Académique Documents
Professionnel Documents
Culture Documents
5 Essential Hypertension
Transféré par
shanfiza_92Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
5 Essential Hypertension
Transféré par
shanfiza_92Droits d'auteur :
Formats disponibles
Essential Hypertension
Hypertension is the persistent elevation of blood pressure as a figure ( 140/90 mmHg). The persistency has its own characteristics and so does the elevation. If a referred patient is complaining of high BP, his/her blood pressure should be measured in order to confirm the diagnosis, making sure that this elevation is persistent. On the first visit, the blood pressure should be measured three times separated by an interval of 5 minutes of rest, both the diastolic and the systolic BP are recorded. The average of the three diastolic BP readings is calculated and so for the readings of the systolic BP. They are then registered in the patients file as two measures in one figure; one for the diastolic and the other for systolic. The patient is asked to schedule an appointment after 2-3 weeks. He/she is advised not to come in a hurry, after eating a large meal, drinking coffee, nor having smoked cigarettes. These four warnings should be avoided for at least half an hour prior to the appointment, as they will affect the blood pressure giving false readings. On this second visit the same procedures done previously are repeated; blood pressure is recorded three times then their average is calculated and registered. After the two visits, if the systolic BP is 140mmHg or above, and/or the diastolic BP is 90mmHg or above, the patient is labeled as hypertensive. A persistent elevation in one of the two readings (systolic or diastolic) is sufficient to reach the diagnosis of hypertension, however most hypertensive patients will probably have an elevation in both readings.
Two variants of Hypertension that are present in a small incidence in the population are: 1) Isolated Systolic Hypertension. 2) Isolated Diastolic Hypertension.
Internal Medicine
Page 1
Isolated Systolic Hypertension is more common in the elderly population (above 69 years of age). A patient with Isolated Systolic Hypertension will have a systolic BP of 140mmHg or above but a diastolic BP below 90mmHg. Isolated Diastolic Hypertension is more common in young healthy patients with Essential Hypertension. A patient with Isolated Diastolic Hypertension will have a diastolic BP of 90mmHg or above but a systolic BP below 140mmHg. It is mostly related to the Hyperdynamic Circulation (abnormally increased circulatory volume due to systemic vasodilation) in those patients.
As mentioned earlier, Hypertension is defined within two elements; elevation and persistency. Elevation of BP as a figure (systolic 140mmHg, diastolic 90mmHg), and this should be confirmed by three measurements in two separate visits, and this elevation should be persistent. A patient that presents those two elements is described as hypertensive. The current classification of Hypertension is the Joint National Committee classification (JNC) 7th report: Normal Blood Pressure: Systolic 120mmHg and Diastolic 80mmHg. Prehypertension: Systolic between120 -139mmHg and Diastolic between 8089mmHg. Stage -1 Hypertension: Systolic 140-159mmHg and Diastolic 90- 99mmHg. Stage -2 Hypertension: Systolic 160mmHg and Diastolic 100mmHg. *Note: The table in slide 4 describes the classifications of BP and the Pharmaceuticals used in its treatment, it is not important to memorize.
Causes of Hypertension:
Essential Hypertension (Primary Hypertension): It accounts for 95% of all cases of Hypertension, where no cause of the disease is found (Idiopathic), it might be because of familial aggregation, as Hypertension runs in families.
Secondary Hypertension: Accounts for about 5% of all cases, where there is an underlying cause of the disease. The following causes are ordered according to their descending frequency where renal diseases being the most common factor followed by drugs, endocrine diseases, then cardiovascular diseases. 1. Renal Diseases: They are the most common factor leading to Hypertension. They are divided into a) Renovascular causes: - Generalized atherosclerosis (more common): Seen in elderly patients. All vessels in the body are susceptible to atherosclerosis; Carotid, Cerebral, Aorta, Coronary and Renal arteries. When Renal arteries (branching from the abdominal aorta) are affected by an atherosclerotic plaque at the ostium(origin), a narrowing of the artery will occur there. The patient here needs constructive surgery. - Fibromuscular dysplasia: Congenital, seen in young adult females. Causes successive constriction and dilatation of the main renal arteries. This will appear as beadings or balloon dilatations on the renal angiogram.
*Note: The doctor mentioned a few points about a procedure called BTCA or PTCA, which were unclear, and were not mentioned in the slides.
b) Renoparenchymal causes: - Pyelonephritis inflammation of the pelvis or ureters (urinary tracts) of the kidney - Chronic glomerulonephritis: Inflammation of the kidney. Note that acute glomerulonephritis does not cause Hypertension. - Obstructive uropathy: Obstruction of urine flow. - Polycystic kidney disease. - Hypernephromas: Tumors of the kidney
Internal Medicine Page 3
2. Drugs: The most common drugs that are associated with Hypertension are Steroids, Contraceptive pills, NSAIDS, Carbenoxolone and Liquorice (outdated drugs, were used to treat peptic ulcer by coating the mucosal layer, now they are replaced by PPIs), sympathomimetics (nasal drops used by elderly to clear nasal stiffness).
3. Endocrine Diseases:
Hyperparathyroidism Pheochromocytoma Hypothyroidism Cushings Syndrome (high levels of Cortisol) Acromegaly (high levels of growth hormone) 1 Aldosteronism (high levels of Aldosterone)
The only Endocrine diseases not associated with hypertension: - Addisons Disease (low levels of steroids) - Hypoparathyroidism
4. Cardiovascular Disease: The only cardiovascular disease that causes Hypertension is Coarctation of the Aorta.
5. Other Causes:
- Brain tumors: Not all brain tumors cause Hypertension, only those that cause increased intracranial pressure. - Bulbar poliomyelitis (form of infection by Poliovirus) - Lead poisoning - Cocaine abuse - Connective tissue disorders i.e SLE and Polyarteritis Nodosa - Diabetes Mellitus Nephropathy - Polycythemia Rubra Vera
Initial and Primary Investigations in Hypertension:
The following investigations are a must for every hypertensive patient once the diagnosis is established, to know if there is an underlying cause behind the disease. Urinalysis (to check for hematuria or proteinuria) Renal profile ECG Chest x-ray Plain U-T x-ray, Plain KUB x-ray ( Kidney, Ureter, Bladder), or renal ultrasound (to assess kidney size and presence of renal stones or associated uropathy) Urine culture: For patients with possible Acute Ascending Pyelonephritis or Reflux Uropathy. This is specially seen in female adult teenagers (12yo-15yo), where it will be the most probable cause of Hypertension in those females. It has a specific investigation called Voiding Urethrogram. HB, PCV FBS, S.lipids ,S.urate Echocardiography
When to investigate for a secondary cause of hypertension
Sophisticated investigations are costly (expensive), invasive(dangerous) in nature and chances of finding an underlying cause is 5%. They are not done unless we have: 1. Clues from the history: for example a patient with a history of triad of palpitations, headache, excessive sweating and a rise in blood pressure, Pheochromocytoma (a tumor of the supra renal gland) might probably be the cause. Investigations may include renal CT scan, selective renal arteriogram or biochemical work up to diagnose this condition.
Internal Medicine
Page 5
2. Clues from physical examination: if masses were detected on one lobe, one might think of Polycystic Kidney Disease. If striae (stretch marks) on the abdomen and mooning of the face, it might be due to Cushings syndrome, and so further investigations are needed to confirm that.
3. Clues from initial investigations: If the lab works up showed persistent hypokalemia, it might be due to Primary Hyperaldosteronism (Conns Syndrome). If urine tests indicate hematuria or proteinuria. It might be Glomerulonephritis, which might require a biopsy depending on the kidney size.
4. Malignant stage hypertension Ex. Renal biopsies, Renal angiogram etc. as they may cause bleeding due to dissection, kidney perforation etc.
Complications of hypertension:
Hypertension is a silent killer, meaning that it is largely an asymptomatic disease. Patients dont usually complain of specific symptoms associated with the disease. For instance, headaches are thought to be closely related to hypertension, but in fact theyre not. They are just a common disease in the community so is Hypertension, and the presence of these two common diseases in the same patient is a common finding. Against traditional believes, hypertension doesnt cause headaches unless it is in the malignant stage or it has caused cerebral bleeding. So, these two diseases are not correlated.
However, Hypertension may be associated with epistaxis, general fatigue or weakness. These symptoms are not that specific for Hypertension as the might be linked to various systemic diseases. Complications of Hypertension are usual; they are summed up in the following points: Cardiovascular: Angina, Myocardial Infarction, Left Ventricular Hypertrophy, Heart failure, dissecting aortic aneurysm, Cardiomegaly. Cerebrovascular: Transient Ischemic Attack, Thrombotic Cerebral Infarction, Intracerebral Hemorrhage, Hypertensive Encephalopathy Peripheral vascular disease (atherosclerosis, Intermittent claudication, gangrene) Retinopathy (Grades 1,2,3,4) Nephropathy: Raise in Creatinine level, Hypokalemia, Nephrosclerosis, Fibrinoid Necrosis. Malignant Hypertension: Severe stage Hypertension with Systolic 180mmHg and Diastolic 110mmHg, and grade 3 or 4 Retinopathy (Grade 3: soft exudate and hemorrhage, Grade 4: papilledema + soft exudate and hemorrhage). If not treated, it may lead to renal failure, heart failure, blindness, and other complications.
Treatment of Hypertension:
Non-pharmacological measures: 1. Diet 2. Weight reduction 3. Stopping smoking and excess alcohol consumption 4. Regular exercise ( behavioral, biofeedback therapy) 5. Treatment of other associated risk factors
Internal Medicine
Page 7
Nowadays, there is six groups of antihypertensive drugs divided into different classes. A physician should be familiar with at least one drug from each class, and familiar here implies that this physician should have complete knowledge of this drug in terms of dosage, frequency of administration, side effects, precautions, and complications
Antihypertensive medications:
*Note: only memorize drug classes. 1. Diuretics - Thiazide: very weak diuretic effect, it stimulates vasodilation in the arterial walls by relaxing the smooth muscles of these vessels. - Loop: they are not used as an antihypertensive drug unless the condition was associated with fluid retention due to heart failure and renal failure. - K+ sparing 2. Beta-Blockers: Widely used drugs, used to treat hypertension as well as many other conditions like heart failure, migraine prophylaxis, tachycardial essential tremor, angina etc Ex:- Non-Cardioselective, Cardioselective, Drugs with ISA, Alpha and Betablockers (labetolol). 3. Alpha-blockers ( prazosin) 4. Central acting drugs: Not used as much nowadays. Ex: Reserpine, Methyldopa, and Clonidine.
5. Vasodilators: a) Direct relaxation of arteriolar smooth muscle: Specially peripheral vasodilators. A common side effect is Orthostatic Hypotension, which causes distress. Have been replaced by other classes. Ex: -Hydralazin -Minoxidil Diazoxide -Na Nitroprusside b) Calcium-channel blockers: - Verapamil - Nifedipine - Amlodipine c) ACE inhibitors: Angiotensin Converting Enzymes Inhibitors Ex: - Captopril - Enalapril - Lysinopril - Quinapril 6. ARBs: Angiotensin Renin Blockers Ex: - Losartan - Candesartan - Irbisartan - Valsartan
Hypertensive Crisis (Hypertensive Emergency): Severe hypertension (>180/110mmHg) with one of the following: 1. Heart failure 2. MI 3. Renal failure 4. Encephalopathy 5. Dissecting aneurysm 6. Intracerebral hemorrhage 7. Accelerated or malignant hypertension Hypertensive crisis requires rapid action and treatment with parenteral medications (Direct IV infusion, direct IV boluses or subcutaneous infusions) to reduce blood pressure in a matter of minutes rather than hours or days. NOTE: Blood pressure shouldnt be reduced to below diastolic of 100 mmHg Parenteral Drugs Used In Hypertensive Emergencies are not to memorize.
Done by: Raya Dawood & Lama Ashour
Internal Medicine
Page 9
Vous aimerez peut-être aussi
- 9 Viral HepatitisDocument15 pages9 Viral Hepatitisshanfiza_92100% (1)
- 5-Ischemic Heart DiseaseDocument7 pages5-Ischemic Heart Diseaseshanfiza_92100% (1)
- Oral ManifestationsDocument40 pagesOral Manifestationsshanfiza_92100% (1)
- 10-Oral Manifestations of Systematic DiseasesDocument11 pages10-Oral Manifestations of Systematic Diseasesshanfiza_92Pas encore d'évaluation
- 4 Bronchial AsthmaDocument9 pages4 Bronchial Asthmashanfiza_92Pas encore d'évaluation
- Infective - Endocarditis 7th Prt1Document32 pagesInfective - Endocarditis 7th Prt1shanfiza_92Pas encore d'évaluation
- 7-Headache and Facial PainDocument11 pages7-Headache and Facial Painshanfiza_92Pas encore d'évaluation
- Oral Manifestatios of Systemic DiseaseDocument43 pagesOral Manifestatios of Systemic Diseaseshanfiza_92Pas encore d'évaluation
- 8 CKDDocument21 pages8 CKDshanfiza_92Pas encore d'évaluation
- Acute Rheumatic Fever 7th Prt2Document18 pagesAcute Rheumatic Fever 7th Prt2shanfiza_92Pas encore d'évaluation
- 9 Viral Hepatitis Dentistry School 2012 2013Document46 pages9 Viral Hepatitis Dentistry School 2012 2013shanfiza_92Pas encore d'évaluation
- Essential HypertensionDocument16 pagesEssential Hypertensionshanfiza_92Pas encore d'évaluation
- 6-Arf & IeDocument26 pages6-Arf & Ieshanfiza_92Pas encore d'évaluation
- 9 Liver CirrhosisDocument25 pages9 Liver Cirrhosisshanfiza_92Pas encore d'évaluation
- ChronicKidneyDisease 2Document37 pagesChronicKidneyDisease 2shanfiza_92100% (1)
- Headache and Facial Pain2Document40 pagesHeadache and Facial Pain2shanfiza_92100% (1)
- CapDocument33 pagesCapshanfiza_92Pas encore d'évaluation
- Ischaemic Heart DiseaseDocument19 pagesIschaemic Heart DiseaseSawsan Z. Jwaied100% (1)
- 3 CopdDocument17 pages3 Copdshanfiza_92Pas encore d'évaluation
- Bronchial Asthma Dental 2012Document37 pagesBronchial Asthma Dental 2012shanfiza_92Pas encore d'évaluation
- 4 CapDocument11 pages4 Capshanfiza_92Pas encore d'évaluation
- Sleep Apnea SyndromesDocument12 pagesSleep Apnea Syndromesshanfiza_92100% (1)
- Sleep Apnea Syndromes: Suleiman M. Momany, MD, FCCPDocument45 pagesSleep Apnea Syndromes: Suleiman M. Momany, MD, FCCPshanfiza_92Pas encore d'évaluation
- Copd DDocument44 pagesCopd Dshanfiza_92Pas encore d'évaluation
- Internal Medicine IIDocument15 pagesInternal Medicine IIshanfiza_92Pas encore d'évaluation
- Anemia LectureDocument56 pagesAnemia Lectureshanfiza_92Pas encore d'évaluation
- Bleeding Tendency For DentistDocument58 pagesBleeding Tendency For Dentistshanfiza_92Pas encore d'évaluation
- Diabetes: Internal MedicineDocument21 pagesDiabetes: Internal Medicineshanfiza_92Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Illusions The Magic Eye of PerceptionDocument12 pagesIllusions The Magic Eye of PerceptionArctic Illusion100% (2)
- Shame and Belonging - Robert LeeDocument16 pagesShame and Belonging - Robert LeeStanculescu AlinaPas encore d'évaluation
- CH 3 - Study GuideDocument13 pagesCH 3 - Study Guide2688giePas encore d'évaluation
- How Finally I Straightened My Spine OutDocument169 pagesHow Finally I Straightened My Spine OutGiuseppe Medina100% (1)
- Naziya & JignaDocument44 pagesNaziya & Jignakishan100% (1)
- Chapter V - The InstrumentDocument6 pagesChapter V - The InstrumentErica Marie BagonPas encore d'évaluation
- ECG Interpretation BookDocument57 pagesECG Interpretation BookLouis Plan100% (2)
- Performed Structural DesignDocument93 pagesPerformed Structural DesignSaiful IslamPas encore d'évaluation
- The Importance of Anaerobic ExerciseDocument13 pagesThe Importance of Anaerobic Exerciseapi-357421918Pas encore d'évaluation
- June 2009 MS - Unit 1 Edexcel Biology A-LevelDocument24 pagesJune 2009 MS - Unit 1 Edexcel Biology A-LevelAyse KerimPas encore d'évaluation
- Neurology SyllabusDocument42 pagesNeurology SyllabusCHALAPATHI ENJAPURIPas encore d'évaluation
- 1 Digestion and AbsorptionDocument12 pages1 Digestion and AbsorptionJared Dela cruzPas encore d'évaluation
- Medication AdministrationDocument88 pagesMedication AdministrationKBD100% (1)
- Lung Work SheetDocument2 pagesLung Work SheetGalo LandivarPas encore d'évaluation
- Neuroscience Pathways Fall 2012Document46 pagesNeuroscience Pathways Fall 2012Yezin ShamoonPas encore d'évaluation
- Head Toe Physical AssessmentDocument2 pagesHead Toe Physical Assessmentzbestgurl100% (2)
- Physiology of The Liver: Corresponding AuthorDocument12 pagesPhysiology of The Liver: Corresponding AuthorMansour HazaPas encore d'évaluation
- MARA TRIAL 2013 BIOLOGY PAPER 1 ANSWER KEYDocument43 pagesMARA TRIAL 2013 BIOLOGY PAPER 1 ANSWER KEYAhmad Imran Idzqandar100% (2)
- 1.introduction To Physiology, The Cell and General PhysiologDocument3 pages1.introduction To Physiology, The Cell and General PhysiologCLEMENT100% (1)
- FixationDocument3 pagesFixationficatPas encore d'évaluation
- Trimestral Exam First GradeDocument3 pagesTrimestral Exam First Gradeemmanuel espinozaPas encore d'évaluation
- Reduce sodium guide for food industryDocument82 pagesReduce sodium guide for food industryperunikicaPas encore d'évaluation
- G9 Science Q1 - Week 1-2 Respiratory-Circulatory-SystemDocument34 pagesG9 Science Q1 - Week 1-2 Respiratory-Circulatory-SystemSandra Lee LigsaPas encore d'évaluation
- Lipoma in Submandibular Region - A Case ReportDocument4 pagesLipoma in Submandibular Region - A Case Reportmaxfac2010Pas encore d'évaluation
- Lesson 1 Forensic 5Document7 pagesLesson 1 Forensic 5Marcos DmitriPas encore d'évaluation
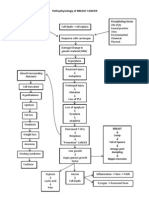
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Nutrition Folio (Basal Metabolic Rate)Document15 pagesNutrition Folio (Basal Metabolic Rate)Nursakinah NajwahPas encore d'évaluation
- Funda Vital SignsDocument63 pagesFunda Vital SignsElia Saph MoonPas encore d'évaluation
- Circulatory System - Class 10Document4 pagesCirculatory System - Class 10Biozeneca classesPas encore d'évaluation
- The Science of Nei Jia Quan ExplainedDocument12 pagesThe Science of Nei Jia Quan ExplainedArran O RuaircPas encore d'évaluation