Académique Documents
Professionnel Documents
Culture Documents
Bleeding During Pregnancy Overview
Transféré par
neleh grayCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Bleeding During Pregnancy Overview
Transféré par
neleh grayDroits d'auteur :
Formats disponibles
Bleeding During Pregnancy Overview Because bleeding during all phases of pregnancy may be dangerous, a woman should call
her health care professional if she has any signs of vaginal bleeding during her pregnancy. Vaginal bleeding is any blood coming from the vagina (the canal leading from the uterus to the external genitals). This usually refers to abnormal bleeding not associated with a regular menstrual period.
First trimester bleeding is any vaginal bleeding during the first 3 months of pregnancy. Vaginal bleeding may vary from light spotting to heavy bleeding with clots. Vaginal bleeding is a common problem in early pregnancy, complicating 20% to 30% of all pregnancies. Any vaginal bleeding during the second and third trimesters of pregnancy (the last 6 months of a 9-month pregnancy) involves concerns different from bleeding in the first 3 months of the pregnancy. Any bleeding during the second and third trimesters is abnormal. Bleeding from the vagina after the 28th week of pregnancy is a true emergency. The bleeding can range from very mild to extremely brisk and may or may not be accompanied by abdominal pain. Hemorrhage (another word for bleeding) is the most common cause of death of the mother in the United States. It complicates about 4% of all pregnancies.
Bleeding During Pregnancy Causes First Trimester Bleeding Causes Vaginal bleeding in the first trimester of pregnancy can be caused by several different factors. Bleeding affects 20% to 30% of all pregnancies. Up to 50% of those who bleed may go on to have a miscarriage (lose the baby). Of even more concern, however, is that about 3% of all pregnancies are ectopic in location (the fetus is not inside the uterus), and vaginal bleeding can be a sign of an ectopic pregnancy. An ectopic pregnancy may be life threatening to the mother. All bleeding associated with early pregnancy should prompt a call to your health care provider for immediate evaluation.
Implantation bleeding: There can be a small amount of spotting associated with the normal implantation of the embryo into the uterine wall, called implantation bleeding. This is usually very minimal, but frequently occurs on or about the same day as your period was due. This can be very confusing if you mistake it for simply a mild period
and don't realize you are pregnant. This is a normal part of pregnancy and no cause for concern. Threatened miscarriage: You may be told you have a threatened miscarriage if you are having some bleeding or cramping. The fetus is definitely still inside the uterus (based usually on an exam using ultrasound), but the outcome of your pregnancy is still in question. This may occur if you have an infection, such as a urinary tract infection, become dehydrated, use certain drugs or medications, have been involved in physical trauma, if the developing fetus is abnormal in some way, or for no apparent reason at all. Other than these reasons, threatened miscarriages are generally not caused by things you do, such as heavy lifting or having sex, or by emotional stress. Completed miscarriage: You may have a completed miscarriage (also called a spontaneous abortion) if your bleeding and cramping have slowed down and the uterus appears to be empty based on ultrasound evaluation. This means you have lost the pregnancy. The causes of this are the same as those for a threatened miscarriage. This is the most common cause of first trimester bleeding. Incomplete miscarriage: You may have an incomplete miscarriage (or a miscarriage in progress) if the pelvic exam shows your cervix is open and you are still passing blood, clots, or tissue. The cervix should not remain open for very long. If it does, it indicates the miscarriage is not completed. This may occur if the uterus begins to clamp down before all the tissue has passed, or if there is infection. Blighted ovum: You may have a blighted ovum (also called embryonic failure). An ultrasound would show evidence of an intrauterine pregnancy, but the embryo has failed to develop as it should in the proper location. This may occur if the fetus were abnormal in some way and not generally due to anything you did or didn't do. Intrauterine fetal demise: You may have an intrauterine fetal demise (also called IUFD, missed abortion, or embryonic demise) if the developing baby dies inside the uterus. This diagnosis would be based on ultrasound results and can occur at any time during pregnancy. This may occur for any of the same reasons a threatened miscarriage occurs during the early stages of pregnancy; however it is very uncommon for this to occur during the second and third trimesters of pregnancy. If it does, the causes also include separation of the placenta from the uterine wall (called placental abruption) or because the placenta didn't receive sufficient blood flow.
Ectopic pregnancy: You may have an ectopic pregnancy (also called tubal pregnancy). This would be based on your medical history and ultrasound, and in some cases laboratory results. Bleeding from an ectopic pregnancy is the most dangerous cause of first trimester bleeding. An ectopic pregnancy occurs when the fertilized egg implants outside of the uterus, most often in the Fallopian tube. As the fertilized egg grows, it can rupture the Fallopian tube and cause life-threatening bleeding. Symptoms are often variable and may include pain, bleeding, or lightheadedness. Most ectopic pregnancies will cause pain before the tenth week of pregnancy. The fetus is not going to develop and will die because of lack of supply of nutrients. This condition occurs in about 3% of all pregnancies. o There are risk factors for ectopic pregnancy. These include a history of prior ectopic pregnancy, history of pelvic inflammatory disease, history of Fallopian tube surgery or ligation, history of infertility for more than 2 years, having an IUD (birth control device placed in the uterus) in place, smoking, or frequent (daily) douching. Only about 50% of women who have an ectopic pregnancy have any risk factors, however. Molar pregnancy: You may have a molar pregnancy (technically called gestational trophoblastic disease). Your ultrasound results may show the presence of abnormal tissue inside the uterus rather than a developing fetus. This is actually a type of tumor that occurs as a result of the hormones of pregnancy, and is usually not life-threatening to you. However, in rare cases the abnormal tissue is cancerous. If it is cancerous it can invade the uterine wall and spread throughout the body. The cause of this is generally unknown. Postcoital bleeding is vaginal bleeding after sexual intercourse. It may be normal during pregnancy. Bleeding may also be caused by reasons unrelated to pregnancy. For example, trauma or tears to the vaginal wall may bleed, and some infections may cause bleeding.
bleed because of this, it is called placenta previa. Late in pregnancy as the opening of your womb, called the cervix, thins and dilates (widens) in preparation for labor, some blood vessels of the placenta stretch and rupture. This causes about 20% of third-trimester bleeding and happens in about 1 in 200 pregnancies. Risk factors for placenta previa include these conditions:
Multiple pregnancies Prior placenta previa Prior Cesarean delivery
Placental abruption: This condition occurs when a normal placenta separates from the wall of the womb (uterus) prematurely and blood collects between the placenta and the uterus. Such separation occurs in 1 in 200 of all pregnancies. The cause is unknown. Risk factors for placental abruption include these conditions:
High blood pressure (140/90 or greater) Trauma (usually a car accident or maternal battering) Cocaine use Tobacco use Abruption in prior pregnancies (you have a 10% risk it will happen again)
Uterine rupture: This is an abnormal splitting open of the uterus, causing the baby to be partially or completely expelled into the abdomen. Uterine rupture is rare, but very dangerous for both mother and baby. About 40% of women who have uterine rupture had prior surgery on their uterus, including Cesarean delivery. The rupture may occur before or during labor or at the time of delivery. Other risk factors for uterine rupture are these conditions:
More than four pregnancies Trauma Excessive use of oxytocin (Pitocin), a medicine that helps strengthen contractions A baby in any position other than head down Having the baby's shoulder get caught on the pubic bone during labor Certain types of forceps deliveries
Late-Pregnancy Bleeding Causes The most common cause of late-pregnancy bleeding is a problem with the placenta. Some bleeding can also be due to an abnormal cervix or vagina. Placenta previa: The placenta, which is a structure that connects the baby to the wall of your womb, can partially or completely cover the cervical opening (the opening of the womb to the vagina). When you
Fetal vessel rupture: This condition occurs in about 1 of every 1,000 pregnancies. The baby's blood vessels from the umbilical cord may attach to the membranes instead of the placenta. The baby's blood vessels pass over the entrance to the birth canal. This is called vasa previa and occurs in 1 in 5,000 pregnancies. Less common causes of late-pregnancy bleeding include injuries or lesions of the cervix and vagina, including polyps, cancer, and varicose veins.
Inherited bleeding problems, such as hemophilia, are very rare, occurring in 1 in 10,000 women. If you have one of these conditions, such as von Willebrand disease, tell your doctor. Bleeding During Pregnancy Symptoms It is helpful for your health care professional to know the amount and the quality of the bleeding that you have. Keep track of the number of pads used and passage of clots and tissue. If you pass a clump of tissue and are going to see your doctor, bring the tissue with you for examination. Other symptoms you may experience are increased fatigue, excessive thirst, dizziness, or fainting. Any of these may be signs of significant blood loss. You may notice a fast pulse rate that increases when you stand up from lying down or sitting. Dizziness may increase when you stand up as well. With late-pregnancy bleeding, you may have these specific symptoms:
your health care professional. Be prepared to give information about the amount of blood lost and a description of how you are feeling overall. If your bleeding is light and you have no pain, your evaluation may be in the doctor's office. Go to a hospital's emergency department if the following conditions develop:
Placenta previa: About 70% of women have painless bright red blood from the vagina. Another 20% have some cramping with the bleeding, and 10% have no symptoms. Placental abruption: About 80% of women have dark blood or clots from the vagina, but 20% have no external bleeding. More than one-third have a tender uterus. About two-thirds of women with placental abruption have the classic "pain and bleeding." Over half of the time the baby shows signs of distress. Most abruptions occur before labor begins. Uterine rupture: Symptoms are highly variable. Classic uterine rupture is described as intense abdominal pain, heavy vaginal bleeding, and a "pulling back" from the birth canal of the baby's head. The pain may initially be intense, then get better with rupture, only to worsen as the lining of the abdomen is irritated. Bleeding can range from spotting to severe hemorrhage. Fetal bleeding: This condition may show up as vaginal bleeding. The baby's heart rate on the monitor will first be very fast, then slow, as the baby loses blood. Lower genital tract injury: This condition usually causes only mild spotting. Cervical cancer is very rare in women of childbearing age. A yeast infection may cause a white or pink discharge and can be itchy. A ruptured vaginal varicose vein can cause heavy bleeding.
If you have severe bleeding or cramps and contractions (call 911) If vaginal bleeding in pregnancy lasts for more than 24 hours and you are unable to get in touch with your health care professional or you don't have one If you faint (pass out) or feel very dizzy If you are bleeding and develop a fever over 100.5 F (38.05 C) If you have pain worse than a normal period, or severe localized pain in your abdomen, pelvis, or back If you have undergone an abortion and develop a fever, abdominal or pelvic pain, or increased bleeding If you have been given medical treatment for ectopic pregnancy with methotrexate (Rheumatrex, Trexall), and you develop increased abdominal or pelvic pain within the first week after the injection
Bleeding During Pregnancy Diagnosis The medical evaluation begins with a thorough history and physical exam. Depending on the setting (medical office or hospital) and the seriousness of your symptoms, laboratory and ultrasound tests may be performed. For bleeding in the early part of pregnancy, the doctor's main goal will be to make sure you don't have an ectopic pregnancy. That is what the evaluation will focus on. For late-pregnancy bleeding, the doctor first will make sure you are stable. Medical History and Physical Exam Medical history: Your health care professional will ask you a lot of questions:
When to Seek Medical Care Bleeding is not normal at any time during pregnancy. Report any vaginal bleeding during pregnancy to
If early in pregnancy, your pregnancy history will be reviewed regarding the certainty of the dates of your pregnancy. If you think you are pregnant, you usually are. Although, in many cases, women who don't think they are pregnant, often can be. You may be asked about recent trauma or sexual intercourse and whether you have abdominal pain or contractions. Your medical history will be reviewed, with emphasis on bleeding disorders, liver problems, and drug or tobacco use.
You will be asked about prior Cesarean deliveries, preterm labor, placenta previa, or placental abruptions.
Physical exam: Regardless of where you are being treated, the first thing that should be established is how sick you are as a result of the bleeding. This is done by evaluating vital signs (pulse and blood pressure), and by a quick physical assessment of volume of blood loss by looking to see if you are pale or if you have abdominal tenderness. If you have lost a significant amount of blood, you will be treated with IV fluids and you may need surgery.
Your abdomen will be examined to see if you are tender and to check the size of your uterus. You will be checked for bleeding from other sites, such as the nose or rectum. The results of the pelvic exam may or may not be very helpful in differentiating between ectopic pregnancy and threatened miscarriage: 10% of women with an ectopic pregnancy will have a completely normal pelvic exam. How enlarged the uterus is on examination may help, because in less than 3% of ectopic pregnancies is the uterus enlarged to greater than 10 cm. Quantity and quality of abdominal pain and vaginal bleeding is important for the doctor to know. Pain is seen in most women with ectopic pregnancy (up to 90%) and vaginal bleeding (50%-80%). Late in pregnancy, you will have an abdominal ultrasound prior to a vaginal exam to see if you have a placenta previa. If ultrasound does not show previa, you will have a sterile speculum vaginal exam to evaluate you for injury to the lower genital tract. If the vaginal exam is normal, you will have a digital exam to check for cervical dilation. You will have monitors attached to your abdomen to check for contractions and for the baby's heart rate. Symptoms and physical examination diagnose uterine rupture. The symptoms that suggest rupture are sudden onset of severe abdominal pain, abnormality of the size and shape of the uterine contour, and regression of the baby's head up the birth canal.
The urine pregnancy test is extremely sensitive for diagnosing pregnancy at or about the same time you miss your period, or possibly a few days before. A urinalysis can diagnose urinary tract infections, regardless of whether you have symptoms of this type of infection. This is because infections, specifically of the urinary tract, are a cause of miscarriage. Also, a urinary tract infection with no symptoms is relatively common in pregnancy, occurring in 2%-11% of pregnant women. Up to a fourth of these women will go on to have kidney infections. Your blood type will be checked. You are being screened for whether your type is Rh negative or positive. If you are negative and the father of the baby is positive, your body may make antibodies against the baby's blood cells. If this occurs without treatment, the next time you are pregnant, these antibodies will appear again and harm that baby. If this is discovered during the first pregnancy and treatment with an injection called RhoGAM is given, this prevents the antibodies from forming. A blood count is routinely obtained to have an estimate of how much bleeding has already occurred. The bhCG level is a measure of the volume of living tissue associated with the developing pregnancy. Both ectopic and intrauterine pregnancies (IUP) produce bhCG, although there is usually a difference in the rate at which the quantitative bhCG level increases. Although a single value of bhCG isn't useful for differentiating between a normal or abnormal pregnancy or an ectopic pregnancy, a variation in the expected rate of rise of the bhCG level can be helpful. A falling bhCG does not exclude the possibility of tubal rupture. The real value of the quantitative bhCG for diagnosis of ectopic pregnancy is when it is used in correlation with the results of a pelvic ultrasound.
Laboratory Tests and Imaging Lab tests: Several lab tests are routinely obtained. They include a urine pregnancy test, a urinalysis, a blood type and Rh, and a complete blood count (CBC). Serum quantitative bhCG, which is a blood hormone marker of pregnancy, is also frequently obtained.
Ultrasound: Ultrasound can often determine if the fetus is healthy and growing inside the uterus. Ultrasound is a form of imaging using sound waves, not X-rays. It is a test that is often able to identify a pregnancy and estimate the age of the fetus. However, a pregnancy may be too early to be seen on ultrasound.
Ultrasound may be able to identify an ectopic pregnancy growing outside of the uterus. It also may be used to look for blood in the pelvis, a very serious complication that can occur when the ectopic pregnancy has ruptured the Fallopian tube. Late in pregnancy, placenta previa is diagnosed almost exclusively by abdominal
ultrasound, which can detect it 95% of the time. Placental abruption is diagnosed by excluding other causes. It often cannot be confirmed until after delivery when the placenta is found to have a blood clot attached to it. An ultrasound is performed to make certain that the bleeding is not from a placenta previa. Ultrasound at best is only able to detect about half of placental abruptions. Fetal bleeding can be distinguished from maternal bleeding by performing a special test on the blood present in the vagina. Also, a special type of ultrasound (Doppler) may be used to see the blood flow within the blood vessels. Lower genital tract problems can easily be diagnosed with a speculum examination. It is important that an ultrasound rule out placenta previa prior to any vaginal exam.
Surgery is usually a laparoscopic procedure (small incisions in your abdomen for tiny instruments) into the Fallopian tube and removal of the ectopic pregnancy, while attempting to save as much of the tube as possible. This may not be possible, however, if there has been much damage to the tube by the ectopic pregnancy itself or from significant bleeding. Threatened miscarriage: If you are diagnosed with a threatened miscarriage, your health care practitioner will give you instructions about activities, what to watch for, and when to return for follow-up. Home care for threatened miscarriages includes restinguntil any pain or bleeding stops. Avoid sexual intercourse for 3 weeks. You should not douche or use tampons. Incomplete/inevitable abortion: You will be admitted to the hospital for a procedure to remove any remaining fetal tissue in your uterus. This is called dilation and curettage (uterine evacuation or D&C) to prevent any further complications such as hemorrhage or infection. Missed abortion: In this case, you may either be admitted to the hospital for a D&C or monitored at home with the possibility of passing the tissue without surgery. This decision is made by you and your doctor after a discussion of the risks and benefits of both choices. The age and size of the fetus may be important when deciding which course of action to pursue. Complete abortion: You may be sent home after complete passage of fetal tissue is ensured or if an ultrasound shows no remaining tissue. Molar pregnancy: Immediate D&C is necessary. Follow-up blood B-hCG levels should be obtained to check for chorionic carcinoma (a type of cancer). Late pregnancy bleeding With late-pregnancy bleeding, you will be monitored for blood loss and signs of shock. You will receive IV fluids and possibly blood transfusions. Your baby will be monitored closely for signs of distress. Your treatment will be guided by the cause of your bleeding, your condition, and the age of the baby (weeks' gestation). Placenta Previa
Bleeding During Pregnancy Treatment The treatment options for vaginal bleeding during pregnancy depend on the diagnosis and the certainty of that diagnosis. Bleeding During Pregnancy Self-Care at Home If you begin to bleed during early pregnancy, until your doctor has seen you and given different instructions, you should take it easy. Rest and relax, do not undertake heavy lifting or strenuous exercise, and abstain from sex, tampon use, or douching. Drink plenty of water and try to avoid against dehydration. Remember to keep track of the number of pads used and if the bleeding is increasing or decreasing. There is no home care for late-pregnancy bleeding. You must see a health care professional immediately. Bleeding During Pregnancy Medical Treatment Early pregnancy bleeding Ectopic pregnancy: If you have been diagnosed with an ectopic pregnancy by ultrasound, you may be given medication or taken into surgery.
Medical management is with methotrexate (Rheumatrex, Trexall), a drug that kills rapidly developing tissue. Surgery is reserved for those women who do not meet certain criteria for receiving medical treatment with methotrexate, and for those who are too sick to wait for the methotrexate to work. Also, if you choose not to have methotrexate therapy, then surgery would be the only other option.
Cesarean delivery (the baby is delivered surgically) is the preferred route of delivery. If you or your baby is in danger from severe bleeding, you will have an emergency Cesarean delivery. If you are having contractions, you may get IV medicine to slow them or stop them.
If your pregnancy is fewer than 36 weeks and your bleeding is not severe, you will be admitted to the hospital for observation, monitoring of your baby's heart rate, and repeated blood counts to check for anemia. You will get a medicine to help your baby's lungs mature. When you are 36 weeks pregnant, the doctor will check your baby's lungs, and, if they are mature, you will have a Cesarean delivery. Almost all deliveries will be Cesarean deliveries because of the high risk of severe bleeding and danger to the baby by a vaginal delivery. In very rare cases, when the placenta is next to but not covering the cervix, a vaginal delivery may be attempted. Even with a Cesarean delivery, you can lose up to 3 pints of blood.
Bleeding During Pregnancy Follow-up If you have any complications including bleeding, abdominal pain, or fever, you should return to the doctor for reexamination. If you have been treated for ectopic pregnancy and have increased pain or any weakness or dizziness, you should call an ambulance or have someone take you to a hospital's emergency department immediately.
Placental Abruption
Vaginal delivery is the preferred delivery. Cesarean delivery is reserved for emergencies. If you have massive bleeding and you or your baby are in danger, then an emergency Cesarean delivery will be performed. If your baby is more than 36 weeks, you will have a rapid but controlled vaginal delivery. You may be given some IV medication to make your contractions more effective. If your pregnancy is fewer than 36 weeks and your bleeding is not severe, you will be admitted to the hospital for observation, monitoring of your baby's heart rate, and repeated blood counts to check for anemia. You will get a medicine to help your baby's lungs mature. When you are 36 weeks pregnant, the doctor will check your baby's lungs, and, if they are mature, you will have a Cesarean delivery.
You may be placed on bed rest with instructions to place nothing into the vagina. Do not douche, use tampons, or have sexual intercourse until the bleeding stops. Follow-up care with your gynecologist should be arranged within 1-2 days. Women who have had a molar pregnancy need regular, long-term follow-up and repeat measurements of beta-hCG to ensure that no cancer will develop.
Bleeding During Pregnancy Prevention The best way to prevent any complication in pregnancy is to have a good relationship with your health care professional and to maintain close contact throughout your pregnancy. This is especially important if you have had prior pregnancies complicated by third-trimester bleeding. Avoid bleeding in pregnancy by controlling your risk factors, especially the use of tobacco and cocaine. If you have high blood pressure, work closely with your health care professional to keep it under control. Bleeding During Pregnancy Prognosis The effects of bleeding during your pregnancy depend on many factors. The cause of the bleeding and whether it is treatable is the most important issue. Early pregnancy bleeding If a normal appearing pregnancy with a normal beating heart is seen by ultrasound inside the uterus and you are younger than 40 years, the pregnancy has a less than 3% chance of being a miscarriage. If you are older than 40 years, then there is an 8% chance of a miscarriage. If there is not a definite pregnancy seen within the uterus, then the likelihood of a miscarriage is really unknown but could be up to 50%. Ectopic pregnancy: For bleeding in early pregnancy caused by ectopic pregnancy, the pregnancy will not survive. If you have such a pregnancy, the
Uterine Rupture
If there is a high suspicion for rupture of the uterus, you will have an immediate Cesarean delivery. Your uterus may have to be removed. If you are stable and want to have more children, the surgeon may be able to repair your uterus. You will probably need to have blood transfusions with several units of blood. Fetal bleeding is treated by performing an immediate Cesarean delivery.
possibilities of future ectopic pregnancies depend on the location, timing, and management of the condition. About 50% of women with ectopic pregnancies later have successful pregnancies. Threatened abortion: You will have an entirely normal pregnancy and birth 50% of the time. Alternatively, you may progress to have a spontaneous abortion or miscarriage. If you have an ultrasound at the time of your evaluation, which shows a fetus with a heartbeat in the uterus, there is a 75%-90% chance of having a normal pregnancy. Complete abortion or miscarriage: For women with recurrent miscarriages, the possibility of having a successful pregnancy is still high. Even after two or more miscarriages, your chances for delivering a child are still high. Molar pregnancy: After having a molar pregnancy, the risk of molar pregnancy in a later conception is about 1%. In addition, the overall risk of a certain form of cancer in women who have had a prior molar pregnancy has been estimated at 1,000 times higher than that of women who have not had a molar pregnancy. Late pregnancy bleeding Placenta Previa: The risk of maternal death is less than 1%, but other complications, such as massive hemorrhage requiring a blood transfusion or a hysterectomy, can also occur.
As the placenta separates from the womb, amniotic fluid and some placental tissue may enter the woman's bloodstream and cause a reaction. Her blood may become very thin and not clot well, which worsens the hemorrhage. She may require additional blood products to help her clot.
Uterine Rupture: This is a very dangerous condition for both the woman and the baby.
The greatest risks to the woman are hemorrhage and shock. An increased rate of transfusion occurs with uterine rupture, and 58% of women require more than 5 units of blood transfused. TThe risk of death for the woman is less than 1%. However, if left untreated, the woman will die. The risk to the fetus is extremely high. The death rate is about one in three. Fetal bleeding is extremely dangerous for the baby. The risk of death for the baby is 50% and is increased to 75% if the membranes rupture (water breaks).
Congenital Bleeding Disorders: TThe risk of complications for the woman is quite low. The most concerning is hemorrhage. The risk to the infant is very low. The largest risk to the baby, especially if it is a male, is inheritance of the bleeding disorder. Dilation and Curettage (D&C) Introduction The dilation and curettage procedure (D&C) involves dilating the uterine cervix so that the lining tissue (endometrium) of the uterus can be removed by scraping or suction. The D&C is a safe procedure that is done for a variety of reasons. It is minor surgery performed in a hospital or ambulatory surgery center or clinic. D&C is usually a diagnostic procedure and seldom is therapeutic. A D&C is often done as an adjunct procedure to a hysteroscopy and/or polypectomy. In addition, a D&C is often used for the following conditions: 1) Irregular or excessive bleeding: Irregular bleeding includes spotting or bleeding between periods. Bleeding with long, heavy periods, or bleeding after menopause, can signal a number of problems. A D&C allows removal of the uterine lining and examination of the tissue under a microscope by a pathologist. This can help establish the cause of the abnormal bleeding. The causes of irregular or abnormal bleeding include:
RRarely, the placenta attaches abnormally deep into the uterus. This is called a placenta accreta, increta, or percreta, depending on the depth. Many women who have this condition have such massive bleeding that a hysterectomy (removal of the uterus) is required to save the woman's life. Up to 8 of every 100 babies with placenta previa die, usually because of premature delivery and lack of lung maturity. Other problems for the baby include size smaller than expected, birth defects, breathing difficulties, and anemia requiring blood transfusion.
Placental Abruption:The risk of maternal death is low, but major blood loss may require transfusions.
The risk of death for the baby with placental abruption is about 1 in 500. This accounts for 15% of all newborn deaths. If the baby survives, about 15% have neurological and behavioral problems as a result of decreased oxygen to the brain. This occurs because placental blood vessels spasm and reduce the flow of oxygen to the baby before delivery.
Fibroids and polyps: These conditions are very common. In fact, they are thought to occur in about 20% of all women. Fibroid tumors are noncancerous growths appearing in and on the uterus. Some even grow out from the uterine wall on a stalk. Fibroids can cause chronic pain and heavy bleeding. Polyps, like fibroids, are noncancerous growths and are a common cause of irregular bleeding. Polyps and fibroids can have symptoms that resemble other more serious causes of bleeding. Endometrial cancer: A D&C and hysteroscopy are often performed to make certain patient's symptoms are not caused by uterine cancer or precancerous changes. It is, of course, important to detect cancer in its earliest, most curable stages.
2) Therapeutic D&C: A D&C is often planned as treatment when the source of the problem is already known. One situation is an incomplete miscarriage or even full-term delivery when, for some reason, the fetal or placental tissue inside of the uterus has not been completely expelled. If tissue is left behind, excess bleeding can result, perhaps even lifethreatening bleeding. Your health care professional will avoid D&C in the following situations, except when absolutely necessary:
Pelvic infection: If you have an infection involving the reproductive organs, there is a chance the surgical instruments that will enter the vagina and cervix can carry the bacteria from your vagina or cervix into your uterus. There is also an increased risk of injury to infected tissue. For these reasons, the doctor may prefer to wait until after the infection is cleared up with antibiotics before performing the D&C. Blood clotting disorders: Doctors depend on the body's natural ability to clot to stop bleeding after curettage. Women with certain blood disorders are usually not given this surgery. Serious medical problems: Heart and lung disease, for example, can make general, and sometimes local, anesthesia more risky.
Hemorrhage: Heavy bleeding is rare, but it can happen if an instrument injures the walls of the uterus. It also can occur if an undetected fibroid is cut during curettage. Infection: There is always a slight possibility of infection once instruments are inserted into the uterus. Most infections can be easily cured with antibiotics. Perforated uterus: This complication, though rare, is more common in women who have a uterine infection at the time of the procedure, in elderly postmenopausal women, and if the procedure is being done for a miscarriage. If the doctor suspects this condition has developed, the patient may be asked to stay in the hospital for observation or further surgery. Asherman syndrome: This complication is rare and involves the formation of scar tissue in the uterus, caused by aggressive scraping or abnormal reaction to the scraping. Thick scars can result, which can fill up the uterus completely. This can lead to infertility and cessation of menstrual periods. Missed disease: Since the procedure cannot completely remove all the endometrium (lining tissue of the uterus), there is a chance that disease could go undetected. This is why the procedure is seldom done without a hysteroscopy (examination of the uterine lining using an instrument that allows direct visualization ).
Dilation and Curettage Preparation Depending on the type of anesthesia used, the doctor's instructions before a D&C will most likely include the following:
In fact, D&C is no longer performed as commonly as it was even a decade ago, thanks to advances in diagnosis (for example, ultrasound and hysteroscopy) and nonsurgical hormonal (for example, oral contraceptives) and antihormonal therapies. Dilation and Curettage Risks and Complications The following are risk factors of dilation and curettage:
Avoid unnecessary drugs: A few days before your D&C, stop taking drugs such as aspirin, which can cause increased risk of bleeding, and any over-the-counter medications, such as cold medication and laxatives. Avoid alcohol and tobacco use. Many surgeons now recommend the patient stop taking any herbal supplements at least two weeks before surgery. Talk with the doctor about all medications you take. Chronic conditions: The doctor will most likely want the patient's other medical problems stabilized prior to the surgery. For example, if the patient has uncontrolled high blood pressure, she may be put on a strict treatment plan in or out of the hospital to improve blood pressure. This is important to avoid any unnecessary complications during the D&C procedure. Eating and drinking: The doctor will also instruct the patient not to eat or drink for 12 hours before your D&C if it is done under general anesthesia (the patient is
completely asleep), or for 8 hours before a local or regional (for example, spinal anesthesia, just the lower portion of your body is numbed and you have no feeling) is used. Preliminary tests: On the day before or day of the procedure, the doctor may want to obtain certain routine blood, urine, and other tests to be sure no medical problems have been missed
10 minutes. If the patient is under local anesthesia, she may experience crampy discomfort caused by stretching of the cervical muscles to accommodate the rods. Another method being used with increasing frequency is to insert laminaria tents (cigaretteshaped pieces of a special dried seaweed) into the cervix 8-20 hours before the procedure. The laminaria absorb water from the tissues and swell up, slowly distending and dilating the cervical canal. This is less traumatic than using the metal dilators. Hysteroscopy and curettage (the second step): After dilation, the doctor holds the vagina open again with the speculum. The doctor may also reach into the cervix with a tiny spoon to obtain a specimen of the cervical lining. At this point, the hysteroscope is usually inserted into the uterus so that the doctor may look at the inside of the uterus. The doctor may see fibroids, polyps, or overgrowths of the endometrium. At that time, instruments may be inserted through the hysteroscope and biopsy, or removal, of the fibroids, polyps, or endometrial overgrowths may be accomplished.
During the Dilation and Curettage Procedure Anesthesia
Local anesthesia: If the patient has a local anesthetic, she will lie on your back in the standard pelvic examination position: legs apart and the knees drawn up. The doctor will insert an instrument called a speculum into the vagina to hold the vagina wall apart. The doctor or assistant will then clean the inner and outer vagina, including the cervix, with a cleaning solution. The doctor will then steady the cervix with a clamp and inject a local anesthetic into the cervix on either side. This is called a paracervical block and relieves pain from the dilating of the cervix. It does not numb any of the rest of the body. Spinal anesthesia: A needle is placed in the lower back, usually while the patient is sitting up. Anesthetic is injected through this needle into the spinal fluid that surrounds the spinal cord. This causes numbness usually from the level of the belly button on down. The anesthesia wears off in 1-3 hours. General anesthesia: If general anesthesia is given, the patient will not be aware of anything including the cleaning step, after the patient loses consciousness. The patient will lie on the table with an anesthesiologist or nurse anesthetist at the head. The paitent may be given an injection of medication to assist in relaxing the patient and to dry up any oral secretions. The patient will then receive an intravenous fast-acting anesthetic and immediately fall asleep for the procedure and the patient's breathing will be monitored.
The doctor will now place a slightly longer and larger curette through the dilated cervix and up into the uterus. This is a metal loop on the end of a long, thin handle. With steady, gentle strokes, the doctor will scrape or suction the uterine wall. This tissue is sent to the lab for analysis. When the curettage is completed, the instruments are removed. If under local anesthesia, the patient will probably experience a tugging sensation deep in the abdomen as the curetting is performed. If this is too painful, the patient should tell the doctor, who may then order pain medicine. The entire procedure, including curettage takes about 20 minutes. At the end, the patient may have cramps that may last about 30 minutes; however, some women experience cramps for a much longer period of time.
After the Dilation and Curettage Procedure
Dilation (the first step): While grasping the cervix with a clamp, the doctor will pass a thin, flexible piece of metal called a sound to determine the depth and angle of the uterus. These measurements allow the doctor to know how far into the uterus the curette can be safely inserted. The usual method of dilation is to insert a thin, smooth metal rod gently along the vaginal canal and up into the tiny cervical opening. The rod is left in place for a moment, then withdrawn and replaced by a slightly larger rod. This process is repeated until the cervix has expanded to about the width of a finger. This method takes about
The recovery time is generally short following a D&C. Cramps, similar to menstrual cramps, will probably be the patient's strongest sensation immediately after a D&C. Although most women experience cramps for less than an hour, some women may have cramps for a day or more. The patient may also have some light bleeding for several days. The patient will most likely be placed in the recovery room immediately after the procedure. Most hospitals and outpatient clinics will keep the patient for an hour or
until she is fully awake. The patient will need to arrange for a ride home. It is suggested that the patient not drive for at least 24 hours after anesthesia. This is recommended even after a sedative/local anesthesia because side effects of these drugs can temporarily impair the coordination and response time. Naproxen or ibuprofen are usually given for relief from cramping. Narcotics are seldom, if ever, needed for the pain following the D&C.
When to Seek Medical Care Call the doctor immediately if you develop any of the following symptoms:
Fever (more than 100.4 F or 38 C) Severe persistent pain or cramps not relieved by ibuprofen or naproxen Prolonged or heavy bleeding (more than 6 hours, or requiring a change of sanitary pads several times in 1 hour) A foul-smelling discharge from the vagina
If you cannot reach your doctor about any of the problems, go to a hospital emergency department. If you become lightheaded or pass out, you should have someone take you to an emergency department because this may indicate excess blood loss. If you feel very ill, have a high fever, or severe abdominal pain, it may be best to go directly to an emergency department by EMS. Dilation and Curettage Follow-up After a D&C, the paient will generally get a list of instructions with the following suggestions:
Avoid intercourse for 2 weeks. The dilated cervix needs a chance to shrink back to normal size. Until this time, bacteria can easily get into the uterus and cause infection. Use only sanitary pads for bleeding. Avoid tampons for at least 2 weeks. Do not use douches. Be sure to return for the follow-up visit with the doctor. At this time, the doctor can discuss all lab reports on your tissue samples. The doctor will also want to examine you for any signs of infection and to make sure your cervix has returned to normal size.
Vous aimerez peut-être aussi
- Glossary of Immune System TermsDocument5 pagesGlossary of Immune System Termsneleh grayPas encore d'évaluation
- Physical Assessment Guide of Head-To-ToeDocument9 pagesPhysical Assessment Guide of Head-To-Toeneleh gray100% (2)
- Fluid & Electrolyte Imbalance/ DehydrationDocument7 pagesFluid & Electrolyte Imbalance/ Dehydrationneleh grayPas encore d'évaluation
- ncm105 /mental HealthDocument8 pagesncm105 /mental Healthneleh grayPas encore d'évaluation
- Fluid & Electrolyte Imbalance/ DehydrationDocument7 pagesFluid & Electrolyte Imbalance/ Dehydrationneleh grayPas encore d'évaluation
- Key Areas of ResponsibilityDocument2 pagesKey Areas of Responsibilityneleh grayPas encore d'évaluation
- Vital Signs TableDocument5 pagesVital Signs Tableneleh grayPas encore d'évaluation
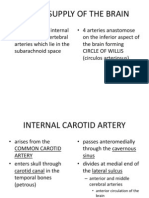
- Blood Supply of The BrainDocument11 pagesBlood Supply of The Brainneleh grayPas encore d'évaluation
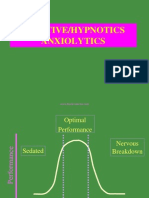
- An Xy Olitics HypnoticsDocument59 pagesAn Xy Olitics Hypnoticsneleh grayPas encore d'évaluation
- Anxiolytic DrugsDocument60 pagesAnxiolytic Drugsneleh grayPas encore d'évaluation
- Rib, Fractures: Background: Thoracic Trauma Often Involves Multiple Organ Systems and Several AnatomicDocument24 pagesRib, Fractures: Background: Thoracic Trauma Often Involves Multiple Organ Systems and Several Anatomicneleh grayPas encore d'évaluation
- Fundamentals of Nursing NotesDocument11 pagesFundamentals of Nursing Notesneleh grayPas encore d'évaluation
- Fundamentals of NursingDocument3 pagesFundamentals of Nursingneleh grayPas encore d'évaluation
- Feeding Via Gastric GavageDocument3 pagesFeeding Via Gastric Gavageneleh gray0% (1)
- Feeding Via Gastric GavageDocument3 pagesFeeding Via Gastric Gavageneleh gray0% (1)
- Broken Rib SymptomsDocument12 pagesBroken Rib Symptomsneleh grayPas encore d'évaluation
- Parotid GlandDocument2 pagesParotid Glandneleh grayPas encore d'évaluation
- Fundamentals of NursingDocument12 pagesFundamentals of Nursingneleh grayPas encore d'évaluation
- Fundamentals of NursingDocument12 pagesFundamentals of Nursingneleh grayPas encore d'évaluation
- Stages of Labor Nursing ConsiderationsDocument5 pagesStages of Labor Nursing Considerationsneleh gray100% (2)
- Abortion CaseDocument41 pagesAbortion Casekaycee_delacruz60% (5)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Negotiation Homework AssignmentDocument3 pagesNegotiation Homework AssignmentEunice Lourenço TanganePas encore d'évaluation
- Evelyn Arizpe - Teresa Colomer - Carmen Martínez-Roldán - Visual Journeys Through Wordless Narratives - An International Inquiry With Immigrant Children and The Arrival-Bloomsbury Academic (2014)Document290 pagesEvelyn Arizpe - Teresa Colomer - Carmen Martínez-Roldán - Visual Journeys Through Wordless Narratives - An International Inquiry With Immigrant Children and The Arrival-Bloomsbury Academic (2014)Lucia QuirogaPas encore d'évaluation
- Practical Econometrics Data Collection Analysis and Application 1st Edition Hilmer Test BankDocument27 pagesPractical Econometrics Data Collection Analysis and Application 1st Edition Hilmer Test Bankdavidhallwopkseimgc100% (28)
- PostmanPat Activity PackDocument5 pagesPostmanPat Activity PackCorto Maltese100% (1)
- Comparison of The EC-GMP Guide Part I With The SFDA-GMP Guideline For Chinese CompaniesDocument7 pagesComparison of The EC-GMP Guide Part I With The SFDA-GMP Guideline For Chinese Companiesrambabukomati472Pas encore d'évaluation
- Bilge Günsel TEL531E Detection and Estimation Theory W #1-2Document25 pagesBilge Günsel TEL531E Detection and Estimation Theory W #1-2ahmetPas encore d'évaluation
- Group Screening Test, English 6Document4 pagesGroup Screening Test, English 6Jayson Alvarez MagnayePas encore d'évaluation
- PmtsDocument46 pagesPmtsDhiraj ZanzadPas encore d'évaluation
- Causal Relationships WorksheetDocument2 pagesCausal Relationships Worksheetledmabaya23Pas encore d'évaluation
- Implementasi Sistem Pengenalan Candi Kecil Di Yogyakarta Menggunakan BerbasisDocument7 pagesImplementasi Sistem Pengenalan Candi Kecil Di Yogyakarta Menggunakan BerbasisRivan AuliaPas encore d'évaluation
- Intercostal Drainage and Its ManagementDocument36 pagesIntercostal Drainage and Its ManagementAnusha Verghese67% (3)
- Siemens 6SL31622AA000AA0 CatalogDocument20 pagesSiemens 6SL31622AA000AA0 CatalogIrfan NurdiansyahPas encore d'évaluation
- 2018-3-27 MIDAS Civil Presentation Curved BridgesDocument57 pages2018-3-27 MIDAS Civil Presentation Curved BridgesShishir Kumar NayakPas encore d'évaluation
- Azure Arc DoccumentDocument143 pagesAzure Arc Doccumentg.jithendarPas encore d'évaluation
- Jazz - Installing LED DRLsDocument16 pagesJazz - Installing LED DRLsKrishnaPas encore d'évaluation
- Salon Building Guidelines PDFDocument8 pagesSalon Building Guidelines PDFtsnie toPas encore d'évaluation
- Minuto hd8761Document64 pagesMinuto hd8761Eugen Vicentiu StricatuPas encore d'évaluation
- EASA Part-66 Module 17 QBDocument53 pagesEASA Part-66 Module 17 QBFaisal Ahmed Newon80% (5)
- Python Versus Matlab: Examples in Civil EngineeringDocument32 pagesPython Versus Matlab: Examples in Civil EngineeringNiranjanAryan100% (1)
- Linic - by SlidesgoDocument84 pagesLinic - by SlidesgoKhansa MutiaraHasnaPas encore d'évaluation
- Heroic Tales Core Rules 1.1.0Document33 pagesHeroic Tales Core Rules 1.1.0Melobajoya MelobajoyaPas encore d'évaluation
- Industrial Marketing Module 2Document32 pagesIndustrial Marketing Module 2Raj Prixit RathorePas encore d'évaluation
- Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale Evaluation Subjective: Noc: NIC: Fluid ManagementDocument10 pagesCues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale Evaluation Subjective: Noc: NIC: Fluid ManagementSkyla FiestaPas encore d'évaluation
- SOP For Production DepartmentDocument5 pagesSOP For Production DepartmentDaniel SusantoPas encore d'évaluation
- 06 Renr5908 08 01 All PDFDocument108 pages06 Renr5908 08 01 All PDFFrancisco Ospino Arrieta100% (2)
- Plasterboard FyrchekDocument4 pagesPlasterboard FyrchekAlex ZecevicPas encore d'évaluation
- Design and Fabrication of Light Electric VehicleDocument14 pagesDesign and Fabrication of Light Electric VehicleAshish NegiPas encore d'évaluation
- Youth and Moral ValuesDocument6 pagesYouth and Moral ValuesAlka SinghPas encore d'évaluation
- AWANA Handbook 2010-2011Document8 pagesAWANA Handbook 2010-2011carriepratchard100% (1)
- Boomer L2 D - 9851 2586 01Document4 pagesBoomer L2 D - 9851 2586 01Pablo Luis Pérez PostigoPas encore d'évaluation