Académique Documents
Professionnel Documents
Culture Documents
Stanford Journal of Public Health Volume 3 Issue 1 Winter 2013
Transféré par
stanfordjphCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Stanford Journal of Public Health Volume 3 Issue 1 Winter 2013
Transféré par
stanfordjphDroits d'auteur :
Formats disponibles
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
Investigation
Emma Makoba
In the Midst of Social Stigma and Violence: A Look at Attacks against Persons with Albinism in Tanzania
Policy
Eileen Mariano
Childhood Obesity: A Growing Epidemic
Experience
Christina Wang
Hepatitis B Eradication: An Unsolved Challenge
Stanford Journal Public Health
An Undergraduate Publication Volume 3 Issue 1 Winter 2013 sjph.stanford.edu
of
Jessie Holtzman Emma Makoba Emily Cheng Christina Wang Gianni Sun Andrew Liao
Editor-in-Chief Editor-in-Chief Internet Marketing Manager Campus Marketing Manager Financial Manager Layout Director
letter from the editors:
Jessie Holtzman and Emma Makoba editors-in-chief Since the Journals founding e would like to extend in 2011, we have had the pleaa warm welcome to the Winter sure of working with dedicated 2012-2013 issue of the Stanford faculty and staff from all corJournal of Public Health, a bian- ners of the campus, including nual undergraduate publication the Stanford Office of Commuthat seeks to connect the enthu- nity Health, the Center for Insiastic, widely distributed public novation in Global Health, the health community at Stanford Program in Human Biology, by encouraging scholarly dis- the Haas Center for Public Sercussion of todays most perti- vice, Stanford Service in Global nent public health issues. As the Health, and the Sexual Health journal enters its third year, we Peer Resource Center. We would are thrilled by the growing inter- like to acknowledge the generest in the public health field at a ous support of The Bingham university that has traditionally Fund for Student Innovation in lacked a unified forum through Human Biology and the ASSU which to address this topic. We Publications Board. feel that this journal fosters the During a recent lecture, Dean spirit of Stanford University in Lloyd Minor of the Stanford its innovative, academic, and in- University School of Medicine terdisciplinary efforts. proposed three basic tenets of
research review
Jennifer Jenks Liz Melton
experience
Lauren Nguyen Madeleine Kane
policy
Jean Guo
investigation
Caroline Zhang Charlotte Greenbaum
graphics
Judith Shanika Pelpola
innovation: combination, collaboration, and chance. Public health is an interdisciplinary field that combines economics, medicine, biology, and public policy. It requires the collaboration of experts across disciplinary and departmental boundaries to provide a robust analysis of a given research question. Yet, Minor argued that, even together, we can only do so much until we open ourselves to the unexpected. By drawing on many different approaches to public health, the Journal hopes to promote the unexpected and encourage the spark of chance. May you encounter new ideas and perspectives as you read this latest issue. Warmly, Jessie Holtzman 14 Emma Makoba 14
writers
Christina Wang Yifei Men Eileen Mariano Judith Shanika Pelpola
with support from
The Bingham Fund for Student Innovation in Human Biology ASSU Publications Board Haas Center for Public Service
HOLTZMAN
Jessie is a Human Biology major with a concentration in the cellular basis of human disease, combining her passions for policy and the natural sciences. She hopes to use her biology background, along with her interest in womens and childrens health, to develop effective policy solutions to growing local, national, and international health disparities. Through the Journal, she looks forward to spreading awareness of public health topics and proposing new, innovative, interdisciplinary ways to address such dilemmas. Emma is an Anthropology major with a concentration in Medical Anthropology and a Human Biology minor. She will attend medical school at Mount Sinai School of Medicine in New York through the Humanities and Medicine Early Acceptance Program. She is interested in exploring the important cultural considerations necessary to improve patient and doctor interactions both in one-on-one clinical settings and in the implementation of broader public health initiatives.
Cover photo courtesy of Jessie Holtzman
Logo courtesy of Kiran Malladi Stanford Journal of Public Health
MAKOBA
Volume 3 Issue 1 Winter 2013
letters from the advisors
contents
Investigation
Public Health Interventions in the Midst of Social Stigma and Violence: A Look at Attacks against Persons with Albinism in Tanzania............................................................... Emma Makoba The Parkinsons Voice Initiative: Early Diagnosis for Parkinsons Disease through Speech Recognition................................................ Yifei Men
Catherine A. Heaney, PhD, MPH Associate Professor (Teaching) Stanford Prevention Research Center
Policy
in print. As always, the Journal is dedicated both to providing an outlet for undergraduates to publish their research and perspectives on public health issues and to bringing important contemporary issues in public health to the wider undergraduate community. As the Journal continues to grow, it has now merged with Stanford Service in Global Health, and in doing so it has added a new Experience section. Because many students wish to pursue professional and programmatic roles in public health as well as scholarly ones, this new section is dedicated to creating a forum for students to share their own personal on-the-ground experiences. The Journal thanks you for your ongoing interest and support.
Grant Miller, PhD, MPP Associate Professor of Medicine; Associate Professor, by courtesy, of Economics and of Health Research and Policy and CHP/PCOR Core Faculty Member
I am delighted to see this academic years first issue of the Stanford Journal of Public Health appear
Childhood Obesity: A Growing Epidemic........................................................................................... Eileen Mariano
13 15
Medi-Cal 2016: What Obamacare Means for California Patients.................................................... Judith Shanika Pelpola
Experience
The Ethics of Striking: A Public Health Concern................................................................................ Jessie Holtzman Hepatitis B Eradication: An Unsolved Challenge............................................................................... Christina Wang
18 20
Research Review
Polio Eradication in India: Lessons for Pakistan?.............................................................................. Ravi Patel
Amy Lockwood Deputy Director Stanford University Center for Innovation in Global Health
23
Infertility: A Plague Gone Unnoticed.................................................................................................. Nitya Rajeshuni
27 33 38
Can Schools Prevent the Next Pandemic: A Study of School-located Influenza Vaccination in Metro Atlanta, Georgia...................................... Julia Brownell
IVF Coverage: A Policy and Cost Conundrum................................................................................... Elizabeth Melton
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
Public Health Interventions in the Midst of Social Stigma and Violence
The
section of the SJPH presents and analyzes pressing public health issues through the lens of epidemiological, medical, and scientific perspectives.
investigation
In this issue, we investigate critical advances in computational technology available to aid in the diagnosis of chronic, degenerative diseases like Parkinsons disease and explore the background and consequences of attacks against individuals with Albinism in Tanzinia.
Photo Courtesy of Emma Makoba This is a photo of a higher security elementary school located in Bukoba, Tanzania where many children with albinism from different parts of the region were moved to in order to ensure their safety.
A Look at Attacks against Persons with Albinism in Tanzania
recent years, a disturbing phenomenon of the systematic killings of persons with albinism in certain parts of East Africa has been documented by both academics and the global media. The motivation behind these attacks in parts of Tanzania involves a highly complex system of social tensions that have erupted in violence against children and adults who have this genetic condition. FurtherVolume 3 Issue 1 Winter 2013
In
Emma Makoba
more, the practice continues today because the limbs and body parts of persons with albinism can be sold at prices ranging from US $500-2000 on the black market. In addition, there is overt discrimination against persons with albinism due to widespread and persistent misunderstanding and misinformation about albinism. This situation serves as an important and tragic example of the need for public health interventions to help improve and protect the lives of innocent but stigmatized and marginalized groups of individuals. More specifically, in regions where persons with albinism have faced violence, they endure not only many health problems resulting from the disease itself such as vision impairment and high susceptibility to skin cancer, but they also suffer life threatening injuries as a re-
Stanford Journal of Public Health
Photo Courtesy of Emma Makoba Pictured is a young boy who was attacked and mutilated by individuals seeking to sell his limbs on the black market for sizable cash rewards.
sult of attacks and often require physical therapy, rehabilitation, and prosthetics if they suffer loss of limbs. Yet, difficulties remain to ensure that persons with albinism have access to the necessary health and rehabilitation services because of both a lack of health infrastructure, as well as the persistent and severe stigma and threats against them. There is an unusually high incidence of occultocutaneous albinism type II, the most severe and the most common type of albinism in Sub-Saharan Africa. The cause for this condition is largely unknown. It is defined biomedically as a genetic condition that causes the defective production of melanin resulting in the lack of pigmentation in the skin, hair, and eyes, vision prob-
lems, and a high susceptibility to skin cancer.1 In Tanzania, it is estimated that the number of persons with albinism ranges between 8,000 and as many as 170,000 individuals in a population of 45 million. If the higher end of the estimation is to be believed, this would make the rate of albinism in Tanzania, approximately one in three thousand as opposed to one in twenty thousand [in] Europe and North America.2 The high concentration of murders and attacks on persons with albinism primarily in northwestern regions of Tanzania began in early 2007. As many as 54 individuals were killed within two years; and to date, a total of 71 murders have been documented.2 Many more
persons with albinism were left disabled due to the attempted dismemberment of their bodies. It must be noted that the actual number of persons with albinism killed and attacked during this time span may never be accurately known and is likely much higher, due to the lack of reporting and documentation in many rural regions of the country. The attacks took place primarily in a particular region of northwestern Tanzania referred to as Sukumaland, in the areas surrounding the cities of Mwanza and Shinyanga. According to Deborah Fahy Brycesons article Miners Magic: Artisanal Mining, the Albino Fetish and Murder in Tanzania, the killings of persons with albinism in this region, are said to trace back to myths perpetuated by witchdoctors, referred to as waganga in Swahili.3 The myth that was disseminated and perpetuated by the waganga is that the body parts of persons with albinism can be used to make a potion which when consumed or bathed in, will bring an individual wealth, luck and success.3 However, many other myths surround persons with albinism, such as the idea they are ghosts, sub-human, immortal, or that their condition is contagious. The physical symptoms of albinism take on a social function in that they set them apart from others within the population that do not share the physical symptoms of the genetic condition. Furthermore, because of their susceptibility to skin cancer, many persons with albinism avoid sunshine, and are thus seen as weak and sedentary in a social context that often deStanford Journal of Public Health
mands hard physical labor in either the dominant mining industry or the agricultural fields in the area. Albinism is not just a genetic disease, but also a socially constructed illness experience in which individuals afflicted are highly stigmatized, dehumanized, discriminated against, and hunted. The persons with albinism do not only endure the physical symptoms of a lack of pigmentation, visual impairment, and increased risk of skin cancer, but they also live in continual fear for their lives because of socially constructed beliefs
that their body parts bring about good luck. Furthermore, having a child with albinism can cause a family to fear for the childs life, seek out ways to keep the child safe, ostracize, or kill the child because the risk may be too great or the family may see the child as not human. Persons with albinism may be deprived of education or job opportunities because of the falsely held belief that their condition is contagious. Children may be forced to stay home from school because leaving the house would put them in jeopardy from people who could potentially attack
and dismember them. Once the complexities of the practice of murdering and attacking persons with albinism in the Sukuma context is understood, it becomes clear the extent to which persons with albinism are victimized. This, in turn, provides a better context to comprehend and address other difficulties that persons with albinism face and how a public health intervention to improve the lives of persons with albinism in this context must take into account the degree to which their health needs are neglected because of social stigmatization.
To find references for this article, please refer to the end of this section.
The Parkinsons Voice Initiative: Early Diagnosis for Parkinsons Disease through Speech Recognition
Yifei Men
arkinsons disease is the second most common neurodegenerative disease, affecting 6.2 million people globally.4 It is most prevalent in the elderly, though 5-10% of diagnoses reflect early-onset Parkinsons disease. For some individuals, symptoms may begin as early as age 20.4 Early warning signs of Parkinsons disease usually involve impairment of movement, including uncontrollable shaking, rigidity, difficulty walking, and unsteady gait. As the disease progresses, cognitive and behavioral complications may arise, commonly leading to dementia.5 There are currently no cures for Parkinsons disease, and the Volume 3 Issue 1 Winter 2013
exact mechanisms leading to the loss of brain cells observed in patients are largely open to debate. Medications, surgery, and multi-disciplinary treatment, however, are widely adopted for relief of disease symptoms. Drugs are especially effective in delaying degeneration of motor functions. For instance, the average time between initial disease onset and complete dependency on care-givers increases from 8 years without treatment to 15 years with regular usage of a single drug, Levodopa.6 However, pharmacological interventions must be initiated in early stages of disease in order to be efficient, as motor symptoms progress aggressively in the early stages if left untreated, leading to irre-
versible disabilities. Effective treatment and early diagnosis for Parkinsons disease are hindered by a lack of quantifiable biomarkers and objective measures of disease progression. As there are no diagnostic lab tests available for Parkinsons disease, the current goldstandard for diagnosis relies on an in-clinic neurological test and brain scans to rule out other
Photo Courtesy of ParkinsonsVoice.org PVI: A new model for diagnosis of Parkinsons based on speech recognition and machine learning technologies.
neurological causes of symptoms.4 This process is extremely costly and requires a high level of expertise, placing stress on existing medical infrastructure. With improving life expectancies in developing countries and an aging population in many developed countries, early and accurate diagnosis of Parkinsons disease will undoubtedly pose an increasing challenge for healthcare systems. Researchers have proposed a new model for diagnosis of Parkinsons based on speech recognition and machine learning technologies. Introduced by Dr. Max Little, Chairman of Parkinsons Voice Initiative, this approach requires only a single sound recording of sustained phonation (saying aaah) from patients. Voice processing tools subsequently analyze the sound recordings and compare them to a database of recordings of Parkinsons patients and nonParkinsons patients that serve as a control. The algorithm developed by this research team is able to detect specific variations in sound vibrations linked to vocal tremors, breathlessness, and weakness. By detecting such voice changes that are indicative
of neurological degeneration, the algorithm is able to generate accurate diagnoses and predict disease progression based on the presence and severity of such degenerative symptoms.7 Although the project is still in the early stages of development, preliminary results are promising; the team claims a 99% success rate in positive diagnoses of Parkinsons disease.8 Accuracy aside, the proposed modality of diagnosis has significant benefits over conventional analytical methods. The research team has not published exact cost estimates, but the method is predicted to be ultralow-cost once it is marketed and fully operational. As the process of analysis is computerized, no medical professionals or additional administration are required for analysis and final diagnosis. This approach is thus very attractive to areas with lessdeveloped medical infrastructure. Speech-based tests can also be easily scaled-up in response to higher demands by increasing computational capacities. Since voice recordings can be readily obtained and transferred using existing telecommunication systems, remote diagnosis
is also possible, increasing access to rural areas or regions with poor healthcare programs. Remote testing also makes largescale screening feasible in areas without the capacity to support high numbers of clinical consultations. Experts suggest that voicebased diagnosis will likely improve early intervention and management of Parkinsons disease. Scientists have long suggested that voice degeneration may be one of the first detectable symptoms of Parkinsons disease.10 Detection of voice changes in Parkinsons disease patients would make it possible for earlier intervention before the onset of disabling physical symptoms. Treatments in the early stages of the disease are critical to delay further aggressive and irreversible neurological degeneration. Voice changes may also serve as an easily assessable and objective proxy to determine disease severity and monitor early trajectories of disease progression. Disease progression is routinely monitored using the 176-point Unified Parkinsons Disease Rating Scale (UPDRS),9 in which patients are scored in categories such as mood, behavior, mo-
tor skills, and ability to carry out daily tasks. However, this assessment requires long interviews and necessitates frequent clinical visits. Although speech tests will not be able to fully capture the degree of physical and mental disability assayed by the UPDRS, they may serve as a proxy to reduce the number of clinical visits and become a lowcost alternative to the UPDRS in resource-scarce regions. While the project holds great promise, it still faces many challenges. Current studies make use of high-quality sound recordings collected in laboratory settings. Although the algorithm remains Photo Courtesy of iStockPhoto.com robust when laboratory-recordThe diagnosis of Parkinsons disease may soon be just a phone call away. ed clips are distorted artificially, it is considerably more difficult initiative has already garnered cal infrastructure or access to to filter out ambient noises that more than half of its target of well-trained professionals. The development of this initiative may confound performance.8 10,000 recordings to date.7 The Parkinsons Voice Initia- also reflects a greater movement The Parkinsons Voice Initiative is currently pooling clips of tive is a promising new approach of data-driven medicine, where phonations sent in by volunteers to facilitate effective early diag- advancements in computational around the globe to build a more nosis of Parkinsons disease. The technology are becoming indisextensive database and formu- cost and capabilities of the initia- pensable in formulating effeclate more precise algorithms for tive are particularly attractive to tive diagnostic and management diagnosis and prediction. The regions without a strong medi- protocols in medical settings. 1. Makulilo, Ernest Boniface. Ablino Killings in Tanzania: Witchcraft and Racism? M.A Thesis, Department of Peace and Justice Studies, University of San Diego; 2010. 2. Kiprono, Samons Kimaiyo, ed. Quality of LIfe and People with Albinism in Tanzania: More than Only a Loss of Pigment. Scientific Reports; 2012: 1-6. 3. Bryceson, D.F, ed. Miners Magic: Artisanal Mining, the Albino Fetish and Murder in Tanzania. The Journal of Modern African Studies; 2010 48(3): 354-382. References for The Parkinsons Voice Initiative article
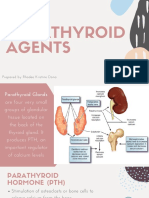
Graphic Illustration by Judith Shanika Pelpola
10
Stanford Journal of Public Health
4. de Lau LM, Breteler MM. Epidemiology of Parkinsons disease. Lancet Neurol. June 2006; 5 (6): 52535 5. Jankovic J. Parkinsons disease: clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry. April 2008; 79 (4): 36876. 6. Raguthu L, Varanese S, Flancbaum L, Tayler E, Di Rocco A. Fava beans and Parkinsons disease: useful natural supplement or useless risk?. Eur. J. Neurol. October 2009; 16 (10): e171 7. Parkinsons Voice Initiative - Science. Available at: http://parkinsonsvoice.org/science.php. Accessed November 13, 2012. 8. A. Tsanas, M.A. Little, P.E. McSharry, J. Spielman, L.O. Ramig. Novel speech signal processing algorithms for highaccuracy classification of Parkinsons disease. IEEE Transactions on Biomedical Engineering. 2012; 59(5):1264-1271. 9. Ramaker, Claudia; Marinus, Johan, Stiggelbout, Anne Margarethe, van Hilten, Bob Johannes. Systematic evaluation of rating scales for impairment and disability in Parkinsons disease. Movement Disorders. September 2002; 17 (5): 867876 10. Hanson, DG, BR Gerratt, and PH Ward. Cinegraphic observations of laryngeal function in Parkinsons disease. Laryngoscope. March 1984; 94 (3): 348-53.
Volume 3 Issue 1 Winter 2013
11
Childhood Obesity: A Growing Epidemic
The SJPH explores the intersection of public health research and innovation and its deployment in the real world. The section approaches health topics at the forefront of scientific debate by integrating legislative, ethical, and economic perspectives. In this issue, the Policy Section explores regulation of public health issues at the state and national levels, investigating the consequences of the Affordable Care Act on Medi-Cal patients and various interventions to address the growing childhood obesity epidemic.
policy
Eileen Mariano
section of the
ven though the HIV virus transferred from monkeys to people in the 1920s, there were eight million people living with the disease by 1990. At that time, with no cures yet definitively proven and a steady climb in the number of diagnoses, HIV/ AIDS appears to be one of the worst epidemics to ever plague the United States. However, at the turn of the 21st Century, yet another problem has taken center stage in the battle for the future health and wellbeing of Americans. Over the past few decades, healthcare professionals have grown increasingly concerned with childhood obesity, an epidemic now affecting an unprecedented proportion of the American population. More than one third of children and adolescents in the United States were overweight or obese in 2008, and that number has not shown any signs of decline.2 3 In fact, since the 1970s, the childhood obesity rate has tripled.4 As a result of this increase, it is estimated that the generation currently in their childhood will be the first in American history to live shorter lives than their parents.5 Healthcare providers worry about obesity because it is closely associated with diabetes. Specifically, Type II diabetes may lead to blindness, hypertension, an increased risk of heart problems, and in extreme cases, Volume 3 Issue 1 Winter 2013
amputation of digits and limbs. For these reasons, obesity and obesity-related illnesses are the leading cause of death in the United States every year, and it is estimated to shorten lives by an average of twelve years.6 Further, the harm of childhood obesity and diabetes transcends the physical symptoms alone. Those who suffer from obesity are also impacted by social discrimination, to the point where individuals have difficulty finding jobs, participating in activities, and even forming desired relationships.7 At a national level, the obesity epidemic has become a national security threat because up to one-quarter of the people trying to join the military are unqualified because of their weight.8 In addition, it is estimated that obesity-related complications cost the United States health care system $344 billion dollars a year.9 What is already being done to combat this growing, harmful trend? Steps are being taken at both the local and national levels. Locally, many propositions and social movements have been enacted. According to Christopher Gardner, Associate Director of Nutrition Studies at the Stanford Prevention Research Center and Associate Professor of Medicine at Stanford University there is room to be optimistic. It is sometimes very difficult to make a big change. So what people have started to do is
play around with little changes, as part of the movement and I think its working, Gardner explained. A few examples of the little changes that Gardner refers to include efforts from New York Citys Mayor Bloomberg, who started an initiative that prohibited the purchase of soda using food stamps in New York10, and Measure N in California, the first proposed soda tax in the country to appear on a ballot.11 In addition, Michigan implemented Double Up Food Bucks, an initiative that gives bonus token rewards when people buy fruits and vegetables from farmers markets12, and the Santa Clara County Toy Ban, which states a toy cannot be sold along with a fast food meal unless the meal meets calorie, fat, salt, and sugar content guidelines. Unfortunately, due to specific restrictions and a limited scope, the ban only affected four restaurants. However, it received national attention and was later implemented by San Francisco and proposed by the state of Kansas. Nationally, the Obama administration has made strong efforts to curtail the epidemic. In January of 2012, President Obama announced that he would add $3.2 billion to the $11 billion school lunch program. The extra support would be used to add more fruits and green vegetables to breakfasts and lunches and reduce the
12
Stanford Journal of Public Health
13
amount of salt and fat. Obamas subsidies also provide the funding for whole grains, lowfat milk, and the technology to monitor the amount of caloric intake per lunch per student.13 Michelle Obama has also played a significant role in the effort to reduce childhood obesity, claiming that she is going to continue to do everything that [she] can to focus [her] energy to keep this issue at the forefront of the discussion in this society.14 Specifically, she established her Lets Move! initiative, which encourages nutritional foods, increased physical activity, and a healthy start for children. The campaign has launched numerous movements, which include paying restaurant chefs to move to schools, awarding subsidies to schools that start a vegetable garden, and initiating a summer food program that allows children to eat healthfully year-round. The First Ladys initiatives have encouraged healthier eating and are influencing student lifestyles all over the country.15 But the question remains, are the current local and national level efforts enough to stop an epidemic? Donald
Medi-Cal 2016: What Obamacare Means for California Patients Judith Shanika Pelpola
edicaid, better known as Medi-Cal in California, will cover a greatly increased number of patients by 2016 as a result of the Affordable Care Act (ACA). Popularly known as Obamacare, this recent healthcare reform has sparked numerous discussions regarding its effect on the already overstretched Medicaid and Medicare systems. California has decided to opt in to the new program established by the ACA, thus ensuring healthcare coverage under Medi-Cal for all individuals with an income below 133% of the federal poverty line. 1 According to the Washington Post, California expects to enroll an additional half a million people in the program by 2014, with that number increasing significantly by 2020. 2 Medi-Cal, like other Medicaid programs across the nation, was originally created for those eligible for welfare, specifically the elderly, the disabled, and single parents with young children. It was set up as a program not for all poor people but for only certain categories of poor people, and it was originally tied to whether you got welfare checks, Don Barr, a professor of Human Biology at Stanford, said. Once a state signed up for the program, it was required to support every person in the above categories. Poor was defined in different ways for each of those Volume 3 Issue 1 Winter 2013
Graphic Illustration by Judith Shanika Pelpola
Barr, Physician and Associate Professor of Sociology and Human Biology at Stanford University, does not think so. He pointed out, if you think its a problem now, its about to be an even bigger one, which is why local, state, and national level government need to increase their efforts, given the severity of the epidemic. To put the anti-childhood obesity efforts into perspective, in 2008, the federal government committed to spending $48
billion over the next five years on HIV/AIDS prevention and treatment efforts. This aid will affect the 1.2 million people living with HIV in the US.16 There are, comparatively, 9 million obese children. Despite the current local and national efforts to reduce childhood obesity, those initiatives are not sufficient. Preventing the expansion of this epidemic is a crucial step toward a healthy future for Americans.
Donald Barr is a physician and an Associate Professor of Sociology and Human biology at Stanford University. He researches a wide variety of topics, one of which is the social and economic factors contributing to health disparities, and specifically to obesity. Christopher Gardner is the Director of Nutrition Studies at the Stanford Prevention Research Center and an Associate Professor of Medicine at Stanford University. He received his PhD from the University of California and now researches dietary intervention and the way that food increases disease risk factors and body weight.
To view the references for this article, please refer to page 43
groups but if you were not in those three groups, even if you were extremely poor, you got zero coverage, explained Barr. Thus many low-income individuals often go without healthcare coverage unless their employers provide it. The federal government partially supports Medi-Cal, basing contributions on the average per capita income in the state. According to the US Department of Health and Human Services, the federal government pays 50% of Medi-Cal costs as of 2012. 3 California covers the remaining 50%, a financial burden that has strained the budget and made it difficult to expand Medi-Cal to other low-income individuals. This affects many other states, though lower-income states receive up to a 75% subsidy of costs from the federal government. By setting an income level of 133% of the federal poverty line, the ACA makes healthcare coverage available for most lowincome people below the specified income level. Currently, the eligible income level in California is around 60% of the federal poverty line, as calculated using Medi-Cal monthly income requirements divided by the poverty line (see 2012 HHS Poverty Guidelines). 4 The Affordable Care Act has said, lets get away from this idea of this being only
for certain categories of poor people; lets make it for all poor people, claimed Barr. In raising the minimum income level, the ACA also eliminates shares of cost for many Medi-Cal and other lower-income patients. The share of cost program applies to those above the minimum income level who still qualify as low income, holding these patients financially responsible for a share of their medical expenses. However, this means that even those who were at 61% of the federal poverty line were forced to pay a share of cost, which is applied before Medi-Cal payment covers the remaining cost of care. 5 With the ACA, any individual or household earning up to 133% of the federal poverty line, currently $15,130 per year for a family of two or $1260 a month, will no longer have to pay healthcare costs. According to the Kaiser Family Foundations summary of the ACA, even those above this line will receive subsidies to help purchase coverage in the private sector. One concern with regard to the ACA is the increase in cost that the program will incur. States like California will continue to cover the cost of patients under the original program, while the federal government will cover all incoming patients for the first few years. By 2020, states will
14
Stanford Journal of Public Health
15
cover 10% of the cost of the new patients, while the federal government covers the remaining 90%. 7 In the long run, the ACA is expected to reduce the federal deficit in part by reducing costs incurred by county hospitals and clinics, which provide uncompensated care for those who do not qualify for Medi-Cal. According to the Milken Institute, California hospitals provided $12 billion in uncompensated care in 2009.8 Uncompensated care is supported only in part by payments from the federal government. In making previously uninsured, low-income patients eligible for Medi-Cal, the ACA ensures that many hospitals and doctors that provide such services will be compensated. All
of a sudden the hospitals and the doctors have a source of payment for these people, clarifies Barr. However, a shortage of doctors and care facilities is expected in places like the Veterans Hospital in Palo Alto, which accept Medi-Cal as payment. According to Barr, this continues to be a very serious problem since Medi-Cal pays doctors less than 70% of what Medi-Care pays, and Medi-Care pays about 80% of what the private market pays. That means its less than half of the usual charges, so lots of doctors just say were not going to take Medi-Cal. This puts strain on community clinics to which Medi-Cal patients turn. According to the New York Times,
the Inland Empire of Southern California has only half of the number of recommended primary care physicians for its population. 10 This is a common concern across California counties. While the ACA provides for roughly 15,000 new doctors in community clinics nationwide, anxiety still remains regarding the number of primary care doctors for newly eligible patients. According to Barr, the question remains regarding the shortage of primary care doctors for new Medi-Cal and Medicaid patients across the country. Thats the issue that is unclearThere are things in the Affordable Care Act to expand community clinic delivery systems and well see if thats going to be adequate.
The
section of the SJPH presents public health challenges that students have encountered personally, highlighting the relevance of such issues to student life on a day-to-day basis. In this issue, our articles explore a range of interests sparked by our writers experiences, from local to international, including the ethics of Spanish healthcare workers striking and the benefits of lobbying legislators to achieve awareness and prevention goals with respect to hepatitis B.
experience
Donald Barr is a physician and an Associate Professor of Sociology and Human biology at Stanford University. He researches a wide variety of topics, one of which is the social and economic factors contributing to health disparities, and specifically to obesity.
1 Compilation of Patient Protection and Affordable Care Act. Available at: http://housedocs.house.gov/energycommerce/ ppacacon.pdf. 2 Kliff, Sarah. Obamacares Medicaid Expansion Already Covering a Half-Million Americans. Washington Post. Available at: http://www.washingtonpost.com/blogs/wonkblog/wp/ 2012/07/03/obamacares-medicaid-expansion-already-covering-a-half-million-americans/. Accessed November 30, 2012. 3 Department of Health and Human Services. Federal Financial Participation in State Assistance Expenditures. Available at: http://aspe.hhs.gov/health/fmap12.shtml. Accessed November 30, 2012. 4 Department of Health and Human Services. 2012 HHS Poverty Guidelines. Available at: http://aspe.hhs.gov/ poverty/12poverty.shtml. Accessed November 30, 2012. 5 California Healthcare Foundation. Share of Cost Medi-Cal. Available at: http://www.chcf.org/ ~/media/MEDIA%20LIBRARY%20Files/PDF/S/PDF%20ShareOfCostMediCal2010.pdf. Accessed November 30, 2012. 7 Kaiser Family Foundation. Summary of Coverage Provisions in the Patient Protection and Affordable Care Act. Available at: http://www.kff.org/healthreform/upload/8023-R.pdf. Accessed November 30, 2012. 8 Milken Institute. Medicaid Expansion May Cripple Californias Burdened Health System. Available at: http://www. milkeninstitute.org/newsroom/newsroom.taf?function= currencyofideas&blogID=523. Accessed November 30, 2012. 9 Lowerey, Annie and Robert Pear. Doctor Shortage Likley to Worsen with Health Law. New York Times. Available at: http://www.nytimes.com/2012/07/29/health/policy/too-few-doctors-in-many-us-communities.html?_r=2&. Accessed on November 30, 2012.
16
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
17
Jessie Holtzman
The Ethics of Striking: A Public Health Concern
healthcare budget in an attempt to revive the floundering economy. Starting in 2000, Spain became an increasingly popular country for immigration due to the generous benefits provided to immigrants. Immigration came with benefits, helping to maintain the population as the countrys growth rate fell to 1.1 children per couple. It came with costs as well, though. The country became a frequent destination for healthcare tourism, with residents of other European Union countries traveling to Spain for its superior healthcare procedures at low costs. As of August 2012, the government no longer provides free healthcare services to undocumented immigrants, and healthcare tourists must reside within Spain for more than three months before receiving free healthcare services.3 Now, the system only provides healthcare to foreigners in cases of grave illness or accident, pregnancy and birth-related care, and to those younger than 18. These changes discourage non-tax-paying residents from using the healthcare system, a worthwhile policy to prevent unfair exploitation of tax-paying citizens. However, further broad cuts to the rest of Spanish society come at a time when Spanish unemployment has climbed to dangerously high levels. Spaniards are paying an increasingly large percentage of their healthcare costs directly, while their salaries are dropping to historically low levels. Retired citizens now contribute a 10 percent copayment toward the costs of medicine, while non-retired citizens pay between 40 and 60 percent copayments, scaled to income level. Citizens now pay for wheelchairs, crutches, and splints, as well as non-urgent transport to hospitals.3 The most controversial element of the recent changes to Spanish public health financing is the Fiscal and Administrative Measures Law, implemented on January 1, 2013. This legislation aims to privatize six major hospitals in Madrid, as well as 27 non-urgent health clinics. In addition, the measure adds a one Euro fixed supplemental charge to the cost of each prescription medication. These proposed changes sparked heated debate, with left-wing deputy Antonio Carmona saying, Privatizing healthcare isnt efficiency; its business. This isnt law; it is a scandal.4 Doctors and nurses went on strike for five weeks before the passage of the law, leading to the cancelation of more than 40,000 patient visits and a 1.74 billion Euro loss in 2012 from work stoppages. Although experts agree that the Spanish public health system needs reform, healthcare workers fear the consequences of these changes. Spanish doctors and nurses see these changes as threatening Stanford Journal of Public Health
late November, more than 75,000 healthcare professionals gathered in Puerta del Sol, in the heart of Madrid, holding signs that read health care cuts kill and public health: not for sale.1 Amidst new austerity measures, these employees were striking to protest a set of cuts particularly worrisome to the public health community. With the Spanish economy in crisis, the conservative government of President Rajoy announced that Spain needed to cut 10 billion Euros of health and education spending each year starting in 2012. Seven billion Euros worth of these cuts are taken from the healthcare budget.2 Spaniards, and specifically members of the healthcare sector, have reacted strongly to this reduction, since it targets a key element of the prized welfare state that developed in the 1970s transition from dictatorship to democracy. While these workers have good intentions and many valid concerns, their strike hurts the patient population rather than targeting the government violating their rights. Instead of striking, doctors and nurses should take up more productive ways of demonstrating dissatisfaction to avoid punishing the patient population for government austerity decisions. With the current state of crisis, the Spanish government must make cuts to its extensive
In
their practices and patients. The healthcare sector claims that it protested not due to a threat to working conditions or privileges, but rather for the right of everyone to have access to quality healthcare. Doctors fear that the changes jeopardize the delicate balance of healthcare expenditure, quality, and benefit in favor of a better business arrangement. They point to claims by government administrators that hospital expenditures per capita will decrease from 600 Euros to approximately 450 Euros.3 Where the measure calls for cuts in treatments with lower proven efficacy, doctors fear that eliminating procedures to save money could reduce quality of care and ease of access. Yet, the extended striking of doctors and nurses, la marea blanca, raises questions about the obligation of health professionals to provide quality healthcare. This essential service sector has a right to negotiate for acceptable working terms, but patients also have a right to expect uninterrupted access to care. The strikes effect of stopping
all non-urgent care challenges the patient-physician contract, which requires that physicians act responsibility and provide continuing care to patients. Doctors have a fundamental obligation to treat their patients to the fullest extent possible, so alternative methods of manifesting dissatisfaction toward the government would be preferable. However, effective non-striking options require fundamental trust between the two parties, which is currently absent in Spain. Historically, Spaniards do not trust the government due to the high levels of corruption and nepotism that lead to concerns about the motives behind government decisions. Nevertheless, given the ethically dubious nature of healthcare professionals striking, the government and the unions must put aside their differences to achieve a feasible level of budgetary cuts in this time of dire economic crisis. The associated doctors of one of the healthcare unions issued a statement saying, We need the patients to know that we do this for them, because
we know the depravity of the systems of incentives in private healthcare. It is a question of responsibility.4 The doctors claim to act out of care for patients rather than interest in their own compensation. Indeed, by striking, union workers accept fines and decreased salaries, in return for calling attention to what they see as unfairly imposed austerity measures. While some patients may agree with the doctors and support the strikes, though, the health care strikes harm the patient population, with the cancelation of thousands of procedures. Striking on behalf of the patient population surely makes a public statement about the dissatisfaction of physicians and nurses, but it also jeopardizes the goal of the public health system to ensure the conditions in which people can be healthy.5 Healthcare workers are essential to society, and as such, their union rights cannot be ignored. Ultimately, a doctors right to strike cannot, and should not, be entirely eliminated. Nevertheless, this does not mean that a strike is the best option.
1. Thousands protest austerity measures in Spain. RT [online]. December 18, 2012. Available at: http://rt.com/ news/spain-union-protest-mass-228. Accessed December 28, 2012. 2. Day, Paul. Spain seeks health care cuts as crisis deepens. Reuters [online]. April 18, 2012. Available at: http://www.reuters.com/article/2012/04/18/us-spain-health-idUSBRE83H0LX20120418. Accessed December 9, 2012. 3. Los recortes sanitarios, uno a uno. El Mundo [online]. April 25, 2012. Available at: http://www.elmundo.es/ elmundo/2012/04/24/espana/1335249973.html. Accessed December 14, 2012. 4. Sevillano, Elena. El bastion de la marea blanca. El Pais [online]. November 10, 2012. Available at: http:// ccaa.elpais.com/ccaa/2012/11/10/madrid/1352585971_ 718417.html. Accessed December 12, 2012. 5. The Future of the Publics Health in the 21st Century. Institute of Medicine of the National Academies: November, 2002.
18
Volume 3 Issue 1 Winter 2013
19
Hepatitis B Eradication: An Unsolved Challenge
Christina Wang
knowing that one in ten people around me suffered from hepatitis B. It wasnt until I came to college that I learned what hepatitis B is and that this disease is in fact ten times more prevalent that AIDS, and 100 times more infectious.1 My childhood ignorance is a testament to the evasive nature of this virus to community public health efforts. Hepatitis B mostly affects Asian Pacific Islanders, a demographic that only comprises six percent of the United States population. In a country that frequently focuses on public health efforts that will affect populations that comprise
I grew up in China without
a greater proportion of society, hepatitis B does not constitute a significant enough threat to motivate sizeable involvement by the public health community. In addition, a vaccination for hepatitis B exists and has been widely implemented. The urgency of addressing hepatitis B lessened beginning in 1992, when all newborns began to be vaccinated against this virus. Thus, for young, American-born individuals, hepatitis B no longer poses an immediate threat. However, in port cities including San Francisco and New York City, immigrants from highly afflicted countries are constantly arriving, warranting continued
focus on this topic. Additionally, the asymptomatic nature of hepatitis B leads to continuing concern, as patients do not know they are infected until they are already significantly ill. As a member of Team HBV, an intercollegiate organization that seeks to eradicate hepatitis B in nearby communities, I have experienced all of these barriers to hepatitis B awareness efforts, first-hand. The goal of the organization is to educate Stanfords campus members through events like the Screening Initiative Program. The premise is simple: visit Vaden Health Center, provide documentation to show that hepatitis B
Graphic Illustration by Judith Shanika Pelpola
screening was performed, and receive a reward. Analysis of the results of 80 test subjects left the organization both optimistic and perplexed. None of the 80 students who had been screened for hepatitis B tested positive. Clearly, Team HBV was not targeting the right audience, as the majority of the test subjects were Stanford undergraduates, born on or after 1992 and who had been vaccinated. Though on campus screening proved to be a rather ineffective measure to reduce hepatitis B prevalence, the organization still wanted to increase on-campus awareness of the disease and its prevalence in a tangible manner. Thus, Team HBV organized a Hepatitis B Awareness Week, during which flyers illustrating hepatitis B facts and a schedule delineating a weeks worth of educational events were distributed across campus, attached to balloons in order to call attention to the event. Yet all of these efforts proved to be largely ineffectual. Some students may now be cognizant of the existence of hepatitis B and the organizations efforts dramatically increased the occurrence of on-campus screening, but the overall effects were strictly limited to the Stanford campus. Despite the narrow improvements on the Stanford campus, other eradication efforts worldwide have shown significantly more promise. I was fortunate enough to have the opportunity to organize
World Hepatitis Day in the summer of 2012. The World Hepatitis Alliance challenged viral hepatitis organizations across the world to participate in a Guinness World Records Challenge of having the most people performing see no evil, hear no evil, speak no evil actions in numerous venues around the world, over a 24hour period. A total of 50 Team HBV high school and college students came out to the Crissy Field location in San Francisco on July 28th, 2012. The worldwide event was featured in articles in the World Journal and the Tsingtao News, the two largest circulating newspapers among the ChineseAmerican population in San Francisco. The publicity that this event received shed light on a more effective method through which to target the population at risk: reaching out to the local media. Not only were we able to communicate directly to the highest risk population in the Bay Area, but we were also communicating to them in their language, through media sources that they trusted. A second event that proved effective was a service trip that addressed the subject of hepatitis B in San Francisco. One of the trip days highlighted advocacy efforts by splitting the group in half and rallying legislative offices to raise awareness of hepatitis B. While the group members were initially skeptical of the potential impact of this type of advocacy work, the
majority of students came out feeling that the representatives of elected officials had heard and understood the message that they were sending. While state budgets were a constraining factor, the offices told the students that they would do their best to advocate for hepatitis B screening in the future. Most interestingly, many of the representatives reported that they had not heard of hepatitis B prior to the students visit, which raises the question, if these elected officials had not heard of this critical public health issue before, how can we expect their constituents to be aware of the disease? The experience of Team HBV highlights the efficacy of discussing key public health issues with legislative offices. In particular, Senator Feinsteins office noted that they greatly enjoy student input because student constituents are not paid for the messages that they deliver, but rather do so out of sheer interest and concern. Team HBV has approached their goal of the eradication of hepatitis B through a variety of methods, several of which offer fresher and arguably more effective methods than on-campus education. While the latter remains an important tactic, the battle with hepatitis B will require use of a wide variety of broadly targeted avenues to educate a greater percentage of residents in the United States. The sooner that awareness is raised, the sooner hepatitis B will be eradicated.
20
Stanford Journal of Public Health
1. Liu, J. and Fan, D. Hepatitis B in China.The Lancet. 2007;369(9573): 15821583. Volume 3 Issue 1 Winter 2013
21
Polio Eradication in India:
The
invites the members of the Stanford community to share their essays, perspectives, and research with a broader audience interested in public health. In this issue, we present a highly varied collection of research from the undergraduate community that addresses national and international topics. Our authors have explored topics relating to the effectiveness of school-located influenza vaccination programs, a cost and policy analysis of in vitro fertilization, a comparative policy analysis of polio eradication methods used in Pakistan and India, and techniques to reduce the psychological and economic burdens on infertile women in America.
Ayurvedic or traditional medicine shop. Karachi, Pakistan. December 2011. Photo Courtesy of Ravi Patel
research
Lessons for Pakistan?
section of the SJPH
Ravi Patel
t has been claimed that, apart from the atomic bomb, Americas greatest fear was polio in post-World War II America. However, this American fear was conquered in 1956, when Dr. Jonas Salk developed the first polio vaccine. Salks polio vaccine has been highly effective, and today, it has led to the eradication of endemic polio in all but three countries worldwide: Afghanistan, Nigeria, and Pakistan. Although separate countries today, Pakistan and India were both carved out in Volume 3 Issue 1 Winter 2013
1947 from a single territory then known as British India. As a result of this common heritage, the two countries face similar social, political, and, most importantly, developmental challenges today. Along with similar historical and social contexts, both India and Pakistan share similar per child cost of vaccination, another factor placing Pakistans polio crisis in context of Indias past experiences (Figure 1). Specifically, this paper analyzes the case of polio eradication in India, and in tandem identifies potential lessons for Pakistan in its quest to eradicate polio.
Today, polio can be found in four main areas in Pakistan: FATA (Federally Administered Tribal Areas), Khyber-Pakhtunkhwa and Baluchistan (along the border with Afghanistan) as well as in parts of Sindh (Figure 2). These locations also happen to experience the greatest security vulnerabilities from radical Islamic groups such as the Tehrik-i-Taliban Pakistan. The poor security conditions in these places enable polio to thrive because of difficulties in sustaining a robust public health infrastructure. The vulnerability of polio workers in Pakistan was best illus-
22
Stanford Journal of Public Health
23
Figure 1: Operations costs per Child for SIAs (Supplementary Immunization Activities)18
trated by a series of coordinated attacks in Khyber-Pakhtunkhwa and Karachi by Taliban associated militants in December 2012 and January 2013. In total, 16 health workers were killed, including 12 women, and the U.N. decided to temporarily suspend its operations against polio in the country. Women health workers are essential in Pakistans battle against polio since women in the conservative Pakistani culture, unlike men, can get access to children and other women in the household. The four regions in Pakistan home to polio are tribal in nature, and have large, migrating populations, making vaccine distribution difficult to organize. The Taliban and other fundamentalist Islamic groups have also banned polio health workers from delivering care in certain parts of the county where they exert influence claiming
that these workers are American spies. This misconception was reinforced with a fake polio vaccination campaign in Abottabad carried out by Dr. Shakil Afridi under CIA supervision to obtain DNA confirming Osama Bin Ladens presence. Coupled with this continuing suspicion, many in Pakistan believe that the polio vaccine is a Western rouse to sterilize Muslim. A similar distrust exists in Nigeria, where some religious leaders have called for boycotting polio vaccination because they believe it causes sterility in girls, spreads HIV and cancer. Resistance ultimately led to several northern Nigerian states boycotting the polio vaccine for about 10 months during 2004.7 The fallout of Nigerias struggles with immunization in 2004 not only led to polio spreading to previously polio-free areas in Nigeria, but to also spread to eight polio-free countries surrounding Nigeria. Beyond these existing issues, Pakistan faces poor public health infrastructure and possesses a critical shortage in human resources. Experts have argued that Pakistan faces a massive funding shortfall for polio eradication. So far, Pakistans government has so far only been allocated half of what was budgeted for 2012-13 by the Global Polio Eradication Initiative (a public-private partnership led by organizations such as the WHO and the U.S. Centers for Disease Control and Prevention to eradicate polio). Clearly, Pakistan faces immense political obstacles as it seeks to eliminate polio. India, Pakistans neighbor to the west, has also faced
a long battle against polio. As recently as 2009, India had the highest number of polio cases in the world.2 Like Pakistan, India faces rampant poverty, high birthrates, large populations, and remotely located communities. Along the same lines, India has weak public healthcare infrastructure, reflected in its poor track record of delivering medical care. For example, India was ranked 112th of 191 by the WHO in terms of its ability to deliver adequate healthcare to its citizens. Despite these challenges, India has implemented measures that such that January 2010 marks the last reported case of polio. Political commitment was the primary change that made India successful in its fight against polio. With political backing from the ruling Congress Party, the Indian government apportioned significant resources to polio eradication campaign. By 2013, India will have invested nearly $2 billion to combat polio. As a result of this political support nearly 170
Figure 2: Map of Polio Hotspots in Pakistan, 201019
million Indian children are immunized through two national polio vaccination campaigns each year. Furthermore, India was effective with targeting nomadic populations by using better mapping technologies in conjunction with the aid of local community workers. Not only did these workers better understand nomadic populations, but they also were able to gain the trust of people they served. Indias robust surveillance and immunization network was crucial to polio eradication operations as well.4 To date, India has 33,700 reporting sites, managed with the assistance of 2.5 million vaccinators.11 The infrastructure established by Indias polio campaign has encouraged additional immunization campaigns. Because of these customized political measures, India has been able to defeat polio, a threat that has dominated the land for hundreds of years. While it is difficult to gauge whether Pakistan will successfully embrace the polio eradication policies exercised in India, it is obvious that failed strategies in Pakistan will require intervention. Polio conditions in India vastly improved subsequent to employing techniques used in neighboring Bangladesh (also carved out from colonial British India like India and Pakistan as well). Bangladesh eradicated endemic polio in 2000. India, in particular, was able to adopt some lessons from Bangladesh (also carved out of British India like India and Pakistan), which eradicated endemic polio in 2000. In the case of Bangladesh, the campaign against polio was particularly successful because Volume 3 Issue 1 Winter 2013
Photo Courtesy of Ravi Patel Children playing after receiving the polio vaccine in Sukkur, Pakistan
it was able to build a robust infrastructure monitoring polio. In Bangladesh, more than 90% of cases of acute flaccid paralysis, a clinical symptom of polio, are investigated within 48 hours of notification. Based on these lessons, India was able to improve its polio surveillance network and this move was one of the key factors that help it win its own battle with polio. A simple cut and paste of Indias public health set up may not by itself eliminate polio in Pakistan. These lessons, nevertheless, do highlight crucial changes that would serve as a starting point for Pakistan to be
more effective against polio. In Pakistan, there is political support against polio at the highest levels of government. For example, Pakistani President Asif Ali Zardari announced at the UN General Assembly in September 2012 that he and his government would work to make Pakistan polio free. This elite political support has not yet trickled down to the local and provincial level. From my informal conversations with local PPP (Pakistan Peoples Party, the ruling political party) workers in rural Sindh, the persistence of polio can be attributed to the lack of coordination on polio eradica-
24
Stanford Journal of Public Health
25
tion efforts between the districts themselves. Even with widespread political backing, failing to coordinate the battle against polio and provide vaccine access to nomadic communities has caused polio to continue to plague the people of Pakistan. Obtaining greater political support at the local levels might also lead to an improved security environment for health workers because obtaining support from these local leaders lessen resistance from local communities.
Pakistan could develop a robust surveillance and immunization network akin to that of India. Adopting Indias approach will bring Pakistan one step closer to eliminating polio, and potentially other preventable diseases, from its own land. Collaborating with India on polio eradication would reduce, if not eliminate, the polio burden from the country, serving as a bridge in an otherwise frosty bilateral relationship. Furthermore, cooperation on
the polio issue between the two countries could be a conduit for further collaboration on other critical public health issues such as HIV/AIDS or tuberculosis. Perhaps, greater cooperation in public health could have implications for other regional development issues such as the prospect of building more cross border trade. By applying lessons from Indias experiences defeating polio, Pakistan can save more lives from experiencing the effects of this disease.
Infertility: A Plague Gone Unnoticed
Nearly 6 million women and their partners in the US suffer from infertility. Most think it is just another medical problem, but the truth is, the suffering of these victims goes far beyond the biology to the psyche, leaving deep lasting scars. Little has been done to rectify this problem at the policy level. But through an active, multidisciplinary effort, a fresh current of change might just be possible.
Nitya Rajeshuni
change and evolution, womens health is just one more hot-button issue to add to the laundry list of contentious policy battles. In recent years, the debate has become particularly intense, involving heated discussions between various demographics, ranging from men versus women to Republicans versus Democrats to old versus young to even women versus women. However, the issues present in the media every daytopics like abortion and contraceptionare only part of the story. In the shadow of such discussions, other equally important issues in womens health have been masked. When is the last time a major national debate took place regarding funding for research on infertility or health care coverage for its treatment? Has any such large-scale debate ever occurred in the first place? What about the ramifications that often come with inability to start a family? Is it likely that current legislatures will fund treatment of the depression and cases of mental illness associated with
1. The Polio Crusade American Experience. Public Broadcasting Service. 2009 2. John, Jacob and Vipin Vashishtha. Path to Polio Eradication in India: A Major Milestone Indian Pediatrics. Volume 49, Number 2 (2012), 95-98. 3. Muhammad, Peer. Security Situation a risk to anti-Polio effort: WHO. The Express Tribune. 2012. Available at: http://tribune.com.pk/story/419545/security-situation-a-risk-to-anti-polio-effort-who/ Accessed Dec 1, 2012 4. The War on Pakistans Aid Workers. The New York Times. 2013.Available at: http://www.nytimes.com/2013/01/05/ opinion/the-war-on-pakistans-aid-workers.html Accessed Jan 10, 2013. 5. Walsh, Declan and Donald McNeil Jr. Female Vaccination Workers, Essential in Pakistan, Become Prey. The New York Times. 2012. Available at: http://www.nytimes.com/2012/12/21/world/asia/un-halts-vaccine-work-in-pakistanafter-more-killings.html?pagewanted=all. Accessed Jan 10, 2013 6. Walsh, Declan. Taliban Block Vaccinations in Pakistan. The New York Times. 2012. Available at: http://www.nytimes.com/2012/06/19/world/asia/taliban-block-vaccinations-in-pakistan.html Accessed Dec 1, 2012 7. Tohid, Owais. Move to Get Bin Laden Hurt Polio Push. The Wall Street Journal. 2011. http://online.wsj.com/article/SB10001424052970204190504577038781784474056.html Accessed Dec 1, 2012 8. Personal Conversations with local Pakistani Political Leaders in December 2011. 9. Jegede AS (2007) What Led to the Nigerian Boycott of the Polio Vaccination Campaign? PLoS Med 4(3): e73. doi:10.1371/journal.pmed.004007 10. Polio boycott is unforgivable. British Broadcasting Corporation. 2004. Available at: http://news.bbc.co.uk/2/hi/ africa/3488806.stm 11. Winsten, Jay and Emily Serazin. Victory Against Polio is Within Reach. The Wall Street Journal. 2012. Available at: http://online.wsj.com/article/SB10000872396390444025204577546562570306028.html Accessed Dec 1, 2012 12. World Health Report 2000. World Health Organization. 13. UN Health agency marks WPD with renewed efforts to eradicate the disease. Available at: http://www.un.org/apps/ news/story.asp?NewsID=43366&Cr=polio&Cr1=#.UIzLBMXA8kk Accessed Dec 1, 2012 14. Building on Indias Success on Polio. The Wall Street Journal. 2012. Available at: http://blogs.wsj.com/indiarealtime/2012/10/24/building-on-indias-success-on-polio/ Accessed Dec 1, 2012 15. Schaffer, Teresita. Polio Eradication in India: Getting to the Verge of Victory and Beyond? Center for Strategic and International Studies. 2012. 16. USAID/Bangladesh. Polio: On the Brink of Eradication. Available at: www1.usaid.gov/bd/files/polio.doc. Accessed Dec 1, 2012 17. Zardaris Pledge to Polio. Dawn. 2012.Available at: http://dawn.com/2012/09/28/govt-taking-polio-eradication-campaign-seriously-zardari/ Accessed Dec 1, 2012 18. Financial Resource Requirements 2012-2013. Global Polio Eradication Initiative. World Health Organization. 19. Available at: http://www.polioeradication.org/Dataandmonitoring/Poliothisweek.aspx Accessed Dec 1, 2012.
In an era of ongoing policy
infertility when most do not even fund the treatment itself? Infertilitymillions of women across the nation today struggle with this condition; yet, despite the prevalence of this plague and the suffering it brings, their plight has gone severely unnoticed, masked by the ever- present discussion on abortion and contraception. However, one must wonder, if society is so concerned regarding policy covering not only the prevention of birth but of conception, shouldnt the creation of life receive equal attention? Infertility is a major problem in the US, proving not only challenging but extremely expensive and psychologically detrimental, particularly to women. Despite these negative implications, very little policy on the subject has been proposed to date. However, that is not to say that national or state legislation would have very little impact on the issue. Rather, the proposal of such legislation could have much to offer, if constructed in a multifaceted and interdisciplinary manner. Through such an approach, combining both
federal and state efforts, access to psychological services and affordability of treatment could certainly be increased as well as improved. Of course, one must ask, how might we achieve this? Although there is much work to be done, an excellent place to start would be through policy proposals such as the specific bill I have constructed and outlined in this paper.
26
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
27
Having a child is a common dream that many women share.
Nearly 6 million women and their partners in the US are infertile, accounting for approximate 10-15% of the entire reproductive population.7 While about 40% of infertility cases can be attributed to male-related factors and 40% to female-related factors, 20% are attributed to a combination of the two, rendering exact diagnosis often difficult.7 Furthermore, even if a particular partner has been identified as the source, diagnosis can prove equally if not more challenging,7 despite the variety of medical treatments available. Approximately 25% of all couples in the US have trouble conceiving.7 Typically, 10-15% can eventually succeed using basic methods, such as regimented sexual intercourse, discontinuation of birth control, and changes in lifestyle, diet, and nutrition. While 80% of those who begin with the basics succeed, the remaining 20% typically move on to fertility drugs, hormonal therapy, and finally assisted conception (intrauterine insemination, in-vitro-fertilization (IVF) and intracytoplasmic sperm injec-
tion (ICSI)), posing a disheartening 20% success rate.7 While these treatments offer potential medical solutions to the problem of infertility, issues of mental health have increasingly garnered more attention due to the lack of efforts and funds in this area. A promising, albeit inadequate, amount of research has been conducted, indicating that the mental health of women facing infertility is indeed a very real problem. However, the findings have hardly been applied. According to the Department of Health and Human Services 2010,4 the seven leading mental health issues faced by infertile women are 1) anxiety 2) depression 3) anger 4) marital problems 5) sexual dysfunction 6) social isolation and 7) low self-esteem. Statistics have shown that amongst infertile couples, women often display higher distress than men, although when infertility is attributed to the male factor, the responses in males and females are the same.2 Furthermore, 15-54% of infertile couples experience depression, much higher than the average percentage of fertile couples experiencing depression.2 8-28% of infertile couples also experience severe anxiety.2 To complicate matters further, couples with a previous history of depression are susceptible to a two-fold increase in the likelihood of experiencing depression.2 This positive feedback loop is perhaps the biggest challenge women face; while previous mental health issues can alter ones ability to deal with the psychological stressors of infertility, the stressors associated with assisted conception often
exacerbate these very feelings of exasperation and anxiety.2 One Harvard Medical School study has even likened this phenomenon to the emotional distress experienced by heart disease and cancer patients.8 Accordingly, knowing when to stop treatment often proves the most difficult decision.8 Now, who exactly qualifies as infertile? According to nationally accepted criteria, women under the age of 33 unable to conceive within a year are considered infertile, as are women over the age of 34 unable to conceive within six months. Over the years, the number of women seeking treatment has risen, due to later childbearing, better treatment options, and increasing awareness of the many services available.2 However, one cannot help but wonder why the mental health implications associated with infertility have not yet been adequately addressed? As is the case with many other health conditions, medical diagnosis is often prioritized over mental health, while research funding for basic science is often easier to obtain than funding for psychological postulations. This coupled with the lack of understanding and empathy for the condition of women struggling with infertility has accordingly, resulted in a dearth of infertility related policy. That being said, some steps towards rectifying this problem have been taken. Current treatments for resulting mental health conditions include cognitive behavioral group psychotherapy, support groups, general stress relieving techniques, and potentially antidepressants. AcStanford Journal of Public Health
cording to the New York Times,8 in the past two years, nearly half of the 370 infertility centers approved by the Society for Assisted Reproductive Technology (SART) have incorporated such services. However, despite the slight progress that has been made, one cannot help but wonderwhy hasnt more been accomplished? The answer to this question is undoubtedly quite complex, however, a good place to start is first recognizing that balancing the interests of the many stakeholders involved is quite challenging. Although the Obama Administration has largely been preoccupied with the push to address more controversial issues in womens health such as abortion, contraception, and health care coverage of these procedures, its point of view (or lack-thereof) is absolutely critical to influencing the policy-field and affecting change. The DHHS and its agencies are also integral, particularly in implementing such policy change. At the other end of the spectrum lies State Legislatures and their constituents, running the gamut from health care providers to private and public hospitals, to special interest groups, to national associations, and finally, to individual voters, particularly infertile women. Balancing these various interests is undoubtedly difficult, reducing the likelihood of passing infertility legislation dramatically. In fact, in the last 10 years, Congress has completely failed to pass infertility legislation on a national scale. What bills have even been proposed in the first place? Two major pieces of legislation in particular that Volume 3 Issue 1 Winter 2013
have repeatedly surfaced: 1) the Family Building Act (2009, 2007, 2005, 2003) requiring all health care plans to provide benefits for treatment of infertility and 2) the Medicare Infertility Coverage Act (2005, 2003) amending Medicare to cover infertility treatments for individuals entitled by reason of disability. Other proposed bills have also discussed research on and coverage of cancer-related infertility, a tax break for qualified infertility treatment expenses, and the creation of an Interagency Task Force. However, not a single one of these bills has ever reached the floors of Congress. At the state-level, fifteen states have now mandated coverage of infertility diagnosis and treatment,5 each outlining its own specific guidelines; however, many of these plans are still incomprehensive, with none in particular addressing mental health.6 The 1998 Supreme Court case Bragdon v. Abbott first fueled this discussion citing reproduction as a major life activity warranting protection under the Americans with Disabilities Act.1 However, while this historic precedent precluded employer discrimination on the basis of infertility, it did not resolve the question of coverage.3 Even more recent events such as the Patient Protection and Affordable Care Act (PPACA) do not directly address issues of infertility, although prevention of unwanted pregnancies as well as maintenance of healthy pregnancies are well represented.9 The shortfalls in current policy are numerous. While, no sustainable, active effort has been made by national or state government, policy directly
targeting the mental health implications of infertility has not been proposed at all. Yet, a few strengths are to be noted; the possibility of financial burden has at least been broached. Furthermore, the infrastructure is already in placeBragdon v. Abbott and the PPACA provide room for more expansive financial coverage; they need only be clarified or amended. So how does one deal with such a problem? One can either 1) alleviate its effects or 2) eliminate the source itself. Below, I have outlined and provided an example of a policy proposal tackling the infertility challenge from both ends. Under each subtitle, I have provided in italics a simple summary of the requirements listed under each respective subsection: STATEMENT OF INTENT: Access to psychological resources must be made more accessible and treatment more affordable, thereby increasing access to care, the possibility of pregnancy, and the reduction of psychological stress. TITLE I: Increased Access to Psychological Services to Facilitate Coping SUBTITLE A: The DHHS (Department of Health and Human Services) should work with SART (Society for Assisted Reproductive Technology) leadership to develop a mandate urging the remaining half of SART-approved infertility centers to incorporate cognitive behavioral therapy and stress reduction services by the end of 2014. Services should be integrated with counseling on adoption and childfree living. Currently, approximately half of the SART-approved in-
28
Image courtesy of Microsoft
29
fertility centers in the nation provide psychological services to couples dealing with infertility to help cope with the stress of being unable to conceive. Such services would also target helping patients deal with other mental and emotional health implications, including depression, anxiety, suicidal thoughts, etc. The form of such services could take a variety of forms, including cognitive behavioral therapy, general stress reduction techniques, and counseling/therapy. Such efforts should also be combined with counseling on the options that are available to couples 1 should) they be unable to afford infertility treatment or 2) should their infertility treatment fail. Such options include adoption and child-free living. This subsection mandates that the remaining half of SART-approved infertility centers that do not already provide such psychological services develop the relevant infrastructure and programs by the end of 2014. SUBTITLE B: Any federally funded hospital currently providing infertility diagnosis and treatment must appropriate some funding towards developing psychological services by the end of 2014. Each center must submit a cost analysis and proposed budget. Federal subsidies should then be provided as deemed necessary. While certain hospitals in the nation are privately funded, many receive funds from the federal (national) government at varying levels and degrees. Accordingly, the federal government has an important say in how such funding is used and allocated. This subtitle mandates
that any hospital that received federal funding must allocate some portion of this funding towards developing psychological services to help patients cope with the implications of infertility. The forms of such services are outlined in the italicized description of TITLE I, SUBTITLE A above. Because evaluation of the enforcement of such policy is integral to successful implementation, each federally funded center must provide a projected budget for the programs they plan to develop. If further funding is needed, the federal government may provide subsidies as needed if deemed appropriate based on proposed budgets submitted by each center. This must be met by the end of 2014. SUBTITLE C: DHHS should consult with Director Francis Collins of the NIH and Director Thomas Insel of the National Institute of Mental Health (NIMH) on increasing the budget or appropriating a larger percentage to research on the psychological effects of infertility and potential facilitators of coping. SECTION I: The possibility of developing relevant extramural grant programs should be discussed. SECTION II: Research on the financial burden of depression (assuming it go untreated) must not be neglected. Interdisciplinary cooperation and collaboration are absolutely critical to tackling an endeavor as ambitious as expanding infertility treatment options, care, research, and health care coverage. Thus, interagency cooperation is crucial. Accordingly, as per this subsection, DHHS leaderships make an ac-
tive effort to collaborate with leaders of the NIMH under the NIH. Although actionable collaboration need not take place immediately, the purpose of this subsection is to encourage the two organizations to immediately begin discussions focused on the possibility of expanding or reallocating funding provided to the NIMH extramural grant program (funding provided to non-NIH affiliated laboratories and institutes) for research on infertility treatment and psychological services. TITLE II: Increased Access to Infertility Treatments through Affordable Cost SUBTITLE A: DHHS must mandate that the 35 states currently offering no coverage of infertility diagnosis and treatment must develop plans addressing this issue by January 1, 2014. SECTION I: Because this is a contentious issue, the specifics will be left up to the states. SECTION II: States should be encouraged to, at the very least, cover basic infertility diagnosis and treatment, including medical counseling, supplements, basic medication, and hormonal therapy. SECTION III: These insurance plans should be prepared independently of ACA State Exchanges. Currently, only 15 of 50 states in the nation provide state-based insurance plans covering infertility treatment. This subsection mandates that the remaining 35 states develop state-based plans that include coverage of infertility treatment by the beginning of 2013. This plans would be developed outside of the PPACA (an expansive national univerStanford Journal of Public Health
sal health care bill passed during the Obama Administration) and because federal mandates on state-based insurance plans is often a contentious issue, the specifics of these plans and the type, form, and amount of coverage will be left up to the State Legislatures. At the very least, states will be encouraged to provide coverage of infertility diagnosis and treatment. SUBTITLE B: Amend the ACA to include a category on infertility under the Essential Health Benefits by January 1, 2014 and, should the amendment fail, encourage State Exchanges to address infertility and mental health potentially under the Essential Health Benefits package. Currently, the recent universal health care bill the Patient Protection and Affordable Care Act (PPACA) does not include provisions for coverage of infertility treatment, although contraception and abortion are addressed. Thus, this subtitle mandates that the Essential Health Benefits section under the
PPACA be amended to include a section on infertility treatment by the beginning of 2014. The Essential Health Benefits section covers the essential services that every government health-care plan must include. However, should this amendment fail to pass through the Congress, the State Exchanges established by the PPACA should be encouraged to incorporate coverage of infertility treatment and mental health services in the plans they develop. State Exchanges are essentially the instrument through which the PPACA will be executed in each respective state. SUBTITLE C: Push through the Family Act of 2011, amending the Internal Revenue Code to allow an income-based tax credit for 50% of qualified infertility treatment expenses. Reintroduce in the 113th Congress if necessary. According to this subtitle, members of Congress should make an active effort to pass the Family Act of 2011, reintroducing the bill as necessary, since all
Image courtesy of Microsoft Infertility can cause frustration for those who want to become parents.
bills that are not passed by the end of a Congressional Session are killed. This act amends the tax code so as to provide a 50% tax credit (reduction of payment) on expenses paid towards the cost of infertility treatment. SUBTITLE D: Reintroduce the Family Building Act and Medical Infertility Coverage Act. According to this subtitle, members of Congress should reintroduce the 1) Family Building Act and 2) Medical Infertility Coverage Act (discussed previously in this paper). These acts respectively require all healthcare plans to provide benefits for infertility treatment and amend Medicare to cover infertility treatments for individuals entitled to this coverage due to their acquirement of a disability related to infertility. TITLE III: Develop an Interagency Task Force to promote awareness, research, interagency cooperation, prevention curriculum, and multidisciplinary partnerships on infertility and its mental health implications. COMMENTARY: Though this multi-pronged approach, the problem of not only access and cost of care but alleviation of mental health challenges could be addressed at a federal and state level. It is not necessary that all provisions pass; rather, it is the hope that a balance between federal and state considerations can be struck. Of course, a bill as expansive as this must make use of adequate and available resources from interdisciplinary sources as well. First and foremost, interagency and private-public sector cooperation amongst various parties including the DHHS,
30
Volume 3 Issue 1 Winter 2013
31
NIH, State Legislatures, and SART are key. Funding is also extremely important. While the NIH may be able to contribute significantly to the research budget, the more difficult financial issue lies at the state levelhow will states be able secure enough capital to fund infertility coverage through state-insurance plans? If they choose to tackle this issue through the PPACA, State Exchanges will be responsible for appropriating money as needed, whereas if they choose to tackle it from the perspective of state-mandated insurance plans, collaboration between State Legislatures and health care providers is critical. From a private sector route, the engagement of SART and other national associations would be integral in convincing private centers to integrate more psychological services into their treatment programs, while bipartisan partnerships and discussion will be integral to passing federal legislation. Thus, lobbyist and advocacy groups should be engaged as should community organizers and clinics. Because coordinating these various interdisciplinary efforts could certainly prove difficult as well as complicated, establishing an appropriate timeline for the enforcement of different titles and subtitles under a bill is critical as well. For the bill outlined above, an appropriate timeline would include the following deadlines: 1) TITLE I: SUBTITLES A and B must be met by the end of 2014 2) TITLE II: SUBTITLES A and B would be subject to the January 1, 2014 deadline imposed on State Exchanges by the ACA 3) TITLE III
establishing an Interagency Task Force and TITLE I: SUBTITLE C targeting NIMH research should be implemented immediately, allowing NIH to begin implementing the findings of these discussions as early as FY 2013 or FY 2014 and 4) TITLE II: SUBTITLES C and D dealing with federal legislations idealistically should be addressed in the current 112th Congress and reintroduced as needed. Finally, evaluation of the enforcement of such a bill must be conducted as well to ensure that progress is being made. Outcomes of the bill above, for instance, could be monitored and evaluated regularly by an Interagency Task Force, which would be required to prepare biannual reports of ongoing policy advancements, incorporating feedback and progress reports submitted by involved agencies as well as private parties one month prior. NIH could be in charge of evaluating research progress, conducting annual reviews of independent research grants, while the DHHS could select a nonpartisan NGO to conduct yearly reviews of both Task Force behavior and policy development. Data at all levels should be collected in the form of statistics, interviews, and progress summaries. Although both national and state environments surrounding the infertility debate are undoubtedly sticky, proposals such as the one outlined in this paper offer not only potential but significantly improved solutions to the neglected plague of infertility and its medical, financial, emotional, and mental implications. Fortunately, the
research and vehicles for change are already partially in place and through effective federal-state and public-private collaborations, could blossom into a more nationally integrated network balancing various stakeholder interests. As evidenced by the research and statistics in this paper as well as the illustrated example of potential policy solutions, interdisciplinary and interagency cooperation is absolutely critical to the success of such an ambitious endeavor, and if executed properly, could have the power to reverse the negative trend of neglect and ignorance that has surrounded the infertility debate at both the popular and governmental levels. The condition of infertility must not be neglected or ignored. Rather, we must embrace it and forge ahead, accepting that people of all medical conditions deserve a fair chance at having a shot at their dreams of better health and improved quality of living. While the road of progress most certainly is undoubtedly difficult, given that the infertility debate is indeed so far behind that of abortion and contraception, if individuals and institutes at various levels are willing to cooperate, a mighty current of change might just sweep through the nationa current those in need can embrace with relief.
To view the references for this paper, please refer to page 43.
Can Scools Prevent the Next Pandemic?
A study of school-located influenza vaccination in metro Atlanta, Georgia
Conclusions: Though the campaign did not prevent flu at the community level, it moderately raised vaccination rates in the intervention counties. Abbreviations: Influenza-like illness (ILI), School-located influenza vaccination (SLIV), Georgia Department of Public Health (GADPH), Georgia Registry of Immunization Transactions and Services (GRITS) Introduction Every year, 5-20% of the United States population is infected with influenza, resulting in an estimated 36,000 deaths and 226,000 hospitalizations. Though deaths are concentrated among the elderly, infection rates are generally highest in school age children (up to 30% attack rate).1 Children have also been found to be important vectors for spreading disease to other household members and throughout the community, increasing the population disease burden. Public health depart-
Julia Brownell
In the wake of the 2009 H1N1 pandemic, Georgia implemented a statewide school-located influenza vaccination (SLIV) campaign, providing a natural experiment through which to evaluate SLIV following H1N1 and the increased policy focus on vaccine-based flu prevention. Methods: This study focused on 12 participating schools in two metroAtlanta counties to assess the effectiveness of the campaign. The socio-demographic groups vaccinated were determined by examining data from parental consent forms. Effectiveness against flu was determined using absenteeism data from the schools and influenza-like illness (ILI) data from sentinel hospitals. Finally the effect on population vaccination rates was evaluated using data from Georgias Immunization Information System, GRITS. Results: Hispanic students were more likely than whites to be vaccinated at the clinics (Prevalence Ratio (PR): 1.18, 95% CI: 0.99-1.40), while blacks were less likely to be vaccinated (PR: 0.43, CI: 0.36, 0.52). There was no significant effect on absenteeism or ILI rates. There was a significant rise in the flu vaccination rate in the intervention county (4.20%) as compared to a neighboring control county (0.73%) (p<0.01). Volume 3 Issue 1 Winter 2013
Background:
ments have therefore instituted programs targeted at vaccinating school-age children as a strategy to control the spread of flu through the community. One such strategy is school-located influenza vaccination clinics (SLIV). Though influenza is vaccinepreventable, vaccination rates among school-age children (5-18 years old) were 26% in 2008, and lower among minorities than whites. In contrast, the Department of Health and Human Services Healthy People 2020 goal is 80% coverage in this age group. Because schools are a convenient location in which children are routinely present and often transmit the flu, mass vaccination campaigns have been implemented at schools across the US since 1970 in an attempt to raise the low vaccination rates among children. In previous studies of SLIV programs, average vaccination rates between 23 and 50% were typically achieved in participating schools, and moderate
32
Stanford Journal of Public Health
33
protective effects against flu in the school and community were observed.12, 13 However, almost all of what is known about SLIV effectiveness comes from data before the 2009-2010 H1N1 pandemic. The H1N1 outbreak was the most serious spike in influenza within the US in decades, leading to an estimated 60 million US cases, 270,000 hospitalizations and over 12,500 deaths (case fatality ratio 0.02%), with 86% of deaths among people less than 65 years old. A record 344 pediatric deaths were reported, and H1N1 attack rates were highest among school-age children.18 Schools were high transmission locations, and school start dates were highly correlated with the beginning of fall outbreaks across the country. In response to the H1N1 influenza outbreak, the Georgia Department of Public Health (GADPH) instituted a statewide SLIV campaign during the 2010-2011 flu season. No previous SLIV efforts had ever been undertaken at the state level in Georgia. The program was implemented in 605 schools across the state, and participation was entirely voluntary on the part of districts, schools, and students. Public health nurses provided free vaccinations to students with parental consent in communal areas such as a school gym or library. To comply with current recommendations, second clinics were held four weeks later in elementary schools to ensure previously unvaccinated children under nine years old were immunized twice. The program provides an excellent natural experiment
34
through which to evaluate the effectiveness of SLIV after H1N1, a topic that has not yet been studied. Due to the high transmission of flu among school-age children, new vaccine guidelines, and increased public health focus on influenza after the pandemic, public health departments, like the Georgia DPH, will likely consider SLIV programs in the future to control influenza. These agencies could use more updated information about their effects in their planning. This study sets out to fill that gap and especially to inform future influenza control strategies in the state of Georgia. Research Aims To examine the effectiveness of the GADPH 2010 SLIV program, this study aimed to: 1. Determine if the clinics reached under-vaccinated demographic groups. 2. Determine the effectiveness of the clinics in preventing flu in the community. 3. Examine the effect of the clinics on population vaccination rates. Methods Study Population: This study focuses on participating public health District 3-1, containing Cobb and Douglas counties in the metro Atlanta area. For parts of the analysis, District 3-1 was compared against the neighboring, demographically similar Gwinnett county. Twelve schools within District 3-1 held SLIV clinics, representing 30% of the total elementary and middle schools in the participating Marietta City (Cobb County) and Douglas school districts. The schools that participated had significantly higher subsidized
school lunch enrollment, higher Hispanic enrollment, and lower white enrollment than non-participating schools. Vaccines were administered to 1,188 children in the participating schools, which had 6,812 total enrolled students. Data Sources Parental consent forms collected by the local public health department at the clinics were used to determine the gender, race, ethnicity, and type of vaccine received by children vaccinated at the SLIV clinic. Publicly available enrollment, racial and ethnic breakdown, school lunch enrollment, and gender distribution data for each school in Marietta City (Cobb) and Douglas school districts was gathered from the Georgia Department of Education (DOE). To determine the effect of the SLIV clinics on flu outcomes, I used school absenteeism data for the months of January to March 2009 and 2011 that was released by the two school districts. Absenteeism is an accepted proxy for childhood flu, and has been used in previous studies.6, 12 The 2008-9 flu season was used as baseline due to the unusual seasonal patterns of H1N1 in 2009-10, spiking in AprilJuly and again in SeptemberDecember, making a consistent absenteeism window difficult. To further explore the effects of SLIV on community flu burden, adult and pediatric (<24 years) influenza-like-illness (ILI) data was gathered over 16 weeks from January March 2009 and 2011 from the sentinel hospital and clinic reporting program in Georgia (n=55) as reported to the flu epidemiology group at the GADPH. Sentinel hospitals Stanford Journal of Public Health
report the percent of their total visits that present with clinically suspected ILI each week defined as a fever >100F accompanied by cough or sore throat without another known cause. Change in overall vaccination rates was examined using the Georgia Registry of Immunization Transactions and Services (GRITS), Georgias immunization information system. Since 2004, vaccine-providers have been required by law to enter any administered immunization into the system, including influenza. Analysis of a random sample of two-year-old children in 2010 showed that GRITS captured 98.1% of core childhood vaccinations [unpublished analysis of Georgia Immunization Study data]. Although the reliability of GRITS may have been lower for flu vaccinations, which are not required for school and are often received outside the doctors office, GRITS is the only central records system that exists for vaccinations in Georgia. All vaccinations from District 3-1 were accessed, but to restrict the sample to school-age children only those ages 5 through 14 on August 1, 2010 were included in the final dataset, which includes demographics of the child, specific vaccine type, county, and date of administration. Analysis At the school level, the vaccinated and unvaccinated student populations were compared using a logistic regression model to determine prevalence ratios for vaccination by demographic group. Correlation of vaccination rate with school lunch enrollment was also examined using Pearsons correlation coefVolume 3 Issue 1 Winter 2013
ficient. The clinics effectiveness in reducing community flu burden was determined by comparing change in absenteeism between January-March 2009 (pre-intervention) and 2011 (post-intervention) between participating and non-participating schools in Cobb & Douglas counties using two-sample proportion tests. Change in ILI rates over the same time frame, both total and pediatric, was compared between Cobb & Douglas counties and the state average not including them. Finally, the programs effect on population vaccination rates was determined by comparing frequency of vaccination between District 3-1 and Gwinnett County before and after the intervention using chi-squared tests of independence. A logistic regression model was then used to determine whether the SLIV clinics replaced vaccinations that would have occurred anyways, or instead vaccinated children who were less likely to be vaccinated without the clinics. Results At participating schools, vaccination rates ranged from 5 to 40% of the student body, averaging 18%. Hispanic students were significantly more likely to be vaccinated at the SLIV clinics than white students, while black students were significantly less likely to be vaccinated than
white students (Table 1). Male students were also significantly less likely than female students to receive a flu shot at the clinics (Table 1). The vaccination rates were not correlated with the percentage of the student body receiving subsidized school lunch (a proxy for student socioeconomic status) (Pearsons r= -0.16, p=0.6; Spearmans r= -0.05, p=0.85). There was no significant difference in change in absenteeism between participating (-0.32%) and non-participating Douglas and Marietta schools (-0.37%) (Table 2). Rates of total ILI increased from January-March 2009 to 2011 in Cobb and Douglas county sentinel hospitals, but decreased in the rest of the state. This difference was significant (p=0.02) using a two-sample proportion test (Table 3). Pediatric ILI showed the same trends of increase in Cobb and Douglas versus decrease at the state level (not including them), but the difference was non-significant (p=0.13) (Table 3). During the baseline flu season of 2008-9, the rates of flu vaccination in the intervention counties of Cobb and Douglas (8.42%) and control county, Gwinnett (8.53%), were similar (X2=0.45, p=0.50). By 201011, the rates rose to 12.62% in Cobb/Douglas, while Gwinnett rose to 9.26%, leaving the two
35
significantly different (X2=310, p<0.001). Each individual increase in vaccination rate was significant, but the jump in Cobb and Douglas rate was significantly larger than the rise in Gwinnetts (Table 4). In a logistic model without interaction, both prior flu vaccination (OR=6.91, p<0.01) and residence in the intervention counties (OR=1.46, p<0.01) were significant predictors of receipt of a flu vaccine in 2010-11. An interaction term was then added between the two predictors, which showed that residence in the intervention counties nonsignificantly lowers the predictive power of prior vaccination on vaccination in 2010-11 (Likelihood Ratio X2=0.84, p=0.36). Residence in the intervention county was therefore determined not to be a significant effect modifier of prior flu vaccination on likelihood of influenza vaccination in 2010-11. Discussion The school-located influenza vaccination (SLIV) campaign in Cobb and Douglas counties in
metro Atlanta, Georgia, failed to show a significant effect in reducing flu in the community, but was associated with a significant rise in vaccination rates as compared to neighboring counties. The ineffectiveness of the campaign in preventing flu at the community level is likely due the small number of children vaccinated. This small proportion of population vaccinated, was insufficient to achieve herd immunity the protection of an entire community by preventing infectious disease spread due to lack of susceptible hosts. The county-level ILI data did not show any effects, likely because only 1,200 children were vaccinated in counties with a total population of over 800,000 people, far too small a ratio to achieve herd immunity, even assuming some baseline external vaccination rate.5 The slightly significant rise in ILI in Cobb/ Douglas compared to the state average was likely due to unexamined factors in the study, including baseline hospital visitation variation, population den-
sity, or reporting methods. Absenteeism in participating schools, a proxy for flu, was expected to demonstrate any effects the clinics may have had on reducing community flu burden, as the school populations were smaller, and the proportion of children vaccinated could conceivably have achieved herd immunity. However, the low proportion of students vaccinated (4.9 40%), was not large enough to reach the herd immunity threshold for flu, leading to our null findings in absenteeism differences. A previous SLIV study showed similar null results for differences in overall absenteeism between intervention and control schools.16 However, in the same study there was a significant difference in absenteeism between vaccinated children and those who did not participate. If absenteeism data was available by individual student for this analysis, perhaps a protective effect would have been observed, though it would demonstrate community-level flu prevention. Within the participating schools, Hispanic students, who are sometimes under-vaccinated, were more likely to participate in whites. However, black students, another traditionally under-vaccinated group, were less likely to get vaccinated than white students. These results are not entirely unexpected, as some previous studies, such as the CDC analysis of H1N1 flu rates measured through the BRFSS, found whites and Hispanics to have similar influenza vaccination rates that were higher than blacks.7 However, they do proStanford Journal of Public Health
vide an important insight that Hispanics, a sometimes undervaccinated group, participated heavily in the vaccination campaign. Females were more likely than males to be vaccinated, an unexpected trend that could be explained by handling of parental consent forms or many other unknown factors. In addition, vaccination rates showed no correlation with school lunch enrollment, likely because only 12 data points (one for each school) were used. Results from GRITS data indicate that Cobb and Douglas counties experienced a significantly higher rise in vaccination rates from 2008-9 to 2010-11 than neighboring control county Gwinnett. Rates actually rose in all three counties, likely indicating that the H1N1 pandemic led to overall rising interest and participation in influenza vaccination. In total, an additional 2,236 vaccinations were observed in 2010-11 compared to baseline in Cobb and Douglas counties. A number of the excess vaccinations came from children
newly vaccinated in the school clinics. However, the reliability of GRITS data for flu vaccinations specifically is not known. If flu vaccinations are not often entered in GRITS, adding 1,188 vaccinations could lead to a spurious rise in vaccination rates in the intervention counties compared to the control. The logistic regression model showed that both previous vaccination status and residence in the intervention county were strong predictors of likelihood of vaccination in 2010-11. Because the effect modification of residence in the intervention county on the predictive power of prior flu vaccination was not significant, we could not conclude that the SLIV clinics vaccinated children who would not otherwise have been immunized. This natural experiment demonstrates the impact of a real-time SLIV program after the H1N1 pandemic. The results indicate that piecemeal SLIV programs that do not involve all schools in a given area or do not vaccinate a large enough portion
of students to achieve herd immunity will not show any effects on community flu outcomes. Achieving protective effects would require significantly more participation than was seen in this program. Going forward, public health officials need to assess whether high levels of participation are feasible, and if true community, rather than individual, prevention of flu is the goal of future programs. Conclusions Within two metro Atlanta counties, Georgias SLIV clinics failed to have a measurable effect on community flu burden, but were associated with a rise in vaccination rates compared to a demographically similar neighboring county. This study provides the first significant evidence-based guideposts that can be used for post-pandemic influenza vaccination programming to reach children in the state of Georgia. Going forward, future SLIV programs may be useful in Georgia, but should be carefully evaluated for their goals and scale of the efforts involved.
36
1. Thompson WW. Mortality Associated With Influenza and Respiratory Syncytial Virus in the United States. JAMA. 2003;289(2):179-186 2. Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333-40. 3. Monto AS, Sullivan KM. Acute respiratory illness in the community. Frequency of illness and the agents involved. Epidemiol Infect. 1993;110(1):145-60. 4. Glezen WP, Couch RB, MacLean RA, et al. Interpandemic influenza in the Houston area, 1974-76. N Engl J Med. 1978;298(11):587592. 5. Glezen W, et al. Direct and indirect effectiveness of influenza vaccination delivered to children at school preceding an epidemic caused by 3 new influenza virus variants. J Infect Dis. 2010; 202(11): 1626-33 6. Neuzil KM, Hohlbein C, Zhu Y. Illness Among Schoolchildren During Influenza Season: Effect on School Absenteeism, Parental Absenteeism From Work, and Secondary Illness in Families. Arch Pediatr Adolesc Med. 2002;156(10):986-991. 7. Setse RW, Euler GL, Gonzalez-Feliciano AG, et al. Influenza Vaccination Coverage --- United States, 2000--2010. MMWR. 2011;60(1):38-41. 8. Centers for Disease Control. Influenza Vaccination Coverage Among Children and Adults --- United States, 2008--09 Influenza Season. MMWR. 2009;58(39):1091 To view the rest of the references for this paper, please refer to page 43.
Volume 3 Issue 1 Winter 2013
37
IVF Coverage: A Policy and Cost Conundrum
Elizabeth Melton
While IVF may be tremendously gratifying for parents rearing healthy babies, a fraction of IVF-conceived children are afflicted by a host of issues. Developmental, cognitive, musculoskseletal, and even related maternal harms warrant attention as literal and figurative costs of IVF. Children born out of IVF tend to be preterm and/or small-for-gestational age (SGA) with respect to the parturient population.4 After extensive matching on maternal characteristics (age, parity, ethnic origin, height, weight, smoking habits, obstetric/medical history), pregnancy outcome, delivery, neonatal outcome, pueriperium, and obstetric department in four Dutch university centers, authors Koudstaal et al discovered that gestational age at delivery was about 3 days shorter in IVF pregnancies. In addition, nearly two-thirds of the Obstetric and perinatal outcome and preliminary results of development of children born after in vitro maturation of oocytes data set was comprised of preemie babies, and SGA was present in half of those.4 What is more, higher SGA proportions in the IVF group (16.2 as opposed to 7.9%) necessitated more intensive neonatal care4. Adverse Outcomes of IVF/ICSI Pregnancies Vary Photo courtesy of Elizabeth Melton Depending on Aetiology of Infertility also utilized Danish Pictured is a premature baby whos life depends on the ventilator
Price of Pregnancy:
national registries to compile preterm and normal delivery statistics. Judging outcomes of 225 IVF pregnancies against those of a 26,870 Finnish controls (naturally conceived live births), Langhoff-Roos et al confirmed that IVF significantly increased odds of having an extremely preterm delivery rather than a very preterm delivery.5 Other studies have concluded that
IVF pregnancies were associated with, higher incidences of preterm birth, low birth weight, small for gestational age (SGA) infants, and NICU admissions.6 Marlow et al further contends that births after less than 26 weeks of gestation have a higher prevalence of neurological and developmental disabilities within the first two years of life. In the UK and Ireland, chil-
dren born in 1995 at less than or equal to 25 weeks of gestation were evaluated for cognitive impairments at 30 months of age.7 Disability was characterized as: severe, moderate, or mild, and classmates were matched for age and sex as controls. Each subject was scored by seven developmental pediatricians and eight psychologists on the Kaufman Assessment Battery for Children scale (K-ABC). Mental Processing Composite Scores were significantly lower in preterm cohorts on the order of ten and nine points for boys and girls respectively, whereas all of the control infants boasted similar scores across four scales of the K-ABC.7 Marlows study elucidates the very real propensity of IVF births to manifest in cognitive, neuromotor, vision, hearing, and overall disability. Twenty percent of extremely preterm babies later revealed signs of spastic and dyskinetic cerebral palsy, and 15% displayed spastic diplegia.7 Statistics highlighting even greater costs are that 21% of IVF children exhibiting some form of cognitive impairment, 12% with cerebral palsy, and of 86% still demonstrating severe retardation at age six4. Fifteen of those children were non-walkers, fifteen had moderate motor disabilities, four were hemiplegic, and nine were quadriplegic.7 Observations in Marlow, LanghoffRoos, and Koudstaals studies illustrate that greater cognitive impairment and poorer educational achievement were repeatedly noted in school-age kids of extremely low birth weight versus those born at full gestational term, raising concerns of costs Volume 3 Issue 1 Winter 2013
beyond payment simply for IVF procedures. Besides neo-natal issues, maternal vaginal blood loss, placenta praevia, and Caesarean sections stem from preterm pregnancies.4 Preterm births are also connected to spontaneous abortions or stillbirths, history of two or more induced abortions, young maternal age, low pre-pregnancy weight, nulliparity, previous preterm birth, intrauterine exposure to DES, incompetent cervix, uterus anomaly, pylelonephritis, and low weekly weight gainall of which demand rigorous medical, and hence economical, attention.4 Modeling the IVF Market: Variances between IVF and control pregnancies yield maladies feeding skyrocketing healthcare expenditures.4 As of late, there have been several cost-effectiveness comparisons across IVF and other infertility solutions available. Previous IVF decision-making models have not been realistic. Pragmatic models must account for cancelled cycles, decreases in pregnancy rates of subsequent cycles, frozen embryo transfers, and dropout. Pashayan et al sought to model the cost-effectiveness of primary offer IVF as opposed to IVF in partners after IUI attempts fell short. Intrauterine Insemination (IUI) and In-Vitro Fertilization (IVF) have been deemed first-line treatments for couples ailing from unexplained or male subfertility.3 IUI, sadly, is seldom successful on its own. Ensuing IVF treatment tacks on to already lofty prices of infertility. UKs 1995-1999 Human Fertilization and Embryology Authority (HFEA) population-
based register served as the standard for average live birth rates of IVF pregnancies. NICE, the UK National Institute for Clinical Excellence, advocates for six cycles of Unstimulated Intrauterine Insemination (U-IUI) for unexplained or male subfertility.3 Consistent with NICEs recommendation, Pashayans model mimics the clinical experience of 100 hypothetical couples randomized to either six rounds of: U-IUI + 1 round of IVF, S-IUI (Stimulated IUI) + 1 round of IVF, or simply 1 round of IVF. Cost was interpreted as the sum of IUI and IVF health services, with an incremental cost-effectiveness ratio represented by: [((cost of IUI + IVF arrangements) (cost of IVF))/ (difference in number of live births produced)]. Six cycles of U-IUI and one cycle of IVF totaled 495,9003. ICER for a primary round of IVF versus U-IUI and subsequent IVF was cited as 18,000 to 14,200 per live birth, and rose with each auxiliary IVF cycle. In the same vein, cost of an S-IUI + IVF combination was circa 369,000, but could reach up to a maximum of 759,800. ICER of regular IVF weighed against S-IUI + IVF ranged from 15,000 to 13,000 for each newborn.3 To put costs in a more societal perspective, six cycles of IUI followed by one IVF cycle amplifies the total fertility expenditure of the 100 modeled couples by a minimum of 174,200.3 More unsettling, this deficit bars 54 (out of the supposed 100) couples from acquiring IVF treatment, and at least 14 of those parents would have achieved live births3. Ultimately, it is more cost-effective
38
Stanford Journal of Public Health
39
for couples with male or unexplained subfertility to solely undergo IVF in preference to pursuing IUI. Even when only S-IUI is employed in lieu of U-IUI, costs up to 438,000 is prevented funds sufficient to cover 136 IVF cycles, facilitating no less than 35 live births. Opportunity costs of IUI-use induce unwanted economic and psychological wastefulness.3 Nelson et al is yet another UK-based research group jumping on the IVF prediction model bandwagon. Past studies have been tainted by inadequate sample size and lack of external validation. Accordingly, Nelson et al developed a prototype feasible with moderate discrimination and excellent calibration.1 Utilizing the Human Fertilisation and Embryology Authority database, predictors of live birth (the universal unit of success in the realm of IVF research) were examined both in IVF and spontaneous pregnancies taking place between 2003 and 2007.9 This model uniquely acknowledged effects of donor oocytes, ICSI cycle frequency, previous spontaneous or IVF-related births, and fetal loss to more accurately predict healthy pregnancies. As a result, Nelson et al learned that odds of one live birth was 23.4 per 100 IVF cycles. Another such model is the Markov model of Fiddelers et al. This model centered around two characteristics: a maximum of three cycles, and choice of similar or constructive transfer policies. Similar referred to one of the following recipes: (1 eSET + 2 STP), (1 eSET + 2 DET), (1 eSET + 1 STP + 1 DET), or (1 STP + 2 DET). Conversely, con-
structive transfer policy consisted of either three eSET, three STP, or three DET cycles.8 Total fertility failure is defined as: no transfer, pregnancy with one or more children, complications such as miscarriage and stillbirth, or no pregnancy. Moreover, the Markov model delineates stopping IVF as: 2 cycles cancelled in a row, personal-initiated dropout, a maximum of three cycles (all variations: eSET, DET, or STP), or a live birth. To generate this model, costs were calculated two weeks prior to randomization for each couple, and then once more six weeks thereafter. Overall, Fiddelers et al found that hormonal stimulation, laboratory fees, embryonic transfer, and maternal medical attention encompassed a majority of IVF expenses.8 Second-order Monte Carlo Simulations communicated poor trajectories of cost-effectiveness for intermixture trials of the three ART selections. Contrastingly, three cycles of eSET, DET, or STP alone were highly cost-effective.8 Among solo rounds of eSET, DET, and STP, cost-effectiveness thresholds were conveyed by cost per live birth. Three eSET cycles required an incremental cost increase of 7,350 for one auxiliary live birth. Alternatively, three rounds of STP call for 7350 - 15,250 cost increases for one live birth.8 Lastly, while DET is the most efficacious of the techniques, it is also the priciest. Three DET cycles necessitate over 15,250 per live birth.8 Cost of Contentment: Although Cost-effectiveness of primary offer of IVF vs. primary offer of IUI followed by IVF (for IUI failures) in couples with
unexplained or mild male factor subfertility, Cost-effectiveness of seven IVF strategies: results of a Markov decision-analytic model, and Prediction of live birth and extremes of response in stimulated cycles implications for individualization of therapy are novel in their field, policymakers must bear in mind that these models are limited by their inability to be extrapolated to the mainstream.3 Technically, substantially larger cohorts in randomized, controlled trials accomplish this goal. Unfortunately, ethical review boards keep studies of this nature on tight leashes. In turn, obtaining sizable, homogeneous cohorts is practically impossible. IUI data, for instance, is heterogeneous in regard to subject demographics, ovarian stimulation regimes, inseminations per cycle, insemination timing, and methods of sperm preparation.3 Omission of diagnostic, incident/followup appointment, and counseling fees (not to mention psychological anguish) renders these models inadequate. For many reasons, these models are not all-inclusive representations of costimpermissible when estimating costs of politically polarizable health policies. ART and ACAAntagonistic?: By and large, insurance plans in the US fail to cover infertility. Distressingly, mandates are not necessarily consigned to where insured individuals live or work. Instead, the location of policy issuance dictates the obligations by which insurance companies abide. Common institutions exempt from requirements in these states are small businesses, reStanford Journal of Public Health
ligious organizations, and selfinsured companies.11 In 2014, reduced savings on non-covered tax-deductible procedures will cause costs for assisted reproductive technologies, namely, IVF, to intensify. Only $2500 will be allocated to Flexible Spending Accounts. Though a cap has not been placed, employers will self-select contribution limits.10 Meanwhile, the deductible medical expenses threshold will be augmented from 7.5 to 10% of Adjusted Gross Income (AGI).10 Fifteen of the fifty states have infertility insurance regulations: Arkansas, California, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia.10 Nonetheless, precisely what coverage entails fluctuates greatly from state to state. On December 16, 2011, consumers, states, employers and issuers were furnished with more timely information as they work towards establishing Affordable Insurance Exchanges and making decisions for 2014. The Department of Health and Human Services issued a comprehensive, affordable and flexible bulletin with policies that giving states more flexibility in ACA protocol.11 ACA of the future ensures that health plans (individual and small group markets both inside and outside of the Affordable Insurance Exchanges), offer a comprehensive package of items and services, known as Essential Health Benefits. Hinging on scientific and economical exploration, IVF may or may not become part and parcel of the Essential Health Benefits. Activists, relatives, politiVolume 3 Issue 1 Winter 2013
cians, and infertility-plagued couples alike are striving to instate a novel federal bill to enhance IVFs chances of attaining Essential Health Benefit status. The Family Act aims to bestow tax credits to couples struggling to surmount the overwhelming out-of-pocket costs of infertility treatment. Presently, families who adopt are tendered similar tax credits. Infertile couples are now demanding the same financial assistance to start their own families. Family Act Legislation would provide a maximum lifetime tax credit of $13,360 to families with an adjusted gross income of less than $182,500, and yearn for children. To utilize IVF, taxpayers must have been diagnosed as infertile by a licensed physician with an indicated course of treatment as IVF.12 In Novem-
ber 2011, espousal for The Family Act grew leaps and bounds when Rep. John Lewis (D-GA) announced the legislation in the U.S. House of Representatives.11 For too many of those people, the cost of treatment will silence their dreams of having children forever. Thats not right, fair or just. I believe that access to decent health care should be a fundamental right, not a privilege, stated Rep. Lewis in the hopes that The Family Act of 2011 will be instated.12 Twenty-one members of the House co-sponsor the Family Act. A preponderance of Representatives aspiring for Family Act passage is LeftWing-affiliated.12 Introduced to the Senate in May of 2011 by Kirsten Gillibrand, (D-NY), Daniel Akaka, HI, Daniel Inouye, HI, and Mary Landrieu, LA agreed to co-spon-
Photo courtesy of Elizabeth Melton In vitro fertilization can provide families previously incapable of having children with the opportunity to do so.
40
41
sor: all of whom hail from the Democratic Party as well.12 Because The Family Act would also apply to treatments to preserve fertility for cancer patients, such as egg-freezing, big-name organizations, namely The American Cancer Society, American Congress for Obstetricians and Gynecologists, American Fertility Association, American Society for Reproductive Medicine, Leukemia and Lymphoma Society, Livestrong, National Hispanic Medical Association, RESOLVE, and the United States Hispanic Chamber of Commerce now lobby for Family Act efforts, too.11 Progress of The Family Act of 2011, S 965/HR 3522, corresponds to 48% Senate support, with 4,830 alerts taken (with a
goal of 10,000).12 Whether or not this bill is enacted into law, its potential incorporation into the Affordable Care Act remains to be seen. IVF for the Win: An upsurge in IVF demand, and the snowballing costs of neonatal services aforementioned due to influx of IVF-related premature babies or multiple births has obviously sparked fear in the healthcare sphere.1 It is inevitable that the rising tide of consumer demand of IVF as treatment options for a legitimate disease, will catalyze much needed change.11 Infertility has a highly heterogeneous etiology, warranting supplementary research. External validity of maternal and natal studies and
economical models must be bettered. Clinical efficacy of infertility treatments brings about a mass of unanswered questions: is there availability of PGD? Can healthcare incorporate infertility screening? Can severity of infertility be assessed via genotyping and preclude individuals from coverage? What will be the protocol for covering family counseling and planning? Health policy opens a whole new can of worms. If Essential Health Benefits sanctions treatment for infertility, what would be the immediate effects? Will adverse enrollee selection ensue? Fundamentally, IVF in US Health Policy is dependent on the value our nation should place on IVF successone live birth.
org/get-involved/the-affordable-ca 12. Family Act of 2011 Takes a Positive Step Forward. Family Act of 2011 Takes a Positive Step Forward. Fertilityauthority.com, Apr. 2011. Web. 20 May 2012. <http://www.fertilityauthority.com/articles/family-act-2011-takes-positivestep-forward>. References for Childhood Obesity: A Growing Epidemic from page 14 1. AIDS Timeline. Website. Available at: http://www.avert.org/aids-timeline.htm. Accessed November 11, 2012. 2. US Obesity Rate Leveling Off, at About One-Third of Adults. Website. Available at: http://usatoday30.usatoday.com/ news/health/weightloss/2010-01-13-obesity-rates_N.htm. Accessed November 11, 2012. 3. Barr, Donald. MD, PhD. Physician and Associate Professor of Sociology and Human Biology at Stanford University. Interviewed November 9, 2012. 4. Childhood Obesity Facts. Website. Available at: http://www.cdc.gov/healthyyouth/obesity/facts.htm. Accessed November 28, 2012. 5. Childhood Obesity. Website. Available at: http://www.healthiergeneration.org/about.aspx?id=3439. Accessed November 26, 2012. 6. US Obesity Rate Leveling Off, at About One-Third of Adults. Website. Available at: http://usatoday30.usatoday.com/ news/health/weightloss/2010-01-13-obesity-rates_N.htm. Accessed November 11, 2012. 7. Gardner, Christopher. PhD. Associate Director of Nutrition Studies at the Stanford Prevention Research Center and Associate Professor of Medicine at Stanford University. Interviewed November 9, 2012. 8. Michelle Obama Agrees: Obesity is Absolutely a National Security Threat. Website. Available at: http://www.theblaze. com/stories/michelle-obama-agrees-obesity-is-absolutely-a-national-security-threat/. Accessed November 11, 2012. 9. US Obesity Rate Leveling Off, at About One-Third of Adults. Website. Available at: http://usatoday30.usatoday.com/ news/health/weightloss/2010-01-13-obesity-rates_N.htm. Accessed November 11, 2012. 10. Gardner, Christopher. PhD. Associate Director of Nutrition Studies at the Stanford Prevention Research Center and Associate Professor of Medicine at Stanford University. Interviewed November 9, 2012. 11. Richmonds Soda Tax Campaigner. Website. Available at: http://www.sfgate.com/health/article/Richmond-s-soda-taxcampaigner-3944783.php. Accessed November 21, 2012. 12. Double Up Food Bucks: How it Works. Website. Available at: http://www.doubleupfoodbucks.org/how-it-works. Accessed November 21, 2012. 13. New Rules for School Meals Aim at Reducing Obesity. Website. Available at: http://www.nytimes.com/2012/01/26/us/ politics/new-school-lunch-rules-aimed-at-reducing-obesity.html?_r=1&. Accessed November 11, 2012. 14. Michelle Obama Unveils Anti-Childhood Obesity Action Plan. Website. Available at: http://www.politicsdaily. com/2010/05/11/michelle-obama-unveils-anti-childhood-obesity-action-plan/. Accessed November 11, 2012. 15. Lets Move! Website. Available at: http://www.letsmove.gov. Accessed November 11, 2012. 16. AIDS Timeline. Website. Available at: http://www.avert.org/aids-timeline.htm. Accessed November 11, 2012. References for Infertility: A Plague Gone Unnoticed page 32 1. Fidler, AT, Bernstein J. Infertility: From a Personal to a Public Health Problem. Available from: PubMed Central. 2. Harvard Medical School, Massachusetts General Hospital. Fertility and Mental Health. Available at: http://www. womensmentalhealth.org/specialty-clinics/infertility-and mental-health/ 3. International Council on Infertility Information Dissemination. Walker PJ. The impact of Bragdon v. Abbot on persons affected by infertility. Available at: http://www.inciid.org/printpage.php?cat=benefits&id=414 4. Mental Health: Trying to conceive, pregnancy, and mental health. womenshealth.gov [online]. Available at; womenshealth.gov database. 5. National Conference of State Legislatures. State Laws Related to Insurance Coverage for Infertility Treatment. Available at: http://www.ncsl.org/issues-research/health/insurance-coverage-for-infertility-laws.aspx 6. Resolve: The National Infertility Association. Insurance Coverage in Your State. Available at: http://www.resolve.org/ family-building-options/insurance_coverage/ state-coverage.html#California 7. The Natural Health Website for Women . Natural Solutions to Infertility. Available at: http://www.marilynglenville. com/infertility.htm 8. The New York Times. Tarkan L. Fertility Clinics Begin to Address Mental Health. Available at: http://www.nytimes. com/2002/10/08/health/fertility-clinics-begin-to-address-mental-health.html?pagewanted=all&src=pm
1. The Oldest and Largest Infertility (INCIID) Adoption. Parenting, Pregnancy Online Community. A History of IVF. The Oldest and Largest Infertility (INCIID) Adoption. Parenting, Pregnancy Online Community), 2004. Web. 20 May 2012. <http://www.inciid.org/printpage.php?cat=ivf>. 2. The Cost-Effectiveness of IVF. IVF News: The Cost-Effectiveness of IVF. American Society for Reproductive Medicine, 17 Oct. 2007. Web. 14 May 2012. <http://www.ivf.net/ivf/the-cost-effectiveness-of-ivf-o3027.html>. 3. Pashayan, N, Lyratzopoulos, G, Mathur, R. Cost-effectiveness of primary offer of IVF vs. primary offer of IUI followed by IVF (for IUI failures) in couples with unexplained or mild male factor subfertility. BMC Health Services Research, vol. 6, article 80, pp. 111, 2006. 4. Koudstaal, J., Braat, D.D.M, Bruinse, H.W., Naaktgeboren, N., Vermeiden, J.P.W., and Visser, G.H.A. Obstetric and perinatal outcome and preliminary results of development of children born after in vitro maturation of oocytes. Hum Reprod (2006) 21(6): 1508-1513. 5. Langhoff-Roos J, Kesmodel U, Jacobsson B, et al. Spontaneous preterm delivery in primiparous women at low risk in Denmark: population-based study. BMJ 332(7547):9379. 2006. 6. Kuivasaari-Pirinen P, Raatikainen K, Hippelinen M, Heinonen S. Adverse Outcomes of IVF/ICSI Pregnancies Vary Depending on Aetiology of Infertility. ISRN Obstet Gynecol. 2012;2012:451915. Epub 2012 Apr 9. 7. Marlow, N., Wolke, D., Bracewell, M.A., & Samara, M., for the EPICure Study Group (2005). Neurologic and developmental disability at six years of age after extremely preterm birth. New England Journal of Medicine, 352, 919. 8. Fiddelers AA, Dirksen CD, Dumoulin JC, van Montfoort AP, Land JA, Janssen JM, Evers JL, Severens JL: Costeffectiveness of seven IVF strategies: results of a Markov decision-analytic model. Hum Reprod 2009, 24(7):16481655. 9. Nelson SM, Yates RW, Fleming R. Prediction of live birth and extremes of response in stimulated cycles implications for individualization of therapy. Hum Reprod 2007;22:241421. 10. State Laws Related To Insurance Coverage for Infertility Treatment. Insurance Coverage for Infertility Laws. National Conference of State Legislatures, Mar. 2012. Web. 15 May 2012. <http://www.ncsl.org/issues-research/health/ insurance-coverage-for-infertility-laws.aspx>. 11. The Affordable Care Act and Infertility. The Affordable Care Act and Infertility RESOLVE: The National Infertility Association. RESOLVE: The National Infertility Association, 31 Jan. 2012. Web. 15 May 2012. <http://www.resolve.
42
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
43
9. What Health Care Reform Means For Infertility Coverage. Available at: http://healthcare.phoenix-blogs.com/whathealth-care-reform-means-for-infertility-coverage/
References continued from page 37
9. Shefer A. Healthy People 2020 Update History of Healthy People Healthy People 2020 launched December 2010 Achievement of Past Healthy People Objectives. 2011:1-11. 10. Monto a S, Davenport FM, Napier J a, Francis T. Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis. 1970;122(1):16-25. 11. Carpenter LR, Lott J, Lawson BM, et al. Mass distribution of free, intranasally administered influenza vaccine in a public school system. Pediatrics. 2007;120(1):e172-8. 12. Effler PV, Chu C, He H, et al. Statewide school-located influenza vaccination program for children 5-13 years of age, Hawaii, USA. Emerg Infect Dis. 2010;16(2):244-50. 13. Piedra PA, Gaglani MJ, Kozinetz CA, et al. Herd immunity in adults against influenza-related illnesses with use of the trivalent-live attenuated influenza vaccine (CAIV-T) in children. Vaccine. 2005;23(13):1540-8. 14. King JC, Stoddard JJ, Gaglani MJ, et al. Effectiveness of school-based influenza vaccination. N Engl J Med. 2006;355(24):2523-32. 15. King JC, Stoddard JJ, Gaglani MJ, et al. Effectiveness of school-based influenza vaccination. N Engl J Med. 2006;355(24):2523-32. 16. Shrestha SS, Swerdlow DL, Borse RH, et al. Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009-April 2010). Clin Infect Dis. 2011;52 52(Suppl 1):S75-82. 17. Redd SC, Shaw MW. Why H1N1 Still Matters. In: CDC Grand Rounds. Centers for Disease Control and Prevention; 2010. Available at: http://www.cdc.gov/about/grand-rounds/archives/2010/09-September.htm. 18. Jhung MA, Swerdlow D, Olsen SJ, et al. Epidemiology of 2009 pandemic influenza A (H1N1) in the United States. Clin Infect Dis. 2011;52(Suppl 1):S13-26. 19. Iuliano AD, Dawood FS, Silk BJ, et al. Investigating 2009 pandemic influenza A (H1N1) in US schools: what have we learned? Clin Infect Dis. 2011;52 (Suppl1):S161-7. 20. Chao DL, Halloran ME, Longini IM. School opening dates predict pandemic influenza A(H1N1) outbreaks in the United States. J Infect Dis. 2010;202(6):877-80. 21. Cawley J, Hull HF, Rousculp MD. Strategies for implementing school-located influenza vaccination of children: a systematic literature review. J School Health. 2010;80(4):167-75.
Interested in joining the journal staff as a writer, editor, or production team member?
Email: stanfordjournalofpublichealth@gmail.com
Want more information about sumbitting your work?
We are looking for research papers in the field of public health from current and former Stanford students, both undergraduate and graduate, from all departments. These papers may stem from honors theses, research and analysis papers, and independent research or projects. Our main criteria are that any research includes methodological rigor, papers are well written, and the content of the submission is relevant and consistent with the four journal sections.
See Submit to SJPH at sjph.stanford.edu
44
Stanford Journal of Public Health
Volume 3 Issue 1 Winter 2013
45
sjph.stanford.edu
Vous aimerez peut-être aussi
- 2009 Book MaternalAndChildHealth PDFDocument584 pages2009 Book MaternalAndChildHealth PDFThierry UhawenimanaPas encore d'évaluation
- Publics and their health: Historical problems and perspectivesD'EverandPublics and their health: Historical problems and perspectivesPas encore d'évaluation
- Stanford Journal of Public Health - Volume 1 - Issue 1 - Spring 2011Document48 pagesStanford Journal of Public Health - Volume 1 - Issue 1 - Spring 2011stanfordjphPas encore d'évaluation
- The Politics of Potential: Global Health and Gendered Futures in South AfricaD'EverandThe Politics of Potential: Global Health and Gendered Futures in South AfricaPas encore d'évaluation
- Research Paper Public HealthDocument4 pagesResearch Paper Public Healthzqbyvtukg100% (1)
- Diseases of Poverty: Epidemiology, Infectious Diseases, and Modern PlaguesD'EverandDiseases of Poverty: Epidemiology, Infectious Diseases, and Modern PlaguesPas encore d'évaluation
- The en Cultured Body-BookDocument174 pagesThe en Cultured Body-BooksidorelaPas encore d'évaluation
- Community Health Final-Nursing Final Turn inDocument8 pagesCommunity Health Final-Nursing Final Turn inapi-719825532Pas encore d'évaluation
- Public Health Group AssignmentDocument7 pagesPublic Health Group AssignmentNANNYONGA OLGAPas encore d'évaluation
- Breast Cancer Screening and Prevention: Health Screening and PreventionD'EverandBreast Cancer Screening and Prevention: Health Screening and PreventionPas encore d'évaluation
- Iastate DissertationDocument8 pagesIastate DissertationWriteMyCollegePaperForMeSingapore100% (1)
- Global health and the new world order: Historical and anthropological approaches to a changing regime of governanceD'EverandGlobal health and the new world order: Historical and anthropological approaches to a changing regime of governancePas encore d'évaluation
- Milestones in Public HealthDocument279 pagesMilestones in Public HealthRick Leung83% (6)
- Lead Wars: The Politics of Science and the Fate of America's ChildrenD'EverandLead Wars: The Politics of Science and the Fate of America's ChildrenÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Evaluation:: Basinang, Rica Kyrie T BSN 2 Community Health NursingDocument7 pagesEvaluation:: Basinang, Rica Kyrie T BSN 2 Community Health NursingloviPas encore d'évaluation
- Critical Medical Anthropology: Perspectives in and from Latin AmericaD'EverandCritical Medical Anthropology: Perspectives in and from Latin AmericaJennie GamlinÉvaluation : 5 sur 5 étoiles5/5 (1)
- Community and Public Health Nursing Evidence For Practice Second NorthDocument61 pagesCommunity and Public Health Nursing Evidence For Practice Second Northpamela.stanley399100% (43)
- Pre-teen and Teenage Pregnancy: a 21st century realityD'EverandPre-teen and Teenage Pregnancy: a 21st century realityÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Mass Media and Mental Illness A Literature ReviewDocument6 pagesMass Media and Mental Illness A Literature ReviewaflsjizafPas encore d'évaluation
- Stat Winter 2015 2Document12 pagesStat Winter 2015 2api-236188238Pas encore d'évaluation
- Ketan Shukla Synopis or Resesarch Proposal.Document11 pagesKetan Shukla Synopis or Resesarch Proposal.ketanshukla.india.123Pas encore d'évaluation
- Health-Related Controversies in The PhilippinesDocument11 pagesHealth-Related Controversies in The PhilippinesAna Marie Lariba TocmoPas encore d'évaluation
- Public Health Research PaperDocument8 pagesPublic Health Research Papersvfziasif100% (1)
- Epidemiology Dissertation IdeasDocument8 pagesEpidemiology Dissertation IdeasBestCustomPapersSingapore100% (1)
- Health Research Paper Topic IdeasDocument8 pagesHealth Research Paper Topic Ideascakdezbr100% (1)
- End-Of-life Issues For Aboriginal Patients A Literature ReviewDocument7 pagesEnd-Of-life Issues For Aboriginal Patients A Literature ReviewafmabreouxqmrcPas encore d'évaluation
- Tugas Merangkum Epidemiologi Safira M.20.02.050Document5 pagesTugas Merangkum Epidemiologi Safira M.20.02.050safira saalPas encore d'évaluation
- Kiran PresentationDocument4 pagesKiran PresentationZaim versePas encore d'évaluation
- Sample Public Health Research PaperDocument8 pagesSample Public Health Research Paperaflbrozzi100% (1)
- A Case Study of Client B.T. and Client M.L. On Their Wellness StatusDocument74 pagesA Case Study of Client B.T. and Client M.L. On Their Wellness StatusClaire MachicaPas encore d'évaluation
- Reimagining Global Health: An Introduction by Paul FarmerDocument13 pagesReimagining Global Health: An Introduction by Paul FarmerUniversity of California Press100% (1)
- Diseases of ChildrenDocument1 092 pagesDiseases of Childrenihb80Pas encore d'évaluation
- Diseases of Children in The Subtropics and TropicsDocument1 092 pagesDiseases of Children in The Subtropics and TropicscaptaincandyPas encore d'évaluation
- How To Write A Public Health Research PaperDocument8 pagesHow To Write A Public Health Research Paperwqbdxbvkg100% (1)
- What+is+Health+Education AJPHDocument12 pagesWhat+is+Health+Education AJPHAthena AlabadoPas encore d'évaluation
- Community MedicineDocument49 pagesCommunity MedicineRiyaz AhamedPas encore d'évaluation
- Introduction To Health Promotion: © John Hubley & June Copeman 2008Document24 pagesIntroduction To Health Promotion: © John Hubley & June Copeman 2008alifzxPas encore d'évaluation
- Local Media2455143450208113591Document13 pagesLocal Media2455143450208113591SadakoPas encore d'évaluation
- The Effects of Poverty On The Accessibility of Health Care in Low Income Families Within Lipa CityDocument23 pagesThe Effects of Poverty On The Accessibility of Health Care in Low Income Families Within Lipa CityAlexa BulataoPas encore d'évaluation
- Running Head: Anti-Vaccination CultureDocument10 pagesRunning Head: Anti-Vaccination Cultureapi-264474518Pas encore d'évaluation
- Public Health Research PapersDocument7 pagesPublic Health Research Papersp1zajywigyd2100% (1)
- JHSPH Prospectus 11 12Document80 pagesJHSPH Prospectus 11 12franz_sitepuPas encore d'évaluation
- Ebook PDF Community and Public Health Nursing Evidence For Practice An Epidemiologic Approach PDFDocument41 pagesEbook PDF Community and Public Health Nursing Evidence For Practice An Epidemiologic Approach PDFvenus.roche638100% (36)
- Thesis Related To Community Health NursingDocument8 pagesThesis Related To Community Health Nursingtfwysnikd100% (1)
- What Makes Your Study Unique?Document3 pagesWhat Makes Your Study Unique?Samantha RubicaPas encore d'évaluation
- Global Health Research Paper TopicsDocument6 pagesGlobal Health Research Paper Topicsgihodatodev2100% (1)
- Communication and Health Media Marketing and Risk 1St Edition Charlene Elliott Full ChapterDocument67 pagesCommunication and Health Media Marketing and Risk 1St Edition Charlene Elliott Full Chaptermarjorie.timchula134100% (4)
- Section IDocument28 pagesSection Iyogi.kristiyantoPas encore d'évaluation
- Intro To PHPDocument18 pagesIntro To PHPHajra MirzaPas encore d'évaluation
- EJ1078866Document12 pagesEJ1078866valentinasecivirPas encore d'évaluation
- History of Public HealthDocument4 pagesHistory of Public HealthVanessa CarreonPas encore d'évaluation
- End of Life Care Literature ReviewDocument7 pagesEnd of Life Care Literature Reviewgvw6y2hv100% (1)
- Why Study Global Health?: Amatya A, Basel PDocument2 pagesWhy Study Global Health?: Amatya A, Basel PRika AskiaPas encore d'évaluation
- Research Paper Topics Public HealthDocument6 pagesResearch Paper Topics Public Healthkquqbcikf100% (1)
- Preventative Healthcare Literature ReviewDocument8 pagesPreventative Healthcare Literature Reviewapi-290166100100% (1)
- Institute For Career Research - Career As An Epidemiologist - Public Health Specialists Searching For The Causes and Cures of Diseases and EpidemicsDocument30 pagesInstitute For Career Research - Career As An Epidemiologist - Public Health Specialists Searching For The Causes and Cures of Diseases and EpidemicsCynthia CPas encore d'évaluation
- Vaccinations History What They Are LessonDocument3 pagesVaccinations History What They Are Lessonsatishyadav8986575032Pas encore d'évaluation
- Sancticity AllDocument21 pagesSancticity AllJames DeHart0% (1)
- XS2 Pharma 0512 103 UK U-NiDocument2 pagesXS2 Pharma 0512 103 UK U-NiMilan MilovanovicPas encore d'évaluation
- Villa VeronicaDocument12 pagesVilla Veronicacj fontzPas encore d'évaluation
- Remo Vs DevanaderaDocument2 pagesRemo Vs DevanaderaZymon Andrew MaquintoPas encore d'évaluation
- Factual DescriptionDocument14 pagesFactual Descriptionaleena'Pas encore d'évaluation
- Basic Foundation of Iv TherapyDocument10 pagesBasic Foundation of Iv Therapyjanna mae patriarcaPas encore d'évaluation
- Corporation Essay ChecklistDocument5 pagesCorporation Essay ChecklistCamille2221Pas encore d'évaluation
- Chat GPT DAN and Other JailbreaksDocument11 pagesChat GPT DAN and Other JailbreaksNezaket Sule ErturkPas encore d'évaluation
- Wardancer 4e HomebrewDocument3 pagesWardancer 4e HomebrewWyjecPas encore d'évaluation
- SANCHEZ V DEMETRIOUDocument3 pagesSANCHEZ V DEMETRIOUShenna SunicoPas encore d'évaluation
- Parathyroid Agents PDFDocument32 pagesParathyroid Agents PDFRhodee Kristine DoñaPas encore d'évaluation
- Infinitives or Gerunds PDFDocument2 pagesInfinitives or Gerunds PDFRosa 06Pas encore d'évaluation
- Human Right and Humanitarian. by Solicitor KaturaDocument12 pagesHuman Right and Humanitarian. by Solicitor KaturaFlavian PangahPas encore d'évaluation
- Gamma Ray Interaction With Matter: A) Primary InteractionsDocument10 pagesGamma Ray Interaction With Matter: A) Primary InteractionsDr-naser MahmoudPas encore d'évaluation
- Coaching Skills For Optimal PerformanceDocument58 pagesCoaching Skills For Optimal PerformanceYodhia Antariksa100% (3)
- Comparative Analysis of Levis Wrangler & LeeDocument10 pagesComparative Analysis of Levis Wrangler & LeeNeelakshi srivastavaPas encore d'évaluation
- Pakistan's Professor Mafia - Pakistan - DAWNDocument5 pagesPakistan's Professor Mafia - Pakistan - DAWNMuhammad Bilal A. RPas encore d'évaluation
- Lesson 6 S and V AgreementDocument6 pagesLesson 6 S and V AgreementLinh Ngọc NguyễnPas encore d'évaluation
- SOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseDocument11 pagesSOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseMonicaPas encore d'évaluation
- When Karl Met Lollo The Origins and Consequences of Karl Barths Relationship With Charlotte Von KirschbaumDocument19 pagesWhen Karl Met Lollo The Origins and Consequences of Karl Barths Relationship With Charlotte Von KirschbaumPsicoorientación FamiliarPas encore d'évaluation
- Glgq1g10 Sci Las Set 4 ColoredDocument4 pagesGlgq1g10 Sci Las Set 4 ColoredPogi AkoPas encore d'évaluation
- 2.2 Push and Pull Sources of InnovationDocument16 pages2.2 Push and Pull Sources of Innovationbclarke113Pas encore d'évaluation
- BA BBA Law of Crimes II CRPC SEM IV - 11Document6 pagesBA BBA Law of Crimes II CRPC SEM IV - 11krish bhatia100% (1)
- Instructional MediaDocument7 pagesInstructional MediaSakina MawardahPas encore d'évaluation
- Last Speech of Shri Raghavendra SwamyDocument5 pagesLast Speech of Shri Raghavendra SwamyRavindran RaghavanPas encore d'évaluation
- Reflection IntouchablesDocument2 pagesReflection IntouchablesVictoria ElazarPas encore d'évaluation
- Food Corporation of India Zonal Office (N) A-2A, 2B, SECTOR-24, NOIDADocument34 pagesFood Corporation of India Zonal Office (N) A-2A, 2B, SECTOR-24, NOIDAEpaper awaazPas encore d'évaluation
- Formulating A PICOT QuestionDocument4 pagesFormulating A PICOT QuestionKarl RoblePas encore d'évaluation
- PSYCHODYNAMICS AND JUDAISM The Jewish in Uences in Psychoanalysis and Psychodynamic TheoriesDocument33 pagesPSYCHODYNAMICS AND JUDAISM The Jewish in Uences in Psychoanalysis and Psychodynamic TheoriesCarla MissionaPas encore d'évaluation
- 002 Constraints and Generalized Coordinates PDFDocument27 pages002 Constraints and Generalized Coordinates PDFNiveCeciliaPas encore d'évaluation
- The Russia Hoax: The Illicit Scheme to Clear Hillary Clinton and Frame Donald TrumpD'EverandThe Russia Hoax: The Illicit Scheme to Clear Hillary Clinton and Frame Donald TrumpÉvaluation : 4.5 sur 5 étoiles4.5/5 (11)
- An Autobiography of Trauma: A Healing JourneyD'EverandAn Autobiography of Trauma: A Healing JourneyÉvaluation : 5 sur 5 étoiles5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisD'EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (9)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryD'EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryÉvaluation : 4.5 sur 5 étoiles4.5/5 (157)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesD'EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesÉvaluation : 5 sur 5 étoiles5/5 (70)
- Stonewalled: My Fight for Truth Against the Forces of Obstruction, Intimidation, and Harassment in Obama's WashingtonD'EverandStonewalled: My Fight for Truth Against the Forces of Obstruction, Intimidation, and Harassment in Obama's WashingtonÉvaluation : 4.5 sur 5 étoiles4.5/5 (21)
- Modern Warriors: Real Stories from Real HeroesD'EverandModern Warriors: Real Stories from Real HeroesÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDD'EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDÉvaluation : 4.5 sur 5 étoiles4.5/5 (167)
- Crimes and Cover-ups in American Politics: 1776-1963D'EverandCrimes and Cover-ups in American Politics: 1776-1963Évaluation : 4.5 sur 5 étoiles4.5/5 (26)
- The Courage to Be Free: Florida's Blueprint for America's RevivalD'EverandThe Courage to Be Free: Florida's Blueprint for America's RevivalPas encore d'évaluation
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeD'EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeÉvaluation : 4.5 sur 5 étoiles4.5/5 (140)
- The Red and the Blue: The 1990s and the Birth of Political TribalismD'EverandThe Red and the Blue: The 1990s and the Birth of Political TribalismÉvaluation : 4 sur 5 étoiles4/5 (29)
- When Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfD'EverandWhen Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfÉvaluation : 5 sur 5 étoiles5/5 (36)
- Game Change: Obama and the Clintons, McCain and Palin, and the Race of a LifetimeD'EverandGame Change: Obama and the Clintons, McCain and Palin, and the Race of a LifetimeÉvaluation : 4 sur 5 étoiles4/5 (572)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionD'EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionPas encore d'évaluation
- The Deep State: How an Army of Bureaucrats Protected Barack Obama and Is Working to Destroy the Trump AgendaD'EverandThe Deep State: How an Army of Bureaucrats Protected Barack Obama and Is Working to Destroy the Trump AgendaÉvaluation : 4.5 sur 5 étoiles4.5/5 (4)
- Power Grab: The Liberal Scheme to Undermine Trump, the GOP, and Our RepublicD'EverandPower Grab: The Liberal Scheme to Undermine Trump, the GOP, and Our RepublicPas encore d'évaluation
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreD'EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreÉvaluation : 5 sur 5 étoiles5/5 (17)
- The Next Civil War: Dispatches from the American FutureD'EverandThe Next Civil War: Dispatches from the American FutureÉvaluation : 3.5 sur 5 étoiles3.5/5 (47)
- Workin' Our Way Home: The Incredible True Story of a Homeless Ex-Con and a Grieving Millionaire Thrown Together to Save Each OtherD'EverandWorkin' Our Way Home: The Incredible True Story of a Homeless Ex-Con and a Grieving Millionaire Thrown Together to Save Each OtherPas encore d'évaluation
- Don't Panic: Taking Control of Anxiety AttacksD'EverandDon't Panic: Taking Control of Anxiety AttacksÉvaluation : 4 sur 5 étoiles4/5 (12)
- Socialism 101: From the Bolsheviks and Karl Marx to Universal Healthcare and the Democratic Socialists, Everything You Need to Know about SocialismD'EverandSocialism 101: From the Bolsheviks and Karl Marx to Universal Healthcare and the Democratic Socialists, Everything You Need to Know about SocialismÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeD'EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeÉvaluation : 4.5 sur 5 étoiles4.5/5 (49)