Académique Documents
Professionnel Documents
Culture Documents
Description: Tags: Qs-And-As
Transféré par
anon-608051Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Description: Tags: Qs-And-As
Transféré par
anon-608051Droits d'auteur :
Formats disponibles
Archived Information Archived Information
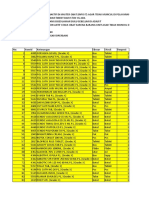
Medicare Prescription Drug Coverage: Q & A
Archived Information
Q: Who Is Eligible For Medicare Prescription Drug Coverage?
¾ A: All People With Medicare Can Enroll In Medicare Prescription Drug Coverage. Anyone who has Medicare is
eligible for the prescription drug benefit.
Q: How Much Will Average Beneficiaries Save By Enrolling In Medicare Prescription Drug Coverage?
¾ A: Average Beneficiaries Can Save More Than 50 Percent Of Their Annual Drug Costs, On Average, When They
Join A Medicare Drug Plan, Compared To What They Were Previously Spending With No Drug Coverage. That's
an average annual savings of $1,100 compared to people without coverage. People can see even larger savings when
they switch to generic medications (which are as safe and effective as brand-name medications) or other brand-name
drugs that are therapeutically equivalent to their original medications. Seniors and persons with disabilities are seeing
Medicare drug plan premiums that are even lower than expected: the average Medicare drug plan premium is down
from $37 per month to $25 per month, nearly $150 per year less than expected. People who qualify for the extra help
will save even more: they can join a Medicare drug plan and pay no premium, no deductible, and $1 – $5 for their
prescriptions. Taxpayers are also saving billions: since last July, the projected cost of providing Medicare prescription
drug coverage has come down by $7.6 billion for 2006, and $30 billion over next five years.
Q: How Can People Get More Information About Choosing And Joining A Medicare Drug Plan?
¾ A: People Can Get More Information And Sign Up Online, Over The Phone, Or In Person At Enrollment Events
In Their Communities. Medicare is providing many ways for people to learn about this new coverage and get help
choosing a plan. These opportunities include: Calling 1-800-MEDICARE (1-800-633-4227; TTY users call 1-877-486-
2048), visiting Medicare's online enrollment center at www.medicare.gov, and attending events at local places in the
community such as schools, senior centers, clubs, faith-based organizations, and pharmacies. The Eldercare Locator
can help people find places to go to get personalized assistance in comparing plan choices. For the telephone number,
visit www.eldercare.gov on the Web. Or, people can call their local office on aging for help.
Q: When Should People With Medicare Join A Medicare Drug Plan?
¾ A: People Should Join As Soon As Possible – People Who Join After May 15, 2006 May Have To Pay A Higher
Premium That Includes A Penalty, And They May Have To Wait To Join. People who don't join a plan by May 15
and don't currently have drug coverage from another source that, on average, covers at least as much as the standard
Medicare prescription drug coverage, may have to wait until November 15, 2006 to join. When they do join, their
premium cost may go up at least one percent per month for every month that they wait to join, and they will have to pay
this penalty as long as they have Medicare prescription drug coverage. For best results, people should sign up for a
Medicare drug plan early in the month, to ensure they get the most out of their coverage from the first day it is effective.
Q: How Extensive Are The Lists Of Drugs Covered By Medicare Drug Plans?
¾ A: Formularies For The Medicare Plans Are Very Extensive, Covering Typically 80 Or More Of The Top 100
Drugs Used By People With Medicare. Formularies must always include more than one drug in each class, and all
plans must have procedures to ensure that people have access to medically necessary drugs not included on their
formularies. Plans are required to have timely and efficient processes in place for people to request exceptions to
formularies, and to get prior authorization (pre-approval from plan sponsors) where clinical information is needed to help
make sure that a drug is being used appropriately and safely. Medicare will monitor plans to ensure these requirements
are being met and can take further enforcement action if plan performance in this area interferes with people's ability to
obtain needed medications on a timely basis.
4/4/2006 White House Office Of Communications
Q: Is It True That Some People Have Access To Fewer Drugs Under Medicare Prescription Drug Coverage?
¾ A: All Medicare Drug Plans Are Required To Cover All Medically Necessary Drugs. For drugs not on a plan's
formulary (list of covered drugs), a safe and effective similar drug should be available. Many of the medications that
plans do not cover have generic equivalents that cost much less and are paid for by the plans. When a specific drug is
not covered, Medicare requires that generic equivalents or other drugs that treat the same condition are covered. It is
misleading to imply plans aren't providing access to needed medications because some specific drugs are not covered.
Q: How Does Medicare Prescription Drug Coverage Help Beneficiaries With Limited Income And Resources?
¾ A: Medicare Will Pay Nearly All Of The Drug Costs For People With Limited Income And Resources. Millions of
people with Medicare are eligible to join a Medicare drug plan without premiums, deductibles, or gaps in coverage. On
average, Medicare will pay for more than 95 percent of the costs of prescription drugs for people who qualify. Last fall,
millions of applications for extra help were mailed to many low-income seniors and Americans with disabilities.
Applications are also available at locations around the country, including over 30,000 pharmacies, or through the Social
Security Administration or 1-800 MEDICARE. People can also apply online at www.socialsecurity.gov or call 1-800-772-
1213 (TTY 1-800-325-0778), or visit any Social Security office. There is no cost or obligation to apply for extra help, and
no financial documents or complicated records are required, so anyone who thinks they may qualify should apply.
Q: Will Some People Be Automatically Enrolled In A Medicare Drug Plan?
¾ A: Individuals On Medicare Who Had State Medicaid Prescription Drug Coverage Were Enrolled In A Medicare
Drug Plan – All Others Who Want Prescription Drug Coverage Must Enroll In A Plan. CMS will automatically
enroll those who automatically qualify for extra help because they receive Supplemental Security Income (SSI) benefits
or receive help from their State paying their Medicare premium (belong to a Medicare Savings Program). CMS will also
automatically enroll those who apply with the Social Security Administration (SSA) or their State and qualify for extra
help. CMS is letting beneficiaries in these groups know which Medicare drug plan they will be enrolled in if they take no
action before April 30 and has begun mailing letters to approximately 1.2 million people who qualify for extra help,
informing them of their plan assignment.
Q: Are There Differences Between The Medicare Drug Plans?
¾ A: Yes, Medicare Drug Plans Are Different In Terms Of What Drugs They Cover, The Premium And Co-Pay
Amounts They Charge Their Members, And Which Pharmacies They Use. However, all Medicare drug plans must
provide at least a basic standard of coverage set by Medicare. For more information on the different drug plans
available in their area, people should visit www.medicare.gov or call 1-800-MEDICARE (1-800-633-4227; TTY users
call 1-877-486-2048). Assistance can also be obtained from State Health Insurance Assistance Programs (SHIPs) and
partner organizations including pharmacists, senior centers, the AARP, and the Council on Aging.
Q: What Is The “Transition Period,” And What Is The Significance Of It Having Ended March 31, 2006?
¾ A: The Transition Period Is Designed To Give People Time To Work With Their Physician And Pharmacist To
Ensure Their Specific Drug Plan Meets Their Needs. During the transition period, Medicare requires drug plans to fill
new prescriptions even if the prescription is for a drug that's not on the plan's formulary. People enrolled in a Medicare
drug plan with coverage effective on January 1, 2006 or February 1, 2006 are covered by the transition policy through
March 31, 2006. People who join a Medicare drug plan March 1, 2006 or later are covered by a one-time, 30-day supply
of the prescription. Prescription drug plans have been notifying beneficiaries about their coverage requirements over the
last few months, and the transition deadlines will not affect drugs in six critical classes (chemotherapy, HIV/AIDS, anti-
depressants, anti-psychotics, anti-convulsant agents and immunosuppressants). CMS requires plans to cover all drugs
in those classes. For drugs not in these six classes, people can ask their physicians to prescribe a medication on their
plan's formulary that will work as well as the medication that they have under the transition policy, ask their plan for help
in filing an exception to the formulary or appeal, or people can call 1-800-MEDICARE for assistance.
4/4/2006 White House Office Of Communications
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 785 - List of References For Submission of New Request Inquiry FormDocument3 pages785 - List of References For Submission of New Request Inquiry Formعبدالعزيز بدر0% (1)
- Summer Internship Report PGDHMDocument53 pagesSummer Internship Report PGDHMAnisha Khundongbam50% (6)
- March 2022 Workbook - Impurities in Drug Products and Drug Substances - A USP ApproachDocument209 pagesMarch 2022 Workbook - Impurities in Drug Products and Drug Substances - A USP ApproachirhamfauzziPas encore d'évaluation
- CSCC43: Tutorial #6: ER ProblemDocument2 pagesCSCC43: Tutorial #6: ER ProblemAziz.3251Pas encore d'évaluation
- TheNewYorkTimes Tuesday October 23 2012Document60 pagesTheNewYorkTimes Tuesday October 23 2012pardostPas encore d'évaluation
- CV May 2020 - Karen DavidgeDocument7 pagesCV May 2020 - Karen Davidgeapi-490357188Pas encore d'évaluation
- Incepta Available Products For RegistrationDocument4 pagesIncepta Available Products For RegistrationDefi 15Pas encore d'évaluation
- Chapter 6 SolutionDocument18 pagesChapter 6 SolutionHardik SharmaPas encore d'évaluation
- ADR Final1Document10 pagesADR Final1Rubina BisankhePas encore d'évaluation
- Module No. 2 Drug Dosage and CalculatioonsDocument7 pagesModule No. 2 Drug Dosage and CalculatioonsJellie An TalattagPas encore d'évaluation
- Rekapitulasi Februari 2023Document13 pagesRekapitulasi Februari 2023hanafiPas encore d'évaluation
- Material Management in HospitalsDocument14 pagesMaterial Management in HospitalsfarmanPas encore d'évaluation
- 2019 - Fedhealth GP Network Practice GuideDocument24 pages2019 - Fedhealth GP Network Practice GuideYarik MechanicPas encore d'évaluation
- Pharmacy and Therapeutics Committee Policies and ProceduresDocument11 pagesPharmacy and Therapeutics Committee Policies and ProceduresJedDesabille67% (3)
- Jyotishwar Naidu - MALE - 55 Yrs +917995685885 APJ1.0015520637 2348391Document2 pagesJyotishwar Naidu - MALE - 55 Yrs +917995685885 APJ1.0015520637 2348391Reviews SanjuPas encore d'évaluation
- ASSIGNMENT On Code of EthicsDocument7 pagesASSIGNMENT On Code of EthicsRinta MoonPas encore d'évaluation
- Review On "Regulatory Approval Process of INDA, NDA and Anda in India and Foreign Countries (Us, Europe, China, Australia, Canada) "Document16 pagesReview On "Regulatory Approval Process of INDA, NDA and Anda in India and Foreign Countries (Us, Europe, China, Australia, Canada) "International Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Galaxo Smith Kline PPT Sector AnalysisDocument16 pagesGalaxo Smith Kline PPT Sector Analysissubhajit812Pas encore d'évaluation
- Medication Error-Hisfarmasi PresentationDocument102 pagesMedication Error-Hisfarmasi PresentationLaura Khristiani MarbunPas encore d'évaluation
- Essential Drug List Therapeutic Categories 4d Edition March 2007 YEMENDocument11 pagesEssential Drug List Therapeutic Categories 4d Edition March 2007 YEMENportosinPas encore d'évaluation
- Transcript ApplicationDocument2 pagesTranscript ApplicationSwetha ReddyPas encore d'évaluation
- 11 PD Drug Interaction EngDocument14 pages11 PD Drug Interaction EngshahrukhziaPas encore d'évaluation
- Project Master ObatDocument69 pagesProject Master Obatbunga200Pas encore d'évaluation
- Amphetamine Mixed Salts ERDocument2 pagesAmphetamine Mixed Salts ERsunil babuPas encore d'évaluation
- 1 PB - En.idDocument8 pages1 PB - En.idAbel Leoni AlvienaPas encore d'évaluation
- Formulation and Evaluation of Enteric CoatedDocument13 pagesFormulation and Evaluation of Enteric Coatedvanvu buiPas encore d'évaluation
- Drug ListDocument127 pagesDrug Listnehal choudharyPas encore d'évaluation
- Philippine National Formulary - Essential Medicines ListDocument66 pagesPhilippine National Formulary - Essential Medicines ListShiraishiPas encore d'évaluation
- Angela Dela Cruz-MunarrizDocument29 pagesAngela Dela Cruz-MunarrizangelaPas encore d'évaluation
- Pharmaceutics Dosage Form and Design: David JonesDocument3 pagesPharmaceutics Dosage Form and Design: David JonesArfan MughalPas encore d'évaluation