Académique Documents
Professionnel Documents
Culture Documents
Appendix A. THE MEDICAL HISTORY (For New Patient) : Immunizations Injuries Broken Bones/fractures, Sutured Lacerations
Transféré par
Piet Pogen Poel0 évaluation0% ont trouvé ce document utile (0 vote)
367 vues1 pagehistory taking
Titre original
Medical History
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documenthistory taking
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
367 vues1 pageAppendix A. THE MEDICAL HISTORY (For New Patient) : Immunizations Injuries Broken Bones/fractures, Sutured Lacerations
Transféré par
Piet Pogen Poelhistory taking
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 1
Appendix A.
THE MEDICAL HISTORY (for new patient)
I. Chief Complaint -- The chief complaint should include the presenting problem/concern in the patients' own words, accompanied by the duration of the complaint. II. History of Present Illness -- In addition to providing a detailed and thorough discussion of the chief complaint, this section should also provide a "thumbnail sketch" of the patient and his/her significant underlying medical problems. It is often quite useful to include patient age, sex, race, occupation, and potentially relevant underlying chronic diseases in the history of present illness. III. Past Medical History A. Allergies --This section should discuss briefly all allergies, including the prior reaction to each allergin (i.e., "rash"): Medication, Foods, Dust, pollen, and plants, Animals B. Current Medications -- Both prescription and nonprescription medications with indications and dates (such as vitamins, analgesics, etc.), should be discussed in this section C. Birth and Development D. Communicable Diseases E. Immunizations F. Injuries Broken bones/fractures, Sutured lacerations G. Surgery -- This section should include dates, procedures, locations, and complications of the procedures (if any) H. Hospitalizations -- All discussed hospitalizations should include dates, illnesses, durations, and hospital locations I. Past Medical Care -- Please include current physicians and the dates the patient was last seen by health care professionals J. Occupation Exposures -- Please include exposures to dusts, heavy metals, radioactivity, asbestos, etc. incurred because of employment and hobbies K. Radiation Exposure -- Be sure to include exposure to therapeutic radiation L. Smoking History M. Alcohol Intake N. Chronic Diseases O. Miscellaneous P. Family History--This section should include data pertaining to the significant illnesses (both past and present) of the genetically related relatives of the patient, and should utilize genealogy-tree format when appropriate. Q. Social History--Please include marital/family background, living arrangements, support systems, education, occupational background, religious affiliations, hobbies/other interests, etc. Also, briefly discuss the daily routine of the patient along with a dietary history, sleep habits, exercise, advanced directives. Review the use of seat belts and sunblock. Ask about guns in the home and smoke detectors) R. Medical Screening Tests (PPD skin test, Chest X-ray, Cholesterol, PSA (male), Pap smear (female), Self-breast exam (female), Mammogram (female), Tetanus, Colonoscopy)
Refer to Review of Systems material which follows in Appendix B to complete the patient history. Also see the Sample Medical History handout for a good example of a complete patient write-up.
Vous aimerez peut-être aussi
- The Yale Way - New Patient PresentationsDocument9 pagesThe Yale Way - New Patient PresentationsAndrew McGowanPas encore d'évaluation
- How To Make An Oral Case Presentation To Healthcare ColleaguesDocument5 pagesHow To Make An Oral Case Presentation To Healthcare ColleaguesYuliana Citra AnggraeniPas encore d'évaluation
- DR Ruvaiz Haniffa: Dept. Family Medicine, Faculty of Medicine, University of Kelaniya 25 September 2006Document17 pagesDR Ruvaiz Haniffa: Dept. Family Medicine, Faculty of Medicine, University of Kelaniya 25 September 2006Nipun M. DasanayakePas encore d'évaluation
- Components of The Comprehensive History and Pe Write UpDocument2 pagesComponents of The Comprehensive History and Pe Write Upnewbie2kPas encore d'évaluation
- Case Write Up TemplateDocument2 pagesCase Write Up TemplateMohd HadzriePas encore d'évaluation
- How To Present Cases (Short File) PDFDocument3 pagesHow To Present Cases (Short File) PDFAmjad SaudPas encore d'évaluation
- Physical Examination Form: Medications AllergiesDocument4 pagesPhysical Examination Form: Medications AllergiesIris Ann PhillipsPas encore d'évaluation
- CSC Proforma - FeverDocument6 pagesCSC Proforma - Fever127 Shruthik Patel ThotaPas encore d'évaluation
- Complications of CABGDocument38 pagesComplications of CABGpriyathasanPas encore d'évaluation
- Internal Medicine 5th MidtermDocument13 pagesInternal Medicine 5th MidtermIashdip iashdipPas encore d'évaluation
- 32 AN Guidelines H&PDocument3 pages32 AN Guidelines H&Pabu alauon abed almohsenPas encore d'évaluation
- The Art Og History TakingDocument3 pagesThe Art Og History TakinglianazulakPas encore d'évaluation
- Scare 2018 GuidelinesDocument2 pagesScare 2018 Guidelinesewqe100% (1)
- Title 1 Key Words 2 3a: SCARE 2018 Checklist Topic Item Checklist Item Description NumberDocument5 pagesTitle 1 Key Words 2 3a: SCARE 2018 Checklist Topic Item Checklist Item Description NumberAmatystPas encore d'évaluation
- EpidemiologyDocument20 pagesEpidemiologyho laPas encore d'évaluation
- Introduction To Oral Manifestations of Systemic DiseasesDocument8 pagesIntroduction To Oral Manifestations of Systemic DiseasesVitória SilvaPas encore d'évaluation
- PediatrichpDocument7 pagesPediatrichpSowjanyaPas encore d'évaluation
- Scare - 2020 - Checklist SURGICAL CASES REPORTDocument7 pagesScare - 2020 - Checklist SURGICAL CASES REPORTBeni Bolng100% (1)
- History Taking - OverviewDocument5 pagesHistory Taking - Overviewأبو حنيفةPas encore d'évaluation
- Collection of Subjective Data Throught InterviewDocument3 pagesCollection of Subjective Data Throught InterviewChuche Marie TumarongPas encore d'évaluation
- (2011!06!29) CMED The Medical Writeup HandoutDocument19 pages(2011!06!29) CMED The Medical Writeup HandoutAdel TaradjiPas encore d'évaluation
- Appendix B-Guidelines For Writing Patient Case Report ManuscriptsDocument5 pagesAppendix B-Guidelines For Writing Patient Case Report ManuscriptsMeriam HalimPas encore d'évaluation
- Health HistoryDocument8 pagesHealth HistoryAhmed MohamedPas encore d'évaluation
- Outline For Pediatric History and Physical Examination History I. Presenting Complaint (Informant/Reliability of Informant)Document4 pagesOutline For Pediatric History and Physical Examination History I. Presenting Complaint (Informant/Reliability of Informant)Hawkar SaeedPas encore d'évaluation
- PCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17Document82 pagesPCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17anon_925247980Pas encore d'évaluation
- Taking A Medical HistoryDocument5 pagesTaking A Medical Historyロシアの医者Pas encore d'évaluation
- History Taking OverviewDocument5 pagesHistory Taking OverviewSutirtha RoyPas encore d'évaluation
- GENERAL WARD Sample Case PresDocument4 pagesGENERAL WARD Sample Case PresCons Tan TinoPas encore d'évaluation
- EPIDEMIOLOGYDocument6 pagesEPIDEMIOLOGYKisha BethelPas encore d'évaluation
- Dictation Discharge Summary TemplateDocument19 pagesDictation Discharge Summary TemplateBobby ReddyPas encore d'évaluation
- Guide To The Comprehensive Pediatric H and P Write Up PDFDocument16 pagesGuide To The Comprehensive Pediatric H and P Write Up PDFnanaPas encore d'évaluation
- Peds History and Physical ExamDocument3 pagesPeds History and Physical Examchris100% (1)
- Formal Patient Case Presentation FormatDocument2 pagesFormal Patient Case Presentation FormatMichael ChangPas encore d'évaluation
- Comprehensive Health HistoryDocument4 pagesComprehensive Health Historyakoeljames8543Pas encore d'évaluation
- SCARE Guideline ChecklistDocument3 pagesSCARE Guideline ChecklistSylviany El Novita100% (1)
- SYSTEM ASSESSMENT GuideDocument5 pagesSYSTEM ASSESSMENT Guidejonathan liboonPas encore d'évaluation
- APPE Requirement Case Presentations1Document2 pagesAPPE Requirement Case Presentations1Omnia El HossienyPas encore d'évaluation
- Case History - Morbi & VitaeDocument2 pagesCase History - Morbi & VitaeAhmad SobihPas encore d'évaluation
- Case Study Format - PGTCNDocument2 pagesCase Study Format - PGTCNFitz JaminitPas encore d'évaluation
- The Comprehensive Health HistoryDocument50 pagesThe Comprehensive Health HistoryAlbert B. Balace100% (1)
- Intra - Operative NursingDocument8 pagesIntra - Operative NursingClaire SoletaPas encore d'évaluation
- Patient Assessment FormDocument8 pagesPatient Assessment Formjerickpacia2000Pas encore d'évaluation
- Module 3 HA Comprehensive Health History 1Document16 pagesModule 3 HA Comprehensive Health History 1Rosalinda LacuestaPas encore d'évaluation
- PAL Pack 2011 KI UpdateDocument41 pagesPAL Pack 2011 KI UpdateLuveon TangPas encore d'évaluation
- Mader's Reptile and Amphibian Medicine and Surgery, 3rd Edition - VetBooksDocument5 pagesMader's Reptile and Amphibian Medicine and Surgery, 3rd Edition - VetBooksazuvillegasduque1Pas encore d'évaluation
- Nursing Health History FormatDocument7 pagesNursing Health History FormatJasmine PoncePas encore d'évaluation
- Nursing Health History FormatDocument7 pagesNursing Health History Formatgeraldine suarezPas encore d'évaluation
- Guidelines For Complete SOAP2Document2 pagesGuidelines For Complete SOAP2Betsy Brown Byersmith100% (1)
- ASSESSMENT of CHILDBEARING MOTHER WordDocument4 pagesASSESSMENT of CHILDBEARING MOTHER WordLorel Faith ToradaPas encore d'évaluation
- Oral and Maxillofacial SurgeryDocument6 pagesOral and Maxillofacial Surgerysunaina chopraPas encore d'évaluation
- His LabDocument3 pagesHis Labnathalie kaye salinasPas encore d'évaluation
- Rle 106 ReqDocument10 pagesRle 106 Reqbeer_ettaaPas encore d'évaluation
- History Taking and PEDocument30 pagesHistory Taking and PEMelissa Salayog100% (1)
- Growth Factors and Wound Healing 1997Document374 pagesGrowth Factors and Wound Healing 1997Vo Ha Phuong NguyenPas encore d'évaluation
- 1.2 - Inquiry 讲课稿 2020Document11 pages1.2 - Inquiry 讲课稿 2020mirabel IvanaliPas encore d'évaluation
- Study Notes PediatricsDocument64 pagesStudy Notes PediatricsSteam LcPas encore d'évaluation
- PEDIA 1 The Pediatric History and Physical Exam HandoutDocument16 pagesPEDIA 1 The Pediatric History and Physical Exam HandoutRyan Loyd MarquezPas encore d'évaluation
- FPD - LEC.SAS.5 Chart Medical Dental History Consent FormDocument11 pagesFPD - LEC.SAS.5 Chart Medical Dental History Consent FormabegailnalzaroPas encore d'évaluation
- SemiologyDocument13 pagesSemiologyAndrei BulgariuPas encore d'évaluation
- Patient History: Prof. Hoda ElguindyDocument14 pagesPatient History: Prof. Hoda Elguindyyahia salah100% (1)
- Dehydration ProcessDocument7 pagesDehydration ProcessSunil BarnwalPas encore d'évaluation
- Hyper Nat Remi ADocument2 pagesHyper Nat Remi APiet Pogen PoelPas encore d'évaluation
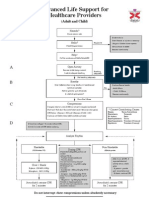
- Sudden Cardic ArrestDocument17 pagesSudden Cardic ArrestPiet Pogen PoelPas encore d'évaluation
- Airway Management - Supraglottic Airway PDFDocument4 pagesAirway Management - Supraglottic Airway PDFPiet Pogen PoelPas encore d'évaluation
- Airway Management - Supraglottic Airway PDFDocument4 pagesAirway Management - Supraglottic Airway PDFPiet Pogen PoelPas encore d'évaluation
- Basic (Level IV) Trauma Facility CriteriaDocument6 pagesBasic (Level IV) Trauma Facility CriteriaPiet Pogen PoelPas encore d'évaluation
- International Trauma Life Support Takes Trauma Training Online With New Itls Etrauma ProgramDocument2 pagesInternational Trauma Life Support Takes Trauma Training Online With New Itls Etrauma ProgramPiet Pogen PoelPas encore d'évaluation
- Flow ChartDocument4 pagesFlow ChartPiet Pogen PoelPas encore d'évaluation
- GelderblomDocument16 pagesGelderblomPiet Pogen PoelPas encore d'évaluation
- Seeking Patients Informed Consent Ethical ConsiderationDocument18 pagesSeeking Patients Informed Consent Ethical ConsiderationPiet Pogen PoelPas encore d'évaluation
- Flow ChartDocument4 pagesFlow ChartPiet Pogen PoelPas encore d'évaluation
- BLS Adult and ChildDocument1 pageBLS Adult and ChildPiet Pogen PoelPas encore d'évaluation
- ALS Adult and ChildDocument1 pageALS Adult and ChildPiet Pogen PoelPas encore d'évaluation
- Anamnesis Form: Name Dose Regularity How Long Have You Been Taking ItDocument3 pagesAnamnesis Form: Name Dose Regularity How Long Have You Been Taking ItĐeŋýzař Đ ZòįđýckPas encore d'évaluation
- Ibsen Timeline and BriefDocument59 pagesIbsen Timeline and BriefArt Levine, Mental Health Inc.Pas encore d'évaluation
- Documentation of Red Flags by Physical Therapists For Patients With Low Back PainDocument8 pagesDocumentation of Red Flags by Physical Therapists For Patients With Low Back PainBwizerPas encore d'évaluation
- Oet 2.0 Writing Practice and Exercises Book For Nurses Vol 2Document184 pagesOet 2.0 Writing Practice and Exercises Book For Nurses Vol 2Dandlers MurrayPas encore d'évaluation
- Test Bank For Lehnes Pharmacology For Nursing Care 10th Edition by BurchumDocument33 pagesTest Bank For Lehnes Pharmacology For Nursing Care 10th Edition by Burchumseesaw.insearchd8k4100% (46)
- Nursing Therapy's NotesDocument121 pagesNursing Therapy's NotesVerline Santiong V. JoanPas encore d'évaluation
- Hippocrates - W.hs. Jones 2.ciltDocument416 pagesHippocrates - W.hs. Jones 2.ciltmahmut sansalPas encore d'évaluation
- Hospital ManualDocument49 pagesHospital ManualsubiPas encore d'évaluation
- Alergia Alimentar - Diagnóstico Clínico e Laboratorial, Tratamento e PrevençãoDocument27 pagesAlergia Alimentar - Diagnóstico Clínico e Laboratorial, Tratamento e PrevençãoBianca FonsecaPas encore d'évaluation
- Rosh Review 11Document6 pagesRosh Review 11Sarwar BaigPas encore d'évaluation
- Sgu CompendiumDocument44 pagesSgu Compendiumdudeman2332Pas encore d'évaluation
- Medicine Lecture 1 - History Taking (Colored)Document4 pagesMedicine Lecture 1 - History Taking (Colored)miguel cuevas100% (2)
- Student Prep - Basics of A SOAP Note-2Document4 pagesStudent Prep - Basics of A SOAP Note-2lovefifteenPas encore d'évaluation
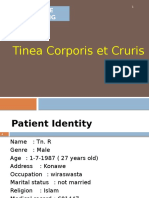
- Tinea Corporis Et CrurisDocument24 pagesTinea Corporis Et CrurisSamuel WilliamsPas encore d'évaluation
- Case Report: Systemic Lupus ErythematosusDocument32 pagesCase Report: Systemic Lupus ErythematosusdesmyyPas encore d'évaluation
- Chapter 3 Client PresentationDocument4 pagesChapter 3 Client PresentationEllePeiPas encore d'évaluation
- CV MaryDocument4 pagesCV MaryKoros ComedyPas encore d'évaluation
- CPO Sample Quiz - Questions and Answers PDFDocument25 pagesCPO Sample Quiz - Questions and Answers PDFSumant YadavPas encore d'évaluation
- OET Online Test 2Document9 pagesOET Online Test 2Bünyamin EmerPas encore d'évaluation
- Morning Report: Pulmonology and Respiratory Medicine Medical Faculty of Sebelas Maret University 2021Document30 pagesMorning Report: Pulmonology and Respiratory Medicine Medical Faculty of Sebelas Maret University 2021debby nirmasariPas encore d'évaluation
- OET Writing 20.1 - 30.2 Case Notes - Mobile VersionDocument72 pagesOET Writing 20.1 - 30.2 Case Notes - Mobile VersionjykaPas encore d'évaluation
- Uml Diagram For Hospital Management SystemDocument34 pagesUml Diagram For Hospital Management SystemVani Garikipati100% (1)
- Nursing Process EBN Format OB PEDIADocument5 pagesNursing Process EBN Format OB PEDIAAnn Nicole UlitPas encore d'évaluation
- DocumentationDocument16 pagesDocumentationAnonymous fj68Ms100% (1)
- 4 5920474042279658151Document618 pages4 5920474042279658151Sasha Khoma100% (3)
- Documentation and Nurse Practitioner RoleDocument5 pagesDocumentation and Nurse Practitioner RoleEnerolisa ParedesPas encore d'évaluation
- Format of Internship Report For Clinical PsychologyDocument10 pagesFormat of Internship Report For Clinical PsychologyAdeel AizadPas encore d'évaluation
- HistoryDocument5 pagesHistoryrawan.sharari0911Pas encore d'évaluation
- Clinical Pharmacy - Simple Notes PDFDocument186 pagesClinical Pharmacy - Simple Notes PDFsmart hussain86% (79)
- Medical QuestionnairesDocument1 pageMedical QuestionnairesTony DawaPas encore d'évaluation