Académique Documents
Professionnel Documents
Culture Documents
Ergonomic Assessment Tool11845
Transféré par
Shanthoshini BaskaranCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ergonomic Assessment Tool11845
Transféré par
Shanthoshini BaskaranDroits d'auteur :
Formats disponibles
Arthritis & Rheumatism (Arthritis Care & Research) Vol. 59, No.
10, October 15, 2008, pp 14951503 DOI 10.1002/art.24116 2008, American College of Rheumatology
SPECIAL ARTICLE: DISABILITY AND REHABILITATION IN THE RHEUMATIC DISEASES
The Ergonomic Assessment Tool for Arthritis: Development and Pilot Testing
CATHERINE L. BACKMAN,1 JUDY VILLAGE,2
AND
DIANE LACAILLE1
Objective. Ergonomic assessment and recommendations may help people with arthritis maintain employment; however, most ergonomic tools are designed to assess injury risk in the general population and are not specic to the needs of people with inammatory arthritis (IA). Our objectives were to design and pilot test an ergonomic assessment tool for people with IA and to propose ergonomic modications to prevent work loss and maintain at-work productivity. Methods. Relevant content was identied in a literature review by an interdisciplinary team. Respecting some clients reluctance to disclose arthritis to employers, no work site visit was required. An initial assessment tool was reviewed by a 4-person expert panel, revised and pretested with 13 adults with IA by 3 occupational therapists (OTs). The nal tool, comprised of a self-assessment, an interview guide, and a solutions summary, was used in a pilot test of a multifaceted program designed to prevent work loss and maintain at-work productivity. One OT conducted all ergonomic consultations and followed up with phone calls at 1 month. Implementation of recommendations was evaluated at 3, 6, and 12 months. Results. Nineteen women (mean age 51 years) with IA (mean disease duration 12 years) completed ergonomic assessments. A range of risks were identied and 87 recommendations were made (mean 4.5 per participant). At 1 year, 85% of recommendations had been implemented by 74% of the participants. Conclusion. The Ergonomic Assessment Tool for Arthritis is a feasible and comprehensive process for identifying ergonomic job accommodations.
INTRODUCTION
Arthritis in the work place is relatively common. Population-based surveys of employed Americans indicate that more than 5% of the work force reports arthritis (1). Among employees ages 40 64 years, this increases from between 10% (1) to 15% (2,3). The economic costs are substantial: lost productivity due to arthritis has been val-
Supported by an operating grant from the Canadian Institutes for Health Research and from The Arthritis Society of Canada. Dr. Lacaille is the Nancy and Peter Paul Saunders Scholar and is supported by an Investigator Award from The Arthritis Society of Canada. 1 Catherine L. Backman, PhD, OT(C), Diane Lacaille, MD, MHSc: University of British Columbia and Arthritis Research Centre of Canada, Vancouver, British Columbia, Canada; 2Judy Village, MSc, CPE: University of British Columbia, Vancouver, British Columbia, Canada. Ms Village has received consultant fees (more than $10,000) for developing the Ergonomic Assessment Tool for Arthritis. Address correspondence to Catherine L. Backman, PhD, OT(C), Department of Occupational Science & Occupational Therapy, The University of British Columbia, T325-2211 Wesbrook Mall, Vancouver, British Columbia, Canada V6T 2B5. E-mail: catherine.backman@ubc.ca. Submitted for publication February 2, 2008; accepted in revised form July 8, 2008.
ued at $7,454 per person per year (3). In patients with rheumatoid arthritis (RA), work disability occurs early in the course of the disease and continues at a steady rate (4,5). A review of work disability studies reported that the prevalence is approximately 10% in the rst year after diagnosis of RA, progressing to 50% or greater after 10 15 years, depending on the year and population studied (6). Prior to stopping work, individuals with arthritis report productivity losses such as working fewer hours, changing to less demanding jobs, or declining promotions (7). Efforts to reduce work and productivity losses have the potential to make important contributions to both individuals and society (8). Rehabilitation approaches aimed at preventing work loss or work disability may be preferred over return-towork strategies, based on the principle that it is easier to maintain employment than to reenter the employment market after a prolonged absence. Such approaches attempt to address the modiable risk factors associated with work disability. A job accommodation is dened as changes made to a job to better match the abilities of a worker. Ergonomic modications, which include physical changes to the work place and alternative methods for work tasks, are one type of job accommodation applicable to people with arthritis (4). Ergonomic assessment draws on multiple disciplinary 1495
1496 perspectives to examine the t between individuals and their work. When risks or problems are noted, ergonomic principles may be applied to redesign the work place, tools, equipment, or work methods to prevent and reduce work-related risks for injury and optimize work performance. Therefore, ergonomics is aimed at preventing work injury and work loss, and ergonomists contribute to work place health and safety in a range of industries. Ergonomic principles are also used by occupational therapists (OTs), physical therapists, and others working in arthritis rehabilitation when recommending joint protection techniques, assistive devices, and alternative methods to accomplish work, leisure, and self-care tasks (9), but formal ergonomic evaluations do not appear to be commonly used in arthritis care. Ergonomic modications may help people with inammatory arthritis (IA) to work more safely, efciently, and in ways that minimize arthritis symptoms and activity limitations. A systematic review of work place ergonomic interventions indicates positive effects on reducing musculoskeletal injuries, symptoms, and absence from work among workers in general (10). Logically, these principles should also improve work for people with arthritis, and indeed there is some evidence demonstrating that ergonomic modications are associated with remaining employed. In a study of predictors of work loss in patients with RA, people who received ergonomic modications were 2.5 times less likely to be work disabled (4). In another study of people with IA, all of whom were employed at the time of diagnosis, failing to adjust job demands or make changes to the work environment was associated with loss of employment (11). However, the use of ergonomic modications by people with IA is low, at 9% in one study (12), whereas we found only 20% reported access to an ergonomic assessment of their work (4). In our review of ergonomic assessment tools, we found little evidence that ergonomic assessments were offered to people with IA, and we could not nd a tool suited to the unique needs of people with arthritis (13). Most tools were designed to identify the risk for musculoskeletal injuries in the general population and did not account for symptoms associated with IA such as pain and fatigue, which may be exacerbated at lower thresholds of work than for healthy populations. Some tools were limited to assessing injury risk to a specic body part such as the upper extremities (14,15), designed for a specic industry such as automotive plants (16), or required work site observations (14 17). IA affects multiple joints among workers in different types of jobs, and some people with arthritis are reluctant to disclose their diagnosis to their employer (7,18). This suggests a need for a tool that considers IA symptoms, is applicable to different jobs, and can be used outside of the work place. As part of a program aimed at preventing work loss and maintaining work productivity among people with IA, we designed an assessment tool to identify ergonomic risk factors in the work place and generate potential solutions. It is a practical guide to assessment and intervention, not an outcome measure. This article describes tool development, content, and results from a pilot test using the tool as part of the Employment and Arthritis: Making it Work program (19).
Backman et al
MATERIALS AND METHODS
Development and pretesting of the ergonomic assessment tool. A review of published ergonomic assessment tools was conducted by an interdisciplinary team (rheumatology, ergonomics, occupational therapy) with experience in arthritis, work disability, work site evaluation, ergonomic risk assessment, and rehabilitation (13). Although none of the tools were appropriate for our purpose, some elements were applicable, including 1) a systems approach to considering risk factors that includes work station, equipment/tools, work environment, and work organization; 2) identication of tasks currently causing problems or exacerbating symptoms; 3) proactive identication of risk factors not yet causing problems but that may in the future; 4) use of a red, yellow, and green colorcoding system (20) to indicate levels of risk; and 5) use of diagrams and photographs to illustrate postures and risk factors when direct observation is not possible. Additionally, ndings from our prior focus-group study (18) provided the patient perspective, indicating that important considerations for ergonomic assessment include attention to arthritis symptoms, an assessment by a person knowledgeable about arthritis, and reluctance to disclose arthritis to employers. An iterative process was used to develop an ergonomic assessment tool involving client self-assessment at work and a semistructured interview by an OT. The rst draft (version 1) incorporated the desired content and program purpose outlined above, asking questions based on known risks for musculoskeletal injuries and factors likely to exacerbate IA symptoms. To enhance content validity, version 1 was reviewed by an independent panel of 4 experts, selected for their knowledge of ergonomics and work disability as judged by publications and professional experience. They evaluated the assessment process and content, responding to 13 questions about whether or not the tool would lead to a good understanding of the clients work tasks, identify risks, lead to ergonomic recommendations, and be applicable to a range of occupations. The tool was modied based on the panels expert opinion (version 2). Version 2 was pretested with 12 women and 1 man with IA by 3 different OTs (one practicing in an arthritis outpatient program, one providing ergonomic consultations in a rehabilitation center, and one academic/researcher). A professional ergonomist observed 2 assessments. The occupations in this pretest included administrative and management positions, school bus driver, ight attendant, laboratory technician, and dog groomer. Clients and OTs completed feedback forms designed to elicit information about ease of use, applicability, and thoroughness of the content, and this formative feedback inuenced ongoing revisions to the tool. Specically, after the rst 3 pretests, minor improvements were made to clarify format and instructions (version 3), and after 10 pretests, participants were given a disposable camera to take photographs in the work place to supplement the self-report (version 4). Because some people were reluctant to disclose arthritis to employers or coworkers, a work site visit was not planned, and the photographs helped overcome the lack of direct observation. Final revisions were made based on observa-
Development and Testing of an Ergonomic Assessment Tool
1497
Table 1. Content of the self-assessment and interview components of the Ergonomic Assessment Tool for Arthritis* Self-assessment 1. Work diary and work layout diagram/photographs Participant keeps diary for 1 work day, identifying main task during each half hour, noting equipment, tools, or materials used and any difculty or discomfort during the task. A sketch of the work station or general layout of main work space is completed at the end of the diary, and photographs are taken of the worker doing key tasks. Participant indicates if any of 6 statements describe their work; e.g., I control how fast or slow I do my work. A drawing is provided of a manikin seated with yes/no/sometimes questions about posture; e.g., feet supported? head upright and facing forward? 11 questions inquire about frequency of maintaining various postures, motions, and repetition, and any associated pain or discomfort. A drawing is provided of a manikin standing with yes/no/sometimes questions about posture; e.g., forearms horizontal? weight shared on both feet? 13 questions inquire about frequency of maintaining various postures, repetition, and tasks like operating foot pedals, walking, climbing stairs or ladders, and oor surface. 5 questions about hand use; e.g., Do you have to grip hard or squeeze with your hand? Do you manipulate small objects or do precise hand movements to use tools? Frequency and discomfort are noted for each. Occupational therapist interview guide/checklist A work task summary is documented, identifying the duration of main tasks. The sketch or photographs of the work station illustrating the physical environment are reviewed prior to beginning the semistructured interview.
2. Work organization
3. Seated work
4. Standing work (includes walking and kneeling)
5. Upper extremity work, gripping, grasping, and using hand tools
6. Lifting and carrying
2 questions address loads lifted close to the body and away from the body, including approximate weight of the load and associated discomfort, if any.
7. Pushing and pulling
3 questions about frequency of moving heavy loads (e.g., full 2-drawer ling cabinet), moderate loads (e.g., a full shopping cart), and small loads (e.g., a shopping cart with 10 small items).
12 items probe for details; e.g., Are there opportunities for rotation of tasks? Is training provided on how to adjust the work station? Are supervisors supportive? 10 items probe for details about the chair (e.g., adjustable armrests, lumbar support), workspace (e.g., adjustable work surface, placement of tools), and if applicable, 10 additional items address computer work (e.g., monitor height, keyboard type) 14 items probe for details about work space and tasks; e.g., Is the work surface height appropriate to the task? Is the work station designed to reduce or eliminate bending and twisting wrist, reaching above the shoulder or below the knee, reaching forward, working with elbows raised? Is the oor at and free of obstacles? 7 items describe hand movements (e.g., During gripping tasks is the force required judged acceptable? Can 2 hands be used?) If applicable, 10 items inquire about hand tools (e.g., Are tools powered where necessary and feasible? Is the tool weight evenly balanced and distributed?) Additional information on lifting, carrying, pushing, and pulling is combined with questions about frequency and load, up to 16 items, depending on the job; e.g., Is the lift, push, or pull task performed infrequently? For short/intermittent periods? Over short distances? Free from pressure of time or at a pace controlled by a machine? Is help available for heavy or awkward tasks? See component 6, lifting and carrying.
* Components 1 and 2 are common to all workers; components 3 to 7 are selected if relevant to the worker, based on the screening questions.
1498
Backman et al
Question Neck Do you have to bend or twist your neck?
Rarely or never
Up to 2 hours per day
2 hours or more per day
Any pain or problem? NO YES
Back Do you have to bend or twist your back?
Shoulder/arm (sitting) Do you work with your hands at or above your head? Shoulder/arm (standing) Do you work with your arms stretched out? Grip Do you have to grip hard or squeeze with your hand while lifting loads of 10 lbs. or more?
Figure 1. Sample items from the self-report component of the Ergonomic Assessment Tool for Arthritis. Clients check the appropriate column for each item in the self-assessment. Items checked in yellow and red zones are the focus of the subsequent consultation with the occupational therapist.
tions gathered throughout pretesting. Feedback from both clients and OTs indicated that the ergonomic assessment was acceptable regarding time and effort and relevant in terms of guiding a thorough review of work tasks. The Ergonomic Assessment Tool for Arthritis. The nal version, the Ergonomic Assessment Tool for Arthritis (EATA; available online at www.arthritisresearch.ca), has 4 components. The rst component is screening to match the assessment form to the persons job. The EATA is individualized to each client by selecting only the relevant job demand sections of the form, based on responses to 5 screening questions: Does your work involve (a) prolonged sitting? (b) prolonged standing, kneeling, walking, or stair climbing? (c) gripping or grasping objects or hand tools? (d) frequent lifting or carrying? (e) pushing or pulling items (e.g., carts or dollies)? Self-assessment was completed by the client prior to the consultation visit (see Table 1 for content overview and Figure 1 for sample items and layout). Responses to the job demand questions in the self-assessment are color coded, indicating incremental levels of risk. Items checked in the yellow and red zones assist the OT to focus on the most pertinent issues during the interview, probing for more detail to understand the potential risk and make appropriate recommendations. The yellow and red levels of risk are based on risk factors for musculoskeletal injuries, such as
prolonged static postures or repetitive motions, where increased duration is associated with increased risk. Regardless of level of exposure, if the worker experiences pain or problems, this is coded red to trigger further evaluation (Figure 1), because people with IA may aggravate their symptoms even at low levels of risk. An interview guide/checklist was completed by the OT during the visit. The self-report and interview guide are parallel forms that begin with a description of work tasks and then assess up to 6 areas of job demands, from work organization to pushing and pulling, with the interview guide going into greater depth (Table 1). During the interview, the client and the OT collaboratively complete a job task summary, identify and prioritize issues, and generate recommendations, leading to the fourth component, the solutions summary page. Issues, recommendations, and resources for implementation (e.g., where to buy specic equipment, identifying human resources or occupational safety personnel who can help) are documented on a solutions summary page given to the client. Pilot testing of the EATA. The Making it Work program (19,21), aimed at preventing work loss and maintaining at-work productivity, is a series of 5 group sessions and 2 individual consultations, 1 with a vocational rehabilitation counselor and 1 with an OT for the ergonomic assessment described here. One group session introduces partic-
Development and Testing of an Ergonomic Assessment Tool ipants to general ergonomic principles, suggestions for job modications, and communicating with employers to implement modications. The full program is described elsewhere (21), and the present article is limited to the ergonomic assessment/intervention. Eligible participants consisted of employed adults with IA (RA, psoriatic arthritis, lupus), uent in English, and ages 18 60 years. A research assistant asked the screening questions and provided applicable sections of the EATA self-assessment form and camera when booking the participants OT appointment. All ergonomic consultations were conducted by the same OT, experienced in arthritis and trained in ergonomic principles by means of a 2-hour self-study module on CD, developed by a certied ergonomist (JV). The OT phoned participants 1 month later to review progress toward implementing recommendations, provide clarication, and if necessary, discuss ways to overcome barriers to implementation or suggest alternative recommendations. When changes had been made, participants were asked about their effect, and if they were ineffective, trouble shooting was offered. Data on usefulness of the ergonomic assessment and implementation of recommendations were collected by a study coordinator conducting telephone interviews at 3, 6, and 12 months. Questions included How useful for you was the ergonomic assessment by the OT? and if ergonomic changes had been made, How useful were the changes? (measured on a 5-point response scale, where 1 very useful and 5 not at all useful). Ethical approval for the project was obtained from the Research Ethics Board of the University of British Columbia, and all participants gave informed consent.
1499
Table 2. Participant characteristics* Characteristic Age, years Diagnosis, no. (%) Rheumatoid arthritis Systemic lupus erythematosus Psoriatic arthritis Disease duration, years HAQ disability index Marital status, no. (%) Single Married or living with a partner Divorced Education, no. (%) High school diploma Technical/trade/vocational college Some university University degree Graduate or postgraduate training Years employed Years in present job Hours of work per week Type of work, no. (%) Administrative/clerical Health sector occupations Education and child care Other# Value 51 7.1 17 (89) 1 (5) 1 (5) 12 11.7 0.41 0.37 2 (11) 15 (79) 2 (11) 4 (21) 5 (26) 3 (16) 4 (21) 3 (16) 28 8 12 11 34 8.6 9 (47) 4 (21) 2 (11) 4 (21)
* Values are the mean SD unless otherwise indicated. HAQ Health Assessment Questionnaire. Range 0 3, where 3 worse. Receptionist, administrative assistant, events coordinator, manager. Laboratory technician, home health case manager. Elementary school teacher, nanny. # Library assistant, fabric artist, building caretaker, buyer.
RESULTS
Nineteen women met eligibility criteria and participated in the proof-of-concept study of the Making it Work program. All participants completed the ergonomic assessment and 1-month telephone call to discuss ergonomic modications. Participant characteristics are shown in Table 2. Participants reported that the ergonomics content of the Making it Work program prepared them for their consultation with the OT (35% stated very well prepared, 41% well prepared, and 24% somewhat prepared). The assessment forms were individualized based on job demands; none of the participants had jobs that required completion of all 5 sections, but all sections were applicable to at least 7 participants (Table 3). Table 4 shows results from implementation of the EATA. Time required to complete the self-assessment and consultation visit varied depending on the complexity of the job and problems reported. The OT made 87 recommendations relating to either work techniques or modications to the physical environment and equipment purchase (Table 4). The most frequent recommendations related to supporting a well-aligned posture when seated, such as obtaining an adjustable chair, changing the height of the computer monitor and/or keyboard, or using a footstool. Five recommendations were for future planning (designing a new work station to
be integrated into upcoming renovations or requesting easier-to-use equipment in the course of routine replacement of capital equipment). The assessment process triggered 14 non-ergonomic recommendations for problems affecting performance of work tasks, and appropriate referrals were made to address the problems, such as obtaining hand splints, foot orthoses, supportive shoes, or eye examination. Implementation of ergonomic recommendations took time (Table 3), and by 12 months, 85% of recommendations had been implemented by 14 (73%) participants. Five participants did not complete any changes. An additional 9% of recommendations were still in progress; that is, equipment had been ordered or accommodations requested from the employer, but had not yet been implemented. Participants reported an additional 10 self-initiated changes, implemented as they became more aware of ergonomics and how to problem solve on their own. Onethird of the changes involved making a request of the employer; i.e., supervisors, human resources, or occupational health and safety. Participants stated that they were experiencing less pain and stiffness, had more energy, less stress, or felt better at work. When asked what was helpful about the ergonomic intervention, comments pertained to easing of symptoms or difculty with tasks, and when recommendations were
1500
Backman et al
Table 3. Summary of ergonomic factors identied in job demands sections of the self-report and interview components of the Ergonomic Assessment Tool for Arthritis (EATA) EATA job demands section Work organization Seated work Participants completing section 19 18 Participants with issues/risks 9 15 Solutions proposed 10 34 Sample issue and proposed solution Meetings impinging on lunch breaks: set priorities, negotiate rescheduling Nonadjustable, ill-tting ofce chair: purchase chair with adjustable seat, back, and armrests Nonadjustable work surface: build or install adjustable height table Difculty using regular scissors: purchase spring-loaded scissors Books, les too heavy to carry: obtain a trolley No risks identied because loads were small, infrequent, and appropriate equipment was already in place.
Standing work Gripping and grasping Lifting and carrying Pushing and pulling
13 12 7 7
8 10 5 0
19 19 5 0
not implemented, it was generally due to a lengthy process for planning substantive changes or because the job demands had changed (Table 5). Asked if they would be willing to have the OT make a work site visit as part of the assessment, 33% said no.
DISCUSSION
We developed an ergonomic assessment tool for the purpose of recommending necessary ergonomic modications as job accommodations for people with IA. Our pilot study demonstrated that the use of the EATA by an OT with arthritis experience is feasible, guides a comprehensive ergonomic assessment, and elicits solutions to reduce er-
gonomic risk factors. The EATA was sufciently exible to assess different occupations, with job demands ranging from seated ofce work to more physically demanding lifting and carrying. In this pilot test of 19 women with IA, it was applicable to administrative, health care, education, and 4 other occupations (library assistant, building caretaker, fabric artist, and buyer). The individualized approach based on 5 screening questions to select only the relevant sections of the form helped minimize response burden to both the person with IA and the OT. The cautionary yellow and red response codes in the self-assessment identied areas for further evaluation by the OT. Used in the context of a multifaceted program to prevent work loss in IA, the EATA led to recommendations for
Table 4. Results from implementation of ergonomic assessment using the Ergonomic Assessment Tool for Arthritis* Implementation factor Time to complete self-assessment, mean (range) minutes Time to complete interview, mean (range) minutes Ergonomic solutions recommended per participant, mean (range) Ergonomic solutions related to technique/work methods (n 87 total recommendations) Ergonomic solutions related to physical environment or equipment (n 87 total recommendations) Ergonomic recommendations implemented (cumulative totals) 3 months 6 months 12 months Participants who implemented 1 recommendation by 12 months (n 19 participants) Participants who reported the ergonomic assessment was useful (n 18 participants answering this question at 12 months) Very useful Useful Somewhat useful Result 29 (1045) 60 (4595) 4.5 (19) 48 (55) 39 (45)
60 (69) 66 (76) 74 (85) 14 (74)
7 (39) 6 (33) 5 (28)
* Values are the number (percentage) unless otherwise indicated. Work diary, work station drawings and/or photographs, and relevant job demand sections. Consultation time with the occupational therapist, including interview to identify issues and risks requiring attention and explanation of recommendations.
Development and Testing of an Ergonomic Assessment Tool
1501
Table 5. Sample participant comments on usefulness of ergonomic modications and reasons for not implementing recommendations Usefulness of ergonomic modications Removing my armrests allowed my chair to be closer to my deskposture is important and self-awareness of posture is difcult. I didnt know I was poking my head forward. Instead of stooping or squatting to work with children, I have a wheeled stool I can sit on and a slanted desktop to use. If I do things a little differently I experience less pain. I pace myself and think about my actions more. Headphones have eased my fatigue. Higher surface makes it easier on back and shoulders to work. Reasons for delays or not implementing ergonomic recommendations My boss said that instead of ordering a new desk that I should move to another area to work where there are ergonomic desks available. However, I didnt want to do that because it means losing my ofce. One year later, I moved. After accomplishing some of the occupational therapy suggestions, I now have a new job where the suggestions no longer apply. Done all I can with the current work setup, the rest can wait because a new library is being built. I was asked specically what I needed: counters on 2 different levels, laminators with hoods, computer placed so I can sit or stand.
ergonomic changes for all participants, and 73% of participants had implemented at least 1 change at 1 year of followup. It was observed that it takes time, and in some cases persistence, to complete ergonomic changes, emphasizing the importance of sufcient support and followup to evaluate the effectiveness of ergonomic interventions at work. This is consistent with evaluations of participatory ergonomics programs in the general work force, which found that a similar proportion of recommendations were implemented (22,23) and noted a need for supervisory support (24,25) to make work place modications. The EATA was designed to be a practical assessment in a typical clinical setting with access to an OT. To be completed in a single visit, however, it requires additional steps prior to the OT encounter: 5 screening questions determine which sections of the self-assessment form the client should complete, instructions need to be provided for the work diary and for taking photographs of the work station, the self-assessment must be sent, and a single-use camera must be provided for those who do not have one available. In this study, participants also had a group session on ergonomics as part of the overall Making it Work program. One advantage is that the client is actively involved in preparing for the consultation by completing the self-assessment component, and this may enhance the evaluation by encouraging the client to observe their work and engage in a collaborative problem-solving process leading to practical solutions. In our pilot test, a 1-month followup phone call to discuss recommendations and encourage changes supplemented the in-person consultation. Keeping in mind the relatively lengthy time required to implement job accommodations, a plan for followup visits or phone calls is advisable. A strength of the EATA is that it aims to identify potential risks associated with work tasks or the environment before they cause pain or aggravate IA, as well as identifying the motions, positions, or tasks that are already associated with pain or fatigue. The tool helps the client and the OT focus on basic ergonomic risk factors and elicits options for resolving problems encountered at work. Some participants reported considerable support from their employers and coworkers, and noted that suggestions they brought to the work place resolved a general ergonomic
concern for all employees. However, like ergonomics programs in general (22,23), not all recommendations were implemented, and future research might more fully explore why suggestions were not viewed as helpful or necessary. The approach described here relies on self-report rather than observation at the work site. It has been reported elsewhere that workers may be poor judges of the magnitude of their exposure to risks (26). Lack of direct observation by a skilled evaluator and relying on a report of current difculties at work may miss detecting risk factors in the job that are not obvious to the client but may present difculties in the future (13). On-site work visits would also enable the OT to communicate directly with employers and encourage support for changes. Two-thirds of the present sample was willing to consider an on-site ergonomic assessment, but one-third did not want to disclose their arthritis to employers or coworkers, and would decline an on-site visit. Given the time (and therefore cost) to conduct, some OT practices may not nd work site visits feasible for all clients. Therefore, there is a place for a tool like the EATA to facilitate an ergonomic consultation for all people with IA. When indicated and agreeable to both parties, the EATA can be augmented with a work site visit. Just over half of the recommended solutions for ergonomic risk factors were simple, technique-based solutions that centered on the person making changes to the way they did things, rather than engineering solutions to modify the work place. This solution preference may reect the training and experience of OTs compared with ergonomists, but because only 1 OT was involved in the present evaluation, this is speculation. It may also be related to the type of jobs assessed. Engineering-based ergonomic modications may improve the work site for all workers, a perspective that is sometimes lost when clients and health professionals focus on managing illness symptoms. The use of the color-coded levels of risk in the selfassessment is based on the guide for preventing musculoskeletal injuries by the Swedish National Board of Occupational Safety and Health (20). Cutoffs in the Swedish guide are based on scientic evidence of increased risk of musculoskeletal injuries in otherwise healthy workers. To overcome the lack of available cutoffs for people with IA,
1502 we included a column in the EATA to indicate pain or aggravation of symptoms. Future research is needed to examine the thresholds for risk factors for vulnerable populations, including IA, because current occupational health and safety guidelines are based on the repetition, reach, force, and loads that precipitate injury in the general population. Pathologic changes such as joint instability, muscle weakness, and systemic fatigue suggest that people with arthritis are prone to exacerbations of injury at much lower levels. This pilot test had its limitations. Only women participated, so the acceptability and applicability of the tool to men with IA is unknown. A limited number of occupations were assessed, although there was a reasonable sampling of different types of work. The most physically demanding occupation among this sample was that of building caretaker. The EATA needs to be tested with other occupations, especially those with more physical demands such as pushing and pulling, because no problems were identied in this area during the pilot test. The tool is best used by OTs who have prior experience or training in both arthritis care and ergonomics, which means that some users may need to participate in continuing education to update their skills in one or both areas before using this kind of assessment. A background in arthritis care helps the assessor to probe during the interview to elicit information about the uctuating nature of symptoms or problems experienced at work and to frame recommendations in the context of managing this chronic illness. Our pilot testing of the tool did not include an assessment of intrarater or interrater reliability. However, 5 subjects participated in both the pretesting of the EATA and the proof-of-concept study, and therefore had the tool administered twice. In 3 clients, no changes were implemented in the interim period and the assessment led to the identication of the same issues and recommendations. In 2 cases, recommendations had been implemented and new issues were identied. Reliability should be evaluated in further studies. Previous research shows that more than one-third of people with RA report limitations in their work as a result of their arthritis (27), and more than one-quarter will leave work prematurely within 10 years of diagnosis (4). Ergonomic assessments and interventions are one approach that can be used by rehabilitation practitioners to facilitate job accommodations aimed at preventing work loss and maintaining at-work productivity. The ergonomic tool introduced here adds to the repertoire of rehabilitation tools and services for people living and working with arthritis. Given the cost of work loss or reduced productivity at work, the time spent assessing and implementing ergonomic recommendations is relatively minimal, and may make an important contribution to reducing work disability. The EATA is specically designed for people with IA, can be used without a work site visit, is completed in a single consultation (with advance planning for self-assessment), and fosters collaboration between clients and OTs in identifying ergonomic risks and solutions aimed at enhancing work performance.
Backman et al
ACKNOWLEDGMENTS
The authors thank Cheryl Shefeld, OT and Gillian Palejko, OT, for testing the ergonomic assessment tool, Cory Anderson for taking photographs and assisting in the design of the rst draft of the EATA, and Pam Rogers for coordinating the pilot test. AUTHOR CONTRIBUTIONS
Dr. Backman had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study design. Backman, Village, Lacaille. Acquisition of data. Backman, Village, Lacaille. Analysis and interpretation of data. Backman, Village, Lacaille. Manuscript preparation. Backman, Village, Lacaille. Statistical analysis. Backman.
REFERENCES
1. Theis KA, Murphy L, Hootman JM, Helmick CG, Yelin E. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18 64: 2002 National Health Interview Survey data. Arthritis Rheum 2007; 57:355 63. 2. Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Pain exacerbation as a major source of lost productive time in US workers with arthritis. Arthritis Rheum 2005;53: 673 81. 3. Muchmore L, Lynch WD, Gardner HH, Williamson T, Burke T. Prevalence of arthritis and associated joint disorders in an employed population and the associated healthcare, sick leave, disability, and workers compensation benets cost and productivity loss for employers. J Occup Environ Med 2003; 45:269 78. 4. Lacaille D, Sheps S, Spinelli JJ, Chalmers A, Esdaile JM. Identication of modiable work-related factors that inuence the risk of work disability in rheumatoid arthritis. Arthritis Rheum 2004;51:84352. 5. Backman CL. Employment and work disability in rheumatoid arthritis. Curr Opin Rheumatol 2004;16:148 52. 6. Verstappen SM, Bijlsma JW, Verkleij H, Buskens E, Blaauw AA, ter Borg EJ, et al, on behalf of the Utrecht Rheumatoid Arthritis Cohort Study Group. Overview of work disability in rheumatoid arthritis patients as observed in cross-sectional and longitudinal surveys [review]. Arthritis Rheum 2004;51: 488 97. 7. Gignac MA, Badley EM, Lacaille D, Cott CC, Adam P, Anis AH. Managing arthritis and employment: making arthritisrelated work changes as a means of adaptation. Arthritis Rheum 2004;51:909 16. 8. Allaire SH. What work changes do people with arthritis make to preserve employment, and are such changes effective? [editorial]. Arthritis Rheum 2004;51:8713. 9. Backman CL, Fairleigh A, Kuchta G. Occupational therapy. In: St Clair EW, Pisetsky D, Hayes BF, editors. RA: rheumatoid arthritis. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 4319. 10. Rivilis I, Van Eerd D, Cullen K, Cole DC, Irvin E, Tyson J, et al. Effectiveness of participatory ergonomic interventions on health outcomes: a systematic review. Appl Ergon 2008;39: 34258. 11. Chorus AM, Miedema HS, Wevers CW, van der Linden S. Work factors and behavioural coping in relation to withdrawal from the labour force in patients with rheumatoid arthritis. Ann Rheum Dis 2001;60:102532. 12. Mancuso CA, Paget SA, Charlson ME. Adaptations made by rheumatoid arthritis patients to continue working: a pilot study of workplace challenges and successful adaptations. Arthritis Care Res 2000;13:89 99. 13. Village J, Backman CL, Lacaille D. Evaluation of selected
Development and Testing of an Ergonomic Assessment Tool
ergonomic assessment tools for use in providing job accommodation for people with inammatory arthritis. Work. In press. McAtamney L, Nigel Corlett E. RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon 1993;24:919. Moore JS, Garg A. The Strain Index: a proposed method to analyze jobs for risk of distal upper extremity disorders. Am Ind Hyg Assoc J 1995;56:44358. Keyserling WM, Stetson DS, Silverstein BA, Brouwer ML. A checklist for evaluating ergonomic risk factors associated with upper extremity cumulative trauma disorders. Ergonomics 1993;36:80731. Hignett S, McAtamney L. Rapid entire body assessment (REBA). Ergonomics 2000;31:2015. Lacaille D, White MA, Backman CL, Gignac MA. Problems faced at work due to inammatory arthritis: new insights gained from understanding patients perspective. Arthritis Rheum 2007;57:1269 79. Lacaille D, White M, Rogers P, Gignac M, Backman C, Esdaile J. Employment and arthritis: making it work. Results of pilot testing [abstract]. Arthritis Rheum 2006;54 Suppl 9:S782. Swedish National Board of Occupational Safety and Health. Ergonomics for the prevention of musculoskeletal disorders.
1503
Solna (Sweden): Statute Book of the Swedish National Board of Occupational Safety and Health (AFS); 1998. Lacaille D, White MA, Rogers P, Gignac MA, Backman CL, Esdaile JM. Employment and arthritis: making it work. A proof of concept study. Arthritis Rheum. In press. De Looze MP, Urlings IJ, Vink P, van Rhijn JW, Miedema MC, Bronkhorst RE, et al. Towards successful physical stress reducing products: an evaluation of seven cases. Appl Ergon 2001;32:52534. St-Vincent M, Kuorinka I, Chicoine D, Beaugrand S, Fernandez J. Assimilation and use of ergonomic knowledge by nonergonomists to improve jobs in two electrical product assembly plants. Hum Factors Ergon Manuf 1997;7:33750. Haims MC, Carayon P. Theory and practice for the implementation of in-house, continuous improvement participatory ergonomic programs. Appl Ergon 1998;29:46172. Wilson JR, Haines HM. Participatory ergonomics. In: Salvendy G, editor. Handbook of human factors and ergonomics. 2nd ed. New York: Wiley; 1997. p. 490 513. Wells S, Norman R, Neumann P, Andrew D, Frank J, Shannon H, et al. Assessment of physical work load in epidemiologic studies: common measurement metrics for exposure. Ergonomics 1997;40:51 62. Backman CL, Kennedy SM, Chalmers A, Singer J. Participation in paid and unpaid work by adults with rheumatoid arthritis. J Rheumatol 2004;31:4757.
21. 22.
14.
15.
16.
23.
17. 18.
24. 25. 26.
19.
27.
20.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Classroom Strategies PosturepositioningDocument1 pageClassroom Strategies PosturepositioningShanthoshini BaskaranPas encore d'évaluation
- Sample (Your Lea/Program Name Here) : Classroom Strategies & Interventions Personal Care and Organizing MaterialsDocument1 pageSample (Your Lea/Program Name Here) : Classroom Strategies & Interventions Personal Care and Organizing Materialscorina_maria_enePas encore d'évaluation
- Classroom Strategies Work BehaviorsDocument1 pageClassroom Strategies Work BehaviorsShanthoshini BaskaranPas encore d'évaluation
- Assessment Telepractice: Table of ContentsDocument2 pagesAssessment Telepractice: Table of ContentsShanthoshini BaskaranPas encore d'évaluation
- Santho Related LiteratrueDocument18 pagesSantho Related LiteratrueShanthoshini BaskaranPas encore d'évaluation
- Wheelchairs: Types of CushionsDocument3 pagesWheelchairs: Types of CushionsShanthoshini BaskaranPas encore d'évaluation
- Transforming Caseload To Workload in School-Based and Early Intervention Occupational Therapy ServicesDocument4 pagesTransforming Caseload To Workload in School-Based and Early Intervention Occupational Therapy ServicesShanthoshini BaskaranPas encore d'évaluation
- PDD Central Sensory Integration DysfunctionDocument26 pagesPDD Central Sensory Integration DysfunctionShanthoshini BaskaranPas encore d'évaluation
- ValvularDocument31 pagesValvularShanthoshini BaskaranPas encore d'évaluation
- Mot SyllabusDocument30 pagesMot SyllabusShanthoshini Baskaran100% (1)
- BookDocument3 pagesBookShanthoshini BaskaranPas encore d'évaluation
- BookDocument3 pagesBookShanthoshini BaskaranPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Essay For AdmissionDocument1 pageEssay For AdmissionValerii EssayPas encore d'évaluation
- Shafiaur CVDocument2 pagesShafiaur CVapi-420514927Pas encore d'évaluation
- Letter of Intent HEtEHE gRAHAMDocument3 pagesLetter of Intent HEtEHE gRAHAMDan FredPas encore d'évaluation
- Catechetics NotesDocument22 pagesCatechetics NotesDaniel Coveyou IIPas encore d'évaluation
- Letter of Reference Ycf 2018Document2 pagesLetter of Reference Ycf 2018Richa ShahiPas encore d'évaluation
- What Not To Put in A Literature ReviewDocument6 pagesWhat Not To Put in A Literature Revieweubvhsvkg100% (1)
- Names: Bongomin Racheal.: Page 1 of 4Document4 pagesNames: Bongomin Racheal.: Page 1 of 4racheal atimPas encore d'évaluation
- Verbal Reasoning ExamplesDocument12 pagesVerbal Reasoning ExamplesTwins Ekop100% (2)
- ĐỀ THAM KHẢO SỐ 1Document6 pagesĐỀ THAM KHẢO SỐ 1Lê Hồng LoanPas encore d'évaluation
- 11 Reasons Why Quo Warranto Decision On Sereno Was CorrectDocument3 pages11 Reasons Why Quo Warranto Decision On Sereno Was CorrectMelvin PernezPas encore d'évaluation
- Action Research Work Plan and TimelinessDocument3 pagesAction Research Work Plan and TimelinessAntonio Ganub86% (7)
- Caritas in Veritate: A Reflection PaperDocument2 pagesCaritas in Veritate: A Reflection PaperMarbert PinquePas encore d'évaluation
- EEE610 Presentation Chapter 4Document31 pagesEEE610 Presentation Chapter 4FIK ZXSPas encore d'évaluation
- School Facilities and Observation ChecklistDocument5 pagesSchool Facilities and Observation ChecklistMhadellaine JunatasPas encore d'évaluation
- 3 New Literacies, 21st Century SkillsDocument66 pages3 New Literacies, 21st Century Skillsirene apiladaPas encore d'évaluation
- Ascension 2014 01Document14 pagesAscension 2014 01José SmitPas encore d'évaluation
- SCC E Class Record Template Updated May27 2021Document67 pagesSCC E Class Record Template Updated May27 2021Christopher Jorge BarredoPas encore d'évaluation
- STADIO Flyer BPP FULLDocument2 pagesSTADIO Flyer BPP FULLBoogy GrimPas encore d'évaluation
- Approved Secure English Language Test CentresDocument1 pageApproved Secure English Language Test CentresFranck Duprey MvogoPas encore d'évaluation
- ARRANGED HEALTH - PEACE.VALUES Catch Up FridaysDocument44 pagesARRANGED HEALTH - PEACE.VALUES Catch Up FridaysVegilla Sinlao Ann Jeeh100% (1)
- Eappgrade12 q4 Week4 v4Document17 pagesEappgrade12 q4 Week4 v4GLEZIEL-AN PIOCPas encore d'évaluation
- Questions For Students 1-6Document3 pagesQuestions For Students 1-6Wu RyanPas encore d'évaluation
- RPT 2022 Bahasa Inggeris Tahun 2 CEFR SumberpendidikanDocument35 pagesRPT 2022 Bahasa Inggeris Tahun 2 CEFR SumberpendidikanNG SIAW MOI MoePas encore d'évaluation
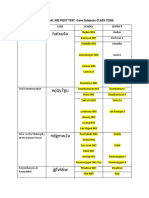
- SHS CORE DIAL ME POST TEST CLASS CODEDocument2 pagesSHS CORE DIAL ME POST TEST CLASS CODEEmmanuel Paul JimeneaPas encore d'évaluation
- College Tuition Cost Research PaperDocument8 pagesCollege Tuition Cost Research Paperhjuzvzwgf100% (1)
- Solution Manual For Staffing Organizations 7th Edition by HenemanDocument35 pagesSolution Manual For Staffing Organizations 7th Edition by Henemanasiatic.arterym39s6100% (46)
- Math 10-Q1-M9Document14 pagesMath 10-Q1-M9Ainee Grace DolletePas encore d'évaluation
- Individuals and Societies - MYP 4 and 5 - Dailey, Farmer, Giles and Woodburn - Hodder 2020Document327 pagesIndividuals and Societies - MYP 4 and 5 - Dailey, Farmer, Giles and Woodburn - Hodder 2020AydanPas encore d'évaluation
- The Technological Institute of Textile & SciencesDocument4 pagesThe Technological Institute of Textile & SciencesaniruddhaPas encore d'évaluation
- Kyle Dunford: Highlights of QualificationsDocument1 pageKyle Dunford: Highlights of Qualificationsapi-272662230Pas encore d'évaluation