Académique Documents
Professionnel Documents
Culture Documents
Hemostasis
Transféré par
kep1313Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hemostasis
Transféré par
kep1313Droits d'auteur :
Formats disponibles
Hemostasis and thrombosis Normal hemostasis is a consequence of a tightly regulated processed that maintain blood in a fluid state in normal
l vessels Permit rapid formation of hemostasis clot at the site of a vascular injury Pathological counter part of hemostasis - thrombosis involves blood clot (thrombus_ formation within intact vessels 3 components o Vascular wall (endothelium) o Platelets o Coagulation cascade NORMAL HEMOSTASIS 1. Endothelial injury expose high thrombogenic subendothelial extracellular matrix which facilitates PLATELET ADHERENCE AND ACTIVATION a. Activation of platelets results in dramatic shape change (disc to flat plans with increased surface area) and release secretory granules b. Secreted product recruit additional platelets (AGGREGATION) to form hemostatic plug c. Formation of platelet plug = primary hemostasis 2. Tissue factor exposed at the site of injury (factor III and thromboplastin) a. TF membrane bound procoagulant glycoprotein made by endothelial cells b. Acts with factor 7 as major in vivo initiator of the coagulation cascade, eventually becoming thrombin c. Thrombin cleaves circulating fibrinogen into fibrin creates fibrin meshwork and induces additional recruitment and activation d. Secondary hemostasis formation of fibrin plug 3. Polymerized fibrin and platelet aggregate form a solid permanent plug to prevent any hemorrhage a. Counter regulatory mechanisms (like tissue plasminogen activator t-PA) set into motion to limit the hemostasis to site of injury
I.
II.
Endothelium key players in the regulation of hemostasis balance between anti and prothrombotic activities determines whether thrombus formation, propagation or dissolution occurs, A. ANTITHROMBOTIC PROPERTIES normally exhibit antiplatelet, anticoagulant and fibrinolytic properties actively prevent thrombosis 1. Antiplatelet effects: prevents platelets and plasma coagulation factors from engaging subendothelial ECM a. Nonactivated platelets dont adhere b. Prostacyclin and NO impede platelet adhesion (vasodilators and inhibitors of platelet aggregation c. Degrade ADP and further inhibit platelet aggregation 2. Anticoagulant effects: mediated by a. Membrane associated heparin like molecules- act indirectly and are cofactors that greatly enhance inactivation of thrombin and anti Thrombin III b. Thrombomodulin binds to thrombin and converts it into an anticoagulant via ability to activate protein C inhibits clotting inactivators factors 5a and 7a i. Also protein S (cofactor for protein C) c. TF pathway inhibitor (TFPI) cells surface protein that direct inhibits TF, factor 7a, and 10a 3. Fibrinolytic effects: make tissue type plasminogen activator (t-PA) protease that cleaves plasminogen to form plasmin, plasmin cleaves fibrin to degrade thrombus B. Prothrombotic properties after injury or activation by infection agents, hemodynamic forces plasma mediator and cytokines procoagulant activities 1. Platelet effects injury allows platelets to contact ECM adhesion occurs through interaction with vWF a. Glycoprotein vWF adhesion bridge between sub endothelial collagen and Gp1 platelet receptor b. Adhesion fibrinogen connects GpIIb-IIIa receptors on different platelets c. ADP incudes conformational change 2. Procoagulant effects in response to cytokines (TNF or IL1) or bacterial endotoxin, endothelial cell make TF, the major activator of the extrinsic clotting cascade a. Increase the catalytic function of activated factors 9a and 10a 3. Anti fibrinolytic effects- endothelial cells secrete inhibitors of plasminogen activator (PAIs)_ which limit fibrinolysis to favor thrombosis Platelets A. Description 1. Disc shaped anucleate cell fragments that are shed from megakaryocytes I BM in blood stream 2. From primary hemostatic plug that initially seals vascular defects and provides a surface that recruits and concentrates activated CF 3. Contain a. Glycoprotein receptors b. Contractile skeleton c. 2 types of cytoplasmic granules i. Alpha granules have adhesion molecule P-selectin on membrane Contain fibrinogen, fibronectin, factors 5 and 8, platelet factor 4, PDGF and TGF beta ii. Dense (delta) granules
III.
Contain ADP/ATP, calcium, histamine, serotonin and epinephrine B. Encounter ECM constituents like collagen and vWF and contact them to under go 1. Adhesion and shape change a. Platelet adhesion to ECM mediated by interactions by vWF which connects Gp1b (platelet surface receptor) and exposed collagen b. WWF-Gp1b bond necessary to overcome high shear forces of flowing blood c. Genetic deficiencies: vWF (vWF disease) and receptor (Bernard-Soldier syndrome) result in bleeding disorder 2. Secretion (release reaction) of both granules occurs after adhesion a. Initiate intracellular protein phosphorylation cascade leading to degranulation b. Release of dense bodies important since calcium is required in coagulation cascade and ADP is potent activator of platelet aggregation i. ADP also makes ADP release, amplifying process ii. Activation negatively charged phospholipids (phosphatidyserine) on their surface Bind calcium and are nucleation site to assemble the complexes containing coagulation factors 3. Aggregation follows adhesion and granule release a. Thromboxane A2 (TxA2) amplifies platelet aggregation which lead to formation of primary hemostatic plug b. Platelet aggregation is reversible, but it activates the coagulation cascade which generates thrombin c. Thrombin stabilizes platelet plug 2 ways i. Binds to protease activated receptor on platelet membrane and causes further platelet aggregation ii. Followed by platelet contraction dependent on platelet cytoskeleton that creates an irreversible fused mass of platelets which makes up the secondary hemostatic plug iii. Thrombin converts fibrinogen to fibrin which cements platelets in place 4. Platelet activation by ADP triggers conformational change in platelet GpIIb-IIIa receptors that induces binding to fibrinogen which forms interactions between platelets C. Platelet endothelial cell interactions 1. Prostacyclin (PGI2) from endothelial cells inhibits platelet aggregation and is vasodilator 2. TxA2 is platelet aggregation and vasoconstrictor 3. At baseline, platelet aggregation is prevented 4. Endothelial damage promotes hemostatic plug formation 5. Aspirin blocks platelet TxA2 synthesis a. PGI2 production inhibited by aspirin, endothelial cells can resynthesize active cyooxyfenase and overcome blockage 6. Like PGi2, NO acts a vasodilator and inhibits platelet aggregation Coagulation cascade A. Description 1. Thrombin ascts at numerous points 2. Each rxn depends on assmelyof ac omplex composed of enzyme, a substrate (proenzyme of next coagulation factor in series) and a cofactor
3. Assembled on pholipid suface and held together by interactions that depend on calcium ions 4. Divided into extrinsic and intriskc and converge at facor X B. Tests 1. Prothrombin time (PT) secreeens for aciivity of the proteins in extrinsisc (7, 10, 2 v and friobrnogen) a. Phsospholipids plus TF to pateints citrated plasma, and calcium and measure the time ti takes for fibrin clot to form b. Factor 7 its vitamin k dpeende coagulation factor w/ shortest time 2. Partilal thromboplast time (PTT) screens fro activity in the intrinsic pathways (factors 12, 11, 9, 8, 1, 2, 5,10) a. Phospholipids plus factor 12 to patients plasma, then Ca and measure the time for clot formation (28-35 seconds0 i. Sensitive to heparin Initiation stage: TF located in the vessel wall from ma monocyte or endotheial cell binds factor 7, which ciruculates in plasama TF-F7a complex cleaves small amounts of both factor 9 and factor 10 Thrombin cleaves factor 8 and 5 to being proprgtaion stage Propgoagtion stage Factors 9 and factor 8 convert 10 to 10a Factor 10a complexds with 5a Compellx vonvert prothrombin to thrombin Essential cofactors are cealciumand phospholipids Thrboming is essential release of factor 8 from vWF and activation aof faa
. B. Platelets bind via glycoprotein Ib (GpIb) receptors to von Willebrand factor (vWF) on exposed extracellular matrix (ECM) and are activated, undergoing a shape change and granule release. Released adenosine diphosphate (ADP) and thromboxane A 2 (TxA 2) induce additional platelet aggregation through platelet GpIIbIIIa receptor binding to fibrinogen, and form the primary hemostatic plug.
C. Local activation of the coagulation cascade (involving tissue factor and platelet phospholipids) results in fibrin polymerization, cementing the platelets into a definitive secondary hemostatic plug.
D, Counter-regulatory mechanisms, mediated by tissue plasminogen activator (t-PA, a fibrinolytic product) and thrombomodulin, confine the hemostatic process to the site of injury.
NORMAL HEMOSTASIS
BLEEDING DISORDERS: Can result from 1. Increased fragility of vessels
2. Platelet deficiency or dysfunction 3. Derangement of coagulation
FIGURE 4-8 Coagulation cascade. Factor IX can be activated either by factor XIa or factor VIIa; in lab tests, activation is predominantly dependent on factor XIa of the intrinsic pathway. Factors in red boxes represent inactive molecules; activated factors are indicated with a lower case a and a green box. Note also the multiple points where thrombin (factor IIa; light blue boxes) contributes to coagulation through positive feedback loops. The red Xs denotes points of action of tissue factor pathway inhibitor (TFPI), which inhibits the activation of factors X and IX by factor VIIa. PL, phospholipid; HMWK, high-molecular-weight kininogen.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Case Studies 10Document5 pagesCase Studies 10kep1313Pas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Case Studies 8Document7 pagesCase Studies 8kep1313Pas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Case Studies 2Document4 pagesCase Studies 2kep1313Pas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- SeizuresDocument3 pagesSeizureskep1313Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Case Studies 5Document4 pagesCase Studies 5kep1313Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Virology 1 3Document5 pagesVirology 1 3kep1313Pas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Case Studies 6Document8 pagesCase Studies 6kep1313Pas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Case Studies 9Document7 pagesCase Studies 9kep1313Pas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Case Studies 7Document6 pagesCase Studies 7kep1313Pas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- Case Studies 4Document4 pagesCase Studies 4kep1313Pas encore d'évaluation
- Case Studies 1Document11 pagesCase Studies 1kep1313Pas encore d'évaluation
- Case Studies 3Document4 pagesCase Studies 3kep1313Pas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313Pas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Neurology Notes For Clerkship ReviewDocument22 pagesNeurology Notes For Clerkship Reviewkep1313Pas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Week 3 Learning ObjectivesDocument12 pagesWeek 3 Learning Objectiveskep1313100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Week 2 Learning ObjectivesDocument21 pagesWeek 2 Learning Objectiveskep1313Pas encore d'évaluation
- Week 5 Learning ObjectivesDocument34 pagesWeek 5 Learning Objectiveskep1313Pas encore d'évaluation
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313Pas encore d'évaluation
- Week 4 Learning ObjectivesDocument24 pagesWeek 4 Learning Objectiveskep1313Pas encore d'évaluation
- Genetics - MMDocument25 pagesGenetics - MMkep1313Pas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- MicroanatomyDocument59 pagesMicroanatomykep1313Pas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Psychiatry - BSDocument15 pagesPsychiatry - BSkep1313Pas encore d'évaluation
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313Pas encore d'évaluation
- Preventative Medicine PM - BSDocument22 pagesPreventative Medicine PM - BSkep1313Pas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313Pas encore d'évaluation
- Anemia DifferentialDocument1 pageAnemia Differentialkep1313Pas encore d'évaluation
- Physiology - BSDocument14 pagesPhysiology - BSkep1313Pas encore d'évaluation
- Physiology - BSDocument14 pagesPhysiology - BSkep1313Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Biogenic AminesDocument5 pagesBiogenic Amineskep1313Pas encore d'évaluation
- 2-5-10 HCT For Immunodeficiency and Autoimmune DisordersDocument2 pages2-5-10 HCT For Immunodeficiency and Autoimmune Disorderskep1313Pas encore d'évaluation
- Week 2 Cellular LevelDocument7 pagesWeek 2 Cellular LevelDayledaniel Sorveto100% (1)
- HR-014 SSS Maternity Benefit AcknowledgementDocument1 pageHR-014 SSS Maternity Benefit AcknowledgementBETH CARANDANGPas encore d'évaluation
- Biosure RGDocument2 pagesBiosure RGJuan Martinez Del AngelPas encore d'évaluation
- Thyroid Diseases in Pregnancy PMK HandoutDocument12 pagesThyroid Diseases in Pregnancy PMK HandoutWikrom Keng WromKiPas encore d'évaluation
- AGada TantraDocument3 pagesAGada TantraGuru Prasad100% (1)
- Bharat India: Extremely Bad Status of Testing & VaccinationDocument308 pagesBharat India: Extremely Bad Status of Testing & VaccinationP Eng Suraj SinghPas encore d'évaluation
- Baby SensesDocument2 pagesBaby SensesCamille LiquePas encore d'évaluation
- 1 - Indocyanine Green-Enhanced Fluorescence To Assess BowelDocument7 pages1 - Indocyanine Green-Enhanced Fluorescence To Assess BowelIcaro DanielPas encore d'évaluation
- BuratDocument5 pagesBuratFreya AvellanoPas encore d'évaluation
- J Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantDocument6 pagesJ Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantTin TomašićPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Healthcare StatisticsDocument20 pagesHealthcare StatisticsAnonymous ibmeej9Pas encore d'évaluation
- Assessment of The Thorax and LungsDocument108 pagesAssessment of The Thorax and LungsJohn Martin Casihan100% (3)
- Implant Failure and ManagementDocument59 pagesImplant Failure and ManagementDrIbrahimShaikh0% (1)
- Greater Political ParticipationDocument12 pagesGreater Political ParticipationBe-COOL State Of MindPas encore d'évaluation
- HC09 ErgonomicsDocument29 pagesHC09 ErgonomicsRegina LiePas encore d'évaluation
- Rearrange The Jumble Letters: 10 1 10Document4 pagesRearrange The Jumble Letters: 10 1 10Shafee ArafatPas encore d'évaluation
- Procedures in Obstetrics and Gynaecology TextbookDocument272 pagesProcedures in Obstetrics and Gynaecology TextbookPriyaPas encore d'évaluation
- Retinoblastoma Clinical and Pathological ClassificationDocument9 pagesRetinoblastoma Clinical and Pathological ClassificationSonia SaulésPas encore d'évaluation
- 2a. Atspph ScaleDocument2 pages2a. Atspph Scaleyani0707Pas encore d'évaluation
- Congenital Anatomic AnomaliesDocument12 pagesCongenital Anatomic Anomaliesmahparah_mumtazPas encore d'évaluation
- Act 1. PhobiasDocument2 pagesAct 1. PhobiasRoxanne CastilloPas encore d'évaluation
- Critical Care Nursing: An OverviewDocument64 pagesCritical Care Nursing: An OverviewProf. Ramsharan Mehta100% (2)
- Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-Central Line Associated Bloodstream Infection)Document50 pagesBloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-Central Line Associated Bloodstream Infection)Luthvia AnnisaPas encore d'évaluation
- Ascitis Quilosa Post Cirugía Abdominal: Caso Clínico y Revisión de La LiteraturaDocument7 pagesAscitis Quilosa Post Cirugía Abdominal: Caso Clínico y Revisión de La LiteraturaJuliet castilloPas encore d'évaluation
- Nursing Skills Checklist - RTDocument6 pagesNursing Skills Checklist - RTapi-309674272Pas encore d'évaluation
- Suz 183Document29 pagesSuz 183Benny Chris TantoPas encore d'évaluation
- Temu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiaDocument1 pageTemu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiabelanjayukdiPas encore d'évaluation
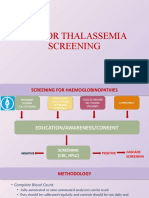
- Sop For Thalassemia Screening Wwith NbsDocument11 pagesSop For Thalassemia Screening Wwith NbsUMMID WashimPas encore d'évaluation
- Treatment of Endometriosis in Women Desiring FertilityDocument23 pagesTreatment of Endometriosis in Women Desiring FertilityVaisnavi Muthoovaloo67% (3)
- Randomized, Placebo-Controlled Trial of Xyloglucan and Gelose For The Treatment of Acute Diarrhea in ChildrenDocument8 pagesRandomized, Placebo-Controlled Trial of Xyloglucan and Gelose For The Treatment of Acute Diarrhea in ChildrenvalenciaPas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (13)