Académique Documents
Professionnel Documents
Culture Documents
Tumor Immunology: M. Nagarkatti Teaching Objectives
Transféré par
99manu99Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Tumor Immunology: M. Nagarkatti Teaching Objectives
Transféré par
99manu99Droits d'auteur :
Formats disponibles
COURSE:
Medical Microbiology, PAMB 650/720 - Fall 2009
Lecture 21
Tumor Immunology
M. Nagarkatti Teaching Objectives: Introduction to Cancer Immunology Know the antigens expressed by cancer cells Understand the nature of immune response to tumors Study how cancers evade immune system Describe the approaches used in Immunotherapy
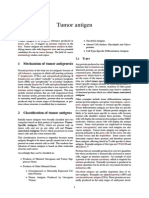
Malignant Transformation: The proliferation of normal cells is carefully regulated. However, such cells when exposed to chemical carcinogens, irradiation and certain viruses may undergo mutations leading to their transformation into cells that are capable of uncontrolled growth, producing a tumor or neoplasm. A tumor may be 1) Benign, if it is not capable of indefinite growth and the host survives. 2) Malignant, if the tumor continues to grow indefinitely and spreads (metastasizes), eventually killing the host. This uncontrolled growth may be due to upregulation of oncogenes (cancer-inducing genes) and/or downregulation of tumor suppressor genes (that normally inhibit tumor growth often by inducing cell death). Evidence for existence of an immune response against tumors The following criteria serve as evidence that tumors can elicit an immune response. 1. Certain tumors regress spontaneously (e.g., melanomas, neuroblastomas).suggesting an immunological response. 2. Tumors that have severe mononuclear cell infiltration have a better prognosis than those that lack it. 3. Some tumor metastases regress after removal of primary tumor which reduces the tumor load, thereby inducing the immune system to kill the residual tumor.. 4. Although chemotherapy leads to rejection of a large number of tumor cells, the few tumor cells that evade the action of the drugs can outgrow and kill the host. However, the immune system may be able to mount an attack against the few tumor cells that are spared by the chemotherapeutic agent. 5. There is an increased incidence of malignancies in immunodeficient patients such as AIDS patients who are susceptible to Kaposi sarcoma and transplant patients who are susceptible to Epstein Barr virus (EBV)induced lymphoma. 6. Tumor-specific antibodies and T lymphocytes (detected in cytotoxicity and proliferative response assays) have been observed in patients with tumors. 7. The young and the old population have an increased incidence of tumors. These members of the population often have an immune system that is compromised. 8. Hosts can be specifically immunized against various types of tumors demonstrating tumor Ags can elicit an immune response. Tumor antigens Tumorigenesis may lead to expression of new antigens or alteration in existing antigens that are found on normal cells. These antigens may include membrane receptors, regulators of cell cycle and apoptosis, or molecules involved in signal transduction pathways. There are 2 main types of tumor antigens. 1. Tumor-specific transplantation antigens (TSTA) which are unique to tumor cells and not expressed on normal cells. They are responsible for rejection of the tumor. 2. Tumor associated transplantation antigens (TATA) that are expressed by tumor cells and normal cells. 1
Although chemical- , UV- or virus-induced tumors express neo-antigens, majority of the tumors are often weakly immunogenic or non-immunogenic. In most cases, tumor-specific transplantation Ags cannot be identified easily. Also, some of these antigens may be secreted while others include membrane-associated molecules. Tumor associated transplantation antigens (TATA) The majority of tumor Ags are the tumor associated transplantation antigens (TATA). They may be expressed at higher levels on tumor cells when compared to normal cells. Alternatively, they may be expressed only during development of cells and lost during adult life but re-expressed in tumors. These include the tumor-associated developmental Ags (TADA) and tumor-associated viral Ags (TAVA). Tumor-associated developmental Ags (TADA) or Onco-fetal antigens These include alpha-fetoprotein (AFP) and carcino-embryonic antigen (CEA) found secreted in the serum. AFP is found in patients with hepatocellular carcinoma whereas CEA is found in colon cancer. These are important in diagnosis. Virus-induced tumors: Viruses that cause tumors include DNA viruses: 1. Papova (papilloma, polyoma) viruses. Ex. Papilloma virus causes cervical cancer. 2. Hepatitis virus: Hepatitis B virus causes hepatocellular cancer. 3. Adenoviruses RNA viruses: Retroviruses: Human T-lymphotropic viruses (HTLV-I and HTLV-II) causes Adult T cell leukemia. Virus-induced tumors express tumor-associated viral Ags (TAVA). These are cell surface antigens that are distinct from antigens on the virion itself. However, these transplantation-associated viral Ags are shared by all tumors induced by the same virus, regardless of tissue origin of the tumor or animal in which the tumor exists. Chemically-induced tumors Chemically-induced tumors are different from virally-induced tumors in that they are extremely heterogeneous in their antigenic characteristics. Thus, any two tumors induced by the same chemical, even in the same animal, rarely share common tumor specific antigens. These unique antigens on chemically-induced tumors are referred to as tumor- specific transplantation antigens (TSTA). Syngeneic, Allogeneic and Xenogeneic Tumors: A tumor that grows in an animal strain will also grow in another animal belonging to the same inbred strain obtained by repeated brother-sister matings. These animals express the same MHC molecules and are referred to as syngeneic. However, most normal animal populations are allogeneic and have various MHC haplotypes. Thus, a tumor transferred from one animal to another animal belonging to an outbred strain is rejected because of the allo-MHC rather than the TSTA. A tumor transferred from an animal belonging to one species to another animal belonging to a different species is rapidly rejected because the animals are xenogeneic. Immune response to tumors: Evidence for immunity against malignancy comes mostly from experimental studies, wherein mice were immunized by administering irradiated tumor cells or following removal of a primary tumor challenged with the same live tumor. These animals were found to be resistant to rechallenge with the same live tumor. While Abs may develop against few cancers, cell-mediated immunity plays a critical role in tumor rejection. Thus, immunity can be transferred, in most cases, from an animal, in which a tumor has regressed, to a naive syngeneic recipient by administration of T lymphocytes. The T helper (Th) cells recognize the tumor Ags that may be shed from tumors and internalized, processed and presented in association with class II MHC on antigen 2
presenting cells. These Th cells when activated will produce cytokines. Thus, the Th cells provide help to B cells in Ab production. The cytokines such as IFN- may also activate macrophages to become tumoricidal. Furthermore, the Th cells also provide help to tumor-specific cytotoxic T cells (CTL) by inducing their proliferation and differentiation. The CTL recognize tumor Ags in the context of class I MHC and mediate tumor cell lysis. In tumors that exhibit decreased MHC Ags, natural killer (NK) cells are important in mediating tumor rejection. How tumors evade immune system: According to the Immune Surveillance Theory, cancer cells that arise in the body are eliminated by the immune system. However, due to impaired immune reactivity, the cancer cells escape destruction. Tumors evade immune recognition by several mechanisms. Some tumors may evade the immune system by secreting immunosuppressive molecules such as interleukin-10 (IL-10) or transforming growth factor-beta (TGF-) and others may induce regulatory cells particularly the CD4+CD25+ FoxP3+ T regulatory cells or myeloid derived suppressor cells (MDSC) which have both granulocyte and macrophage markers (Gr1+CD11b+). Also, some tumors may shed their antigens which in turn may interact and block antibodies and T cells from reacting with the tumor cells. Tumors may not express neo-antigens that are immunogenic or they may fail to express co-stimulatory molecules required for the activation of T cells. In addition, certain tumors are known to lack or be poor expressers of MHC antigen. Such tumors are however, susceptible to NK cell cytotoxicity. Another reason for failure of immune surveillance may be the fact that in the early development of a tumor, the amount of antigen may be too small to stimulate the immune system (low dose tolerance) or due to the rapid proliferation of malignant cells (high dose tolerance), the immune system is quickly overwhelmed. Tumor cells may express the death inducing ligand, FasL (CD95L) whereas the T cells express the death receptor, Fas (CD95), thereby leading to killing of the T cells. However, CTL have been shown to express FasL and some tumors may express Fas. Immunotherapy Immunotherapy has been used as a novel mode to treat cancer. Both active and passive means of stimulating the non-specific and specific immune system have been employed, in some cases with significant success. 1) Active Immunotherapy: Wherein the host actively participates in mounting an immune response a) Specific activation using vaccines: i) Hepatitis B vaccine useful against development of hepatocellular cancer. ii) Human Papilloma virus (HPV) vaccine (Gardasil) has been successfully used to prevent cervical cancers b) Nonspecific activation which results in stimulation of generalized immune response is achieved by immunization with: i) Bacillus Calmette-Guerin (BCG) mycobacteria. ii) Corynebacterium parvum These microbes lead to activation of macrophages which are tumoricidal. 2) Passive Immunotherapy: This involves transfer of preformed Abs, immune cells and other factors into the hosts. a) Specific: Preformed Abs or CTL directed against tumor Ags are used in the treatment of tumors i) Antibodies against tumor Ags (e.g. Abs against Her2/Neu for treatment of breast cancer) ii) Abs against interleukin-2 receptor (IL-2R) are used in the treatment of Human T lymphotropic virus (HTLV-1)-induced adult T cell leukemia as this virus infects T cells and leads to production of IL-2 that binds to IL-2R and induces the T cell proliferation. iii) Abs against CD20 expressed on all B cells are used in the treatment of non Hodgkins B cell lymphoma. 3
These Abs bind to tumor Ags on the cell surface and activate complement (C) to mediate tumor cell lysis. In addition, Fc receptor bearing cells such as NK cells, macrophages and granulocytes may bind to the Ag-Ab complexes on tumor cell surface and mediate tumor cell killing through Ab-dependent cell-mediated cytotoxicity. iv) Abs conjugated to toxins, radioisotopes and anti-cancer drugs have also been used. These enter the cells and inhibit protein synthesis because of the toxin. e.g. anti-CD20 conjugated to Pseudomonas toxin or ricin toxin has been used in the treatment of B cell tumors. There are several problems with the use of Abs (1) Abs are not efficient because the tumor Ags are associated with class I MHC Ags. (2) The tumors may shed Ag or Ag-Ab complexes. Thus, immune cells cannot mediate tumor destruction. (3) Some Abs may not be cytotoxic. (4) Abs may bind nonspecifically to immune cells expressing the Fc receptors which include NK cells, B cells, macrophages and granulocytes without binding to tumor cells. v) Dendritic cells pulsed with tumor Ags may be administered which can present tumor Ags in the context of class II MHC to tumor-specific Th cells. As tumor Ags are usually not known, tumor lysates are used. The Th cells may in turn produce cytokines which lead to development of CTL activity. On the other hand, the dendritic cells may be transfected with the gene for tumor Ags, in which case, the Ags will associate with the Class I MHC and elicit a CTL response.
b) Nonspecific: i) Adoptive Transfer of lymphocytes: (1) Lymphokine-activated killer (LAK) cells which are IL-2 activated T cells and NK cells can be used in the treatment of melanoma and renal cell carcinoma (2) Tumor-infiltrating lymphocytes (TIL) include T cells and NK cells. While the infiltrating NK cells will kill tumors nonspecifically, the CTL will be able to kill specific tumor targets. ii) Cytokines (1) Interleukin-2 (IL-2): Activates T cells/NK cells which express IL-2 receptors and leads to their proliferation. Used in the treatment of renal cell carcinoma and melanoma, (2) Interferon-alfa (IFN): Activates NK cell activity against tumors and also used in the treatment of Kaposi sarcoma, renal cell carcinoma and melanomas. (3) IFN-: ncreases class II MHC expression; used in the treatment of ovarian cancers. (4) Tumor necrosis factor (TNF)-: Kills tumor cells. (5) Granulocyte-macrophage colony stimulating factor (GM-CSF): Useful in overcoming neutropenia due to chemo- or radiation therapy iii) Cytokine gene transfected tumor cells may also be used which can activate T or LAK cells that can mediate anti-tumor immunity. Reading: Immunology By Male, Brostoff, Roth and Roitt 7th Edition Pages 401-419
Vous aimerez peut-être aussi
- Anatomy & Physiology: For Health Professions: An Interactive JourneyDocument60 pagesAnatomy & Physiology: For Health Professions: An Interactive JourneyEllani A RoldanPas encore d'évaluation
- Homeopathic Care, Don Hamilton DVM PDFDocument48 pagesHomeopathic Care, Don Hamilton DVM PDFBibek Sutradhar0% (1)
- Pediatric EndrocinologyDocument453 pagesPediatric Endrocinologyrayx323100% (1)
- Cancer ImmunologyDocument37 pagesCancer ImmunologyBeenish SarfrazPas encore d'évaluation
- Tumor ImmunologyDocument3 pagesTumor ImmunologyStaz Reiya KiraPas encore d'évaluation
- 3 CancerDocument47 pages3 Cancerkirubel getyePas encore d'évaluation
- Basic Life SupportDocument29 pagesBasic Life SupportRyan-Jay AbolenciaPas encore d'évaluation
- Psychological DisordersDocument21 pagesPsychological DisordersMark100% (2)
- Tumor ImmunityDocument16 pagesTumor ImmunityBeenish RazzaqPas encore d'évaluation
- 7 Tumor ImmunityDocument51 pages7 Tumor ImmunityNanda SalmasPas encore d'évaluation
- Otalgia & TinnitusDocument19 pagesOtalgia & Tinnitushonda matizPas encore d'évaluation
- Karibaldi Triastara Windy Juliandra M. ArsyiDocument37 pagesKaribaldi Triastara Windy Juliandra M. ArsyiPeri Hidayat100% (1)
- Visual ImpairmentDocument9 pagesVisual ImpairmentMeti Guda100% (1)
- Tumour Immunology PPT PayaliiDocument14 pagesTumour Immunology PPT PayaliisachinPas encore d'évaluation
- Mohammad Altamimi, MD, PHD Jordan UniversityDocument16 pagesMohammad Altamimi, MD, PHD Jordan UniversityDaniel AtiehPas encore d'évaluation
- Account Statement As of 13-06-2022 13:53:34 GMT +0530Document9 pagesAccount Statement As of 13-06-2022 13:53:34 GMT +053099manu99Pas encore d'évaluation
- MCN - P2 Post Test (Reviewer)Document3 pagesMCN - P2 Post Test (Reviewer)cianixPas encore d'évaluation
- Case Studies - Apollo Hospitals, DhakaDocument7 pagesCase Studies - Apollo Hospitals, Dhakasakil khan100% (1)
- University of Sulaimaniah: College of Dentistry Presentation:-Asked by Presented ByDocument61 pagesUniversity of Sulaimaniah: College of Dentistry Presentation:-Asked by Presented ByNina MoradPas encore d'évaluation
- Fast Facts: Managing immune-related Adverse Events in Oncology: Early recognition, prompt intervention, effective managementD'EverandFast Facts: Managing immune-related Adverse Events in Oncology: Early recognition, prompt intervention, effective managementPas encore d'évaluation
- Immune Response To TumorDocument14 pagesImmune Response To TumorFebrian Alfaro100% (1)
- Engorgement & Mastitis MM RH SJDocument18 pagesEngorgement & Mastitis MM RH SJbrown_chocolate87643Pas encore d'évaluation
- Antitumor Effector Mechanisms & Immune Surveillance: Imelda Salas LorenzoDocument11 pagesAntitumor Effector Mechanisms & Immune Surveillance: Imelda Salas LorenzoironPas encore d'évaluation
- Clinical Practice Guidelines - 2017Document54 pagesClinical Practice Guidelines - 2017Cem ÜnsalPas encore d'évaluation
- Mohammad Altamimi, MD, PHD Jordan UniversityDocument16 pagesMohammad Altamimi, MD, PHD Jordan UniversityDaniel AtiehPas encore d'évaluation
- Tumor ImmunologyDocument36 pagesTumor ImmunologyAmina DinarPas encore d'évaluation
- Invasion of ECM Degradation of ECMDocument8 pagesInvasion of ECM Degradation of ECMJezreel NicolasPas encore d'évaluation
- Immunity To TumorDocument38 pagesImmunity To TumorAaryan PatelPas encore d'évaluation
- Umor ImmunityDocument28 pagesUmor ImmunityGunjan sahuPas encore d'évaluation
- Tumor Immunology: ObjectivesDocument20 pagesTumor Immunology: ObjectivesMarl EstradaPas encore d'évaluation
- 17-Cancer and The Immune SystemDocument25 pages17-Cancer and The Immune SystemRami AlhilliPas encore d'évaluation
- Host Defence Mechanisms Against TumorsDocument7 pagesHost Defence Mechanisms Against TumorsHamam AmastrdamPas encore d'évaluation
- CancerDocument11 pagesCancerironPas encore d'évaluation
- Ecancermedicalscience 2014 Article 441Document15 pagesEcancermedicalscience 2014 Article 441YulianaPas encore d'évaluation
- Review Article: The Immune Response To Tumors As A Tool Toward ImmunotherapyDocument12 pagesReview Article: The Immune Response To Tumors As A Tool Toward ImmunotherapyFrontiersPas encore d'évaluation
- How Does The Immune System Recognize Tumor Cells As Foreign?Document4 pagesHow Does The Immune System Recognize Tumor Cells As Foreign?cfournier1982Pas encore d'évaluation
- Tumor Immunology ShowDocument42 pagesTumor Immunology Showreza8960Pas encore d'évaluation
- Cancer ImmunologyDocument27 pagesCancer ImmunologyMasrizal Dt.MangguangPas encore d'évaluation
- Tumor Immune Escape Mechanisms: Yi Ting Koh,, M. Luz García-Hernández,, and W. Martin KastDocument26 pagesTumor Immune Escape Mechanisms: Yi Ting Koh,, M. Luz García-Hernández,, and W. Martin KastTina HerreraPas encore d'évaluation
- Is Module 8Document26 pagesIs Module 8gladyskheyagamPas encore d'évaluation
- BMS4227 The Immune Response To Tumours 2020Document47 pagesBMS4227 The Immune Response To Tumours 2020Sandhya VivekanandPas encore d'évaluation
- Immuno TherapyDocument20 pagesImmuno TherapyAttis PhrygiaPas encore d'évaluation
- Immunotherapy in Uterine Cancers: January 2011Document9 pagesImmunotherapy in Uterine Cancers: January 2011Nurul Ulya RahimPas encore d'évaluation
- Host Defense Against TumorsDocument13 pagesHost Defense Against TumorsironPas encore d'évaluation
- Tumor Immunology: Ineffective in Eliminating Tumors or Preventing Their Growth. (3) Various Means May BeDocument5 pagesTumor Immunology: Ineffective in Eliminating Tumors or Preventing Their Growth. (3) Various Means May BeHillary Desiree RPas encore d'évaluation
- Immunity To TumorDocument52 pagesImmunity To TumorSurya indra FirdausPas encore d'évaluation
- Cellular Immunity: The Immune Response To Foreign Antigens Consists ofDocument8 pagesCellular Immunity: The Immune Response To Foreign Antigens Consists ofAnonymous dc9oF7H3tPas encore d'évaluation
- Tumor Immunity PDF1Document2 pagesTumor Immunity PDF1Shane FernandezPas encore d'évaluation
- CANCERDocument84 pagesCANCERhydrocodooniePas encore d'évaluation
- Chapter 10 - Immune Responses Against Tumors and TransplantsDocument11 pagesChapter 10 - Immune Responses Against Tumors and TransplantsFYMPas encore d'évaluation
- 3 Tumor ImmunologyDocument12 pages3 Tumor ImmunologyWard KhalidPas encore d'évaluation
- Lecture 13 Part 1 Tumuor ImmunologyDocument18 pagesLecture 13 Part 1 Tumuor Immunologygayathri132006Pas encore d'évaluation
- Cancer ImmunologyDocument31 pagesCancer ImmunologyAbdul FarooqPas encore d'évaluation
- Avances en Nuevas Estrategias de Vacunas para La Inmunoterapia y Prevención Del Cáncer JAY A. BERZOFSKY 2004Document11 pagesAvances en Nuevas Estrategias de Vacunas para La Inmunoterapia y Prevención Del Cáncer JAY A. BERZOFSKY 2004Ramiro J. Rodriguez GarciaPas encore d'évaluation
- Actualización de Inmunoterapia en CáncerDocument13 pagesActualización de Inmunoterapia en CáncerAli BelloPas encore d'évaluation
- Reviews: Systemic Immunity in CancerDocument15 pagesReviews: Systemic Immunity in Cancerliliana-contrerasPas encore d'évaluation
- 2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyDocument11 pages2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyCristian Felipe Sandoval QuiñonezPas encore d'évaluation
- Tumor ImmunologyDocument14 pagesTumor ImmunologyEdo RezaprasgaPas encore d'évaluation
- Weiner 1Document8 pagesWeiner 1Raúl ChoquePas encore d'évaluation
- 2.2. Cancer Immunotherapy Co-Stimulatory Agonists and Co-Inhibitory AntagonistsDocument11 pages2.2. Cancer Immunotherapy Co-Stimulatory Agonists and Co-Inhibitory AntagonistsDiego EskinaziPas encore d'évaluation
- Tumor Antigen: 1 Mechanism of Tumor AntigenesisDocument3 pagesTumor Antigen: 1 Mechanism of Tumor AntigenesisZiedTrikiPas encore d'évaluation
- Blood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDocument23 pagesBlood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDaniel SutantoPas encore d'évaluation
- Wedekind2018 Article PediatricCancerImmunotherapyOpDocument14 pagesWedekind2018 Article PediatricCancerImmunotherapyOpKAREN JAZMIN RUIZ MONROYPas encore d'évaluation
- (24508608 - Journal of Veterinary Research) Mechanisms of Tumour Escape From Immune SurveillanceDocument8 pages(24508608 - Journal of Veterinary Research) Mechanisms of Tumour Escape From Immune Surveillancekalppena naiduPas encore d'évaluation
- Cancer Immunosurveillance: AngiogenesisDocument2 pagesCancer Immunosurveillance: AngiogenesisBrenda Bastos LevanoPas encore d'évaluation
- ImmunoteraphyDocument28 pagesImmunoteraphyMagnusPas encore d'évaluation
- Cancer Ii - 230522 - 095514Document30 pagesCancer Ii - 230522 - 095514Tharuka ChandrasiriPas encore d'évaluation
- 3 Tumor ImunotherapyDocument60 pages3 Tumor ImunotherapyXu FanPas encore d'évaluation
- Tumor Immunology BMS 3.1Document38 pagesTumor Immunology BMS 3.1Kato CalebPas encore d'évaluation
- Cancer VaccinesDocument80 pagesCancer VaccinesKishoreChandraKoradaPas encore d'évaluation
- Fast Facts: Managing Immune-Related Adverse Events in OncologyD'EverandFast Facts: Managing Immune-Related Adverse Events in OncologyPas encore d'évaluation
- TFT NotesDocument13 pagesTFT Notes99manu99Pas encore d'évaluation
- CricDocument9 pagesCric99manu99Pas encore d'évaluation
- Presentation 1 HDocument4 pagesPresentation 1 H99manu99Pas encore d'évaluation
- Skip To Navigation Top Events World Cup Match Delayed by RainDocument21 pagesSkip To Navigation Top Events World Cup Match Delayed by Rain99manu99Pas encore d'évaluation
- People AppealDocument3 pagesPeople Appeal99manu99Pas encore d'évaluation
- EucephalusDocument1 pageEucephalus99manu99Pas encore d'évaluation
- William RoseDocument21 pagesWilliam Rose99manu99Pas encore d'évaluation
- HeinzDocument8 pagesHeinz99manu99Pas encore d'évaluation
- Danske SpilDocument1 pageDanske Spil99manu99Pas encore d'évaluation
- OberleutnantDocument1 pageOberleutnant99manu99Pas encore d'évaluation
- Ariana Alyse BerlinDocument1 pageAriana Alyse Berlin99manu99Pas encore d'évaluation
- HeinzDocument36 pagesHeinz99manu99Pas encore d'évaluation
- Rando AyamineDocument1 pageRando Ayamine99manu99Pas encore d'évaluation
- RichardDocument1 pageRichard99manu99Pas encore d'évaluation
- Solomon AbigdorDocument1 pageSolomon Abigdor99manu99Pas encore d'évaluation
- Mid ClubDocument1 pageMid Club99manu99Pas encore d'évaluation
- WMTADocument1 pageWMTA99manu99Pas encore d'évaluation
- Michael CDocument1 pageMichael C99manu99Pas encore d'évaluation
- Table TingDocument1 pageTable Ting99manu99Pas encore d'évaluation
- Hyacienth Diva MantalabaDocument1 pageHyacienth Diva Mantalaba99manu99Pas encore d'évaluation
- Charles RojzmanDocument1 pageCharles Rojzman99manu99Pas encore d'évaluation
- Jim JonesDocument1 pageJim Jones99manu99Pas encore d'évaluation
- Shrub Wheatbelt Western Australia: Grevillea Calliantha Is ADocument1 pageShrub Wheatbelt Western Australia: Grevillea Calliantha Is A99manu99Pas encore d'évaluation
- OberleutnantDocument1 pageOberleutnant99manu99Pas encore d'évaluation
- WaittDocument4 pagesWaitt99manu99Pas encore d'évaluation
- Web Page 2nd List of 5565Document31 pagesWeb Page 2nd List of 556599manu99Pas encore d'évaluation
- Press Note - HPAS (PRLM) Examination-2014Document2 pagesPress Note - HPAS (PRLM) Examination-201499manu99Pas encore d'évaluation
- AattDocument5 pagesAatt99manu99Pas encore d'évaluation
- 01 - Properties & SafetyDocument50 pages01 - Properties & SafetyKaled AmerPas encore d'évaluation
- Assessing Female Genitalia, Anus, and RectumDocument27 pagesAssessing Female Genitalia, Anus, and RectumCrestyl Faye R. CagatanPas encore d'évaluation
- Superficial Corneal Injury and Foreign BodyDocument1 pageSuperficial Corneal Injury and Foreign BodyandinurulpratiwiPas encore d'évaluation
- Ankle SprainDocument3 pagesAnkle SpraindrakbarbabPas encore d'évaluation
- Andrew Eastman Resume 3Document2 pagesAndrew Eastman Resume 3api-281509868Pas encore d'évaluation
- Labor Monitoring RecordDocument4 pagesLabor Monitoring RecordFrancis PeterosPas encore d'évaluation
- Intracavernosal Injection InformationDocument4 pagesIntracavernosal Injection InformationJason ArbogastPas encore d'évaluation
- Derma OLUWOLE OLUMODEJIDocument13 pagesDerma OLUWOLE OLUMODEJIbrightagbotuiPas encore d'évaluation
- IDSP BelgaumDocument36 pagesIDSP BelgaumJ Nuchin100% (1)
- Segmented Arch or Continuous Arch Technique? A Rational ApproachDocument1 pageSegmented Arch or Continuous Arch Technique? A Rational ApproachSantos TicaPas encore d'évaluation
- Resume - Asghar Nazerian JaziDocument2 pagesResume - Asghar Nazerian JaziSepideh MirzaeiPas encore d'évaluation
- Laws On Notifiable DiseaseDocument43 pagesLaws On Notifiable DiseaseKenji ToleroPas encore d'évaluation
- IMF Screw Set. For Temporary, Peri Operative Stabilisation of The Occlusion in AdultsDocument12 pagesIMF Screw Set. For Temporary, Peri Operative Stabilisation of The Occlusion in AdultsAnonymous LnWIBo1GPas encore d'évaluation
- Amboss CACES-EcuadorDocument44 pagesAmboss CACES-EcuadorStorage Liz0% (1)
- HSG PresentationDocument18 pagesHSG Presentationashikin92Pas encore d'évaluation
- Composite Hemangioendothelioma An Unusual Presentation of A Rare Vascular TumorDocument5 pagesComposite Hemangioendothelioma An Unusual Presentation of A Rare Vascular TumorTian Nopita SariPas encore d'évaluation
- CH 29Document39 pagesCH 29Jann Zaniel Allayne RiPas encore d'évaluation
- Avenir Hip System Surgical TechniqueDocument16 pagesAvenir Hip System Surgical Techniquesuraj mahadikPas encore d'évaluation
- Epidemiology, Prevention and Control of Dengue: DR Tahira JaffarDocument36 pagesEpidemiology, Prevention and Control of Dengue: DR Tahira JaffarRaza UzuPas encore d'évaluation
- BioFire RP2 1 RP2 1plus Control Panel M441Document4 pagesBioFire RP2 1 RP2 1plus Control Panel M441Cecil James BuguisPas encore d'évaluation