Académique Documents
Professionnel Documents
Culture Documents
GOLJAN - Special Pathology (Resp)
Transféré par
bobiome0 évaluation0% ont trouvé ce document utile (0 vote)
266 vues21 pagesgoljan special respiratory system notes
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentgoljan special respiratory system notes
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
266 vues21 pagesGOLJAN - Special Pathology (Resp)
Transféré par
bobiomegoljan special respiratory system notes
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 21
Respiratory system
Arterial blood gas (ABC) interpretation:
1. review Fluids and Hemodynamics and Acid-Base
2. r espiratory acidosis:
A. pH <7.35
O. PCO,> 45
c. compensation is metabal ic alkalosis:
(1) HCOl ~ o mEq/L is aellie respiratory acidosis
(2) HCO
l
>30 mEq/L is chronic respiratory acidosi s
3. respiratory alkalosis:
A. pH >7.45
B. PCO, <33
C. metabolic acidos is is compensati on:
(1) HeOl ~ t 8 mEq/L is acute respi ratory alkalos is
(2) HeO
l
<12 mEqIL is chronic respi ratory alkalosis
4. metabolic acidosis:
A. pH <7.35
B. HeO, <22
C. respiratorY alkalosis is compensation: peo
2
decreased
5. metabolic alkalosis:
A. pH >7.45
B. HCO, >28
C. respiratorY acidosis is compensarion: PCD, increased
6. mixed disorders:
A. if the pH is nonnal (7.35-7.45). it must be a mixed disorder since there is no full
compensation
B. if pH is very low, it must be 2 acidoses: e.g., cardiorespiratory arrest with respiratory
acidosis + metabolic acidosis
C. if pH is very high, it must by 2 alkaloses: e.g .. respiratory alkalosis and metabolic
alkalos is)
D. example: salicylate intoxication Me mixed ABG asked on USMLE:
( \ ) normal pH
(2) PCO, <22
a. respiratory a lkalosis
b. saJi cylates overstimulate the CNS respiratory center
(3) HCO, <22
a. metabolic acidos is
b. salicylate is an acid and salicylates damage mitochondria leading to ti ssue
hypoxia and lactic acidosis
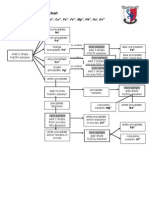
Pulmonary functi on tests in restrictive a nd obstructive lung disease: see schematic
1. restrictive lung disease-
A. problem in gening air inlo the lungs: decreased compliance
S. elasticity is increased: once ai r is in the lungs, it comes Oul rapidly on expirat ion
C. all volumes and capacities are equally decreased
D. forced expiratory volume in I second (FEV ~ ) is decreased:
78
Seconds
a 1 2 3 4
1
2
RV FRC
t t
6
FIGURE 11-1. Schematic of the normal lung volumes and Cil-
pacities and the forced expiratory volume 1 second (FEVt.,.J
and forced vital capacity (FVC) I.n a normal penon (A) , a person
with restrictive lu.ng disease (8), and a person with obstructive
lung disease (C). me (functional residual capacity) represents
the volume of gas that remains in the lung at rest at the end of a
normal respiration and Is the most reproducible part of a
nary function test, since It does not require patient effort. Person
A (nonnal Individual) has an FEV,_ 01 4 L and an FVC of 5 L,
with FEVu.JFVC ratio = 0.80. Person B with restrictive lung
disease has a "mlniaturlfed" curve of person A. Note that the
FEV
t
-: and FVC are the same (3 L) owing to the lncrease In
elasticity In the lungs. hence FEVb.JFVC ratio::; 1.0. Person C
with the obstructive pattern Is having dlificulty in expelllng air
from the lungs owing to decreased lung elasticity. FEV
t
....: = I L,
FVC 3 L, and FEV b..fFVC ,.tio 0.33. Both people B and C
have _reduced values for FEV
tocc
and FVe when compared with
the normal person; however. person B with restrictive lung dis-
ease has values between those of the normal Individual and
person C With obstruction. Person B has decreased compliance
In the lungs. hence less air enters the lungs. but owing to the
Increased elasticity, the air that Is In the lungs is expelled faster.
Person C has Increased compliance (alr easily enters the lungs) ;
however, reduced elasticity causes the lungs to trap aIr on expira
tion, hence and FVe are much lower than In person B and
the FEV t.,JFVC ratio Is reduced. nc, total lung capacity; TV,
tidal volume; ve, vital capacity.
"'"
(1) FEV IJ is how much air a person can expel from the lungs in I second after a
ma.ximal inspiration
(2) normal FEY he: is 4 liters
(3) usually <3 liters in restrictive disease
E. forced vital capacity (FYC) is decreased:
( l ) FVC is how much air the patien! can expel from the lungs after a maxi mal
inspiration
(2) normal is 5 liters
(3) often the same value as FEV 1m due to increased elasticity of the lungs
F. rat io ofFEV1 ,c/ FVC is increased:
(1) normal is 4/5 "" 0.80
(2) in resu ictivc disease, il is usually increased (3/3 "" 100%)
2. obs tructi ve lung disease-
A. problem with gening air out of tile lungs rather than into the lungs:
(1) compliance increased
(2) elasticity decreased
B. residual volume is increased. since all the air cannot get OUI of the lungs:
(1) this automalicall y increases the total lung capacity
(2) other volumes and capacities afe decreased
C. forced expiratory volume in I second (FEV Inc) is dec reased:
(I) normal FEV
I
",. is 4 liters
(2) usually <2 liters in obmuctive disease
D. forced vital capacity (FVC) is decreased:
( 1) normal is 5 liters
(2) usually <2 liters, due to decreased elasti city of the lungs
E. ratio of FEVlw'FYC is decreased:
( 1) normal is 4/5 = 0.80
(2) in obstructive disease, il is usually decreased (1 /3 = 0.33)
3 s ri r b d d' . umman' 0 ' pu monarv uncbon tests ID 0 structl vc a n r estrictIVe une I Isease
Par a meter Obstructivc Rest'r ieth-'e
TOial lung capacity (TLC) Increased Decreased
.
Residual volume (R V) Increased Decreased
Tidal volume (TV) Decreased Decreased
Vital capacity (VC) Decreased Decreased
FEV l Decreased Decreased
FVC Decreased Decreased
FEV'R.lFVC
Decreased Nonnal to increased
DLeo
Decreased Decreased
FEV luc - forced expiratory volume I second, Fye - forced Vital capaCity, Oleo - diffuSion capacity
with carbon monoxide
Causes oran increased alveolar-ttrt erial grad ient (A-a gr ndient):
1. A-a- difference between the alveolar PA0
2
and anerial Pa02 in the lungs
2. causes or i,ncreased gr ad ient -
A. ventilation without perfus ion:
(1) e.g., atelectasis
(2) produces intrapulmonary shun!ing
(3) giving 100% 0
,
does not increase the Pa02
79
I
I
I
B. perfus ion without ventilation:
(1) e.g., puLmonary embolus
(2) increased dead space
(3) giving 100% O
2
does increase POl since nomall)' ventilated lung can make up
the difference
C. diffusion abnonnalities: e.g., interstitial fibrosis
D. right to left shunts in the heart: e.g., cyanotic congenital hean disease
J. rormulo used to caltuhue A-a gradient-
A. I'AO, - % oxygen (713) - PaCO,! 0.8:
B. using normal values- PAOl "" 0.2 1 (7 13) 40/0.8 . 100 mm Hg
4. caUJ6 orbypoumia " 'ilh a Dormat A-a gradinl-
A. depression of the respiratory center in the medulla:
(1) e.g . blU'bilurates
(2) CNS injury
B. obstruction of upper airway:
(1) e.g., cafe coronary
(2) epi glonil is
(3) croup
C. chest bellows dysfunction: c.g., paralyzed diaphragm
ani polyps!
1. aUergic-
A. MC type
8. occurs in adults
2. aspirin-re.lated-
A. clllled triad asthma:
(I ) take aspirin
(%) develop asthma
(3) nasal polyps
B. usually occurs in patients with chronic pain syndromes
C. non-immune mechanism:
,
( I) aspirin blocks cycloo1C.ygenase and leaves the lipoxygenast pathway open
(2) LTC-, D-. E. are increased., which cause bronchoconstriction
3. cystic fibrosis- any child with nasal polyps and a history of repeated respiratory infections
and diarrhea should have a sweat (est
Laryngeal nrdooma:
I. eausC5-
A. smoking: MCC
B. alcohol
C. asbestos
2. sile-
A. supraglottic area is MC location
B. squamous cell carcinoma
3. cUnieal-
A. hoarseness
80
cr Alelecta5i,,:
I. MCC of revu 24 hs arter s urgery
2. palbophysiology-
A. collapse of alveoli due to mucus blocking terminal bronchioles
B. distal resorption of air through the pores of Kohn
l . dinical- signs of consolidation:
A. increased tactile m:mirus (lAJA.hc ,.L i<d-";'.
B. decreased percussion
C. elevated diaphragm (diaphragm moves up when alveol i collapse)
D. chest lag on inspiration
cr urraclanl :
l. drugs Ihal increase "uriaetanl synthesis-
A. glueoeortieoids- women who must deliver prematurely are ghlen glucoconicoids to
increase surfactant synthesis in the baby
n. thyroxine
2. eorn!lollon-
A. Laplace's law states that coll apsing pressure or alveoli P - 2 T (surface tension)/r
(radi us of alveoli)
B. s urfacta nl deereases s urface tension and keeps the alveoli open on expiration
C. surfactant :
(I) lecithin (phosphatidylchol ine)
(2) synthesized by type II pneumocytes
(l) stored in lamellar bodies
Respiralory distnss syndrome:
1. palbogcacsis-
A. deerused surfactant in rCIUJ due 10:
( 1) baby is.premature
(2) poor glycemic control in mother with diabetes
hyperglycemia in
b. hyperglycemia in fetus-t
c. increase in fetal release of
d. insulin inhibits surfactant synthesis)
(3) c;sw:can section
. no stress on baby-+
b. no increase in conisol
2. palhophysiology-
A. widespread atelectasis-+
8 . musive iDtrapulmonary
C. hyaline membranes composed of protein from vesselleakllge (diffusion defect)
l. cliniCAl-
A. respiratory difficulty shonly after binh
8 . cyanosis
4. complic.atjoDJ-
A. supe.roxide free radical damage:
(1) retrolental fibroplasia
(l) bronchopulmonary dysplasia
8 . necrotizing enterocolitis
81
C. intraventricular hemorrhage
O. patent ductus arteriosis with machinery murmur: due to persistent hypoxemia
5. JU olRDS-
A. positive end. expiratory pressure PEEP)-keeps airways from collapsing on expiration
B. deliver)' of surfactan t via PEEP therapy
C. oxygen
Adult disl.ress syndrome (ARDS):
I. (,Il uses-
2.
3.
A. endotoxic s hock MCC
B. gastric aspiration
C. trauma
D. pneumonia
E. smoke inhalation
pathophysiology-
A. non.cardiogenic pulmonary edema
D. neutrophil-relnt ed injury with destruction of'type II pncumocytes (loss of surfactant)
and damage to pulmonary capi llaries ("leaky capil lary syndrome"
C. massive intrapulmonur)' shunli ng from loss of surfactant is the most important
abnormal ity
D. hyaline membranes from protein leaking from capi llaries
separate from cardiognic pulmonary edema by pulmonary capillary wedge press ure
(measure of left ventricular end-diastolic press ure)-
A. low in PCWP in ARDS
8. increased PCWP in cardiogenic shock
4. higb morta lity
SpoDt.aneous pneumothorax:
1. causes-
A. idiopathic:
( I) MCC
(2) tall, thin males ,
(3) .!l!plUt<..IlLs.ubpkll,al bullae in a x of lung
B. iatrogenic: e.g., needle puncture of lung after performing II subclavian vei n Slick
C. Marfans syndrome
2. pathogenesis- portion of the lung collapses: pleural cavity pressure is the same as the
atmospheric pressure
3. clinical-
A. sudden onset of pleuritic type of chest pain
B. tympanitic percuss ion note
C. absent breath sounds
D. diaphragm elevated
E. tracbea de" iate! to the side of the colla pse
4. l'1JSMLE sudden onset of pleuri tic chest pain in a scuba diver with collapsed lung,
elevation of the diaphragm, and shi ft of Il11chea to the side of the collapse: spontaneous
pneumothora.x
Tension pneumothorax:
I. cuuse-
A. penetrating trauma to the lungs
82
B. tension pneumatocysts:
(1) occur in patients with S. alll'eUS pneumonia (e.g .. cystic fibrosis)
(2) intrapleural blebs occur thai may rupture
2. palhophysiology-
A. tear in the pleura allows air into the pleural cavity bUI prevents its exit
B. increased intrapleural press ure sbifu tbe mediaslinal Sl rUCI ures to tbe opposite
side: compromises blood flow int'O the heart and OUI of the heart
C. diaphragm is depressed on the affected side
D. breath sounds absent on affected side
E. tympanitic percussion notc
3. Rt- insert needle into the pleural cavity to relieve pressure
Typical VI atypi cal pneumooia:
I. typk.l-
A. sudden onset of symptoms
B. high fever
C. productive cough: usuall y positive gram stain for bnctcrin
D. signs of consolidation on physical exam and x-ray
E. StreplococCW; pneumolliae MeC
F. chest x-ray is first step in management
2. atypical-
A. insidious onset
B. low grade fever
C. non to mildly productive cough
D. no signs of consolidation (interstitial pneumonia)
E. Mycoplasma pneumonioe MCC followed by Chlamydia pnelimoniQe (TWAR agent)
Community-acquired \ '5 nosocomial pneumonia:
t . community a c q u i ~ d - MC due toSrreplococcus p"eumo"iae
2. nosocomial-
A. develops while in the hospital
B. organisms in descending order:
( I ) E. coli
(2) P. aeruginosa (Me if a respi rator is involved)
(3) S. allreus
Differential for rusty colored sputum:
1. Streptococcus pneumonioe pneumonia
2. chronic congestive beart failure- heart failure cells
3. mit ral stenosis
4. Goodpas ture's syndrome
SummarY tables of infectious disease
Microbial Epidem iology
Piltboeen
Minol,irus
MCC (25-30%) of common cold. Main
reservoir are school children. Direct hand to
hand transfer of infected materiaVrespiratory
droplet infection. -100 serotypes (vaccine
Clinical
Increased mucus secretions. sneezing
and coughing. URI Me infection in
clinical practice.
I
unlikely).
J
83
Respiratory
syncYlia/ virus
(RSI?
lnfluen=avirus
Rubeola
(regulor
mewles)
I Chlamydia
! pslrraci
Mec of interstitia.) pneumonia (20%) and
bronchiolitis with wheezing (50%) in infants.
Late falVwinter. Hand [0 hand transfer of
infected materiaVrespiratory droplet infection.
Significant cause of monality especially
among those over 55 years of age who have
underlying renal, cardiac or lung problems.
Type A virus produces pandemics and
epidemics (most severe form). Type B
produces epidemics. Type C is involved in
sporadic cases. Hemagglutinins bind the virus
to cell receptors in the nasal passages.
Neuraminidase dissolves mucus and
facilitates the release of viral particles from
the infected cell . Local epidemics resuh from
minor changes in the antigeniciry or the
organisms, called antigeni c drifts (point
mutations). Pandemics are due [0 Jlntigenjc
lb.i&. which involve mutations in
hemaJlJllutinin (need new
Symptoms of rubeola begin to appear after the
7- 14 d incubation period is finished.
Ornithosis, or psittacosis, is a zoonosis (a
disease contracted frpm animalS). lnhalation
of C. pS;lIocl from birds (parrots,
Ox with direct immunonuorncent
techniques or ELISA test on
nasopharyngeal swabs. Rx: ribavirin
for very severe infections.
Mild cold to bronchitis to severe
pneumonias (with exudate). Pneum
onia allen has a superimposed
bacterial pneumonia (Staphylococcus
aureus). Vaccine is effective in
preventing Du in 10 to 90% of healthy
young people. 1n older people. it is
only 50% effective in preventing flu
but 85% effective in preventing
death. Reye syndrome may occur in
children. R.x: amantadine (inhibits
viral uncoating or transcription of
vi ral RNA) .
Fever. cough, conjunctivitis, and
coryza (excessive nasal mucus
production) initially occur. K2R.I..ik
}IKU1 in the mouth precede the onset
of the maculopapular rash. Pneum
onia is the Me coo. Wanhin
Finkeldy multinucleated Riant cells.
Primarily results in interstitial
pneumonitis. Rx: erythromycin.
I I Darakeets. Di.eons, and turkeys).
pneumonlae intermediate. 5% of community acquired
I (11VAR) atypical pneumonias. SeroeDjdemiologic
__ __ ____ ______ __
I Chlamydia Newborn pneumonia. -10 to 20% of Presents with 51accaro cough. can
fraclromatls newborns that pass through an infected birth juncti ... it' is, tachypnea, bilateral lnspir
I canal develop pneumonia. 8tory crackles, scattered expiratory
I wheezes. and hyperinnation (trap air).
t Afebrile. Eosinophilia. Rx: erylhro-
mycin.
t
bumeri; (Q Inhalation. Contracted by dairy fanners, chest pain, myalgias. Interstitial
veterinarians associated with the birthi ng pneumonia. Other problems: granu1o-
process of infected sheep, cattle and goats and matous hepatitis (50%), infective
J handling of milk in these animals. USMLE: endocarditis. Rx: doxycycline.
IL-________ .. __________ _L ______________________ --"
!
84
Mycoplasma
pneumoniae
Microbial
Pathogen
Streptococcus
I pneumo,tlae
Staphylococcus
(IlIre,u
Hemophilus
injluetrzoe
Pseudomonas
aerugitto.ra
Klebsiella
pneumonlae
Nocardia
Qsreroidu
Actinomyces
Israeli
Legionella
pneumophila
MCC of primary atypical pneumonia. I Nonproducti ve cough. Upper respira-
15- 20% of pneumonias in adolescents. 50% lOry tract symptoms (pharyngitis.
of pneunlonias in military recruits. earache) precede pneumonic manifest-
lncubation period 1- 2 wks ations. Interstitial pneumonia. Low
Gram Stain
Gram + lancel-shaped
diolococcus
Gram + coccus
Gram-rod
Gram - thin rod.
Gram - fat rod with
capsule
Sirict aerobe. Gram +
filnmentous bacteria.
Panially acid fast
Anaerobe. Gram +
filamentous bacteria.
Gram - rod (need IF
staiD or Dieterle silver
stain
Comments
grade fever. Complications: bullous
myringitis (hemorrhagic vesicles on
the membranes), erythema mulriforme
(target-like leSions), and Stevens
Johnson syndrome (involves skin and
mucus membranes in a disseminated
manner), cold autoimmune hemolytic
anemia due to anti J. Lab: increa.sed
cold agglutinin titers. Rx:
mvcin or tetracvcline.
Mec of community acquired tyPjcal pneumonia
I (bronchooneumoniB or lobar oneumonia). Rx: erYthromycin.
Pneumonia commonly foIlQ''''s influenza infections (Me
bacterial pathogen), Major pathogen in cystic fibrosis.
Common cause of nosocomial pneumonia. Hemorrhagic
puJmonary edema, abscess formation, and tension
pneumatocyslS (intrapleural blebs), which may rupture and
I produce oneumotborax. y,.l lnw I'!nlor,.d c.nutum.
Common cause of pneumonja in cystic fibrosis and COPO.
Rx: TMP/SMX. Acute epiglottis in children. Decreased
incidence due to immunization. Cause of inspiratQry stridor.
Thumbprint sil!;tl on lateral x-ray of neck. Rx: cefuroxime
Water loving bacteria transmitted by respirators. Common
cause of nosocomial pneumonia and MeC of pneumonia in
cystic fibrosis. Me pneumonia in ICU/CCU (due to
respirators). Blood vessel invader (hemorrhagic infarctions).
Green colored sputum (pyocyanin). Rx: antipseudomonalj3-
lactamase susceptib.le oenjoiUins . mezlocill in)'
Pneumonia commonly associated with alcoholics and Me
pneumonia in nursing homes. Blood-tinged. mucoid sputum.
Tends to involve the upper Jobes and cavjtales like
reactivation lB. Lobar consolidation and abscess formation
are common. Rx: third generation cephalosporin
Granulomatous microabscesses in the lungs in
immunocompromised patients. Rx: TMP/SMX
Draining sinuses in the jaw. chest cavity, and abdomen.
Sulfur granUles contain bacteria. R.x: ampicillin or penicillin
G.
Water loving bacteria (water coolers). Pneumonia with dry
cough. malaise, fluHke symptoms, bloody sputum, and
sttikinR. fever. Other flndintts: anhrule.ias renal and CNS
85
Mycoboclerium
tuberculosis
Candido
olbicans
Coccidioides
Immilis
CryPIOCOCCUS
neojormolls
HislopifUmo
capsulolum
Strict aerobe. Acid-
fast
Not dimomhjc. Sud-
ding yeastS and pseudo-
hypha. Lung disease
contracted from infect-
ions of indwelling cath-
eters.
Djmorphic. Spberules
with endospores in tis-
sues. Inhaling arthro-
spores while li ving or
passing through the
Southwest or San Joa
quin vaHey in Califor-
nia ("valley fever").
Not dimornbjt. Sud-
ding yeast with narrow
based buds. Found in
pigeon eXcreta (around
buildings, outside of-
fice windows, under
bridges). Me fungal
opportunistic infection.
Dimorphic. Me syste-
mic fungal infection.
Me in Midwest Inhal-
ation of spores. Assoc-
iation wilh lUrm
(Starlings), cave em:
lorers (spelunkers),
abandoned warehous-
n. yeaSt fonus in mac-
roPhaacs.
8
00
findings. Macrophage rather than a neutrophil response in
tissue. Can produce hyponatremia secondnry to hypo-
reninemie hypoaldosteroojsm from interslitial nephritis. Rx:
erythromycin or tetracycline + rifumpin.
Droplet infection. Primary IB: upper pan lobe, lower
pan of upper lobe. Ghan complex. Usually resolves.
Reactivation IS: upper lobe, cavitary lesion. Kidney Me
exuapulmonary site.
Vessel invasion produces hemorrhagic
amphotericin S or fluconazole
infarcts. Rx:
Flu-like symptoms and erythema oodosum (pai nful nodules
on lower legs). Pneumonia may be localized (egg shell
cavity in lower lobes). "coin lesions". miliary spread in the
lungs andl or throughoUi the body. African-Americans
3
Mexicans, and Filipinos have severe infections. Lab:
culture, direct visualization of the spherules with
endospares, skin test (useful), and serologic tests (useful).
Rx: fluconazole
Primary lung disease (40%). Produces a granulomatous
reaction. if immunity is intact but no in'flammatory
ifimmunocompromise<i. Lab: culture., direct visualization of
the organisms and by serologic tests. Rx; amphotericin B or
fluconazole
Simulates TB lung disease. Donnant phase like TB (can
reactivate). Produces coin lesions, consolidation, miliary
spread. cavitation. Old infection sites characteristically
contain c.alcified granulomas. Mec of sclerOSing
mediastinitis (fibrous tissue In mediastinum with
encroachment on all mediastinal structures). Lab: culture,
direct visualization in tissue (organisms in macrophages),
skin tests (useful), and serologic tests (useful). Rx:
ilraconazole (moderate disease), amphotericin B (severe
disease)
-
86
BlastomYCl!s Dimorphic. Yeasts lnyolves skin (skin has a verrucoid appearance resembHng
dermatitidis have b[oad based buds. squamous can:: inoma) andlor .lung. Male dominance. Lab:
Primarily along the culture, direot visuali zation of the yeast forms in tissue. R.x:
Southeast coast and itraconazole
into Midwest. AJong
inland waterwa.ys with
beaver darns. Inhalat
ion.
Aspergillus Not dimol]hic. Fruiting Aspcrgilloma, refers to a fungys ball (visible on :Nny) of
fumigatus .QQQy and narrowangl matted hyphae and fruiting bodies that develops in a
sel2tate preexisting cavity in the lung (e.g., old TB site). Cause of
hl!l1hae. massive hem!:H2lY:ti5:. Allergic Q[Q(lcbol2ulmonm disense
involves both type J and type III hypersensitivity reactions.
IgE levels increased. Vessel invader with hemorrhagic
infarctions and a necrotizing bronchopneumonia. Common
sinus infection in AlDS. Lab: culture, direct visualization.
Rx: amphotericin B or itraconazole
Absidi .. diwQmbiSl, Wide
Clinical settings: diabetes, immunosuppressed patients.
Mucor. angled h:mhae withoy! Vessel invader and produces hemorrhagic infarcts in the
Rhizopus septa. lung. Invades tbe frQntal Jobes in diabetic Lab:
culture, direct visualization. Rx.: amphotericin B
Pneumocyslis Reclassified as fungus. Opponunjsli c infection. Me initial AIDS-defining infection.
carinil CySts attach to type I Lungs are dry and consolidated. Patients present with low-
pneurnocytes. Poorly grade fever, dyspnea and tachypnea. Bronchoalveolar
visualized with gram lavage and lung Bx identify organisms. Chesl xray: diffuse
stains but stajn well alveolar and interstitial infiltrates. Rx: TMP/SMX. Given
with silver and Qiemsa prophylactically when CD
4
counts <200 ceUslJ,LL.
stains. Foamy alveolar
infillTBte. Occ\lrs when
CD" T count
<200 celisiuL. >
Parasites with Ascaris, hookworm.
larval phase in
cr
1. mliiiii Iii
<-ft6 .... 1s deIItJ-USOe:lited wttIlL._Ur.U
rpjij ii:ijiII po 11
A. pneumonia
B. bronchiectasis
C. sepsis
D. tension pneumothorax from ruptured pneumatocysts
2. ot:paeumoatalD aerugill osa
3. v e_ 10 lirizoaa: itb _" Jra ory Infemoa+- coccidioidomycosis (nol
histoplasmosis, too dry a climate and mainly in Ohio and Midwest)
4. fl'iiIge.poID.er In N. '" Clty:Mili .... pliiifOi'jIlar.dlo
A. most likely histoplasmosis (starling dung) or cryptococcus (pigeons)
B. may ask what to Rx the patient with: amphotericin
5. (!!J!lraroo:Jllji)JJem usoclat&l Wltbfll!!i!arno R!e<llDS aUU\l...OH WlDdiJ.l" illl or aad
cryptococcus
87
6. dilHles wbere StreplOC:OC:cUJ paeumoa.iae is MCC-
A. community acqui red pneumonia
B. meningitis in adults > 18
C. otilis media
D. spontaneous peritonitis in children with asci tes
E. in children with HbSS disea.R
F. sinusitis
7. dlieuetl "lIere PSt!lIIiolftDnas ae'''IiJrosa is MCCI-
A. ICU pneumonia (respirators)
n. COD in bum patients
C. COD in cyst ic fibrosis
D. cellul iti s/osteomyelitis in puncture wounds of foot in patient's with rubber footwear
E. malignant external ot ili s in diabetes
f . ecthyma gangrenosum
G. hot tube folliculiti s
8. di.Hatet wbere BC!mophUus IDOueDZIIe ".MCC- nc ute epiglottit is due to Hib
immunizat ion)
9, Me !JDs-denDiDg IDfeedOD!... Pneumocyslis cari" U pneumonia
10. eldetty mIlA, wlio lives .1 bome wlda It.ia wife. develops pDe.moDia- Slreprococcils
pnellmonia
II. ellat Jr.y'Widt ricIIt middle lobe p.eamo .... (obscures ri ght ma rgin of the heart)-
A. probably related 10 obstruction by a bronchogenic carcinoma
8. could also be aspiration with the patient lying down on the right side
11. dell"le le'aat wfth mttllto cough, 'igas of hype. .... ratioa. Chlamydia
trocMmalis pneumonia
Lung
I. caUSe5-
A. aspiration of oropharyngeal male rial Is MCC: mixed acrobe/anaerobe infection
8. lobar pneumonia
C. hematogenous spread
2. lIi rlnuid level on x-ray
Lung locations wilh aspi ration:
I. standing/s il'ting- poslerobasal segmeDl right lower lobe
2. lyi ng down on back- s uperior segment ri gbt lower lobe (MC site for abscess)
3. lyi ng on right side-
A. ri ght middle lobe
B. posterior segmenl of right upper lobe
4. lyi ng on len side- lingula
PulmoDaryembolus:
I . sou rce- femoral vein
2. pathopbys lology-
A. perfusion defect: increases dead space
B. majoriry of peripheral emboli do nOI infarct the lungs
C. produce mild hypoxemia
3. dinical setting-
A. postpartum
B.
88
4. clio lcal-
A. sudden onset of dyspnea and tachypnea: Me symptom and sign. respectively
B. fever
C. pleuritic chest pain
S. lab-
A. perfusion scan first step in work-up
B. respiratory alkalosis
C. mild hypoxemia
D. increased A-a gradient
E. pulmonary angiogram gold standard for Ox.
6. 118MLE e a ~ gross photo of a large saddle embolus in a patient on prolonged bed rest;
usuall y die of acute right heart strain
Pulmonary hyperlension:
I. causes-
2.
l .
A. chronic hypoxemia:
(1) hypoxemia vasoconstricts pulmonary vessels and vasodiJates peripheral vessels
(2) high altitude residents
(3) chronic lung disease
B. loss of pulmonary vasculature: e.g.,
(I ) COPD
(2) restrictive lung diseases
C. left to right shunts with eventual volume overload of ri ght hean
D. mitral stenosis with backup of blood into pulmonary veins
patbology-
A. atherosclerosis of pulmonary arteries
B. smooth muscle hypertrophy of pulmonary vessels
C. angiomatoid lesions
clinieal- ,
A. accentuated P
2
8. cor pulmonale:
(1) pulmonary hypertension (PH) leads 10 ri ghl ventricular hypertrophy
(2) definiti on applies to primary PH of pulmono.f)' Ilrlel)' or PH due to lung disease
(3) does not apply to PH and RVH of cardiac origin of primary origin
a. e.g., mitral stenosis
b. left to ri ght shunts
C. primary PH occurs mainly in youne women: progressive dyspnea, chesl pain.
syncopal e p i ~ e s
D. pruning of pulmonary arteries noted on x-ray
Immotlle cilia syndrome (Kartagener's syndrome):
1. abse_DI dynein arm in cilia
2. dinical-
A. situs inversus:
(1) vessels and chamber in the hean are Slill nonnal (USMIZ)
(2) not a complete transposition
B. infenility in males/females
C. bronchiectasis
D. sinus infections
89
Restrictive lung diseues:
I. decreased compliance and increaJed elasticit)' due to Interstidal fibrosis
2. tau es-
A. pneumoconioses MeC: dust borne diseases
B. sarcoidosis
C. hypersensitivity lung diseases
O. drugs: see Environmental pathology notes
J. coal worker's pneumoconio5is-
A. exposure to coal dust
O. "black lung" disease
C. increased Incidence af TS but not cancer
D. Caplan syndrome: rheumatoid nodules in lungs + coal worker's pneumoconiosis
4. !'I ilicosi!'l-
A. exposure to s ilica dust: e.g., sandblaster
B. nodular, fibrotic masses in the lungs: filled with silicA crystals
C. increased risk for TB but not cancer
O. association with Caplan's syndrome
S. as bes losls-
A. exposure: to asbestos:
( I ) pipe finer in shipyard
(2) roofer for over 20 ys
8. no risk for TB
C. smoker + asbestos exposure predisposes to primary lung cancer > mesothelioma
D. non-smoker + asbestos exposure predisposes to primlll)' lung cancer > mesothelioma
E. asbestos body (ferruginous body) looks like a dumbbell (fiber covered by iron)
6. bypersensitivi ty pneumonilis-
A. farmer'S lung:
( I) inhalation of thermophilic actinomycetes
(2) see Immunopathology notes
B. silo filler 's: inhalation of nitrogen di oxide fumes
C. byss inosis:
(1) "Monday morning blues"
(2) patient works in a te:<tile factory and has contaci with cOllon. linen. hemp
7. lIumman Rich lung-
A. honeycomb lung
B. end-stage of alveolitis syndromes: interstitial pneumon itis syndromes- e.g., usual
internitial pneumonitis
8. sarcoidos ls-
A. ..&DllJuJomatous disease of unknown etiology
B. primarily targets noncasealing granulomas in hilar nodes and parenchyma
C. uveitis with blurry vision )
D. salivary gland enla'l!,men\:.d<.t<h j , S
E. MCC of hepatitis
F. nodules in skin contain granulomas
G. la b:
(1) increase in angiotensin converting enzyme
(2) anergy to common antigens
(3) low CD. T helper cell counts- used up in produci ng granulomas
90
(4) hypercalcemia
Obstructi ve lung dinuc:
I . types-
A. chronic bronchitis:
( I ) MC Iype
(2) clinical Dx.- productive cough > 3 mths for 2 consecutive yrs
B. emphysema
C. bronchial asthma
D. bronchiectasis
2 . .s umman ' c b
b b
art COmpanD}! C rORlc
h" . h
rone IUS w ll h empt vsemu-
Parametl!r Empb\'sema Cbronic Bronchitis
Onset of dyspnea
Progressive. constant. severe Imerminent and often exacerbates
with infection
Sputum production Scanl Increased and purulent
Appearance
" Pink puffer" (not cyanotic), thin, "Blue bloater" (cyanotic due 1O
weight loss respiratory acidosis). obese
AP diameter
increased (hyperinflation) Less hyperinflati on than emphysema
Breath sounds
Diminished to hyperinflation Wheezes and sibilant rhonchi
PaD,
Mild hvpoxemia at rest- Moderate to severe hYPOxemia
PaCO, Normal 10 low (respiratory Increased owing 1O respiratory
alkalosis. reason for "pink puffer")
acidosis- trap C02 behind tenninal
bronchioles filled with mucous
Totallunfl capacitY Markedly increased Nonnal to slighlly incrt3SCd
Residual volume Markedly increased Mildlv increased
I Cor pulmonale
Infrequent untillal'e in the disease Commonl y present
Vent"illltionlperfu- Matched losses of ventilation (resp- Major mismatch owi ng to primary
sion iratory unit ) Ilnd perfusion (loss of involvement of the tenninal bronch
capillary bed) iole (prox..imal lo the respiratory uni!.
hence more units are affected)
J . types or
A. emphysema involves
(I) respiratory bronchiole '
(2) alveolar duct
(3) alveo,:Ii::-:=:-;:::==,
B ... ccnlrilobular emphysema:
( I)
(2) destruction of elastic tissue suppon in the respiratory bronchiole
(3) EEper involved
C. *" panllcinar emphysema:
(1) a.-I antitrypsin (AAT) deficiency
D. primary AR disease
b. in smakw;: chemicals in smoke inactivllie AA T
(2) involves the enlire res irarorv unit (respiratory bronchiole. alveolar du;:t, and
alveoli)
(3) lower lobe disease
D. IlMLE ..... rIo:
( I) identify x-ray of a patient with emphysema
(2) look for increased AP diameter and
91
4. bronchiectasis-
A. cystic nbrosis is the MCC in the- United States: TB is the MCC in third world
countries
B. pathogenesis:
( 1)
(2) broDcbi extend to the lUll!!, periphe'l'
C. clinical : cough up cupfuls of foul smelling sputum
5. bronchial asthma-
A. MC chronic respiratory disease in children
B. episodic, hyperreactive, reversible, small airway disease that primarily targets the
temlinal bronchioles
C. causes:
D.
E.
(I) exposure to allergens
. MeC
b. IgE-mediated type I hypersensitivity
(2) non-immunologic
a. aspirinfNSAID sensi ti vity
b. cold temperature
c. exercise
d.
clinical :
environmental pollutants
smoke
(I) epi sodic wheezing
(2) nocturnal cough
(3) increased AP due to air trapping
lab findings: l:" ...... d l't )
(1) respiratory may progress inlo respiratory acidosis if bronchospasm
(2)
(3)
(4)
(5)
Rx:
(1)
(2)
"fs nol relieved
hypoxemia
decreased FEV fltt values
eosinophilia
positive skin tests for allergens
albuterol medihaler for mild disease
corticosteroid medihaler for moderate to severe disease
Lung cancer:
1. cause!-
2.
3.
A. see neoplasia
B. decreasing incidence in men/i ncreasing incidence in women
C. 2nd MC cancer in men and women
D. MCC of death due to cancer in men and women
MC primary cancers in descending order-
A. adenocarcinoma
B. squamous carcinoma: ectopically secrete PTH-like peptide (hypercalcemia)
C. small cell carcinoma: ectopicall y secrete ACTH (eel'opic Cushings) and ADH (SiADl:I)
MC cancers of lung- metastasis:
A. breast MCC
B. renal adenocarcinoma
92
C. choriocarcinoma
D. colorectal cancers
... lung sites-
A. centrally located:
( I) squamous cell
(2) ,mall cell
8 . peripherally located: adenocarcinoma
S. smoking rehllionsbips-
A. squamous and small cell cancers: strongest relationship
n. adenocarcinoma:
(I ) Me primary lung cancer in smokers and non-smokers
(2) bronchioloalveolo.T carci noma has no smoking relationship
6. eliniclll -
A. cougb Me symptom
o. weight loss
C. hemoptysis: someti mes massive
D. Pancoast tumor (superior sulcus tumor):
(1) squamous cancer at lung npc:( involvi ng brachial plexus and superior cervical
ganglion (Homer's syndrome)
(2) includes ips ilatcrallid Illg. miosjs. anhvdr sis
E. superior vcna caval syndrome r /
F. clubbing
1. sites ror melUtasis outside bilar lymph Dodu-
ad",n.I, MCC ,ite f3<.
B. liver -
C. brain ho.v;JP,?/*
O. bone: lytic metastases .. (It;"
8. prognosit- !Sk.'ao "'j
A. best for squamous
8. worst for small cell : usuall y non-opc::rable
9. bronchial carclnoid-
A. low grade malignant APUD tumor
8. cl inical:
(I ) hemoptysis
(2) local metastasis
(3) carci noid syndrome wi thout need to metastasize
r:r lJSMLE 4 ..... boat roofer for l! yean ........ oker for 10 yean: I
I. &rt! alest riJk is for primary IUDg cancer
2. primary lung cancer is more com mOD tban a mesothelioma, ,,'hetber a R.r
3. mHotbelioma-
A. no smoking relationship
8 . asbestos relationship in most cases
C. highly malignant tumor originaling from the pleura
D. takes 20-30 yrs to develop
<r CIWIiCIIq lo .. d II ....... ia tile _k .... uterlo bat III palin. lllvoIvttl III ..... d-o.
collision (USMLE): ruptured esophagus (Boerhaave's syndrome)-
1. Hamman's sign in tbe chesl due to subcuta neous emphysema from air dissecting into
che tiu ue
93
2. other scena rios could be an alcoholic who is recthing or n bulimic who is vomiting
Solita ry coin les ions:
1. causes-
A. MCC is granulo matous disease; e.g .. TB. hist'oplasmosi s
B. most are benign i n patients <35 years old
C. most are malignant in patients >50 years old
O. calcifications and lack of growth are benign reatures
1. bronchial bama rtoma -
A. solimry coin lesion
B. localized overgrowth or cani lage: nol a neoplasm
C. " popcorn type" or configuration on x-ray
Mcdia"Unum:
1. anterior ruedi ustinum Me involved with disease-
A. thymoma Me tumor fo llowed by nodular scleros ing Hodgkin's disease
B. neuroblastoma in children, ganglioneuroma in adu lts Are Me overaH mediastinnl
tumors: located in posterior mediastinum
2. thymus ond myastbenia gravis-
A. J!!y.!l1ic is Me fi ndi ng in thymus; enninal fo llicles composed of B cell s
that s nthcsize: antibodies against acerylcholine receptors
B. thymoma is less common finding: pure RBe aplasia sometimes noted with thymomas
C. thymectomy is sometimes used in R.lo: of myasthenia gravis
3. middle mediastioum- pericardial cyst Me disorder
C'ir Pleural nuid:
I. la b fiodings (hat diSiinguish a transudat e from exudate in pleural nuid-
A. PF protei n/serum prolein ratio >0.5 is exudate
B. PF LDHlserum LOB 0.6 is exudate
C. PF LOH twcrthirds the upper limit of nonnal of the serum LDH is exudate
2. PF uudates-
A. pneumonia MeC
B. pulmonary infarction: hemorrhagic exudate
C. cancer: hemorrhagic exudate
3. PF transudates- congestive heart fai lure MeC
4. PF fiodings in TB- e:<.udate with a lymphocyte dominalll cell count
5. PF with amylase-
A. acute pancreatitis: left-sided pleural effusion
B. Bocrhl18vc ' s syndrome
QaestioDl ..... duria, lb. board revl ... :
In which of the following cl inical scenarios involving patients with lung disease would you expect
pulmonary function studies to exhibit decreased compliance. increased elasticity, and an increased
FEV InJFVC rario?
A. 6 year old child with recurrent respiratory inrections and sleatorrhea
B. 28 year old nonsmoking male with bilateral lower lobe emphysema
C. 56 year old smoker with productive cough, dyspnea, and cyanosis
D. 10 year old girl with bronchial asthma requi ring systemic steroids
E. 39 year old dyspneic African American with bilateral hUar nodes
94
E (sarcoidosis. restrictive lung disease)
CiI'"
A
CiI'"
E
A 45-year old woman 24 hours post-cholecystecl0my devel ops fever and dyspnea. Physical exam
revellis decreased percussion, increased tactile fremilus. and decreased breath sounds in the right
lower lobe. The diaphragm is ele,'ated and there is inspiratory lag on the right side. The patient
MOST LIKELY h .....
A. atelectasis
B. B lung abscess
c. bronchopneumonia
D. a pulmonary infarction
E. :I spontaneous pneumothora.lo:
An afebri le 23-year-old man develops a sudden onset of left-sided, stabbing chest pain with
dyspnea. Physical exam of the left chest reveals hyperresonance to percussion, deviation of the
lrachea to the left. elevation of the diaphragm. decreased tactile frernirus. and decreased breath
sounds. The MOST LlKEL Y diagnosis is ...
A. pleural effusion
B. bronchopneumoni3
C. tension pneumothora.t
D. n pulmonary infarction
E. spontaneous pneumothorax
r:8" A newborn child develops dyspnea., tachypnea, intercostal muscle retractions. and cyanosis 4 hours
after binh. The mother developed gestational diabetes mell itus and was in poor glycemic control
throu8hout the pregnancy. A chest x-ray reveals a "ground glass" appearance in both lungs. The
primary mechanism for this patient's respiratory problem is ...
A. aspiration of amniotic fluid
B. group B Slrl!ptococcus pneumonia
C. decreased production of surfactant
D. Chlamydia trachomaris pneumonia
E. heart failure from congenital heart disease
C (RDS)
Which of the fo llowing describes 8 pneumonia due to MycoplllSf1/n pneumoniae rather than
Streptococcus pneumoniae?
A. High fever
B. Insidious onset
C. Productive cough
D. lncreased tactile fremitus
E. Neutrophilic leukocytosis
B (all other choices are those ofrypical pneumonia)
CiI'"
A 58-year-old smoker presents with weight loss and cough. Physical eum reveals a mild lid lag on
the left and a pinpoint pupil, scanered sibilant rhonchi throughout all lung fields that clear with
coughing, and an increased anteroposterior diameter. Based on these findinl!$. you suspect the
patient has ...
A. a Pancoast rumor
B. a thoracic outlet syndrome
C. the superior vena caval syndrome
D. obstructive lung disease without pri mary cancer
E. obstructive lung disease with metastatic cancer from another primary site
95
A (Homer's syndrome also present)
<Jf"
A 6S year old man wilh urinary retention secondary to prostatic hyperplasia. develops spiking
fever. and tachypnea. Physical exam reveals intercostal muscle retractions and bilateral inspiratory
crackles. A chest exhibits bilateraJ interstitial and alveolar infi ltrates. ABGs demonstrate
severe hypoxemia. You expect the blood cuhure reveals ...
A. gram positi ve diplococci
B. grum negative diplococ.ci
C. gram positive cocci
D. gram negative rods
E. grnm positive rods
o (Gram negative sepsis due to E. coli [gram negat'ive rod1 into an AROS)
<Jf"
Inspirotory stridor is commonly associated with ...
A. a respirOlory syncytial virus infection
B. 3 parainfluenza vi rus infection
C. aspirin induced asthma
D. rhi novirus infections
E. choanal atresia
8 (croup or laryngotracheobronchitis due to parainfluenza vi rus, obstruction is in the trachea, "steeple"
sign on lateral xray of neck)
r.r Chlamydia trachoma!is and the respiratory syncytial virus are BOTH commonly with .. .
A. an interslitinllype of pneumonia
B. laryngotr8chcobronchilis (croup)
C. the respiratory distress syndrome
D. typical community-acquired pneumonia
E. (nosocomial) pneumonia
A (RSV MeC of pneumonia Ilnd bronchiolitis in chilrlrf!n)
<Jf"
Which of Ihe foll owing is more often associated with Klebsiella pneltmoniae than P5eudomoIJa5
aerugi"osa?
A. Upper lobe cavitarion
B. sputum
C. Assoc iation with cystic fibrosis
D. Association with respirators
E. Productive cough
A (choices B, C. 0 are features of P. aeruginosa, both have producti ve cough fchoice ED
"'"
In a 30 year old man who lives in Tennessee. you would expect a calcified solitary coin lesion in
the lung to represent.. .
A. n foreign body
8. an old granuloma
C. metastatic cllncer
D. a pri mllty lung cancer
E. 3 bronchial hamartoma
B (histoplasmosis)
96
13
1\ 55-ycar-old non-smoking coal \\orker has anhri lis and nodulnr lesions III the lungs His PPO sl..in
le:,1 b. negll li vc. You suspecllhe patient has . ..
A. systemic lupus erythematosus
B. Caplan's syndrome
C mctast.1tic lung disease
D pnmary lung cancer
l: miliar) tuberculosis
In a 6:! year old man who ha) been a roorer for :!5 years and a :,m" l..c:r f(l r 10 ) ears. \\ h,,:h oi Ihe
follO\\ 111 cancc:rs would he be most likel) prone 10 dc\'clopmg7
A 1)lcuralml!sOI hclioma
B. PrimaJ) lung cancer
C Laryngeal carcinoma
D Oral c:mcer
E. Pancrcntic cancer
A fa:.bc:slO$ exposure. same answ\.': r even if hc was not a smoker}
97
Vous aimerez peut-être aussi
- RespiDocument58 pagesRespiIshani PatelPas encore d'évaluation
- Goljan Blue NotesDocument1 pageGoljan Blue NotesCarl NieweldPas encore d'évaluation
- Renal SystemDocument76 pagesRenal SystemDaNy ChiriacPas encore d'évaluation
- UW 2021 Notes - Lungs UsmleDocument422 pagesUW 2021 Notes - Lungs Usmlekathi raja sekhar100% (1)
- 2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksDocument25 pages2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksRushi ShahPas encore d'évaluation
- Embryology: Lung DevelopmentDocument91 pagesEmbryology: Lung DevelopmentPrarthanaPas encore d'évaluation
- UW (Step 1) Renal - Educational Objectives PDFDocument50 pagesUW (Step 1) Renal - Educational Objectives PDFDrbee10Pas encore d'évaluation
- Goljan Step 1 QuestionsDocument3 pagesGoljan Step 1 QuestionsMary0% (1)
- Biochem Genetics USMLE Practice Questions (2 of 4)Document13 pagesBiochem Genetics USMLE Practice Questions (2 of 4)MedSchoolStuff100% (2)
- Medical Student Amnesia USMLE Step 1 - Flash Cards by CueFlashDocument13 pagesMedical Student Amnesia USMLE Step 1 - Flash Cards by CueFlashMuhammad Farhan KhaliqPas encore d'évaluation
- Cell InjuryDocument23 pagesCell InjuryFiori MedPas encore d'évaluation
- Nbme 12 Block 4 Some ExplanationsDocument14 pagesNbme 12 Block 4 Some ExplanationsMuqaddam Ahmed SalimPas encore d'évaluation
- 2 Renal Buzzword ChartDocument6 pages2 Renal Buzzword ChartTyler KingPas encore d'évaluation
- ERRATA 2020 First Aid For The USMLE Step 1Document4 pagesERRATA 2020 First Aid For The USMLE Step 1Rakesh TiwaryPas encore d'évaluation
- NeurologyDocument14 pagesNeurologyMedSchoolStuffPas encore d'évaluation
- NBME 1 BLOCK 1-4 (With Answers)Document204 pagesNBME 1 BLOCK 1-4 (With Answers)Bhuvana UsmlePas encore d'évaluation
- CardiovascularDocument18 pagesCardiovascularMedSchoolStuff100% (1)
- HY SystemsDocument720 pagesHY SystemsYassandra CalderónPas encore d'évaluation
- 'Aliah's Physio NotesDocument30 pages'Aliah's Physio NotesLuqman Al-Bashir FauziPas encore d'évaluation
- Usmle Step 1 Terms ResumeDocument16 pagesUsmle Step 1 Terms ResumeJorge Luis LopezPas encore d'évaluation
- HY GeneticsDocument104 pagesHY Geneticsndifor bonnyPas encore d'évaluation
- Physio 50qDocument70 pagesPhysio 50qAnonymous t5TDwd67% (3)
- General Pathology: Growth AdaptationsDocument93 pagesGeneral Pathology: Growth AdaptationsPrarthanaPas encore d'évaluation
- Goljan Step 1 PDFDocument3 pagesGoljan Step 1 PDFTrey0% (1)
- Goljan Lecture OrderDocument2 pagesGoljan Lecture OrderKweku Grant-AcquahPas encore d'évaluation
- Anatomy High Yield From Usmleworld ForumDocument9 pagesAnatomy High Yield From Usmleworld Forumabe8284Pas encore d'évaluation
- Goljan Respiratory NotesDocument21 pagesGoljan Respiratory Notesmedic2424100% (1)
- DirtyUSMLE Bioethics Video NotesDocument3 pagesDirtyUSMLE Bioethics Video NotesjohntheuglyllamaPas encore d'évaluation
- USmle Radiology 1Document5 pagesUSmle Radiology 1JamesIwuPas encore d'évaluation
- UW Allergy + Immuno - Educational Objectives PDFDocument25 pagesUW Allergy + Immuno - Educational Objectives PDFDrbee10Pas encore d'évaluation
- AMBOSS and RX NotesDocument21 pagesAMBOSS and RX NotesBatool Aldaher100% (1)
- Step1 Journey-To 271Document7 pagesStep1 Journey-To 271Nilay BhattPas encore d'évaluation
- 5 Days To Step 1Document4 pages5 Days To Step 1Deborah PetersPas encore d'évaluation
- NBME Samples Qs - PathologyDocument7 pagesNBME Samples Qs - PathologyAli AlshehhiPas encore d'évaluation
- DO Student Write Up 265 780Document3 pagesDO Student Write Up 265 780aloverofdancePas encore d'évaluation
- Clinical SignsDocument26 pagesClinical SignswiraandiniPas encore d'évaluation
- Nbme 22 NotesDocument1 pageNbme 22 NotesGeovy YépezPas encore d'évaluation
- Chromosome Abnormalities Flash CardsDocument3 pagesChromosome Abnormalities Flash CardsAmirreza ReyPas encore d'évaluation
- Irfan Mir Physiology Usmle Step 1Document37 pagesIrfan Mir Physiology Usmle Step 1sammieahemdPas encore d'évaluation
- Immunology Notes From Uworld, DR-KYDocument16 pagesImmunology Notes From Uworld, DR-KYLayan MohammadPas encore d'évaluation
- IVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesDocument151 pagesIVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesMarc Imhotep Cray, M.D.100% (2)
- High Yields Fact From UWORLDDocument6 pagesHigh Yields Fact From UWORLDBang QuachPas encore d'évaluation
- IVMS USMLE Step 1 Flash Facts Studies Collection GuideDocument3 pagesIVMS USMLE Step 1 Flash Facts Studies Collection GuideMarc Imhotep Cray, M.D.100% (1)
- Goljan High Yield Flash CardsDocument2 pagesGoljan High Yield Flash Cardshabdulhye100% (1)
- Pediatric Pathology: Disease Cause/Risk Factors SymptomsDocument12 pagesPediatric Pathology: Disease Cause/Risk Factors SymptomsherethemindPas encore d'évaluation
- Lippin NotesDocument8 pagesLippin Noteswalt65100% (1)
- USMLE High YieldDocument13 pagesUSMLE High YieldShirkeIncPas encore d'évaluation
- Research Methods Prevalence CensusesDocument6 pagesResearch Methods Prevalence Censusesmoped00100% (1)
- Respiratory: QuestionsDocument18 pagesRespiratory: QuestionskonstanpatPas encore d'évaluation
- El Husseinys Essentials of General PrinciplesDocument92 pagesEl Husseinys Essentials of General PrinciplesSara Alsubaie100% (1)
- USMLE Vignette Flashcards: Micro, Path and Pharm - SidebysideDocument18 pagesUSMLE Vignette Flashcards: Micro, Path and Pharm - SidebysideMedSchoolStuffPas encore d'évaluation
- Nbme 7 Block 3 AnswersDocument20 pagesNbme 7 Block 3 AnswersVictoria Blentiran100% (2)
- Backup of Goljan TransciptsDocument178 pagesBackup of Goljan TransciptsSarah RyanPas encore d'évaluation
- DIT QuestionsDocument183 pagesDIT QuestionsJake ChuengPas encore d'évaluation
- NEUROLOGY Goljan FootnotesDocument10 pagesNEUROLOGY Goljan FootnotesPrince DuPas encore d'évaluation
- Master The Boards Usmle Step 2 CK ErrataDocument1 pageMaster The Boards Usmle Step 2 CK Erratausmle2014success0% (1)
- Actinic KeratosisDocument19 pagesActinic Keratosisattydoc1234Pas encore d'évaluation
- Blank Patient Note For Step2csDocument1 pageBlank Patient Note For Step2csbobiomePas encore d'évaluation
- Nbme 1Document39 pagesNbme 1rockPas encore d'évaluation
- Sharma USMLE Study ScheduleDocument10 pagesSharma USMLE Study SchedulebobiomePas encore d'évaluation
- Pharmacology - Antimicrobial Flash CardsDocument32 pagesPharmacology - Antimicrobial Flash CardsbobiomePas encore d'évaluation
- Pharmacology Pharmacokinetics Flash CardsDocument17 pagesPharmacology Pharmacokinetics Flash Cardsbobiome100% (1)
- Step 1 Physiology Flash CardsDocument22 pagesStep 1 Physiology Flash CardsbobiomePas encore d'évaluation
- High-Yield Behavioral Science 2nd EdDocument121 pagesHigh-Yield Behavioral Science 2nd Edbobiome100% (2)
- Genius 7 On Bill Acceptor ManualDocument10 pagesGenius 7 On Bill Acceptor ManualJose Maria PerezPas encore d'évaluation
- Endovascular Skills CourseDocument20 pagesEndovascular Skills CourseAbdullah JibawiPas encore d'évaluation
- CPHQ Text BookDocument20 pagesCPHQ Text BookCphq Cphq Ali100% (2)
- Qualification Handbook v1-1Document92 pagesQualification Handbook v1-1rafael espinosa semperPas encore d'évaluation
- Stern TubesDocument8 pagesStern Tubesweesweekwee8652Pas encore d'évaluation
- API 16C ErrataDocument1 pageAPI 16C ErrataDinesh KumarPas encore d'évaluation
- The Assignment Vol.4 - The Pain - Mike Murdock PDFDocument168 pagesThe Assignment Vol.4 - The Pain - Mike Murdock PDFEmmanuel Temiloluwa67% (3)
- PNOZ E1vp EN-23-27Document5 pagesPNOZ E1vp EN-23-27Rachid MoussaouiPas encore d'évaluation
- Grades 4-10: Search Jobs in IndiaDocument2 pagesGrades 4-10: Search Jobs in IndiaMD AKIL AHMEDPas encore d'évaluation
- Flock MenuDocument5 pagesFlock MenuWilson TayPas encore d'évaluation
- Gardobond 24d Imu Sds Ver1Document6 pagesGardobond 24d Imu Sds Ver1stuart3962Pas encore d'évaluation
- ISO 9001 Required DocumentationDocument3 pagesISO 9001 Required Documentationdnmule100% (1)
- DICGC - For Depositors - A Guide To Deposit InsuranceDocument10 pagesDICGC - For Depositors - A Guide To Deposit InsuranceSachinPas encore d'évaluation
- 06 - Flexible Operation of Thermal Power Plants - OEM Perspective and Experiences PDFDocument22 pages06 - Flexible Operation of Thermal Power Plants - OEM Perspective and Experiences PDFRavishankarPas encore d'évaluation
- Quorum Sensing PDFDocument9 pagesQuorum Sensing PDFShareenMuneebPas encore d'évaluation
- Jurnal Kasus Etikolegal Dalam Praktik KebidananDocument13 pagesJurnal Kasus Etikolegal Dalam Praktik KebidananErni AnggiePas encore d'évaluation
- Polycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentDocument19 pagesPolycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentAkshay HarekarPas encore d'évaluation
- Lesson 5: Prejudice and StereotypesDocument31 pagesLesson 5: Prejudice and StereotypesZeynep SulaimankulovaPas encore d'évaluation
- 432.01 Managing HSE in A Geophysical Nov 2017Document138 pages432.01 Managing HSE in A Geophysical Nov 2017Andrei Savu100% (1)
- Full Download Book Microbiome Immunity Digestive Health and Nutrition Epidemiology Pathophysiology Prevention and Treatment PDFDocument41 pagesFull Download Book Microbiome Immunity Digestive Health and Nutrition Epidemiology Pathophysiology Prevention and Treatment PDFmildred.walker324100% (15)
- Modelling The Effects of Condensate Banking On High CGR ReservoirsDocument11 pagesModelling The Effects of Condensate Banking On High CGR ReservoirslikpataPas encore d'évaluation
- Tutorials 2016Document54 pagesTutorials 2016Mankush Jain100% (1)
- InvoiceDocument1 pageInvoicesunil sharmaPas encore d'évaluation
- Zook Rupture Disc URADocument2 pagesZook Rupture Disc URAmd_taheriPas encore d'évaluation
- Testing For Cations Flow ChartDocument2 pagesTesting For Cations Flow Chartapi-252561013Pas encore d'évaluation
- AT-502 - AT-504 - OM-0-Introduction-1 - 10-12-2019Document6 pagesAT-502 - AT-504 - OM-0-Introduction-1 - 10-12-2019Vinicius RodriguesPas encore d'évaluation
- Premium Connections Catalogue ENGDocument134 pagesPremium Connections Catalogue ENGsubzwarijPas encore d'évaluation
- Bars Performance AppraisalDocument6 pagesBars Performance AppraisalPhillip Miler0% (1)
- Material Safety Data Sheet Roto-Inject FluidDocument5 pagesMaterial Safety Data Sheet Roto-Inject FluidQuintana JosePas encore d'évaluation
- Expository Cause and Effect OUTLINEDocument2 pagesExpository Cause and Effect OUTLINEAutoDefencePas encore d'évaluation
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (170)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Pas encore d'évaluation
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (4)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- To Explain the World: The Discovery of Modern ScienceD'EverandTo Explain the World: The Discovery of Modern ScienceÉvaluation : 3.5 sur 5 étoiles3.5/5 (51)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisD'EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (58)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)