Académique Documents
Professionnel Documents
Culture Documents
Salem Hospital Plan of Correction 7-28-11
Transféré par
Statesman JournalTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Salem Hospital Plan of Correction 7-28-11
Transféré par
Statesman JournalDroits d'auteur :
Formats disponibles
Corrective Action Plan Provider Number 38-0051
Oregon Department of Human Resources Complaint Numbers OR6875 and OR6831
RESPONSE TO PREFIX TAG A 395
CFR 482.23(8)(3) RN SUPERVISION OF CARE
A registered nurse must supervise and evaluate the nursing care for each patient.
This STANDARD is not met as the hospital failed to ensure that the registered nurse evaluated all of the patient's nursing care needs on admission and throughout the hospitalization. There was a lack of initial and on-going assessment related to 6 of 6 alterations of the patient's skin conditions. The Hospital implemented a new electronic clinical documentation system for nursing assessment on admission, reassessment by as defined by hospital policies, nursing care plans, and patient education in February, 2011. The Hospital's Skin Care Team, recognizing that documentation of skin and wound assessment and care planning were complicated and at times not completed because of the complexity of data entry and staff was not well educated on the electronic documentation tools related to wound assessment and care prior to the time of this investigation. The Team had already petitioned the Clinical Documentation Council to redesign the electronic tools to improve ease of use. The Plan of Correction was developed in collaboration with the Skin Care Team.
Plan of Correction:
Review current skin assessment and wound documentation in the electronic medical record (EMR) and design future state EMR documentation workflow. (Done 8/15/2011) 2. The Skin Integrity Record and the Wound Assessment Record which includes the photograph of the wound will remain in paper forms in the EMR; electronic communication "reminders" will be designed in the EMR to refer the nursing staff to review the forms, transcribe the initial wound assessment in the EMR, and update as necessary. 3. Per the CMS Present on Admission rule, physicians are required to stage pressure ulcers. If this form is not completed on admission when the physician is not present or during emergent or urgent situations when the form cannot be completed, a electronic note to the physician to review/complete the Wound Integrity Record will appear at the time the physician signs into the EMR. 4. A check box and "document wound assessment in Epic" (the EMR) will be placed on the Wound Integrity Record as a visual cue to nursing staff reminding them that the initial assessment needs to be in Epic. 5. Review/revise the Skin Care and Wound Care/Skin Integrity-Photo documentation/Evidence Collection policies to combine all skin and wound assessment and care into one single policy entitled Wound Care Protocol to provide consistency of information for staff. 6. Educate all clinical staff who assess and treat wounds on the new EMR documentation workflows and policy changes via didactic, and coaching, mentoring by Epic SuperUsers. 7. The Skin Care Team members will monitor compliance for all patients during Skin Care Rounds conducted in each patient care unit biweekly. Audits will continue in all units until 95% compliance is reached, and sustained for two months Data will be shared with unit staff and management team, and reported to the Staff Practice Council regularly. 8. Metrics are: a. #completed skin assessments completed per policy/#total patients reviewed b. #completed Wound Assessment Records completed/#total patients reviewed 1.
<
\
Corrective Action Plan Provider Number 38-0051
c. d.
Oregon Department of Human Resources Complaint Numbers OR6875 and OR6831
#completed Skin Integrity Records/ #total patients reviewed #completed wound documentations completed per identified wound/#total patients with wounds.
Responsible Person:
Kristin Haydon, BSN, RN, BC Director Clinical Excellence and Medical Unit, and Nursing Director Liaison to the Skin Care Team October 18, 2011
Completion Date:
RESPONSE TO PREFIX TAG A 396
CFR 482.23(b)(4) NURSING CARE PLAN The hospital must ensure that the nursing staff develops, and keeps current, a nursing care plan for each patient. This STANDARD is not met as evidenced by that an individualized care plan for alterations in the patient's skin condition was developed and kept current by the nursing staff, and based on the assessment of the patient and identified patient needs.
Plan of Correction:
1. Design, test, and implement Wound Care plan of care in the EMR.
2. 3. Include care plan in the education to be provided ( #6 of page 1 of this document). The Skin Care Team members will monitor compliance for all patients during Skin Care Rounds conducted in each patient care unit biweekly. Audits will continue in all units until 95% compliance is reached, and sustained for two months Data will be shared with unit staff and management team, and reported to the Staff Practice Council regularly. Metric: #wound care plans completed per policy/#total patients with wounds.
4.
Responsible Person:
Kristin Haydon, BSN, RN, BC Director, Clinical Excellence and Medical Unit, and Nursing Director Liaison to Skin Care Team October 18, 2011
Completion Date:
Vous aimerez peut-être aussi
- 28-Nursing Assessment For Admission ofDocument3 pages28-Nursing Assessment For Admission ofakositabon100% (1)
- Salem Hospital Plan of Correction 6-11-12Document4 pagesSalem Hospital Plan of Correction 6-11-12Statesman JournalPas encore d'évaluation
- Charge Nurse ResponsibilitiesDocument4 pagesCharge Nurse ResponsibilitiesdocpanchuPas encore d'évaluation
- Self Assessment ToolkitDocument19 pagesSelf Assessment ToolkitJasmeet KaurPas encore d'évaluation
- Don't Lose PatientsDocument9 pagesDon't Lose PatientsdrustagiPas encore d'évaluation
- Protocol: Submitted by Sonali Mishra Intern Department of Hospital AdministrationDocument8 pagesProtocol: Submitted by Sonali Mishra Intern Department of Hospital Administrationsonali mishraPas encore d'évaluation
- In Accordance With PRC Board of Nursing Memorandum No. 01 Series 2009Document3 pagesIn Accordance With PRC Board of Nursing Memorandum No. 01 Series 2009Stef ReyesPas encore d'évaluation
- MAJ OR PRS - Per CaseDocument4 pagesMAJ OR PRS - Per CaseAbbie Gail BorromeoPas encore d'évaluation
- Applying Technology Acceptance (TAM) Model To Determine The Acceptance of Nursing Information System (NIS) For Computer Generated Nursing Care Plan Among NursesDocument5 pagesApplying Technology Acceptance (TAM) Model To Determine The Acceptance of Nursing Information System (NIS) For Computer Generated Nursing Care Plan Among NursesseventhsensegroupPas encore d'évaluation
- Preparing A Duty Roster 2.0 PDFDocument6 pagesPreparing A Duty Roster 2.0 PDFAnirudh Gupta100% (1)
- Structure Standard Med-Surg Dept.Document22 pagesStructure Standard Med-Surg Dept.Jerry de la CruzPas encore d'évaluation
- TPH Quality PolicyDocument8 pagesTPH Quality PolicyAl Sah HimPas encore d'évaluation
- Guidebook For Hospitals - 4th EditionDocument239 pagesGuidebook For Hospitals - 4th EditionJobin JamesPas encore d'évaluation
- Salem Hospital Nurse Staffing PlanDocument3 pagesSalem Hospital Nurse Staffing PlanKathlyn Joy EclarinalPas encore d'évaluation
- OR EVAL SHEET ColoredDocument2 pagesOR EVAL SHEET ColoredKim XiaoPas encore d'évaluation
- JCI Handbook for SKMCH&RCDocument61 pagesJCI Handbook for SKMCH&RCWAQASPas encore d'évaluation
- NABH 3rd EditionDocument259 pagesNABH 3rd Edition19112281s3785Pas encore d'évaluation
- Draft Standards For MIS - 2nd EditionDocument35 pagesDraft Standards For MIS - 2nd Edition22g4colgPas encore d'évaluation
- CHC Staffing Plan Procedure ExampleDocument20 pagesCHC Staffing Plan Procedure ExampleAko C Kristal100% (1)
- Bernard Narrative Evaluation ReportDocument4 pagesBernard Narrative Evaluation ReportAldwin Compra QuiñoPas encore d'évaluation
- Policies and Procedures On Conducting Initial Assessment Inefficient and Systematic MannerDocument9 pagesPolicies and Procedures On Conducting Initial Assessment Inefficient and Systematic MannerKari Kris Buenaflor Isanan100% (1)
- Operating Room RenstahDocument2 pagesOperating Room RenstahRubi BorromeoPas encore d'évaluation
- NABH Guidelines PDFDocument71 pagesNABH Guidelines PDFAshish kumarPas encore d'évaluation
- Medical Records: Standard MOI.9Document5 pagesMedical Records: Standard MOI.9Azza FaroukPas encore d'évaluation
- 3364-110-07-06 Nursing ServiceDocument2 pages3364-110-07-06 Nursing ServiceMr. BamsPas encore d'évaluation
- Week 1011 Guidelines Protocols Tools in Documentation Related To Client CareDocument59 pagesWeek 1011 Guidelines Protocols Tools in Documentation Related To Client CareobnimagashelinaPas encore d'évaluation
- Nursing AuditDocument3 pagesNursing AuditJoe Shewale0% (1)
- Orientation Plan and Evaluation ToolDocument10 pagesOrientation Plan and Evaluation Toolapi-259047759100% (2)
- Laboratory Data in EHRs 2014Document20 pagesLaboratory Data in EHRs 2014sairi_nagarajuPas encore d'évaluation
- Self Assessment ToolkitDocument16 pagesSelf Assessment ToolkitsudheervermaPas encore d'évaluation
- QA Medical Record ReviewDocument4 pagesQA Medical Record ReviewJames JavierPas encore d'évaluation
- Applying Technology Acceptance (TAM) Model ToDocument5 pagesApplying Technology Acceptance (TAM) Model ToHaikal FaqihPas encore d'évaluation
- Surgical Self-Assessment ChecklistDocument8 pagesSurgical Self-Assessment ChecklistJyoti KumarPas encore d'évaluation
- (A) Policy Statement: Name of Policy: Policy Number: Department: Approving Officer: Responsible Agent: ScopeDocument2 pages(A) Policy Statement: Name of Policy: Policy Number: Department: Approving Officer: Responsible Agent: ScopeMr. BamsPas encore d'évaluation
- UntitledDocument4 pagesUntitledHeba Al-DeekPas encore d'évaluation
- CDD Gustavson 6 17Document15 pagesCDD Gustavson 6 17api-361857481Pas encore d'évaluation
- NABH Manual - Draft - Accreditation - Standards - For - Hospital - 4thedition PDFDocument102 pagesNABH Manual - Draft - Accreditation - Standards - For - Hospital - 4thedition PDFhannah86% (21)
- NABH Accreditation Standards For Ayurveda ClinicsDocument59 pagesNABH Accreditation Standards For Ayurveda Clinicsabhimanyu nehraPas encore d'évaluation
- RoilspaperDocument5 pagesRoilspaperapi-530717893Pas encore d'évaluation
- Setting Safe Staff Nursing Levels (5812984)Document39 pagesSetting Safe Staff Nursing Levels (5812984)Franz WagenerPas encore d'évaluation
- Hospital Registration Orientation 3 - EQRs With Operating ManualDocument33 pagesHospital Registration Orientation 3 - EQRs With Operating ManualElshaimaa AbdelfatahPas encore d'évaluation
- Contingency Plan For Hardware and or EHR Failure WhiteriverDocument6 pagesContingency Plan For Hardware and or EHR Failure Whiteriveriratxe_sartagudaPas encore d'évaluation
- OBM752 HM Unit-IV NotesDocument34 pagesOBM752 HM Unit-IV NotesRajanPas encore d'évaluation
- Paper Nursing 3 Nursing DocumentationDocument6 pagesPaper Nursing 3 Nursing DocumentationGoewoon EunsyukPas encore d'évaluation
- Roils ReportDocument5 pagesRoils Reportapi-632526087Pas encore d'évaluation
- Nursing DocumentationDocument17 pagesNursing Documentationprema100% (4)
- NYU HOSPITALS CENTER MEDICAL EQUIPMENT MANAGEMENTDocument32 pagesNYU HOSPITALS CENTER MEDICAL EQUIPMENT MANAGEMENTHind Chehabeddine100% (2)
- Quality Operating Process: Manual of Operations Care of PatientsDocument4 pagesQuality Operating Process: Manual of Operations Care of PatientsPrabhat KumarPas encore d'évaluation
- Documentation and Reporting in NursingDocument9 pagesDocumentation and Reporting in NursingMuruganPas encore d'évaluation
- Alcohol Treatment Facility Business Plan FY-02Document7 pagesAlcohol Treatment Facility Business Plan FY-02Keith BeckerPas encore d'évaluation
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankDocument13 pagesAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankAlexisLewisbjds100% (62)
- Online Clinic Management SystemDocument14 pagesOnline Clinic Management SystemCha LazaroPas encore d'évaluation
- dm2020 0426Document4 pagesdm2020 0426JeffreyReyesPas encore d'évaluation
- 3rd Edition NABH Guidebook 2012 New PDFDocument258 pages3rd Edition NABH Guidebook 2012 New PDFraamki_99Pas encore d'évaluation
- Rad Proc 10.12Document3 pagesRad Proc 10.12Mohamed Nawas AliPas encore d'évaluation
- Utilization ManagementDocument7 pagesUtilization ManagementCommunityBridgesPas encore d'évaluation
- Final Assignment of Big Data in Hospital Wendry Pasorong MHM Batch 3 UphDocument11 pagesFinal Assignment of Big Data in Hospital Wendry Pasorong MHM Batch 3 UphwendryPas encore d'évaluation
- Documentation & Reporting in Nursing - EFNDocument4 pagesDocumentation & Reporting in Nursing - EFNadellia onyPas encore d'évaluation
- SRS For CMS ENDocument4 pagesSRS For CMS ENMohammed AlshamiPas encore d'évaluation
- Newman's Certified Electronic Health Records Technician Study GuideD'EverandNewman's Certified Electronic Health Records Technician Study GuidePas encore d'évaluation
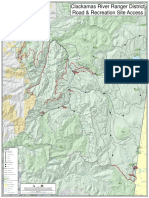
- Cedar Creek Vegitation Burn SeverityDocument1 pageCedar Creek Vegitation Burn SeverityStatesman JournalPas encore d'évaluation
- Roads and Trails of Cascade HeadDocument1 pageRoads and Trails of Cascade HeadStatesman JournalPas encore d'évaluation
- Letter To Judge Hernandez From Rural Oregon LawmakersDocument4 pagesLetter To Judge Hernandez From Rural Oregon LawmakersStatesman JournalPas encore d'évaluation
- Mount Hood National Forest Map of Closed and Open RoadsDocument1 pageMount Hood National Forest Map of Closed and Open RoadsStatesman JournalPas encore d'évaluation
- Complaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Document4 pagesComplaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Statesman JournalPas encore d'évaluation
- School Board Zones Map 2021Document1 pageSchool Board Zones Map 2021Statesman JournalPas encore d'évaluation
- Cedar Creek Fire Soil Burn SeverityDocument1 pageCedar Creek Fire Soil Burn SeverityStatesman JournalPas encore d'évaluation
- Cedar Creek Fire Sept. 3Document1 pageCedar Creek Fire Sept. 3Statesman JournalPas encore d'évaluation
- LGBTQ Proclaimation 2022Document1 pageLGBTQ Proclaimation 2022Statesman JournalPas encore d'évaluation
- Revised Closure of The Beachie/Lionshead FiresDocument4 pagesRevised Closure of The Beachie/Lionshead FiresStatesman JournalPas encore d'évaluation
- Cedar Creek Fire Aug. 16Document1 pageCedar Creek Fire Aug. 16Statesman JournalPas encore d'évaluation
- Social-Emotional & Behavioral Health Supports: Timeline Additional StaffDocument1 pageSocial-Emotional & Behavioral Health Supports: Timeline Additional StaffStatesman JournalPas encore d'évaluation
- Windigo Fire ClosureDocument1 pageWindigo Fire ClosureStatesman JournalPas encore d'évaluation
- Matthieu Lake Map and CampsitesDocument1 pageMatthieu Lake Map and CampsitesStatesman JournalPas encore d'évaluation
- Salem Police 15-Year Crime Trends 2007 - 2021Document10 pagesSalem Police 15-Year Crime Trends 2007 - 2021Statesman JournalPas encore d'évaluation
- Salem Police 15-Year Crime Trends 2007 - 2015Document10 pagesSalem Police 15-Year Crime Trends 2007 - 2015Statesman JournalPas encore d'évaluation
- All Neighborhoods 22X34Document1 pageAll Neighborhoods 22X34Statesman JournalPas encore d'évaluation
- Zone Alternates 2Document2 pagesZone Alternates 2Statesman JournalPas encore d'évaluation
- WSD Retention Campaign Resolution - 2022Document1 pageWSD Retention Campaign Resolution - 2022Statesman JournalPas encore d'évaluation
- Proclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedDocument1 pageProclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedStatesman JournalPas encore d'évaluation
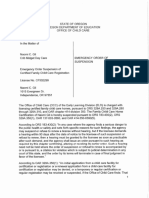
- Crib Midget Day Care Emergency Order of SuspensionDocument6 pagesCrib Midget Day Care Emergency Order of SuspensionStatesman JournalPas encore d'évaluation
- Salem Police Intelligence Support Unit 15-Year Crime TrendsDocument11 pagesSalem Police Intelligence Support Unit 15-Year Crime TrendsStatesman JournalPas encore d'évaluation
- Failed Tax Abatement ProposalDocument8 pagesFailed Tax Abatement ProposalStatesman JournalPas encore d'évaluation
- BG 7-Governing StyleDocument2 pagesBG 7-Governing StyleStatesman JournalPas encore d'évaluation
- Salem-Keizer Parent and Guardian Engagement in Education Month ProclamationDocument1 pageSalem-Keizer Parent and Guardian Engagement in Education Month ProclamationStatesman JournalPas encore d'évaluation
- All Neighborhoods 22X34Document1 pageAll Neighborhoods 22X34Statesman JournalPas encore d'évaluation
- SIA Report 2022 - 21Document10 pagesSIA Report 2022 - 21Statesman JournalPas encore d'évaluation
- SB Presentation SIA 2020-21 Annual Report 11-9-21Document11 pagesSB Presentation SIA 2020-21 Annual Report 11-9-21Statesman JournalPas encore d'évaluation
- Salem-Keizer Discipline Data Dec. 2021Document13 pagesSalem-Keizer Discipline Data Dec. 2021Statesman JournalPas encore d'évaluation
- Oregon Annual Report Card 2020-21Document71 pagesOregon Annual Report Card 2020-21Statesman JournalPas encore d'évaluation
- NVS List ResultDocument131 pagesNVS List ResultShubham Kumar TiwariPas encore d'évaluation
- Gla Life of Pi Unit Lesson PlanDocument4 pagesGla Life of Pi Unit Lesson Planapi-272664433Pas encore d'évaluation
- Una Vida Sin GloriaDocument64 pagesUna Vida Sin Gloriafelixpujols007Pas encore d'évaluation
- The Recursive Loop of Shame - An Alternate Gestalt TherapyDocument15 pagesThe Recursive Loop of Shame - An Alternate Gestalt TherapyblackstarfallPas encore d'évaluation
- Lawyer ProfileDocument3 pagesLawyer ProfilenitschemistryPas encore d'évaluation
- Guidelines For Pastoral Care in Catholic SchoolsDocument62 pagesGuidelines For Pastoral Care in Catholic SchoolsJoeN100% (1)
- A2-8 Review Life SkillsDocument2 pagesA2-8 Review Life SkillsnygaPas encore d'évaluation
- Food and Beverage Services NC II Scholars InsuredDocument3 pagesFood and Beverage Services NC II Scholars InsuredRendon AndrinoPas encore d'évaluation
- Presidents Day: Biography Close Read UnitDocument7 pagesPresidents Day: Biography Close Read Unitamelia ionescuPas encore d'évaluation
- Benefits of Learning LanguagesDocument13 pagesBenefits of Learning Languagesnefglobal91Pas encore d'évaluation
- Importance of Sports in EducationDocument2 pagesImportance of Sports in EducationAh TaiPas encore d'évaluation
- Austin E.F. Sheppe ResumeDocument2 pagesAustin E.F. Sheppe ResumeAustin SheppePas encore d'évaluation
- 4MPV KELAS 2016 - Copy 1Document35 pages4MPV KELAS 2016 - Copy 1Anonymous I1m68mssPas encore d'évaluation
- Online Examination System ProjectDocument31 pagesOnline Examination System ProjectMohammed Sajeer79% (14)
- PDS CS Form No 212 Revised2017Document2 pagesPDS CS Form No 212 Revised2017Mae Aila100% (1)
- Bilingual Education: Some Policy Issues: Pádraig Ó Riagáin and Georges LüdiDocument35 pagesBilingual Education: Some Policy Issues: Pádraig Ó Riagáin and Georges LüdiProfesoraELEPas encore d'évaluation
- RationaleDocument3 pagesRationaleapi-281029860Pas encore d'évaluation
- Task 4 (M5 LA2) Present A Coherent Discussion TextDocument2 pagesTask 4 (M5 LA2) Present A Coherent Discussion TextAmrullah 12Pas encore d'évaluation
- Modalidad de Exámenes - Semana 4 - Revisión Del Intento PDFDocument1 pageModalidad de Exámenes - Semana 4 - Revisión Del Intento PDFGriffo MinosPas encore d'évaluation
- Choice Board 3Document3 pagesChoice Board 3api-433840880Pas encore d'évaluation
- Impact of A Broken Family To School Aged ChildrenDocument10 pagesImpact of A Broken Family To School Aged ChildrenCourtney Dela Pena100% (2)
- Allain CST101 Spring 2023Document3 pagesAllain CST101 Spring 2023Cesar AllainPas encore d'évaluation
- Short VowelsDocument3 pagesShort Vowelsceeu_strongPas encore d'évaluation
- Ipgp 2017 - 2018Document3 pagesIpgp 2017 - 2018api-299571561Pas encore d'évaluation
- International Marketing T2 2021Document9 pagesInternational Marketing T2 2021NgơTiênSinhPas encore d'évaluation
- Ib Econ Ia Student RubricDocument2 pagesIb Econ Ia Student Rubricapi-19671923350% (2)
- The Determination of Psychiatric Illness SeverityDocument18 pagesThe Determination of Psychiatric Illness SeverityArct John Alfante ZamoraPas encore d'évaluation
- Medical Certificate SaherrDocument1 pageMedical Certificate SaherrPrajot SapatPas encore d'évaluation
- CB To Fill Up Items 1,2 & 4 and Col 3 of The Checklist NABCB AT To Fill The RestDocument75 pagesCB To Fill Up Items 1,2 & 4 and Col 3 of The Checklist NABCB AT To Fill The RestBS AnilKumarPas encore d'évaluation
- CH07 Measurement of Variables - Scaling, Reliability, ValidityDocument17 pagesCH07 Measurement of Variables - Scaling, Reliability, ValidityMaliha NazarPas encore d'évaluation