Académique Documents
Professionnel Documents
Culture Documents
Abdominal Pain
Transféré par
Reiciel Joy GombioDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Abdominal Pain
Transféré par
Reiciel Joy GombioDroits d'auteur :
Formats disponibles
Abdominal pain is pain that is felt in the abdomen.
The abdomen is an anatomical area that is bounded by the lower margin of the ribs and diaphragm above, the pelvic bone (pubic ramus) below, and the flanks on each side. Although abdominal pain can arise from the tissues of the abdominal wall that surround the abdominal cavity (such as the skin and abdominal wall muscles), the term abdominal pain generally is used to describe pain originating from organs within the abdominal cavity. Organs of the abdomen include the stomach, small intestine, colon, liver, gallbladder, spleen, and pancreas.
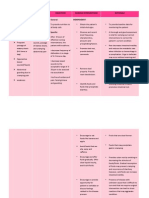
Abdominal Pain Nursing Care Plan - Acute Pain Nursing Assessment:
1. General: Anorexia and malaise, fever, tachycardia, diaphoresis, pale, abdominal rigidity, failure to issue a rectal feces or flatus, increased bowel sounds (early obstruction), decreased bowel sounds (advanced), retention of urination and leukocytosis. 2. Specific: Small intestine Weight, such as cramping abdominal pain, distension increased mild distension Nausea Vomiting: at the beginning containing food is not digested and kim; water and then vomit contains bile, black and faecal Dehydration Colon mild abdominal discomfort severe distension Vomiting latent faecal latent Dehydration: acidosis rarely
o o
Nursing Diagnosis and Nursing Intervention for Abdominal Pain Nursing Care Plan - Acute Pain Pain related to distention, rigidity Goal: pain is resolved or controlled Criteria for outcome: patients revealed a decrease discomfort; expressed pain at tolerable levels, indicating relaxed. Intervention:
Maintain bed rest in a comfortable position, do not support the knee. Assess the location, weight and type of pain Assess effectiveness and monitor side effects anlgesik; avoid morphine Provide a planned rest period. Review and recommend doing lathan active or passive range of motion every 4 hours. Change positions frequently and give her back rubbing and skin care. Auscultation bowel sounds; kekauan or notice increasing pain; give enema slowly when ordered. Give and recommend alternative pain relief measures.
Acute pain related to the accumulation of hard stool in the abdomen Goal: show pain has been reduced Expected Outcomes:
Relaxation techniques individually demonstrate effective to achieve comfort Maintaining the level of pain on a small scale Reported physical and psychological health Recognize factors and using measures to prevent pain Using action to reduce the pain with analgesics and non-analgesic appropriately
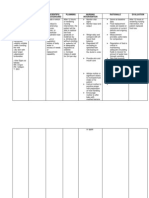
Nursing Interventions Acute Pain related to Constipation 1. Help the patient to focus more on the activity of the pain by doing penggalihan through television or radio. Rationale: The client can distract from pain. 2. Note that the elderly have increased sensitivity to the analgesic effects of opiates. Rational: Be careful in giving anlgesik opiates. 3. Consider the possibility of drug interactions in the elderly. Rational: Be careful in the provision of drugs in the elderly. 4. Ask the patient to assess pain or lack of comfort on a scale of 0-10 Rationale: Knowing the client's level of perceived pain 5. Use the pain flow sheet Rationale: Knowing the characteristics of pain 6. Perform a comprehensive pain assessment Rational: In order for the specific pain mngetahui 7. Instruct patient to meminformasikan on nurses if the pain-reducing achieved less Rationale: Nurses can perform appropriate action in addressing the client's pain 8. Give pain neighbor information Rational: In order for the patient does not feel anxious.
Nursing diagnosis: acute Pain related to Hyperperistalsis, prolonged diarrhea, skin and tissue irritation, perirectal excoriation, fissures, fistulas Possibly evidenced by Reports of colicky, cramping abdominal pain; referred pain Guarding or distraction behaviors, restlessness Facial mask of pain; self-focusing Desired Outcomes/Evaluation CriteriaClient Will Pain Level Report pain is relieved or controlled. Appear relaxed and able to sleep and rest appropriately. Nursing intervention with rationale: 1. Encourage client to report pain. Rationale: May try to tolerate pain rather than request analgesics. 2. Assess reports of abdominal cramping or pain, noting location, duration, and intensity (such as 010 scale). Investigate and report changes in pain characteristics. Rationale: Colicky intermittent pain occurs with Crohns disease. Predefecation pain frequently occurs in UC with urgency, wh ich may be severe and continuous. Changes in pain characteristics may indicate spread of disease or developing complications, such as bladder fistula, perforation, and toxic megacolon. 3. Note nonverbal cues, such as restlessness, reluctance to move, abdominal guarding, withdrawal, and depression. Investigate discrepancies between verbal and nonverbal cues. Rationale: Body language or nonverbal cues may be both physiological and psychological and may be used in conjunction with verbal cues to determine extent and severity of the problem. 4. Review factors that aggravate or alleviate pain. Rationale: May pinpoint precipitating or aggravating factors (e.g., stressful events, food intolerance) or identify developing complications. 5. Encourage client to assume position of comfort, such as knees flexed. Rationale: Reduces abdominal tension and promotes sense of control.
6. Provide comfort measures (e.g., back rub, reposition) and diversional activities. Rationale: Promotes relaxation, refocuses attention, and may enhance coping abilities. 7. Cleanse rectal area with mild soap and water (or wipes) after each stool and provide skin care with a moisture barrier ointment (e.g., A&D ointment, Sween ointment, karaya gel, Desitin, petroleum jelly, zinc oxide, dimethicone). Rationale: Protects skin from bowel acids, preventing excoriation. 8. Implement prescribed dietary modifications, for example, commence with liquids and increase to solid foods as tolerated. Rationale: Complete bowel rest can reduce pain and cramping. 9. Provide sitz bath, as appropriate. Rationale: Enhances cleanliness and comfort in the presence of perianal irritation and fissures. 10. Observe and record abdominal distension, increased temperature, and decreased BP. Rationale: May indicate developing intestinal obstruction from inflammation, edema, and scarring.
Vous aimerez peut-être aussi
- Wet Cell and Radial DeviceDocument21 pagesWet Cell and Radial DeviceChava Chavous100% (1)
- Vet Tech ExamDocument39 pagesVet Tech Examransingh100% (1)
- Laboratory Tests for Hemostasis EvaluationDocument5 pagesLaboratory Tests for Hemostasis EvaluationCMLPas encore d'évaluation
- NCP-fluid Volume DeficitDocument4 pagesNCP-fluid Volume DeficitChrissa Mae Aranilla MayoPas encore d'évaluation
- Tachycardia NCPDocument2 pagesTachycardia NCPRemita Hutagalung50% (4)
- Application of Roy TheoryDocument32 pagesApplication of Roy TheoryAnusha VerghesePas encore d'évaluation
- Internet Book of Critical Care (IBCC) : Rapid ReferenceDocument1 pageInternet Book of Critical Care (IBCC) : Rapid Referenceian porterPas encore d'évaluation
- Nursing Care Plan Rheumatoid ArthritisDocument4 pagesNursing Care Plan Rheumatoid ArthritisLighto RyusakiPas encore d'évaluation
- NCP - ConstipationDocument3 pagesNCP - ConstipationDaniel Dave KapunanPas encore d'évaluation
- SchistosomiasisDocument92 pagesSchistosomiasisIvan Juan75% (4)
- Nursing care plan for skin lesions, nutrition, and activity toleranceDocument3 pagesNursing care plan for skin lesions, nutrition, and activity toleranceElisa Kerr100% (1)
- NCP - Ineffective Airway ClearanceDocument2 pagesNCP - Ineffective Airway Clearancelarapatricia1215Pas encore d'évaluation
- NCP HemorrhoidDocument2 pagesNCP HemorrhoidJojo Malana100% (7)
- Article Dietschi VeenersDocument18 pagesArticle Dietschi VeenersRoberto PucPas encore d'évaluation
- Psychiatric Nursing Mastery Test Part 2Document16 pagesPsychiatric Nursing Mastery Test Part 2Rika MaePas encore d'évaluation
- Cues Nursing DX Objectives Nursing Interventions RationaleDocument5 pagesCues Nursing DX Objectives Nursing Interventions RationaleJamie IcabandiPas encore d'évaluation
- NCP HyperthermiaDocument6 pagesNCP HyperthermiaGrax DeePas encore d'évaluation
- NCP Ineffective Tissue PerfusionDocument2 pagesNCP Ineffective Tissue PerfusionYasminGianneDeOcampoBarizoPas encore d'évaluation
- NCP For Acute PainDocument2 pagesNCP For Acute PainEmman RamosPas encore d'évaluation
- NCP AppendicitisDocument5 pagesNCP AppendicitisElbert Kay SerranoPas encore d'évaluation
- Assessment Diagnosis Planning ImplementationDocument4 pagesAssessment Diagnosis Planning ImplementationMG PolvorosaPas encore d'évaluation
- Mod 5 Health TeachingDocument4 pagesMod 5 Health TeachingMabelle SorianoPas encore d'évaluation
- NCP Acute PainDocument1 pageNCP Acute PainFielMendozaPas encore d'évaluation
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityAl-Qadry NurPas encore d'évaluation
- NCPDocument4 pagesNCPJahmie RiveraPas encore d'évaluation
- Ineffective Breathing PatternDocument185 pagesIneffective Breathing PatternSusi LambiyantiPas encore d'évaluation
- Assist withambulation- Assist withactivities ofdaily living- To promotehealing- To promoteindependenceDocument2 pagesAssist withambulation- Assist withactivities ofdaily living- To promotehealing- To promoteindependenceDanielJosephLimPas encore d'évaluation
- Nursing Care PlanDocument11 pagesNursing Care Planaycee0316100% (1)
- Pneumo Hemoperitoneum Stab Wound Case StudyDocument7 pagesPneumo Hemoperitoneum Stab Wound Case StudyMari Jasmeen Estrada Noveda100% (1)
- Ineffective Airway Clearance Nursing Care PlanDocument2 pagesIneffective Airway Clearance Nursing Care Planrois romaPas encore d'évaluation
- Nursing Care Plan Process Analysis Planning and ImplementationDocument2 pagesNursing Care Plan Process Analysis Planning and ImplementationVanessa Prieto100% (2)
- VIGOCIDDocument2 pagesVIGOCIDKaren DamoPas encore d'évaluation
- Nursing Care Plan for Impaired Gas ExchangeDocument6 pagesNursing Care Plan for Impaired Gas ExchangePrincess Andrea Bulatao100% (1)
- NCP Making (Ulcerative Colitis & Crohn's Disease)Document2 pagesNCP Making (Ulcerative Colitis & Crohn's Disease)R Hornilla ArcegaPas encore d'évaluation
- NCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingDocument3 pagesNCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingCedie BarcaPas encore d'évaluation
- FractureDocument4 pagesFractureRaveen mayiPas encore d'évaluation
- Diarrhea Care PlanDocument2 pagesDiarrhea Care Planzepoli_zepoly6232100% (1)
- Pain NCP BillrothDocument2 pagesPain NCP BillrotharjayPas encore d'évaluation
- Care Plan ExampleDocument2 pagesCare Plan Exampleincess27100% (1)
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesPas encore d'évaluation
- Activity IntoleranceDocument2 pagesActivity IntoleranceDiane AbanillaPas encore d'évaluation
- Deficit)Document2 pagesDeficit)Lee DeePas encore d'évaluation
- CHD With NCPDocument10 pagesCHD With NCPJohanna Kirsten F. DaguioPas encore d'évaluation
- NCPDocument1 pageNCPanon-61963867% (3)
- A Nursing Care Plan VaDocument3 pagesA Nursing Care Plan VaArianne Paola QuindoyPas encore d'évaluation
- Bladder Infection Nursing CareDocument8 pagesBladder Infection Nursing CareJoseph Anthony Benitez VerzosaPas encore d'évaluation
- Compartment Syndrome NCP (PAIN)Document2 pagesCompartment Syndrome NCP (PAIN)eunica16Pas encore d'évaluation
- Acute PainDocument3 pagesAcute PainGerardeanne ReposarPas encore d'évaluation
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Drug StudyDocument7 pagesDrug Studykymsh_kimPas encore d'évaluation
- NCPDocument4 pagesNCPPrincess Camille ArceoPas encore d'évaluation
- Nursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDocument4 pagesNursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDaniel Garraton0% (1)
- Hyperthermia NCPDocument3 pagesHyperthermia NCPJayr DiazPas encore d'évaluation
- NCP MiDocument4 pagesNCP MiPitaca Madiam Annabehl PaulPas encore d'évaluation
- Final NCP AppendicitisDocument4 pagesFinal NCP AppendicitisCha Ry100% (1)
- Heart Perfusion Nursing CareDocument12 pagesHeart Perfusion Nursing CareSesinando Niez Quilao Jr.100% (1)
- NCP Alcoholic NeuropathyDocument5 pagesNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- NCP Anorexia NervosaDocument5 pagesNCP Anorexia NervosaJohn Ver Tolentino AdaoPas encore d'évaluation
- Nursing Priority Problem List for Fluid Volume ExcessDocument1 pageNursing Priority Problem List for Fluid Volume ExcessJackyleen Kate BenetuaPas encore d'évaluation
- Activity IntoleranceDocument2 pagesActivity Intoleranceayra_alegrePas encore d'évaluation
- Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocument8 pagesWhich It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranPas encore d'évaluation
- NCP Inactivity ToleranceDocument16 pagesNCP Inactivity ToleranceChrisTine M. MoralesPas encore d'évaluation
- Dehydration Nursing CareDocument2 pagesDehydration Nursing CareAdrian MallarPas encore d'évaluation
- Teaching Plan For DiarrheaDocument2 pagesTeaching Plan For DiarrheaSheila Nones50% (6)
- Dynastat: What Is in This LeafletDocument4 pagesDynastat: What Is in This LeafletBenj GilbuenaPas encore d'évaluation
- Signs and Symptoms Nursing Diagnosis Rationale Objective Nursing Intervention Rationale EvaluationDocument5 pagesSigns and Symptoms Nursing Diagnosis Rationale Objective Nursing Intervention Rationale EvaluationRemuelMagsinoPas encore d'évaluation
- NCP AppendicitisDocument2 pagesNCP AppendicitisSHAMUS DANIPas encore d'évaluation
- What Exactly Is LeukemiaDocument7 pagesWhat Exactly Is LeukemiaReiciel Joy GombioPas encore d'évaluation
- Anatomy CallangDocument2 pagesAnatomy CallangReiciel Joy GombioPas encore d'évaluation
- Anatomy and PhysiologyDocument2 pagesAnatomy and PhysiologyReiciel Joy GombioPas encore d'évaluation
- 4 Protozoans With Their DiseasesDocument2 pages4 Protozoans With Their DiseasesReiciel Joy GombioPas encore d'évaluation
- Abortion, Anc, and CS: Focus+ Lecture SeriesDocument24 pagesAbortion, Anc, and CS: Focus+ Lecture SeriesTianah davisPas encore d'évaluation
- Dasar Dasar VirologiDocument28 pagesDasar Dasar Virologiiif adwiyatu iffaPas encore d'évaluation
- Cannabis Phenolics and Their BioactivitiesDocument44 pagesCannabis Phenolics and Their BioactivitiesTomislav ĆurićPas encore d'évaluation
- A Novel Lymphocyte Transformation Test (LTT-MELISAR) For Lyme BorreliosisDocument8 pagesA Novel Lymphocyte Transformation Test (LTT-MELISAR) For Lyme Borreliosisdebnathsuman49Pas encore d'évaluation
- SwatiDocument97 pagesSwatiswati malikPas encore d'évaluation
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangPas encore d'évaluation
- Bulimia NervosaDocument17 pagesBulimia NervosaJheanAlphonsineT.Means100% (1)
- Biochemistry Aspect in Human Reproduction: Lastri Mei WinarniDocument19 pagesBiochemistry Aspect in Human Reproduction: Lastri Mei WinarniLastri Mei WinarniPas encore d'évaluation
- Bhs Inggris - Health and Nursing Related Vocabulary-1Document9 pagesBhs Inggris - Health and Nursing Related Vocabulary-1septynovitaPas encore d'évaluation
- Types of Feeding TubesDocument8 pagesTypes of Feeding TubesElda KuizonPas encore d'évaluation
- Epidemiology SlidesDocument30 pagesEpidemiology SlidesHongMingPas encore d'évaluation
- Primer: Gastro-Oesophageal Reflux DiseaseDocument23 pagesPrimer: Gastro-Oesophageal Reflux Diseasejcacia17Pas encore d'évaluation
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDocument5 pagesBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliPas encore d'évaluation
- Understanding Contraceptive Knowledge and Practices Among Breastfeeding WomenDocument286 pagesUnderstanding Contraceptive Knowledge and Practices Among Breastfeeding WomenAastha JainPas encore d'évaluation
- Cardiovascular Embryology StagesDocument109 pagesCardiovascular Embryology StagesBir Singh100% (1)
- Gtbr2016 Main TextDocument214 pagesGtbr2016 Main TextRaimundo Isidro MachavaPas encore d'évaluation
- PMO - Pasteurized Milk OrdinanceDocument340 pagesPMO - Pasteurized Milk OrdinanceTato G.k.Pas encore d'évaluation
- Joint Mobilization EnhancesDocument12 pagesJoint Mobilization EnhancesDavid BrunoPas encore d'évaluation
- Neuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrDocument24 pagesNeuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrdeepuphysioPas encore d'évaluation
- Third Quarter Summative Test No. 4 EnglishDocument3 pagesThird Quarter Summative Test No. 4 EnglishJoanaPas encore d'évaluation
- Bacterial ReproductionDocument12 pagesBacterial Reproductionchann.maahiPas encore d'évaluation
- Nina Rajan Pillai & Ors. Vs Union of India and Ors. On 13 May, 2011Document33 pagesNina Rajan Pillai & Ors. Vs Union of India and Ors. On 13 May, 2011Sanjayan KizhakkedathuPas encore d'évaluation
- 10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DDocument11 pages10 DOH Approved Herbal Medicine: Prepared By: Washington, Luis D. Student Nurse BSN 2H-DLuis WashingtonPas encore d'évaluation