Académique Documents
Professionnel Documents
Culture Documents
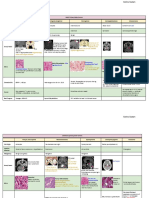
CNS Tumor Classification (Full)
Transféré par
borstCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CNS Tumor Classification (Full)
Transféré par
borstDroits d'auteur :
Formats disponibles
Classification of Brain Tumors
I. Primary tumors of the brain A. Gliomas B. C. Lowest grade tumors Pilocytic astrocytoma Subependymal giant cell astrocytoma Protoplasmic astrocytoma Ganglioglioma Xanthomatous astrocytoma Subependymoma Lower grade malignancies Fibrillary (gemistocytic, protoplasmic) astrocytoma Ependymoma Oligodendroglioma Mixed oligo-astrocytoma Optic nerve glioma Higher-grade malignancies Anaplastic astrocytoma Anaplastic oligodendroglioma Anaplastic mixed glioma Highest-grade malignancies Glioblastoma multiforme Gliosarcoma Gliomatosis cerebri Meningioma Benign Atypical Malignant Primitive Neuroectodermal Tumors (Pnet) Medulloblastoma Ependymoblastoma Pineoblastoma
D. E. F. G. H. I. J.
Pituitary tumors Pituitary adenoma Pituitary carcinoma Craniopharyngioma Rathke's cleft cyst Pineal Tumors Pineal cyst Pineocytoma Pineoblastoma Germinoma Mixed germ cell tumor Pineal gliomas Pineal teratoma Choroid plexus tumors Choroid plexus papilloma Choroid plexus carcinoma Other, more benign primary tumors Neurocytoma Dysembroplastic neuroepithelial tumor (DNT) Lipoma Hemangioblastoma Hamartoma Teratoma Tumors of nerves and/or nerve sheaths Neuroma Schwannoma Neurofibroma Cysts Colloid cyst Arachnoid cysts Dermoid Epidermoid Rathke's cleft cyst Pineal cyst Other primary tumors, including skull base Chondroma
K. II.
Chordoma Sarcomas Gliosarcoma Chondrosarcoma Rhabdomyosarcoma Primary Central Nervous System Lymphoma (PCNSL) Metastatic brain tumors and carcinomatous meningitis
This information has been provided by the AANS/CNS Section on Tumors A listing of most of the tumors that occur in the brain or its surrounding structures is presented here. Sometimes a tumor may have more than one
name. The descriptions of how the tumors behave refer to the most common patterns since there are always exceptional cases (both better and worse). Higher grade malignancies are, in general, expected to grow faster than lower grade malignancies. The comments on tumor treatment usually refer to conventional therapy (surgery, radiation and cytotoxic chemotherapy) and may not include promising new, investigational or experimental treatments. Radiosurgery may be an option for most of these tumors and its use depends upon tumor size, location and the individual patient's case. If a tumor continues to grow despite treatment, additional surgery may be recommended. This also depends on the individual patient. Clinical trials are available for many of these tumors, particularly if they are malignant or recurrent. Specific tumors are listed alphabetically in the pages to follow. Discussions of spinal cord tumors , familial syndromes and the remote effects of carcinoma follow the alphabetical listing. It should be noted that this information is provided for educational purposes only, and should not be considered to be medical advice. Questions about a specific patient should be referred to a qualified surgeon or other physician. I. Primary tumors of the brain A. Gliomas Lowest grade tumors Pilocytic astrocytoma Subependymal giant cell astrocytoma Protoplasmic astrocytoma Ganglioglioma Xanthomatous astrocytoma Subependymoma Lower grade malignancies Fibrillary (gemistocytic, protoplasmic) astrocytoma Ependymoma Oligodendroglioma Mixed oligo-astrocytoma Optic nerve glioma Higher-grade malignancies Anaplastic astrocytoma Anaplastic oligodendroglioma Anaplastic mixed glioma Highest-grade malignancies Glioblastoma multiforme Gliosarcoma
B. C. D. E. F. G. H.
Gliomatosis cerebri Meningioma Benign Atypical Malignant Primitive neuroectodermal tumors (PNET) Medulloblastoma Ependymoblastoma Pineoblastoma Pituitary tumors Pituitary adenoma Pituitary carcinoma Craniopharyngioma Rathke's cleft cyst Pineal Tumors Pineal cyst Pineocytoma Pineoblastoma Germinoma Mixed germ cell tumor Pineal gliomas Pineal teratoma Choroid plexus tumors Choroid plexus papilloma Choroid plexus carcinoma Other, more benign primary tumors Neurocytoma Dysembroplastic neuroepithelial tumor (DNT) Lipoma Hemangioblastoma Hamartoma Teratoma Tumors of nerves and/or nerve sheaths Neuroma Schwannoma Neurofibroma
I. J. K. II.
Cysts Colloid cyst Arachnoid cysts Dermoid Epidermoid Rathke's cleft cyst Pineal cyst Other primary tumors, including skull base Chondroma Chordoma Sarcomas Gliosarcoma Chondrosarcoma Rhabdomyosarcoma Primary Central Nervous System Lymphoma (PCNSL) Metastatic brain tumors and carcinomatous meningitis
PRIMARY TUMORS OF THE BRAIN
Acoustic schwannoma This is a schwannoma (i.e. tumor of the nerve sheath cells -- see " schwannoma ".) which arises in the region of the eighth cranial nerve. It is located in the posterior fossa (the lower, back part of the cranial cavity, above the neck) in the angle between the cerebellum and pons. It is usually found in adults who develop hearing loss on one side. Tinnitus, a buzzing or ringing sound, may also be present; other symptoms are also possible. The tumor is benign, grows slowly, and is treated with surgery or radiosurgery. It is also known as an acoustic neuroma. There is an Acoustic Neuroma Association, which can be reached at www.ANAUSA.org . Anaplastic astrocytoma This tumor is a locally aggressive, destructive form of astrocytoma. It spreads into, or "infiltrates"normal brain, and is considered malignant. It may
occur anywhere within the central nervous system (CNS). Conventional treatment options include surgery and radiation therapy. Even after these treatments, it may recur. About half of the patients can be expected to have a partial response to chemotherapy. Experimental therapies are often recommended if the tumor continues to progress despite these standard treatments. Anaplastic mixed glioma This is an infiltrating glioma that grows relatively rapidly and contains more than one type of tumor cell -- an aggressive combination of an astrocytoma and an oligodendroglioma. Conventional treatment options include surgery and radiation therapy. The response of this tumor to chemotherapy is intermediate between anaplastic astrocytoma and anaplastic oligodendroglioma. Anaplastic oligodendroglioma An anaplastic oligodendroglioma is an aggressive (malignant) type of oligodendroglioma. Conventional treatment options include surgery and radiation therapy. Also, most of these tumors would be expected to respond to chemotherapy. A combination of procarbazine, CCNU and vincristine, called "PCV" is used. Recent evidence suggests that specific chromosomal abnormalities may predict the response to chemotherapy. Arachnoid cyst This is a sac of cerebrospinal fluid (CSF), which has been "trapped" outside or inside the brain. It might also be called a "leptomeningeal cyst". Some of these cysts may date to birth; others may arise or be diagnosed after a head injury. Usually such a cyst produces no symptoms and is found by coincidence when a patient gets scanned for a headache or after a head injury. However, the fluid (CSF) might be able to enter the sac more easily than exit, so the cyst might grow over time. On rare occasions, these cysts may cause loss of neurologic function due to stretching normal nerve cells or putting pressure on the brain, producing seizures, or even causing a hemorrhage if a blood vessel is stretched across the cyst. When surgery is warranted, either endoscopic (i.e. through an "endoscope" or small tube) or open surgery can be used, depending on the surgeon's choice and the patient's situation. The goal of the surgery is to allow for a larger passage to be created (called a fenestration) between the cyst and the normal CSF compartments. Alternatively, the collecting fluid is sometimes diverted by a tube (called a shunt) to another body cavity. Even after treatment, the cyst may not appear to change in size, since the brain often adopts the shape permanently. Similar structures that arise off the ventricular system have been called ependymal cysts. Astrocytoma An astrocytoma is a tumor that arises from astrocytes, which are cells that support and nourish the neurons of the brain. Astrocytes are one type of glia; astrocytomas are a main category of the gliomas, the tumors arising from the glia. There are many types of astrocytomas -- please refer to the specific type, such as pilocytic astrocytoma or anaplastic astrocytoma.
Butterfly glioma A tumor of the glial cells (see "glioma") that has spread across the corpus callosum (which connects the two sides of the brain) so that it involves both of the cerebral hemispheres. Surgery is rarely helpful, other than for diagnosis (biopsy). Brain stem glioma A tumor arising from the glial cells and located in the brainstem, the deepest portion of the brain. Children are often affected by this tumor. Several different pathologic types are possible; the type determines how fast the tumor will grow. Surgery, stereotactic surgery, radiation and/or chemotherapy may be used depending on the particular patient. Carcinomatous meningitis Sometimes a cancer may spread to the space around the brain or spinal cord, which contains the meninges. Here, there are no barriers to further spread throughout this space. The function of individual nerves and/or nerve roots (serving the head and body) becomes impaired. Progression is usually relentless despite radiation and chemotherapy, even when the drugs are delivered directly into the spinal fluid. These therapies are often used to attempt to stop the disease, however. This disease is also called leptomeningeal cancer. Chondroma A chondroma is a tumor that arises from cartilage, usually arising at the base of the skull. It usually grows slowly, and can become very large. The tumor can be treated by surgical removal. Chondrosarcoma This is a rare, malignant tumor arising from cartilage. It may occur in the skull at the joints between bones, or elsewhere in the skeleton. It is locally invasive, but rarely spreads to other parts of the body. Treatment consists of surgical removal, which may be followed by radiation therapy. Chordoma A chordoma is a tumor that comes from a part of the spine or skull -- called the notochord -- that is left over from fetal life. It occurs at the base of the skull, or at the end of the spine. Although this tumor is relatively grows relatively slowly and appears benign under the microscope, the behavior is more like that of a malignant tumor because it has a tendency to recur and spread. Treatments include surgery, radiation therapy, radiosurgery and in some cases, chemotherapy. Choroid plexus carcinoma This is a malignant variety of the choroid plexus papilloma (see below). It usually occurs in children, and can invade normal brain. A few patients have been cured with complete surgical removal of the tumor. Otherwise, radiation and high dose chemotherapy may be used to attempt control this tumor, because it is highly aggressive and can often be fatal. Choroid plexus papilloma This is a benign tumor that arises within the brain's ventricles from the cells (in the "choroid plexus") that make spinal fluid. A choroid plexus papilloma
generally becomes apparent during infancy or early childhood. It may cause over-production (or blockage) of spinal fluid, resulting in an accumulation of this fluid within the ventricular cavities of the brain -- this is called "hydrocephalus". The tumor is treated with surgical removal. In rare instances, the tumor may re-grow or spread throughout the nervous system. Colloid cyst This benign cyst arises in the third ventricle and is usually filled with thick, mucous-like, fluid. Thought to be present since birth, the cyst gradually grows and eventually blocks the normal flow the cerebral spinal fluid (CSF) from the lateral ventricles into the third ventricle. This is one type of hydrocephalus. If it occurs gradually, the patient may develop headache, double vision, difficult walking, memory problems or other difficulties. Sometimes a colloid cyst may produce an abrupt fluid blockage that may cause sudden coma or even death without prior warning. For this reason, many surgeons consider the discovery of a colloid cyst an indication for surgery. Management options include stereotactic aspiration, endoscopic removal (surgery through a small tube called and "endoscope") or microsurgical removal. Removing the cyst without causing brain damage can be difficult. Treatment should be individualized and take into account the experience of the surgeon. Craniopharyngioma This is a cystic tumor that arises just above the pituitary gland. It is usually first diagnosed at one of two ages -- childhood or the elderly. It grows relatively slowly. The principle threat is to vision (as the tumor may compress the optic nerves) and to the function of the pituitary gland. When very large, this tumor may threaten neurologic function or life itself due to pressure on the brain. It may also block the drainage of spinal fluid, causing hydrocephalus. Surgery is usually considered the first line treatment because a craniopharyngioma can sometimes be cured at the first operation if it is completely removed. Complete removal may not be possible however, because of "fingers" of the tumor that invades into adjacent brain structures. In some cases, simple drainage of the cyst fluid and/or injection of radioactive fluid can control the symptoms and growth. Radiosurgery or radiation therapy may be used in some cases. Although this is a relatively benign tumor, the progressive growth may be difficult to control and some patients die of this disease. Cysts These are not true tumors in the sense of being neoplasms (i.e. "new growths") or cancers; nonetheless they may expand over time putting pressure on vital brain or spinal structures. They are characterized by the accumulation of fluid or some other substance within a confining layer. Cysts may occur in isolation, or as part of a true tumor (such as a glioma, metastasis, or hemangioblastoma). Please see the specific type of brain cyst (or tumor) for further information. Dermoid or epidermoid cyst
These benign growths are due to left over (or implanted) skin tissue (dermis) within the head or spinal canal. The skin tissue grows, producing pearly scales that would be analogous to the shedding of dead skin. As this material has nowhere to go (unlike on the surface of the skin where it would be shed), it accumulates and eventually forms a mass. Treatment is surgical, although it may not be possible to cure the cyst, as often the skin cells are firmly adherent to small nerves and blood vessels. Epidermoid cysts contain just the outer layer of skin and its waste, while dermoids also include deeper layers of skin tissue that produce hair. Dysembryoplastic neuroepithelial tumor (DNT) This recently described tumor presents with intractable epilepsy in infancy and early childhood. It is usually located in the frontal or temporal lobe of the brain. A complete surgical resection can cure both the tumor and the seizures. Possible use of radiation is unclear at this point. Ependymoblastoma See primitive neuroectodermal tumors (PNETs). Ependymoma This tumor arises from the ependymal cells lining the cerebrospinal fluid sacs (ventricles) of the brain. It commonly affects children but can occur at any age. An ependymoma is a low-grade malignancy that is best treated by removing as much as is safely possible by surgery. Sometimes the tumor cells can spread through the spinal fluid. Radiation therapy is sometimes used. It has not yet been determined whether or not chemotherapy is useful in these tumors. A myxopapillary ependymoma is a benign tumor that occurs in the spine. Epidermoid See dermoid cyst. Fibrillary astrocytoma This is a tumor that grows relatively slowly, arising from astrocytes, the glial cells that nourish and support the neurons within the brain. The tumor cells of astrocytomas mix and coexist with normal brain tissue. While often referred to as "benign" tumors, they are more accurately considered lowgrade malignancies because they have the potential to, and usually do, recur or turn into high-grade malignancies over time. They are often found in young adults but can occur at any age. Other types of astrocytomas in this category are the gemistocytic and protoplasmic varieties. Treatment is dictated by the tumor's location and patient's symptoms. Surgery may benefit patients whose tumors are located in parts of the brain that are not functionally important, those with large tumors exerting pressure on the brain, or those that cause seizures. Because tumor cells grow into the normal brain and may extend an inch or more from the visible edge of the tumor, not every cell can be removed surgically. Cells left behind can lead to tumor recurrence. Because of this, follow-up scans may be needed. The role of radiation therapy is controversial for low-grade astrocytomas. Although radiation therapy may lead to longer survival, the side effects of radiation, such as impaired thinking and memory, limit its practical use in
people with these tumors. In addition, the inability to then use radiation treatments when the tumor progresses has led many doctors to defer radiation treatments in patients who are not having symptoms and whose tumors are not actively growing. Gangliocytoma This tumor arises from nerve cells and may also be called a ganglioneuroma. It usually is found in children and is rarely malignant. It may cause seizures and is usually treated by surgical removal. Ganglioglioma This tumor contains nerve cells and glial (supportive) cells and typically produces seizures beginning in childhood. The seizures may be difficult to control with medicine. Surgical removal is often feasible and is associated with good long-term tumor and seizure control for most patients. Germ cell tumor There are several types of germ cell tumors, including the germinoma (see below), embryonal carcinoma, choriocarcinoma, and yolk sac (endodermal sinus) tumors. They are relatively uncommon, and usually occur in young adults. Usual locations are near the pineal gland or in the suprasellar region (above the pituitary gland). These tumors may spread through the spinal fluid. Sometimes "tumor markers" (in the blood and or spinal fluid) are used to make the diagnosis. Treatment may include biopsy, chemotherapy and/or radiation therapy. Germinoma This tumor looks just like ovarian or testicular cancer under the microscope. It is the most common of the germ cell tumors of the brain. It may spread or "seed" through the spinal fluid. About one third of tumors in the pineal region are germinomas; however, this tumor can occur in many locations within the brain. This tumor may cause headaches, visual problems, hormonal disturbances and blockage of spinal fluid (hydrocephalus). It is treated with surgery (often a biopsy for making the diagnosis), radiotherapy and sometimes chemotherapy. The germinoma is very responsive to radiation therapy, but doctors may attempt to avoid the use of radiation in the very young. Glioblastoma multiforme This is the most common primary (i.e. from the brain itself) brain tumor affecting adults. Unfortunately, it is a rapidly growing, destructive tumor that may lead to death within months. Under the microscope, the tumor has the features of an anaplastic astrocytoma with the addition of areas of dead tissue (necrosis). Necrosis occurs because the tumor cells grow faster than new blood vessels can be produced to nourish the tumor cells. Surgery, radiation and chemotherapy are first line treatments that may prolong life to a year or so. Not all patients are candidates for surgical removal of the tumor, for example if the tumor has already spread into vital structures or to both sides of the brain (e.g. "butterfly glioma"). It is extremely rare for this tumor to be completely removed by surgery. This is because at the time of first diagnosis, it has usually already spread deep
into the brain. Removing the part of the tumor that "lights up" on the MRI or CT scan does not mean that all the malignant cells have been removed. While radiation therapy does help most patients to live a bit longer, chemotherapy only benefits about a quarter of patients. Another treatment that has been approved by the U.S. Food and Drug Administration (FDA) for these tumors is the surgical implantation of wafers containing chemotherapy directly into the area of the tumor. Radiosurgery has also been used. Immunotherapy, gene therapy and other experimental treatments are currently under investigation for this very serious disease. Glioma This is a general term for any tumor that arises from tissues of the brain other than nerve cells and blood vessels -- i.e. the "glia". There are many types of gliomas (see scheme above). The behavior of a glioma may range from truly benign to highly malignant, depending on exactly what type it is, and the individual patient. Gliomatosis cerebri The best way to think of gliomatosis cerebri is as a diffuse, infiltrating highgrade astrocytoma without a definite mass. The tumor cells are intermixed with normal tissue throughout the majority of the brain. Gliomatosis cerebri does not respond well to radiation or chemotherapy, although these may be used to attempt to slow the course of the disease. Surgery other than biopsy is also usually not an option. Gliosarcoma This tumor has the characteristics of a glioblastoma, but also includes malignant tissue that is not glial in origin (sarcoma) -- which may come, for instance, from the membranes that cover the brain. The tumor tends to be even more resistant to conventional treatments (surgery, radiation therapy and chemotherapy) than glioblastoma. Small tumors might be partially controlled by radiosurgery. Hamartoma Not a neoplasm in the usual sense, this "mass" may either be an overgrowth of tissue at its native site, or tissue growing normally but in the wrong place. A common site is in the hypothalamus where it may produce seizures. If treatment is needed at all, surgery or radiosurgery are used. Hemangioblastoma These are usually benign tumors of blood vessels, often found in the lower part of the brain (posterior fossa). They may be associated with cysts. Although usually solitary, multiple hemangioblastomas can occur in Von Hippel-Lindau disease (see below), a hereditary disorder that may also be associated with tumors of the retina, pancreas and/or kidney. This tumor may cause dysfunction of the cerebellum (causing difficulty with walking and/or co-ordination, for instance). It also may block the drainage of spinal fluid, leading to hydrocephalus. Treatment is usually by surgical removal, and can be curative. There are some reports of successful treatment with radiosurgery. Radiation therapy or radiosurgery may also be used if the tumor cannot be removed completely.
Hemangiopericytoma This is a fairly rare tumor that arises from the same cells as a meningioma. It tends to recur and spread, even to locations outside the nervous system. Treatment usually includes surgery and radiation therapy. After these treatments, patients need to be followed with scans for local recurrence, and also with studies to evaluate other organs, such as the liver and lungs. Lipoma This is a benign tumor composed of fat cells (adipose tissue). Lipomas in the head rarely cause symptoms and are often diagnosed coincidentally. Those in the spine may cause the spinal cord to become stretched or "tethered". Management, if necessary, is usually surgical. Lymphoma This is a tumor arising from lymphatic tissue (like the lymph nodes) -- which is a main component of the body's immune system. Although lymphomas from elsewhere in the body may spread to the brain, most cases of lymphoma affecting the brain originate within the brain itself. Such a tumor is called a "primary CNS lymphoma". Unless a tumor is large enough to be life threatening from its mass, treatment usually does not include surgery (except for biopsy). Symptoms may be due to increased intracranial pressure, or due to where the tumor (or tumors) are located more specifically within the brain. Traditionally, radiation was the preferred treatment, however, early chemotherapy now appears to result in longer and better survivals. One treatment for lymphoma involves disruption of the "bloodbrain barrier", so that higher doses of chemotherapy can be delivered. In many cases, CNS lymphoma occurs in patients with AIDS (acquired immunodeficiency syndrome) or in people infected with HIV (human immunodeficiency virus). Such patients do not respond to treatment in the same way as patients without AIDS/HIV. Medulloblastoma See primitive neuroectodermal tumors (PNETs). A medulloblastoma is a PNET that arises in or near the fourth ventricle. It is a fast-growing, invasive tumor, which may spread through the spinal fluid. Children are usually affected, boys more commonly than girls. Treatment includes surgical removal, staging (see PNET), and radiation and/or chemotherapy, depending on the patient's age. Meningioma A meningioma is a tumor that arises from the membranes that cover the brain and surround the central nervous system (i.e. the "linings" of the skull and spine). It is the most common benign brain tumor in adults. Meningiomas usually grow slowly; some may not grow at all and the doctor may choose to follow possible growth of the tumor with scans done over time. Symptoms may include headache, seizure, loss of brain function (such as weakness, incoordination, sensory problems), visual problems, hearing or swallowing difficulties, loss of smell or taste, or other problems depending on the location and behavior of the mass. This tumor may grow to be quite large before it produces symptoms. The explanation for this is that some
meningiomas grow so slowly that the brain can gradually shift or adapt to the presence of the tumor. On the other hand, meningiomas can be found coincidentally on scans that are being done for other reasons. Removing a small meningioma, for example, wouldn't necessarily be expected to cure someone's headaches. The preferred treatment for a meningioma is usually considered to be surgery if the lesion can be largely removed at sufficiently low risk. A more complete removal is associated with a lower risk of recurrence or progression. The surgical removal usually includes bone and/or dura (one of the layers of the meninges) into which the tumor has spread. Replacement of these structures may be needed. Radiation therapy, radiosurgery and/or growth-modifying drugs may be considered as treatment options for incompletely-removed tumors or at time of tumor recurrence or progression. A small fraction of meningiomas may be aggressive or malignant. Malignant meningiomas are treated with surgery, radiation therapy and possibly chemotherapy. Metastatic brain tumors About 1 in 4 patients with cancer will develop tumors that spread to the central nervous system (CNS), most commonly through the blood stream to the brain. Tumors that often spread to the brain include those originating in the lung, kidney (renal cell carcinoma), or breast, and also melanoma. However, almost any cancer has this potential. Metastatic tumors typically arise where the white and gray matter of the brain meet. The symptoms depend upon the function of the affected part of the brain, but also can include headache or seizures -- or no symptoms at all, when first detected. The results of treatment for metastatic brain tumors was once considered to be bleak, with survival on the order of several weeks. It has been convincingly shown, however, that aggressive surgical management combined with radiation treatment can lead to a substantially better outcome in some patients, both in terms of survival and quality of life. Control of a single metastasis to the head is better when surgery is combined with radiation therapy, in comparison to either treatment alone. The benefit of aggressive management of multiple brain metastases is less clear, yet depending on the particular patient, surgery is sometimes considered when there are life-threatening tumors, especially if the patient otherwise is in good condition. Radiosurgery has taken on an increasingly important role in the management of brain metastases. Control is thought by many to be comparable to that achieved by surgery, particularly when combined with conventional radiation treatments. Radiosurgery may also prove effective in controlling some tumors that are resistant to conventional radiation (such as melanoma and kidney cancer). The equivalence of radiosurgery to surgery for brain metastases has not been proven, however, and there are those who believe that conventional surgery is superior just as there are those who are advocates of radiosurgery. Treatment should be individualized for each patient, and the patient's medical condition and extent of cancer elsewhere
in the body must be considered. Mixed oligo-astrocytoma (mixed glioma) This tumor shares the microscopic appearance and behavior of both astrocytomas and oligodendrogliomas (see separate listings). Treatment options include surgery, radiation and/or chemotherapy. Neurinoma Note: sometimes schwannomas or neurofibromas are referred to as neuromas or neurinomas -- see descriptions of these other tumors. Neuroblastoma A neuroblastoma usually occurs outside the central nervous system. Rarely, it can occur within the brain, more commonly in children. It usually grows rapidly, causing seizures and other neurologic symptoms. It may also spread through the spinal fluid. Some may call it a PNET. Surgery, radiation therapy and/or chemotherapy may be used to attempt to control it. Neurocytoma These tumors usually arise in the fluid sacs (ventricles) of the brain and often affect young or middle aged adults. Because of this, it may cause hydrocephalus. Although usually slowly-growing and benign, some neurocytomas may be malignant. This tumor is sometimes called a "central neurocytoma". Maximal surgical resection is the treatment of choice; the tumor may be vascular (i.e. contain many blood vessels). Radiation therapy is usually reserved for progressive or more malignant-appearing neurocytomas. Neurofibroma This is a tumor of a nerve, which mixes with normal nerve tissue. It usually occurs in the nerves outside the spine and head. Since it is mixed with normal nerve tissue, surgical removal would be expected to lead to loss of function of that nerve. If left untreated, however, the tumor may continue to grow, or possibly turn into malignant tumor over time. Note: sometimes schwannomas or neurofibromas are referred to as neuromas or neurinomas. Neuroma These are benign growths of abnormal nerve tissue that usually occur at the site of a nerve injury. Neuromas may be quite painful and treatment is usually medical. Surgery can be considered for cases where pain fails to respond to medical management. Note: sometimes schwannomas or neurofibromas are referred to as neuromas or neurinomas. Oligodendroglioma These tumors are thought to arise from the oligodendrocytes, which are the cells that wrap around nerve cells and act as a form of electrical insulation for conducting the nerve impulses. Recent evidence suggests that they may actually arise from progenitor cells that are immature oligodendrocytes. These tumors also tend to occur in young adults and may contain calcium deposits that appear on brain scans. They tend to be slower growing than low-grade astrocytomas, but have the potential to turn into more aggressive tumors. Treatment is usually surgical and radiation therapy may be recommended. Chemotherapy is considered for progressive tumors, and
usually recommended for anaplastic (i.e. more malignant) oligodendrogliomas. (Also see anaplastic oligodendroglioma). Optic nerve glioma Optic nerve gliomas occur in about 10% of patients with neurofibromatosis type I (NF I -- see below), usually during childhood. They may involve the optic nerve, optic chiasm and/or optic tract, which are various parts of the visual system. The tumor usually does not spread to other parts of the brain, unless it is a higher grade (more malignant) glioma. In those without NF I, they may occur at any age. These tumors may be treated with radiation and/or chemotherapy; surgery is also sometimes used depending on the patient. Pilocytic astrocytoma This tumor is usually found in a child or young adult. The name comes from the "hair-like" appearance of the tumor cells under the microscope. The tumor is typically slowly- growing and often can be cured by complete surgical removal. Some pilocytic astrocytomas, however, may behave more aggressively or be surgically inaccessible. Treatment with radiation may eventually lead to malignant progression (more rapid growth, and brain invasion). Pineal cyst This is generally considered to be a benign lesion, rarely causing symptoms. A pineal cyst is often discovered coincidentally when a patient is scanned for an unrelated reason such as a headache. Pineal tumors These are growths that occur in the region of the pineal gland, situated deep within the brain. They may obstruct the cerebrospinal fluid (CSF) pathways, causing hydrocephalus, which is treated with a surgery to "shunt" the fluid that is accumulating. Because they are difficult to reach safely, indirect means of diagnosing these lesions may be recommended, such as special blood and/or spinal fluid tests ("marker" studies -- see germ cell tumors) or a trial of low dose radiation. A biopsy, or removal of the tumor might also be recommended, depending on the patient and test results. Also see the specific type of pineal tumor, e.g. pineocytoma. Pineoblastoma This is a PNET of the pineal gland (see PNET). It tends to grow rapidly and chemotherapy and radiation therapy is usually recommended. Pineocytoma This is a tumor derived from pineal gland tissue, but it grows more slowly than a pineoblastoma. It is treated with surgery and radiotherapy; radiosurgery has also been used. Pituitary adenomas These are common benign tumors of the pituitary gland. It is said that up to 10 percent of people will have a pituitary adenoma (which might never have caused a problem) by the time of their death. The pituitary gland is considered the "master gland" of the body; it produces hormones that regulate the other glands. Some tumors secrete one or more of these
hormones in excess. Such so-called secretory pituitary adenomas are usually found due to hormonal imbalances that affect bodily functions. They may be relatively small when detected. Syndromes of secreting pituitary adenomas:
Name
Prolactinoma
Hormone
Prolactin
Symptoms
Women: breast milk production, change in menstrual period. Men: breast enlargement, impotence. Weight gain, high blood pressure Enlarging tissue and organs, diabetes, gigantism Weight loss, irritability, heat intolerance
Cushing's disease Acromegaly Hyperthyroidism TSH & Thyroid
ACTH & Cortisone Growth Hormone
Treatment of a secretory pituitary adenoma is directed not only at controlling tumor growth, but also at eliminating hormone over-production. True prolactinomas may often be successfully treated with medicine alone, however many tumors may cause small elevations of blood prolactin but not respond to this treatment. Other secreting tumors (or prolactinomas that do not respond well to medical therapy) are treated with surgery, radiosurgery, standard radiation therapy alone, or some combination. If unchecked, some secreting pituitary adenomas may prove fatal. In contrast, non-secreting pituitary adenomas are rarely detected until they grow large enough to compress the optic nerves, resulting in some loss of vision. Again, surgery, radiosurgery, standard radiation therapy alone or a combination of these is used for treatment. These tumors tend to recur and may be quite difficult to control as they are often too large to be safely cured by surgery when found. Unchecked, patients may go blind, suffer other neurologic loss or die from pressure or infection of the brain. Pituitary carcinoma These are rare cancers of the pituitary gland. They are difficult to control locally and are usually treated with surgery and some type of radiation (radiotherapy and/or radiosurgery). They may spread to other organs of the body. Pituitary region tumors In addition to tumors of the pituitary gland itself, tumors or cysts may arise from nearby structures -- see the specific type of tumor, e.g. pituitary adenoma. Primitive neuroectodermal tumor (PNET)
This is a malignant tumor arising from cells that are believed to remain from fetal brain development. They usually occur in early childhood but may become symptomatic in adult life. In children, they commonly occur in or near a spinal fluid sac known as the fourth ventricle and are called medulloblastomas. Under the microscope, a PNET is seen to consist of densely-packed small cells that are usually blue in color (when common tissue processing is performed). PNETs have a tendency to spread over the brain and spinal cord by way of the spinal fluid. Treatment usually begins with surgery. Radiation therapy is used in adults, along with chemotherapy. Young children are usually treated with chemotherapy alone, since radiation may stunt intellectual development when given at an early age. PNET staging is an important consideration, since the extent of treatment needed depends on how widely the PNET has spread at the time of diagnosis. This "staging process" requires MRI scans of the brain and spinal column, as well as examination of the spinal fluid under the microscope to look for tumor cells. Protoplasmic astrocytoma This is a rare tumor which is typically slow-growing and displaces rather than mixes in with (i.e. infiltrates) normal brain tissue. The tumor is therefore somewhat better controlled by surgery than the more common low-grade astrocytoma. Additional treatment may include radiation therapy or radiosurgery if the tumor progresses. Pseudotumor cerebri (benign intracranial hypertension) This condition does not involve a tumor at all, hence the use of the prefix "pseudo". It refers to an increase in pressure inside the head, which can lead to loss of vision and changes in the optic nerves -- findings which can also be caused by true brain tumors. The condition may due to high levels of vitamin A, or to a major blood channel (sinus) shutting down inside the head (usually due to an infection or blood clotting disorder). In other cases the cause is unknown, but may be related to obesity. Treatment options include medical treatment of the pressure, a shunt to drain spinal fluid and lower the pressure, and/or optic nerve sheath decompression, to relieve pressure on the optic nerves. For obese patients, weight loss is also needed. Rathke's cleft cyst This is a slowly-growing fluid-filled cyst, thought to be left over from the fetal stage. The theory is that cells that should have migrated to the nasal/throat area became trapped in the region of the pituitary gland. Treatment includes observation, surgery and/or radiosurgery. Rhabdomyosarcoma This is a malignant tumor of the muscle cells. It may arise anywhere a muscle normally exists, such as near the eye. Sarcoma A sarcoma is a malignant tumor arising from connective or structural tissue such as bones, cartilage or dura (one of the linings of the skull and spine). Sarcomas are generally malignant but encompass a range of behaviors. They tend to be resistant to conventional treatments (such as surgery, radiation
and chemotherapy). Surgery and sometimes radiosurgery may be useful. Please refer to the specific type of sarcoma, e.g. gliosarcoma. Schwannoma A schwannoma typically arises along a nerve, since it is comprised of cells that normally provide the "electrical insulation" for the nerve cells. Usually benign, traditional management has consisted of surgical removal. Schwannomas often displace the remainder of the normal nerve, instead of mixing in with it (see neurofiboma). Common locations include along the nerves in the head (especially the balance or "vestibular" nerve [also known as an acoustic schwannoma]), in the spine, and, more rarely, along nerves that go to the limbs. Some schwannomas in the head may be treated with radiosurgery instead of, or in addition to, conventional microsurgery. Rarely the tumors may be malignant. Note: sometimes schwannomas or neurofibromas are referred to as neuromas or neurinomas. Subependymoma Like an ependymoma, this tumor also arises from tissue that lines the ventricles. However, it more often occurs in elderly patients. The behavior is benign. Unfortunately, subependymomas often arise from the brainstem and surgeons may have to leave some tumor behind if they are to avoid neurologic damage. Subependymal giant cell astrocytoma Generally a benign tumor, arising from tissue off the fluid sacs (ventricles) of the brain. This tumor is often seen in children and some adults with a condition called Tuberous Sclerosis. Tuberous Sclerosis is characterized by seizures, certain skin abnormalities of the face, and varying degrees of mental retardation. Treatment usually consists of surgical removal, or observation if it is not causing symptoms. Skull base tumors Please refer to the specific tumor, such as chordoma, meningioma, etc. Teratoma A benign tumor, which is a complex accumulation of normal tissue, but growing in the wrong place. The tumor may include hair, teeth, muscle and a variety of other tissues. Treatment is surgical. Xanthomatous astrocytoma (pleomorphic xanthastrocytoma) This is a rare tumor usually seen in young adults, often found in a temporal lobe after a seizure. It tends not to infiltrate (mix) with normal brain tissue, but may spread along the meninges. The tumor and further seizures are usually controlled by its surgical removal, but it is intermediate in its' grade (i.e. degree of malignancy). Follow-up scans over time are recommended. Radiation, radiosurgery and/or re-operation may be suggested for a recurrent tumor.
ADDITIONAL INFORMATION
SPINAL TUMORS Many of the types of tumors described above (especially glioblastoma,
astrocytoma and ependymoma) can affect the spinal cord (without being present in the brain). Metastatic tumors often involve the bones of the spine, and/or the spinal cord. There are also tumors of the spinal nerves (such as neurofibromas or schwannomas), lining of the spinal canal (meningiomas), and spinal fluid compartment (meningeal carcinomatosis or gliomatosis). Primary tumors may arise from the bones of the spine itself. Treatment is often the same as for their cranial counterparts, although radiosurgery for the spine is in its infancy and is generally considered investigational. FAMILIAL SYNDROMES In some cases, tumors affecting the nervous system are part of a constellation of problems as opposed to being an isolated tumor. In addition, these syndromes may be passed on to the children of the affected person. For autosomal dominant illnesses the risk of a child getting the disorder from one affected parent is 1 in 2 or 50 per cent. Neurofibromatosis This disease is also known as von Recklinghausen's Disease and is generally divided into two types: Neurofibromatosis type I is characterized by tumors of the "peripheral" nerves that run throughout the limbs, trunk and head. These tumors may include plexiform neurofibromas and/or schwannomas. It is associated with particular patches of skin discoloration called "caf-au-lait" spots. In extreme cases the skin tumors can be disfiguring. Abnormalities of other organs and bones may also occur. Although many cases occur spontaneously, they persons afflicted with NF I can pass it on to their offspring as an autosomally dominant trait. Neurofibromatosis type II is often associated with schwannomas (neuromas) of both vestibular nerves. It often leads to deafness, due either to the tumors or their treatment. Other tumors such as gliomas of the optic nerves or hypothalamus, ependymomas or multiple meningiomas are common. Both spontaneous and hereditary forms occur and the disease is passed on as an autosomcal dominant disorder. Lindau Syndrome This disease (also known as von Hippel-Lindau disease) is characterized by the presence of multiple hemangioblastomas, usually in the cerebellum, and the spinal cord, as well as tumors of the retina, pancreas and kidney. Surgery can be used to treat both the brain and spinal cord lesions while radiosurgery has been reported to control some brain lesions. Inheritance is autosomal dominant. Information about the von Hippel-Lindau Family Alliance can be viewed atwww.vhl.org . Tuberous Sclerosis This syndrome often presents in childhood and is characterized by seizures, mental retardation, specific facial lesions (hamartomas) and areas of skin discoloration. Tumors of the lining of the ventricles (subependymal giant cell astrocytomas) may block flow of the cerebrospinal fluid leading to a backup of the fluid called hydrocephalus. The tumors and hydrocephalus are usually treated with surgery. Inheritance is autosomal dominant.
Remote effects of carcinoma Some tumors produce chemicals or hormones that can directly or indirectly cause nerve cells to die or malfunction without physically contacting those nerve cells. These chemicals are carried through the blood stream to remote areas. Although these remote effects of carcinoma are rare, they can be incapacitating. Treatment usually requires effective control of the tumor producing the substances.
Vous aimerez peut-être aussi
- Louis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFDocument2 424 pagesLouis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFPan50% (2)
- AAP January 2022 Complete Issue Pediatrics in ReviewDocument71 pagesAAP January 2022 Complete Issue Pediatrics in ReviewsureshPas encore d'évaluation
- WHO Classification of Tumours of The Central Nervous System 4th EdDocument313 pagesWHO Classification of Tumours of The Central Nervous System 4th EdRandy UlloaPas encore d'évaluation
- Brain TumorsDocument72 pagesBrain Tumorsmo_mibPas encore d'évaluation
- CNS Tumors: Adult Tumors Tend To Be Supratentorial (70%) Pediatric Tumors Tend To Be Infratentorial (70%)Document8 pagesCNS Tumors: Adult Tumors Tend To Be Supratentorial (70%) Pediatric Tumors Tend To Be Infratentorial (70%)Jessica Febrina WuisanPas encore d'évaluation
- Depression in Temporal Lobe EpilepsyDocument33 pagesDepression in Temporal Lobe EpilepsysheranadhilaPas encore d'évaluation
- Why Creation of Universe Is Not An AccidentDocument48 pagesWhy Creation of Universe Is Not An AccidentsmtdrkdPas encore d'évaluation
- Tumors of The Nervous SystemDocument43 pagesTumors of The Nervous SystemAli Can Gunes100% (1)
- National Parks of Canada Summative TaskDocument7 pagesNational Parks of Canada Summative Taskapi-265754486Pas encore d'évaluation
- EpilepsyDocument133 pagesEpilepsyMartinPas encore d'évaluation
- Jaguar X-TYPE 2003.5 Drivers HandbookDocument188 pagesJaguar X-TYPE 2003.5 Drivers HandbookamlatasPas encore d'évaluation
- Temporal o Be EpilepsyDocument35 pagesTemporal o Be EpilepsyLivilia MiftaPas encore d'évaluation
- 13 Signs of Narcissists Who Sabotage Your Happiness - Diseases CureDocument6 pages13 Signs of Narcissists Who Sabotage Your Happiness - Diseases Curetigerlo75100% (1)
- Pathology of CNS TumorsDocument58 pagesPathology of CNS TumorsNaglaa RamadanPas encore d'évaluation
- Living with A TBI (Traumatic Brain Injury): From My PerspectiveD'EverandLiving with A TBI (Traumatic Brain Injury): From My PerspectivePas encore d'évaluation
- Psychological DisordersDocument48 pagesPsychological DisordersBrian WuPas encore d'évaluation
- The Spectrum of Mitochondrial Disease Ep-3-10Document8 pagesThe Spectrum of Mitochondrial Disease Ep-3-10F4AR100% (1)
- Terminology of Phylogenetic TreesDocument36 pagesTerminology of Phylogenetic TreesDimo PratannaPas encore d'évaluation
- In the Midst of It All: Depression and the Bible Verses that Got Me ThroughD'EverandIn the Midst of It All: Depression and the Bible Verses that Got Me ThroughPas encore d'évaluation
- Neurophysiology of Juvenile Myoclonic EpilepsyDocument10 pagesNeurophysiology of Juvenile Myoclonic EpilepsyDiana Marcela Cornejo SanchezPas encore d'évaluation
- Dissociative NewDocument15 pagesDissociative NewJennifer DixonPas encore d'évaluation
- T-Lymphocyte and Inflammatory Cell Research in AsthmaD'EverandT-Lymphocyte and Inflammatory Cell Research in AsthmaG. JollesPas encore d'évaluation
- 8 Strategies For Effective Trauma RecoveryDocument7 pages8 Strategies For Effective Trauma RecoveryPine HIllPas encore d'évaluation
- Missing The Diagnosis - The Hidden Medical Causes of Mental Disorders by William Matteson, PHDocument134 pagesMissing The Diagnosis - The Hidden Medical Causes of Mental Disorders by William Matteson, PHjonascarvPas encore d'évaluation
- Brain CancerDocument22 pagesBrain CancerNatália Martins HoffmannPas encore d'évaluation
- Appendix 4 A Exploring Challenging Behaviors Pulling It Together WorksheetDocument5 pagesAppendix 4 A Exploring Challenging Behaviors Pulling It Together WorksheetrafaelPas encore d'évaluation
- Alzheimer Disease and Other DementiasDocument28 pagesAlzheimer Disease and Other DementiasIlham 123456Pas encore d'évaluation
- Inflamed Blood Vessels (Vasculitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandInflamed Blood Vessels (Vasculitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Brain Brief Right Brain-Left Brain FinalDocument2 pagesBrain Brief Right Brain-Left Brain FinalGlaiza Leigh AgonoyPas encore d'évaluation
- Psychiatric Disorders: Iwan Arijanto, DR., SPKJ, MkesDocument40 pagesPsychiatric Disorders: Iwan Arijanto, DR., SPKJ, MkesNabila Shery LarasatiPas encore d'évaluation
- Neuron Communication LectureDocument31 pagesNeuron Communication LectureJennifer Isom Schmidtke, Ph.D.100% (1)
- Week 5 - Clinical PsychologyDocument89 pagesWeek 5 - Clinical PsychologyDora SimunovicPas encore d'évaluation
- Hereditary Hemochromatosis? and Vitamin D Deficiency from Uvb Radiation (Sunlight) Originating from Northern Europe: The Cause of Multiple SclerosisD'EverandHereditary Hemochromatosis? and Vitamin D Deficiency from Uvb Radiation (Sunlight) Originating from Northern Europe: The Cause of Multiple SclerosisPas encore d'évaluation
- 11 Diabetic FootDocument37 pages11 Diabetic Footkim suhoPas encore d'évaluation
- Neuroplasticity: How to Boost Neurogenesis and Rewire Your Brain (Active Pain Management That Helps You Get Back to the Life You Love)D'EverandNeuroplasticity: How to Boost Neurogenesis and Rewire Your Brain (Active Pain Management That Helps You Get Back to the Life You Love)Pas encore d'évaluation
- Radiation Toxicity: 31.1 Principles of RadioactivityDocument9 pagesRadiation Toxicity: 31.1 Principles of RadioactivityVarshith GandlaPas encore d'évaluation
- Movement Disorders & Multiple Sclerosis-Kumar & Clark'sDocument8 pagesMovement Disorders & Multiple Sclerosis-Kumar & Clark'sindia2puppyPas encore d'évaluation
- ICD-10 F60-62 Personality Disorders - F62.0 Chronic PTSDDocument8 pagesICD-10 F60-62 Personality Disorders - F62.0 Chronic PTSDDavid A CohenPas encore d'évaluation
- Neurocognitive DisordersDocument26 pagesNeurocognitive Disordershaidar aliPas encore d'évaluation
- Assertiveness Training Guide The Importance of Connecting Physical, Intellectual, Emotional, and Spiritual Energies to Build Strong Relationships with PeopleD'EverandAssertiveness Training Guide The Importance of Connecting Physical, Intellectual, Emotional, and Spiritual Energies to Build Strong Relationships with PeoplePas encore d'évaluation
- Multiple Sclerosis, A Simple Guide To The Condition, Treatment And Related ConditionsD'EverandMultiple Sclerosis, A Simple Guide To The Condition, Treatment And Related ConditionsPas encore d'évaluation
- Scorn Not Her Complexity (Epilepsy, My Love!)D'EverandScorn Not Her Complexity (Epilepsy, My Love!)Pas encore d'évaluation
- Get Psyched! Volume 1, Fall 2011Document29 pagesGet Psyched! Volume 1, Fall 2011Danlan WhitworthPas encore d'évaluation
- Psychogenic Nonepileptic Seizures - Management and Prognosis - UpToDateDocument18 pagesPsychogenic Nonepileptic Seizures - Management and Prognosis - UpToDateAndré MendonçaPas encore d'évaluation
- Modern Anti Depression Management, Recovery, Solutions and Treatment: A Guidebook for healing, mindfulness & understanding depression in relationships, men & women, husbands, teenagers, kids, etc.D'EverandModern Anti Depression Management, Recovery, Solutions and Treatment: A Guidebook for healing, mindfulness & understanding depression in relationships, men & women, husbands, teenagers, kids, etc.Pas encore d'évaluation
- Brain TumorDocument9 pagesBrain TumorSara SabirPas encore d'évaluation
- AstrositomaDocument29 pagesAstrositomaFitria NurulfathPas encore d'évaluation
- Glioma in Adults - Beyond The Basics (High-Grade)Document9 pagesGlioma in Adults - Beyond The Basics (High-Grade)Hugh Ell - auPas encore d'évaluation
- Brain CancerDocument29 pagesBrain CancerMaria VisitacionPas encore d'évaluation
- Anaplastic AstrocytomaDocument9 pagesAnaplastic AstrocytomaputsaputraPas encore d'évaluation
- Brain Cancer: by Cara KlingamanDocument16 pagesBrain Cancer: by Cara KlingamanLouis FortunatoPas encore d'évaluation
- B.2. 0Document7 pagesB.2. 0Bahna LucianPas encore d'évaluation
- Brain Tumor: Classification and External ResourcesDocument5 pagesBrain Tumor: Classification and External ResourcestheamaciasPas encore d'évaluation
- BRAIN TUMOR-Online Learning 1Document11 pagesBRAIN TUMOR-Online Learning 1エルミタ ジョイ ファティマPas encore d'évaluation
- BRAIN Tumors PDFDocument44 pagesBRAIN Tumors PDFHalima Assi100% (1)
- Meningioma BrochureDocument16 pagesMeningioma BrochureAyu Rahmi AMyPas encore d'évaluation
- Brain Tumor - Adults: Contents of This PageDocument5 pagesBrain Tumor - Adults: Contents of This PageSam StancerPas encore d'évaluation
- Brain Cancer: by Cara KlingamanDocument16 pagesBrain Cancer: by Cara Klingamanrenu_gang1552Pas encore d'évaluation
- TUMOURS IN PAED-WPS OfficeDocument6 pagesTUMOURS IN PAED-WPS OfficePraise ToluwalasePas encore d'évaluation
- Brain TumorsDocument34 pagesBrain TumorsbenedictusPas encore d'évaluation
- Glioma in Adults - Beyond The Basics (Low-Grade)Document9 pagesGlioma in Adults - Beyond The Basics (Low-Grade)Hugh Ell - auPas encore d'évaluation
- Nodal Stations of The AbdomenDocument8 pagesNodal Stations of The Abdomenborst0% (1)
- DOAC - Review Article Direct Oral AnticoagulantsDocument12 pagesDOAC - Review Article Direct Oral AnticoagulantsborstPas encore d'évaluation
- Brain Herniation - Smirniotopoulos (RSNA 2007)Document20 pagesBrain Herniation - Smirniotopoulos (RSNA 2007)borstPas encore d'évaluation
- Phakomatoses - Smirniotopoulos (RSNA 2007)Document17 pagesPhakomatoses - Smirniotopoulos (RSNA 2007)borstPas encore d'évaluation
- Intraaxial Masses - Astrocytoma - Smirniotopoulos (AFIP 2008)Document18 pagesIntraaxial Masses - Astrocytoma - Smirniotopoulos (AFIP 2008)borstPas encore d'évaluation
- Common Adult Brain Tumors - Smirniotopoulos (RSNA 2003)Document11 pagesCommon Adult Brain Tumors - Smirniotopoulos (RSNA 2003)borstPas encore d'évaluation
- Ring Enhancing Lesions - SmirniotopoulosDocument5 pagesRing Enhancing Lesions - SmirniotopoulosborstPas encore d'évaluation
- Schreibman - Shoulder ImagingDocument21 pagesSchreibman - Shoulder ImagingborstPas encore d'évaluation
- Ring Enhancing Lesions - SmirniotopoulosDocument5 pagesRing Enhancing Lesions - SmirniotopoulosborstPas encore d'évaluation
- Schreibman - BoneTumors ChartDocument1 pageSchreibman - BoneTumors ChartborstPas encore d'évaluation
- Schreibman - Radiology of Joint Disease - My Practical ApproachDocument16 pagesSchreibman - Radiology of Joint Disease - My Practical ApproachborstPas encore d'évaluation
- Schreibman - Bone Tumors in 1 Simple ChartDocument31 pagesSchreibman - Bone Tumors in 1 Simple ChartborstPas encore d'évaluation
- Schreibman Arthrography HandoutDocument11 pagesSchreibman Arthrography HandoutborstPas encore d'évaluation
- Neuroradiology DDXDocument4 pagesNeuroradiology DDXborstPas encore d'évaluation
- Principles of Computerized Tomographic ImagingDocument335 pagesPrinciples of Computerized Tomographic Imagingborst100% (2)
- Radiology Notes - UltrasoundDocument15 pagesRadiology Notes - UltrasoundborstPas encore d'évaluation
- J Neurol Neurosurg Psychiatry 1999 Catsman Berrevoets 755 7Document4 pagesJ Neurol Neurosurg Psychiatry 1999 Catsman Berrevoets 755 7Mihaela LitovcencoPas encore d'évaluation
- Radiation Oncology For Pediatric CNS Tumors - Mahajan & Paulino, 1E (2018)Document625 pagesRadiation Oncology For Pediatric CNS Tumors - Mahajan & Paulino, 1E (2018)Bogdan Alexandru CristeiPas encore d'évaluation
- S974 Abstract Book ESTRO 2022: Variable N (%)Document1 pageS974 Abstract Book ESTRO 2022: Variable N (%)andresPas encore d'évaluation
- Childhood Solid Tumors: For C-1 StudentsDocument72 pagesChildhood Solid Tumors: For C-1 StudentsYemata HailuPas encore d'évaluation
- Article OralDocument36 pagesArticle Oralamina-fakirproPas encore d'évaluation
- Central Nervous System Tumours: WHO Classification of Tumours - 5th EditionDocument584 pagesCentral Nervous System Tumours: WHO Classification of Tumours - 5th EditionSamira KhalilPas encore d'évaluation
- Childhood MedulloblastmaDocument17 pagesChildhood MedulloblastmaIrenaPas encore d'évaluation
- Arab Board Final 2018 - 2Document12 pagesArab Board Final 2018 - 2lonsilord17Pas encore d'évaluation
- Ielts Essay Writing Task 2Document8 pagesIelts Essay Writing Task 2ezke4pq2100% (2)
- First Aid Q&A EmbryologyDocument13 pagesFirst Aid Q&A EmbryologyzyadPas encore d'évaluation
- MedulloblastomaDocument2 pagesMedulloblastomaAnurag KashyapPas encore d'évaluation
- Kyle's DDXDocument47 pagesKyle's DDXEva Yeung100% (2)
- Intracranial Tumors DeangelisDocument419 pagesIntracranial Tumors DeangelisMuhammad Taufiq Regia ArnazPas encore d'évaluation
- Tumours of The Central Nervous System: FM Brett MD., FrcpathDocument57 pagesTumours of The Central Nervous System: FM Brett MD., FrcpathRerendhutPas encore d'évaluation
- In Braunds Clinical Neurology in Small Animals LoDocument24 pagesIn Braunds Clinical Neurology in Small Animals LoNxyz GxyzPas encore d'évaluation
- Epidemiology, Natural History, Pathology and Management of Medulloblastoma in ChildrenDocument48 pagesEpidemiology, Natural History, Pathology and Management of Medulloblastoma in ChildrenSam OlukaPas encore d'évaluation
- Embryonal Tumors of The Central Nervous System: Robert Y. Shih, LTC, MC, USA Kelly K. Koeller, MDDocument17 pagesEmbryonal Tumors of The Central Nervous System: Robert Y. Shih, LTC, MC, USA Kelly K. Koeller, MDAkhileshPas encore d'évaluation
- Advances in Molecular Pathology Into Brain Tumor DiajDocument29 pagesAdvances in Molecular Pathology Into Brain Tumor DiajAkshhata NarulkarPas encore d'évaluation
- Pathology of The Nervous SystemDocument163 pagesPathology of The Nervous SystemEmmanuel De Leon100% (1)
- Brain TumorsDocument3 pagesBrain TumorsDrashty DesaiPas encore d'évaluation
- Cancer CellDocument146 pagesCancer CellmanbastiPas encore d'évaluation
- Tumours of The Central Nervous System: FM Brett MD., FrcpathDocument57 pagesTumours of The Central Nervous System: FM Brett MD., FrcpathDrGasnasPas encore d'évaluation
- Pediatric Brain TumorsDocument19 pagesPediatric Brain TumorsTezza DinayantiPas encore d'évaluation
- Pediatric Cancer v2 Teratoid Rhabdoid (UnitedVRG)Document358 pagesPediatric Cancer v2 Teratoid Rhabdoid (UnitedVRG)Andreea100% (1)
- Case PresentationDocument31 pagesCase PresentationYogaPratayogaMPas encore d'évaluation
- Pediatric Brain TumorsDocument19 pagesPediatric Brain TumorsAngeline Pankaj TirkeyPas encore d'évaluation
- MedulloblastomaDocument67 pagesMedulloblastomaAmira YasminePas encore d'évaluation