Académique Documents
Professionnel Documents
Culture Documents
The Effect of Aqueous Leave Extract of Nicotiana Tabacum (Tobacco) On
Transféré par
Alexander DeckerCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
The Effect of Aqueous Leave Extract of Nicotiana Tabacum (Tobacco) On
Transféré par
Alexander DeckerDroits d'auteur :
Formats disponibles
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.
5, 2013
www.iiste.org
The Effect of Aqueous Leave Extract of Nicotiana Tabacum (Tobacco) On Some Reproductive Parameters and Micro-Anatomical Architecture Of The Testis In Male Albino Wistar Rats
Ibraheem M. Gambo 1* Nanyak Z. Galam1, Glory Adamu1 , Ayaka louis O1, , Ali A. Habeeb2 , Mohammed M. Bello3 , Najimuddeen Bello4 , Ahmed M. Rabiu1, Samuel O. Odeh1 1 Department of human physiology, university of Jos 2 Department of human physiology, university of Maiduguri 3 Department of anatomy, university of Jos 4 Department of science laboratory technology, university of Jos. *Corresponding aurthor: ibrobabs@yahoo.com ABSTRACT The tobacco plant (Nicotiana tabacum) has been in used for several years irrespective of the location of human races. Tobacco is used in different ways but cigarettes constitute the largest share of manufactured tobacco products in the world, accounting for 96% of total sales. The present study was undertaken to investigate the effect of aqueous extract of Nicotiana tabacum leaves on some reproductive parameters. 20 male young wistar rats weighing between 160 to 190g were used for the study. The extract was administered orogastrically in doses of 30, 20 and 10mg/kg body weight per day in 0.5ml of distilled water for 21 days and the control group was given equal volume of distilled water as well. The results showed that at the dose of 20 and 30mg/kg the extract decreased significantly the percentage motility (P<0.01) and (P<0.001) to 21.81.0 and 15.60.8 respectively, while the sperm concentration was significantly decreased (P<0.01) to 55.7x 1062038480 at the dose of 30mg/kg. The testicular histology showed decrease spermatogonic cells at doses of 20mg/kg and 30mg/kg respectively. It is concluded that nicotine could adversely affect fertility by sperm count, motility and testicular spermatogenesis in a dose- and time-dependent manner. Keywords Nicotiana tabacum, reproductive parameters, testicular histology Background Cigarette smoking is a widely recognized health hazard, yet despite worldwide antismoking campaigns, some people continue to consume cigarettes on a regular basis, and the highest prevalence of smoking is observed in young adult males during their reproductive period (Langgassner, 1999). A consistent number of studies have claimed that cigarette smoking is correlated with alterations in sperm quality such as semen volume, sperm concentration, motility, and morphology (Vine et al, 1994; Zavos et al, 1998a,b; Ozgur et al, 2005; Guo et al, 2006; Pasqualotto et al, 2006, 2008; Ramlau-Hansen, 2007a), concomitant with a reduced concentration mainly of citrate and also of fructose (Kunzle et al, 2003). The effects of any drug (including tobacco) vary from person to person. How tobacco affects a person depends on many things including their size, weight and health, also whether the person is used to taking it. The effects of tobacco, as with any drug, also depend on the amount taken (Collins & Lapsley, 2008). Male reproductive toxicity includes altered sperm parameters, such as lower density, decreased motility or abnormal morphology, and effects on fertility. Infertility is common among couples of child bearing age. Approximately half of known causes of primary infertility are attributable to male factor (Yales et al, 1989 and Yeilli et al, 2005). However the etiology of male factors infertility is poorly understood. While some individuals may be genetically predisposed to be sub-fertile (Reijo et al, 1996), there are major epigenetic factors which are implicated as potential causes of male infertility. The male reproductive system is known to be highly sensitive to many chemicals and drugs which have been found to pose adverse effects on male reproductive capacity under certain conditions ( Bonde et al, 1996). The health consequences of cigarette smoking and the use of tobacco products are well known. These are an important cause of increased mortality and morbidity in the developed countries and the prevalence is increasing in the developing world as well (Kapoor et al, 2005). There are more than 4000 chemicals in tobacco smoke. Many of these chemicals are poisonous and at least 43 of them are carcinogenic (cause cancer). The three major chemicals in tobacco smoke are: Nicotinethe chemical on which smokers become dependent. Tarwhich is released when a cigarette burns. Carbon monoxide (CO)a colourless, odourless and very toxic gas. Smokers typically have high levels of CO in the blood. Many plants contain nicotine, a powerful neurotoxin to insects. However, tobaccos contain a higher concentration of nicotine than most other plants. Smoking tobacco in cigars and pipes is less popular. When
137
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
tobacco is smoked, nicotine is absorbed through the membranes of the mouth and upper respiratory tract. When tobacco is chewed (as chewing tobacco or wet snuff), the nicotine is absorbed through the membranes in the mouth. It can also be sniffed (dry snuff) and the nicotine is then absorbed through the lining of the nose. Cigarette smoking is not only a potent cause of lung cancer but also has been associated with low birth weight, preterm delivery and abortion in women who are addicted to it. It also causes menstrual irregularities, pregnancy complications, and decreased fertility in women (Weisberg et al, 1985) Moreover, cigarette smoking inhibits spermatogenesis and causes decreased steroidogenesis in men (Aydos et al, 2001, Mlynarcikova et al, 2005). Cigarette smoking has also been shown to have anti-estrogenic effects in women (Tank et al, 2004). In males, the effects of smoking on androgen is important, given the recent interest in the association between low androgen levels, the metabolic syndrome and coronary heart disease (Jones et al, 2003). Other adverse effects of smoking include premature ejaculation and reduced penile erection; however, these depend on individual sensitivity or susceptibility (Jones et al, 2003). It has been previously demonstrated that exposure to reference cigarette smoke resulted in reduced birth weight in rats under experimental condition (Carmines et al, 2003 , Gaworski et al, 2004 ) while oral administration of nicotine have been associated with testicular degeneration, disorganization of the cytoarchitecture and decreased serum testosterone levels (Oyeyipo et al, 2010). In addition, nicotine has been shown to have adverse effects on fertility potentials of female albino rats by reducing the weight and disorganizing the histology of some vital visceral and reproductive organs (Iranloye et al, 2009). In spite of the growing knowledge on the adverse reproductive effects of smoking, it is relatively unclear whether or not, nicotine has the same effects on male reproductive activities as it relates to its effects on sperm cells and male fertility indices. It has been suggested that cigarette smoking increases the percentage of morphologically altered spermatozoa (Evans et al, 1981; Elshal et al, 2008), especially in men who are heavy smokers or who have smoked for many years (Gaur et al, 2007); however, the extent and the localization of the morphological damage is still being debated (Mak et al, 2000; Guo et al, 2006). The present study was, therefore, designed to investigate or evaluate the aqueous extract of leave of Nicotiana tabacum (TOBACCO) for possible toxicological effect on some reproductive parameters in male albino wistar rats. And to determine if it has any effect on the micro-anatomical architecture of the testis Methods 100grams of the plant material was extract by maceration in 1000ml of distilled water with intermittent agitation (8hrs day) for 3days using mechanical shake. Afterwards the mixture was filtered using filter paper (whatman) and the filtrate concentrate by rotary evaporation to dryness and yield 23.5g (23.5) of solid residue was obtained. The residue in form of pest dark brown product was transferred to an airtight bottle and stored in the refrigerator at -4C until use. The concentration of the extract was determined using this formula Weight of leaves(g) Concentration = Quantity of water (ml)
And the actual dose to be administered was obtained using this formula:
Dosage (mg)/ Body weight (kg) Dose (ml) = Concentration (mg/ml)
CHEMICALS AND REAGENT Stock solution of crude extract Formalin (BDH chemical, England) Distilled water Xylene Normal saline (0.9g of sodium chloride to 100ml of D.1 HO) Twenty sexually active male albino rats (Wister strains) weighing between 110g-160g obtained from animal house , university of jos, Nigeria were used for this study. The rats were kept in the animal house for the period of study. The rats were fed ad libitum with commercially prepared rat feeds made up of 2l% protein 3, .5%f at, 6 % fiber, 0.8% phosphorus (Top Feeds Limited, Jos, Nigeria) and given fresh water. They were kept in cages which have wood shaven as bedding and cleaned twice a week. The feeds and water was provided ad libitum in earthen troughs. Their cages were used and each measured about 19 by 12 inches. To be able to monitor, observe and record their individual weight daily. The rats were in groups of five (N= 5) in each cage marked A, B, C and
138
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
D respectively under the same environmental and management conditions. The experiment was conducted in accordance with the Guidelines of the U.S. National Institute of Health (NIH) on the care and use of laboratory animals. After 3 weeks of stabilization the rats in groups B, C and D were given aqueous extract of Nicotiana tabacum leaf at 10 mg/kg, 20mg/kg body weight and 30mg/kg'' body weight respectively for a period of 21 days using needle and canular to introduce the extract directly into the stomach through the oesophagus (orogastrically) per day, the dose are in 0.5ml of distilled water. Group A rats were the control with no administration of Nicotiana tabacum extract but given equal volume of distilled water as well (0.5ml). SEMEN COLLECTION: The rats were then anaesthetized by placing them into a glass chamber(dessicator) containing cotton wool soaked in chloroform till they lost consciousness. The testicles were then removed through a lower abdominal incision. The testes were then separated from the epididymis with the scalped blade. Sperm cells were sucked into a pre-warmed (37"C) Pasteur pipette from the caudal epididymis. It was flushed with 2-3 drops of 2.9% sodium citrate solf kept at 37"C. Half of the spermatozoal samples collected were mixed with 0.5 ml of 2.9% sodium citrate solution (7.C) for head forward unidirectional progressive motility. These were studied at x40 magnifications of the microscope .The mean percentages and standard error of mean were calculated for motility, live/dead ratio and Sperm concentration. ANOVA (Analysis of variance) was used to establish any significant difference in all these parameters using the Graphpad instat statistical tool (July 2009). Results are presented as mean standard error of mean. Semen analysis; The semen samples were analysed by method described by Zemjanis (1977). STATISTICAL ANALYSIS : Kruskal-Wallis Test (Nonparametric ANOVA) was used to analyze the sperm motility .The P value is 0.0005, considered extremely significant. Variation among column medians is significantly greater than expected by chance. The P value is approximate (from chi-square distribution) because at least one column has two or more identical values. While one way ANOVA was used to analyze the sperm count. RESULTS Table 1: Group A(control) S/NO % motility 1 2 3 4 5 67 77 66 78 60
Concentration 106/ml 69.4 70.5 62.4 65.0 65.0
Table 2: Group B (10mg/kg) S/NO % motility 1 2 3 4 5 31 38 42 32 31
Concentration 106/ml 51.1 60.5 62.0 60.0 71.3
139
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
Table 3: Group C (20mg/kg) S/NO % motility 1 2 3 4 5 21 20 25 20 23
Concentration 106/ml 62.9 61.7 60.0 62.3 57.2
Table 4: Group D S/NO 1 2 3 4 5
% motility 14 18 15 14 17
Concentration 106/ml 53.8 53.3 58.6 52.0 45.9
Table 5 The average percentage motility and sperm concentration It was observed that the groups of rats that had the higher doses of the aqueous extract (30mg/kg and 20mg/kg body weight had their percentage motility15.60.8, and 21.81.0 respectively) significantly lower (P<0.01 and S/NO Control(A) Group1(B) Group2(C) Group3(D) *P<0.05 significant . % Motility 69.63.4 34.82.2 21.81.0** 15.60.8*** **P<0.01 highly significant Sperm Concentration 106/ml 66.51511820 61.03212071 60.81026353 55.72038480** ***P<0.001 extremely significant
P< 0.001) when compared to the control group (69.63.4%). This shows that there was a dose dependent decrease in motility. There was also a highly significant decrease in sperm count at the dose of 30mg/kg. HISTOLOGY The histological plates shows the transverse section of testicular histology of the rats, fig I being the control (group A) and fig II,III and IV represents group B,C, and D given 10mg, 20, and 30mg/kg respectively. In fig.I, the seminiferous tubules, which are the sites of sperm production, have no abnormalities. It also showed germ cells at different levels of development. Fig III and IV shows the transverse section of testicular histology of the rats as Fig I and II respectively. In Fig. III and IV the seminiferous tubules, which are sites of sperm production have no abnormalities. But the spermatozoans in fig.III and IV shows much scanty developing cells in their various stages as evidenced by the decreased thickness of spermatogonic cells when compared to the control.
140
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
Fig I(control)
fig II(10mg/kg)
fig III(20mg/kg)
Fig IV(30mg/kg)
Discussion Sperm motility, sperm concentration and morphology are important sperm parameter in determine male fertility. Also the testicular histology too is used to shed more light on the indices in male fertility. This study shows a dose dependent decrease in sperm count and motility as well as a decrease in the spermatogonic cell layers on histology of the testis, this is in agreement with other studies that have examined the effects of cigarette smoking on male fertility, and the results have suggested a substantial negative effect on sperm production, motility, and morphology (Weber et al, 2002; Kunzle et al, 2003; Ramlau-Hansen, 2007a). Sperm concentration less than 10 106 /ml show a significant reduction in fertilization (De-Geyter el al 1992). The attainment of significant oligospermia cause failure of conception. Sperm motility also affects fertilization (Aitken et al 1989), Sperm motility of 50% and above consisting of rapid forward progression movement is essential for conception in human (WHO, 1987). Sperm motility less than 50% is known to result in failure of conception. The slight decrease in motility of sperm in this study is in agreement with the work carried out by Horimoto et al., 2000 on spermatozoan abnormalities and male infertility in the rats following sulfasalazine treatment, the work revealed that on administering the drug orally reduces motility of sperm and fertility of animals. It is also in agreement with the work carried out by Raji et al 2006 on the effect of methanol extract of Ricinus Communis seeds on sperm parameters. The study also revealed that there was decreases in motility are the cause of conception motility of sperm. The slight low concentration and motility are the cause of conception which result in the epididymis sperm cell that is cause by the effect of the extract on the testis are specifically of the spermatogenic process can be seen by the production of sperm cells. The testis is the male reproduction organ and consists of seminiferous tubules, which are the sites of sperm production. A cross section of the testis shows spermatogenic cells at various stages of development as well as other Histological component of the testis. In the growing rats treated rats have scanty developing cells in the seminiferous tubules but not in control. Also in the histological structure of adult testis both the seminiferous tubules and the spermatozoans are scantly, but normal in the control. Also the immature spermatogenic cells are arranged in the lumen of the seminiferous tubules. Though there was a relatively lower decrease in sperm count when compared with other studies it was significant when compared with control. This may suggest that higher doses of the tobacco extract be used in future studies and perhaps for a longer period of time.
Conclusion In conclusion the aqueous extract of nicotiana tabacum at doses of 20mg/kg and 30mg/kg when administered for a period of 21 days showed a significant decrease in sperm motility and concentration as well as decreased spermatogonic cells in the histology of the testis.
141
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
References Langgassner J. Rauchgewohnheiten der osterreichischen Bevolkerung. Satistische Nachr. 1999;5:319326. Vine MF, Margolin BH, Morrison HI, Hulka BS. Cigarette smoking and sperm density: a meta-analysis. Fertil Steril. 1994;61:3543. Zavos P, Correa J, Antypas S, Zarmakoupis-Zavos P, Costantinos N. Effects of seminal plasma from cigarette smokers on sperm viability and longevity. Fertil Steril. 1998a;69:425429. Ozgur K, Isikoglu M, Seleker M, Donmez L. Semen quality of smoking and non-smoking men in infertile couples in a Turkish population. Arch Gynecol Obstet. 2005;271:109112. Guo H, Zhang HG, Xue BG, Sha YW, Liu Y, Liu RZ. Effects of cigarette, alcohol consumption and sauna on sperm morphology. Zhonghua Nan Ke Xue. 2006;12:215217, 221 Pasqualotto F, Sobreiro B, Hallak J, Pasqualotto E, Lucon A. Cigarette smoking is related to a decrease in semen volume in a population of fertile men. BJU Int. 2006;97:324326. Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007a;22:188196. Kunzle R, Mueller M, Hanggi W, Birkhauser M, Drescher H, Bersinger N. Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril. 2003;79:287291. Collins & Lapsley, 2008 Effect of tobacco Yales CA, Thomas C, Kovacs GT, De Krester DM. Androgen, male factor, infertility and IVF. In: Wood C, Trouson A, editors. Clinical in vitro fertilization. USA: Springer-Verlag; 1989. pp. 95-111. Yeilli C, Mungan G, Sekiner I, Akduman B, Aikgz S, Altan K, et al. Effect of varicocelectomy on sperm creatine kinase, HspA2 chaperone protein (creatine kinase-M type), LDH, LDH-X, and lipid peroxidation product levels in infertile men with varicocele. Urology. Zemjanis R (1977). Collection and evaluation of semen. In: Diagnostic and Therapeutic Techniques in Animal Reproduction. William and Wilkins Company, Baltimore, USA. p. 242. Reijo R, Alagappan RK, Patrizio P, Page DC. Severe oligozoospermia resulting from deletions of azoospermia factor gene on Y chromosome. Lancet. 1996;347(9011):1290-3. Bonde JP. Male fertility. In: Comhaire FM, editor. Chapman and Hall Medicals. New York: Chapman and Hall; 1996. p. 266-84. Kapoor D, Jones TH. Smoking and hormones in health and endocrine disorders. Eur J Endocrinol. 2005;152(4):491-9. Weisberg E. Smoking and reproductive health. Clin Reprod Fertil. (1985) 3(3):175-86 Aydos K, Gven MC, Can B, Ergn A. Nicotine toxicity to the ultrastructure of the testis in rats. BJU Int. 2001;88(6):622-6. Mlynarcikova A, Fickova M, Scsukova S. Ovarian intrafollicular processes as a target for cigarette smoke components and selected environmental reproductive disruptors. Endocr Regul. 2005;39(1): 21-32. Tank LB, Christiansen C. An update on the antiestrogenic effect of smoking: a literature review with implications for researchers and practitioners. Menopause. 2004;11(1):104-9. Jones TH, Jones RD, Channer KS. Testosterone and its beneficial actions on cardiovascular disorders. In: Plotsky PM, Hunzicke-Dunne M, Rose JC, Brenner RM, editors. Recent research developments in endocrinology & metabolism, Volume 1. USA: Transworld research network; 2003. p. 143-68. Carmines EL, Gaworski CL, Faqi AS, Rajendran N. In utero exposure to 1R4F reference cigarette smoke: evaluation of developmental toxicity. Toxicol Sci. 2003;75(1):134-47. Gaworski CL, Carmines EL, Faqi AS, Rajendran N. In utero and lactation exposure of rats to 1R4F reference cigarette mainstream smoke: effect on prenatal and postnatal development. Toxicol Sci. 2004;79(1):157-69. Oyeyipo IP, Raji Y, Emikpe BO, Bolarinwa AF. Effects of oral administration of nicotine on organ weight, serum testosterone level and testicular pathology in adult male rats. Niger J Psychol Sci. 2010;25(1):81-86. Iranloye BO, Bolarinwa AF. Effect of nicotine administration on weight and histology of some vital visceral organs in female albino rats. Niger J Physiol Sci. 2009;24(1):7-12. Evans HJ, Fletcher J, Torrance M, Hargreave TB. Sperm abnormalities and cigarette smoking. Lancet. 1981;21:627629. Elshal MF, El-Sayed IH, Elsaied MA, El-Masry SA, Kumosani TA. Sperm head defects and disturbances in spermatozoal chromatin and DNA integrities in idiopathic infertile subjects: association with cigarette smoking. Clin Biochem. 2008;Dec 6. [Epub ahead of print] Gaur DS, Talekar M, Pathak VP. Effect of cigarette smoking on semen quality of infertile men. Singap Med J. 2007;48:119123. Mak V, Jarvi K, Buckspan M, Freeman M, Hechter S, Zini A.Smoking is associated with the retention of cytoplasm by human spermatozoa. Urology. 2000;56:463466.
142
Journal of Natural Sciences Research ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.3, No.5, 2013
www.iiste.org
De Geyter , 1992 evaluation of sperm motility Aitken RJ, Clarkson JS and Fishel S (1989) Generation of reactive oxygen species, lipid peroxidation and human sperm function Biology of reproduction 40 183-197. World Health Organization (1987)WHO Laboratory Manual for the Examination of Human Semen and SemenCervical Mucus Interaction.2nd edn. Cambridge University Press,Cambridge Raji Y, Oloyo AK, Morakinyo AO(2006) effect of methanol extract of Ricinus communis seed on reproduction of male rats. Asian J Androl.;8(1):115-21 Horimoto et al(2000) Rat epididymal sperm motion changes induced by ethylene glycol monoethyl ether, sulfasalazine, and 2,5-hexandione Reprod Toxicol;14(1):55-63.
143
This academic article was published by The International Institute for Science, Technology and Education (IISTE). The IISTE is a pioneer in the Open Access Publishing service based in the U.S. and Europe. The aim of the institute is Accelerating Global Knowledge Sharing. More information about the publisher can be found in the IISTEs homepage: http://www.iiste.org CALL FOR PAPERS The IISTE is currently hosting more than 30 peer-reviewed academic journals and collaborating with academic institutions around the world. Theres no deadline for submission. Prospective authors of IISTE journals can find the submission instruction on the following page: http://www.iiste.org/Journals/ The IISTE editorial team promises to the review and publish all the qualified submissions in a fast manner. All the journals articles are available online to the readers all over the world without financial, legal, or technical barriers other than those inseparable from gaining access to the internet itself. Printed version of the journals is also available upon request of readers and authors. IISTE Knowledge Sharing Partners EBSCO, Index Copernicus, Ulrich's Periodicals Directory, JournalTOCS, PKP Open Archives Harvester, Bielefeld Academic Search Engine, Elektronische Zeitschriftenbibliothek EZB, Open J-Gate, OCLC WorldCat, Universe Digtial Library , NewJour, Google Scholar
Vous aimerez peut-être aussi
- Assessment of Some Micronutrient (ZN and Cu) Status of Fadama Soils Under Cultivation in Bauchi, NigeriaDocument7 pagesAssessment of Some Micronutrient (ZN and Cu) Status of Fadama Soils Under Cultivation in Bauchi, NigeriaAlexander DeckerPas encore d'évaluation
- Asymptotic Properties of Bayes Factor in One - Way Repeated Measurements ModelDocument17 pagesAsymptotic Properties of Bayes Factor in One - Way Repeated Measurements ModelAlexander DeckerPas encore d'évaluation
- Assessment of The Practicum Training Program of B.S. Tourism in Selected UniversitiesDocument9 pagesAssessment of The Practicum Training Program of B.S. Tourism in Selected UniversitiesAlexander DeckerPas encore d'évaluation
- Assessment of Relationships Between Students' Counselling NeedsDocument17 pagesAssessment of Relationships Between Students' Counselling NeedsAlexander DeckerPas encore d'évaluation
- Assessment of Knowledge, Attitude and Practices Concerning Food Safety Among Restaurant Workers in Putrajaya, MalaysiaDocument10 pagesAssessment of Knowledge, Attitude and Practices Concerning Food Safety Among Restaurant Workers in Putrajaya, MalaysiaAlexander DeckerPas encore d'évaluation
- Availability, Accessibility and Use of Information Resources and Services Among Information Seekers of Lafia Public Library in Nasarawa StateDocument13 pagesAvailability, Accessibility and Use of Information Resources and Services Among Information Seekers of Lafia Public Library in Nasarawa StateAlexander DeckerPas encore d'évaluation
- Assessment of The Skills Possessed by The Teachers of Metalwork in The Use of Computer Numerically Controlled Machine Tools in Technical Colleges in Oyo StateDocument8 pagesAssessment of The Skills Possessed by The Teachers of Metalwork in The Use of Computer Numerically Controlled Machine Tools in Technical Colleges in Oyo StateAlexander Decker100% (1)
- Assessment of Teachers' and Principals' Opinion On Causes of LowDocument15 pagesAssessment of Teachers' and Principals' Opinion On Causes of LowAlexander DeckerPas encore d'évaluation
- Availability and Use of Instructional Materials and FacilitiesDocument8 pagesAvailability and Use of Instructional Materials and FacilitiesAlexander DeckerPas encore d'évaluation
- Barriers To Meeting The Primary Health Care Information NeedsDocument8 pagesBarriers To Meeting The Primary Health Care Information NeedsAlexander DeckerPas encore d'évaluation
- Attitude of Muslim Female Students Towards Entrepreneurship - A Study On University Students in BangladeshDocument12 pagesAttitude of Muslim Female Students Towards Entrepreneurship - A Study On University Students in BangladeshAlexander DeckerPas encore d'évaluation
- Application of Panel Data To The Effect of Five (5) World Development Indicators (WDI) On GDP Per Capita of Twenty (20) African Union (AU) Countries (1981-2011)Document10 pagesApplication of Panel Data To The Effect of Five (5) World Development Indicators (WDI) On GDP Per Capita of Twenty (20) African Union (AU) Countries (1981-2011)Alexander DeckerPas encore d'évaluation
- Assessment of Housing Conditions For A Developing Urban Slum Using Geospatial AnalysisDocument17 pagesAssessment of Housing Conditions For A Developing Urban Slum Using Geospatial AnalysisAlexander DeckerPas encore d'évaluation
- Assessment of Survivors' Perceptions of Crises and Retrenchments in The Nigeria Banking SectorDocument12 pagesAssessment of Survivors' Perceptions of Crises and Retrenchments in The Nigeria Banking SectorAlexander DeckerPas encore d'évaluation
- Assessment of Factors Responsible For Organizational PoliticsDocument7 pagesAssessment of Factors Responsible For Organizational PoliticsAlexander DeckerPas encore d'évaluation
- Are Graduates From The Public Authority For Applied Education and Training in Kuwaiti Meeting Industrial RequirementsDocument10 pagesAre Graduates From The Public Authority For Applied Education and Training in Kuwaiti Meeting Industrial RequirementsAlexander DeckerPas encore d'évaluation
- Assessment of Productive and Reproductive Performances of CrossDocument5 pagesAssessment of Productive and Reproductive Performances of CrossAlexander DeckerPas encore d'évaluation
- Antibiotic Resistance and Molecular CharacterizationDocument12 pagesAntibiotic Resistance and Molecular CharacterizationAlexander DeckerPas encore d'évaluation
- Assessment in Primary School Mathematics Classrooms in NigeriaDocument8 pagesAssessment in Primary School Mathematics Classrooms in NigeriaAlexander DeckerPas encore d'évaluation
- Application of The Diagnostic Capability of SERVQUAL Model To An Estimation of Service Quality Gaps in Nigeria GSM IndustryDocument14 pagesApplication of The Diagnostic Capability of SERVQUAL Model To An Estimation of Service Quality Gaps in Nigeria GSM IndustryAlexander DeckerPas encore d'évaluation
- Assessment For The Improvement of Teaching and Learning of Christian Religious Knowledge in Secondary Schools in Awgu Education Zone, Enugu State, NigeriaDocument11 pagesAssessment For The Improvement of Teaching and Learning of Christian Religious Knowledge in Secondary Schools in Awgu Education Zone, Enugu State, NigeriaAlexander DeckerPas encore d'évaluation
- Antioxidant Properties of Phenolic Extracts of African Mistletoes (Loranthus Begwensis L.) From Kolanut and Breadfruit TreesDocument8 pagesAntioxidant Properties of Phenolic Extracts of African Mistletoes (Loranthus Begwensis L.) From Kolanut and Breadfruit TreesAlexander DeckerPas encore d'évaluation
- Assessing The Effect of Liquidity On Profitability of Commercial Banks in KenyaDocument10 pagesAssessing The Effect of Liquidity On Profitability of Commercial Banks in KenyaAlexander DeckerPas encore d'évaluation
- Applying Multiple Streams Theoretical Framework To College Matriculation Policy Reform For Children of Migrant Workers in ChinaDocument13 pagesApplying Multiple Streams Theoretical Framework To College Matriculation Policy Reform For Children of Migrant Workers in ChinaAlexander DeckerPas encore d'évaluation
- Analysis The Performance of Life Insurance in Private InsuranceDocument10 pagesAnalysis The Performance of Life Insurance in Private InsuranceAlexander DeckerPas encore d'évaluation
- An Investigation of The Impact of Emotional Intelligence On Job Performance Through The Mediating Effect of Organizational Commitment-An Empirical Study of Banking Sector of PakistanDocument10 pagesAn Investigation of The Impact of Emotional Intelligence On Job Performance Through The Mediating Effect of Organizational Commitment-An Empirical Study of Banking Sector of PakistanAlexander DeckerPas encore d'évaluation
- Analysis of Frauds in Banks Nigeria's ExperienceDocument12 pagesAnalysis of Frauds in Banks Nigeria's ExperienceAlexander DeckerPas encore d'évaluation
- Analyzing The Economic Consequences of An Epidemic Outbreak-Experience From The 2014 Ebola Outbreak in West AfricaDocument9 pagesAnalyzing The Economic Consequences of An Epidemic Outbreak-Experience From The 2014 Ebola Outbreak in West AfricaAlexander DeckerPas encore d'évaluation
- Analysis of Teachers Motivation On The Overall Performance ofDocument16 pagesAnalysis of Teachers Motivation On The Overall Performance ofAlexander DeckerPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Pharmacy Calculations Review: Pharmacy Tech Topics™ Volume 16 Number 3 July 2011Document24 pagesPharmacy Calculations Review: Pharmacy Tech Topics™ Volume 16 Number 3 July 2011Mirumbi Kefa MomanyiPas encore d'évaluation
- Timetable 1Document1 pageTimetable 1sunilbijlaniPas encore d'évaluation
- Bacteriological Quality and Safety of Street Vended Foods in Delta State, NigeriaDocument6 pagesBacteriological Quality and Safety of Street Vended Foods in Delta State, NigeriaAlexander DeckerPas encore d'évaluation
- Group 11 Research ReportDocument18 pagesGroup 11 Research ReportjoesayikPas encore d'évaluation
- The Fig and Olive MiracleDocument2 pagesThe Fig and Olive MiracleIman Syafar100% (1)
- Tanganyika Nacte Past Paper-1Document116 pagesTanganyika Nacte Past Paper-1Mnawaru KhalfaniPas encore d'évaluation
- Wyeth Laboratories - Intramuscular InjectionsDocument36 pagesWyeth Laboratories - Intramuscular InjectionsflexionPas encore d'évaluation
- Psychiatric Drugs Are Neurotoxins-Power-Point-OutlineDocument30 pagesPsychiatric Drugs Are Neurotoxins-Power-Point-OutlineAugustaPas encore d'évaluation
- Classification of Mental Disorder, Antisocial Personalities, Drug and Alcohol DependenceDocument15 pagesClassification of Mental Disorder, Antisocial Personalities, Drug and Alcohol DependenceAdrian SingsonPas encore d'évaluation
- TOC MillerDocument5 pagesTOC MillerNikhil KumarPas encore d'évaluation
- First AidDocument22 pagesFirst Aidlinaj67% (3)
- Menastil Complete Clinical Trials - Pain Relief That Works.Document43 pagesMenastil Complete Clinical Trials - Pain Relief That Works.emoryholstPas encore d'évaluation
- Urban IssuesDocument8 pagesUrban IssuesdreamspacearchitectsPas encore d'évaluation
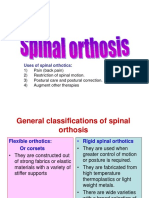
- Spinal OrthosisDocument16 pagesSpinal OrthosisChristya Ari NugrahaPas encore d'évaluation
- Career Project - Elizabeth TretoDocument9 pagesCareer Project - Elizabeth Tretoapi-258367028Pas encore d'évaluation
- Underwriting PacketDocument9 pagesUnderwriting Packetapi-207980596Pas encore d'évaluation
- Sleeping Pattern Among Students ReportDocument15 pagesSleeping Pattern Among Students ReportHazwani RahmanPas encore d'évaluation
- Betz Rebecca ResumeDocument2 pagesBetz Rebecca Resumeapi-316054946Pas encore d'évaluation
- Company IndexingDocument10 pagesCompany IndexingRushank ShuklaPas encore d'évaluation
- Prospekt BR 102plusDocument4 pagesProspekt BR 102plusAnonymous zynaalZPas encore d'évaluation
- Case OSCEsDocument74 pagesCase OSCEsHassan R. G.75% (4)
- TahbsoDocument4 pagesTahbsomichZ_13Pas encore d'évaluation
- Blood Cold ChainDocument74 pagesBlood Cold Chainشريف عبد المنعمPas encore d'évaluation
- OFLOXACINDocument3 pagesOFLOXACINfayrouz fathiPas encore d'évaluation
- Synthesis PaperDocument19 pagesSynthesis Paperapi-330084238Pas encore d'évaluation
- Resume 6 2015Document2 pagesResume 6 2015api-290445636Pas encore d'évaluation
- 51 Diseases of Ruminants - Dr. SulaDocument92 pages51 Diseases of Ruminants - Dr. SulaCholid MawardiPas encore d'évaluation
- Avena SativaDocument46 pagesAvena SativaJuliana VarelaPas encore d'évaluation
- Intro To HematologyDocument9 pagesIntro To HematologyDayledaniel SorvetoPas encore d'évaluation
- Running Head: Normal Saline vs. Heparin 1Document9 pagesRunning Head: Normal Saline vs. Heparin 1MaureenAmilcaPas encore d'évaluation