Académique Documents
Professionnel Documents
Culture Documents
Ent
Transféré par
Geliza RamosTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ent
Transféré par
Geliza RamosDroits d'auteur :
Formats disponibles
Subject Topic Date Lecturer
ENT
Otorrhea 13 October 2010 Dr. Brendan Ferrolino
Pages
AY 2010-2011
Transcriber Jmie Editor
14
OUTLINE X-Section of the ear suppurative Otorrhea Tuberculosis External Ear Disorder microbiology Diffuse Otitis Externa Furuculosis Herpes Zoster Oticus Other External Ear Disorders media IV. Middle Ear Disorder Source: ppt. past tranx, book
ii. Pathogenesis iii. Sequences of event iv. Diagnosis v. Types 1. Suppurative a. Aerotitis Barotrauma b. Otitis Media with Effusion
c. Chronic d. Vi. Vii. management viii. Antimicrobial agents ix. Acute otitis media x. Recurrent otitis xi.
2. Non-Suppurative
I.
X-SECTION OF THE EAR
Malleus Incu s
Semicircul ar Canals Vestibular nerve Cochl ea Stapes Tympanic m
Auricle Tempora l bone External Auditory Meatus
Tensor Tympani
Eustachia n Tube
OTOSCOPIC EXAMINATION In performing otoscopic examination, you must first stabilize the ear by holding it so the patient wont feel pain as the speculum is being inserted. The mobile cartilaginous part of the ear must be pulled upward and backward before inserting the speculum Very basic , helps in determining the problem Mainstay for the investigation of the middle ear disease normally otoscopy will reveal nothing more of the middle ear than the lateral aspect of the tympanic membrane.
II.
OTORRHEA
abnormal discharge from the ear Characteristic (you must identify the appearance of the discharge as you examine and as you take the
history, in able to determine the pathology)
1. 2. 3. 4.
Consistency Color Amount Odor
serous, mucoid, purulent (transudate to exudates) clear, whitish, yellowish, bloody scanty, copious/ profuse non-foul, foul smelling (commonly ignored characteristic)
Possible Sources
a.
(anatomy and histology of ear canal must be considered)
1. External Ear Canal
stratified squamous epithelium
Bony portion formed by the tympanic part of the temporal bone skin is very thin and adherent the periosteum sothere is not much subcutaneous tissue accounting for the temperature and pain sensitivity of the medial canal skin Otorrhea 1 of 14
and can influence the pathogenesis and course of ear canal diseases such as necrotizing otitis externa. b. Cartilaginous portion Forms the lateral 2/3 of the external auditory canal Angled downward and forward relative to the bony medial third. So at otoscopy, the ear is pulled upward and backward. Has skin appendages such as hair follicles
2. Middle Ear Canal cells 3. Tissue/Bone Necrosis 4. CSF Leak comes out)
columnar, ciliated with mucous secreting goblet suppurative inflammation
( necrosis of the external,
middle or even the mastoid )
tear in dura mater due to trauma (blood or fluid
Pathogenesis off External Ear Otorrhea
*usually patients are very religious in cleaning their ear which is wrong! normally the ear canal cleans itself as its skin desquamates and move laterally, mm everyday,, so if ear is clean the migration is impeded, and pushed inside, so the canal is then filled with cerumen, etc.. so cotton bud tip must not be inserted all the way inside as the ear canal is only an inch long. it is the most common predisposing factor leading to trauma and irritation
Canal Skin Irritation or Trauma Bacterial Infection and Inflammation
(canal becomes very narrow since it is swollen)
Diffuse - transudate
Circumsribed -pus
(localized only in outer portion of canal involving the hair follicles)
III.
EXTERNAL EAR DISORDER
Parts 1. o o 2. o
Auricle (pinna) shape defined by the elastic cartilaginous plate no actual subcutaneous tissue in this region
External Auditory Canal (external acoustic meatus, ear canal) lateral two-third consists of fibrocartilaginous framework that is angled downward and forward relative to the bony medial third o bony portion (medial 3rd of the ear canal) is formed by the tympanic part of the temporal bone o bony ear canal grows less than the cartilaginous ear canal o bony ear and cartilaginous ear equal length by 5-6 years o ear canal in adults: 2.5 cm long medial boundary of the external ear is the tympanic membrane Anatomical Relations o Anterior Temporomandibular joint o Anteriorly and Inferiorly Parotid Gland o Posterior Mastoid o Superiorly Temporalis muscle and Squamous part of the temporal bone Function: Acoustic antenna which transmit sound waves to the sensitive middle ear structures in a discriminating way Amplification of sound does not involve an increase in the amplitude of sound waves but is based on resonance (vibration) [naaalala nio pa ba sabi sa Physics? Sound is made by the vibration of molecules sa object.] Innervations o Sensory 1. Great Auricular Nerve (from the cervical plexus) 2. Auriculotemporal Nerve (from the third division of the trigeminal) o potions of the concha and ear canal are supplied by the auricular branch of the vagus nerve
Complications: perichondritis ( if it spreads to the auricular cartilage)
A. Diffuse Otitis Externa Also known as swimmers ear
(after swimming, water gets into the ear, so the skin gets very soft and subtle , so as you clean it with cotton buds the skin is macerated or peels off, and is pushed inside the canal, exposing the deeper layers to contamination of the normal flora )
Signs and Symptoms o Pain (present with an acute infection) and Tenderness - touch, chewing *swallowing is not affected, it is only with the act of opening when pain is felt this is because
the outer portion of the canal skin is behind the TMJ so as one opens the mouth the condyle moves also allowing the cartilaginous portion to move.
o Scanty discharge
Otorrhea 2 of 14
Etiologic Organism o Pseudomonas o Proteus o Staphylococcus o Streptococcus o Gram negative Treatment
(usually there is multiple organism causing swimmers ear)
(never let the patient clean his ears as it only aggravates the problem) o Gentle cleaning (first and most important step which involves removing the debris and drying the ear canal)
Fig.2 Appearance of a swollen ear canal, very narrow lumen due to the edema and swelling of the skin, with dry secretion and scanty discharge
o Ear wick + Topical Antibiotic Drops (antibiotic
must not reach the deeper portion, so an ear wick is inserted an elongated gauze which also helps to open the ear canal, and it is place for 48 hours and ear drops is placed )
o Analgesics/Antipyretics
(given until infection subsides) o Oral Antibiotics (is not usually given, only given if inflammation has reached the soft tissue inside the ear, or when enlarge lymphnodes are already palpated)
Ear wick
*remember approach is not always the same so you have to do otoscopy and the rest of physical exams and history Pathogenesis: An inflammatory condition of the external auditory canal involving the canal skin (eczema. Dermatitis due to a mechanical injury, toxicity or allergy) gives rise to an acute bacterial infection of the skin with a mixed flora that includes gram-negative organisms (P. aeruginosa, P. mirabilis) and anaerobes. A warm , moist climate promotes the development of a diffuse otitis externa Itching- main initial symptoms Diagnosis: Otoscopy: appears dry, cracked and scaly Bacteriologic exam: necessary only in cases with persistent or recurrent infection or if the diagnosis is uncertain Complications: perichondritis, cellulites or abscess formation Necrotizing otitis media in predisposed patient Steroid- and antibiotic-containing ear drops should be used for no more than two weeks due to the risk of sensitization, antibiotic resistance, and the development of a fungal infection. These are contraindicated in patients with a fungal infection of the ear canal, antibiotic hypersentivity, or a
B. Furuculosis
*Infection of the pilosebaceous glands, appear as small abscess, skin easily ruptures so discharge comes out
Also known as Circumscribed Otitis Externa Signs and Symptoms
* symptoms basically the same with diffuse otitis externa, but the ear canal are not really occluded, just the outer portion
o Oral Antibiotics
(only if infection results to cellulites around the ear)
o o
Pain and Tenderness -touch, chewing (can cause mild hearing
loss and rarely leads to otorrhea)
Purulent discharge -if ruptured Etiologic Organism: Staphylococcus aureus ( as it is
very common in superficial skin infection)
Treatment o Gentle cleaning o Incision and drainage
(for abscess that have clearly become demarcated)
o Analgesics/Antipyretics
Otorrhea 3 of 14
A circumscribed lesion caused by an acute bacterial infection of the cartilaginous portion of the ear canal Pathogenesis: local mechanical trauma and contamination of the ear canal (e.g. from an ear plug, dusty environment, bath water, or attempted self-cleaning of the ear) lead to obstruction of the hair follicles or glandular ducts, followed by a staphylococcal infection of the pilosebaceous units. Diagnosis: Inspection and palpation: tragal tenderness accompanied by a circumscribed, very painful swelling in the cartilaginous portion of the ear canal Otoscopy: pronounced swelling of the ear canal with debris in the residual lumen. Frequently the tympanic membrane cannot be seen, but it is normal Simple hearing test: The ear canal may be swollen shut, causing some degree of conductive hearing loss Bacteriologic examination: the purulent center of the lesion (pus pocket) can be opened with small, blunt hook to obtain a smear Complications: perichondritis ( if it spreads to the auricular cartilage) Necrotizing otitis externa in predisposed patients as a result of superinfection with Pseudomonas
C.
Herpes Zoster Oticus
*not a common condition but is very disturbing for the patient
vesiculo-pustular lesions with swelling and erythema of the skin which is very painful (the vesicles initially contains
clear fluid but yellowish and bloody as it ruptures due to the bacteria it contains, painful since the facial nerve that supplies the ear canal and pinna has sensory innervations in the ear])
o Surgery ( reserved for those who already have degeneration of facial nerve)
external ear canal is narrowed due to swelling there may be ipsilateral facial paralysis due to involvement of Geniculate Ganglion of CN VII
(infection is not the problem as it resolves after two weeks but it is the resulting facial paralysis) Treatment Analgesic Wound Care Antibiotic Antiviral HERPES ZOSTER OTICUS Also known as Ramsay Hurt Syndrome Pathogenesis: caused by reactivation of the dormant varicella-zoster virus (VZV) in ganglion cells. Involves CN VII and/or VIII (and occasionally IX and X) Symptoms: px initially experience ear pain or burning on one side in the absnce of physical findings Vesicles erupt a few days after symptom onset Followed by hearing loss, vestibular complaints such as vertigo and disequilibrium and often by facial nerve palsy Diagnosis: diagnosiss can be made clinically Inspection: vesicles along the meatus and concha and occasionally and pinna. Accompanying lymphadenitis of the high cervical lymph nodes Signs and symptoms Confirmation by the direct electron microscopic detection of VZV in vesicular aspirate or by ATleast a four-fold titer increase on serologic testing. Differential Diagnosis: Bullous otitis externa Otitis media, mastoiditis, labyrynthitis, cholesteatoma, aand tumors of the ear and lateral skull base other causes of 7th and 8th CN lesion Complications: secondary bacterial infection (usually with staphylococci and pseudomonas species Zoster meningoenehalitis which results from the intracranial spread of the VZV Post-zoster neuralgia late complication, esp. in older patient
o
o
D. Other External Ear Disorders 1.Otomycosis
Chief complaint of the patient: ITCHINESS (The problem is not pain but itchiness accounting for secondary infection due to the manipulation inside the ear) *Refers to patient that have fungal infection of the ear. Most cases with otitis externa have fungal infection, either before or after the episode of acute infection.
Otorrhea 4 of 14
Fig. Whitish debri ear canal + debri.
Fig. With hyphae in the
Otomycosis Pathogenesis: cerumen often harbors saprophytic fungi that have no specific pathologic significance. A warm, most climate is conducive to f ungal infections, which are most common during summer months. Symptoms: manifested by severe itching and a feeking of fullness in the affected ear Diagnosis: Otoscopy- white, yellow or black membrane lining the swollen erythematous skin of the ear canal Bony portion affected most exclusively Mycelia identified in direct samples Microbiologic exam- to determine the causative agent Course: runs refractory course and has a tendency to recur Complications: perforation and subsequent otitis media Treatment: clean and dry the ear canal Local antimycotics Salicylate-containing solution- in the uppermost epithelial layer, to enhance the antifungal action of specific medications Systemic antimycotic therapy is necessary only in immune-suppressed patients
2.
Chief Complaint: BLOCKED HEARING in the AFFECTED SIDE (cerumen is normal in the outer portion, the abnormality relies in the amount of cerumen produce, and as it is pushed inside the px complains of blocked hearing. )
Impacted Cerumen
Impacted Cerumen
Physiology: cerumen or earwax is producedby the cerumen and sebaceous glands in the skin of the ear canal. It forms a protective film in which fatty acids, lysozymes and the creation of an acid mileu effectively protect the skin of the ear canal. Self- cleansing of the ear canal, with natural removal of accumulated cerumen, is normally accomplished by epithelial migration from the tympanic membrane toward the external meatus. Pathophysiology: Cerumen impaction may result from a disturbance of the normal self-cleansing mechanism or or from excessive cerumen secretion. The cerumen plug consists mainly of secretions from the cerumen glands mixed with sebum, exfoliative debris, and contaminants. Imprudent cleaning of the ear canal can interfere with the self-cleansing mechanism and displace the cerumen toward the tympanic membrane. Obstruction of the ear canal by cerumen may be caused by the impaction or swelling of a cerumen plug. This occurs after contact with water. With ageing, drying of the meatal skin and changes in the secretions can lead to the formation of a hard cerumen that tends to be retained in the ear, especially with a narrow canal. Symptoms: pressure sensation in the ear with concomitant hearing loss. Some may also complain of vertigo or tinnitus Diagnosis: Otoscopy- obstruction of ear canal by a yellowish-brown to black material, variable consistency Particular attention is given to tympanic membrane perforations and previous temporal bone fractures or otologic surgery. Differential diagnosis: choleastoma, tumor, foreign bodies and crusted blood Complications: Otitis externa Treatment: removal of cerumen and cerumen plugs using a hook or curette Aural irrigation
3.
Aural Polyp
4.
Psoriasis
*Mass is seen in the ear canal, can present with bleeding *biopsy must be done to determine if its benign or malignant
*Scaly, whitish discoloration
Otorrhea 5 of 14
IV.
MIDDLE EAR DISORDER
* bounded
laterally by the ear drum * important structure: Ossicular chain Eustachian tube * A very small confined chain that is important for hearing and balance
MIDDLE EAR Occupies a central position in the temporal bone consists of: 1. Tympanic cavity bounded laterally by the tympanic membrane a. Tympanic Cavity o allows for unrestricted mobility of the tympanic membrane b. Tympanic Membrane o Function gather sounds like the microphone provides sonic shielding of the round window membrane o consists of pars tensa and pars flaccid 2. System of temporal bone air cells o mucosa lined air cells of the temporal bone .3 Eustachian Tube o connects the tympanic cavity/middle ear with the nasopharynx o Equalize static air pressure air-filled cavity subdivided into: 1. Tympanic cavity 2. Mastoid air cells communicate with the nasopharynx via the Eustachian tube Function: 1. Impedance matching 2. equalize static pressure
A. OTITS MEDIA inflammation of the middle ear Classification based on Duration of Symptoms 1. Acute < 3 weeks 2. Subacute 3. Chronic > 3 months Abnormal Eustachian Tube: most important prognostic factor in pathogenesis
(It can be affected in all age groups especially in neonates up to elder, what happens in the Eustachian tube reflects what happens to the ear drum)
Eustachian Tube connects middle ear with nasopharynx ( in the nasopharynx, airway passes, adenoids is also located just beside the opening, in children it is usually enlarged until 2-3 yrs old.) lined by columnar ciliated secretory epithelium normally closed opens on contraction of Tensor Veli Palatini muscle which is attached to the palate *if one has congenital anomaly of the palate he usually have ventilation problem. Eustachian tube can also be affected by tumors, recurrent infection of sinuses Anatomical difference of the Eustachian Tube of Infants VS Adults *infants are really prone to development of Otitis media Infants Adults Shorter and horizontally Longer and angulated oriented (45) Prone to reflux from Drains better nasopharynx Poor function of Tensor Veli Palatini *Because of its anatomical location, reflux of milk intake in infants goes to the middle ear initiating the inflammatory process. Functions 1. Drains the middle ear secretion by mucociliary clearance of respiratory epithelium 2. Protects the middle ear from nasopharyngeal secretions and sound pressure opens only by contraction of TVP 3. Ventilates the middle ear for optimum hearing most important function, if pressure inside is not equal to the environment, there is an effect in the eardrum affecting the hearing. If pressure is too high= eardrum bulges
Otorrhea 6 of 14
i.
Eustachian Tube Dysfunction in Otitis Media 1. Obstruction The lateral third is bony the medial 2/3 is cartilaginous, so it is very soft so when it collapse it closes unabling it to functionas a drainage and for ventilation a. Functional collapse of tube inability to open as in cleft palate, cranio-facial deformity, Pierre-Robin, Downs, Crouzons b. Mechanical Intrinsic - inflammation (URTI), allergy ( infection and inflammation from the nose, nasopharynx and adenoids that obstructs the eustatian tube) Extrinsic - tumor, adenoid 2. Abnormal Patency patulous (always open) - loss of weight leads to reflux otitis media (reflux from secretion of the nasopharynx which is not sterile as the middle ear so bacteria can access the middle ear through it)
Patulous Eustachian Tube Etiopathogenesis: when there is weight loss, there is a diminished amount of fat and connective tissue surrounding the eutaschian tube leading to a permanently open connection may be established bet. the nasopharynx and tympanic membrane Symptoms: aural fullness, vague hearing problems without objective hearing loss, occasional roaring tinnitus. Diagnosis: Otoscopy Hearing tests Normal Endoscopic exam Treatment: treat the underlying cause
ii.
Pathogenesis of Otitis Media Factors 1. Infection (URTI) 2. Eustachian tube dysfunction 3. Immunologic status 4. Allergy 5. Environment 6. Social Factors
Especially true in infants and young children (esp. those in enrolled in daycare centers)
iii.
Sequences of Events in Otitis Media Upper Respiratory Tract Infection Mucosal Congestion Eustachian Tube Dysfunction Persistent Negative Middle Ear Pressure Otitis Media with Effusion Eustachian Tube suddenly opens Nasopharynx secretions insuffiated Bacterial Otitis Media
*when there is negative pressure there is effusion due to transudation of fluid from the blood vessel, capillaries and mucosa to the middle ear space causing clear whitish secretion. * persistent negative pressure caused the eardrum to retracts causing atelectasis of the eardrum, so in some cases the Eustachian tube suddenly opens,allowing the secretions from nasopharynx which contains bacteria to go in the middle ear causing bacterial otitis media- thick yellowish secretion with intact eardrum
Otorrhea 7 of 14
iv.
Diagnosis of Otitis Media 1. Clinical History (concise) 2. PE Findings (otoscopic findings) 3. Pneumatic otoscopy (otoscope+bulb) 4. Audiometry and Tympanometry Types of Otitis Media 1. Suppurative a. Aerotitis - Barotrauma Barotrauma - when pressure difference outside and inside the middle ear is more than 90 mmHg - differences in atmospheric pressure when you ride an airplane. During Ascent during ascent there is passive opening of Eustachian tube atmospheric pressure is less than middle ear pressure Eustachian tube opens up easily to equalize pressure
v.
(When the plane takes off there is passive opening of the Eustachian tube since the pressure withing the atmospheric pressure is lower and the pressure within the ear is higher, so air moves from the middle ear and goes out the eustachian tube, so no problem as it can easily open up)
During Descent during descent, there is no passive opening of the Eustachian tube atmospheric pressure is greater than the middle ear pressure eardrum retracts
Eustachian tube closes and TVP needs to open
(but during landing there is problem with the opening of the Eustachian tube, since the atmospheric pressure is higher than the middle ear and it impinges with the openingof the Eustachian tube so that it closes. So Longer problem in hearing during landing. And kids cry during the flight because of the pain due to change in pressure. ) BAROTRAUMA A rapid change in air pressure can have acute traumatic effects on the tympanic membrane and middle ear due to a negative pressurein the tympanic cavity. The Teed scale classifies barotraumas into five grades of severity based on otoscopic findings: I- erythema of the pars flaccid II- erythema of the entire tympanic membrane III- Hematoma of the tympanic membrane IV- Hematotympanum V- Rupture of the tympanic membrane Etiopathogenesis: barotraumas is caused mainly by compression events associated with airplane landings or diving. When the ambient pressure rises and there is inadequate pressure equalization through the Eustachian tube, a negative pressure will develop in the tympanic cavity relative to the environment. This can lead to swelling and bleeding of the middle ear mucosa.the tympanic membrane is retracted inward, and the round window bulges into the middle ear. This can result in a perforation of the tympanic membrane or round window membrane Symptoms: initial symptom is severe ear pain Conductive hearing loss (unnoticed due to pain) Vertigo and nystagmus (in some cases) Diagnosis: History Otoscopy: reveals tympanic membrane changes, a middle ear effusion, or a rupture of the tympanic membrane, depending on the grade of injury Complications: during diving- cold water can enter the middle ear, causing caloric irritation of the vestibular organ with associated vertigo, loss of orientation and possible vomiting. Bacterial infection Permanent cochleovestibular dysfunction Treatment: Paracentesis to relieve the negative pressure
b. Serous Otitis Media or Otitis Media with Effusion Acute or Chronic Closed ET results in fluid transudation from blood vessel Causes: allergy, sinusitis, enlarged adenoid, rhinitis ,nasopharyngeal tumor Chief complaint: HEARING LOSS Work-up needed: check the nose, sinuses, and nasopharynx Treatment: Antihistamines - Decongestants
Antibiotics Mucolytics Allergy Management Eustachian tube inflation Myringotomy with ventilation tube Adenoidectomy
Otorrhea 8 of 14
Otitis Media with Effusion Refers t o an inflammation effusion behind an intact tympanic membtrane that is not associated with acute otologic symptoms or systemic signs. Classification: Acute- last up to 3 weeks Subacute up to 3 months Chronic more than 3 mos. Epidemiology: common in pre-school-age chil;dren Symptoms: In children- Hearing loss , Speech and language delay and perceptual impairment (may occur in bilateral cases) In adult- clogged or pressure sensation, pain (rarely present, popping or sloshing sound, hearing loss and pressure sensation (very troublesome unlike in children) Complications: acute otitis media, labyrinthitis Treatment: Acute:- improve nasal breathing and euustachian tube function with: Short-term use of decongestant nose drops Moisturizing and hygienic measures Topical steroids Inflation of a balloon with nose Valsava maneuver Chronic: paracentesis
>CHRONIC OME: Chronic Otitis Media with Effusion mucoid to purulent effusion in middle ear intact, thickened, opaque eardrum 2. Non-suppurative a. Acute Suppurative Stages 1. Hyperemia onset of disease ear fullness, earache, fever Physical Examination: congestion and retraction of eardrum Treatment a. Bed Rest b. Analgesics c. Decongestant 2. Exudation fluid under pressure in the middle ear more severe ear pain, fullness and fever Physical Examination: red, thickened bulging ear drum Treatment a. Antibiotics b. Decongestant c. Analgesics d. Myringotomy 3. Suppuration ear drum ruptures profuse otorrhea maybe blood-tinged relief of pain and fever hearing loss worsens Treatment a. Clean ear canal of discharge b. Systemic antibiotics c. Ear drop if discharge lessens disease process may stop at this stage
4. Coalescence and Surgical Mastoiditis breakdown of mastoid air cells with pus accumulation post aural pain and mastoid tenderness, fever sagging bony canal wall Treatment a. Antibiotics b. Mastoidectomy 5. Stages of Complications pathways for spread a. Bone erosion b. Thrombophlebitis c. Preformed opening d. Surgical opening e. Hematogenous
6. Stage of Resolution may occur at any stage
Otorrhea 9 of 14
b. Acute Necrotizing in acutely ill young children, low resistance Etiology: Hemolytic Streptococcus Profuse, foul otorrhea Large eardrum perforation with necrotic middle ear Treatment a. IV Antibiotics b. Mastoidectomy
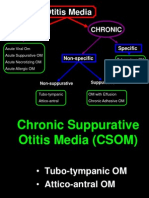
c. Chronic Suppurative o chronic inflammation of middle ear and mastoid non-intact ear drum discharge present Treatment a. Aural cleaning b. Treat predisposing factor (allergy, infection) c. Topical antibiotics d. Surgery Safe Central perforation Mucoid-purulent, non-foul, profuse otorrhea Mucosa, edematous, with small granulation Conductive hearing loss X-ray; no cholesteatoma Treatment: medical + surgery to preserve hearing Dangerous Marginal, attic, total Purulent, foul, scanty otorrhea Large polyp and granulation Mixed hearing loss X-ray; with cholesteatoma Treatment: surgery for complications
Chronic SuppurativeOtitis Media Chronic tympanic membrane perforation- does not healspontaneously after a few weeks Classification: a. Dry- without active inflammatory signs such as pain, discharghe, and swelling of the mucosa b. Wet or draining form- presence of discharge Etiopathogenesis: a. Chronic inflammation secondary to E.T. dysfunction b. Genetic and constitutional factors that affect the healing capacity and resistance of the mucosa c. Special anatomic characteristics of the middle ear spaces such as pneumatization and relative sizes d. Nature, pathogenecity, virulence and resistance of the infecting organisms Symptoms: presents with chronic otorrhea- mucopurulent discharge Pain only felt on recurrence Chronic drainage- odorless, stringy mucus Diagnosis: History Otoscopy- in dry ear, central perforation in the tympanic membrane that does not involve the fibrocartilaginous ring Wet ear, with secretions, inflamed and swollen Valsava maneuver Complications: mastoiditis or abscess formation (rare and atypical) Conductive hearing loss with cochlear hearing loss Treatment: cleaning and drying Ear drops containing ototoxic substance aminoglycoside antibiotics tympanoplasty
d. Tuberculous vi. Microbiology in Otitis Media 1. Acute Otitis Media and Otitis Media with Effusion a. S. pneumoniae (AOM: 35%) b. H. influenza (AOM: 23%) Microbiological Findings in Middle Ear Aspirates from c. Moraxella catarrhalis 38 infants and children (51 ears) with Chronic d. Others Suppurative Otitis Media 2. Chronic Suppurative Otitis Media a. P. aeruginosa b. S. aureus c. Anaerobes d. Others: E.coli, H. influenza, Proteus, Strep growth in Cultures Non-bacterial organism (virus, chlamydia) Anaerobic organism Immune response to pollens, antigen Prior antibiotic treatment Effect of host enzymes vs bacteria (lysozymes, immunoglobulins) Management 3. No o o o o o
Species Pseudomonas aeruginosa S. aureus (7-lactamase inhibitor) Diphtheroids S. epidermidis Streptococcus, alpha S. pneumonia E. coli C. albicans H. influenza, non typable C. parapulosis Enterococcus species Pseudomonas maltophilia Proteus mirabilis S. pyogenes No. of Isolates 34 10 10 6 4 3 2 2 2 2 2 2 2 1
vii.
Otorrhea 10 of 14
viii.
Antimicrobial Agents for Therapy of Acute Otitis Media (United States, 1994) Approved Amoxicillin Amoxicillin-clavulanate Cefaclor Cefixime Cefuroxime axetil Cefprozil Cefpodoxime Loracarbef Trimethoprim/sulfamethoxa zole Erythromycin/sulfisoxazole Under Investigation Ceftibuten Ceftriaxone Clarithromycin Azithromycin
ix.
Acute Otitis Media Treatment:
chemoprophylaxis with antimicrobials amoxicillin 25 mg/kg HS cotrimoxazole 75 mg/kg HS myringotomy with tube insertion adenoidectomy pneumococcal vaccines
Otorrhea 11 of 14
Acute Otitis Media Epidemiology: common disease in infants and small children but can occur in any age Pathogenesis: generally caused by infections that ascends to the middle ear through the E.T. Etiologic Organisms: S. pneumonia, H. influenza, catarrhalis Factors that increase risk: craniofacial anomalies Previous episode of acute otitis media Presence of chronic serous otitis media Parental smoking Leaving infants at day-care center Factor that reduces risk: breastfeeding Symptoms: often preceeded by a viral infection of the upper respiratory tract Severe earache- initial symptom Fever within the 1st 24 hrs. Irritability Vomiting Diarrhea Aural discharge manifesting tympanic membrane perforation Diagnosis: P.E. mastoid shows no swellingbut may be tender Otoscopy opaque thickened, erythematous and sometimes bulging tympanic membrane Immobile tympanic membrane by pneumatic otoscopy Features of conductive hearing loss Bacteriologic examination (done only in px with sponatneoius perforation or paracentesis Paracentesis for bacteriologic exam (in immunocompromised px, treatment failures and complications) Differential Diagnosis:otitis externa, chronic otitis media Course: spontaneous perforation of the tympanic membrane may occur. After the acute phase of the inflammation has subsided, a residual inflammatory effusion will persist in the tympanic cavity for several weeks with associated conductive hearing loss. Complications: acute mastoiditis Treatment: non-steroidal anti-inflammatory analgesics (acetaminophen) for pain relief Decongestant nose drops Irrigation Antibiotic therapy as a rule it is started right away though improvement may occur in 1-2 days w/o antibiotic.
x.
Recurrent Otitis Media chemoprophylaxis with antimicrobials amoxicillin 25 mg/kg HS cotrimoxazole 75 mg/kg HS myringotomy with tube insertion adenoidectomy pneumococcal vaccines
Recurrent Otitis Media Occurrence of 5 or more acute middle ear inflammations in 1 year, or 3 inflammmations in 6 mos. The middle ear heals between episodes, no effusion in the tympanic membrane Epidemiology: disease of infants and small children Etiopathogenesis: same as acute otitis media Symptoms, diagnosis and course: same as acute otitis media Allergy should be excluded if the hx is suspicios for an allergic rxn Treatment: adenoidectomy can decrease the bacterial burden in the nasopharynx and improve Eustachian tuibe fxn.
xi. Cholesteatoma
accumulation of squamous epithelial debris enlarges like a tumor destroys bone by pressure necrosis and enzymatic action Types Choleastatoma a. Congenital 2 characteristics: a. Keratinizing squamous is found in bony spaces at an abnormal location b. Acquired due to epithelium COM b. Bone is destroyed through an inflammatory osteoclastic process retraction pocket
Types: a. Congenital or true very rare and usually found behind an intact tympanic membrane. Can occur anywhere in the temporal bone b. Acquired arises in connection with inflammations and ventilations problems of the middle ear Two forms: primary (pars flaccid choleastatoma) and secondary ( pars tensa cholesteatoma) Epidemiology: occurs in any age grp., rare in small children Pathogenesis: primary cause of acwuired is impairment of middle ear ventilation SymptomsL acwuired c. usually present as chronic otitis media a. Dry, uninfected cholesteatoma does not cause otalgia or otorrhea. Manifested clinically as functional deficits. Aural pressure- common initial symptomsignifying impaired middle ear ventilation Facial nerve palsy and vestibular dysfxn (rotary vertigo and disequilibrium) b. Infected with discharge- present as chronic otitis media with otorrhea. Generally fetid With hearing loss Pain with acute exacerbation Facial nerve palsy or vestibular dysfxn Abscess formation Meningitis diagnostic work-up: Otoscopy- white epithelial debris in a retraction pocket in the attic or in postsuperior quadrant of the tympanic membrane. Occasional bone erosion in the post superior canal wall. In dry cholesteatoma, brownish-blackcrust in the sup. Canal wall Otorrhea Screening for complications: Hearing test, indicates conductive hearing loss 12 of 14 Facial nerve function test Fistula sign Imaging studies: CT scan Treatment: Surgery necessary due to the bone destruction caused by cholesteatoma. a. Main goal: eradicate the destructive inflammatory process in the mastoid and
V.
COMPLICATIONS OF OTITIS MEDIA A. Extracranial 1. Facial Nerve Paralysis peripheral type affects upper and lower half of face 2. Mastoiditis Subperiosteal Abscess Types a. Post-auricular (most common) b. Pre-auricular c. Bezolds (tip of mastoid to neck) d. Parapharyngeal e. Intracanal
MASTOIDITIS Inflammation of the aircells of the mastoid process. Present when the inflammatory process is focused on the mucous membranes and bony structures of the mastoid Etiopathogenesis: usually originates from an infection of the middle ear. Most frequent complication of otitis media. Can also be cause by an inflammatory destructive process (Wegener diseasea0 Important pathogenetic factors: a. degree of mastoid pneumatization b. virulence of the infecting organism c. host immune status d. treatment for optitis media Symptoms: fever, local pain Diagnosis: classical triada. Prominent auricle with retroauricular swelling b. Tenderness over the mastoid c. Otorrhea Otoscopy- reveals the feat. Of acute or subacute otitis media w/ or w/o tympanic membrane perforations. Erythematous or swollen post. Wall of external auditory canal CT scan- best diagnosis, demonstrates clouding of mastoid air cells and middle ear spaces and erosion of the mastoid bone Elevation of inflammatory parameters (WBC, CRP, ESR Treatment: mastoidectomy Paracentesis and placement of myuringotomy tube for middle ear decompression Antibiotics
3. Labyrinthitis direct extension of infection or by bone erosion to inner ear Types Vertigo Hearing Loss
Otorrhea 13 of 14
Circumscr ibed Serous Suppurati ve
Mild Moderate to Severe Severe
Conductiv e Mixed Sensorineu ral
4. Petrositis infected air cells at Petrous apex of temporal bone Gradenigos Syndrome - discharging ear - retro-orbital pain (CN VI) - diplopia (CN VI palsy) B. Intracranial 1. Extradural Abscess pus between bone and dura severe otalgia and headache Subdural Abscess pus between dura and brain fever, headache, seizures, hemiplegia, coma 2. Lateral Sinus Thrombophlebitis extension of infection to lateral sinus venous drainage from brain picket fence fever, chills, headache and severe otalgia Treatment a. Mastoidectomy with ligation of internal jugular vein b. IV antibiotics 3. Meningitis most common stiff neck, fever, headache and vomiting, seizures, (+) Kernigs and Brudzinski signs lumbar puncture (+) Treatment a. High dose of antibiotics b. Mastoidectomy after adequate medical treatment
Meningitis Etiology: result from a clinically overt otitis media, esp. with cholesteatoma. Can also arise from an occult process involving the lateral skull base Can result from the spread of amiddle ear infection through performed channels (blood vessels, diploic veins) through the labyrinth, through bone gaps caused by laterobasal fractures, or by contiguous spread from infected osteitis or cholesteatoma. Symptoms: severe headache, fever, clouding of consciousness and nuchal stiffness Diagnosis: CT scan of the temporal bone with contrast agent administration and lumbar puncture Treatment: antibiotics, corticosteroids Surgery diagnostic to establish cause of infection and therapeutic to eradicate the infectiopus focus and eliminate its route of spread. Course: otogenic meningitis can lead to inner ear disorder or even bilateral blindness
4. Brain Abscess associated with meningitis, petrositis lateral sinus thrombosis Cerebellar - aphasia, seizures, visual defects Temporal - ataxia, tremors, hypotonia, dysdiadokinesia signs of increased intracranial pressure
Stages of Brain Abscess a. Stage of encephalitis + signs of meningitis b. Stage of encapsulation (symptom free) c. Stage of expanding brain abscess (classic signs of increased intracranial pressure) d. Stage of rupture (leads to death) 5. Otitic Hydrocephalus due to decreased absorption of CSF at arachnoid villi signs of increased intracranial pressure - papilledema, headache, otitis media - sterile CSF CT Scan: to rule out brain abscess Treatment - generally self limited - directed at otitis media and increased intracranial pressure ---END---
Otorrhea 14 of 14
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Diagnosis of Ear PainDocument8 pagesDiagnosis of Ear PainJoyce TeoPas encore d'évaluation
- Middle Ear Nerve Damage After Thyroid SurgeryDocument32 pagesMiddle Ear Nerve Damage After Thyroid Surgerykishorechandra75% (4)
- Chronic Suppurative Otitis MediaDocument11 pagesChronic Suppurative Otitis MediaaditiarrtuguPas encore d'évaluation
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghPas encore d'évaluation
- Ear Disorders ExplainedDocument8 pagesEar Disorders ExplainedVinz Khyl G. CastillonPas encore d'évaluation
- Endoscopic Atlas of Pediatric EntDocument72 pagesEndoscopic Atlas of Pediatric EntAyman Yakout100% (1)
- Otitis Media: Prepared By: - Priyanka ThapaDocument38 pagesOtitis Media: Prepared By: - Priyanka ThapaKalo kajiPas encore d'évaluation
- Fellowships in OtolaryngologyDocument17 pagesFellowships in OtolaryngologyasiyazaidiaPas encore d'évaluation
- Chronic Otitis Media GuideDocument50 pagesChronic Otitis Media GuideKhalid MahidaPas encore d'évaluation
- AtelektasisDocument15 pagesAtelektasisMuhammad Ade RahmanPas encore d'évaluation
- Cholesteatoma Report06Document3 pagesCholesteatoma Report06KatherineCentenoIlaganRNPas encore d'évaluation
- Colour Atlas of The Anatomy and Pathology of The EpitympanumDocument110 pagesColour Atlas of The Anatomy and Pathology of The Epitympanumapi-26081450Pas encore d'évaluation
- Cholesteatoma of The Ear CanalDocument9 pagesCholesteatoma of The Ear CanalWanda DamayantiPas encore d'évaluation
- Comparison of Graft Uptake and Post Operative Hearing Between Cartilage Rim Augmented Fascia and Temporalis Fascia TympanoplastyDocument7 pagesComparison of Graft Uptake and Post Operative Hearing Between Cartilage Rim Augmented Fascia and Temporalis Fascia TympanoplastyInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Csom Atticoantral (Modified)Document24 pagesCsom Atticoantral (Modified)Muhammad MunawarPas encore d'évaluation
- Easy Peasy EardrumsDocument52 pagesEasy Peasy EardrumsUCD GEMPas encore d'évaluation
- Toacs Fcps Ii: by Maj Atif Najam Mbbs FcpsDocument400 pagesToacs Fcps Ii: by Maj Atif Najam Mbbs FcpsFurqan MirzaPas encore d'évaluation
- Kode ICD 10 THTDocument10 pagesKode ICD 10 THTAnung Setiawan0% (1)
- 20.short Notes and Short Cases in ENT PDFDocument116 pages20.short Notes and Short Cases in ENT PDFpakistan100% (1)
- Dekker Surgical Atlas of Pediatric OtolaryngologyDocument865 pagesDekker Surgical Atlas of Pediatric OtolaryngologyDaniel Rajkumar100% (2)
- Mastoidectomy: Surgical Techniques: Key PointsDocument14 pagesMastoidectomy: Surgical Techniques: Key PointsMichel Dayanna Serrano TasconPas encore d'évaluation
- Earnose 1 10091Document4 pagesEarnose 1 10091Annisa KartikasariPas encore d'évaluation
- Ent-Pearls and Personal NotesDocument161 pagesEnt-Pearls and Personal Notesapi-296021545100% (2)
- My Lecture NEMEC Temporal Bone CourseDocument37 pagesMy Lecture NEMEC Temporal Bone CourseAileen Delos Santos-GarciaPas encore d'évaluation
- Review and Read ENT MCQDocument13 pagesReview and Read ENT MCQanas_marzouk100% (1)
- Csom - Squamosal Type AnilaDocument80 pagesCsom - Squamosal Type AnilaThimmaiah SrirangapuraPas encore d'évaluation
- Acute Tonsillitis: Causes, Symptoms and TreatmentDocument19 pagesAcute Tonsillitis: Causes, Symptoms and TreatmentainaPas encore d'évaluation
- CholesteatomaDocument2 pagesCholesteatomaOvamelia JulioPas encore d'évaluation
- Ent MCQ 1Document17 pagesEnt MCQ 1sushil466Pas encore d'évaluation
- Omsk KomplikasiDocument10 pagesOmsk KomplikasiYudwari Adhicha Nuredis HarahapPas encore d'évaluation