamoxifen therapy SE: C1: allergies, patient has not been through menopause yet, pregnancy and breastfeeding
-25mg po everyday with meals. -aoid use during premenopause or with renal or nepatic dysfunction. - (ho flashes, GI upset, anxiety, depression, and headache are common.)
* Aspirin C: (aspilet) T Antipyriene, tab OD po Analgesic, antiinflammatory, Antirheumatic , anti- platelet salicylate, NSAID M: Analgesic and antirheumatic effect are, attributable to cupirine ability to inhibit he synthesis of prostaglandins
I. mild to moderate pain fever Inflammatory conditions Rheumatic fever rheumatoid arthritis, osteoarthritis CI: Allerge use continuously with impaired renal function, chicken pox, influenza SE: Acute aspirin toxicity: hyperpnea , tachypnea, hemorrhage
-give drug with food or after meals if GI upset occurs. -give drug with fullglass of H2O to reduce risk or tablet or capsule lodging in the esophagus - do not crush and ensure that patient does not chew SR preparation -Do not use aspirin that has a strong vinegar
-provide rest periods -mpnitor for any side effects that may occur -provide a quite and comfortable environment -maintain clients general well-being and hygiene -provide safety and comfort measures to the client. -elevate the leg of the patient. -assist client in doing ROM exercises -provide comfort measures such as back rub. -provide rest periods -do not allow client to do strenuous activities
-growth of tumor cells were inhabit
-there is al improvemen t of patients gout ant the patient was able to slight move her extremities
40
, important mediators of inflammation antipyretic effects are not fully understood but aspirin probably acts in the thermoregulat ory center of the hypothalamus to block effects of endogenous purogen by inhibiting synthesis of the prostaglandin intermediately . Inhibition of platelet aggregation is attributable to the inhibition of platelet synthesis of thromboxane A21 a potent vasoconstricto r and inducer of platelet aggregation. This effects occurs at low doses and last for the life of the platelet(8 days) These doses inhibit the synthesis of
Aspirin intolerance: -shinitis exacerbation of broncho spasm -nausea, dyspnea, occult blood loss, dizziness tinnitus
like odor -take extra precautions to keep this drug out of the reach of children
41
*Clexane 0-4 cc SQ OD
prostaglandin, a patient vasodilator and inhibitor of platelet aggregation. C: lowmolecular weight heparin antithrombotic M: lowmolecular weight heparin that inhibits thrombus and clot formation by checking factor XA, factor II a, preventing the formation of clots.
I. prevention of deep vein thrombosis, which may lead to pulmonary embolism following hip replacement. Prevention of ischemic complications. CI: hypersensitivity use cautiously with pregnancy or lactation history of GI blood, spinal top SE: Bruishing, thrombocytopenia , chills, fever, pain, local irritation.
*lericoxib (arcoxta) 90mg T tab OD
C: nonsteroidal anti inflammatory drug (NSAID) M: work DY blocking the action of a substance in the body called cyclooxygenare is
I. Acute and chronic treatment of asteoarthritis and RA CI: Children and adolescent under 16 yrs. Of age -severely to liver function SE: headache, dizziness
-give deep subcutaneous injections, Do not give clexane by IM injection -patient should be lying down. Activities between the left and right anterolateral and posterolateral abdomen wall -apply pressure to all injection sites after needle is withdrawn -do not mix with other injections or infusions -store at room temperature fluid should be clear, colorless to pale yellow -can be taken with or without food, but may start to work quicker if taken without food. -do not exceed the prescribed dose -maybe taken with low dose
-provide for safety measures (electric razor, soft toothbrush) to prevent injury to patient, who is at risk of bleeding -check patient for signs of bleeding. Monitor blood test -provide a safety and comfortable environment -provide rest periods -avoid patient from dying strenuous activities -position client in a comfortable position. -divert patients attention -guide imagery -encourage
-further complicatio ns were prevented.
-there is an improvemen t of patients gait and the patient was able to slightly move her extremities
42
* vitamin B complex (sangubio n) T tab OD
involved on producing prostaglandins in response to injury or certain diseases. There prostaglandins , cause pain or swelling and inflammation. Because NSAIDS block the production of prostaglandins they are effective at relieving pain and inflammation C: Phospholipid + multivitamins M: mainly function as eatalysts for reactions within the body. They contain no useful energy, but as catalysts, they serve as essential link and regulators in metabolic reaction that release energy from food. Control the processes of
Constipation, nausea, vomiting, indigestion, flatulence
(76 mg daily) aspirin. However the combination may carry an increased risk of ulceration or bleeding in the stomach or intestine -it is important to tell your doctor or pharmacist what medicine you are already taking including those bought with out prescription and herbal medicine -maybe taken with meals if GI discomforts occurs. -best to take after meals. -initially 1 capsule every 8 hours. Follow up treatment 1 capsule daily
DBE -hot compress is applied to the affected site or area. -provide rest periods -avoid client to perform strenuous activities -provide a safety environment
I. treatment of chronic liver disease , liver cirrhosis and fatty liver. For liver protection eases of intoxication (alcohol abuse) CI: hypersensitivity, lactation SE: sedation, dizziness, dry mouth, nausea, constipation
-encourage client to eat foods rich in vitamins and minerals -instruct client to minimize the intake of fatly foods -lifestyle modificatio n -exercise regularly -impart to patient the importance of taking adequate amount of nutritious
-the patient was able to gain more energy and increase its function
43
*CaCo3 (Calvit) T tab OD every 6pm
*Ketoprof en (fortum) Gel apply to right
tissue synthesis and aid in protecting the integrity of the cells plasma membrane; assist growth, maintenance of health metabolism C: electrolyte Antacid M: Essential element of the body; helps maintain the functional integrity if nervous and muscular system,; helps maintain cardiac function, blood coagulation: is an enzyme cofactor and affects the secretom activity of endocrine and exocrine glands; neutralizes or reduces gastric acidity. C: NSAID Non-opioid analgesics M: Antiinflammatory
foods
I: Dietary supplement when calcium intake is in adequate, treatment of calcium deficiency, prevention of hypocalcemia during exchange transfusions. CI: Allergy, use cautiously withdrawal; dysfunction pregnancy, lactation. Se: Slowed heart rate, tingling, heat waves, local irritation, hypercalcemia, and pain dry mouth.
- do not administer oral drugs within 12 hour of antacid administration. - report loss of appetite, nausea, vomiting, abdominal pain, constipation, dry mouth, thirst, increase voiding.
- encourage client to eat foods rich in calcium such as milk, cheese. - assist client be expose to sunlight for 5-15 minutes. - impart [atient the importamce of takiln adequate amount of nutritious foods. - encourage client to exercise regularly.
- the strength of patients bones were improved as evidenced by standing or walking with assistance.
I: Acute and long treatment of RA and osteoarthritis. - relief of mild to moderate pain.
For over-thecounter Use: Do not take for more than 10 days. If
- elevate the leg of the patient - provide rest periods
- there was an improvemen t of patients gait and the
44
thigh and right knee twice a day.
and analgesic activity, inhibits prostaglandin and has antibradykinin and lysosomal or membrane stabilizing actions.
*Dibencos ide (heraclene ) Mg tav T tab HD
C: Appetite stimulants M: Improes appetite and preents faulty nutrition and other chronic ailments.
CI: Significant renal impairment, pregnancy, lactation allergy to ketoprofen, use cautiously the impaired hearing allergies hepatic, CV and GI conditions. SE: Headache, dizziness, rash, pruritus, nausea, dyspepsia, dysuria, renal impairment, dyspnea, peripheral edema. I: Poor appetite in adult, adjuvant to the treatment of TB, and other chronic ailments, convalescence from acute infection: CI: Hypersensitivity
symptoms persist contact your HC provider.
- provide comfort measures - encourage client to do DBE - promote a quite, relaxing and comfortable environment .
patient was able to slightly move her extremities.
- the dosage must be reduced to patients with liver damage. - liver functions should be assessed before and regularly during treatment. - should be used with caution in patients with diabetes mellitus as their management may become more difficult.
*Calmose ptine ointment appky to affected
C: Topical antivirals M: Protects, soothes and helps promote
I: Wound drainage, urinary and fecal incontinence, bedsores, ileo
- cleanse skin, pat dry and apply once daily or as necessary
- provide small frequent feelings - offer foods that are attractive or presentable enough to stimulate appetite. - instruct patient to eat adequate nutritious foods. - impart to patient the importance of taking adequate nutritious foods. - maintain general well-being and hygiene of the
- the patient was able to improve her appetite as evidenced by eating her meals an time and avoiding to skip meals.
- patients wound was easily healed and bedsores
45
site BID
healing in those with impaired skin integrity.
anal, reservoirs, moistures of perspirations CI: Hypersensitivity
*Acarbose (glucobay) 50 mg tab TID with meals
C: Antidiabetic M: Alphaglucosidase inhibitorobtained from the fermentation process of a microorganis m; delays the digestion of ingested carbohydrates heading to a smaller increase in blood glucose following meals and in glycosylated
I: Adjunct to diet to lower blood glucose in those patients with tipe2 (non-insulin dependent) DM whose hypercalcemia cannot be managed alone. CI: Hypersensitivity, use cautiously with renal impairment pregnancy and lactation. SE: Hypoglycemia, abdominal pain, flatulence,
- do not use this medication if you are allergic to zinc, dime thicone, lanolin, cod liver oil, petroleum, jelly, parabens, mineral oil or wax. - call your doctor if you have any signs of redness and warmth or oozing skin lesions. - avoid getting this medication in your mouth or eyes. If it does rinse with water right away. - give drug TID with the first bite of each meal. - monitor serum glucose level frequently to determine drug effectiveness and dosage. - inform patient of likelihood of abdominal pain and flatulence. - do not discontinue this drug without consultation from health care provider.
patients. were - provide a prevented. clean and comfortable environment . - meticulous skin care - promote proper environment al sanitation.
- impart to patient to eat a nondiabetic diet. - consult with a dietician to establish weight loss program and dietary control. - encourage client to do regular exercise assisted by the SO. - impart to client the
- further complicatio ns were being prevented and appearance of signs and symptoms slowly diminished
46
*Ranitidin e (ulcin) 75 mg tab PC 3x a day 6 am 6 pm
hemoglobin, does not enhance insulin secretion, so its effects are addictive to those of the sulfonyl areas, in controlling blood glucose. C: Histanine, antagonists M: Competitively inhibits the action of histamine At h2 receptors of the parietal cells of the stomach inhibiting basal gastric acid secretion that is stimulated by food, insulin, histamine, cholinergic agonists, gastrin and pentagastrin.
leucopenia, anemia, thrombocytopenia .
importance of taking nutritious foods. - avoid the client from eating foods rich in fats and cholesterol. - administered oral drug with meals and hours. - decrease doses in renal and liver failure. - if you are using antacid, take it exactly as prescribed, being careful of the time administered. - have regular medical follow up care to evaluate your response. - provide rest periods - encourage client to ear adequate nutritious foods at a regular meal time. - impart to client not to skip meals. - position client into a comfortable position. - the patient was able to feel more comfortable as evidenced resting and sleeping comfortably .
I: Short term treatment of active duodenal ulcer, treatment of heart burn, acid ingestion, sour stomach. CI: Hypersensitivity, use cautiously the impaired renal or hepatic function pregnancy. SE: Headache, malaise, dizziness, tachycardia, bradycardia, rash, constipation, diarrhea.
47
3.5 SOAPIE
SOAPIE #1 S- Dili gehapon ayu malihuk akong tiil day.
O- Received patient lying on bed with head elevated to 30 degrees, awake, conscious, coherent, communicative, without IV, with the following v/s T= 35.5 degree Celsius, P= 86 pm, R= 20 bpm and BP= 120/70 mmHg, the patient is reading a newspaper, has difficulty in changing position while lying on bed, has difficulty in moving the extremities, inability to walk or stand alone, limited range of motion in the extremities, slowed movement, difficulty initiating in gait.
A= Impaired physical mobility, inability to stand alone related to skeletal impairment 2 degrees to fracture on the right femoral neck.
P= To promote adequate mobility of the client.
I= Introduced name to the patient; assessed the condition, of the patient; monitored v/s, assisted patient in doing ROM exercises, assisted patient upon doing gait training; set siderails up; provided comfort measures such as backrub; encouraged patient to do DBE; supported affected body parts/ joints using pillows/ rolls; consulted with physical or occupational therapist as indicated; documented the v/s and I and O of the patient.
E= The patient was able to demonstrate increasing function of the extremities as evidenced by standing and walking between parallel bars with assistance.
48
SOAPIE #2 S= Naproblema man ko sa akong tiil day kay pila na ni ka adlaw walay lihok- lihok, murag lain na kaayu akong feeling, as verbalized by the patient.
O= Received patient sitting up on bed, , conscious, coherent, communicative, without IV, with the following v/s T= 35.7 degrees Celsius, R= 19 bpm, P= 76 bpm, BP= 120/70 with feet supported by rolled towels, limited movement of the lower extremities.
A= Risk for altered blood flow r/t immobility 2 degrees to fracture of the right femoral neck.
P= To enhance blood circulation
I= Introduced name to the patient; assessed the condition of the patient; monitored v/s; administered medications; noted signs of changes in respiratory rate, depth, use of accessory muscles, pursed top breathing, areas or pallor/ cyanosis; auscultated breath sounds if there is a decrease or adventitious breath sounds as well as fremitus; monitored
cardiac rhythm; reviewed risk factors; reinforced need for adequate rest while encouraging activity within clients limitations; encouraged frequent position changes and DBE / coughing exercises; check the CRT of the patient; documented the v/s, I and O and medications taken by the patient. E= The clients extremities are warm and pink, remains intact, CRT results of 2 seconds, no verbalization of pain, swelling on the area and demonstrates calm breathing.
49
Objective General Objectives: After 3 day of varied learning activities, the patient as well as the significant others or family will be able to acquire knowledge, attitude and skills in preventing complications of immobility. Specific Objectives: After 45 minutes of teaching, the patients as well as the significant other or family will be able to: 1. explain the goals of frequent position changes.
HEALTH TEACHING PLAN Content Methodology
Evaluation
Positioning (Goals) * to prevent contractures * stimulate circulation and prevent pressure sores * prevent thrombophiebitis and pulmonary embolism. * promote lung expansion and prevent pneumonia * decrease edema of the extremities * changing position from lying to sitting several times a day can help prevent changes in the CVS known as deconditioning. *the recommendation is to change body position at least every 2 hours, and preferably more frequently in patients who have no spontaneous movement.
Informal discussion
-the patients was able to explain the goal of frequent position changes and she was motivated to perform the different positions to become at ease from pain or any discomfort felt
50
2. enumerate the positions for proper body alignment
Proper Body Alignment 1. Dorsal or Supine Position. a. the head is in line with the spine both laterally and anteroposteriority. b. the trunk is positioned so traction of the hips is minimized to prevent hip contractive. c. The Arms are flexed at the elbow with the hands resting against the lateral abdomen. d. the legs are extended in a neutral position with the toes pointed towards the ceiling. e. the neels are suspended in a space between the mattress and the footboard to prevent neel pressure. f. trochanter tons are place under the greater trochanter in the hip joint areas. 2. Side lying or lateral position a. the head is in line with the spine b. the body is an alignment and is not twisted c. the uppermost hip joint silently forward and supported by a pillow in a position of slight abduction. d. a pillow supports the arm which is flexed of both the elbow and shoulder joints. 3. Prone position a. the head is turned laterally and is in alignment with the rest of the body b. the arms are abducted and externally rotated at the shoulder joint; the elbow are fexed
Informal discussion
-the patient was able to verbalize the different proper positions for proper body alignment
51
c. a small flat support is placed under the pelvis extending from the level of the umbilicus to the upper third of the thigh. d. the lower extremities remain in a neutral position. 3. discuss the different therapeutic exercises Therapeutic Exercises 1. Positive range of motion exercise 2. active assistive range of motion 3. active range of motion 4. Resistive exercise 5. Isometric or muscle settings exercise. Range of motion * Flexion extension of shoulder. * Fexion extension of elbow * adduction-abduction of shoulder. * Pronation-supination of elbow. * Dorsiflexion and palmar flexion of wrist. * Ulnar-radial deviation of wrist. * Adduction-abduction and opposition of thumb * Adduction-abduction, flexion-hyper extension of fingers. *Dorsiflexion-Plantarflexion, Eversion of the ankle. * Flexion-extension; adduction-abduction of toes * Adduction-abuction; internal rotation or external rotation of the hip. * Flexion-hyperextension; rotation of cervical spine Informal discussion and demonstration -the patient was able to discuss the different therapeutic exercises and was able to demonstrate them with assistance
4. practice the different kinds of range of motion
Informal discussion and demonstration
The patient was able to practice the different kinds of ROM exercise with assistance
52
* Lateral bending of cervical spine. 5. participate attentively to the discussion Informal discussion and demonstration -the patient was able to listen attentively and asked some question related to the discussion and she was also able to participate during demonstration.
53
V. Evaluation and Recommendation
Prognosis of the patient
After 3 days of intervention, the student nurse observed certain changes from the patient. The patient reports decreased pain with elevation, ice and analgesic. The patient also exhibits unlabored respirations; alert and oriented, a febrile, using affected extremity for light activity as allowed, no signs of neurovascular compromise, v/s stable; urine output adequate and no calf pain reported: Homans sign negative. The patient also performs active ROM correctly, hygiene and dressing practices with minimal assistance and denies acute symptoms of stress; reports working through feelings about trauma.
Recommendation
As a researcher in this case study, the student nurse recommends the patient to adjust in usual lifestyle and responsibilities to accommodate limitations imposed by fracture and to prevent recurrent fractures safety considerations, avoidance of fatigue and proper footwear. The patient is instructed about exercises to strengthening upper extremity muscles If crutch walking is planned, methods of safe ambulation walker, crutches, care, emphasizes instructions concerning amount of weight bearing that will be permitted on fractured extremity, teaches symptoms needing attention, such as numbness, decreased function, increased pain and elevated temperature and explains basis for fracture treatment and need for patient participation in therapeutic regimen. The patient and the family were also informed that the patient must have an adequate balanced diet to promote bone and soft tissue healing.
54
VI. Evaluation and Implication of this case study to:
Nursing Practice
The result of this case study would provide the student nurse with sufficient knowledge, attitude and skills towards the management of patients with fracture on the right femoral neck. This study would help the student nurse in providing a higher quality of care of patients with the same condition. It is important that the proper and ideal managements and interventions are done in order to give a more holistic approach and optimum care to clients with fracture on the right femoral neck. This would ensure the timely healing of injury and the prevention of complications.
Nursing Education
Education can promote enhancement of professionalism through an on- going learning process, whether self- motivated, people- oriented and having a commitment to the organization, nurses are likely to become well respected through the formal
educational programs. Through this case study, it is important to know all areas of patient are both knowledge and skills to manage effectively in all aspects of their professional nursing practice.
Nursing Research
Nursing research is essential for the development of scientific knowledge that enables nurses to provide evidenced-based health care. Broadly nursing is accountable to society for providing quality, cost effective care and for seeking ways to improve that care. More specifically, nurses are accountable to their patients to promote a maximum level of health. This case study would contribute more information and facts about fracture on the right femoral neck. This could contribute to the development of the case study of fracture its prevention, causes, signs and symptoms, and nursing management. Hopefully, this 55
case study will lead to development of new skills and new approaches to the care of patients with fracture on the right femoral neck. This case study could also as basis for related study and will provide facts for further research in aiming for the improvement of these patients. VII Referral and Follow-Up
The patient was informed to have a continuous appointment with the Rehabilitation Care Program Health Care providers after discharge. The patient was encouraged for follow-up medical supervision to monitor for union problems. VIII Bibliography
Bare, Brenda I. and Smeltzer, Suzzane C., Textbook of Medical-Surgical Nursing. 10th Edition Philadelphia: I.B Lippincott Company. 2004. Nettina, Sandra M., Manual of nursing Practice. 7th Edtion. I.B. Lippincott Company. 2001. Rozler, Barbara et al. Fundamentals of Nursing. 5th Edition. Newyork: AddisonWeatleylongman, Incorporated. 1998. Marleb, Elaine N. Essential of Human Anatomy and Physiology. 7th Edition. Singapore. Pearson Education South Asia Pte. Ltd. 2004. Potter, Patricia and Perry, Anne. Fundamentals of Nursing. 6th Edition Baltimore: C.V. Mosby and Company. 2005. Doenges, M., Moorhouse, M.F. , Geissler Murr, A. Nurses Pocket Guide, Diagnosis, interventions and rationales, 9th Edition (2004).
56
Doenges, M., Moorhouse, M.F. , Geissler Murr, A., Nursing Care Plans. Guidelines for Individualizing Patient Care. 6th Edition. F.A. Davis Company, 2002.
57
58
Vous aimerez peut-être aussi
- Chicken and Rice: IngredientsDocument1 pageChicken and Rice: IngredientsVanessa SantosPas encore d'évaluation
- Critical Care Calculations Study GuideDocument6 pagesCritical Care Calculations Study GuideAja Blue100% (2)
- Y Study CalculusDocument5 pagesY Study CalculusVanessa SantosPas encore d'évaluation
- Ps Calc GuideDocument30 pagesPs Calc GuideMzee321Pas encore d'évaluation
- Chicken Mole EnchiladasDocument2 pagesChicken Mole EnchiladasVanessa SantosPas encore d'évaluation
- Asian Recipes - Dessert Delights (With I - Ho, CharlesDocument154 pagesAsian Recipes - Dessert Delights (With I - Ho, CharlesVanessa Santos100% (4)
- Personality Drawing TestDocument1 pagePersonality Drawing TestVanessa SantosPas encore d'évaluation
- A Spark of ExistenceDocument16 pagesA Spark of ExistenceVanessa SantosPas encore d'évaluation
- Philippine Constitution PDFDocument53 pagesPhilippine Constitution PDFVanessa SantosPas encore d'évaluation
- Common Communicable DiseasesDocument213 pagesCommon Communicable Diseasesɹǝʍdןnos100% (24)
- Vs Circumference X 3.5Document1 pageVs Circumference X 3.5Vanessa SantosPas encore d'évaluation
- Personality Drawing TestDocument1 pagePersonality Drawing TestVanessa SantosPas encore d'évaluation
- Copar Final3Document4 pagesCopar Final3Vanessa SantosPas encore d'évaluation
- Republic Act No 9173Document5 pagesRepublic Act No 9173Vanessa SantosPas encore d'évaluation
- 40 Items Comprehensive NCLEX ReviewDocument20 pages40 Items Comprehensive NCLEX Reviewclumsy16Pas encore d'évaluation
- Characteristics of Greek LiteratureDocument2 pagesCharacteristics of Greek LiteratureVanessa Santos100% (2)
- The CourtDocument6 pagesThe CourtVanessa SantosPas encore d'évaluation
- IMCIDocument57 pagesIMCIwyndzPas encore d'évaluation
- Stone LowOxalateDiet PDFDocument7 pagesStone LowOxalateDiet PDFVanessa Santos0% (1)
- Acute Abdominal Pain and Acute AppendicitisDocument8 pagesAcute Abdominal Pain and Acute AppendicitisdrtpkPas encore d'évaluation
- Shock Case Presentation: General DataDocument1 pageShock Case Presentation: General DataVanessa SantosPas encore d'évaluation
- Spinal Disc HerniationDocument12 pagesSpinal Disc HerniationVanessa SantosPas encore d'évaluation
- LymphomaDocument15 pagesLymphomaVanessa SantosPas encore d'évaluation
- GreekDocument7 pagesGreekVanessa SantosPas encore d'évaluation
- AgingDocument9 pagesAgingVanessa SantosPas encore d'évaluation
- 1º Energy FailureDocument1 page1º Energy FailureVanessa SantosPas encore d'évaluation
- Adrenergic ReceptorsDocument6 pagesAdrenergic ReceptorsVanessa SantosPas encore d'évaluation
- IMCIDocument57 pagesIMCIwyndzPas encore d'évaluation
- CDPDocument9 pagesCDPVanessa SantosPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Orthopedic Study Guide 2018Document9 pagesOrthopedic Study Guide 2018Alif AllahPas encore d'évaluation
- 1885 2Document73 pages1885 2JuhiJahan AmanullahPas encore d'évaluation
- Metabolic Bone ConditionsDocument66 pagesMetabolic Bone ConditionsNaeem AminPas encore d'évaluation
- Women's Health Physiotherapy (Pelvic Health)Document24 pagesWomen's Health Physiotherapy (Pelvic Health)syed imran100% (1)
- Diseases of Bones and JointsDocument2 pagesDiseases of Bones and JointsAnna FalcoPas encore d'évaluation
- OsteoporosisDocument16 pagesOsteoporosisldw627Pas encore d'évaluation
- Persuasive Outline Speech FormatDocument4 pagesPersuasive Outline Speech FormatoboroPas encore d'évaluation
- A Decade of Bisphosphonate Bone Complications: What It Has Taught Us About Bone PhysiologyDocument12 pagesA Decade of Bisphosphonate Bone Complications: What It Has Taught Us About Bone PhysiologyNatalia Camila Rodríguez LatorrePas encore d'évaluation
- OsteoprosisDocument25 pagesOsteoprosisForat ObaidPas encore d'évaluation
- NSE121 - Care PlanDocument7 pagesNSE121 - Care Planramyharoon2004Pas encore d'évaluation
- Archives of Osteoporosis, 2021, 16, 102 - The Indian Society For Bone and Mineral Research (ISBMR) Position Statement For The DiagnosisDocument13 pagesArchives of Osteoporosis, 2021, 16, 102 - The Indian Society For Bone and Mineral Research (ISBMR) Position Statement For The DiagnosisBHUENDOCRINE SRPas encore d'évaluation
- SpondyloarthritisDocument77 pagesSpondyloarthritisRapid MedicinePas encore d'évaluation
- Vitamins D3 and K2 Another Dynamic Duo by DR EcclesDocument12 pagesVitamins D3 and K2 Another Dynamic Duo by DR Ecclesgeorgeta.dumitru1987Pas encore d'évaluation
- FMcase 1Document24 pagesFMcase 1Ryan Townsend100% (2)
- Young Old Middle-Old Old-Old (Ages Elite OldDocument5 pagesYoung Old Middle-Old Old-Old (Ages Elite OldReignlyPas encore d'évaluation
- Vitamin D EbookDocument26 pagesVitamin D EbookBelinda100% (3)
- Strength Training For WomenDocument232 pagesStrength Training For WomenGanescu Vlad100% (3)
- Comprehensive Geriatric Assessment: by Dr. Zinab AlatawiDocument37 pagesComprehensive Geriatric Assessment: by Dr. Zinab AlatawiOne life To live SaudiahPas encore d'évaluation
- Hydrocortisone (Systemic) - Drug InformationDocument13 pagesHydrocortisone (Systemic) - Drug InformationjjjkkPas encore d'évaluation
- Osteoprosis Presentation 2Document38 pagesOsteoprosis Presentation 2Shaz RizwanPas encore d'évaluation
- Passmedicine MRCP Notes-RheumatologyDocument84 pagesPassmedicine MRCP Notes-RheumatologyHashim Ahmad50% (2)
- Agriculture Essay TopicsDocument8 pagesAgriculture Essay Topicsertzyzbaf100% (2)
- Medicographia 86Document95 pagesMedicographia 86brave_ftPas encore d'évaluation
- Osteoporosis MergedDocument73 pagesOsteoporosis MergedrlpmanglicmotPas encore d'évaluation
- WP-00068 HistoryDXADocument4 pagesWP-00068 HistoryDXASehbaz SinghPas encore d'évaluation
- Crohn's Disease NutritionDocument8 pagesCrohn's Disease NutritionWin van OosterwijckPas encore d'évaluation
- Metabolisme Calsium Dan Hormon PTHDocument71 pagesMetabolisme Calsium Dan Hormon PTHzeddPas encore d'évaluation
- Simple Exercises To Prevent OsteoporosisDocument10 pagesSimple Exercises To Prevent OsteoporosisrasikaaPas encore d'évaluation
- Osteoporosis Edited 100201092008 Phpapp02Document32 pagesOsteoporosis Edited 100201092008 Phpapp02Maya SwariPas encore d'évaluation